
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med., 26 March 2025
Sec. Family Medicine and Primary Care
Volume 12 - 2025 | https://doi.org/10.3389/fmed.2025.1488023
 Ashenafi Kibret Sendekie1,2*
Ashenafi Kibret Sendekie1,2* Liknaw Workie Limenh3
Liknaw Workie Limenh3 Gizachew Kassahun Bizuneh4
Gizachew Kassahun Bizuneh4 Asmamaw Emagn Kasahun3
Asmamaw Emagn Kasahun3 Samuel Agegnew Wondm5
Samuel Agegnew Wondm5 Fasil Bayafers Tamene5
Fasil Bayafers Tamene5 Ephrem Mebratu Dagnew5
Ephrem Mebratu Dagnew5 Kalab Yigermal Gete6
Kalab Yigermal Gete6 Abebe Tarekegn Kassaw7
Abebe Tarekegn Kassaw7 Abera Dessie Dagnaw8
Abera Dessie Dagnaw8 Yabibal Berie Tadesse8
Yabibal Berie Tadesse8 Biruk Beletew Abate9,10
Biruk Beletew Abate9,10Background: Diabetes distress is the emotional and mental burden of living with diabetes. It can include feelings of frustration, guilt, anxiety, and worry. Understanding the factors contributing to psychological distress and how it affects glycemic control can be crucial for improving patient outcomes. Therefore, this study investigated the association between psychological distress levels and glycemic control in patients with diabetes. It also identified factors associated with severity of psychological distress.
Methods: A multicentre cross-sectional study was conducted among patients with diabetes at selected hospitals in Northwest Ethiopia. Psychological risk distress was measured using the Kessler 10 (K10) questionnaire, validated for this population. Glycemic control was categorized as poor and good based on patients’ current glucose records and following recommended guidelines. Logistic regression examined the association between psychological distress levels and glycemic control. Linear regression assessed the association between psychological distress score and other independent variables. p-value <0.05 was considered statistically significant.
Results: More than half (218, 54.2%) of the participants had severe psychological distress with a 27.4 (±4.6) mean score. Patients with moderate [AOR = 1. 85, 95% CI: 1.05–3.76] and severe [AOR = 2.84, 95% CI: 1.32–7.31] distress levels significantly had poor glycemic control compared to those with no distress. BMI [β = 0.61, 95% CI: 0.42, 71], monthly salary [β = −0.41, 95% CI: −67, −0.25], source of healthcare cost [β = −0.75, 95% CI: −2.36, −0.03], SMBG practicing [β = −0.85, 95% CI: −1.93, −0.25], lifestyle modifications [β = −1.66, 95% CI: −3.21, −0.18], number of medical conditions [β = 0.72, 95% CI: 0.57, 2.81], number of medications [β = 2.26, 95% CI: 1.05, 4.57], hypoglycaemia perception [β = 2.91, 95% CI: 1.32, 7.01], and comorbidity and/or complications [β = 3.93, 95% CI: 1.08, 6.72] were significantly associated with severity of psychological distress.
Conclusion: Most patients reported having moderate to severe psychological distress, which in turn, negatively impacted their glycemic control. Interventions incorporating mental health and psychosocial support should be implemented to relieve psychological distress and improve glycemic control.
Diabetes mellitus (DM) is a chronic metabolic disorder characterized by hyperglycemia, or high blood sugar, resulting from defects in insulin secretion, insulin action, or both (1). It is a global health crisis, affecting hundreds of millions worldwide significantly burdening healthcare systems (2, 3). Beyond its physical complications, diabetes also has a significant psychological impact, leading to distress that includes emotional, behavioral, and psychological responses to the disease (4, 5). Diabetes distress refers to the emotional and mental burden of managing diabetes, characterized by frustration, anxiety, guilt, and feelings of being overwhelmed (6).
The experience of psychological distress in diabetes is multifaceted. Patients grapple with the constant burden of managing their condition, including adhering to medication regimens, monitoring blood sugar levels, and adjusting diet and lifestyle (7, 8). This ongoing responsibility can lead to feelings of anxiety, frustration, and fear of complications (9). Additionally, the potential for social stigma associated with diabetes can exacerbate emotional distress (10). The interplay between these factors and the psychological demands of managing diabetes can create a vicious cycle, negatively impacting self-care behaviors and overall well-being.
Unlike general psychological disorders such as depression, diabetes distress is directly linked to the challenges of diabetes self-care, including medication adherence, blood sugar monitoring, and lifestyle modifications (11). Elevated distress levels are associated with poorer glycemic control, increased risk of complications, and decreased adherence to treatment plans (12–16). Furthermore, psychological distress can contribute to declining quality of life, affecting emotional well-being, social interactions, and daily functioning (12, 17). Studies worldwide also have shown a link between distress and poor glycemic control in patients with diabetes (18–23).
Identifying the factors contributing to psychological problems in patients with diabetes is critical for developing effective interventions (7). These determinants can be broadly categorized into individual, disease-related, and social aspects (24–27). Individual factors include personality traits, coping mechanisms, and social support networks, and patients with lower levels of resilience and limited social support may be more susceptible to developing distress (28, 29).
Disease-related factors encompass the type and severity of diabetes, the presence of complications, and the treatment burden. Patients with long-standing diabetes, complex treatment regimens, or existing complications may experience heightened distress (13, 26, 30). Social factors include socioeconomic status, access to healthcare, and cultural influences (31). Financial strain (32), limited access to healthcare resources (33), and social stigma (34) can increase distress. While diabetes distress stems from the daily struggles of managing the disease, diabetes stigma refers to societal judgment or discrimination against individuals with diabetes that can create distress (35).
Research on diabetes distress in Ethiopia has highlighted its prevalence and associated factors, emphasizing the role of socioeconomic and clinical factors in contributing to the experience of diabetes-related distress (26, 36, 37). In addition, existing studies have investigated factors associated with glycemic control in patients with diabetes, demonstrating relationships between sociodemographic, socioeconomic, clinical, and personal factors (38–43). However, none of these studies considered psychological parameters and their impact on patients’ glycemic control. Further research is needed to understand psychological distress levels, contributing factors, and impact on glycemic outcomes in these regions. This study investigates the association between the level of psychological distress and glycemic control among patients with diabetes. Additionally, the study demonstrated associated factors of psychological distress in this population.
An institutional-based multicenter cross-sectional study was conducted between July and October 2022. The research was carried out at outpatient follow-up clinics of four tertiary care hospitals in Northwest Ethiopia. These hospitals were chosen at random by a lottery method. The included hospitals were the University of Gondar Comprehensive Specialized Hospital (UoGCSH), Felege Hiwot Comprehensive Specialized Hospital (FHCSH), Tibebe-Ghion Comprehensive Specialized Hospital (TGCSH), and Debre Markos Comprehensive Specialized Hospital (DMCSH). All four hospitals offer diabetic care.
The study included all eligible patients with diabetes, considering their willingness, capability, and ethical aspects of participation. To be included, patients met the following criteria: (I) Diagnosed with diabetes according to the American Diabetes Association (ADA) criteria using fasting blood glucose (FBG) or HbA1c and were 18 years of age or older. (II) They had been followed in the outpatient clinics of the selected hospitals for at least 3 months and received treatment, allowing them to appreciate their psychological impact more.
Patients who could not communicate questions for an interview had severe illness/complications, or had incomplete records were excluded. Additionally, pregnant mothers were not included due to ethical considerations for vulnerable populations.
The sample size was calculated based on the single population proportion formula with the following assumptions: p = 0.5 (assuming 50% of the population with psychological distress found to have poor glycemic control because of lack of previous evidence to obtain an optimum estimate for sample size), W = 0.05 (5% margin of error for the two-tailed type-I error), Z = 1.96 (at a two-sided 95% confidence level)
When n was calculated, the sample size resulted in 384. Considering the 10% non-response rate, the final sample size was adjusted to 423. Then, to ensure representation among the selected hospitals, it was proportionally allocated based on the number of patients with diabetes identified from hospital records before the study. Consequently, we approached 155, 112, 101, and 55 samples from UoGCSH, FHCSH, DMCSH, and TGCSH, respectively.
A systematic random sampling technique was used to approach participants from selected hospitals using their unique medical identification numbers. To achieve this, an initial sample was chosen using a simple random sampling technique to ensure all patients with diabetes in the hospital records had an equal chance of being selected. Then, based on this starting point, participants were included using a sampling interval until the allocated number for each hospital was reached.
Data were collected using a structured questionnaire administered through a face-to-face interview. Clinical data and medication information were extracted concurrently from the patient’s medical records. The questionnaire, initially developed in English, was translated into the local language (Amharic) by experts to ensure consistency.
The data collection tool consists of three parts. The first part gathers participants’ sociodemographic characteristics (age, gender, marital status, education level, employment status, average monthly household income, and social history) as well as diabetes-related clinical characteristics. This includes the duration of diagnosis, body mass index (BMI), self-monitoring of blood glucose (SMBG) status, lifestyle modification status, medications, diabetes-related complications and comorbidities, and blood glucose readings like fasting blood glucose (FBG) and HbA1c. The second section is a scale that assesses patients’ perceptions of hyperglycemia and hypoglycemia. Scores range from 0 (never) to 4 (always), with higher scores indicating a greater perceived frequency of hyperglycemia and hypoglycemia. The third section of the questionnaire is a tool used to assess patients’ psychological distress over the previous 4 weeks.
To ensure the questionnaire’s clarity, consistency, and ease of use, a pilot test was conducted with 20 patients (approximately 5% of the final sample size) at UoGCSH. These pilot participants were excluded from the main study. Experts in the field (diabetes specialists and public health researchers) who are experienced in questionnaire validation and translation also assessed the questionnaire’s face validity. Based on the pilot test and expert feedback, minor modifications were made to the questionnaire related to clarity and consistency of wording before the actual data collection began.
Four nurses and two pharmacists from the selected hospitals collected the data. Data collectors participated in a half-day training session covering the study’s purpose, the data collection instruments, and ethical considerations. After entering the medical record identification numbers of patients into Microsoft Excel 2013 to check for duplicates, they interviewed the patients and extracted relevant information from their medical records. Throughout the data collection period, completed questionnaires were reviewed daily to ensure completeness, clarity, and cleanliness to ensure logical responses, error detection, handling of missing values, and standardized data entry for accurate analysis. The supervisor strictly monitored adherence to the data collection procedures.
This study determined the level of psychological distress and examined its association with glycemic control in patients with diabetes as the main outcome variable. The study also identified associated factors of psychological distress in patients with diabetes as a secondary outcome.
The Kessler Psychological Distress Scale (K10) assesses the frequency of mental distress in the past 4 weeks, focusing on symptoms of anxiety and depression. It uses a five-point scale where 1 indicates no symptoms and 5 indicates experiencing symptoms all the time. The K10 questionnaire has been used in the Ethiopian population and has good internal consistency, with Cronbach’s alpha of 0.83, indicating a reliable measurement of psychological distress (44). The exploratory factor analysis (EFA) revealed a two-factor structure, explaining approximately 66% of the total variance. However, confirmatory factor analysis (CFA) indicated that the best-fitting model for this setting was a unidimensional model with correlated errors. This model demonstrated an acceptable fit with a comparative fit index (CFI) of 0.90 and a root mean square error of approximation (RMSEA) of 0.10. The ten questions address common depression and anxiety symptoms like tiredness, nervousness, restlessness, hopelessness, sadness, feelings of worthlessness, and lack of motivation. Scores range from 10 (lowest) to 50 (highest), with higher scores indicating greater psychological distress. Scores below 20 suggest good mental health, 20–24 indicate mild distress, 25–29 moderate distress, and 30 or above indicate severe distress (45, 46).
Glycemic control was assessed using fasting blood glucose (FBG) levels obtained from participants’ medical records. The hospitals primarily utilized FBG for routine glycemic monitoring, and we could not find records of hemoglobin A1C (HbA1C) except for a small number of patients who had undergone testing at private clinics outside the hospital. After confirming a normal distribution, the average FBG over the past 3 months was calculated for each participant. Glycemic control was then categorized based on the American Diabetes Association (ADA) recommendations: Good glycemic control: FBG between 70 and 130 mg/dL and poor glycemic control: FBG below 70 mg/dL or above 130 mg/dL. FBG is a widely used method for assessing glycemic control in diabetes patients in research settings (40, 42).
Before data entry, it was checked for quality, completeness, consistency, and clarity. The data was then entered into Epi Info version 8 and subsequently imported to IBM SPSS Statistics version 26 for statistical analysis.
The normal distribution of the data was examined using normal probability (P–P) plots and histograms. Continuous variables are presented as means with standard deviations (SD), while categorical variables are presented as frequencies with percentages.
Linear regression analysis was used to identify factors potentially associated with psychological distress risk score. As a continuous outcome variable, a higher score indicates an increase in distress severity. Variables with a p-value less than or equal to 0.2 in this initial analysis were considered for further investigation. To identify the most important factors related to psychological distress, a multivariable analysis was performed on the significant variables from the initial screening.
The quality of the final model was found statistically significant (F = 207.5, p < 0.001) and assessed using several tests: Adjusted R-squared (81.6%) indicates how well the model explains the variation in psychological distress scores, variance Inflation Factor (VIF) (< 5 for all variables) suggest that multicollinearity was not a major concern, and Durbin-Watson score was 1.4 that indicates no significant autocorrelation in the model’s residuals.
The regression results were presented using unstandardized coefficients. Beta coefficients, measured in standard deviations, represent the average change in psychological distress scores for a one-unit increase in the corresponding predictor variable. A p-value <0.05 (with a 95% CI) was considered statistically significant.
A separate analysis using binary logistic regression was employed to assess the association between psychological risk distress levels and glycemic control levels while adjusting for potential confounding effects of sociodemographic, socioeconomic, personal, and clinical characteristics. A p-value <0.05 at the 95% CI in the multivariable logistic regression analysis was considered statistically significant.
423 patients were initially approached, and 402 (95.3% response rate) participated in this study. More than half (218, 54.2%) of the participants were male, with an average age of 55.1 years (standard deviation ±10.7). Most participants (342, 85.1%) had type 2 diabetes. At least eight out of ten participants (324, 80.6%) had comorbidities and/or complications. On average, each patient had 3.7 (±1.4) medical conditions and received 5.2(±1.6) medications (Table 1).
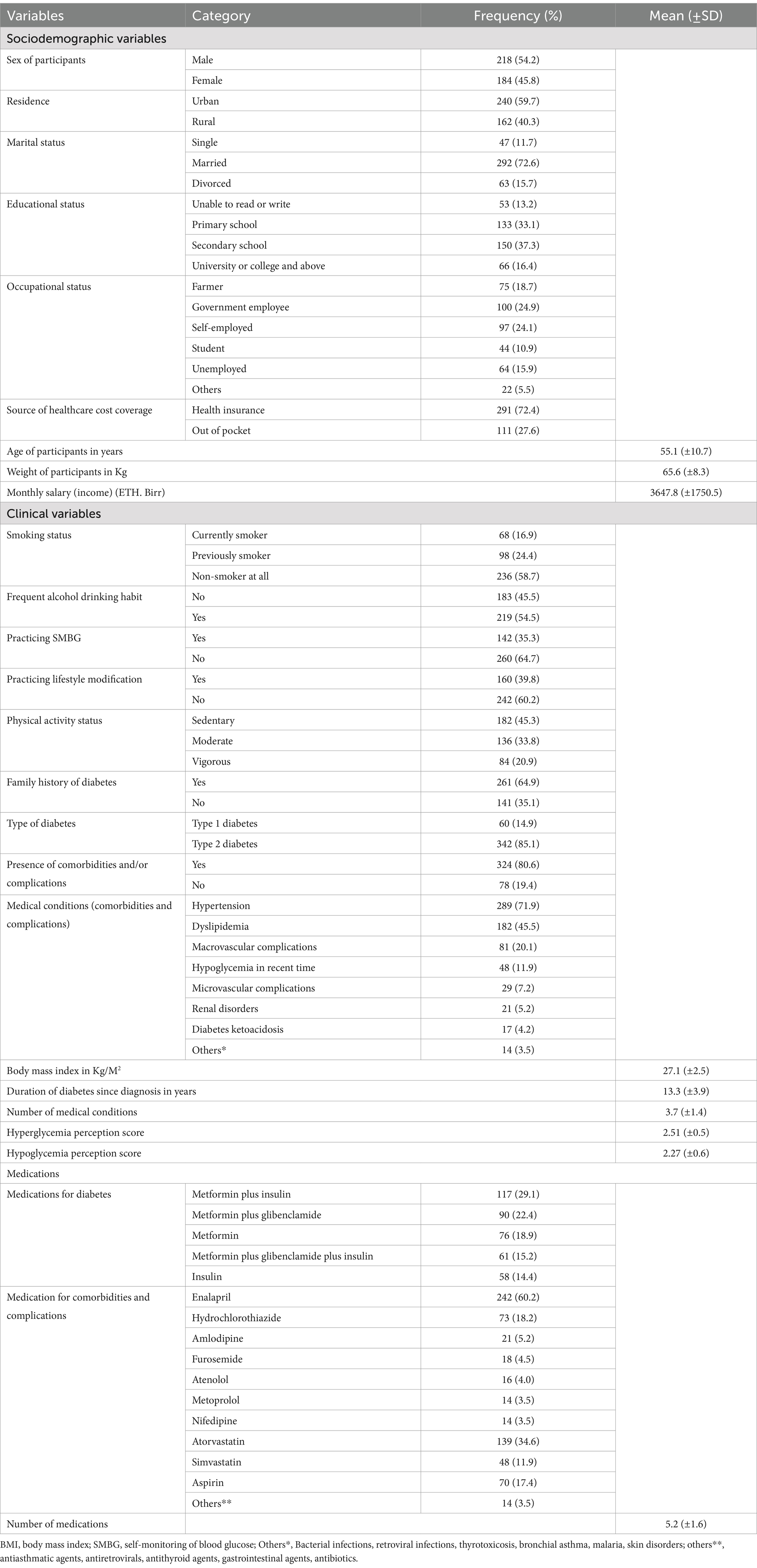
Table 1. Sociodemographic and clinical characteristics of patients with diabetes at selected hospitals in Northwest Ethiopia from July to October 2022 (N = 402).
More than half (218, 54.2%) of the participants reported severe psychological distress. The average K10 score was 27.4 (±4.6) out of 50 (Table 2).
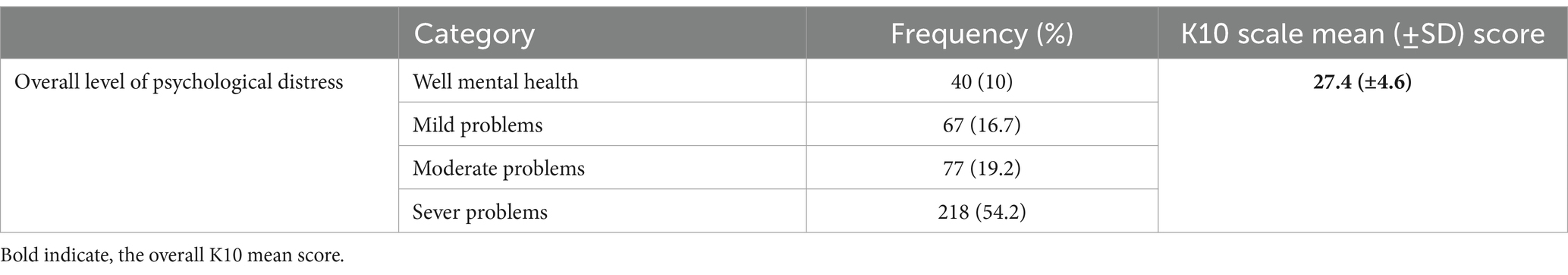
Table 2. Levels of psychological distress among patients with diabetes at selected hospitals in Northwest Ethiopia from July to October 2022 (N = 402).
The multivariate regression analysis showed that the BMI of patients, monthly salary, sources of healthcare cost coverage, SMBG practice status, lifestyle modification status, number of medical conditions, number of medications, hypoglycemic perception, and comorbidities and/or complications were associated with psychological distress level.
Patients with higher body mass index [β = 0.61, 95% CI: 0.41, 0.71], higher number of medical conditions [β = 0.72, 95% CI: 0.57, 2.81], higher number of medications [β = 2.26, 95% CI: 1.05, 4.57], higher hypoglycemia perception score [β = 2.91, 95% CI: 1.32, 7.01], and those patients with comorbidity and/or complications [β = 3.93, 95% CI: 1.08, 6.72] had severe psychological distress score compared with their counterparts. On the other hand, patients with higher monthly salaries [β = −0.41, 95% CI: −67, −0.25], those who used health insurance-based healthcare cost coverage [β = −0.75, 95% CI: −2.36, −0.03], and those patients practiced SMBG [β = −0.85, 95% CI: −1.93, −0.25] and lifestyle modifications [β = −1.66, 95% CI: −3.21, −0.18] were significantly associated lower likelihood of psychological distress score (Table 3).
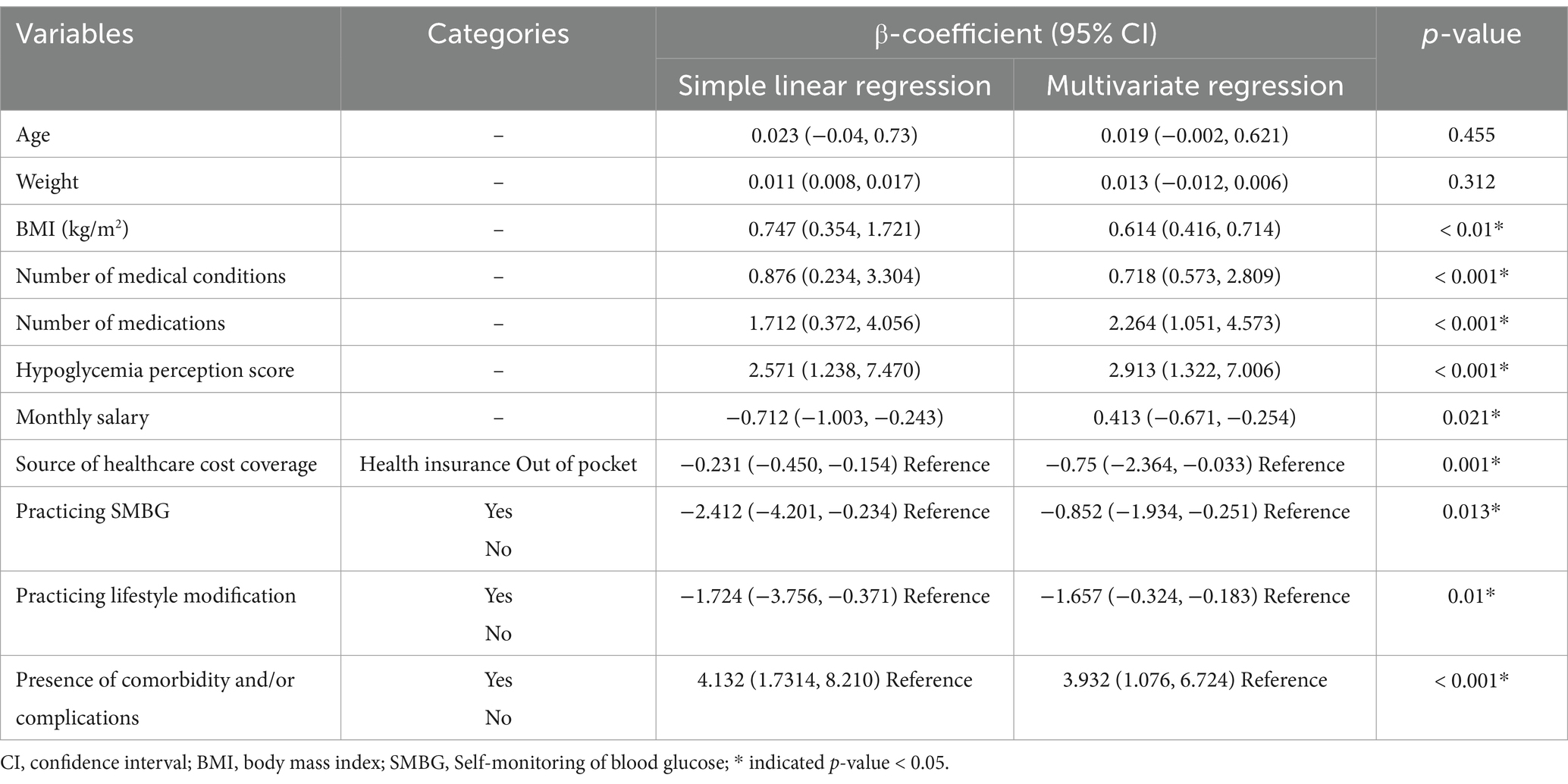
Table 3. Factors associated with psychological risk distress score among patients with diabetes at selected hospitals in Northwest Ethiopia from July to October 2022 (N = 402).
Most of the patients, 306 (76.1%) had poor glycemic control and the average level of blood glucose measured in FBG was 176.5(±51.6) mg/dl (Table 4).
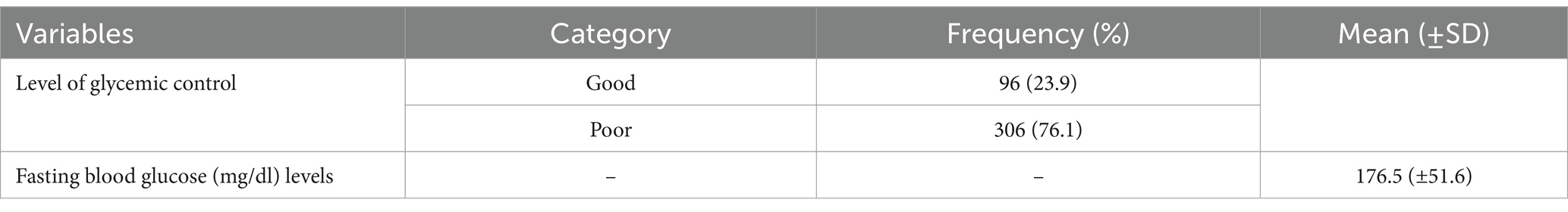
Table 4. Level of glycemic control among patients with diabetes at selected hospitals in Northwest Ethiopia from July to October 2022 (N = 402).
After adjusting other variables, the multivariable logistic regression analysis showed that the level of psychological distress had a significant association with glycemic control. Consequently, patients with moderate [AOR = 1. 85, 95% CI: 1.05–3.76] and severe [AOR = 2.84 (1.32–7.31)] psychological distress problems had significantly poor glycemic control compared with those who were mentally well patients (Table 5).
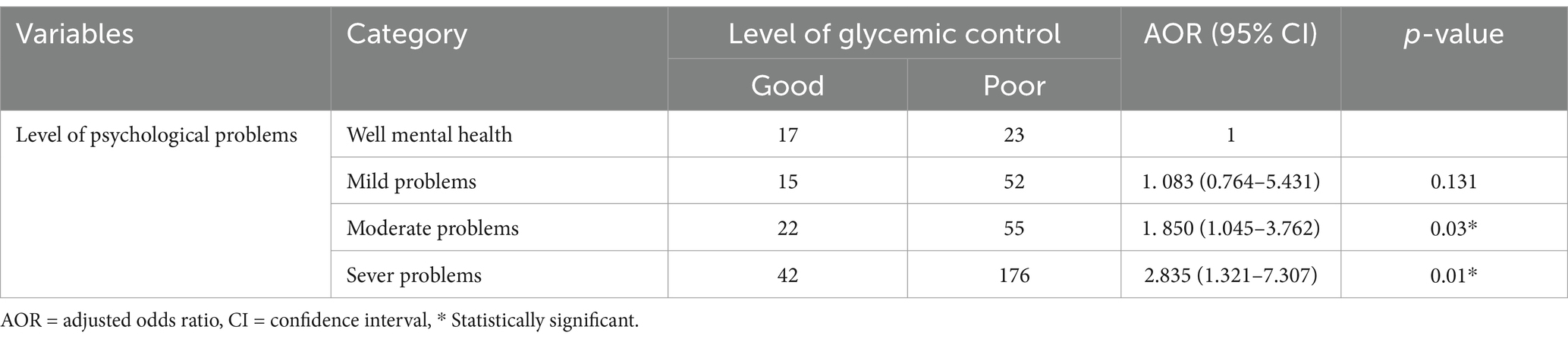
Table 5. Association between level of psychological distress and glycemic control among patients with diabetes at selected hospitals in Northwest Ethiopia from July to October 2022 (N = 402).
This study investigated the level of psychological distress and its impact on glycemic control in patients with diabetes. The findings revealed a high prevalence of severe psychological distress among participants with diabetes. The severity of psychological distress was significantly associated with various factors including BMI, socioeconomic indicators (monthly salary, healthcare coverage), diabetes self-management practices (SMBG, lifestyle modifications), number of medical conditions and medications, hypoglycemia perception, and presence of comorbidities/complications. Patients with moderate or severe psychological distress were more likely to have poor glycemic control compared to those with good mental health.
The current study’s prevalence of high severe psychological distress in patients with diabetes aligns with existing research (47). These results underscore the significant mental health burden faced by individuals with diabetes, which may be attributed to the chronic nature of the disease, the demands of self-management, and the fear of complications (7, 8). Additionally, social stigma associated with diabetes could contribute to heightened distress (10). However, another study reported a relatively lower prevalence of severe diabetes distress (48). This difference may be attributed to variations in the sociodemographic and clinical backgrounds of the study populations. Additionally, differences in the availability and utilization of psychosocial healthcare services across healthcare facilities could be another contributing factor. The high prevalence of severe psychological distress in the current study may not only affect patients’ quality of life but can also impact treatment adherence and overall health outcomes. Given the public health significance of this issue, early identification and routine screening for psychological distress should be integrated into diabetes care. Furthermore, incorporating mental health services and exploring the benefits of psychosocial interventions are essential steps toward improving both psychological well-being and glycemic control in patients with diabetes.
Consistent with previous studies (49, 50), this study identified a significant association between high BMI and psychological distress in patients with diabetes. This could be because of some mechanisms. Body image concerns are among the mechanisms (51). People with high BMI might experience social stigma and dissatisfaction with their bodies, leading to distress. The other reason is because of underlying health issues. High BMI can be a marker for underlying health conditions that contribute to both physical and mental health problems. Inflammation which is related to chronic low-grade inflammation associated with obesity might hurt mental well-being (52). The relationship between BMI and psychological distress might be bidirectional (53). Psychological distress can also lead to unhealthy behaviors like overeating, contributing to weight gain. Future research may be needed to explore the underlying mechanisms of this association. The findings may suggest the importance of addressing both physical and mental health aspects of diabetes. Thus, considering potential strategies for weight management in patients with diabetes that consider the mental health aspects, such as incorporating cognitive-behavioral therapy alongside dietary and exercise interventions will be important.
The association between socioeconomic factors monthly salary, healthcare coverage and psychological distress in patients with diabetes aligns with a growing body of research that highlights social determinants of health (31, 54). This could be a financial strain. Those people with lower incomes might face financial difficulties affording mental healthcare, medication, and healthy food choices. Particularly those patients with diabetes and comorbidities could have multiple health complications that need a higher number of medications. This in turn leads patients to become distressed more and more. Lack of access to healthcare could also play a role that limited access to mental health specialists, which can create barriers to receiving proper treatment for distress. In addition, lower socioeconomic status can be associated with greater exposure to social stressors like discrimination, unemployment, and poor living conditions, which can contribute to mental health problems. The findings suggest potential barriers to mental healthcare access and resources. This needs to be addressed to improve overall well-being through expanding access to affordable mental healthcare through insurance coverage or public programs, and community-based mental health programs that cater to underserved populations. Addressing social determinants of health through policies promoting economic opportunity and social justice is needed. In addition, emphasizes the importance of considering the social context of a patient’s life when managing diabetes needs to be considered. Advocate for healthcare providers to screen for social determinants of health and connect patients with relevant resources, such as financial assistance programs or social support services.
This study found that patients who practiced self-management were found to have a lower likelihood of experiencing psychological distress. The finding is in line with previous studies (55). The link between self-management practices (SMBG, lifestyle modifications) and distress highlights the importance of holistic diabetes management programs that address both physical and mental health. Studies also show a positive correlation between regular blood sugar monitoring and better glycemic control (40, 42). This empowers patients and reduces feelings of helplessness. Similarly, stress management is among the crucial aspects of diabetes management like healthy eating habits and regular physical activity (56). These require ongoing effort but can significantly improve overall well-being. Therefore, this study may suggest applying holistic self-management and lifestyle programs that integrate diabetes education with mental health support and stress management techniques. This empowers patients to manage their condition effectively and improve their overall quality of life by incorporating a holistic approach to diabetes self-management including psychological support to improve self-efficacy, reduce distress, and better glycemic control than traditional programs (57, 58).
Comorbidities and complications, number of medical conditions and medications, and hypoglycemic perceptions: The association between comorbidities/complications and distress is likely due to the additional burden of managing multiple health conditions. People with diabetes are more likely to have co-existing conditions like hypertension, heart disease, and kidney disease (39). In this study, most of the patients had comorbidities. These comorbidities further complicate management and increase the treatment burden, in turn, this causes distress for patients with diabetes. Chronic hyperglycemia can lead to various complications affecting the eyes, nerves, kidneys, and feet. The fear of these complications and the ongoing management needs can be a significant source of stress (9). In addition, managing multiple chronic conditions often requires numerous medications (polypharmacy), leading to complex regimens and potential medication adherence issues (40). This experience causes distress for patients. The fear of low hypoglycemia is a major concern for patients with diabetes. This fear can lead to anxiety and avoidance of necessary medications, impacting overall glycemic control (59). While traditional diabetes management often prioritizes blood sugar control, studies emphasize the importance of addressing emotional aspects (29, 60). Programs integrating psychological support, medication management, and comorbidity education can significantly enhance patient well-being and reduce distress (61, 62).
The study disclosed that patients who had moderate to severe psychological distress were found to have poor glycemic control. Studies also have shown a clear link between psychological distress, such as anxiety and depression, and poorer glycemic control in patients with diabetes (18–22, 63–65). This can manifest as difficulties with medication adherence, healthy eating habits, and overall self-management. Distress can impact self-care behaviors through various mechanisms. It can lead to decreased motivation, increased stress hormones affecting blood sugar levels, and difficulty managing emotions that might lead to unhealthy coping mechanisms like overeating (29). This negative impact of psychological distress linked to poor glycemic control underscores the importance of addressing mental health as part of diabetes management to improve overall health outcomes. Research suggests that diabetes-specific distress, encompassing feelings of burden, fear, and frustration related to managing the disease, is a significant contributor to poor glycemic control (14, 63). This might be bidirectional in that poor glycemic control itself can also contribute to psychological distress (66). Fluctuations in blood sugar levels can lead to fatigue, mood swings, and difficulty concentrating, which can exacerbate anxiety and depression. Studies have shown the effectiveness of interventions that address both psychological distress and diabetes management skills (22, 67, 68). These interventions can lead to improved glycemic control and reduced emotional burden. Generally, psychological distress and glycemic control are intricately linked to diabetes. Distress can hinder self-management efforts, leading to poorer glycemic control, while poor glycaemia control can further exacerbate distress. Healthcare professionals need to recognize this cycle and implement strategies to address both physical and mental health aspects of diabetes.
In general, diabetes-related psychological distress refers to the emotional and psychological burden experienced by individuals managing diabetes, often stemming from the complexities of self-care, disease progression, and associated health challenges. This study also highlights that most patients experience moderate to severe psychological distress which significantly impacts glycemic control. Key contributing factors include sociodemographics, socioeconomic status, self-management practices, and clinical characteristics. Given these findings, effective diabetes management should integrate mental health and psychosocial support to address these underlying stressors and improve overall health outcomes.
Despite the study’s valuable contribution to both practitioners and patients by aiding treatment decisions through consideration of mental health interventions, it has some limitations. Psychological burden was assessed using self-reported measures, which, while reliant on patient honesty, may lead to potential overestimation or underestimation of outcomes. Additionally, the study design does not allow for a definitive conclusion about the cause-and-effect relationship between glycemic levels and psychological distress risk levels.
The short-term nature of the study limits generalizability, as changes in mental health status may vary over a longer period. Furthermore, the generalizability is constrained by sample characteristics, as the majority of participants had type 2 diabetes. The study settings used FBG instead of HbA1C for routine glycemic monitoring; however, FBG may not accurately reflect long-term glycemic control as HbA1C does. Therefore, future research using prospective follow-up on a large population will be recommended to explore the association of different variables with psychological distress and the impact of psychological distress on glycemic control in patients with diabetes.
Future research with a prospective follow-up on a larger population is recommended to explore the associations between various factors and psychological distress, as well as the impact of psychological distress on glycemic control in patients with diabetes.
The study underscores the critical role of mental health in managing diabetes. It highlights that psychological distress is a significant factor affecting glycemic control, suggesting that traditional approaches focusing solely on blood sugar management may be insufficient. The findings emphasize integrating mental health and psychosocial support into diabetes care. This approach can help alleviate the psychological burden on patients, leading to improved glycemic control and overall well-being. The study also has implications for healthcare policy and guidelines. It suggests that policymakers and healthcare providers should consider incorporating mental health and psychosocial interventions into diabetes care programs to address the needs of patients experiencing psychological distress.
The study contributes to a growing body of research that recognizes the complex interplay between physical and mental health in diabetes. It expands our understanding of the factors influencing glycemic control, beyond just blood sugar levels. The findings provide evidence for the need for mental health and psychosocial interventions in improving glycemic control and overall patient outcomes in patients with diabetes. This can inform the development and implementation of evidence-based interventions to address the needs of this population. The study conducted in Northwest Ethiopia can contribute to understanding health disparities and the specific needs of patients in different regions. It highlights the importance of culturally sensitive and context-appropriate interventions to address mental health and diabetes in diverse populations.
This study found that most patients with diabetes reported to have moderate to severe psychological distress, which significantly impacted glycemic control. The severity of psychological distress was significantly associated with factors such as sociodemographics, socioeconomic status, self-management practices, and clinical characteristics like co-existing conditions, number of medications, and hypoglycemia perception. Therefore, diabetes management and interventions should address these contributing factors and should be integrated with mental health and psychosocial support.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving humans were approved by Debre Markos University Department of Pharmacy’s ethical review committee. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
AS: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Writing – original draft, Writing – review & editing. LL: Data curation, Formal analysis, Investigation, Methodology, Validation, Visualization, Writing – review & editing. GB: Methodology, Formal analysis, Validation, Visualization, Software, Writing – review & editing. AsK: Data curation, Formal analysis, Investigation, Methodology, Validation, Visualization, Writing – review & editing. SW: Methodology, Formal analysis, Validation, Visualization, Software, Writing – review & editing. FT: Data curation, Formal analysis, Investigation, Methodology, Validation, Visualization, Writing – review & editing. ED: Data curation, Formal analysis, Investigation, Methodology, Validation, Visualization, Writing – review & editing. KG: Data curation, Formal analysis, Investigation, Methodology, Validation, Visualization, Writing – review & editing. AbK: Data curation, Formal analysis, Investigation, Methodology, Validation, Visualization, Writing – review & editing. AD: Data curation, Formal analysis, Investigation, Methodology, Validation, Visualization, Writing – review & editing. YT: Investigation, Methodology, Validation, Visualization, Writing – review & editing, Data curation, Formal analysis. BA: Data curation, Formal analysis, Investigation, Methodology, Software, Supervision, Validation, Visualization, Writing – review & editing.
The author(s) declare that no financial support was received for the research and/or publication of this article.
The authors thank Debre Markos University for their ethical approval and support in conducting this study. We also extend our gratitude to the selected hospitals for their cooperation, and most importantly, to the experts who assessed the face validity of the questionnaire, data collectors and study participants for their invaluable contribution.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
BMI, body mass index; DM, diabetes mellitus; FBG, Fating blood glucose; SMBG, self-monitoring blood glucose.
1. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. (2010) 34:S62–9. doi: 10.2337/dc11-S062
2. World Health Organization. Home/newsroom/fact sheets/detail/diabetes. (2024). Available online at: https://www.who.int/news-room/fact-sheets/detail/diabetes. Accessed: 25 October 2022.
3. GBD 2021 Diabetes Collaborators. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: a systematic analysis for the global burden of disease study 2021. Lancet. (2023) 402:203–34. doi: 10.1016/S0140-6736(23)01301-6
4. de Groot, M, Golden, SH, and Wagner, J. Psychological conditions in adults with diabetes. Am Psychol. (2016) 71:552–62. doi: 10.1037/a0040408
5. Whittemore, R, Jaser, S, Chao, A, Jang, M, and Grey, M. Psychological experience of parents of children with type 1 diabetes: a systematic mixed-studies review. Diabetes Educ. (2012) 38:562–79. doi: 10.1177/0145721712445216
6. CDC. Diabetes and mental health. (2024). Available online at: https://www.cdc.gov/diabetes/living-with/mental-health.html#:~:text=Diabetes%20distress,after%20years%20of%20good%20management (Accessed February 22, 2025).
7. Fisher, L, Polonsky, WH, and Hessler, D. Addressing diabetes distress in clinical care: a practical guide. Diabet Med. (2019) 36:803–12. doi: 10.1111/dme.13967
8. Perrin, NE, Davies, MJ, Robertson, N, Snoek, FJ, and Khunti, K. The prevalence of diabetes-specific emotional distress in people with type 2 diabetes: a systematic review and meta-analysis. Diabet Med. (2017) 34:1508–20. doi: 10.1111/dme.13448
9. Co, MA, Tan, LS, Tai, ES, Griva, K, Amir, M, Chong, KJ, et al. Factors associated with psychological distress, behavioral impact and health-related quality of life among patients with type 2 diabetes mellitus. J Diabetes Complicat. (2015) 29:378–83. doi: 10.1016/j.jdiacomp.2015.01.009
10. The Lancet Diabetes Endocrinology. Diabetes stigma and discrimination: finding the right words. Lancet Diabetes Endocrinol. (2018) 6:673. doi: 10.1016/S2213-8587(18)30235-3
11. Tanenbaum, ML, Kane, NS, Kenowitz, J, and Gonzalez, JS. Diabetes distress from the patient's perspective: qualitative themes and treatment regimen differences among adults with type 2 diabetes. J Diabetes Complicat. (2016) 30:1060–8. doi: 10.1016/j.jdiacomp.2016.04.023
12. Guo, X, Wong, PNF, Koh, YLE, and Tan, NC. Factors associated with diabetes-related distress among Asian patients with poorly controlled type-2 diabetes mellitus: a cross-sectional study in primary care. BMC Prim Care. (2023) 24:54. doi: 10.1186/s12875-023-02012-w
13. Luzuriaga, M, Leite, R, Ahmed, H, Saab, PG, and Garg, R. Complexity of antidiabetic medication regimen is associated with increased diabetes-related distress in persons with type 2 diabetes mellitus. BMJ Open Diabetes Res Care. (2021) 9:e002348. doi: 10.1136/bmjdrc-2021-002348
14. Fisher, L, Mullan, JT, Arean, P, Glasgow, RE, Hessler, D, and Masharani, U. Diabetes distress but not clinical depression or depressive symptoms is associated with glycemic control in both cross-sectional and longitudinal analyses. Diabetes Care. (2010) 33:23–8. doi: 10.2337/dc09-1238
15. Adriaanse, MC, Pouwer, F, Dekker, JM, Nijpels, G, Stehouwer, CD, Heine, RJ, et al. Diabetes-related symptom distress associated with glucose metabolism and comorbidity: the Hoorn study. Diabetes Care. (2008) 31:2268–70. doi: 10.2337/dc08-1074
16. van Bastelaar, KM, Pouwer, F, Geelhoed-Duijvestijn, PH, Tack, CJ, Bazelmans, E, Beekman, AT, et al. Diabetes-specific emotional distress mediates the association between depressive symptoms and glycaemic control in type 1 and type 2 diabetes. Diabet Med. (2010) 27:798–803. doi: 10.1111/j.1464-5491.2010.03025.x
17. Oh, J, and Kim, S. The relationship between psychological distress, depressive symptoms, emotional eating behaviors and the health-related quality of life of middle-aged korean females: a serial mediation model. BMC Nurs. (2023) 22:132. doi: 10.1186/s12912-023-01303-y
18. Cherrington, AL, Bebu, I, Krause-Steinrauf, H, Hoogendoorn, CJ, Crespo-Ramos, G, Presley, C, et al. Does emotional distress predict worse glycemic control over time? Results from the Glycemia reduction approaches in diabetes: a comparative effectiveness study (GRADE). Diabetes Care. (2024) 47:620–8. doi: 10.2337/dc23-0642
19. Elotla, SF, Fouad, AM, Mohamed, SF, Joudeh, AI, Mostafa, M, Hayek, SE, et al. Association between diabetes-related distress and glycemic control in primary care patients with type 2 diabetes during the coronavirus disease 2019 (COVID-19) pandemic in Egypt. J Family Community Med. (2023) 30:42–50. doi: 10.4103/jfcm.jfcm_238_22
20. Fayed, A, AlRadini, F, Alzuhairi, RM, Aljuhani, AE, Alrashid, HR, Alwazae, MM, et al. Relation between diabetes related distress and glycemic control: the mediating effect of adherence to treatment. Prim Care Diabetes. (2022) 16:293–300. doi: 10.1016/j.pcd.2021.12.004
21. Schmitt, A, Bendig, E, Baumeister, H, Hermanns, N, and Kulzer, B. Associations of depression and diabetes distress with self-management behavior and glycemic control. Health Psychol. (2021) 40:113–24. doi: 10.1037/hea0001037
22. Indelicato, L, Dauriz, M, Santi, L, Bonora, F, Negri, C, Cacciatori, V, et al. Psychological distress, self-efficacy and glycemic control in type 2 diabetes. Nutr Metab Cardiovasc Dis. (2017) 27:300–6. doi: 10.1016/j.numecd.2017.01.006
23. James, E. Aikens; prospective associations between emotional distress and poor outcomes in type 2 diabetes. Diabetes Care. (2012) 35:2472–8. doi: 10.2337/dc12-0181
24. Wong, MH, Kwan, SM, Dao, MC, Fu, SN, and Luk, W. Prevalence and factors associated with diabetes-related distress in type 2 diabetes patients: a study in Hong Kong primary care setting. Sci Rep. (2024) 14:10688. doi: 10.1038/s41598-024-61538-w
25. Blangeti, GK, Chima, T, Kamanga, CN, and Mkwinda, E. Prevalence and associated factors of psychological distress among diabetic patients at Thyolo District Hospital in Malawi: a hospital-based cross-sectional study. Diabetes Metab Syndr Obes. (2024) 17:893–901. doi: 10.2147/DMSO.S445146
26. Adugnew, M, Fetene, D, Assefa, T, Kedir, S, Asmamaw, K, Feleke, Z, et al. Diabetes-related distress and its associated factors among people with type 2 diabetes in Southeast Ethiopia: a cross-sectional study. BMJ Open. (2024) 14:e077693. doi: 10.1136/bmjopen-2023-077693
27. Wardian, J, and Sun, F. Factors associated with diabetes-related distress: implications for diabetes self-management. Soc Work Health Care. (2014) 53:364–81. doi: 10.1080/00981389.2014.884038
28. Wojujutari, AK, Idemudia, ES, and Ugwu, LE. Psychological resilience mediates the relationship between diabetes distress and depression among persons with diabetes in a multi-group analysis. Sci Rep. (2024) 14:6510. doi: 10.1038/s41598-024-57212-w
29. Kalra, S, Jena, BN, and Yeravdekar, R. Emotional and psychological needs of people with diabetes. Indian J Endocrinol Metab. (2018) 22:696–704. doi: 10.4103/ijem.IJEM_579_17
30. German, J, Kobe, EA, Lewinski, AA, Jeffreys, AS, Coffman, C, Edelman, D, et al. Factors associated with diabetes distress among patients with poorly controlled type 2 diabetes. J Endocrine Soc. (2023) 7:bvad031. doi: 10.1210/jendso/bvad031
31. Levy, NK, Park, A, Solis, D, Hu, L, Langford, AT, Wang, B, et al. Social determinants of health and diabetes-related distress in patients with insulin-dependent type 2 diabetes: cross-sectional, mixed methods approach. JMIR Form Res. (2022) 6:e40164. doi: 10.2196/40164
32. Guan, N, Guariglia, A, Moore, P, Xu, F, and Al-Janabi, H. Financial stress and depression in adults: a systematic review. PLoS One. (2022) 17:e0264041. doi: 10.1371/journal.pone.0264041
33. Coombs, NC, Meriwether, WE, Caringi, J, and Newcomer, SR. Barriers to healthcare access among U.S. adults with mental health challenges: a population-based study. SSM Popul Health. (2021) 15:100847. doi: 10.1016/j.ssmph.2021.100847
34. Guo, X, Wu, S, Tang, H, Li, Y, Dong, W, Lu, G, et al. The relationship between stigma and psychological distress among people with diabetes: a meta-analysis. BMC Psychol. (2023) 11:242. doi: 10.1186/s40359-023-01292-2
35. CDC. Diabetes. Diabetes Stigma. (2024). Available online at: https://www.cdc.gov/diabetes/articles/diabetes-stigma.html#:~:text=What%20is%20diabetes%20stigma?,difficulty%20maintaining%20relationships%20and%20friendships (Accessed February 22, 2025).
36. Geleta, BA, Dingata, ST, Emanu, MD, Eba, LB, Abera, KB, and Tsegaye, D. Prevalence of diabetes related distress and associated factors among type 2 diabetes patients attending hospitals, Southwest Ethiopia, 2020: a cross-sectional study. Patient Relat Outcome Meas. (2021) 12:13–22. doi: 10.2147/PROM.S290412
37. Borie, YA, Tamiso, A, Gutema, K, Jisso, M, Deribe, B, Fikre, R, et al. Psychological distress and its associated factors among people with specific chronic conditions (diabetes and/or hypertension) in the Sidama region of southern Ethiopia: a cross-sectional study. PLoS One. (2024) 19:e0303196. doi: 10.1371/journal.pone.0303196
38. Tegegne, KD, Gebeyehu, NA, Yirdaw, LT, Yitayew, YA, and Kassaw, MW. Determinants of poor glycemic control among type 2 diabetes in Ethiopia: a systematic review and meta-analysis. Front Public Health. (2024) 12:1256024. doi: 10.3389/fpubh.2024.1256024
39. Sendekie, AK, Dagnew, EM, Tefera, BB, and Belachew, EA. Health-related quality of life and its determinants among patients with diabetes mellitus: a multicentre cross-sectional study in Northwest Ethiopia. BMJ Open. (2023) 13:e068518. doi: 10.1136/bmjopen-2022-068518
40. Sendekie, AK, Netere, AK, Kasahun, AE, and Belachew, EA. Medication adherence and its impact on glycemic control in type 2 diabetes mellitus patients with comorbidity: a multicenter cross-sectional study in Northwest Ethiopia. PLoS One. (2022) 17:e0274971. doi: 10.1371/journal.pone.0274971
41. Bitew, ZW, Alemu, A, Jember, DA, Tadesse, E, Getaneh, FB, Seid, A, et al. Prevalence of glycemic control and factors associated with poor glycemic control: a systematic review and Meta-analysis. Inquiry. (2023) 60:60. doi: 10.1177/00469580231155716
42. Sendekie, AK, Belachew, EA, Dagnew, EM, and Netere, AK. Rate of glycaemic control and associated factors in patients with type 2 diabetes mellitus treated with insulin-based therapy at selected hospitals in Northwest Ethiopia: a multicentre cross-sectional study. BMJ Open. (2022) 12:e065250. doi: 10.1136/bmjopen-2022-065250
43. Nigussie, S, Birhan, N, Amare, F, Mengistu, G, Adem, F, and Abegaz, TM. Rate of glycemic control and associated factors among type two diabetes mellitus patients in Ethiopia: a cross sectional study. PLoS One. (2021) 16:e0251506. doi: 10.1371/journal.pone.0251506
44. Milkias, B, Ametaj, A, Alemayehu, M, Girma, E, Yared, M, Kim, HH, et al. Psychometric properties and factor structure of the Kessler-10 among Ethiopian adults. J Affect Disord. (2022) 303:180–6. doi: 10.1016/j.jad.2022.02.013
45. Kessler, RC, Andrews, G, Colpe, LJ, Hiripi, E, Mroczek, DK, Normand, SLT, et al. Short screening scales to monitor population prevalence’s and trends in non-specific psychological distress. Psychol Med. (2002) 32:959–76. doi: 10.1017/S0033291702006074
46. Andrews, G, and Slade, T. Interpreting scoPsyres on the Kessler psychological distress scale (k10). Aust N Z J Public Health. (2001) 25:494–7. doi: 10.1111/j.1467-842X.2001.tb00310.x
47. Sendhilkumar, M, Tripathy, JP, Harries, AD, Dongre, AR, Deepa, M, Vidyulatha, A, et al. Factors associated with high stress levels in adults with diabetes mellitus attending a tertiary diabetes care center, Chennai, Tamil Nadu, India. Indian J Endocrinol Metab. (2017) 21:56–63. doi: 10.4103/2230-8210.196006
48. Sayed Ahmed, HA, Fouad, AM, Elotla, SF, Joudeh, AI, Mostafa, M, Shah, A, et al. Prevalence and associated factors of diabetes distress, depression and anxiety among primary care patients with type 2 diabetes during the COVID-19 pandemic in Egypt: a cross-sectional study. Front Psych. (2022) 13:937973. doi: 10.3389/fpsyt.2022.937973
49. Sacco, WP, Wells, KJ, Vaughan, CA, Friedman, A, Perez, S, and Matthew, R. Depression in adults with type 2 diabetes: the role of adherence, body mass index, and self-efficacy. Health Psychol. (2005) 24:630–4. doi: 10.1037/0278-6133.24.6.630
50. Kokoszka, A, Pacura, A, Kostecka, B, Lloyd, CE, and Sartorius, N. Body self-esteem is related to subjective well-being, severity of depressive symptoms, BMI, glycated hemoglobin levels, and diabetes-related distress in type 2 diabetes. PLoS One. (2022) 17:e0263766. doi: 10.1371/journal.pone.0263766
51. Troncone, A, Cascella, C, Chianese, A, Zanfardino, A, Piscopo, A, Borriello, A, et al. Body image problems and disordered eating behaviors in Italian adolescents with and without type 1 diabetes: an examination with a gender-specific body image measure. Front Psychol. (2020) 11:556520. doi: 10.3389/fpsyg.2020.556520
52. Ellulu, MS, Patimah, I, Khaza'ai, H, Rahmat, A, and Abed, Y. Obesity and inflammation: the linking mechanism and the complications. Arch Med Sci. (2017) 13:851–63. doi: 10.5114/aoms.2016.58928
53. Emery, CF, Finkel, D, Gatz, M, and Dahl Aslan, AK. Evidence of bidirectional associations between depressive symptoms and body mass among older adults. J Gerontol B Psychol Sci Soc Sci. (2020) 75:1689–98. doi: 10.1093/geronb/gbz022
54. Alegría, M, NeMoyer, A, Falgàs Bagué, I, Wang, Y, and Alvarez, K. Social determinants of mental health: where we are and where we need to go. Curr Psychiatry Rep. (2018) 20:95. doi: 10.1007/s11920-018-0969-9
55. Eshete, A, Mohammed, S, Deresse, T, Kifleyohans, T, and Assefa, Y. Association of stress management behavior and diabetic self-care practice among diabetes type II patients in north Shoa zone: a cross-sectional study. BMC Health Serv Res. (2023) 23:767. doi: 10.1186/s12913-023-09752-6
56. Zamani-Alavijeh, F, Araban, M, Koohestani, HR, and Karimy, M. The effectiveness of stress management training on blood glucose control in patients with type 2 diabetes. Diabetol Metab Syndr. (2018) 10:39. doi: 10.1186/s13098-018-0342-5
57. Gómez-Velasco, DV, Almeda-Valdes, P, Martagón, AJ, Galán-Ramírez, GA, and Aguilar-Salinas, CA. Empowerment of patients with type 2 diabetes: current perspectives. Diabetes Metab Syndr Obes. (2019) 12:1311–21. doi: 10.2147/DMSO.S174910
58. Ofori, SN, and Unachukwu, CN. Holistic approach to prevention and management of type 2 diabetes mellitus in a family setting. Diabetes Metab Syndr Obes. (2014) 7:159–68. doi: 10.2147/DMSO.S62320
59. Huang, J, Peng, W, Ding, S, Xiong, S, and Liu, Z. Fear of hypoglycemia and associated factors in hospitalized patients with type 2 diabetes: a cross-sectional study. Sci Rep. (2022) 12:20338. doi: 10.1038/s41598-022-24822-1
60. Massey, CN, Feig, EH, Duque-Serrano, L, Wexler, D, Moskowitz, JT, and Huffman, JC. Well-being interventions for individuals with diabetes: a systematic review. Diabetes Res Clin Pract. (2019) 147:118–33. doi: 10.1016/j.diabres.2018.11.014
61. Abbas, Q, Latif, S, Ayaz Habib, H, Shahzad, S, Sarwar, U, Shahzadi, M, et al. Cognitive behavior therapy for diabetes distress, depression, health anxiety, quality of life and treatment adherence among patients with type-II diabetes mellitus: a randomized control trial. BMC Psychiatry. (2023) 23:86. doi: 10.1186/s12888-023-04546-w
62. Chew, BH, Vos, RC, Metzendorf, MI, Scholten, RJ, and Rutten, GE. Psychological interventions for diabetes-related distress in adults with type 2 diabetes mellitus. Cochrane Database Syst Rev. (2017) 9:CD011469.doi: 10.1002/14651858.CD011469.pub2
63. Mizokami-Stout, K, Choi, H, Richardson, CR, Piatt, G, and Heisler, M. Diabetes distress and glycemic control in type 2 diabetes: mediator and moderator analysis of a peer support intervention. JMIR Diabetes. (2021) 6:e21400. doi: 10.2196/21400
64. Saenz, JL, and Villarreal, VR. Prevalence of depression among adults with diabetes mellitus and the relationship between improvement in depressive symptoms and glycemic control. Cureus. (2023) 15:e48241. doi: 10.7759/cureus.48241
65. Park, HS, Cho, Y, Seo, DH, Ahn, SH, Hong, S, Suh, YJ, et al. Impact of diabetes distress on glycemic control and diabetic complications in type 2 diabetes mellitus. Sci Rep. (2024) 14:5568. doi: 10.1038/s41598-024-55901-0
66. Al-Atram, AA. A review of the bidirectional relationship between psychiatric disorders and diabetes mellitus. Neurosciences (Riyadh). (2018) 23:91–6. doi: 10.17712/nsj.2018.2.20170132
67. Indelicato, L, Dauriz, M, Santi, L, Negri, C, Cacciatori, V, and Bonora, E. Effects of a psychological intervention on glycemic control and psychological distress in individuals with type 2 diabetes. J Psychosom Res. (2018) 109:109–10. doi: 10.1016/j.jpsychores.2018.03.075
Keywords: psychological distress, glycemic control, diabetes management, diabetes distress, mental health and diabetes, emotional burden, Ethiopia
Citation: Sendekie AK, Limenh LW, Bizuneh GK, Kasahun AE, Wondm SA, Tamene FB, Dagnew EM, Gete KY, Kassaw AT, Dagnaw AD, Tadesse YB and Abate BB (2025) Psychological distress and its impact on glycemic control in patients with diabetes, Northwest Ethiopia. Front. Med. 12:1488023. doi: 10.3389/fmed.2025.1488023
Received: 29 August 2024; Accepted: 10 March 2025;
Published: 26 March 2025.
Edited by:
Antonio Sarría-Santamera, Nazarbayev University, KazakhstanReviewed by:
Sridhar R. Gumpeny, Endocrine and Diabetes Centre, IndiaCopyright © 2025 Sendekie, Limenh, Bizuneh, Kasahun, Wondm, Tamene, Dagnew, Gete, Kassaw, Dagnaw, Tadesse and Abate. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ashenafi Kibret Sendekie, YXNodWtpYjAyQHlhaG9vLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.