
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Med. , 05 March 2025
Sec. Family Medicine and Primary Care
Volume 12 - 2025 | https://doi.org/10.3389/fmed.2025.1501918
This article is part of the Research Topic The Increasing Relevance of Traditional Medicine Systems for the Primary Health Care Sector and General Practice: Global Research Perspectives – Volume II View all 9 articles
 Runbing Xu1†
Runbing Xu1† Yanan Sun2†
Yanan Sun2† Yifei Liu3†
Yifei Liu3† Jiajun Pan1
Jiajun Pan1 Yingying Han1
Yingying Han1 Xinyu Zhang4
Xinyu Zhang4 Hequn Zhao1
Hequn Zhao1 Mengfei Li1
Mengfei Li1 Yu Wu1
Yu Wu1 Changhe Yu5*
Changhe Yu5* Miao Jiang1,6*
Miao Jiang1,6*Background: The complementary role of Traditional Chinese Medicine (TCM) in cancer management has been widely acknowledged. However, its implementation continues to face numerous challenges. Identifying and elucidating the factors that influence the integration of TCM into cancer therapy is essential. Developing effective implementation strategies is crucial to transitioning from theoretical evidence to practical application.
Methods: A total of nine databases were systematically searched from their inception until 1 October 2023. The review includes qualitative and mixed-method studies examining the attitudes and perceptions of patients and healthcare providers toward the use of TCM in cancer treatment. The studies included were evaluated using a quality assessment tool. An appropriate model or framework was to identify potential facilitators and impediments affecting TCM implementation. Based on the identified barriers, potential behavior change interventions were subsequently developed.
Results: A total of 39 studies are included in the review, comprising 31 qualitative and eight mixed-methods studies. The quality of these studies is acceptable. Key barriers to the implementation of TCM were identified as follows: insufficient knowledge and experience in TCM, neglect of details in doctor-patient communication, limited number of specialists, lack of funding, and absence of a multidisciplinary collaborative atmosphere. In response to these barriers, we recommend improving structured referral pathways, developing a structured communication manual, and other targeted interventions to enhance the integration of TCM in cancer care.
Conclusion: This study identifies 48 factors that influence the implementation of TCM and tentatively proposes a series of intervention strategies. Future research should focus on localized empirical studies of factors and strategies in different healthcare settings.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=421822, identifier CRD42023421822.
Traditional Chinese Medicine (TCM), including diverse modalities such as herbal medicines, dietary therapy, acupuncture, Qigong, and therapeutic massage, constitutes a critical component of Traditional, Complementary, and Integrative Medicine (TCI) (1, 2). Recently, the role of TCM in integrative oncology (IO) care has garnered increasing attention (3). Certain TCM therapies, such as acupuncture, acupressure, and Qigong, have been supported by a range of clinical evidence for their positive effects in cancer supportive care (4–6), particularly in alleviating cancer-related symptoms, reducing treatment side effects, and improving quality of life (7). Authoritative clinical guidelines also recommend these therapies for reducing the adverse effects of conventional treatments. For example, the ASCO-SIO guidelines strongly recommend low- to moderate-intensity Tai Chi and Qigong for cancer-related fatigue (8). In contrast, the ESO-ESMO guidelines endorse acupuncture for managing menopausal hot flashes, chemotherapy-induced nausea, vomiting, and fatigue (9). Moreover, an increasing body of research provides preliminary evidence for the role of herbal medicine in enhancing the efficacy of conventional cancer treatments. For instance, a study involving 1,052 patients with hepatocellular carcinoma found that those receiving adjunctive herbal therapy had significantly higher overall survival rates at 1, 3, and 5 years than compared to those receiving conventional treatment alone (10). Another randomized, double-blind, placebo-controlled trial involving 354 EGFR mutation-positive advanced lung adenocarcinoma patients showed that the combination of herbal medicine and EGFR-TKI treatment significantly improved median progression-free survival (PFS) compared to EGFR-TKI monotherapy (11).
Although the evidence above aforementioned evidence indicates the unique role of TCM in adjunctive cancer care, its actual clinical application remains insufficient. One study showed that only 33.3% of American cancer patients used TCI in the past year, with acupuncture at just 2.0%, compared to 64% TCM utilization among Chinese cancer patients (12, 13). This disparity reflects differing efficacy perceptions, cultural influences, and challenges in promoting TCM across patients, healthcare providers (HCPs), healthcare systems, and society. Some original studies have also identified barriers to the clinical practice of TCM in oncology, such as low awareness among oncologists (14), limited related discussions with patients (15), and inadequate insurance coverage (16). However, no comprehensive analysis has addressed the facilitators and barriers to implementing TCM in integrated cancer care.
To fill this gap, this study analyzes the literature on patient and HCP attitudes toward TCM in cancer care, summarizing key facilitators and barriers to its implementation. Recognizing that stakeholder perceptions influence intervention adoption (17), we propose general intervention strategies based on an implementation science framework to promote the application of TCM in supportive cancer care.
This study integrates evidence from published qualitative studies through qualitative meta-synthesis; the PROSPERO registration number is CRD42023421822. This study did not involve ethical approval and was reported adhering to the PRISMA guideline (18) (Supplementary Table 1).
Considering the geographical nature of TCM, we mainly searched English and Chinese databases, and we searched a total of nine databases, including five English databases: Cochrane, PubMed, Embase, Web of Science, CINAHL, and four Chinese data China National Knowledge Infrastructure (CNKI), Wanfang Medicine Online, Chinese Scientific Journal Database (VIP) and SinoMed. The search was conducted from the database construction to 1 October 2023. The search strategy is described in the Supplementary Table 2.
The phenomenon of interest was the attitudes of cancer patients, their dependent caregivers, and Health Professionals toward TCM for cancer treatment, broadly including views, opinions, and experiences. We developed the following detailed inclusion-exclusion criteria (Table 1).
The two authors carried out the screening process independently (Xu and Sun), and disputes were resolved by a third party (Jiang). Literature screening was performed using Endnote X9, independently by two authors (Zhang and Pan), with initial screening by title and abstract, followed by reading the full text to determine the final inclusion of articles. The differences in the summary of results were finalized by a third party (Yu). Information was extracted from the included articles using Excel based on the study purpose, including (1) general characteristics, (2) characteristics of the study population, (3) research objectives, (4) research design and theory, (5) data collection methods and analysis methods, and (6) final themes and conclusions.
Two authors (Sun and Liu) independently assessed the methodology of the articles included in this study through a 10-item Critical Appraisal Skills Program (CASP) (19), and dissent was agreed upon through discussion with (Han). The CASP tool consists of 10 terms (see Supplementary Table 3), with entry scores of 0-No, 0.5-Can’t Tell, and 1-Yes, which allows for a complete assessment of the rigor, relevance, and reliability of the study (20, 21). The quality assessment does not exclude any study but only aims to increase research transparency.
To achieve the research goals, this study applied the “best-fit” framework synthesis method (22) and thematic synthesis (23) for data integration and analysis. The process, conducted by four researchers, followed a sequential combination of deductive and inductive approaches: (1) A priori framework selection: Based on similar studies identifying behavioral barriers and facilitators (24–26), the Theoretical Domains Framework (TDF) (27) and the Capability-Opportunity-Motivation-Behaviour (COM-B) (28) model were selected as the a priori frameworks for this study. TDF categorizes behavioral determinants into 14 domains, addressing the complexity of implementing TCM in oncology care, while COM-B simplifies this process by mapping determinants into three key components: Capability, Opportunity, and Motivation. These frameworks provide a comprehensive approach for analyzing the factors influencing the application of TCM in cancer care; (2) Line-by-line coding: Extracted barrier and facilitator data from the literature through line-by-line coding; (3) Code aggregation: Categorized and summarized codes to identify factors influencing TCM use in oncology care; (4) Mapping and classification: Mapped barriers and facilitators to COM-B components and TDF domains, with unmapped factors marked as potential new themes; (5) Theme extraction and framework refinement: Synthesized factors into theme labels using thematic analysis, extending the TDF framework to include unmatched theme. The differences were resolved through team consensus, and one author (Li) conducted the final code review.
A total of 4,525 articles were retrieved, with 39 studies included: 31 qualitative and eight mixed-methods (see Figure 1 for the PRISMA flowchart). These studies were conducted in nine countries and regions, mostly China, United States, and United Kingdom (Figure 2). A total of 849 individuals were involved, including 813 patients and 36 health professionals. Key therapeutic modalities included acupuncture, herbal medicine, Qi Gong, TCM dietary therapy, and massage. Western countries focused on non-drug therapies, while East Asia emphasized comprehensive TCM approaches. Data collection relied on interviews and open-ended questionnaires, with analysis using content, thematic, and grounded theory methods. The characteristics of the included literature are shown in the Supplementary Table 4.
The methodological evaluation using the CASP tool is shown in Table 2. The results indicated that majority of the studies (n = 28, 71.8%) met at least the 8/10 criteria, so the evidence was considered credible. Most studies (n = 33, 84.6%) provided the necessary elaboration on data analysis, while some studies (n = 24, 61.5%) missed reporting the researcher-participant relationship. In addition, few studies discussed how the researcher responded to problems during data collection.
We summarized enablers and barriers to using TCM in cancer care from patients’ and HCPs’ perspectives, aligned with COM-B and TDF. Patients identified 28 facilitators and 10 barriers across capability, motivation, opportunity components, and 13 TDF domains. HCPs noted fewer factors: one facilitator and nine barriers. No new themes emerged that could not be categorized within the existing frameworks (Details in Figure 3 and the Supplementary Table 5).
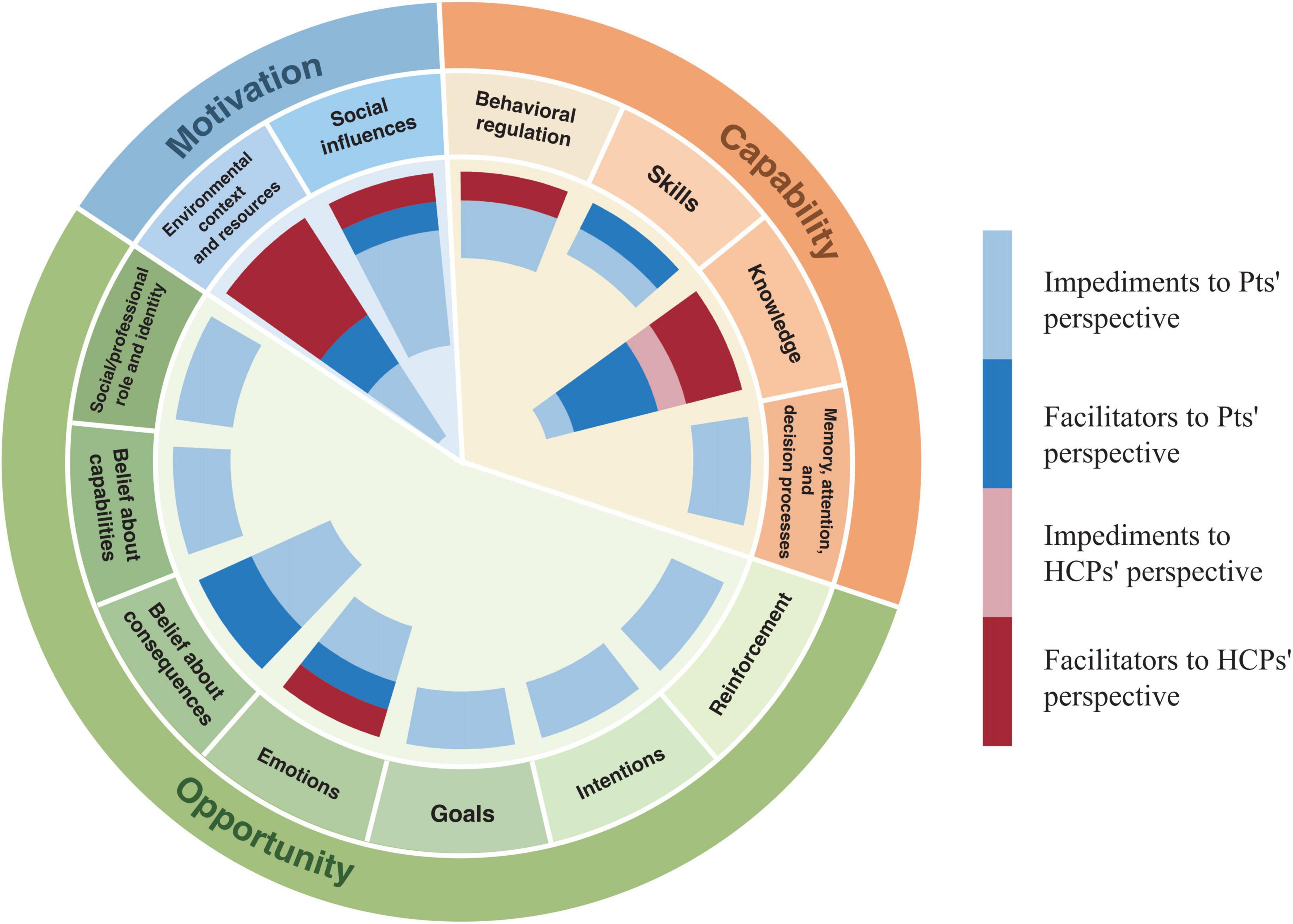
Figure 3. Frequency of impact factors mapped to Capability-Opportunity-Motivation-Behaviour (COM-B) and Theoretical Domains Framework (TDF) frameworks.
Capability is defined as the physical and mental abilities that affect the use of TCM by cancer patients and HCPs (28, 29). A total of 10 patients’ perspective themes based on the capability component were generated in this study, with six facilitating and four impeding themes, four HCPs’ perspective themes, one facilitating and three impeding themes.
For patients, the ability to understand and process information related to TCM and the self-management of health plays a critical role in facilitating behavioral choices. Specifically, patients can obtain information about TCM through multiple channels, including its benefits in enhancing the efficacy of conventional treatments (30, 31), reducing side effects (30–42), improving mental health (32, 33, 35, 39, 40, 42–45), enhancing well-being and coping (30, 32, 33, 35, 41–48). Through the evaluation and assessment of the above information, patients may be more likely to choose TCM as a supportive therapy in tumor treatment (30–34, 42, 49–51). Additionally, by practicing TCM self-management skills in daily life, such as acupressure (46, 51), auricular pressure (52), and dietary therapy (35), patients can more effectively manage health issues and improve treatment adherence, ultimately increasing the likelihood of choosing TCM therapies.
Moreover, TCM therapy, rooted in traditional Chinese culture, adopts a holistic perspective that views health as an interconnected whole and emphasizes balance in body, mind, and spirit (40, 41). While addressing physical discomfort, it also focuses on the regulation and management of emotions and stress (33, 50). Additionally, by fostering an understanding of healthy behaviors and lifestyle changes, TCM enhances patients’ health awareness and their sense of self-efficacy in pursuing a healthier lifestyle (41). This process strengthens their psychological capability and indirectly promotes the adoption of TCM treatments.
The barriers influencing patients’ decision to adopt TCM therapies can be mapped to two domains: knowledge and skills. In the knowledge domain, barriers include a lack of understanding of existing efficacy evidence, as well as doubts regarding the mechanism of action (53), effectiveness (30, 33, 38, 49, 50), duration of therapeutic benefits, and safety of the therapies (42). Furthermore, information asymmetry between patients and healthcare providers is another potential barrier, primarily reflected in insufficient patient education by doctors regarding treatment frequency and precautions (36, 38, 48, 51, 54). In the domain of skills, patients found it challenging to locate TCM physicians with oncology expertise, which hinders their choices (55).
From HCP’s perspective, the potential factors associated with capability can be mapped to the knowledge and behavioral modification domains. In terms of knowledge, recognizing the benefits of TCM as a supportive therapy in clinical practice can encourage behavioral choices (32, 53, 55–59). Conversely insufficient evidence on efficacy, a lack of evidence-based data, and limited access to reliable information significantly hinder behavioral choices (32, 55). Behavioral regulation-related impediments involve a lack of interdisciplinary communication (32), which greatly hampers the likelihood that oncologists and physicians will be able to understand the mechanisms, and effectiveness of TCM.
Motivation refers to the cognitive processes that stimulate and guide the selection of TCM in cancer care (28). It can be categorized as reflective and automatic motivation, which can map to multiple domains in the TDF (28, 29, 60). A total of 18 patients’ perspective themes were generated in this study, with 16 facilitating themes and three hindering themes; one hindering theme from the HCPs’ perspective was related to the domain of emotions, and no relevant facilitating themes were found.
Key factors influencing patients’ choice of TCM include positive expectations of its supportive therapeutic effects (33–35, 39–42, 44, 50, 53, 54, 56), negative emotions regarding the side effects of conventional treatments (31, 33, 39, 44, 47, 49, 61, 62), emotional distress related to the disease (30, 40, 42, 44, 47, 50, 55, 59, 63), the pursuit of integrated TCM and conventional therapies (31, 33, 39, 41, 42, 44, 51, 55, 56, 61–64), and behavioral reinforcement from positive treatment experience (40, 46, 53, 62, 63). Additionally, cultural beliefs (31, 48, 51, 56, 63, 65), trust in the authority of practitioners (34, 62, 66), and the desire for a safer medical environment in resource-limited settings (65) play significant roles. Notably, in terms of intention, minority of patients view TCM as a potential alternative therapy, believing it can directly treat cancer by reducing tumor size, with some even claiming it cured their primary or metastatic lesions (34, 56, 63). However, such subjective views should be interpreted with caution, as they lack robust clinical evidence and may be influenced by individual experiences or cognitive bias. Finally, patients’ pursuit of control over their illness and a desire for self-help further drive the choice of TCM in cancer care (41, 44, 55).
Factors limiting patients’ choice of TCM include distrust in its treatment outcomes (32, 37, 38, 42, 51, 54, 65), and concerns about the quality and safety of the products associated with herbal medicines (35, 42, 44, 48). Negative emotions associated with the treatment process, such as needle phobia (32, 33, 36), shame from body exposure (33, 40), nausea and discomfort after consuming herbal medicines (31, 33, 35, 50), and fear triggered by the treatment environment (33), decrease the likelihood of patients choosing TCM.
Under motivation, the main barrier to HCP behavior is patients’ discomfort with TCM use (59).
Opportunity refers to external factors influencing the use of TCM in cancer care by patients and HCPs, categorized into social and physical opportunities (28). A total of 10 patients’ perspective themes based on the opportunity component were generated in this study, including seven facilitating themes, three hindering themes, and five themes from the HCPs’ perspective, all hindering factors.
From the patients’ perspective, key facilitators within the social influence cluster include positive influences from significant others, such as family members, colleagues, and doctors (30, 32, 35, 41, 42, 44, 49, 51, 52, 56, 62–65), the media (32, 49, 63, 64), and ward-mates (40, 43, 47, 50, 56, 67). Studies indicate that patients immersed in positive doctor-patient relationships, such as through listening (30, 32, 40, 41, 43, 45, 50, 51, 62, 64, 66), encouragement (39), and support (32, 34, 39, 44, 50, 51, 62, 67), play an important role in decision-making behaviors. Facilitating factors related to environmental context and resources include a comfortable treatment environment (40, 45), the authority of the clinic environment (65), economic feasibility and policy support (31, 34, 36, 41, 55, 56) (e.g., health insurance, health care policy, etc.). Three potential barriers include oncologists’ negative attitudes toward TCM (36, 41, 42, 44, 56, 62), false advertising (30), and inadequate medical resources (e.g., high treatment and transportation costs, long treatment duration, and excessive waiting times) (30, 32, 33, 36, 40–42, 44, 49, 52, 54–56, 59, 61, 63, 66).
From the perspective of healthcare professionals (HCPs), similar to patients’ views, the main barriers include oncologists’ negative attitudes toward TCM (32, 56) and the limited healthcare budgets (55, 56). Furthermore, TCM experts emphasized that the absence of cross-disciplinary communication with oncologists impedes their comprehension of the efficacy and safety of TCM (32), thereby indirectly influencing the adoption of TCM treatments.
This subgroup analysis of eight TCM therapies shows that the overall results remain robust despite minor variations due to intervention characteristics, with three facilitating factors and six barriers varying across interventions (Supplementary Table 6).
Among facilitating factors, HCPs and patients recognize TCM’s role in supportive cancer care and its position as an adjunct therapy. Some doctors also use anticancer herbs to enhance supportive effects, such as inhibiting tumor growth and metastasis (68). In contrast, some patients may view herbal therapy as an alternative to conventional treatment (34, 63). TCM interventions with self-care characteristics exhibit distinct advantages: acupressure is simple to learn and easy to apply (46); non-prescribed functional herbal products are available in various forms (e.g., tablets, teas, foods) and are easily accessible (35); dynamic therapies in mind-body practices (e.g., Qigong, Tai Chi) enhance physical function at appropriate intensity levels (35).
Regarding barriers, different TCM models present unique challenges. Regarding the perception of TCM efficacy and safety, some patients consider acupuncture may stimulate tumor growth (56) and are uncertain about its long-term efficacy (37, 38). In herbal therapy, both doctors and patients express concerns about the potential risks of herb-drug interactions (48, 68). In terms of economic burden, acupuncture increases costs due to its treatment frequency and duration (40, 61). In comparison, the high prices of standard herbal products, such as Lingzhi (Ganoderma lucidum) powder, add to the financial strain (44, 56). Negative experiences with TCM include needle phobia (32, 33, 36), and body exposure (39, 58) in acupuncture, pain and discomfort in acupressure (46, 51), unpleasant taste in herbal medicine and supplements (35, 63), and noise perception in Five Elements music therapy within mind-body therapies (31). Furthermore, unique barriers to non-prescribed functional herbal products include deceptive advertising (30), concerns about product transparency (35, 48), and lack of usage guidance (35, 48, 51).
Limited research on herbal footbath and moxibustion identified no distinct facilitating or barrier factors for these modalities. Therefore, this subgroup analysis highlights the diverse characteristics of TCM interventions in supportive cancer care, emphasizing their potential benefits and challenges in clinical application.
This study systematically reviewed 39 qualitative studies exploring using single or multiple TCM therapies as supportive care in cancer management. As such, we analyzed the enablers and barriers influencing healthcare providers’ and patients’ choices of TCM. Although guidelines and clinical research supporting TCM as a complementary therapy in oncology have increased in recent years, its implementation barriers and practical challenges in real-world clinical settings remain underexplored. To our knowledge, this is the first systematic review to specifically address the implementation factors influencing the use of TCM in oncology. This study also represents a critical first step in bridging this pervasive implementation gap. Furthermore, we propose a series of theory-based behavioral interventions to address these challenges. Importantly, the factors and interventions identified in this study can guide clinicians and policymakers in adapting integrated management strategies and allocating resources to enhance the well-being of cancer patients.
From the included studies, Western countries focus more on non-pharmacological TCM therapies such as acupuncture, Qigong, and massage. In contrast, research in Asian countries, particularly China, is more diverse, significantly emphasizing herbal treatment. This disparity is closely linked to the cultural and healthcare system differences between East and West. For example, acupuncture has been integrated into the healthcare systems of some Western countries (69). However, due to strict Good Manufacturing Practice (GMP) regulations in Western countries (70), issues related to the quality, purity, and standardization of herbal medicine remain unresolved. Consequently, research in the West often centers on single herbs and their active components, resulting in lower clinical use and research frequency compared to Asian countries. Unfortunately, our studies include participants from diverse age groups and disease backgrounds, challenging traditional stereotypes of TCM users and indicating broader cultural acceptance (71).
Our study indicates that the lack of evidence-based data and the cognitive gap between HCPs and patients are significant barriers to integrating TCM into cancer care. This aligns with challenges commonly observed in implementing other complementary and alternative therapies (72).
Evidence gaps are primarily reflected in the following areas: (1) Lack of research and standardized assessment of symptom clusters: Cancer patients often experience interrelated symptoms, collectively referred to as “symptom clusters,” sharing common mechanisms or pathways (44). Multiple studies included in this research suggest that TCM offers effective interventions for managing symptom clusters (53). However, standardized methods for measuring these clusters remain lacking. Future studies should focus on developing precise and consistent outcome measures to better evaluate the dynamic changes and treatment effects of symptom clusters (73); (2) Incomplete research on herbal toxicity and safety: There are notable differences in how healthcare professionals perceive the safety of herbal medicines. Oncologists, in particular, express caution regarding potential herb-drug interactions (HDIs) when herbal treatments are combined with chemotherapy or other conventional therapies (74). As such, they often cite concerns about compromised efficacy or increased toxicity. Moreover, the hepatic and renal toxicity of herbal medicines requires further investigation (75); (3) Insufficient clinical evidence for direct anti-tumor effects of herbal medicines: Although some TCM practitioners use specific herbal medicines for their purported anticancer effects (68), laboratory and preclinical studies have demonstrated anti-tumor activity in certain herbs (e.g., Astragalus) (13). However, high-quality RCTs are lacking to validate their clinical efficacy and identify appropriate patient populations; (4) Limited evidence on the long-term effectiveness of interventions: Subgroup analyses reveal that some patients remain skeptical about the long-term efficacy of acupuncture (38). Consequently, current evidence on the sustained benefits of acupuncture in cancer management is inconsistent (4). Future research should prioritize well-designed, long-term RCTs to provide robust evidence for their long-term efficacy.
The cognitive gap is primarily reflected in limited knowledge of key areas, including cancer biology, the scope and efficacy of TCM treatments, mechanisms of action, safety, and the optimal timing for integration into conventional cancer care. From the perspective of HCPs, concerns include doubts about the quality of evidence, a disconnect between research findings and clinical practice, and cross-cultural differences in understanding. Additionally, TCM practitioners may lack expertise in oncology and herbal pharmacology. For instance, some rely on traditional knowledge and clinical experience to prescribe herbs, such as using phytoestrogen-containing Yin-tonifying herbs for estrogen-positive breast cancer patients, as reported in certain studies (68).
Despite systematic reviews supporting the efficacy and safety of TCM in IO, the translating this evidence into practice faces several barriers. These include: (1) Trial design based on syndrome differentiation: TCM emphasizes individualized treatment based on syndrome differentiation, which introduces subjectivity in defining inclusion criteria, intervention, and outcome measures in RCTs (76). While this approach highlights TCM’s unique ability to address patients’ symptoms and conditions dynamically, it also demands higher standards of training and quality control, potentially compromising the reliability and clinical applicability of results; (2) Limited representativeness of populations: Most TCM research is conducted in East Asia, with culturally homogeneous populations, limiting the generalizability of findings to diverse settings and populations; and (3) Lack of effective evidence network collaboration: Evidence networks play an important role in connecting researchers, policymakers, and practitioners to facilitate the generation, dissemination, and application of evidence to inform decisions (77). However, the absence of a structured evidence network in the TCM field hinders the global dissemination and application of TCM research findings.
In Integrative Cancer Care (ICC), combining biomedical treatments with TCM demonstrates notable complementary strengths. Biomedical treatments are disease-centered care, focusing on tumor control and clinical outcomes. In contrast, TCM adopts patient-centered care, prioritizing holistic health, psychological support, and quality of life. Thus, this synergistic model provides a valuable framework for optimizing cancer care and improving patient outcomes, quality of life, and overall care experiences (78).
In patient-centered care models, Shared Decision Making (SDM) has garnered increasing attention. SDM emphasizes providing evidence-based, comprehensive recommendations while respecting patients’ preferences, beliefs, and priorities, enabling healthcare professionals and patients to collaboratively develop personalized treatment plans (79). This approach not only reduces decision-making conflicts but also enhances patients’ engagement and trust in their treatment. Our study found that the application of SDM demonstrates significant advantages in real-world TCM clinical practice. The “patient-centered” philosophy of TCM aligns closely with the core objectives of SDM, fostering a sense of involvement in decision-making (80). For instance, prioritizing patients’ most pressing symptoms and incorporating their preferences in selecting herbal formulations further underscores TCM’s personalized approach, improving the overall care experience.
Moreover, our research indicated that in this patient-centered model, patients often report that a supportive environment, active listening by doctors, and therapeutic alliance play an important role in psychological well-being. This relationship improves mental health and promotes holistic recovery, enhancing the quality of care (32, 51). Interestingly, from the physicians’ perspective, trust-based patient-provider relationships and patient-centered communication are tools to encourage patients to express their needs and disclose health issues (58). Like other chronic disease management settings, both doctors and patients emphasize the importance of building long-term trust to improve clinical outcomes and ensure adequate care (81).
However, despite these benefits, integrating TCM into integrative cancer care poses challenges, mainly due to differences in treatment models and the lack of interdisciplinary communication. Notably, some patients in our included studies reported withholding information about their use of TCM due to perceived negative attitudes from physicians. Studies indicate that approximately 29.3% of patients in the United States do not disclose their use of complementary and alternative medicine (CAM) to their doctors (12). This lack of communication hinders the proper integration of TCM with conventional therapies and negatively impacts optimal medical decision-making.
To advance the integration of TCM into IO services, this study identified potential strategies to address the implementation barriers. These barriers were mapped to eight of the 14 TDF domains, highlighting the multifaceted nature of obstacles to TCM adoption. Using the Behavior Change Wheel (BCW) (82) and Behavior Change Techniques (BCTs) (60), targeted interventions were designed to address key implementation challenges, as detailed in Table 3.
Through the “education” intervention function, evidence-based knowledge, guidelines, and research on TCM can be disseminated via various media channels, including online learning platforms, patient guidelines, educational brochures, and courses (83). Importantly users should critically evaluate online information, as research shows most online discussions about CAM are commercially and potentially misleading (84).
To overcome the challenge of limited evidence and low utilization of TCM guidelines, we propose systematic improvements through the intervention functions of “Enablement” and “Environmental restructuring.” First, conducting more high-quality TCM clinical trials is essential to supplement existing evidence for clinical practice. Second, standardized TCM utilization and risk management tools should be developed, drawing on examples such as the questionnaire tool by Shalgouny et al. (72). Finally, existing guideline implementation frameworks [e.g., Knowledge-to-Action framework (85), Guideline Implementability Decision Excellence Model (86)] can be utilized to systematically analyze barriers in diverse implementation contexts and design tailored solutions.
Establishing a multidisciplinary environment is crucial for integrating TCM into oncology care. This includes adopting the Collaborative Care Management (CoCM) model, organizing regular case discussions, and incorporating CAM education into medical training to enhance understanding and acceptance of TCM.
Utilizing patient-directed knowledge tools to address information gaps in doctor-patient interactions. For example, using a structured checklist (87) to address key patient concerns for more efficient doctor-patient communication, and creating informational leaflets (88) to provide guidance on treatment timelines, efficacy, and dietary therapies.
To address the shortage of TCM specialists, interventions should incorporate Environmental Restructuring, Training, and Enablement. Environmental Restructuring can be achieved by developing structured referral pathways that integrate TCM services into existing oncology care workflows. For example, oncology clinics could implement a standardized checklist or decision-support tool embedded within electronic health records (EHR) to streamline referrals to TCM practitioners. Additionally, creating formal partnerships between oncology centers and TCM clinics would facilitate coordinated care (89). Training involves training TCM practitioners in specialized oncology knowledge, such as cancer biology, pharmacology, and the management of treatment-related side effects. Enablement focuses on fostering patient-centered initiatives, such as establishing community-based Tai Chi classes and training patients in auricular acupuncture self-care, to empower individuals in managing their symptoms and improving quality of life.
To reduce safety risks, regional and cultural differences will be considered to formulate strict laws and regulations to restrict misleading advertisements of herbal dietary supplements and improve the transparency of production.
As the cost of TCM-related products and services is high, financial barriers may impact TCM implementation more (90). To address financial barriers impacting TCM implementation, it is necessary to assess healthcare needs and adjust financial support while considering variations in healthcare policies and payment models across countries.
As we identified impediments mostly at the systemic level, some of the structural changes proposed are complicated. Future research should focus on developing targeted interventions and implementation strategies. Furthermore, the research could be refined through interviews with relevant stakeholders to adapt to the specific contexts of different countries.
The primary strength of this study lies in its innovative approach to examining attitudes toward the application of TCM in oncology from both patient and healthcare provider perspectives. By using established theoretical frameworks (TDF and COM-B), the study systematically identifies key factors influencing the implementation of TCM. Moreover, it applies the BCW and BCT techniques to propose potential solutions for advancing integrative oncology care. As a key component of TCI, the findings of this study not only complement existing research on implementation factors but also uncover previously underexplored barriers (91), such as misleading advertising and communication gaps.
Moreover, the factors and strategies identified in this study are not limited to TCM but may also be broadly applicable to other complementary medicine practices in oncology care (92). These practices similarly face challenges such as insufficient interdisciplinary collaboration, a lack of trust between patients and providers, and evidence gaps. Like TCM, their implementation may also be constrained by cultural acceptance, the adequacy of healthcare infrastructure, and the availability of trained professionals.
This meta-synthesis has several recognized limitations. Most included studies were conducted in single regions or institutions, limiting the representativeness of the findings and the ability to explore how cultural and geographical differences affect TCM implementation. Consequently, this also hindered detailed subgroup analyses by profession, ethnicity, or knowledge level. Moreover, some studies span over 15 years, during which the context of TCM practices may have undergone significant changes, such as shifts in research priorities for intervention models and adjustments to insurance coverage. These changes could impact the generalizability of the findings and their relevance to current clinical settings. Overlaps between certain TDF domains were also identified, complicating factor classification and intervention development, highlighting the need for framework refinement. Finally, the proposed interventions lack empirical validation, requiring further research to assess their real-world effectiveness.
The efficacy of TCM in supportive cancer care is supported by evidence; however, as a complex intervention, its outcomes are influenced by multiple variables, such as treatment dosage, practitioner expertise, and cultural context (93). As such, these factors place higher demands on its clinical translation and implementation. Therefore, this study identifies key influencing factors and proposes potential interventions to facilitate the effective integration of TCM into clinical practice.
Policymakers should first assess the suitability of TCM within local healthcare systems and its cross-cultural applicability. Based on these evaluations, recommended policy measures include optimizing healthcare policies and funding, strengthening TCM education and training for healthcare providers, establishing efficient TCM referral systems, and enhancing the safety regulation of herbal and dietary supplements. Additionally, increasing funding for TCM cancer research, particularly for empirical studies on intervention strategies and improvements, is essential to provide scientific evidence for its integration into oncology care. At the same time, efforts should focus on advancing multi-center and cross-regional RCTs to generate robust evidence reflecting TCM’s effectiveness across diverse populations, healthcare systems, and cultural contexts, thereby enhancing its global applicability in oncology.
Traditional Chinese Medicine plays an important role in integrative oncology care, and patients’ interest in complementary therapy has grown. However, several complex challenges hinder its implementation. Our study identifies key behavioral determinants affecting TCM use in oncology using the COM-B model and TDF framework. Knowledge gaps, lack of multidisciplinary communication, low number of practitioners with specialist knowledge, and lack of an economically supportive environment are the main impeding factors. Guided by BCW theory and BCT technology, we propose several generalizable intervention functions for the above impediments, with the expectation that they will provide a foundation for filling the practice gap of TCM in oncology care. Future research should also first assess the suitability of TCM in cancer care based on local clinical evidence, identifying appropriate interventions and their implementation strategies. Building on this, targeted interventions should be evaluated and implemented across diverse healthcare systems, accompanied by localized empirical studies to further enhance the integration of TCM into clinical oncology practice.
The original contributions presented in this study are included in this article/Supplementary material, further inquiries can be directed to the corresponding authors.
RX: Data curation, Formal Analysis, Investigation, Methodology, Validation, Visualization, Writing – original draft. YL: Investigation, Software, Validation, Visualization, Writing – original draft. YS: Formal Analysis, Investigation, Methodology, Validation, Writing – original draft. JP: Data curation, Formal Analysis, Investigation, Software, Writing – original draft. HZ: Data curation, Writing – review and editing. YW: Data curation, Writing – review and editing. XZ: Data curation, Formal Analysis, Investigation, Writing – original draft. YH: Data curation, Formal Analysis, Validation, Writing – original draft. ML: Data curation, Formal Analysis, Investigation, Supervision, Writing – original draft. CY: Conceptualization, Funding acquisition, Project administration, Supervision, Validation, Writing – review and editing. MJ: Conceptualization, Funding acquisition, Project administration, Supervision, Writing – review and editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by the National Natural Science Foundation of China (82374617), the National Natural Science Foundation of China for Young Scientists (81803956), the 2024 Beijing University of Chinese Medicine Double First-Class Discipline Project, the Capital Health Development Scientific Research Special Project (2020-4-4195). Additional support was provided by the Beijing University of Chinese Medicine Special Funding for Basic Research Operating Costs of Central Universities (No. 2022-JYB-JBZR-022).
We thank AiMi Academic Services (www.aimieditor.com) for English language editing and review services.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1501918/full#supplementary-material
1. Worl Health Oranization. Traditional, Complementary and Integrative Medicine. (2024). Available online at: https://www.who.int/health-topics/traditional-complementary-and-integrative-medicine (accessed December 25, 2024).
2. Fang L, Zhu R, Sang Z, Xu XT, Zheng LY, Xiang Y, et al. World health organization survey on the level of integration of traditional chinese medicine in chinese health system rehabilitation services. Integr Med Res. (2023) 12:100945. doi: 10.1016/j.imr.2023.100945
3. Gowin K, Muminovic M, Zick S, Lee R, Lacchetti C, Mehta A. Integrative therapies in cancer care: An update on the guidelines. Am Soc Clin Oncol Educ Book. (2024) 44:e431554. doi: 10.1200/EDBK_431554
4. Weng Y, Ren X, Zu Z, Xiao L, Chen M. Efficacy and safety of acupuncture for the treatment of insomnia in breast cancer patients: A systematic review and meta-analysis. Complement Ther Med. (2024) 86:103087. doi: 10.1016/j.ctim.2024.103087
5. Alhusamiah B, Almomani J, Al Omari A, Abu Attallah A, Yousef A, Alshraideh J, et al. The effectiveness of P6 and auricular acupressure as a complimentary therapy in chemotherapy-induced nausea and vomiting among patients with cancer: Systematic review. Integr Cancer Ther. (2024) 23:15347354241239110. doi: 10.1177/15347354241239110
6. Sun L, Xu Y, Chen N, Zhang C, Wu A, Wang H, et al. Chinese herbal medicine (JianPi-BuShen) and completion rate of adjuvant chemotherapy for patients with stage II and III colon cancer: A randomized clinical trial. Eur J Cancer Oxf Engl. (2024) 213:115109. doi: 10.1016/j.ejca.2024.115109
7. Zhang X, Qiu H, Li C, Cai P, Qi F. The positive role of traditional Chinese medicine as an adjunctive therapy for cancer. Biosci Trends. (2021) 15:283–98. doi: 10.5582/bst.2021.01318
8. Bower J, Lacchetti C, Alici Y, Barton D, Bruner D, Canin B, et al. Management of fatigue in adult survivors of cancer: ASCO–society for integrative oncology guideline update. J Clin Oncol. (2024) 42:2456–87. doi: 10.1200/JCO.24.00541
9. Cardoso F, Paluch-Shimon S, Senkus E, Curigliano G, Aapro M, André F, et al. 5th ESO-ESMO international consensus guidelines for advanced breast cancer (ABC 5). Ann Oncol. (2020) 31:1623–49. doi: 10.1016/j.annonc.2020.09.010
10. Liu X, Li M, Wang X, Dang Z, Yu L, Wang X, et al. Effects of adjuvant traditional Chinese medicine therapy on long-term survival in patients with hepatocellular carcinoma. Phytomedicine. (2019) 62:152930. doi: 10.1016/j.phymed.2019.152930
11. Jiao L, Xu J, Sun J, Chen Z, Gong Y, Bi L, et al. Chinese herbal medicine combined with EGFR-TKI in EGFR mutation-positive advanced pulmonary adenocarcinoma (CATLA): A multicenter, randomized, double-blind, placebo-controlled trial. Front Pharmacol. (2019) 10:732. doi: 10.3389/fphar.2019.00732
12. Sanford N, Sher D, Ahn C, Aizer A, Mahal B. Prevalence and nondisclosure of complementary and alternative medicine use in patients with cancer and cancer survivors in the United States. JAMA Oncol. (2019) 5:735–7. doi: 10.1001/jamaoncol.2019.0349
13. Leng J, Lei L, Lei S, Zhu Z, Ocampo A, Gany F. Use of traditional Chinese herbal medicine concurrently with conventional cancer treatment among Chinese cancer patients. J Immigr Minor Health. (2020) 22:1240–7. doi: 10.1007/s10903-020-01017-2
14. Yang G, Zhang H, Xu Y, Zhao A, Shu P, Wang W, et al. Basic characteristics, status, and challenges of integrative oncology in China. Integr Cancer Ther. (2021) 20:15347354211063504. doi: 10.1177/15347354211063504
15. Yang G, Lee R, Zhang H, Gu W, Yang P, Ling C. National survey of China’s oncologists’ knowledge, attitudes, and clinical practice patterns on complementary and alternative medicine. Oncotarget. (2017) 8:13440–9. doi: 10.18632/oncotarget.14560
16. Veleber S, Cohen M, Weitzman M, Maimon Y, Adamo C, Siman J, et al. Characteristics and challenges of providing acupuncture and Chinese herbal medicine in oncology treatment: Report of survey data and experience of five unique clinical settings. Integr Cancer Ther. (2024) 23:15347354241226640. doi: 10.1177/15347354241226640
17. Sun L, Mao J, Vertosick E, Seluzicki C, Yang Y. Evaluating cancer patients’ expectations and barriers toward traditional Chinese medicine utilization in China: A patient-support group–based cross-sectional survey. Integr Cancer Ther. (2018) 17:885–93. doi: 10.1177/1534735418777117
18. Page M, McKenzie J, Bossuyt P, Boutron I, Hoffmann T, Mulrow C, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
19. CASP Checklists. Critical Appraisal Skills Programme. CASP - Critical Appraisal Skills Programme. (2024). Available online at: https://casp-uk.net/casp-tools-checklists/ (accessed May 27, 2024).
20. Lawrence V, Fossey J, Ballard C, Moniz-Cook E, Murray J. Improving quality of life for people with dementia in care homes: Making psychosocial interventions work. Br J Psychiatry J Ment Sci. (2012) 201:344–51. doi: 10.1192/bjp.bp.111.101402
21. Yan L, Liu L, Wang F, Zhao F, Hu X. Barriers and facilitators to feeling safe for inpatients: A model based on a qualitative meta-synthesis. Front Public Health. (2024) 12:1308258. doi: 10.3389/fpubh.2024.1308258
22. Carroll C, Booth A, Leaviss J, Rick J. “Best fit” framework synthesis: Refining the method. BMC Med Res Methodol. (2013) 13:37. doi: 10.1186/1471-2288-13-37
23. Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. (2008) 8:45. doi: 10.1186/1471-2288-8-45
24. Torkel S, Wang R, Norman R, Zhao L, Liu K, Boden D, et al. Barriers and enablers to a healthy lifestyle in people with infertility: A mixed-methods systematic review. Hum Reprod Update. (2024) 30:569–83. doi: 10.1093/humupd/dmae011
25. Shankar M, Hazfiarini A, Zahroh R, Vogel J, McDougall A, Condron P, et al. Factors influencing the participation of pregnant and lactating women in clinical trials: A mixed-methods systematic review. PLoS Med. (2024) 21:e1004405. doi: 10.1371/journal.pmed.1004405
26. Brown C, Richardson K, Halil-Pizzirani B, Atkins L, Yücel M, Segrave R. Key influences on university students’ physical activity: A systematic review using the theoretical domains framework and the COM-B model of human behaviour. BMC Public Health. (2024) 24:418. doi: 10.1186/s12889-023-17621-4
27. Atkins L, Francis J, Islam R, O’Connor D, Patey A, Ivers N, et al. A guide to using the theoretical domains framework of behaviour change to investigate implementation problems. Implement Sci. (2017) 12:77. doi: 10.1186/s13012-017-0605-9
28. West R, Michie S. A brief introduction to the COM-B model of behaviour and the PRIME Theory of motivation. Qeios. (2020). doi: 10.32388/WW04E6.2 [Epub ahead of print].
29. Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci. (2012) 7:37. doi: 10.1186/1748-5908-7-37
30. Wang J, Yang Z, Liu C, Chen S, Shen Q, Zhang T, et al. Cancer survivors’ perspectives and experience on western medicine and traditional Chinese medicine treatment and rehabilitation: A qualitative study. Patient Prefer Adherence. (2014) 9:9–16. doi: 10.2147/PPA.S76617
31. Yu H, Wang S, Liu J, Lewith G. Why do cancer patients use Chinese medicine?—A qualitative interview study in China. Eur J Integr Med. (2012) 4:e197–203. doi: 10.1016/j.eujim.2012.02.007
32. Mackereth P, Stringer J. Receiving acupuncture for chemotherapy-induced peripheral neuropathy: A nested qualitative study. Eur J Integr Med. (2023) 60:102258. doi: 10.1016/j.eujim.2023.102258
33. De Valois B, Asprey A, Young T. “The monkey on your shoulder”: A qualitative study of lymphoedema patients’ attitudes to and experiences of acupuncture and moxibustion. Evid Based Complement Alternat Med. (2016) 2016:1–14. doi: 10.1155/2016/4298420
34. Liu C, Tang W, Wang H, Lee K. Cancer patients’ experience of combined treatment with conventional and traditional Chinese medicine: A biopsychosocial phenomenon. Cancer Nurs. (2011) 34:495–502. doi: 10.1097/NCC.0b013e31820d4da9
35. Chan H, Chui Y, Chan C, Cheng K, Shiu A, So W, et al. Exploring the influence of traditional Chinese medicine on self-care among chinese cancer patients. Eur J Oncol Nurs. (2014) 18:445–51. doi: 10.1016/j.ejon.2014.05.005
36. Ee C, Singleton A, de Manincor M, Elder E, Davis N, Mitchell C, et al. A qualitative study exploring feasibility and acceptability of acupuncture, yoga, and mindfulness meditation for managing weight after breast cancer. Integr Cancer Ther. (2022) 21:15347354221099540. doi: 10.1177/15347354221099540
37. Eriksen W, Singerman L, Romero S, Bussell J, Barg F, Mao J. Understanding the Use of acupuncture for insomnia among cancer survivors: A qualitative study. J Altern Complement Med. (2018) 24:962–7. doi: 10.1089/acm.2018.0156
38. Romero S, Jiang E, Bussell J, Eriksen W, Duhamel K, Barg F, et al. What makes one respond to acupuncture for insomnia? Perspectives of cancer survivors. Palliat Support Care. (2020) 18:301–6. doi: 10.1017/S1478951519000762
39. Billhult A, Stener-Victorin E, Bergbom I. The experience of massage during chemotherapy treatment in breast cancer patients. Clin Nurs Res. (2007) 16:85–99. doi: 10.1177/1054773806298488
40. Oberoi D, Reed E, Piedalue K, Landmann J, Carlson L. Exploring patient experiences and acceptability of group vs. individual acupuncture for Cancer-related pain: A qualitative study. BMC Complement Med Ther. (2022) 22:155. doi: 10.1186/s12906-022-03600-6
41. Porter D, Cochrane S, Zhu X. Current usage of traditional Chinese medicine for breast cancer—A narrative approach to the experiences of women with breast cancer in Australia—A pilot study. Medicines. (2017) 4:20. doi: 10.3390/medicines4020020
42. Chen K, Chung K, Hsu C. The intention of utilization and experience toward traditional chinese medicine among breast cancer patients in the early and late stages: a qualitative study. BMC Complement Med Ther. (2023) 23:226. doi: 10.1186/s12906-023-04054-0
43. Murley B, Haas B, Hermanns M, Wang Y, Stocks E. Influence of Tai Chi on self-efficacy, quality of life, and fatigue among patients with cancer receiving chemotherapy: A pilot study brief. J Holist Nurs. (2019) 37:354–63. doi: 10.1177/0898010119867557
44. Hung Y, Leung S, Chiu S, Li P, Kan A, Lo C, et al. Perceptions about traditional Chinese medicine use among Chinese breast cancer survivors: A qualitative study. Cancer Med. (2023) 12:1997–2007. doi: 10.1002/cam4.5046
45. Dmb S, Dmm C, Dmcm W, Dmb B. Prophylactic acupuncture treatment during chemotherapy in patients with breast cancer: results of a qualitative study nested in a randomized pragmatic trial. Integr Cancer Ther. (2021) 20:15347354211058207. doi: 10.1177/15347354211058207
46. Özdemir Ü, Taşcı S. Acupressure for cancer-related fatigue in elderly cancer patients: A randomized controlled study. Altern Ther. (2023) 29:57–65.
47. Osypiuk K, Kilgore K, Ligibel J, Vergara-Diaz G, Bonato P, Wayne P. “Making peace with our bodies”: A qualitative analysis of breast cancer survivors’ experiences with qigong mind–body exercise. J Altern Complement Med. (2020) 26:827–34. doi: 10.1089/acm.2019.0406
48. Burrows Simpson P. Family beliefs about diet and traditional Chinese Medicine for Hong Kong women with breast cancer. Oncol Nurs Forum. (2003) 30:834–40. doi: 10.1188/03.ONF.834-840
49. Mao J, Leed R, Bowman M, et al. Acupuncture for hot flashes: Decision making by breast cancer survivors. J Am Board Fam Med. (2012) 25:323–32. doi: 10.3122/jabfm.2012.03.110165
50. Walker G, De Valois B, Davies R, Young T, Maher J. Ear acupuncture for hot flushes—The perceptions of women with breast cancer. Complement Ther Clin Pract. (2007) 13:250–7. doi: 10.1016/j.ctcp.2007.06.003
51. Li X, Yang L, Du J, Chen X, Zhan DW. A qualitative study on the dietary therapy needs of cancer-related fatigue patients in Traditional Chinese Medicine. Guangming J Chin Med. (2023) 38:22–6.
52. Zhang Y. The Effect of Auricular Point Pressing Therapy on Cancer-Related Fatigue in Lung Cancer Patients Undergoing Chemotherapy. Master’s thesis. Soochow: Soochow University (2020).
53. Price S, Long A, Godfrey M. Exploring the needs and concerns of women with early breast cancer during chemotherapy: Valued outcomes during a course of traditional acupuncture. Evid Based Complement Alternat Med. (2013) 2013:1–7. doi: 10.1155/2013/165891
54. Song C, Wang M. A qualitative study on the experience of traditional Chinese medicine nursing in lung cancer patients. Chin J Mod Nurs. (2014) 20: 2538–40.
55. Kweku Sey A, Hunter J. Finding the value in oncology massage: A mixed-method study of cancer services and survivors in Australia. Adv Integr Med. (2020) 7:126–34. doi: 10.1016/j.aimed.2020.01.003
56. Xu W, Towers A, Li P, Collet J. Traditional Chinese medicine in cancer care: perspectives and experiences of patients and professionals in China. Eur J Cancer Care (Engl). (2006) 15:397–403. doi: 10.1111/j.1365-2354.2006.00685.x
57. Hu H, Shear D, Thakkar R, Thompson-Lastad A, Pinderhughes H, Hecht F, et al. Acupressure and therapeutic touch in childhood cancer to promote subjective and intersubjective experiences of well-being during curative treatment. Glob Adv Health Med. (2019) 8:216495611988014. doi: 10.1177/2164956119880143
58. Price S, Long A, Godfrey M. What is traditional acupuncture - Exploring goals and processes of treatment in the context of women with early breast cancer. BMC Complement Altern Med. (2014) 14:201. doi: 10.1186/1472-6882-14-201
59. Yu M. Factors influencing subject compliance and improvement strategies: An exploration in TCM oncology trials. Master’s thesis. Chaoyang: Beijing University of Chinese Medicine (2021). doi: 10.26973/d.cnki.gbjzu.2021.000787
60. Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Ann Behav Med. (2013) 46:81–95. doi: 10.1007/s12160-013-9486-6
61. Schapira M, Mackenzie E, Lam R, Casarett D, Seluzicki C, Barg F, et al. Breast cancer survivors willingness to participate in an acupuncture clinical trial: A qualitative study. Support Care Cancer. (2014) 22:1207–15. doi: 10.1007/s00520-013-2073-3
62. Qin W. Quantitative and Qualitative Study on Improving Postoperative Prognosis of Stage II and III Colorectal Cancer with TCM Intervention. Master’s thesis. Bejing: China Academy of Chinese Medical Sciences (2021).
63. Wang JB. A Cohort Study and Qualitative Research on Improving Postoperative Radical Cure Rate of Colorectal Cancer with Integrated Traditional Chinese Medicine Treatment. Doctoral Dissertation. Bejing: China Academy of Chinese Medical Sciences (2010).
64. Zhang L, Guo Z, Yang Y. Analysis and Qualitative Research on Comprehensive TCM Treatment Plans for Advanced Colorectal Cancer. in: Chinese Medical Doctor Association, Integrative Medicine Branch. Fuzhou: Fujian University of Traditional Chinese Medicine (2012).
65. Liu C, Tang W, Wang H, Lee K. How cancer patients build trust in traditional Chinese medicine. Eur J Integr Med. (2013) 5:495–500. doi: 10.1016/j.eujim.2013.08.003
66. Yin D, Yu X. Qualitative study on the experiences of TCM nursing techniques among cancer patients undergoing chemotherapy. Qilu J Nurs. (2017) 23: 65–8.
67. Peter M, Joy B, Jacqueline F, Jennifer F, Alexander M. Receiving or not receiving acupuncture in a trial: The experience of participants recovering from breast cancer treatment. Complement Ther Clin Pract. (2014) 20:291–6. doi: 10.1016/j.ctcp.2014.10.002
68. McPherson L, Cochrane S, Zhu X. Current usage of traditional chinese medicine in the management of breast cancer: a practitioner’s perspective. Integr Cancer Ther. (2016) 15:335–42. doi: 10.1177/1534735415607656
69. Candon M, Nielsen A, Dusek J. Trends in insurance coverage for acupuncture, 2010-2019. JAMA Netw Open. (2022) 5:e2142509. doi: 10.1001/jamanetworkopen.2021.42509
70. Waissbluth S, Peleva E, Daniel S. Platinum-induced ototoxicity: A review of prevailing ototoxicity criteria. Eur Arch Oto Rhino-Laryngol. (2017) 274:1187–96. doi: 10.1007/s00405-016-4117-z
71. Ali H, Alharbi S, Iskandar R, Mira G, Yanogue A, Alboualy E. Perception and use of herbal medicine in general practice patients: A cross-sectional study in Saudi Arabia. Cureus. (2024) 16:e56806. doi: 10.7759/cureus.56806
72. Shalgouny M, Bertz-Lepel J, Weikersthal L, Herbin J, Meier-Höfig M, Mücke R, et al. Introducing a standardized assessment of patients’ interest in and usage of CAM in routine cancer care: chances and risks from patients’ and physicians’ point of view. J Cancer Res Clin Oncol. (2023) 149:16575–87. doi: 10.1007/s00432-023-05182-3
73. Kwon K, Lacey J, Kerin-Ayres K, Heller G, Grant S. Acupuncture for the treatment of the pain-fatigue-sleep disturbance-numbness/tingling symptom cluster in breast cancer survivors: A feasibility trial. Support Care Cancer. (2024) 32:332. doi: 10.1007/s00520-024-08529-9
74. Lam C, Koon H, Ma C, Au K, Zuo Z, Chung V, et al. Real-world data on herb-drug interactions in oncology: A scoping review of pharmacoepidemiological studies. Phytomedicine Int J Phytother Phytopharm. (2022) 103:154247. doi: 10.1016/j.phymed.2022.154247
75. Strandell J, Wahlin S. Pharmacodynamic and pharmacokinetic drug interactions reported to VigiBase, the WHO global individual case safety report database. Eur J Clin Pharmacol. (2011) 67:633–41. doi: 10.1007/s00228-010-0979-y
76. Luo M, Huang J, Wang Y, Li Y, Liu Z, Liu M, et al. How fragile the positive results of Chinese herbal medicine randomized controlled trials on irritable bowel syndrome are? BMC Complement Med Ther. (2024) 24:300. doi: 10.1186/s12906-024-04561-8
77. Garavito G, Moniz T, Mansilla C, Iqbal S, Dobrogowska R, Bennin F, et al. Activities used by evidence networks to promote evidence-informed decision-making in the health sector– a rapid evidence review. BMC Health Serv Res. (2024) 24:261. doi: 10.1186/s12913-024-10744-3
78. Theunissen I, Bagot J. Supportive cancer care: Is integrative oncology the future? Curr Opin Oncol. (2024) 36:248–52. doi: 10.1097/CCO.0000000000001027
79. Rostoft S, Bos van den F, Pedersen R, Hamaker ME. Shared decision-making in older patients with cancer - What does the patient want? J Geriatr Oncol. (2021) 12:339–42. doi: 10.1016/j.jgo.2020.08.001
80. Berger S, Braehler E, Ernst J. The health professional–patient-relationship in conventional versus complementary and alternative medicine. A qualitative study comparing the perceived use of medical shared decision-making between two different approaches of medicine. Patient Educ Couns. (2012) 88:129–37. doi: 10.1016/j.pec.2012.01.003
81. van den Bemd M, Koks-Leensen M, Cuypers M, Leusink G, Schalk B, Bischoff E. Care needs of chronically ill patients with intellectual disabilities in Dutch general practice: Patients’ and providers’ perspectives. BMC Health Serv Res. (2024) 24:732. doi: 10.1186/s12913-024-11155-0
82. Michie S, van Stralen M, West R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement Sci. (2011) 6:42. doi: 10.1186/1748-5908-6-42
83. Le T, Campbell S, Andraos A, Ahlmark P, Hoang H, Isserman S, et al. Implementation of an intervention aimed at deprescribing benzodiazepines in a large US healthcare system using patient education materials: A pre/post-observational study with a control group. BMJ Open. (2024) 14:e080109. doi: 10.1136/bmjopen-2023-080109
84. Arif N, Ghezzi P. Quality of online information on breast cancer treatment options. Breast Edinb Scotl. (2018) 37:6–12. doi: 10.1016/j.breast.2017.10.004
85. Graham I, Logan J, Harrison M, Straus S, Tetroe J, Caswell W, et al. Lost in knowledge translation: Time for a map? J Contin Educ Health Prof. (2006) 26:13–24. doi: 10.1002/chp.47
86. Brouwers M, Makarski J, Kastner M, Hayden L, Bhattacharyya O. The Guideline Implementability decision excellence model (GUIDE-M): A mixed methods approach to create an international resource to advance the practice guideline field. Implement Sci. (2015) 10:36. doi: 10.1186/s13012-015-0225-1
87. Nedbal C, Naik N, Davis N, Madaan S, Tokas T, Cacciamani G, et al. Comprehensive consent in urology using decision aids, leaflets, videos and newer technologies: Empowering patient choice and shared decision-making. Ther Adv Urol. (2024) 16:17562872241301729. doi: 10.1177/17562872241301729
88. Almanasef M. Patient information leaflet in the era of digitalisation: A cross-sectional study on patients’ attitudes and practices. Ir J Med Sci. (2024) 193:777–82. doi: 10.1007/s11845-023-03515-2
89. Kennedy M, Bayes S, Newton R, et al. Building the plane while it’s flying: Implementation lessons from integrating a co-located exercise clinic into oncology care. BMC Health Serv Res. (2022) 22:1235. doi: 10.1186/s12913-022-08607-w
90. Ampomah I, Malau-Aduli B, Seidu A, Malau-Aduli A, Emeto T. Perceptions and experiences of orthodox health practitioners and hospital administrators towards integrating traditional medicine into the Ghanaian health system. Int J Environ Res Public Health. (2021) 18:11200. doi: 10.3390/ijerph182111200
91. Kwong M, Ho L, Li A, Zissiadis Y, Spry N, Taaffe D, et al. Integrative oncology in cancer care - Implementation factors: mixed-methods systematic review. BMJ Support Palliat Care. (2023): doi: 10.1136/spcare-2022-004150 Online ahead of print.
92. Mentink M, van Vliet L, Busch M, Timmer-Bonte A, Noordman J, van Dulmen S, et al. Communication and information about complementary medicine in a Dutch oncology setting: Interviewing patients and providers on their experiences and needs. Complement Ther Clin Pract. (2024) 57:101916. doi: 10.1016/j.ctcp.2024.101916
Keywords: Traditional Chinese Medicine, meta-synthesis, integrated oncology, implementation barriers, modifiable determinants
Citation: Xu R, Sun Y, Liu Y, Pan J, Han Y, Zhang X, Zhao H, Li M, Wu Y, Yu C and Jiang M (2025) Factors influencing the utilization of Traditional Chinese Medicine in cancer treatment: a qualitative meta-synthesis of patient and healthcare professional perspectives. Front. Med. 12:1501918. doi: 10.3389/fmed.2025.1501918
Received: 02 October 2024; Accepted: 10 February 2025;
Published: 05 March 2025.
Edited by:
Christian S. Kessler, Immanuel Hospital Berlin, GermanyReviewed by:
Carolyn Ee, Western Sydney University, AustraliaCopyright © 2025 Xu, Sun, Liu, Pan, Han, Zhang, Zhao, Li, Wu, Yu and Jiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Changhe Yu, eWFrbm8yQDE2My5jb20=; Miao Jiang, NzAwNTg5QGJ1Y20uZWR1LmNu
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.