- 1Department of Orthopaedic Surgery, Yangpu Hospital, Tongji University School of Medicine, Shanghai, China
- 2Department of Orthopaedics, Zhongda Hospital, School of Medicine, Southeast University, Nanjing, China
- 3Orthopaedic Trauma Institute (OTI), School of Medicine, Southeast University, Nanjing, China
Background: Various factors contribute to postoperative delirium (POD) in elderly patients undergoing hip fracture surgeries. Sarcopenia was defined as the progressive loss of skeletal muscle mass and strength associated with aging. The aim of this study was to explore the prevalence of POD and sarcopenia in geriatric patients undergoing hip fracture surgeries and to investigate the correlation between preoperative sarcopenia and POD.
Methods: After applying specific inclusion and exclusion criteria, the information of 234 patients were retrospectively collected. POD was screened for with 4A’s Test and diagnosed with DSM-5 criteria. The incidences of POD and sarcopenia were calculated. The demographic and perioperative features as well as comorbidities of delirious and non-delirious patients were analyzed and the risk factors analysis for POD in elderly hip fracture patients were conducted through univariate analysis and multivariate regression analysis.
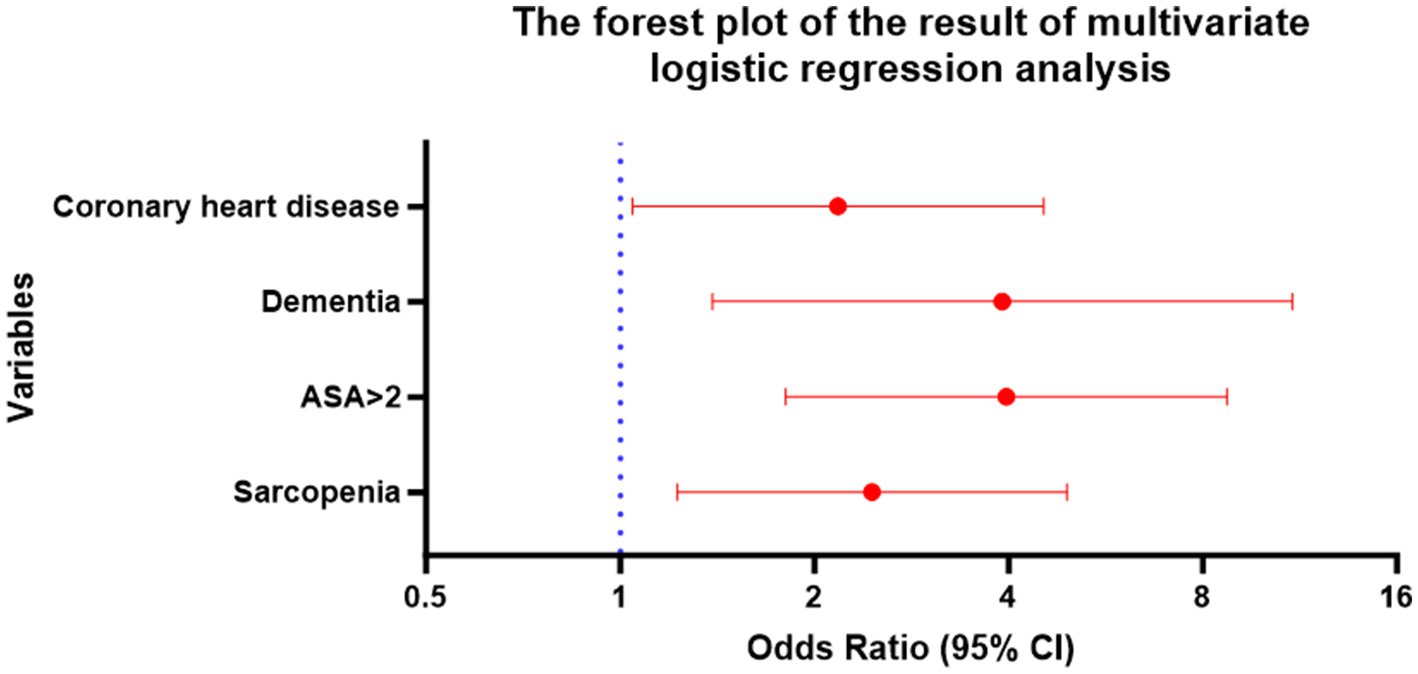
Results: 48.7% patients were diagnosed of POD, 78.95% of which were females. The average age of delirious and non-delirious patients were 84.75 years and 80.63 years, respectively. The incidence of sarcopenia was 41.02% for all the included patients with 60.53% for delirious patients and 20.55% for non-delirious patients. Results of univariate analysis showed that sarcopenia (OR:5.281, 95%CI 2.988–9.337, p = 0.000), age increase per year (OR:1.128, 95CI 1.070–1.190, p = 0.000), operation duration increase (OR:1.017, 95%CI 1.004–1.030, p = 0.011), intertrochanteric fracture (OR:2.571, 95%CI 1.517–4.358, p = 0.000), dementia (OR: 6.029, 95%CI 2.532–14.359, p = 0.000), ASA > 2 (OR: 6.955, 95%CI 3.461–13.976, p = 0.000), coronary heart disease (OR: 2.201, 95%CI 1.257–3.854, p = 0.006), renal insufficiency (OR: 2.215, 95%CI 1.187–4.133, p = 0.012) and COPD (OR: 2.554, 95%CI 1.414–4.615, p = 0.002) were risk factors for POD. Results of multivariate analysis identified sarcopenia (OR: 2.457, 95% CI 1.226–4.923, p = 0.011), ASA > 2 (OR: 3.968, 95% CI 1.805–8.722, p = 0.001), dementia (OR: 3.912, 95% CI 1.390–11.014, p = 0.010) and coronary heart disease (OR: 2.176, 95% CI 1.044–4.538, p = 0.038) as independent risk factors for POD in geriatric hip fracture patients.
Conclusion: The incidences of POD and sarcopenia in geriatric hip fracture patients are high. Sarcopenia is an independent risk factor for POD in geriatric hip fracture patients.
1 Introduction
Delirium is a reversible cognitive disorder caused by temporary damage to neurons due to an underlying systemic disturbance (1). Delirium diagnosis is elucidated in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), which is published by the American Psychiatric Association. The DSM-5 offers guidelines for classifying and diagnosing mental health disorders. As per the DSM-5, delirium is identified by acute impairments in attention, cognition, and/or consciousness that manifest rapidly, fluctuate in intensity, and are accompanied by a deviation from normal cognitive functioning. Delirium can be provoked by various potential factors, which encompass acute medical conditions, substance use or withdrawal, as well as trauma or surgical procedures (2).
Postoperative delirium (POD) is a common complication observed among patients undergoing hip surgery. The incidence of POD in hip fracture patients may reach as high as around 50% (3, 4). POD is linked to several negative outcomes, including prolonged hospital stays (5, 6), greater healthcare costs (6); diminished rehabilitation progress with impaired functional and cognitive recovery, and even the potential development of new-onset dementia (7–9) and increased short-term and long-term mortality (10, 11).
Various factors contribute to the likelihood of POD in elderly patients undergoing hip fracture surgeries. Previous research has identified advanced age, preoperative dementia, low albumin levels, diabetes, surgical delay and pain as contributors to delirium (12–14). Fortunately, delirium prevention strategies works in reducing the incidence of delirium and associated adverse outcomes (15). Therefore, it is crucial to screen for risk factors associated with POD in hip surgery patients to implement preventive measures effectively.
Sarcopenia was defined as the progressive loss of skeletal muscle mass and strength associated with aging (16). It is a common condition in older patients with hip fracture, ranging from 21 to 74% in men and 12 to 68% in women, depending on the diagnostic criteria used. In recent years, evidences globally suggested that sarcopenia is associated with cognitive impairment (17). Experimental studies indicated that delirium and sarcopenia might share similar pathophysiologic mechanisms including inflammatory reaction and reactive oxidative stress and a potential biological cross-talk (18).
However, whether sarcopenia at admission is a risk factor for POD in hip fracture patients has not been studied. Thus, we designed a study to provide insights into the issue. This study retrospectively analyzes medical records to delineate the incidence of POD and sarcopenia in geriatric hip fracture patients and explore whether sarcopenia at admission serves as a potential risk factor for POD.
2 Materials and methods
2.1 Study design and patients
After having got approval from the institutional ethical committee, this retrospective cohort study utilized data from electronic medical records at a tertiary care university hospital in Shanghai, China. From February 1, 2022 to January 31, 2024, a total of 361 patients were admitted to the tertiary hospital for hip fracture treatment.
Researchers gathered data by scrutinizing patients’ records obtained from the electronic medical records system. Inclusion criteria were defined as follows: (1) patients aged 65 years or older; (2) patients who received internal fixation for an intertrochanteric fracture or hemiarthroplasty for a femoral neck fracture; (3) hip fractures caused by low energy. Exclusion criteria were defined as follows: (1) individuals with multiple fractures including hip fractures; (2) patients demonstrating delirium at admission or before surgery; (3) patients whose fracture happened more than 3 days before admission; (4) pathological fracture; (5) the American Society of Anesthesiologists (ASA) rating scale was Classes V; (6) patients who died before surgery or with 3 days after surgery; (7) patients with incomplete medical records.
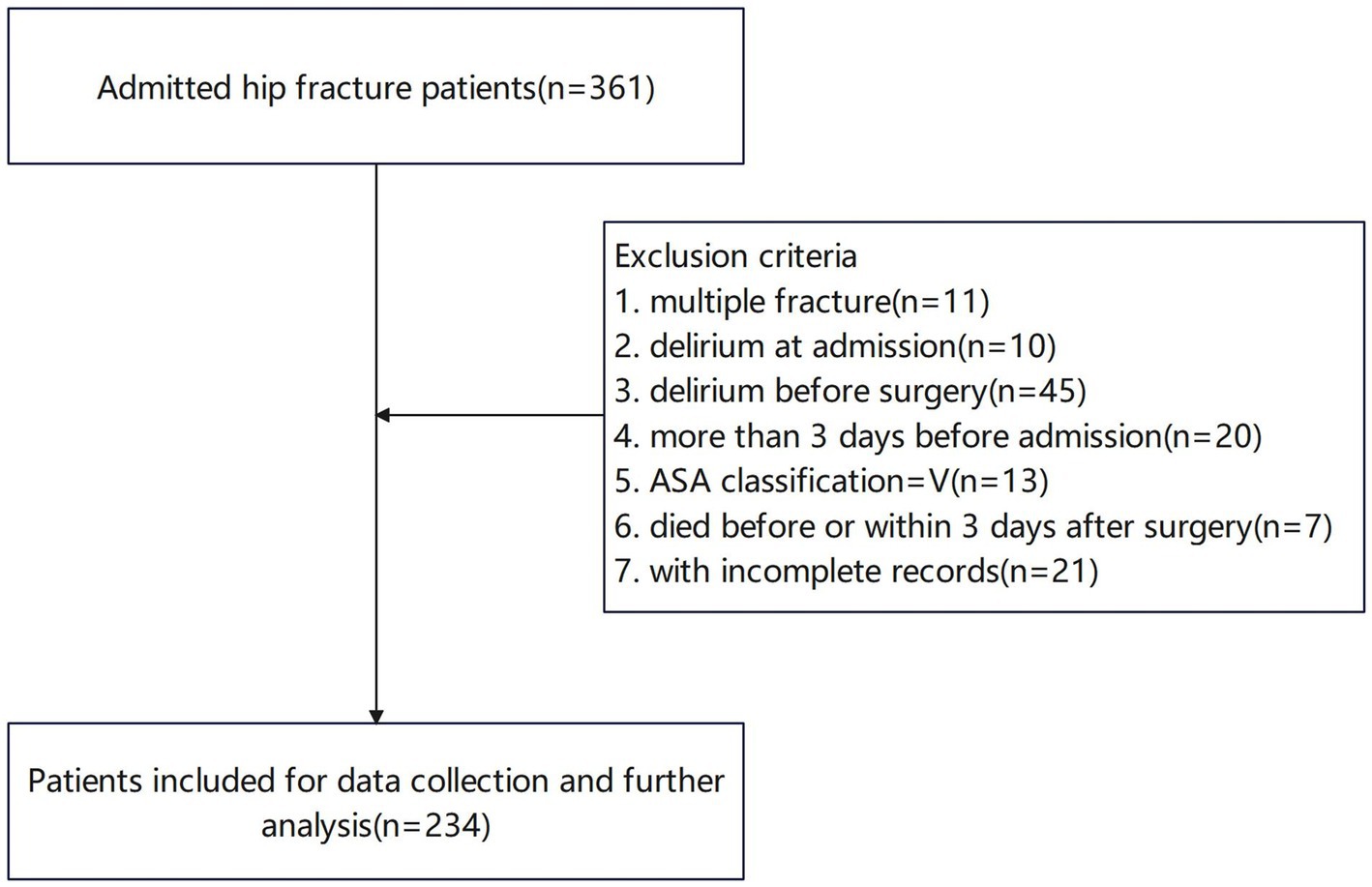
After applying specific inclusion and exclusion criteria, 234 patients fulfilled the criteria and their information were collected for further analysis (Figure 1).
2.2 Data collection
The demographic, clinical, and perioperative information of patients was obtained from the hospital information system and patients’ medical records. The first two authors reviewed the medical records to verify patients’ demographic, clinical, and perioperative information independently. Any inconsistencies or disagreements were resolved by the corresponding author.
Variables were grouped into the following categories:(1) sociodemographic data (age and gender) and body mass index (BMI); (2) past medical history (dementia, sarcopenia, hypertension, coronary heart disease, diabetes mellitus, chronic obstructive pulmonary diseases (COPD), stroke, and renal insufficiency); (3) post-injury factors (operation delay, fracture type), among which the operation delay means the days from admission to operation; (4) surgery related factors [ASA classification, anesthesia type, operation duration (min), and whether the patient received intraoperative blood transfusion] and post-operative factors (the lowest hemoglobin within 5 postoperative days, the lowest albumin within 5 postoperative days, and whether the patient received transfusion within 5 days after surgery).
2.3 Assessment criteria for delirium and sarcopenia
Delirium was screened with the 4AT (19). The 4AT is a brief and pragmatic tool for the screening of delirium which has demonstrated acceptable diagnostic test accuracy in acute medical wards. A score higher than 4 is strongly predictive of delirium. Patients screened positive during the 4AT assessment will be further evaluated for the presence of delirium using the DSM-5 criteria (20). The sarcopenia was evaluated for every patient on the day of admission. Sarcopenia was evaluated according to the Asian Working Group for Sarcopenia (AWGS) 2019 consensus. Those who demonstrated both low muscle strength (handgrip strength <28 kg for men and <18 kg for women) and low calf circumference (<34 cm in men, <33 cm in women) were identified as sarcopenia patients (46).
2.4 Statistical analysis
We conducted statistical analysis with SPSS 23.0 software. Statistical significance was established at a threshold of p < 0.05. Measurement data are depicted as mean ± standard deviation (mean ± SD). To compare data between two groups, we employed the t-test. Counting data underwent analysis using the chi-squared test (χ2). The Variance Inflation Factor (VIF) was employed to assess multicollinearity among the variables and measure the extent to which the estimated regression coefficient is inflated because of correlations among predictor variables. A cut-off point was established, with the VIF being required to be less than 5. We found that the VIFs of all the variables were less than 5. Following this, the Hosmer–Lemeshow Test was conducted to assess the goodness of fit of the binary logistic regression model. We got a p-value of 0.144 that was larger than 0.05, which showed that the model fits well. Then we conducted a comparison between patients with delirium and those without using univariate analysis. Variables with a p-value less than 0.05 from the univariate analysis were included in the multivariate analysis to ascertain the independent risk factors for POD. The Graphpad Prism 10.1.2 was use to generalize the forest plot for the visualization of multivariate logistic regression analysis results.
3 Results
3.1 Subjects’ characteristics
A flowchart depicting the screening process for hip fracture patients derived from our center’s hip fracture database was presented in Figure 1. After excluding patients who did not meet the inclusion criteria, a total of 234 patients were deemed eligible for the study.
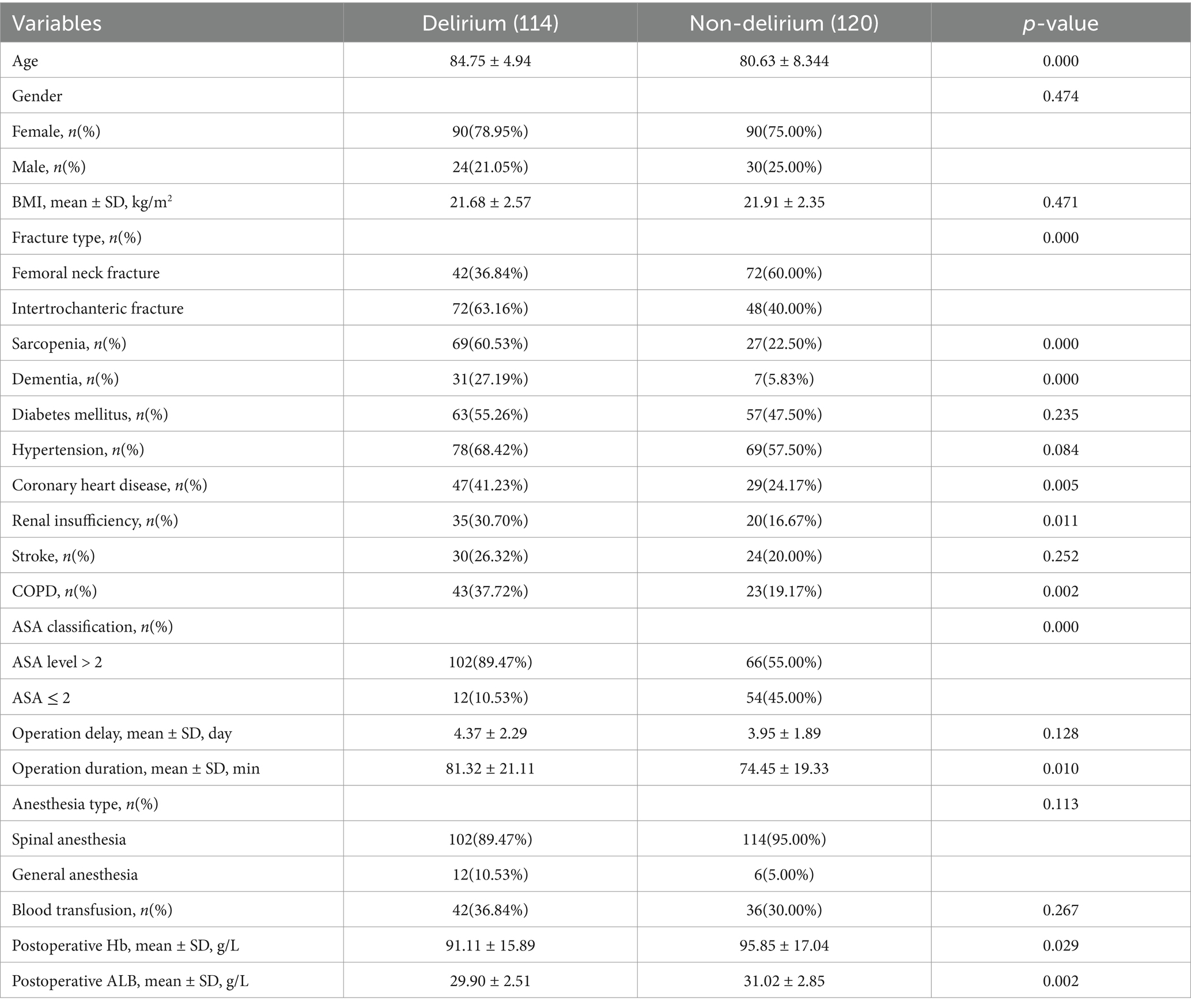
The demographic and perioperative characteristics of these 234 patients were showed in Table 1. 48.72% patients were diagnosed of POD, 78.95% of which were females. The delirious patients were significantly older than non-delirious patients (84.75 vs. 80.63 years, p = 0.000). In delirious patients, 63.16% patients suffered from intertrochanteric fractures while only 40% non-delirious patients were diagnosed with intertrochanteric fractures (p = 0.000). The incidence of sarcopenia was 41.02% for all the included patients and the incidence in delirious patients was about 3 times (60.53% vs. 20.55%, p = 0.000) that in non-delirious patients. The average waiting time for surgery from admission to surgery were 4.37 days and 3.95 days, respectively, for the two group (p = 0.128). In the two groups, 89.47% (102 out of 114) and 55.00% (66 out of 120) patients had an ASA level > 2 (p = 0.000). Two hundred sixteen patients received spinal anesthesia and 78 patients received intraoperative/postoperative blood transfusion (p = 0.113). Besides, delirious patients showed significantly larger incidence of dementia (27.19% vs. 5.83%, p = 0.000), coronary heart disease (41.23% vs. 24.17%, p = 0.005), renal insufficiency (30.70% vs. 16.67%, p = 0.011), COPD (37.72% vs. 19.17%, p = 0.002), longer operation duration (81.32 ± 21.11 min vs. 74.45 ± 19.33 min, p = 0.010), lower postoperative hemoglobin level (91.11 ± 15.89 g/L vs. 95.85 ± 17.04 g/L, p = 0.029) and albumin level (29.90 ± 2.51 g/L vs. 31.02 ± 2.85 g/L, p = 0.002).
3.2 The results of univariate analysis
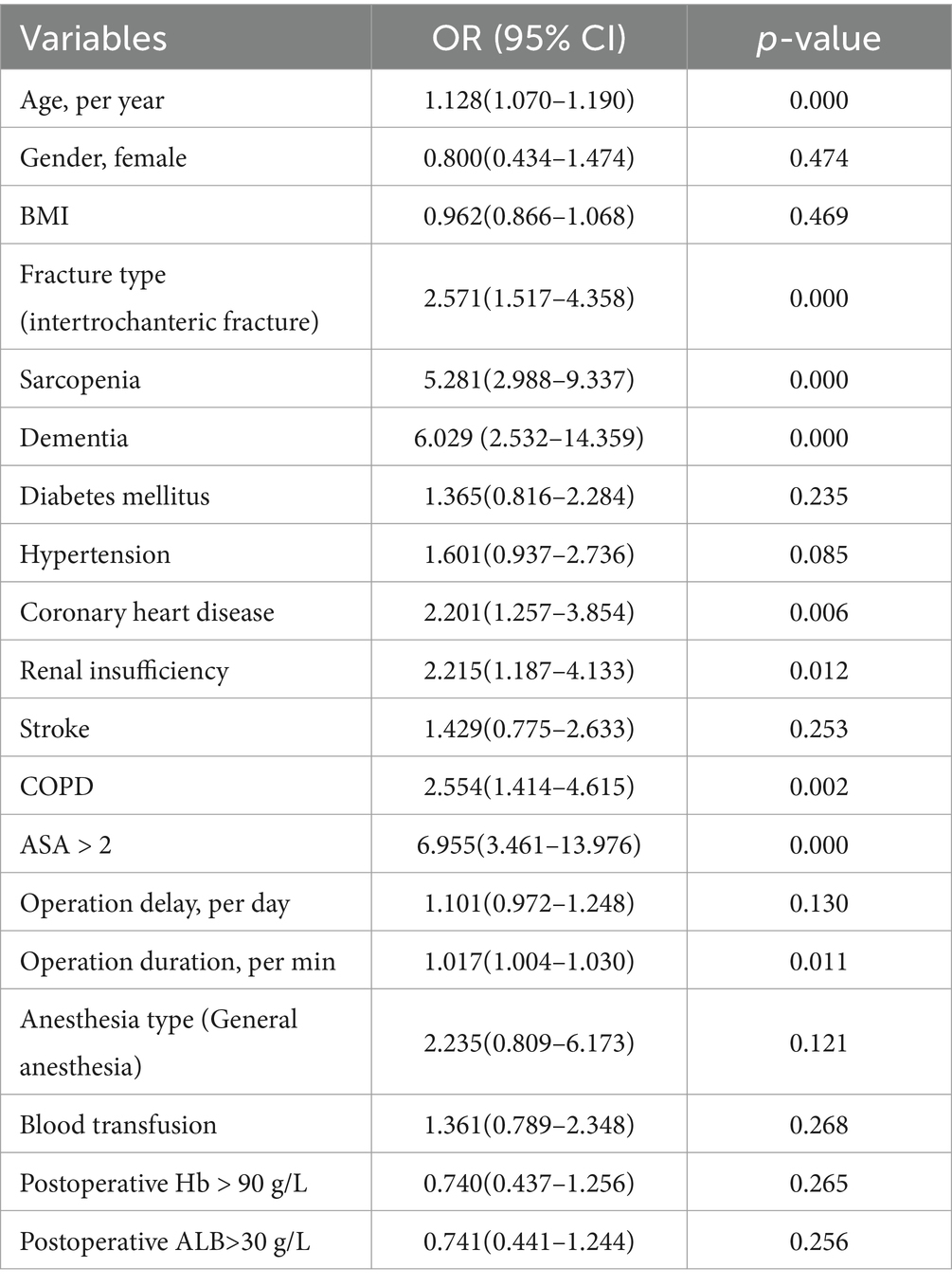
Risk factors for POD in geriatric hip fracture patients were analyzed. The results of univariate analysis of risk factors for POD in elderly hip fracture patients showed that patients with sarcopenia were at a higher risk of POD (OR: 5.281, 95% CI 2.988–9.337, p = 0.000). Further, age increase (OR: 1.128, 95% CI 1.070–1.190, p = 0.000), operation duration increase (OR: 1.017, 95% CI 1.004–1.030, p = 0.011) also increased the incidence of delirium. Intertrochanteric fracture patients suffered more from POD compared with femoral neck fracture patients (OR: 2.571, 95% CI 1.517–4.358, p = 0.000). Those with coexisting dementia were also more likely to suffer from POD than those without preoperative dementia (OR: 6.029, 95% CI 2.532–14.359, p = 0.000). Besides, ASA > 2, coronary heart disease, renal insufficiency and COPD were risk factors for POD (Table 2).
3.3 The results of multivariate logistic regression analysis
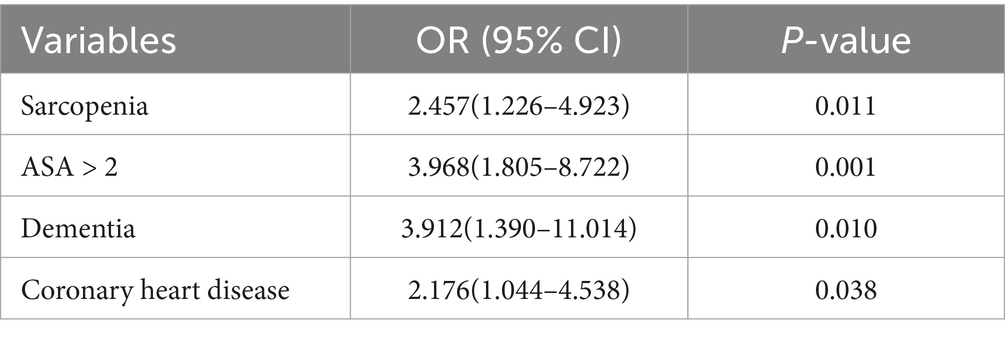
Multivariate logistic regression analysis was performed using variables showing statistical significance in the univariate analysis. Results of multivariate analysis identified sarcopenia (OR: 2.457, 95% CI 1.226–4.923, p = 0.011), ASA > 2 (OR: 3.968, 95% CI 1.805–8.722, p = 0.001), dementia (OR: 3.912, 95% CI 1.390–11.014, p = 0.010) and coronary heart disease (OR: 2.176, 95% CI 1.044–4.538, p = 0.038) as independent risk factors for POD in geriatric hip fracture patients (Table 3 and Figure 2).
4 Discussion
The POD is a common postoperative complication in geriatric hip fracture patients. Its high incidence and adverse outcomes make it crucial to identify modifiable risk factors and to implement effective interventions to prevent its occurrence (1). Despite loads of studies investigated risk factors for POD, to our knowledge, this is the first study to explore the potential association between sarcopenia and POD in hip fracture patients. The results provided a compelling evidence of a link between sarcopenia and POD in older patients undergoing hip fracture surgeries. Consequently, clinicians should be vigilant for postoperative delirium in patients who are diagnosed with preoperative sarcopenia. Then actions including analgesics, multi-disciplinary comprehensive care and pharmacological treatment should be taken for postoperative delirium prevention (10).
4.1 High incidence of POD and sarcopenia
We identified the high incidences of POD (48.72%) and sarcopenia (41.02%), which are compatible to some former studies. In our study, we excluded 55 delirious patients at admission or before surgery, so the incidence of POD in the whole patients may be higher than this. In the studies of Jeon and Sohng et al. (22) and Shin et al. (4), 45.02 and 51.28% patients were diagnosed of delirium, respectively. In the study of Oberai et al. (23) in 2021 including 6,672 geriatric hip fracture patients, 2,599 (39.0%) patients were delirious. The incidence of sarcopenia in hip fracture patients may reach about 50% in different races (21, 24, 25). In our study, the incidence of sarcopenia was less than 50% (41.02%) for all the included patients. This may due to that patients with preoperative delirium or delirium at admission were excluded, who may be more susceptible to sarcopenia. According to former studies, sarcopenia is a risk factor for hip fractures (26–28), which underscores the importance of addressing possible sarcopenia as a preventive measure to reduce the incidence of hip fractures. The high incidence may result from that sarcopenia is associated with osteoporosis and falls among elderly people (29). And the coexistence of osteoporosis and sarcopenia has been recently defined as a syndrome termed ‘osteosarcopenia’. Besides, the prevalence of sarcopenia will increase after hip fracture surgeries (27). Postoperative treatment concerning sarcopenia including long-term exercise therapy and anti-osteoporosis drugs should be utilized to decrease the incidence of postoperative sarcopenia and to prevent the aggravation of sarcopenia (27).
4.2 Clinical studies concerning the association between POD and sarcopenia
Very few papers studied the association between delirium and sarcopenia. Mosk et al. (30) found that low skeletal muscle mass was independently associated with POD in elderly patients undergoing colorectal cancer surgery. Zucchelli et al. (31) verified that low muscle mass is independently associated with delirium in acute hospital medical wards, emergency departments, rehabilitation wards, nursing homes and hospices in Italy. However, these studies only explored the association between POD and low muscle mass rather than sarcopenia. According to Dong et al. (32), preoperative sarcopenia was independently associated with POD in geriatric patients after gastrointestinal cancer surgery. Moellmann et al. (33) carried out a prospective clinical study on 421 patients from 4 different surgical disciplines including orthopedic and trauma, finding that if there is an indication of sarcopenia, the association with delirium will increase 5.56-fold. Our study is the first study having identified sarcopenia as an independent risk factor for POD in elderly hip fractures.
4.3 Potential pathophysiological mechanisms shared by POD and sarcopenia
Although little studies have been conducted to explore the shared pathophysiological mechanisms linking brain and muscle disorders, there are still some evidences suggesting similar pathophysiologic mechanisms that may be shared by delirium and sarcopenia.
Firstly, elderly hip fracture patients often show elevated serum levels of pro-inflammatory cytokines, including tumor necrosis factor-alpha (TNF-α), interleukin-1 (IL-1), IL-6, and IL-8 (18, 34). Once these inflammatory mediators cross the blood–brain barrier, they can activate microglia, resulting in synaptic and neuronal dysfunction, which may ultimately contribute to the onset of delirium (35). Meanwhile, inflammatory reaction plays an important role in sarcopenia development. Elevated IL-6 and TNF-α plasma level were found in geriatric patients and TNF-α was proved to be a factor associated with muscle mass and strength decline (36–38). Secondly, reactive oxidative stress (ROS) was found to be associated with both delirium and sarcopenia. Under specific circumstances, such as during surgery, the brain becomes particularly susceptible to damage from oxidative stress, which may result in neuronal dysfunction and delirium (39). ROS was found directly associated with muscle mass in normal aging and the intake of antioxidants, circulating antioxidant levels, and markers of oxidative damage have shown varying correlations with sarcopenia (40, 41). Thirdly, the direct association between them was provided by Nemoto et al. (42) that low skeletal muscle mass is associated with perioperative neurocognitive disorder due to decreased neurogenesis.
4.4 Other risk factors for POD
In our study, higher ASA level was identified as an independent risk factor for POD. This is consistent with some previous research findings of Haynes et al. (43), Kim et al. (44), and Wang et al. (14). It suggested that physiological reserve may be associated with the evolution of cognitive deficits after surgery for the preoperative ASA classification serves as an initial evaluation of a patient’s ability to tolerate anesthesia and provides a fundamental indication of their overall physical condition.
As in our study, many former studies recognized dementia as an independent risk factor for POD (13, 43, 44). As two distinct clinical syndromes, delirium and dementia are connected by overlapping clinical characteristics and shared pathogenic mechanisms. Delirium can influence the progression of dementia by accelerating cognitive decline, functional deterioration, and the loss of independence. Furthermore, delirium may serve as an initial indicator of dementia (34).
Seldom studies found that coronary heart disease act as a risk factor for POD. Wang et al. found that delirium was significantly associated with coronary heart disease through univariate analysis (45). However, it was found an insignificant factor through multivariate regression analysis. Our study suggests that more attention be paid to those suffering from coronary heart disease.
Some former studies listed age increase and male as independent risk factors for POD (43–45), although the results of our multivariate logistic regression analysis show that advanced age and male are not an independent risk factor. More attention still should be paid to older patients in routine care.
4.5 Strengths and limitations
The findings of our study should be interpreted considering certain limitations. Firstly, this is a single-center retrospective study, and the sample size is not very big. In the future, multi-center prospective cohort studies of large samples should be conducted for further verification. Secondly, the diagnosis of sarcopenia were based on low muscle strength and low calf circumference. Although calf circumference is strongly correlated with skeletal muscle mass, patients with obesity or other conditions that can lead to increased calf circumference and decreased muscle mass may not have been accurately identified. Lastly, as those diagnosed with delirium at admission or before operation were excluded, our findings need further validation for whether the results can be generalized to all the hip fracture patients.
Strength of this study is that it is the first study to list sarcopenia as a potential risk factor for POD and has identified sarcopenia as an independent risk factor for POD in elderly hip fractures. This provides a reference for the identification of high-risk patients for postoperative delirium. Besides, delirium was screened with validated screening tools and diagnosed with standard criteria during routine care.
5 Conclusion
In conclusion, the incidences of POD and sarcopenia in hip fracture patients are high. Sarcopenia is an independent risk factor for POD in geriatric hip fracture patients. We recommend prospective large-sample clinical studies and experimental studies exploring the underlying mechanisms of the association between POD and sarcopenia be conducted in the future.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of Yangpu Hospital, Tongji University School of Medicine. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin due to the retrospective nature of the research.
Author contributions
Y-MQ: Conceptualization, Formal analysis, Writing – original draft. H-TL: Formal analysis, Writing – review & editing. S-MC: Conceptualization, Funding acquisition, Supervision, Writing – review & editing. S-JH: Methodology, Writing – review & editing. S-CD: Methodology, Writing – review & editing. C-DL: Formal analysis, Writing – review & editing. Y-QC: Formal analysis, Writing – review & editing. Y-FR: Conceptualization, Supervision, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by National Natural Science Foundation of China (No. 81772323) and Natural Science Foundation of Shanghai (No. 23ZR14593000).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Swarbrick, CJ, and Partridge, J. Evidence-based strategies to reduce the incidence of postoperative delirium: a narrative review. Anaesthesia. (2022) 77:92–101. doi: 10.1111/anae.15607
2. Wilson, JE, Mart, MF, Cunningham, C, Shehabi, Y, Girard, TD, MacLullich, A, et al. Delirium. Nat Rev Dis Primers. (2020) 6:90. doi: 10.1038/s41572-020-00223-4
3. Pollmann, CT, Mellingsæter, MR, Neerland, BE, Straume-Næsheim, T, Årøen, A, and Watne, LO. Orthogeriatric co-management reduces incidence of delirium in hip fracture patients. Osteoporos Int. (2021) 32:2225–33. doi: 10.1007/s00198-021-05974-8
4. Shin, JE, Kyeong, S, Lee, JS, Park, JY, Lee, WS, Kim, JJ, et al. A personality trait contributes to the occurrence of postoperative delirium: a prospective study. BMC Psychiatry. (2016) 16:371. doi: 10.1186/s12888-016-1079-z
5. Hecht, G, Slee, CA, Goodell, PB, Taylor, SL, and Wolinsky, PR. Predictive modeling for geriatric hip fracture patients: early surgery and delirium have the largest influence on length of stay. J Am Acad Orthop Surg. (2019) 27:e293–300. doi: 10.5435/JAAOS-D-17-00447
6. Schubert, M, Schurch, R, Boettger, S, Garcia, ND, Schwarz, U, Bettex, D, et al. A hospital-wide evaluation of delirium prevalence and outcomes in acute care patients – a cohort study. BMC Health Serv Res. (2018) 18:550. doi: 10.1186/s12913-018-3345-x
7. Inouye, SK, Westendorp, RG, and Saczynski, JS. Delirium in elderly people. Lancet. (2014) 383:911–22. doi: 10.1016/S0140-6736(13)60688-1
8. Low, S, Wee, E, and Dorevitch, M. Impact of place of residence, frailty and other factors on rehabilitation outcomes post hip fracture. Age Ageing. (2021) 50:423–30. doi: 10.1093/ageing/afaa131
9. Meyer, M, Gotz, J, Parik, L, Renkawitz, T, Grifka, J, Maderbacher, G, et al. Postoperative delirium is a risk factor for complications and poor outcome after total hip and knee arthroplasty. Acta Orthop. (2021) 92:695–700. doi: 10.1080/17453674.2021.1980676
10. Chen, Y, Liang, S, Wu, H, Deng, S, Wang, F, Lunzhu, C, et al. Postoperative delirium in geriatric patients with hip fractures. Front Aging Neurosci. (2022) 14:1068278. doi: 10.3389/fnagi.2022.1068278
11. Jin, Z, Hu, J, and Ma, D. Postoperative delirium: perioperative assessment, risk reduction, and management. Br J Anaesth. (2020) 125:492–504. doi: 10.1016/j.bja.2020.06.063
12. Ahn, EJ, and Bang, SR. Risk factors associated with treatment of hyperactive postoperative delirium in elderly patients following hip fracture surgery under regional anesthesia: a nationwide population-based study. Braz J Anesthesiol. (2022) 72:213–9. doi: 10.1016/j.bjane.2021.03.020
13. Qi, YM, Li, YJ, Zou, JH, Qiu, XD, Sun, J, and Rui, YF. Risk factors for postoperative delirium in geriatric patients with hip fracture: a systematic review and meta-analysis. Front Aging Neurosci. (2022) 14:960364. doi: 10.3389/fnagi.2022.960364
14. Wang, Y, Zhao, L, Zhang, C, An, Q, Guo, Q, Geng, J, et al. Identification of risk factors for postoperative delirium in elderly patients with hip fractures by a risk stratification index model: a retrospective study. Brain Behav. (2021) 11:e32420. doi: 10.1002/brb3.2420
15. Fong, TG, and Inouye, SK. The inter-relationship between delirium and dementia: the importance of delirium prevention. Nat Rev Neurol. (2022) 18:579–96. doi: 10.1038/s41582-022-00698-7
16. Cruz-Jentoft, AJ, Baeyens, JP, Bauer, JM, Boirie, Y, Cederholm, T, Landi, F, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European working group on sarcopenia in older people. Age Ageing. (2010) 39:412–23. doi: 10.1093/ageing/afq034
17. Hu, Y, Peng, W, Ren, R, Wang, Y, and Wang, G. Sarcopenia and mild cognitive impairment among elderly adults: the first longitudinal evidence from charls. J Cachexia Sarcopenia Muscle. (2022) 13:2944–52. doi: 10.1002/jcsm.13081
18. Gamberale, R, D’Orlando, C, Brunelli, S, Meneveri, R, Mazzola, P, Foti, G, et al. Study protocol: understanding the pathophysiologic mechanisms underlying delirium in older people undergoing hip fracture surgery. BMC Geriatr. (2021) 21:633. doi: 10.1186/s12877-021-02584-1
19. Bellelli, G, Morandi, A, Davis, DH, Mazzola, P, Turco, R, Gentile, S, et al. Validation of the 4at, a new instrument for rapid delirium screening: a study in 234 hospitalised older people. Age Ageing. (2014) 43:496–502. doi: 10.1093/ageing/afu021
20. European Delirium Association, American Delirium Society. The dsm-5 criteria, level of arousal and delirium diagnosis: inclusiveness is safer. BMC Med. (2014) 12:141. doi: 10.1186/s12916-014-0141-2
21. Chen, YP, Wong, PK, Tsai, MJ, Chang, WC, Hsieh, TS, Leu, TH, et al. The high prevalence of sarcopenia and its associated outcomes following hip surgery in taiwanese geriatric patients with a hip fracture. J Formos Med Assoc. (2020) 119:1807–16. doi: 10.1016/j.jfma.2020.02.004
22. Jeon, EJ, and Sohng, KY. Risk factors and clinical outcomes of delirium after hip fracture surgery in Korean older adults: a retrospective study. Int J Gerontol. (2021) 15:25–9. doi: 10.6890/IJGE.202101_15(1).0005
23. Oberai, T, Oosterhoff, J, Woodman, R, Doornberg, JN, Kerkhoffs, G, and Jaarsma, R. Development of a postoperative delirium risk scoring tool using data from the Australian and New Zealand hip fracture registry: an analysis of 6672 patients 2017-2018. Arch Gerontol Geriatr. (2021) 94:104368. doi: 10.1016/j.archger.2021.104368
24. Kim, YK, Yi, SR, Lee, YH, Kwon, J, Jang, SI, and Park, SH. Effect of sarcopenia on postoperative mortality in osteoporotic hip fracture patients. J Bone Metab. (2018) 25:227–33. doi: 10.11005/jbm.2018.25.4.227
25. Yoo, JI, Kim, H, Ha, YC, Kwon, HB, and Koo, KH. Osteosarcopenia in patients with hip fracture is related with high mortality. J Korean Med Sci. (2018) 33:e27. doi: 10.3346/jkms.2018.33.e27
26. Ho, AW, Lee, MM, Chan, EW, Ng, HM, Lee, CW, Ng, WS, et al. Prevalence of pre-sarcopenia and sarcopenia in Hong Kong Chinese geriatric patients with hip fracture and its correlation with different factors. Hong Kong Med J. (2016) 22:23–9. doi: 10.12809/hkmj154570
27. Park, JW, Kim, HS, Lee, YK, Yoo, JI, Choi, Y, Ha, YC, et al. Sarcopenia: an unsolved problem after hip fracture. J Bone Miner Metab. (2022) 40:688–95. doi: 10.1007/s00774-022-01334-6
28. Yoo, JI, Ha, YC, Kwon, HB, Lee, YK, Koo, KH, and Yoo, MJ. High prevalence of sarcopenia in Korean patients after hip fracture: a case-control study. J Korean Med Sci. (2016) 31:1479–84. doi: 10.3346/jkms.2016.31.9.1479
29. Clynes, MA, Gregson, CL, Bruyère, O, Cooper, C, and Dennison, EM. Osteosarcopenia: where osteoporosis and sarcopenia collide. Rheumatology. (2021) 60:529–37. doi: 10.1093/rheumatology/keaa755
30. Mosk, CA, van Vugt, J, de Jonge, H, Witjes, CD, Buettner, S, Ijzermans, JN, et al. Low skeletal muscle mass as a risk factor for postoperative delirium in elderly patients undergoing colorectal cancer surgery. Clin Interv Aging. (2018) 13:2097–106. doi: 10.2147/CIA.S175945
31. Zucchelli, A, Manzoni, F, Morandi, A, Di Santo, S, Rossi, E, Valsecchi, MG, et al. The association between low skeletal muscle mass and delirium: results from the nationwide multi-Centre Italian delirium day 2017. Aging Clin Exp Res. (2022) 34:349–57. doi: 10.1007/s40520-021-01950-8
32. Dong, B, Yu, D, Zhang, H, Li, P, Li, Y, Li, C, et al. Association between preoperative sarcopenia and postoperative delirium in older patients undergoing gastrointestinal cancer surgery. Front Aging Neurosci. (2024) 16:1416569. doi: 10.3389/fnagi.2024.1416569
33. Moellmann, HL, Alhammadi, E, Boulghoudan, S, Kuhlmann, J, Mevissen, A, Olbrich, P, et al. Risk of sarcopenia, frailty and malnutrition as predictors of postoperative delirium in surgery. BMC Geriatr. (2024) 24:971. doi: 10.1186/s12877-024-05566-1
34. Simone, MJ, and Tan, ZS. The role of inflammation in the pathogenesis of delirium and dementia in older adults: a review. CNS Neurosci Ther. (2011) 17:506–13. doi: 10.1111/j.1755-5949.2010.00173.x
35. Maldonado, JR. Acute brain failure: pathophysiology, diagnosis, management, and sequelae of delirium. Crit Care Clin. (2017) 33:461–519. doi: 10.1016/j.ccc.2017.03.013
36. Bian, AL, Hu, HY, Rong, YD, Wang, J, Wang, JX, and Zhou, XZ. A study on relationship between elderly sarcopenia and inflammatory factors il-6 and tnf-α. Eur J Med Res. (2017) 22:25. doi: 10.1186/s40001-017-0266-9
37. Marzetti, E, Calvani, R, Cesari, M, Buford, TW, Lorenzi, M, Behnke, BJ, et al. Mitochondrial dysfunction and sarcopenia of aging: from signaling pathways to clinical trials. Int J Biochem Cell Biol. (2013) 45:2288–301. doi: 10.1016/j.biocel.2013.06.024
38. Sanchez-Castellano, C, Martin-Aragon, S, Bermejo-Bescos, P, Vaquero-Pinto, N, Miret-Corchado, C, Merello, DMA, et al. Biomarkers of sarcopenia in very old patients with hip fracture. J Cachexia Sarcopenia Muscle. (2020) 11:478–86. doi: 10.1002/jcsm.12508
39. Karlidag, R, Unal, S, Sezer, OH, Bay, KA, Battaloglu, B, But, A, et al. The role of oxidative stress in postoperative delirium. Gen Hosp Psychiatry. (2006) 28:418–23. doi: 10.1016/j.genhosppsych.2006.06.002
40. McKenzie, D, Bua, E, McKiernan, S, Cao, Z, and Aiken, JM. Mitochondrial dna deletion mutations: a causal role in sarcopenia. Eur J Biochem. (2002) 269:2010–5. doi: 10.1046/j.1432-1033.2002.02867.x
41. Muller, FL, Song, W, Jang, YC, Liu, Y, Sabia, M, Richardson, A, et al. Denervation-induced skeletal muscle atrophy is associated with increased mitochondrial ros production. Am J Physiol-Regul Integr Comp Physiol. (2007) 293:R1159–68. doi: 10.1152/ajpregu.00767.2006
42. Nemoto, A, Goyagi, T, Nemoto, W, Nakagawasai, O, Tan-No, K, and Niiyama, Y. Low skeletal muscle mass is associated with perioperative neurocognitive disorder due to decreased neurogenesis in rats. Anesth Analg. (2022) 134:194–203. doi: 10.1213/ANE.0000000000005681
43. Haynes, MS, Alder, KD, Toombs, C, Amakiri, IC, Rubin, LE, and Grauer, JN. Predictors and sequelae of postoperative delirium in a geriatric patient population with hip fracture. J. Am. Acad. Orthop. Surg. Glob Res Rev. (2021) 5:e20.00221. doi: 10.5435/JAAOSGlobal-D-20-00221
44. Kim, EM, Li, G, and Kim, M. Development of a risk score to predict postoperative delirium in patients with hip fracture. Anesth Analg. (2020) 130:79–86. doi: 10.1213/ANE.0000000000004386
45. Wang, CG, Qin, YF, Wan, X, Song, LC, Li, ZJ, and Li, H. Incidence and risk factors of postoperative delirium in the elderly patients with hip fracture. J Orthop Surg Res. (2018) 13:186. doi: 10.1186/s13018-018-0897-8
Keywords: sarcopenia, postoperative delirium, risk factor, geriatric, hip fracture
Citation: Qi Y-M, Li H-T, Chang S-M, Hu S-J, Du S-C, Liu C-D, Chu Y-Q and Rui Y-F (2025) Sarcopenia is a risk factor for postoperative delirium in geriatric hip fracture patients: a retrospective study. Front. Med. 11:1526240. doi: 10.3389/fmed.2024.1526240
Edited by:
Vahid Rashedi, University of Social Welfare and Rehabilitation Sciences, IranReviewed by:
Mingxing Lei, Chinese PLA General Hospital, ChinaHiroyuki Hisada, The University of Tokyo, Japan
Copyright © 2025 Qi, Li, Chang, Hu, Du, Liu, Chu and Rui. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shi-Min Chang, c2hpbWluY2hhbmcxMUBhbGl5dW4uY29t; Yun-Feng Rui, cnVpeXVuZmVuZ0AxMjYuY29t
 Yi-Ming Qi
Yi-Ming Qi Hao-Tao Li1
Hao-Tao Li1 Shi-Min Chang
Shi-Min Chang Sun-Jun Hu
Sun-Jun Hu Yun-Feng Rui
Yun-Feng Rui