- 1Peking University Hepatology Institute, Peking University People’s Hospital, Beijing, China
- 2Department of Liver Diseases, The First Hospital of Lanzhou University, Lanzhou, China
- 3The First Department of Neurology, The Third People’s Hospital of Liaoyang, Liaoyang, China
- 4Department of Marketing, School of Business, Renmin University of China, Beijing, China
- 5Department of Hepatobiliary Surgery, Peking University People’s Hospital, Beijing, China
Introduction: Liver disease remains a significant global health concern. In China, the number of patients with liver cirrhosis is estimated to reach 7 million. In addition to the high risk of death, cirrhosis leads to several severe complications. Patients with cirrhosis have significantly longer hospital stays and higher total hospital costs than those without cirrhosis. We aimed to investigate the predictors of readmission among patients with cirrhosis in China.
Materials and methods: We conducted a retrospective study to evaluate adult patients with cirrhosis. Data on various sociodemographic, clinical, and hospitalization characteristics were collected. We defined the primary endpoint as the first liver-related readmission occurring within 30–90 days of initial hospitalization. Adult patients with cirrhosis admitted to our hospital between January 2009 and December 2022 were included. Differences between groups were analyzed using Student’s t-test and chi-square test. Logistic and multiple linear regression analyses were performed to identify predictors associated with readmission and the length of the first hospitalization.
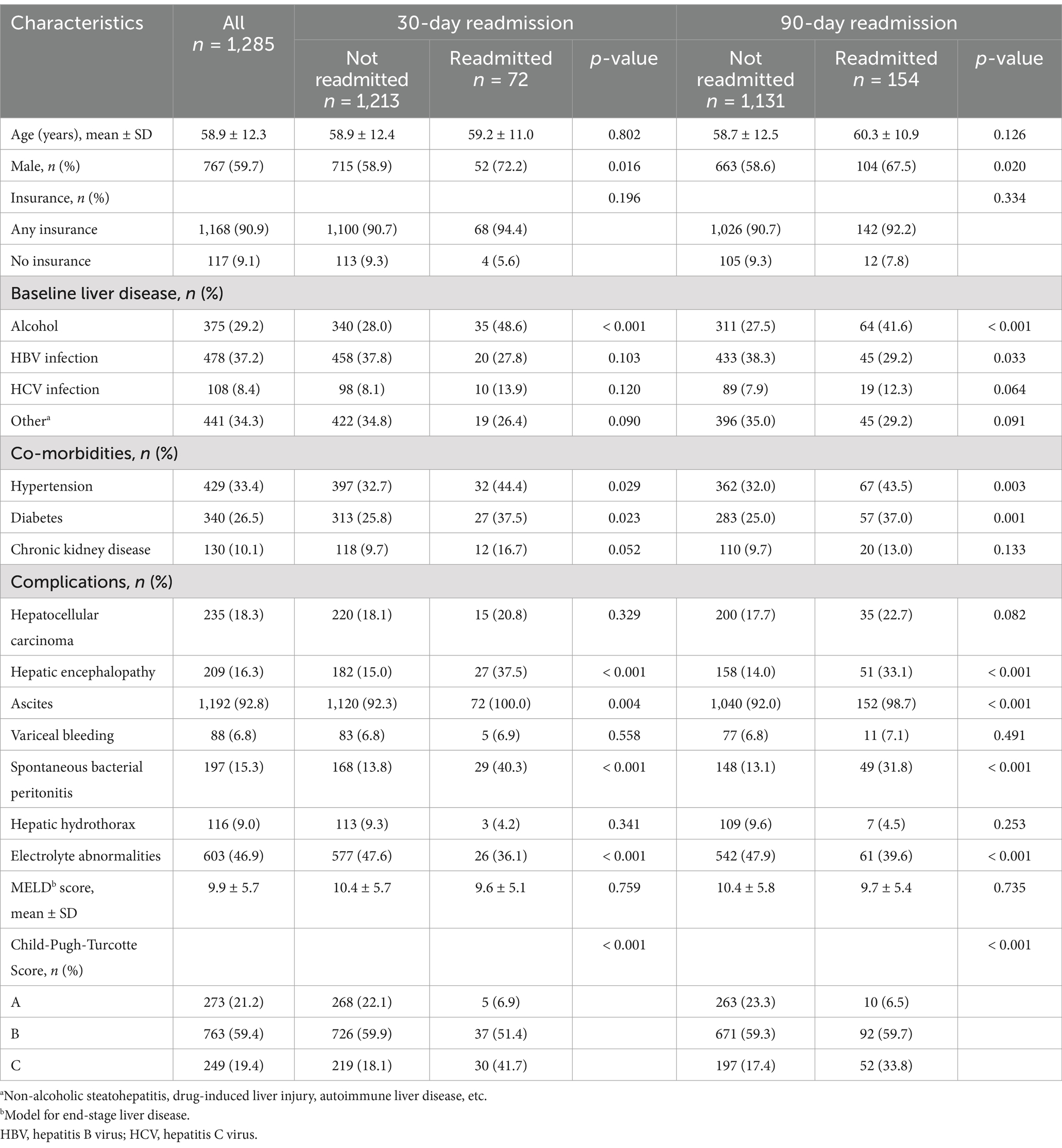
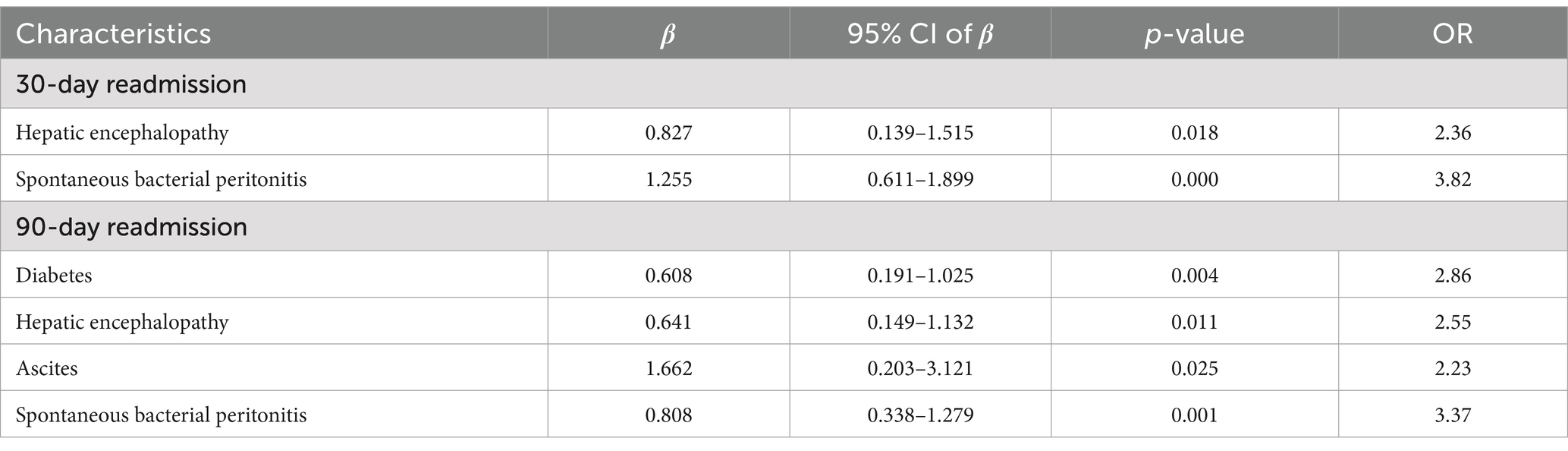
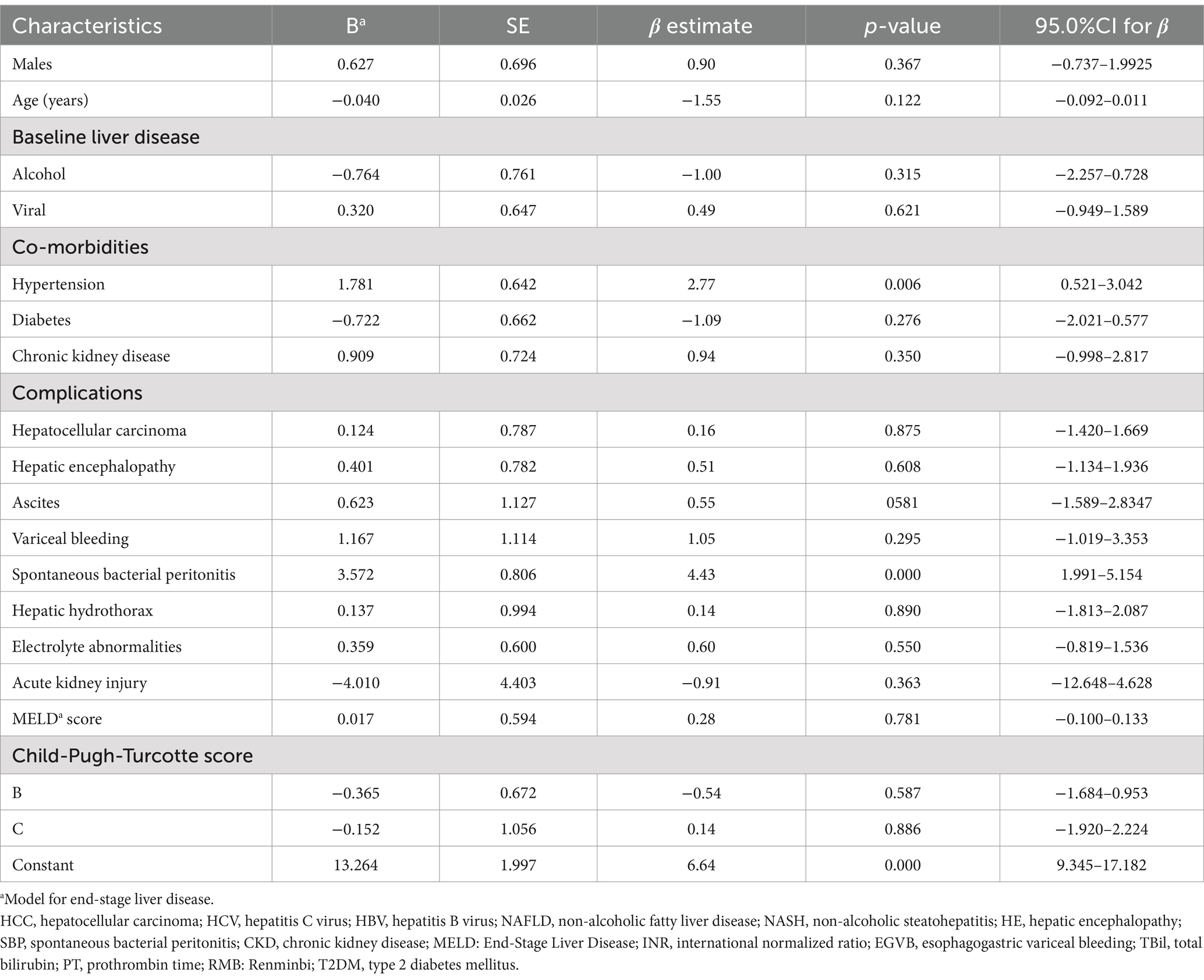
Results: In total, 1,285 patients were diagnosed with cirrhosis. Among these patients, 767 (59.7%) were males, and the mean age was 58.9 ± 12.3 years. Seventy-two (5.6%) and 154 (12.0%) patients were readmitted within 30 and 90 days, respectively. Compared with those who were not readmitted, patients readmitted at 30-day and 90-day had a higher proportion of males, ascites, spontaneous bacterial peritonitis, electrolyte abnormalities, higher Child-Pugh–Turcotte scores, longer initial hospital stays, and higher initial hospitalization costs. Logistic regression analysis indicated that hepatic encephalopathy, spontaneous bacterial peritonitis, diabetes, and ascites were predictors of 30- and 90-day readmission. Hypertension and spontaneous bacterial peritonitis were significant predictors of the length of the first hospitalization.
Conclusion: Patients with cirrhosis presenting with hepatic encephalopathy, ascites, and spontaneous bacterial peritonitis may have a higher risk of rehospitalization.
1 Introduction
Liver disease remains a significant global health concern, resulting in approximately 2 million deaths annually worldwide, with 1 million fatalities attributed to cirrhosis complications. Cirrhosis is the 11th most common cause of death globally (1). In 2017, cirrhosis led to over 1.32 million deaths, comprising 2.4% of all global deaths (2). In China, the number of patients suffering from liver cirrhosis is estimated to approach 7 million (3), in whom approximately 460,000 new cases of hepatocellular carcinoma (HCC) are reported each year (4). Patients with compensated cirrhosis have a 4.7 times higher risk of death than the general population, whereas those with decompensated cirrhosis have a 9.7 times higher risk (5). Besides the high risk of death, cirrhosis leads to several severe complications, including ascites, variceal hemorrhage, hepatic encephalopathy (HE), HCC, spontaneous bacterial peritonitis (SBP), and malnutrition. These complications can significantly affect the patients’ quality of life, prevent them from working due to worsened physical and mental health, and impose substantial financial burdens (5, 6). Compared to individuals without cirrhosis, patients with cirrhosis experience significantly longer hospital stays and higher total hospital charges (7). Additionally, those with comorbid cirrhosis face a higher likelihood of 30-day and 90-day readmissions than patients without cirrhosis (7).
Patients with advanced liver disease have high readmission rates (8). Previous studies estimated the 30-day readmission rate in patients with cirrhosis to be 26% (9). Similarly, the readmission rate within 1 year was reported to be 28.7% in China (10). A study conducted in Texas showed that patients with chronic liver disease (25%) had a higher 30-day readmission rate than those with congestive heart failure (21.9%) or chronic obstructive pulmonary disease (20.6%) (11). Readmission of inpatients with cirrhosis is associated with a deteriorated quality of life and a higher risk of death (12). These readmissions not only pose challenges to patient health but also impose an increased financial burden (13). In the United States, the cost of cirrhosis-related hospitalizations doubled from $4.8 billion to $9.8 billion between 2001 and 2011 (14).
Numerous factors are associated with readmission in patients with cirrhosis, including socioeconomic characteristics, cirrhosis type, hepatorenal syndrome, ascites, variceal hemorrhage, HCC, Charlson Comorbidity Index, and HE (13, 15). In particular, HE has been identified as a significant predictor of 30-day and 90-day readmission in patients with cirrhosis, along with the presence of >3 cirrhotic complications (15). These structural changes have led to the pathogenesis of cirrhosis in recent years (16) The application of antivirals for hepatitis B virus (HBV) and hepatitis C virus (HCV), as well as large-scale neonatal HBV vaccination, has reduced the prevalence of cirrhosis related to viral hepatitis (14, 17, 18). To date, non-alcoholic steatohepatitis (NASH) and alcohol-related liver disease are the most common causes of liver cirrhosis (19–21). Therefore, further research is needed to identify the factors that influence readmitted hospital admissions in patients with cirrhosis, to treat patients, and to avoid the deterioration of these conditions early. We conducted a retrospective study to gain insight into the predictors influencing readmission in patients with cirrhosis in China.
2 Materials and methods
2.1 Data source
We conducted a retrospective study at a single center to evaluate adult patients with cirrhosis. The study period spanned from January 2009 to December 2022. We identified patients through our hospital’s electronic medical records using admission diagnoses of cirrhosis with the International Classification of Diseases, 10th revision, Clinical Modification (ICD-10-CM) codes K74.100 and K74.607. We excluded patients with incomplete information, those who were lost to follow-up, or those who died during the index hospitalization. The study was conducted in accordance with the ethical guidelines outlined in the 1975 Declaration of Helsinki (6th revision, 2008) and was approved by the Ethics Committee of Peking University People’s Hospital (No. 2023PHB214-001). Given the retrospective nature of the study, the requirement for informed consent was waived, and none of the enrolled patients were asked to provide informed consent.
2.2 Participants
Adult patients with cirrhosis who were admitted to our hospital between January 2009 and December 2022 were included in this study.
2.3 Main measures
We collected a comprehensive range of sociodemographic, clinical, and hospitalization characteristics, including sex, age, type of medical insurance (Chinese resident medical insurance and Chinese worker medical insurance), and baseline liver disease etiology (alcohol-related liver disease, viral hepatitis, or other causes, such as non-alcoholic steatohepatitis, drug-induced liver injury, or autoimmune liver disease). Comorbidities were documented, including hypertension (I10. ×00 × 002), diabetes mellitus (E14.900 × 001), and chronic kidney disease (CKD) (N18.900 × 005). We also recorded liver disease-related complications, such as HCC (C22.70D), HE (K72.90B), and ascites (R18. ×00), variceal bleeding (K92.201), SBP (K65.016), hepatic hydrothorax (J94.80D), and electrolyte disturbances (E87.800 × 011, E87.600, E87.500, E87.102, and E87.001). In addition, we documented the Model for End-Stage Liver Disease (MELD) and Child-Pugh–Turcotte scores at the time of the patient’s first discharge.
Alcoholic liver disease was diagnosed when alcohol consumption was ≥40 g/day in males and ≥ 20 g/day in females, with a history of alcohol intake spanning at least 5 years (22). Liver diseases other than alcoholic liver disease or viral hepatitis were identified based on admission and discharge diagnoses, with only the first occurrence of each diagnosis recorded. Laboratory data were retrieved from the hospital’s clinical data center.
The MELD score was calculated using parameters such as total bilirubin level, creatinine level, international normalized ratio (INR), and history of cholestatic liver disease. The Child-Pugh–Turcotte score was also calculated, and patients were categorized into three groups: A, good hepatic function; B, moderately impaired hepatic function; and C, advanced hepatic dysfunction, based on five clinical and laboratory criteria: serum bilirubin, serum albumin, ascites, neurological disorder, and clinical nutrition status.
2.4 Hospitalization characteristics
The recorded hospitalization characteristics included cirrhosis complications observed during the first admission and readmission. These complications included volume-related issues such as ascites (R18. × 00), hepatic hydrothorax (J94.80D), edema (R60.900), SBP (K65.016), variceal bleeding (K92.201), HCC (C22.70D), HE (K72.90B), liver function deterioration, infections, or other related factors.
Liver function deterioration was diagnosed based on at least one of the following criteria (23, 24): an increase in Child-Pugh score by 2 points or more from baseline; total bilirubin (TBil) levels ≥51 μmol/L or an increase in TBil levels from baseline of ≥34.2 μmol/L; and any increase in prothrombin time (PT) from baseline of ≥3 s. Infections were diagnosed according to international and local guidelines. Patients may have had multiple liver-related reasons for admission, and the major reasons for each admission were recorded. Furthermore, we collected data on the cost of the initial admission and the length of stay for the first hospitalization, calculated from admission to discharge.
2.5 Study outcomes
We defined the primary endpoint as the first liver-related readmission occurring within 30–90 days of initial hospitalization. To capture episodes of hospitalization at other hospitals, we contacted patients who had liver-related readmissions to any hospital since their first hospitalization. Liver-related readmission was defined as previously described. All other readmissions were excluded from the analysis. If a patient had more than one readmission within 30 days, only the first readmission was considered for the analysis. The secondary endpoint was the length of hospitalization at the time of admission.
We collected comprehensive information on readmissions by accessing the electronic medical records of our hospital, including medical histories, physical examinations, daily notes, laboratory results, and discharge summaries. To track hospitalizations at other facilities, we contacted patients with liver-related readmissions via telephone or conducted in-person interviews during subsequent visits to our outpatient clinic or inpatient department.
2.6 Statistical analysis
The normality of the data was evaluated using the Kolmogorov–Smirnov test. Mean ± standard deviation (SD) was used to present as continuous variables were normally distributed. Categorical variables are presented as numbers (%). Differences between groups were analyzed using Student’s t-test for variables such as age, MELD score, cost of admission, and length of stay. The chi-square test was used to analyze variables such as insurance, baseline liver disease, comorbidities, complications, treatment, and cause of readmission. Logistic regression analysis using a stepwise selection approach was performed to identify predictors associated with readmission, whereas multiple linear regression analysis was used to identify predictors associated with the length of the first hospitalization. For logistic model diagnostics, we employed the Hosmer-Lemeshow goodness-of-fit test to evaluate the calibration of our logistic regression models. A p-value <0.05 was considered statistically significant. All data analyses were conducted using SPSS version 23.0 (IBM Corp, Armonk, NY, USA).
3 Results
3.1 Baseline characteristics of patients with cirrhosis
We enrolled 1,285 patients who were admitted with cirrhosis. Their baseline characteristics are shown in Table 1. Within 30 days, 72 (5.6%) patients were readmitted, and within 90 days, the number increased to 154 (12.0%) patients. Among the patients, 767 (59.7%) were male, and the mean age was 58.9 ± 12.3 years. A total of 117 (9.1%) patients had no insurance coverage. Alcoholic cirrhosis was observed in 375 (29.2%) patients. On admission, 209 (16.3%), 1,192 (92.8%), and 88 (6.8%) patients presented with HE, ascites, and esophagogastric variceal bleeding, respectively. The mean MELD score was 9.9 ± 5.7. Regarding the Child-Pugh–Turcotte score, 726 (59.9%) and 219 (18.1%) patients were classified as Grade B and Grade C, respectively.
Considering 30-day and 90-day readmission cases This subgroup consisted of a higher proportion of males (30-day: 52 [72.2%] vs. 715 [58.9%], p = 0.016; 90-day: 104 [67.5%] vs. 663 [58.6%], p = 0.020) and individuals with alcoholic cirrhosis (30-day: 35 [48.6%] vs. 340 [28%], p < 0.001; 90-day: 64 [41.6%] vs. 311 [27.5%], p < 0.001) compared to those who did not experience readmission within the 30-day or 90-day timeframe. Patients admitted for 90 days had a lower proportion of HBV infections (45 [29.2%] vs. 433 [38.3%], p = 0.016). Furthermore, among the readmitted patients, a higher prevalence of HE (30-day: 27 [37.5%] vs. 182 [15.0%], p < 0.001; 90 day: 51 [33.1%] vs. 158 [14%], p < 0.001), ascites (30 day: 72 [100%] vs. 1,120 [92.3%], p = 0.004; 90-day: 152 [98.7%] vs. 1,040 [92.0%], p < 0.001), SBP (30-day: 29 [40.3%] vs. 168 [13.8%], p < 0.001; 90-day: 49 [31.8%] vs. 148 [13.1%], p < 0.001), and electrolyte abnormalities (30-day: 26 [36.1%] vs. 577 [47.6%], p < 0.001; 90-day:61 [39.6%] vs. 542 [47.9%], p < 0.001) was observed. Notably, readmitted patients had significantly higher Child-Pugh Turcotte scores than those who were not readmitted (30-day, p < 0.001, 90-day, p < 0.001).
3.2 Hospitalization characteristics
The major causes of first admission were volume-related (568, 44.2%), liver function deterioration (285, 22.2%), HE (101, 7.9%), and other causes (164, 12.8%). Among the patients readmitted within 30 and 90 days, a higher proportion had volume-related issues, and HE was the primary reason for their initial hospitalization. The mean cost for first admission was 25,035 ± 51,529 Renminbi (RMB). Among the patients readmitted within 30 and 90 days, there was a higher prevalence of longer initial hospital stays (30-day: 19.8 ± 13.1 vs. 15.1 ± 12.0 days, p = 0.001; 90-day: 17.8 ± 11.5 vs. 15.0 ± 12.2 days, p = 0.007) and higher initial hospitalization costs (30-day: 33833 ± 29,829 vs. 24,509 ± 52,504 RMB, p = 0.136; 90-day: 27461 ± 26,636 vs. 24,702 ± 54,056 RMB, p = 0.533). The primary causes of readmission within 30 days were volume-related issues (n = 30, 41.7%), liver function deterioration (n = 12, 16.7%), and HE (n = 11, 15.3%). For readmissions within 90 days, the major causes were volume-related issues (n = 80, 51.9%), deterioration of liver function (n = 20, 12.9%), and other miscellaneous causes (n = 15, 9.7%). Of the patients who were readmitted within 30 days, 33 (45.8%) were readmitted for the same cause. Similarly, among patients readmitted within 90 days, 72 (46.8%) were readmitted for the same cause (Table 2).
3.3 Predictors of 30-day and 90-day readmission
The results of the logistic regression analysis for the predictors of readmission within 30 and 90 days are presented in Table 3. Significant predictors of readmission within 30 days included HE and SBP. For readmission within 90 days, the significant predictors included diabetes, HE, ascites, and SBP (Table 3).
3.4 Predictors of length of hospitalization at the first admission
Table 4 demonstrates that hypertension (p = 0.001) and SBP (p < 0.001) were significant predictors of the length of hospitalization of patients during their initial admission.
4 Discussion
Data and evidence on the rates and reasons for readmission among patients with cirrhosis in China are currently lacking. Moreover, the causes of cirrhosis in China differ significantly from those in Europe and the United States, with a higher proportion of cirrhosis cases attributed to viral hepatitis. Our study, which included a large sample size, identified the predictors of readmission in Chinese patients with cirrhosis. These findings provide valuable insights for the targeted management of complications, with the aim of reducing readmission risks and optimizing medical resource utilization for patients with cirrhosis in China. This retrospective study revealed that patients with cirrhosis who presented with HE, ascites, or SBP had a higher risk of rehospitalization. Additionally, the study found that hypertension and SBP could predict the length of hospitalization during initial admission. Along with variceal hemorrhage, ascites and HE are manifestations of hepatic decompensation in patients (25). Based on these results, it is crucial to focus on controlling the progression of patient complications, particularly HE, ascites, and SBP, in order to reduce readmissions in patients with cirrhosis and alleviate their financial burden. Diuretics, antibiotics, and albumin should be administered early and reasonably to control the progression of ascites and SBP. To control the progression of HE, the American Association for the Study of Liver Diseases recommends the assessment of covert HE in patients with cirrhosis, as covert HE is a precursor of overt HE (26). A prospective trial suggested that a high dose/frequency treatment of overt HE would reduce readmission within 30 days in patients with cirrhosis (27). By implementing these strict measures to manage the development of complications in patients with cirrhosis, we can improve their physical condition and overall quality of life, as well as reduce their readmission.
HE is a significant complication of decompensated cirrhosis and is associated with poor outcomes (28). Overt HE results in hospital admissions and high 1-year and 5-year mortality (29). The interplay among increased ammonia concentrations, alterations in amino acid metabolism, and inflammation is central to this disease (30). The presence of HE in patients with cirrhosis is thought to be associated with hospital readmission, increased mortality, impaired quality of life, and greater fall risk (31). A study concluded that HE was most strongly associated with readmission within 30 (OR 3.23, 95%CI 2.97–3.52) and 90 days (OR 3.07, 95%CI 2.86–3.30) (15). Patients who were diagnosed with HE had median survivals of 0.95 and 2.5 years for those aged <65 or ≥ 65 years, respectively (32). A cohort study of 1,560 patients concluded that patients with grade 3–4 HE during hospitalization had higher MELD scores and mortality (72%) than those with grade 1–2 or no HE (33). HE was also the main reason for repeated readmission within 3 months (34). Our study aligns with these findings, emphasizing the importance of early identification and intervention in controlling the progression. According to the practice guidelines, controlling precipitating factors of overt HE is of paramount importance. Special drug treatments, such as lactulose, antibiotics, and rifaximin, are part of management (26). This proactive approach serves as a robust strategy to effectively reduce readmissions in patients with cirrhosis.
Ascites and SBP are significant complications commonly observed in patients with cirrhosis and are closely linked to their worsening condition. Specifically, ascites has been associated with a higher risk of 30-day readmission (15). Other features of cirrhosis, including gastrointestinal bleeding, infections, and renal failure, pose significant risks to the patients’ overall outcomes. These factors contribute to higher readmission rates, and a consistent relationship exists between readmission and subsequent mortality (9). SBP is a complication that specifically occurs in patients with ascites and tends to recur (35). Reports have indicated that the 30-day readmission rate for SBP is 25.6% (36). Ascites is a common complication of decompensated cirrhosis and increases the risk of further complications such as SBP and umbilical hernias, which may lead to readmission for further therapy (37). Our study concluded that ascites and SBP were associated with rehospitalization in patients with cirrhosis, which is similar to the reports above. Consequently, when patients develop ascites, it is essential to implement preventive measures against infections to mitigate the risks associated with SBP and reduce the likelihood of readmission. In this study, esophageal variceal bleeding did not increase the risk of readmission. This may be due to variceal eradication through early endoscopic control after endoscopic band ligation, which has been identified as a significant predictor of 90-day readmission in patients with cirrhosis. Similarly, a comprehensive review concluded that cirrhotic patients with diabetes had a higher risk of HE, elevated portal pressure, gastrointestinal bleeding, and increased susceptibility to bacterial infections and HCC (38). These factors contributed to the patient readmission rates. In a retrospective cohort study involving 12,442 patients who underwent liver transplantation, recipients with diabetes had longer hospital stays, higher peri-transplant mortality, inferior graft outcomes, and lower patient survival (39). Additionally, another study highlighted that patients with liver cirrhosis and type 2 diabetes mellitus (T2DM) had a significantly increased median length of hospital stay, doubled rate of non-cirrhosis-related admissions, and 1.35-fold increased rate of cirrhosis-related admissions compared to those without T2DM (40). While our study did not find diabetes to be a predictor of length of hospitalization, it revealed that diabetes affects long-term readmission in patients with cirrhosis. These findings suggest that patients with cirrhosis who also had diabetes were at a higher risk of prolonged hospital stay, and their overall condition would deteriorate if diabetes remained uncontrolled. Therefore, it is crucial to rigorously manage the development of comorbidities in patients with cirrhosis and diabetes to delay disease progression and improve outcomes.
In our cohort, we observed that hypertension and SBP were predictors of the length of hospitalization in patients with cirrhosis. Hypertension is a prevalent chronic disease worldwide and is often associated with other conditions, such as cardiovascular disease and non-alcoholic fatty liver disease (41, 42). Recent research has revealed several factors related to the length of hospital stay in patients with cirrhosis, including malnutrition, diabetes, infection, paracentesis use, SBP, and bariatric surgery (38, 43–46). Interestingly, there is limited research specifically exploring the relationship between hypertension and length of hospitalization in patients with cirrhosis. According to the literature, patients with cirrhosis often experience decreased splanchnic resistance and increased peripheral resistance. These changes are influenced by altered circulating vasoactive substances and the reactivity of the vasomotor and regulatory systems. Consequently, patients may present with hypotension, normotension, or hypertension (47, 48). One possible reason for the scarcity of studies is that arterial hypertension is not commonly observed in patients with cirrhosis. Some studies have suggested that hypertension exerts a protective effect against the occurrence of ascites or other complications related to circulatory dysfunction (49). Nevertheless, certain types of liver diseases, such as alcoholic fatty liver and HBV with renal involvement, may be accompanied by arterial hypertension (47). Our study population consisted predominantly of patients with alcohol-related and viral liver diseases, accounting for 74.3% of enrolled patients. This could explain why hypertension emerged as a significant predictor of the length of hospitalization in our study. Combined with previous literature, we believe that the prolonged hospital stay of patients with cirrhosis and hypertension may be related to kidney injury caused by hypertension and may also be related to the damage of some target organs by inflammatory factors released by the body during hypertension (48). However, further investigations are necessary to validate and elucidate the relationship between hypertension and length of hospitalization in patients with cirrhosis, particularly to explore its association with different types of liver diseases, such as alcohol-related and viral liver diseases. A potential research direction may be that hypertension leads to abnormal vasomotor function, which leads to abnormal secretion of hormones regulating blood pressure, adversely affecting liver function, and thus prolonging hospital stay in patients with cirrhosis.
Our study has several limitations. First, the indications for readmission varied over time, even within the same hospital, which was a major limitation of this retrospective analysis. Second, a notable omission in our study was the lack of data on specific treatments received by the patients, which could potentially serve as predictors of readmission and duration of hospitalization. Future studies should incorporate treatment data to provide more comprehensive insight. Third, the underlying mechanisms by which HE and SBP affect readmission rates in patients with cirrhosis have not yet been explored. Further investigations into these mechanisms are necessary as they could help develop more effective strategies to reduce readmission rates. Mortality is a key factor that may have influenced the outcomes of this study. However, because this was a retrospective study, we were unable to obtain mortality data, which is another limitation. Post-discharge management, including treatment of the underlying liver disease, medications for complications (such as beta-blockers, rifaximin, and diuretics), treatment of comorbidities, and patient adherence, could significantly affect the risk of readmission. Unfortunately, the lack of comprehensive post-discharge data prevented us from investigating this aspect. Moreover, non-liver-related deaths and readmissions are common among patients with cirrhosis. This area requires further exploration in future studies. Finally, although our study identified hypertension as a predictor of the length of hospitalization in patients with cirrhosis, we did not extensively explore this relationship. Future research should thoroughly examine the association between hypertension and hospitalization duration, particularly in the context of different liver diseases, such as alcohol-related and viral liver diseases. Our study highlighted hypertension as a predictor of the length of hospitalization in patients with cirrhosis; however, we did not extensively investigate this relationship. Therefore, additional research should be conducted to thoroughly explore the association between hypertension and the length of hospitalization, particularly considering different types of liver diseases, such as alcohol-related and viral liver diseases.
5 Conclusion
Patients with cirrhosis and conditions such as HE, ascites, SBP, and diabetes may have a higher risk of rehospitalization. Additionally, hypertension and SBP appear to be associated with the length of hospitalization in these patients. Clinicians might benefit from focusing on the early management of complications such as HE, SBP, and diabetes in patients with cirrhosis. However, these conclusions should be interpreted with caution, and additional studies are required to confirm these associations.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by ethics committee of Peking University People’s Hospital (No. 2023PHB214-001). The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because this is a retrospective study and we collected enrolled patients’ sociodemographic, clinical, and hospitalization characteristics.
Author contributions
SW: Writing – original draft, Writing – review & editing. LZ: Writing – original draft, Writing – review & editing. JL: Writing – original draft. JF: Formal analysis, Methodology, Writing – original draft. JG: Methodology, Supervision, Writing – review & editing, Formal analysis, Funding acquisition, Investigation, Resources, Writing – original draft. RH: Methodology, Supervision, Writing – review & editing, Formal analysis, Funding acquisition, Investigation, Resources, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This project (RDL2024-06, RDJ2022-21) was supported by Peking University People’s Hospital Scientific Research Development Funds and Peking University Hepatology Institute Qi-Min Project.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Asrani, SK, Devarbhavi, H, Eaton, J, and Kamath, PS. Burden of liver diseases in the world. J Hepatol. (2019) 70:151–71. doi: 10.1016/j.jhep.2018.09.014
2. Collaborators, GBDC. The global, regional, and national burden of cirrhosis by cause in 195 countries and territories, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet Gastroenterol Hepatol. (2020) 5:245–66. doi: 10.1016/S2468-1253(19)30349-8
3. Xiao, J, Wang, F, Wong, NK, He, J, Zhang, R, Sun, R, et al. Global liver disease burdens and research trends: analysis from a Chinese perspective. J Hepatol. (2019) 71:212–21. doi: 10.1016/j.jhep.2019.03.004
4. Chen, W, Zheng, R, Baade, PD, Zhang, S, Zeng, H, Bray, F, et al. Cancer statistics in China, 2015. CA Cancer J Clin. (2016) 66:115–32. doi: 10.3322/caac.21338
5. Ge, PS, and Runyon, BA. Treatment of patients with cirrhosis. N Engl J Med. (2016) 375:767–77. doi: 10.1056/NEJMra1504367
6. Stepanova, M, De Avila, L, Afendy, M, et al. Direct and indirect economic burden of chronic liver disease in the United States. Clin Gastroenterol Hepatol. (2017) 15:e5:759–766.e5. doi: 10.1016/j.cgh.2016.07.020
7. Rosenblatt, R, Cohen-Mekelburg, S, Shen, N, Tafesh, Z, Lucero, C, Kumar, S, et al. Cirrhosis as a comorbidity in conditions subject to the hospital readmissions reduction program. Am J Gastroenterol. (2019) 114:1488–95. doi: 10.14309/ajg.0000000000000257
8. Ebhohon, E, Ogundipe, OA, and Adejumo, AC. Alarming rate of 30-day hospital readmissions in patients with liver cirrhosis. Ann Transl Med. (2021) 9:1608. doi: 10.21037/atm-21-5258
9. Orman, ES, Ghabril, M, Emmett, TW, and Chalasani, N. Hospital readmissions in patients with cirrhosis: a systematic review. J Hosp Med. (2018) 13:490–5. doi: 10.12788/jhm.2967
10. Dai, J, Zhao, J, Du, Y, McNeil, EB, and Chongsuvivatwong, V. Biomarkers and sociodemographic factors predicting one-year readmission among liver cirrhosis patients. Ther Clin Risk Manag. (2019) 15:979–89. doi: 10.2147/TCRM.S203883
11. Asrani, SK, Kouznetsova, M, Ogola, G, Taylor, T, Masica, A, Pope, B, et al. Increasing health care burden of chronic liver disease compared with other chronic diseases, 2004-2013. Gastroenterology. (2018) 155:e4:719–729.e4. doi: 10.1053/j.gastro.2018.05.032
12. Hui, Y, Wang, H, Guo, G, Yang, W, Zhang, X, Yang, J, et al. Association between quality of life defined by euro Qol group 5 dimension and composite inferior outcome among inpatients with cirrhosis. Clin Interv Aging. (2024) 19:551–60. doi: 10.2147/cia.S444842
13. Garg, SK, Goyal, H, Obaitan, I, Shah, PA, Sarvepalli, S, Jophlin, LL, et al. Incidence and predictors of 30-day hospital readmissions for liver cirrhosis: insights from the United States National Readmissions Database. Ann Transl Med. (2021) 9:1052. doi: 10.21037/atm-20-1762
14. Allen, AM, Kim, WR, Moriarty, JP, Shah, ND, Larson, JJ, and Kamath, PS. Time trends in the health care burden and mortality of acute on chronic liver failure in the United States. Hepatology. (2016) 64:2165–72. doi: 10.1002/hep.28812
15. Tapper, EB, Halbert, B, and Mellinger, J. Rates of and reasons for hospital readmissions in patients with cirrhosis: a multistate population-based cohort study. Clin Gastroenterol Hepatol. (2016) 14:e2:1181–1188.e2. doi: 10.1016/j.cgh.2016.04.009
16. Ginès, P, Krag, A, Abraldes, JG, Solà, E, Fabrellas, N, and Kamath, PS. Liver cirrhosis. Lancet. (2021) 398:1359–76. doi: 10.1016/s0140-6736(21)01374-x
17. Backus, LI, Belperio, PS, Shahoumian, TA, and Mole, LA. Impact of sustained Virologic response with direct-acting antiviral treatment on mortality in patients with advanced liver disease. Hepatology. (2018) 69:487–97. doi: 10.1002/hep.29408
18. Carrat, F, Fontaine, H, Dorival, C, Simony, M, Diallo, A, Hezode, C, et al. Clinical outcomes in patients with chronic hepatitis C after direct-acting antiviral treatment: a prospective cohort study. Lancet. (2019) 393:1453–64. doi: 10.1016/s0140-6736(18)32111-1
19. Tonon, M, and Piano, S. Alcohol-related cirrhosis: the most challenging etiology of cirrhosis is more burdensome than ever. Clin Mol Hepatol. (2021) 27:94–6. doi: 10.3350/cmh.2020.0305
20. Yip, TC-F, Fan, J-G, and Wong, VW-S. China’s fatty liver crisis: a looming public health emergency. Gastroenterology. (2023) 165:825–7. doi: 10.1053/j.gastro.2023.06.008
21. Wong, MCS, Huang, JLW, George, J, et al. The changing epidemiology of liver diseases in the Asia–Pacific region. Nat Rev Gastroenterol Hepatol. (2018) 16:57–73. doi: 10.1038/s41575-018-0055-0
22. Committee of Hepatology, Chinese Research Hospital Association; Fatty Liver Expert Committee, Chinese Medical Doctor Association; National Workshop on Fatty Liver and Alcoholic Liver Disease, Chinese Society of Hepatology; National Workshop on Liver and Metabolism, Chinese Society of Endocrinology, Chinese Medical Association. Expert recommendations on standardized diagnosis and treatment for fatty liver disease in China. Zhonghua Gan Zang Bing Za Zhi. (2019) 27:748–53. doi: 10.3760/cma.j.issn.1007-3418.2019.10.003
23. Horan, TC, Andrus, M, and Dudeck, MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. (2008) 36:309–32. doi: 10.1016/j.ajic.2008.03.002
24. Jalan, R, Fernandez, J, Wiest, R, Schnabl, B, Moreau, R, Angeli, P, et al. Bacterial infections in cirrhosis: a position statement based on the EASL special conference 2013. J Hepatol. (2014) 60:1310–24. doi: 10.1016/j.jhep.2014.01.024
25. Yanny, B, Winters, A, Boutros, S, and Saab, S. Hepatic encephalopathy challenges, burden, and diagnostic and therapeutic approach. Clin Liver Dis. (2019) 23:607–23. doi: 10.1016/j.cld.2019.07.001
26. American Association for the Study of Liver Diseases; European Association for the Study of the Liver. Hepatic encephalopathy in chronic liver disease: 2014 practice guideline by the European Association for the Study of the Liver and the American Association for the Study of Liver Diseases. J Hepatol. (2014) 61:642–59. doi: 10.1016/j.jhep.2014.05.042
27. Tapper, EB, Finkelstein, D, Mittleman, MA, Piatkowski, G, Chang, M, and Lai, M. A quality improvement initiative reduces 30-day rate of readmission for patients with cirrhosis. Clin Gastroenterol Hepatol. (2016) 14:753–9. doi: 10.1016/j.cgh.2015.08.041
28. Zhang, L, Zhang, W, Wang, J, Jin, Q, Ma, D, and Huang, R. Neutrophil-to-lymphocyte ratio predicts 30-, 90-, and 180-day readmissions of patients with hepatic encephalopathy. Front Med. (2023) 10:10. doi: 10.3389/fmed.2023.1185182
29. Jepsen, P, Ott, P, Andersen, PK, Sørensen, HT, and Vilstrup, H. Clinical course of alcoholic liver cirrhosis: a Danish population-based cohort study. Hepatology. (2010) 51:1675–82. doi: 10.1002/hep.23500
30. Wijdicks, EFM, and Longo, DL. Hepatic encephalopathy. N Engl J Med. (2016) 375:1660–70. doi: 10.1056/NEJMra1600561
31. Frenette, CT, Levy, C, and Saab, S. Hepatic encephalopathy-related hospitalizations in cirrhosis: transition of care and closing the revolving door. Dig Dis Sci. (2022) 67:1994–2004. doi: 10.1007/s10620-021-07075-2
32. Tapper, EB, Aberasturi, D, Zhao, Z, Hsu, CY, and Parikh, ND. Outcomes after hepatic encephalopathy in population-based cohorts of patients with cirrhosis. Aliment Pharmacol Ther. (2020) 51:1397–405. doi: 10.1111/apt.15749
33. Bajaj, JS, O’Leary, JG, Tandon, P, Wong, F, Garcia-Tsao, G, Kamath, PS, et al. Hepatic encephalopathy is associated with mortality in patients with cirrhosis independent of other extrahepatic organ failures. Clin Gastroenterol Hepatol. (2017) 15:e4:565–574.e4. doi: 10.1016/j.cgh.2016.09.157
34. Bajaj, JS, Reddy, KR, Tandon, P, Wong, F, Kamath, PS, Garcia-Tsao, G, et al. The 3-month readmission rate remains unacceptably high in a large north American cohort of patients with cirrhosis. Hepatology. (2016) 64:200–8. doi: 10.1002/hep.28414
35. Abdel-Razik, A, Abdelsalam, M, Gad, DF, Abdelwahab, A, Tawfik, M, Elzehery, R, et al. Recurrence of spontaneous bacterial peritonitis in cirrhosis: novel predictors. Eur J Gastroenterol Hepatol. (2020) 32:718–26. doi: 10.1097/MEG.0000000000001578
36. Mousa, N, Abdel-Razik, A, Elbaz, S, Salah, M, Abdelaziz, M, Habib, A, et al. A risk score to predict 30-day hospital readmission rate in cirrhotic patients with spontaneous bacterial peritonitis. Eur J Med Res. (2023) 28:168. doi: 10.1186/s40001-023-01126-2
37. European Association for the Study of the Liver. EASL clinical practice guidelines for the management of patients with decompensated cirrhosis. J Hepatol. (2018) 69:406–60. doi: 10.1016/j.jhep.2018.03.024
38. Coman, LI, Coman, OA, Badarau, IA, Paunescu, H, and Ciocirlan, M. Association between liver cirrhosis and diabetes mellitus: a review on hepatic outcomes. J Clin Med. (2021) 10:10. doi: 10.3390/jcm10020262
39. Hoehn, RS, Singhal, A, Wima, K, Sutton, JM, Paterno, F, Steve Woodle, E, et al. Effect of pretransplant diabetes on short-term outcomes after liver transplantation: a national cohort study. Liver Int. (2015) 35:1902–9. doi: 10.1111/liv.12770
40. Ahn, SB, Powell, EE, Russell, A, Hartel, G, Irvine, KM, Moser, C, et al. Type 2 diabetes: a risk factor for hospital readmissions and mortality in Australian patients with cirrhosis. Hepatol Commun. (2020) 4:1279–92. doi: 10.1002/hep4.1536
41. Al Ghorani, H, Gotzinger, F, Bohm, M, and Mahfoud, F. Arterial hypertension - clinical trials update 2021. Nutr Metab Cardiovasc Dis. (2022) 32:21–31. doi: 10.1016/j.numecd.2021.09.007
42. Liu, J, Lv, H, Wang, J, Zhu, Q, Chen, G, Jiang, Y, et al. Blood pressure stratification for predicting liver fibrosis risk in metabolic dysfunction associated fatty liver disease. Ann Hepatol. (2023) 28:100892. doi: 10.1016/j.aohep.2022.100892
43. Yang, W, Guo, G, Cui, B, Li, Y, Sun, M, Li, C, et al. Malnutrition according to the global leadership initiative on malnutrition criteria is associated with in-hospital mortality and prolonged length of stay in patients with cirrhosis. Nutrition. (2023) 105:111860. doi: 10.1016/j.nut.2022.111860
44. Singal, AK, Salameh, H, and Kamath, PS. Prevalence and in-hospital mortality trends of infections among patients with cirrhosis: a nationwide study of hospitalised patients in the United States. Aliment Pharmacol Ther. (2014) 40:105–12. doi: 10.1111/apt.12797
45. Gaetano, JN, Micic, D, Aronsohn, A, Reddy, G, te, H, Reau, NS, et al. The benefit of paracentesis on hospitalized adults with cirrhosis and ascites. J Gastroenterol Hepatol. (2016) 31:1025–30. doi: 10.1111/jgh.13255
46. Khajeh, E, Aminizadeh, E, Eslami, P, Ramouz, A, Kulu, Y, Billeter, AT, et al. Outcomes of bariatric surgery in patients with obesity and compensated liver cirrhosis. Surg Obes Relat Dis. (2022) 18:727–37. doi: 10.1016/j.soard.2022.03.011
47. Henriksen, JH, and Moller, S. Liver cirrhosis and arterial hypertension. World J Gastroenterol. (2006) 12:678–85. doi: 10.3748/wjg.v12.i5.678
48. Wenzel, UO, Bode, M, Köhl, J, and Ehmke, H. A pathogenic role of complement in arterial hypertension and hypertensive end organ damage. Am J Phys Heart Circ Phys. (2017) 312:H349–54. doi: 10.1152/ajpheart.00759.2016
Keywords: liver cirrhosis, readmission, hepatic encephalopathy, spontaneous bacterial peritonitis, hypertension
Citation: Wang S, Zhang L, Li J, Feng J, Gao J and Huang R (2025) Hepatic encephalopathy and spontaneous bacterial peritonitis are associated with increased liver-related readmissions in cirrhosis. Front. Med. 12:1417222. doi: 10.3389/fmed.2025.1417222
Edited by:
Xingshun Qi, General Hospital of Northern Theater Command, ChinaReviewed by:
Samer Al-Dury, Sahlgrenska University Hospital, SwedenWaleed Eldars, Mansoura University, Egypt
Copyright © 2025 Wang, Zhang, Li, Feng, Gao and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rui Huang, c3RyYW5nZWhlYWRAMTYzLmNvbQ==; Jie Gao, Z2FvamllXzExMzFAMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Shan Wang1,2†
Shan Wang1,2† Jiajun Feng
Jiajun Feng Jie Gao
Jie Gao Rui Huang
Rui Huang