- 1Department of Radiology, Suining Central Hospital, Suining, China
- 2Department of Radiology, Shehong Municipal Hospital of Traditional Chinese Medicine, Shehong, China
- 3Department of Gastroenterology, Suining Central Hospital, Suining, China
- 4Department of Radiology, The Third Hospital of Mianyang and Sichuan Mental Health Center, Mianyang, China
- 5Department of Radiology and Imaging, Institute of Rehabilitation and Development of Brain Function, The Second Clinical Medical College of North Sichuan Medical College, Nanchong Central Hospital, Nanchong, China
Background: Knowledge of the rare arc of Bühler (AOB) is limited but clinically important. At present, there is no publication of systematic review and meta-analysis on AOB in computed tomography angiography (CTA) and digital subtraction angiography (DSA) examinations.
Objective: The objective of this study was to evaluate the pooled prevalence and clinical implications of the AOB by using CTA and DSA examinations.
Methods: The PubMed, Web of Science, Scopus, Embase, Google Scholar, CBM, CNKI, WanFang, VIP, and Baidu Scholar databases were comprehensively searched for AOB-related literature. Stata 17.0 software was used to conduct the meta-analysis.
Results: Eleven publications with 3,837 patients and 65 AOB cases were included. The pooled prevalence of AOB was 1.9% (95% confidence interval: 0.8–3.2%). CTA showed a pooled prevalence of AOB of 2.0% (95% confidence interval: 0.5–4.3%) and DSA showed a pooled prevalence of AOB of 1.8% (95% confidence interval: 0.5–3.9%).
Conclusion: AOB is a rare anatomical variant, with a pooled prevalence of 1.9% in the general population. General surgeons, vascular surgeons, and interventional radiologists should consider its existence when performing relevant abdominal procedures to avoid intraoperative difficulties, visceral organ ischemia or bleeding, and other complications.
Introduction
The arc of Bühler (AOB) was first described by Bühler in 1904, and it is currently defined as the anastomotic artery between the superior mesenteric artery and the celiac trunk or its branches (1). AOB is a rare anatomical variation that may affect various interventional radiological operations (e.g., interventional embolization of aneurysms) and abdominal surgeries (e.g., pancreaticoduodenectomy) (2, 3). However, most general surgeons, vascular surgeons, and interventional radiologists do not have a sufficient understanding of the anatomy and function of AOB, which may lead to a lack of awareness of potential adverse outcomes (such as iatrogenic injuries) during or after surgeries (4, 5). Therefore, when performing abdominal related surgeries, it is important to keep in mind the existence of AOB.
Computed tomography angiography (CTA) can noninvasively evaluate vascular diseases and anatomical variations in various parts of the body, and digital subtraction angiography (DSA) is currently considered the reference standard to diagnose vascular diseases in all parts of the body (6, 7). As a result, both CTA and DSA are clinically valuable to evaluate the prevalence and clinical implications of AOB.
With the rapid development of evidence-based medicine (EBM), the theory and concept of evidence-based anatomy (EBA) came into being. EBA applies the basic principles and research methods of EBM to the field of anatomy (8, 9). The actual prevalence of AOB remains unclear, with estimates in the literature suggesting it to be less than 3% (1). Thus, this study aimed to use a systematic review and meta-analysis (i.e., EBA) to review and analyse the literature on AOB and evaluate its reported prevalence and clinical implications based on CTA and DSA to guide the diagnosis and treatment of clinically related diseases.
Materials and methods
Inclusion and exclusion criteria
Studies of the general population who underwent abdominal CTA or DSA to evaluate the presence of anatomical variations in the abdominal vasculature were included in this systematic review and meta-analysis. The outcome index was the prevalence of AOB. In this present study, AOB was defined as the anastomotic artery between the superior mesenteric artery and the celiac trunk or its branches (1). The exclusion criteria were: (I) reviews, case reports, editorials, comments, and conference abstracts; (II) autopsies of animal or human cadavers; (III) duplicate publications; and (IV) an inability to obtain the full text, incomplete literature data, or data that could not be used to calculate the prevalence of AOB.
According to our previous experience in systematic review and meta-analysis, there are two common types of duplicate publications. The first type is multiple publication of the same research data in different languages. The second type is that some time following the publication of a study, a second study by the same author(s) on the same topic, with a larger sample size, was published. In the second situation, we will exclude the earlier study and only include the latest study with the largest sample size.
Literature retrieval strategy
The English databases of PubMed, Web of Science, Embase, Scopus, and Google Scholar; and the Chinese databases of CBM (China Biology Medicine Disc), CNKI (China National Knowledge Infrastructure), WanFang, VIP, and Baidu Scholar were all comprehensively searched. All cross-sectional studies on the prevalence of AOB were collected. The time frame for retrieval was from the establishment of each database to September 30, 2024. A combination of subject and free words that were modified based on the characteristics of each database was used for retrieval. Simultaneously, the references included in the study were searched to supplement and obtain relevant data. The searched words included in this study were Bühler, Buhler, arc, Bühler arc, Buhler arc, coeliac, coeliac trunk, celiac, celiac trunk, coeliac artery, celiac artery, celiac axis, celiac axis, trunk, axis, and superior mesenteric artery.
Literature screening and data extraction
Two researchers (with eight and 10 years of experience in abdominal radiology) independently examined the literature, extracted the data, and cross-checked it. If there were disagreements, they were resolved by discussion or consultation with a third researcher (with 15 years of experience in abdominal radiology). The title of the article was reviewed first throughout the literature screening procedure. Upon eliminating studies that were clearly irrelevant, the abstract and complete text were examined to decide whether or not to incorporate the study into the analysis. If necessary, the authors of the original study were contacted by e-mail or telephone to obtain data that were not reported but were important for this study. First author, publication time (year), country, research type (CTA or DSA), total sample size, number and prevalence of AOB (%), and AOB type were all included in the data.
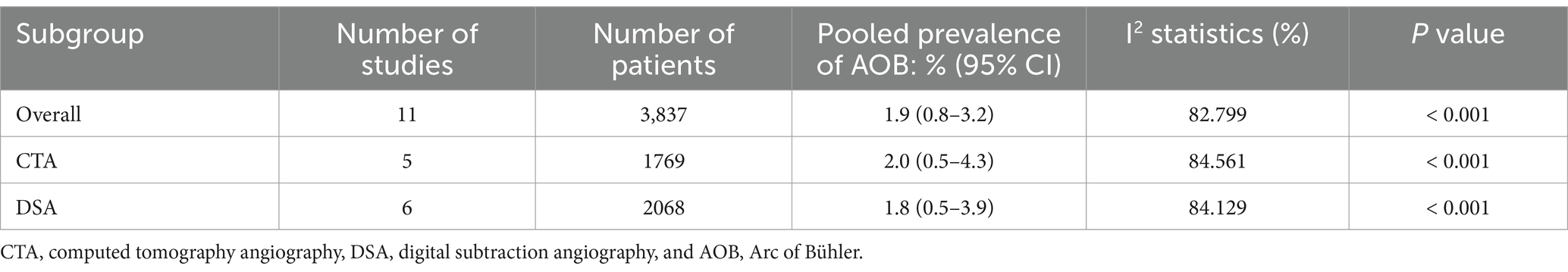
Bias risk assessment
The same two researchers who performed the literature screening and data extraction procedures independently evaluated the risk of bias and cross-checked the results. Bias risk assessment was performed by using the “Anatomical Quality Assessment Tool” recommended by the International Evidence-Based Anatomy Working Group (10). The tool consisted of a series of questions in five domains: (I) research objectives and characteristics of research subjects, (II) research design, (III) methodology characterization, (IV) descriptive anatomy, and (V) reporting of results. If all questions in a particular domain were answered ‘yes’, then the risk of bias in that domain was determined to be ‘low’; if any question in a particular domain was answered ‘no’ or ‘unclear’, the risk of bias in this domain was, respectively, determined to be ‘high’ or ‘unclear’.
Statistical analysis
Data were collected and collated by using an Excel (Microsoft Corp., Redmond, WA, USA) table, and a single-group meta-analysis was performed using the metaprop module of Stata software (version 17.0; StataCorp, College Station, TX, USA). The prevalence of AOB was used as the statistic for effect analysis, and a 95% confidence interval (CI) was provided. Heterogeneity between studies was evaluated using χ2 tests and I2 statistics. χ2 tests (p < 0.10) indicated statistical heterogeneity. An I2 value of 0–40% was considered “might not be important,” that of 30–60% was considered “may represent moderate heterogeneity,” that of 50–90% was considered “may represent substantial heterogeneity,” and that of 75–100% was considered “considerable heterogeneity” (8). For the meta-analysis, the fixed-effects model was to be applied if there was no statistical heterogeneity among the outcomes. In cases where there was statistical heterogeneity in the data, the source of the heterogeneity was investigated further, and after ruling out the impact of clear clinical heterogeneity, a random-effects model was employed for the meta-analysis. The level of the meta-analysis was set as α = 0.05. A subgroup analysis was conducted according to the type of study (CTA or DSA) to further explore the possible factors affecting the AOB prevalence.
Results
Literature screening procedures and results
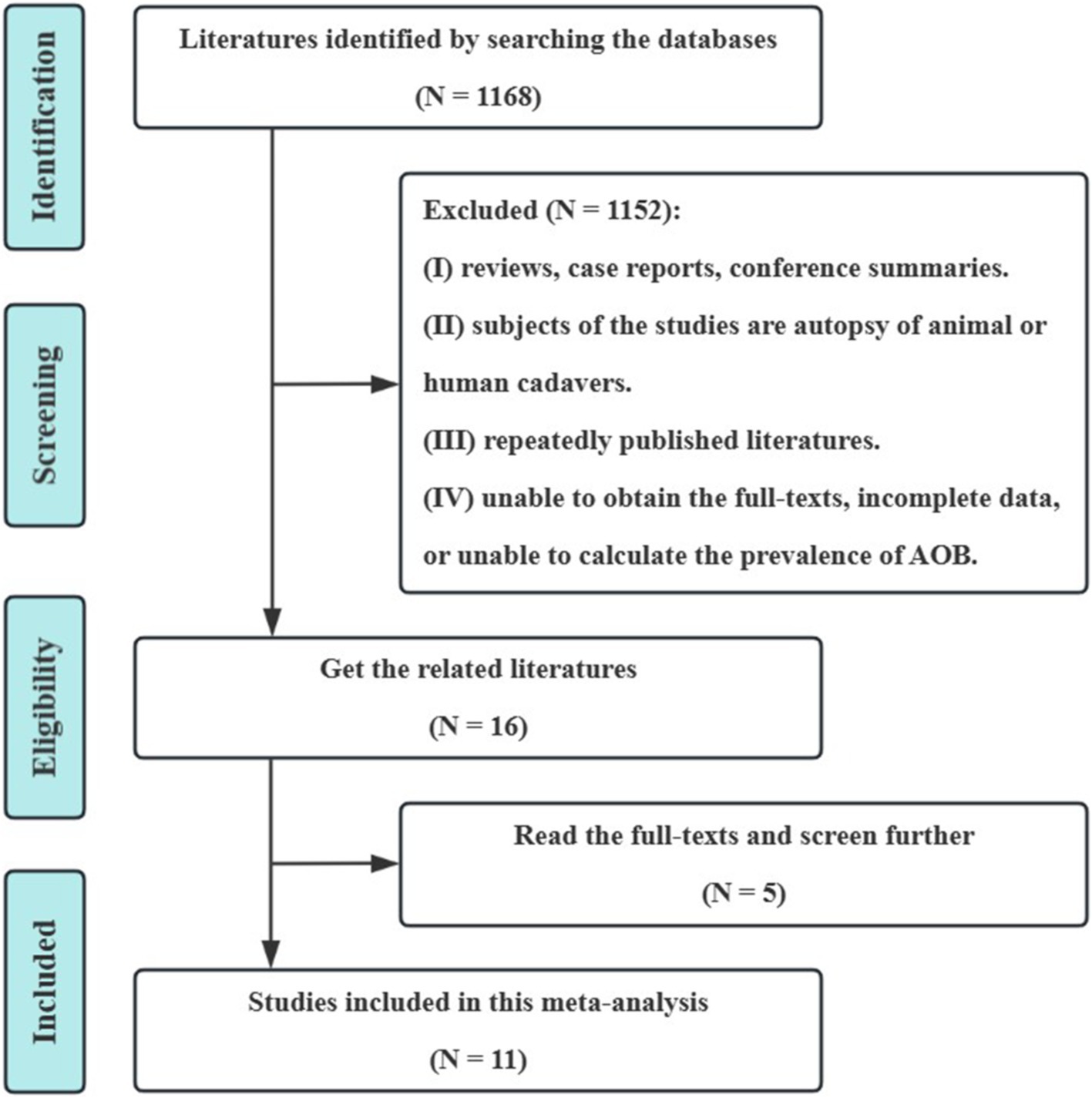
On the basis of the preliminary screening, 1,168 pertinent studies were included. Eleven cross-sectional studies were eventually included following layer-by-layer screening (11–21). These included 3,837 participants (with 65 cases of AOB), of which 1769 were examined using CTA and 2068 were examined using DSA. The literature screening procedure and the results are shown in Figure 1.
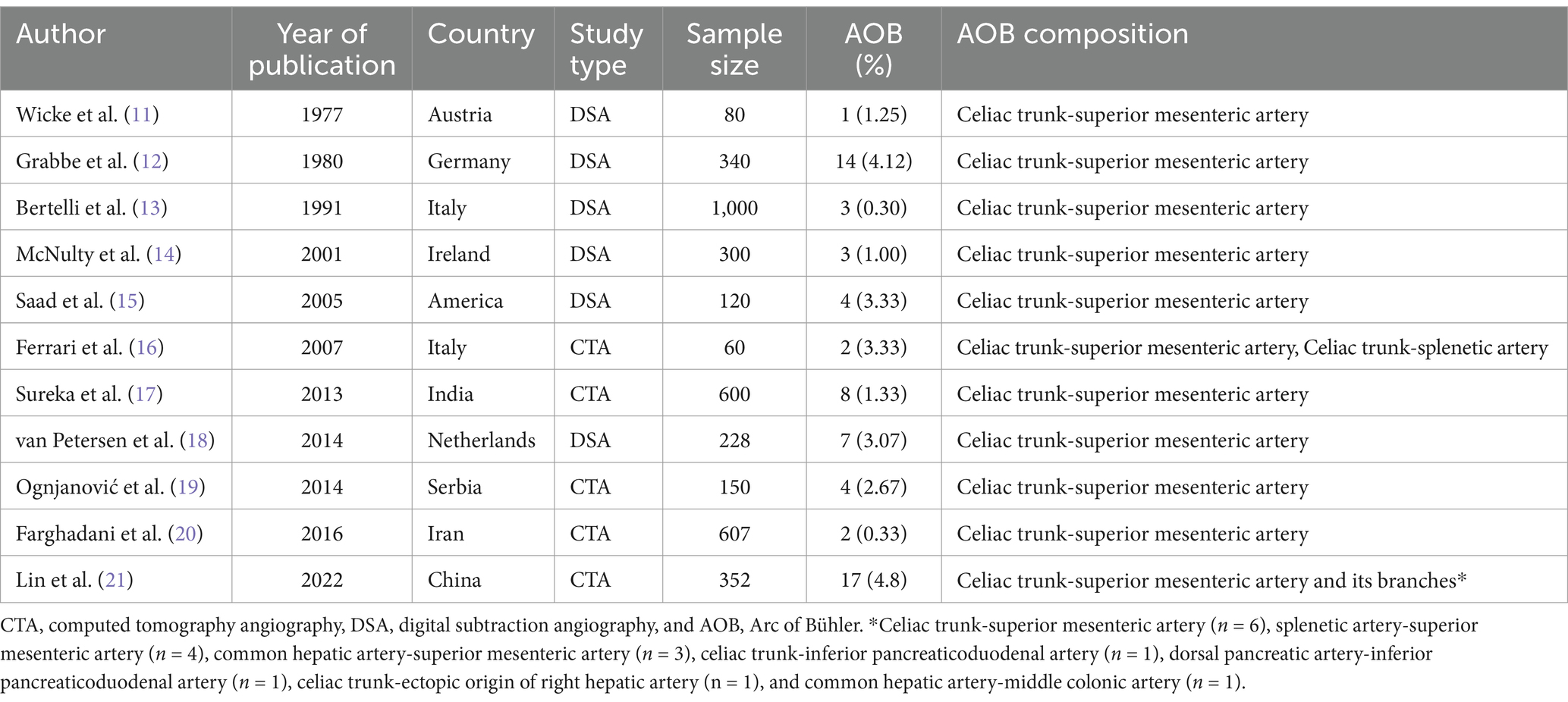
Basic features and bias risk assessment results
The basic characteristics of the included studies and the results of the bias risk evaluation are presented in Tables 1, 2, respectively. The bias risk of eight studies in terms of “research objectives and characteristics of research subjects” was determined to be ‘high’, as the method of subject selection introduced bias into the study to some extent (n = 8), and that of seven studies in “methodology characterization” was determined to be ‘high’ due to the absence of appropriate measures for reducing inter- and intra-observer variability (n = 7). The bias risk in the remaining domains was determined to be ‘low’ (Figure 2).
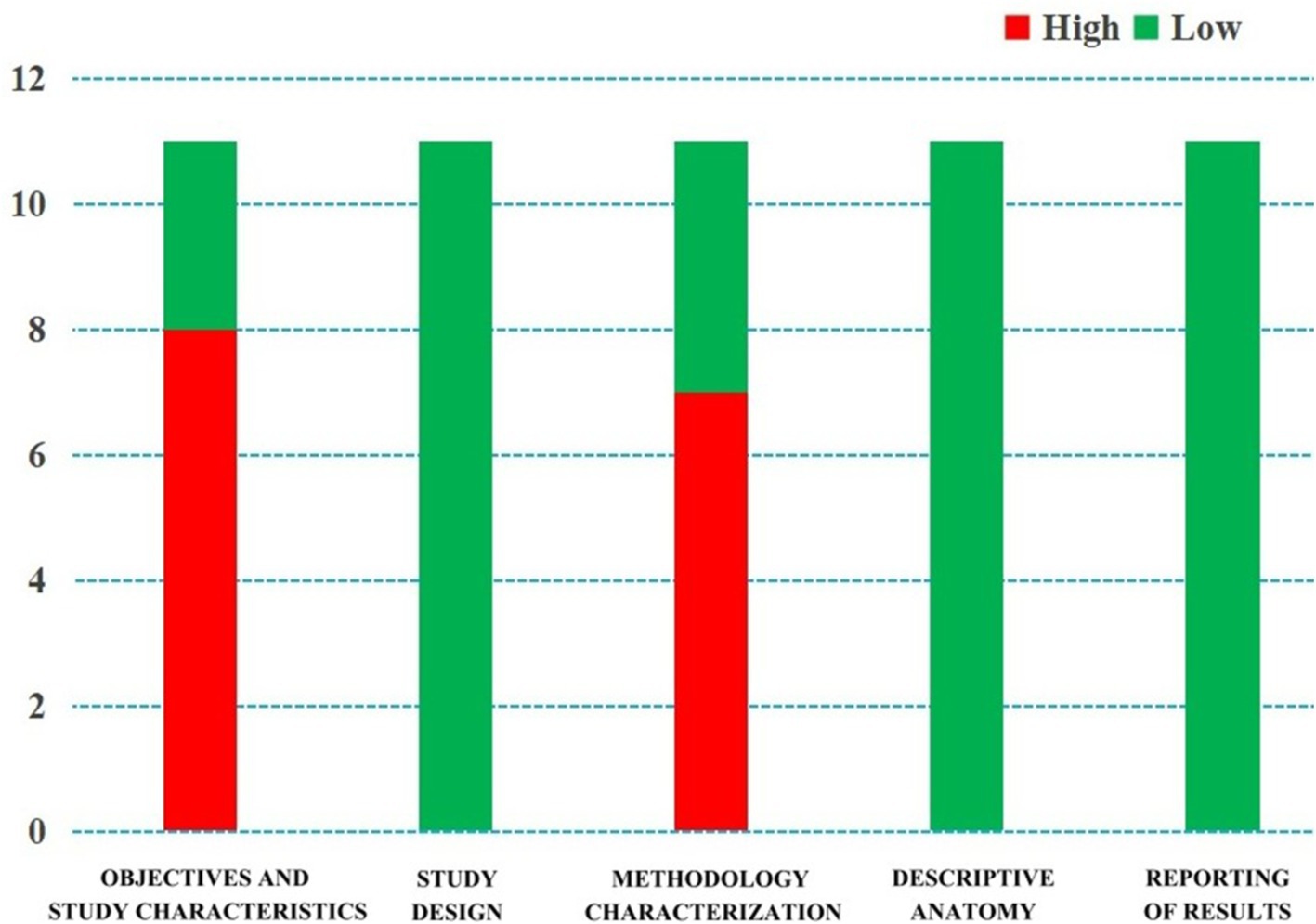
Figure 2. Quality evaluation by the “Anatomical Quality Assessment (AQUA) Tool” for the included studies.
Results of the meta-analysis
Pooled prevalence
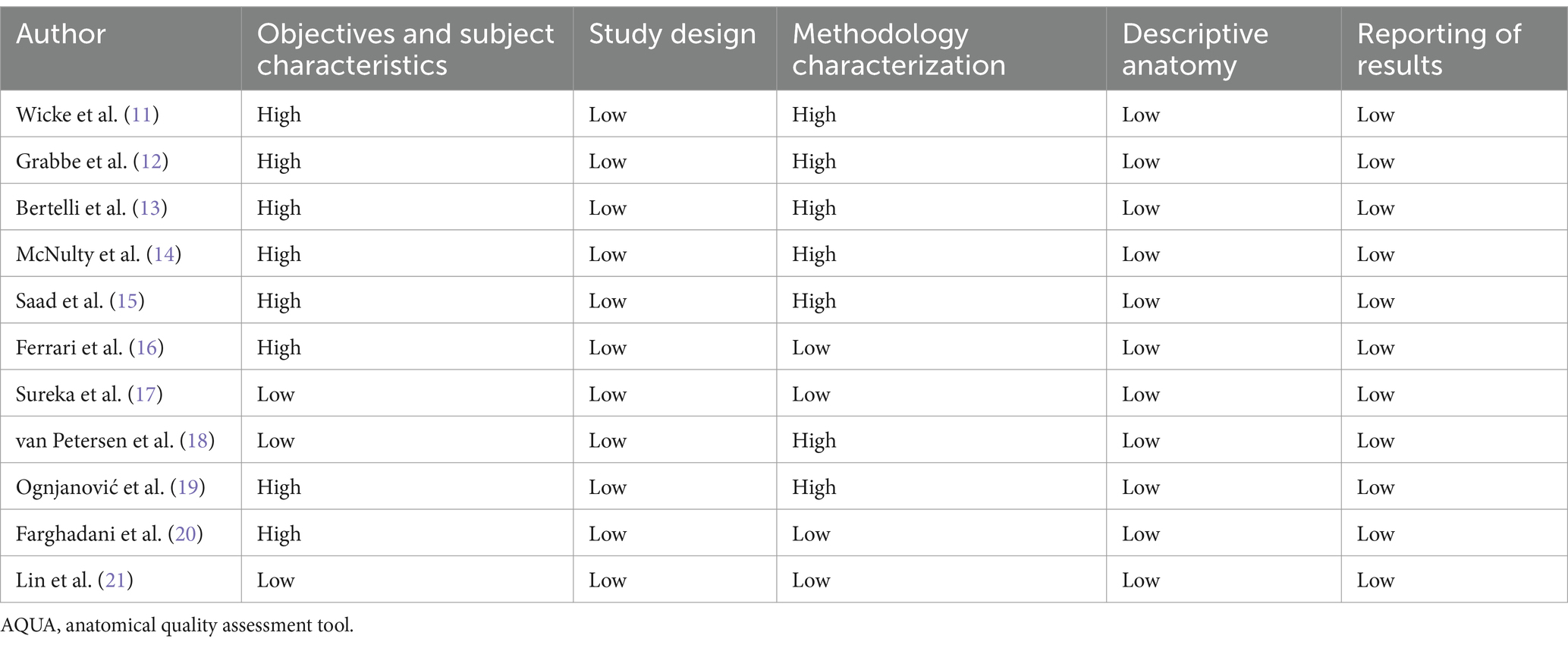
Eleven studies were included (11–21). The χ2 test identified a p value of less than 0.10, and the I2 statistic was 82.80%. Both of the results indicated statistically significant heterogeneity between the eleven included studies. The results of the random effect model meta-analysis (Table 3 and Figure 3) showed that the pooled prevalence of AOB was 1.9% (95% CI: 0.8–3.2%).
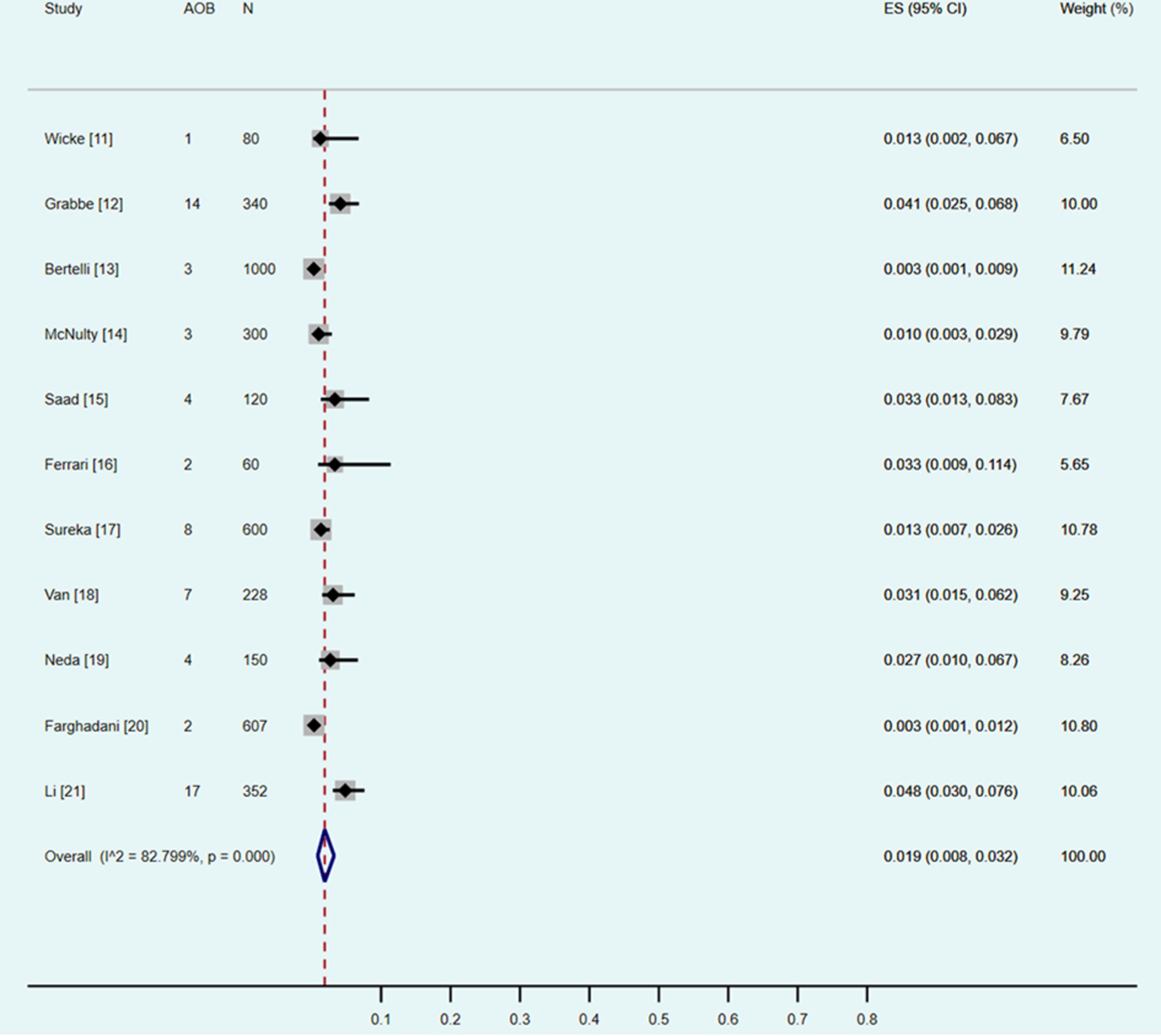
Figure 3. Forest plot showing a pooled incidence of the arc of Bühler (AOB) of 1.9% (95% confidence interval, 0.8–3.2%).
Subgroup analysis
Five CTA and six DSA studies were included into the subgroup analysis (Table 3). The χ2 tests identified both of the p values were less than 0.10, and the I2 statistics were 84.56 and 84.13%, respectively. All the results indicated statistically significant heterogeneity between the studies included into the subgroup analysis. According to the subgroup analysis of the included studies with the random effect models, the pooled prevalence of the AOB using CTA was 2.0% (95% CI: 0.5–4.3%), and that using DSA was 1.8% (95% CI: 0.5–3.9%).
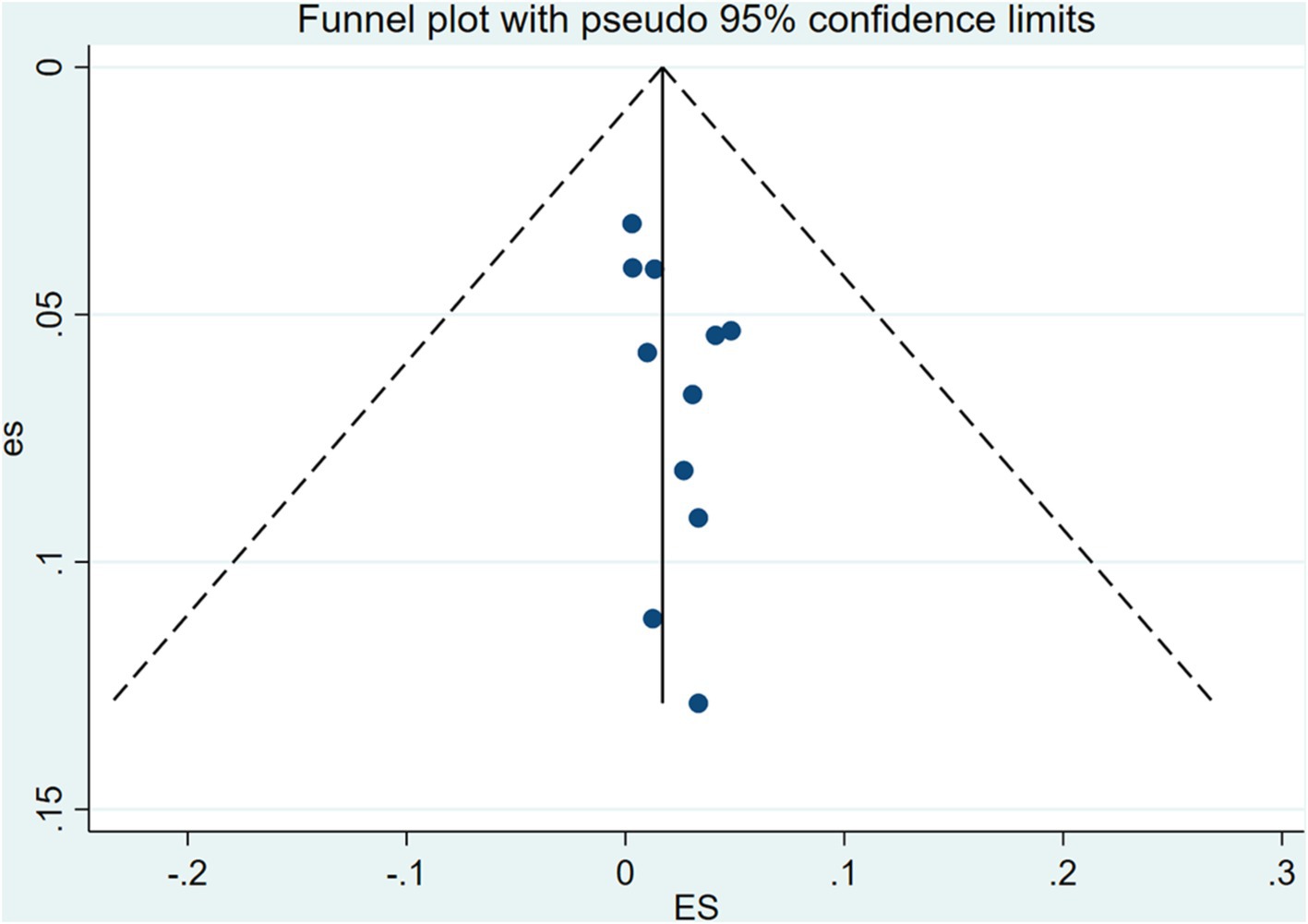
Sensitivity analysis and publication bias test
Sensitivity analysis was performed by eliminating individual studies; the results showed no significant change in the combined estimates, suggesting that the results of this study are relatively stable. The publishing bias of the included studies was assessed by using funnel plots, Begg’s test, and Egger’s test (Figure 4). The findings indicated no significant publication bias (p > 0.05).
Discussion
Definition, prevalence, and anatomical types of the AOB
AOB is a rare anatomical variation. Bühler was the first to describe AOB as “the anastomotic artery between the celiac artery and the middle colonic artery, usually as an additional collateral circulation between the celiac artery and the superior mesenteric artery” (1). With the increase in subsequent reports and a deepening of understanding, current studies have found that such anastomotic vessels can also occur in multiple branches of the celiac trunk and superior mesenteric artery including the following: celiac trunk and superior mesenteric artery, celiac trunk and inferior pancreaticoduodenal artery, celiac trunk and middle colonic artery, celiac trunk and first jejunal artery, celiac trunk and ectopic origin of right hepatic artery, splenetic artery and superior mesenteric artery, common hepatic artery and superior mesenteric artery, common hepatic artery and middle colonic artery, proper hepatic artery and first jejunal artery, gastroduodenal artery and pancreaticoduodenal artery, and pancreatic integument artery and anterior/posterior/inferior pancreaticoduodenal artery (1, 11–21). At present, AOB has been redefined as the anastomotic artery between the superior mesenteric artery and the celiac trunk or its branches (1).
In this meta-analysis, the AOB included in the study was primarily found between the celiac trunk and superior mesenteric artery (11–20), while Li and colleagues (21) reported many other types of AOB (Table 1). The author believes that the reasons may be as follows. First, in the early literature, researchers had insufficient understanding of the AOB, which was only defined as “the anastomotic artery between the celiac artery and the superior mesenteric artery”; thus, the reported frequency of AOB type is fairly low. Second, in subsequent studies, researchers had a deeper understanding of the AOB, which was redefined as “the anastomotic artery between the superior mesenteric artery and the celiac trunk or its branches”; thus the reporting frequency of AOB type was improved.
In this present meta-analysis, the overall prevalence of AOB was 1.9% (0.8–3.2%). For the subgroup analysis according to the type of inclusion study (Table 3), the pooled prevalence of AOB detected by CTA was 2.0% (95% CI: 0.5–4.3%) and that detected by DSA was 1.8% (95% CI: 0.5–3.9%). This is consistent with previous reports by Dubel et al. (22) and Xiao et al. (23) who demonstrated that the prevalence of AOB in the general population is less than 4.0% (Figure 5) (24).

Figure 5. Diagram of the arc of Bühler (24). The arc of Bühler (AOB) is shown as an anastomotic artery between the celiac trunk and the superior mesenteric artery.
Embryological mechanism of AOB
The MacKay arch theory and Handler’s longitudinal anastomosis are two commonly used models to explain anatomical variation in abdominal aortic branches (25). According to the aforementioned model (25), the 10th–13th ventral segmental arteries (which develop into the left gastric artery, splenetic artery, common hepatic artery, and superior mesenteric artery, respectively) originate from the dorsal aorta in the initial stages of embryonic development. They communicate temporarily through ventral longitudinal anastomoses (Figure 6a). Under normal circumstances, the 11th and 12th ventral segmental arteries and ventral longitudinal anastomotic arteries degenerate and disappear, while the 10th and 13th ventral segmental arteries remain, finally forming the celiac trunk and the superior mesenteric arteries. Thus, both the celiac trunk and superior mesenteric artery originate separately from the abdominal aorta (Figure 6b). If the 13th ventral segmental artery and ventral longitudinal anastomotic artery persist and the 10th–12th ventral segmental arteries degenerate, the celiac trunk and superior mesenteric artery are formed. An AOB may form when the ventral longitudinal anastomotic artery persists (Figure 6c). These embryological mechanisms were further clarified in later studies (26–28).
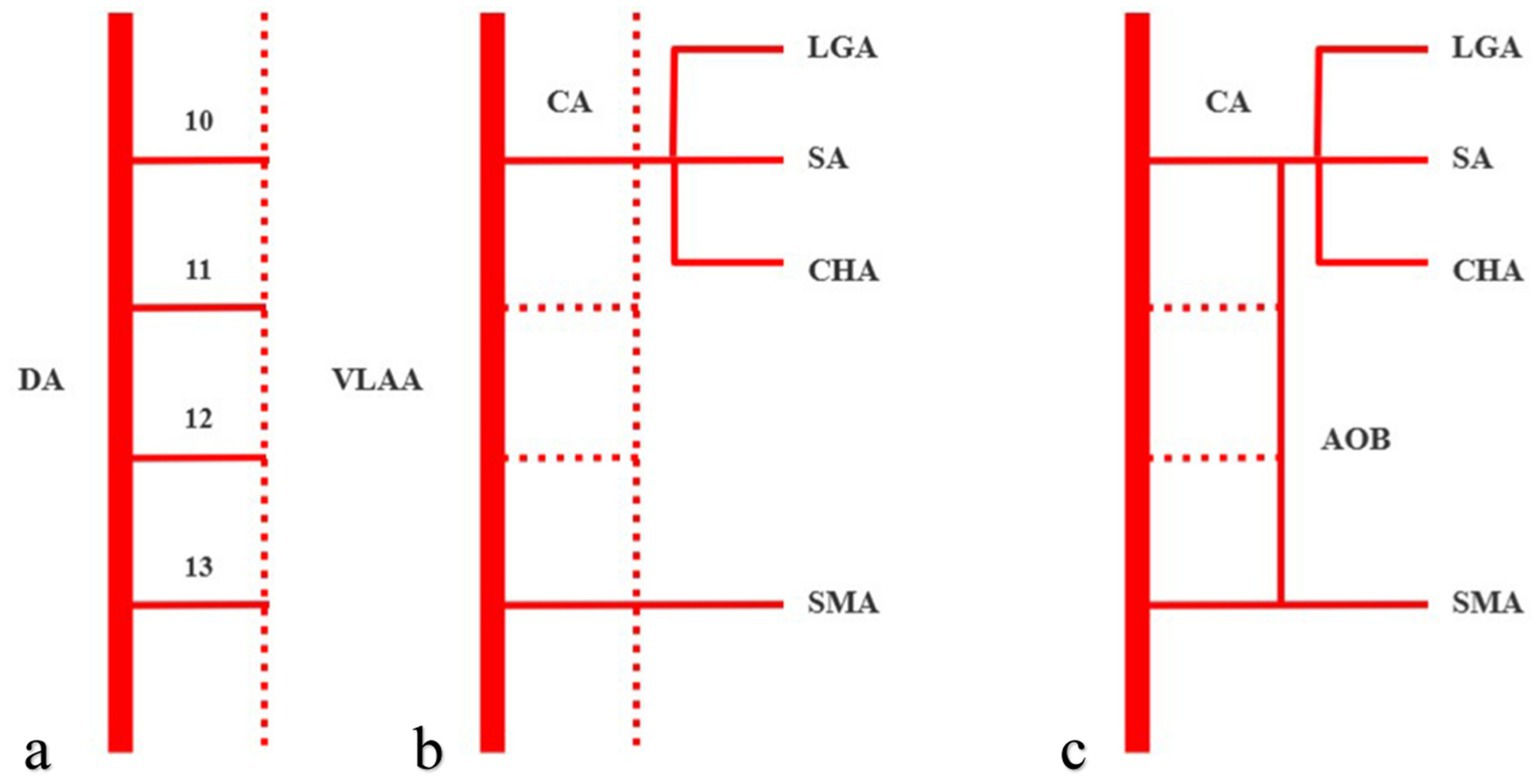
Figure 6. Arc of Bühler (AOB) schematic diagram of the embryological mechanism, with solid lines representing persistent blood vessels and dotted lines representing degenerated blood vessels. The 10th–13th ventral segmental arteries communicate temporarily through ventral longitudinal anastomoses (a). When the 10th and 13th ventral segmental arteries remain, then the celiac trunk and superior mesenteric artery will originate separately from the abdominal aorta (b). An AOB may form when the ventral longitudinal anastomotic artery persists (c). DA, dorsal aorta, VLAA, ventral longitudinal anastomoses artery, CA, celiac axis, LGA, left gastric artery, SA, splenetic artery, CHA, common hepatic artery, and SMA, superior mesenteric artery.
Physiological function and clinical symptoms of AOB
The main physiological function of AOB is to act as a collateral circulation between the celiac trunk and the superior mesenteric artery. Saad et al. (15) used a 1.67 mm ductus arteriosus as a reference and estimated the AOB diameter to be 1.5–2.5 mm. In another study, Grabbe and Bühler (12) estimated that the AOB diameter was 2.0–7.0 mm. Therefore, the AOB is usually very small, and the blood flow may be negligible under normal conditions; however, the hemodynamic behavior of the AOB may change in cases of stenosis or occlusion of the celiac trunk or superior mesenteric artery. In such cases, blood circulates through the collateral circulation of the AOB, ensuring blood circulation to the abdominal organs. However, this collateral circulation mechanism may also lead to the formation of AOB aneurysms because increased local blood flow may lead to increased arterial pressure, thickening of local arterial walls, and the formation of true aneurysms (29). AOB can also form an arterial shunt between the celiac trunk and superior mesenteric artery, resulting in decreased blood flow through the common hepatic artery (30).
The vast majority of patients with AOB did not have any clinical symptoms (86.79%), with it being incidentally detected on CTA or DSA. A few patients (13.21%) may have had epigastric discomfort, postprandial pain, gastrointestinal bleeding, obstructive jaundice, bleeding after endoscopic retrograde cholangiopancreatography, intraabdominal or retroperitoneal bleeding due to pressure phenomena, endovascular hemorrhage, or ruptured aneurysms (1, 23, 31–34).
Clinical correlation of AOB
The anatomy of the retropancreatic space is important during pancreaticoduodenectomy. The tissue structures in this area include the celiac trunk, superior mesenteric artery, portal vein, lymph nodes, and nerves. During pancreaticoduodenectomy, accidental injury to the AOB may lead to iatrogenic damage, such as abdominal organ ischemia or bleeding (35, 36). For interventional radiologists, in some cases (e.g., abdominal trunk occlusion), an unobstructed AOB can also become an alternative route for some abdominal surgeries, or even “an anatomical variation that saves patients’ lives” (37, 38). Shah et al. (37) reported a patient who underwent AOB intubation chemoembolization for hepatocellular carcinoma due to abdominal trunk occlusion.
In another study, Nikolaos et al. (38) reported a patient with complex type B aortic dissection, whose abdominal trunk was almost completely occluded due to the involvement of the dissection, and faced a huge risk of abdominal organ malperfusion syndrome. However, after careful examination by the physicians, it was discovered that there was an AOB anatomical variation between the common hepatic artery and the superior mesenteric artery in the patient, which allowed for the maintenance of blood supply to the abdominal organs. As a result, the patient ultimately underwent endovascular repair surgery for aortic dissection to save his life.
Using PubMed for a literature retrieval with the keywords “arc of Bühler,” “arc of Buhler,” “Bühler,” and “Buhler” (December 20, 2024), we identified a few publications on AOB in some clinical scenarios. For example, Quaretti et al. (39) reported a case of large Buhler aneurysm in the context of chronic celiac trunk occlusion, which was successfully treated by means of covered stent assisted coil embolization; Abouzaid et al. (40) presented a unique AOB variant that connecting the arteries of the foregut, midgut, and hindgut, which was more complex than what had previously been reported; and in another study, Ehemann and Kim (41) reviewed an extremely rare vascular complication of extracorporeal shock wave lithotripsy (ESWL) pseudoaneurysm of AOB, with only one other case recorded in the literature. Publications regarding AOB indexed in the PubMed from 2020 to 2024 have been summarized in Table 4 (n = 10).
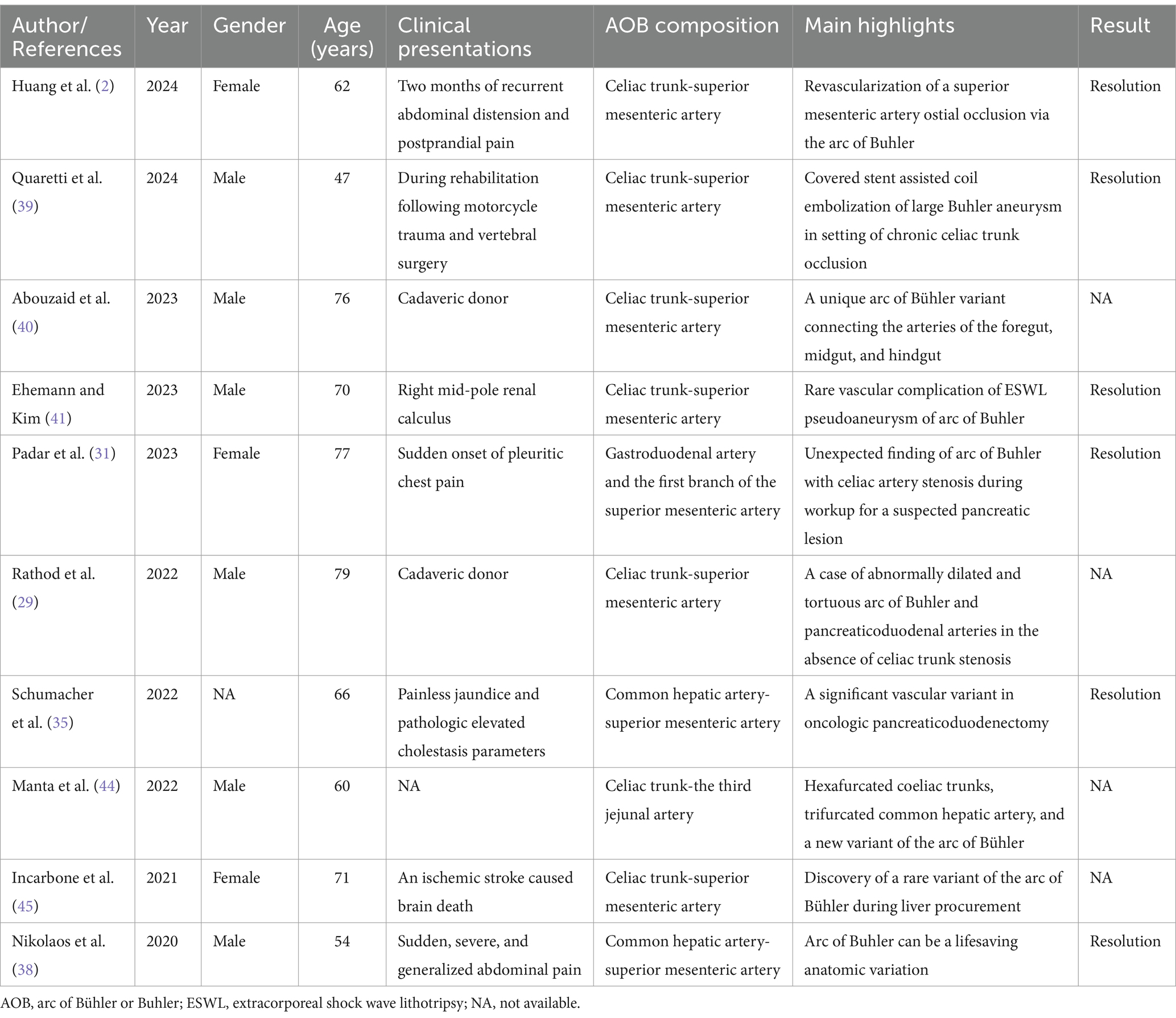
Table 4. Publications regarding arc of Bühler or Buhler indexed in the PubMed from 2020 to 2024 (n = 10).
Limitations and future directions
According to the guideline on conducting a systematic review and meta-analysis of anatomical study published by Henry et al., the heterogeneity in anatomical meta-analysis is almost always high (8). As such, due to the intrinsic heterogeneity in anatomical studies and for the purpose of maximizing the validity of the results, we used a random-effects model in our study. In our study, the χ2 test identified a p value of less than 0.10, and the I2 statistic was 82.80% for the eleven included studies. Both of the results indicated statistically significant heterogeneity between the studies.
The sources of heterogeneity in anatomical meta-analysis studies should always be explored. To probe them, according to the guideline published by Henry et al., subgroup analysis and sensitivity analysis can be performed (8). In our study, the subgroup analysis was performed by the modalities of the included studies (i.e., CTA vs. DSA). Other subgroup analyses, such as by geographical distribution of the studies (seven studies were performed in Europe, while the other four studies were performed in America, India, Iran, and China, respectively), or by gender, age, laterality, and side (left vs. right) were not conducted because the data were not applicable. Using confidence intervals (CIs) to assess for statistically significant differences between the CTA and DSA subgroups, an overlap between the two CIs (Table 3) was present. We may consider that the differences between the two groups were statistically insignificant. We also performed a sensitivity analysis to help explore the sources of heterogeneity in our study. The findings of the sensitivity analysis were robust to decisions made in the process of performing the meta-analysis. As a result, we may attribute the heterogeneity of our study to the inherent factors related to the complexity of the human body and diversity.
For methodology characterization and reporting among the included studies, since the concept of evidence-based anatomy was introduced by Henry et al. (8) and Yammine (9) it has emphasized the need for original anatomical studies with high clarity, transparency, and comprehensiveness in reporting. In our study, we used the “Anatomical Quality Assessment (AQUA) Tool” to evaluate the quality of the eleven included studies. The results showed that eight studies had high risk of bias in “objective (s) and subject characteristics” and seven studies had high risk of bias in “methodology characterization.” Tomaszewski et al. (42) and Ottone et al. (43) introduced a checklist of reporting items that should be addressed by authors of original anatomical studies (i.e., the “Anatomical Quality Assurance (AQUA) Checklist”). In this checklist, twenty-nine items, crucial for reporting anatomical studies, have been designed and arranged. The items consist of eight sections, which include title (one item), abstract (one item), introduction (two items), methodology (twelve items), results (five items), discussion (four items), conclusions (one item), and other information (three items). For studies reporting anatomical findings in the future, we would highly recommend using this checklist as a reference.
For future directions, the number and quality of the currently included eleven studies are limited. This indicates the necessity for more investigations involving a large number of subjects, so as to provide a more precise evaluation of the prevalence of AOB, and improve consciousness among general surgeons, vascular surgeons, and interventional radiologists. When preparing to report anatomical findings in the future, we would also highly recommend the researchers involved to use the AQUA checklist as a reference.
Conclusion
AOB is a rare anatomical variation, with a pooled prevalence of approximately 1.9% in the general population. Although rare, such cases may play a significant role in general surgery, vascular surgery, and interventional radiology. General surgeons, vascular surgeons, and interventional radiologists should consider the existence of AOB when performing associated abdominal operations to avoid complications such as difficulty in the operation, abdominal organ ischemia, or bleeding. Higher-quality, larger-sample studies are required to corroborate the above conclusions because of the restricted number and quality of the included studies in this meta-analysis.
Data availability statement
The datasets presented in this article are not readily available because the raw data supporting the conclusions of this article will be made available by the authors, without undue reservation. Requests to access the datasets should be directed to eWFuZ2Fvd3UxOTg5QDE2My5jb20=.
Author contributions
GY: Supervision, Writing – original draft, Writing – review & editing, Conceptualization, Funding acquisition. YL: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. SH: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. HL: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. MM: Writing – original draft, Writing – review & editing. QL: Investigation, Software, Writing – review & editing, Data curation, Writing – original draft, Formal analysis. JY: Investigation, Software, Writing – review & editing, Data curation, Writing – original draft, Formal analysis. HW: Data curation, Formal analysis, Investigation, Software, Writing – original draft, Writing – review & editing. LZ: Data curation, Formal analysis, Investigation, Software, Writing – original draft, Writing – review & editing. XF: Data curation, Formal analysis, Investigation, Software, Writing – original draft, Writing – review & editing. JY: Data curation, Formal analysis, Investigation, Software, Writing – original draft, Writing – review & editing. SW: Data curation, Formal analysis, Investigation, Software, Writing – original draft, Writing – review & editing. WG: Data curation, Formal analysis, Investigation, Software, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. The present study was supported by grants from the Sichuan Provincial Commission of Health (No. 19PJ284), Sichuan Medical Association (2024HR125), Sichuan Medical and Health Care Promotion Institute (KY2023QN0065), Science and Technology Association of Suining City (No. 6), and Suining Central Hospital (Nos. 2021y09 and 2022ypj01).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Michalinos, A, Schizas, D, Ntourakis, D, Filippou, D, and Troupis, T. Arc of Bühler: the surgical significance of a rare anatomical variation. Surg Radiol Anat. (2019) 41:575–81. doi: 10.1007/s00276-018-2168-0
2. Huang, W, Wang, K, Liu, Y, Wang, QQ, Wei, HJ, and He, CS. Revascularization of superior mesenteric artery occlusion via the arc of Buhler: a case report and literature review. Vascular. (2024) 27:17085381241289485. doi: 10.1177/17085381241289485
3. Sugihara, F, Murata, S, Uchiyama, F, Watari, J, Tajima, H, and Kumita, SI. Successful coil embolization of an aneurysm in the arc of Bühler. J Nippon Med Sch. (2016) 83:196–8. doi: 10.1272/jnms.83.196
4. Kowalczyk, KA, Majewski, A, Wysocki, W, and Tomaszewski, K. Anatomy is the key to mastery in cancer and general surgery: the results of a survey on anatomical knowledge among surgeons. J Oncol. (2022) 72:226–30. doi: 10.5603/NJO.a2022.0033
5. Kowalczyk, KA, and Majewski, A. Analysis of surgical errors associated with anatomical variations clinically relevant in general surgery: review of the literature. Trans Res Anat. (2021) 23:100107. doi: 10.1016/j.tria.2020.100107
6. Deng, J, Ma, T, Yan, J, Wu, S, Yan, G, Li, H, et al. Effect of low tube voltage (100 kV) combined with ASIR-V on the visualization and image quality of the Adamkiewicz artery: a comparison with 120 kV protocol. Diagnostics. (2023) 13:2495. doi: 10.3390/diagnostics13152495
7. Yan, GW, Li, HW, Yang, GQ, Bhetuwal, A, Liu, JP, Li, Y, et al. Iatrogenic arteriovenous fistula of the iliac artery after lumbar discectomy surgery: a systematic review of the last 18 years. Quant Imaging Med Surg. (2019) 9:1163–75. doi: 10.21037/qims.2019.05.12
8. Henry, BM, Tomaszewski, KA, and Walocha, JA. Methods of evidence-based anatomy: a guide to conducting systematic reviews and meta-analysis of anatomical studies. Ann Anat. (2016) 205:16–21. doi: 10.1016/j.aanat.2015.12.002
10. Henry, BM, Tomaszewski, KA, Ramakrishnan, PK, Roy, J, Vikse, J, Loukas, M, et al. Development of the anatomical quality assessment (AQUA) tool for the quality assessment of anatomical studies included in meta-analyses and systematic reviews. Clin Anat. (2017) 30:6–13. doi: 10.1002/ca.22799
11. Wicke, L, Feigl, W, Firbas, W, Sinzinger, H, and Olbert, F. Anastomoses between the coeliac and the superior mesenteric artery in radiological and anatomical material. Radiol Clin. (1977) 46:11–7.
12. Grabbe, E, and Bücheler, E. Bühler's anastomosis. Rofo. (1980) 132:541–6. doi: 10.1055/s-2008-1056615
13. Bertelli, E, Di Gregorio, F, and Civeli, L. Various cases of direct connections between the celiac artery and the superior mesenteric. Arch Ital Anat Embriol. (1991) 96:281–9.
14. McNulty, JG, Hickey, N, Khosa, F, O’Brien, P, and O’Callaghan, J. Surgical and radiological significance of variants of Bühler's anastomotic artery: a report of three cases. Surg Radiol Anat. (2001) 23:277–80. doi: 10.1007/s00276-001-0277-6
15. Saad, WE, Davies, MG, Sahler, L, Lee, D, Patel, N, Kitanosono, T, et al. Arc of Buhler: incidence and diameter in asymptomatic individuals. Vasc Endovasc Surg. (2005) 39:347–9. doi: 10.1177/153857440503900407
16. Ferrari, R, De Cecco, CN, Iafrate, F, Paolantonio, P, Rengo, M, and Laghi, A. Anatomical variations of the coeliac trunk and the mesenteric arteries evaluated with 64-row CT angiography. Radiol Med. (2007) 112:988–98. doi: 10.1007/s11547-007-0200-2
17. Sureka, B, Mittal, MK, Mittal, A, Sinha, M, Bhambri, NK, and Thukral, BB. Variations of celiac axis, common hepatic artery and its branches in 600 patients. Indian J Radiol Imaging. (2013) 23:223–33. doi: 10.4103/0971-3026.120273
18. van Petersen, AS, Kolkman, JJ, Meerwaldt, R, Huisman, AB, van der Palen, J, Zeebregts, CJ, et al. Mesenteric stenosis, collaterals, and compensatory blood flow. J Vasc Surg. (2014) 60:111–119.e2. doi: 10.1016/j.jvs.2014.01.063
19. Ognjanović, N, Jeremić, D, Živanović-mačužić, I, Sazdanović, M, Sazdanović, P, Tanasković, I, et al. MDCT: angiography of anatomical variations of the celiac trunk and superior mesenteric artery. Arch Biol Sci. (2014) 66:233–40. doi: 10.2298/ABS1401233O
20. Farghadani, M, Momeni, M, Hekmatnia, A, Momeni, F, and Baradaran Mahdavi, MM. Anatomical variation of celiac axis, superior mesenteric artery, and hepatic artery: evaluation with multidetector computed tomography angiography. J Res Med Sci. (2016) 21:129. doi: 10.4103/1735-1995.196611
21. Lin, B, Wang, FW, Qiu, ZQ, Zhang, JX, Miu, YN, Zhang, HQ, et al. Imaging anatomy of celiac trunk-superior mesenteric artery system and its clinical significance in 352 cases of biliary tract disease. Chin J Pract Surg. (2022) 42:179–86. doi: 10.19538/j.cjps.issn1005-2208.2022.02.11
22. Dubel, GJ, Ahn, SH, and Saeed, MA. Interventional management of arc of Buhler aneurysm. Semin Intervent Radiol. (2007) 24:076–81. doi: 10.1055/s-2007-971193
23. Xiao, N, Ahuja, A, Patel, R, Desai, SS, Nemcek, A Jr, and Resnick, S. Median arcuate ligament compression associated with flow-related visceral aneurysms. J Vasc Interv Radiol. (2023) 34:1176–82. doi: 10.1016/j.jvir.2023.03.026
24. McCracken, E, Turley, R, Cox, M, Suhocki, P, and Blazer, DG III. Leveraging aberrant vasculature in celiac artery stenosis: the arc of Buhler in Pancreaticoduodenectomy. J Pancreat Cancer. (2018) 4:4–6. doi: 10.1089/pancan.2017.0020
25. Douard, R, Chevallier, JM, Delmas, V, and Cugnenc, PH. Clinical interest of digestive arterial trunk anastomoses. Surg Radiol Anat. (2006) 28:219–27. doi: 10.1007/s00276-006-0098-8
26. Mao, Y, Yao, Y, Li, X, Zhang, C, Chen, X, and Wang, Y. Absence of the celiac trunk: definition, classification, multidetector computed tomography angiographic findings, and their probable embryological mechanisms. Vascular. (2023) 31:1214–21. doi: 10.1177/17085381221106318
27. Tang, W, Shi, J, Kuang, LQ, Tang, SY, and Wang, Y. Celiomesenteric trunk: new classification based on multidetector computed tomography angiographic findings and probable embryological mechanisms. World J Clin Cases. (2019) 7:3980–9. doi: 10.12998/wjcc.v7.i23.3980
28. Wang, Y, Cheng, C, Wang, L, Li, R, Chen, JH, and Gong, SG. Anatomical variations in the origins of the celiac axis and the superior mesenteric artery: MDCT angiographic findings and their probable embryological mechanisms. Eur Radiol. (2014) 24:1777–84. doi: 10.1007/s00330-014-3215-9
29. Rathod, S, Kolus, R, Kim, B, Gurnani, S, Kim, A, Kim, E, et al. A case of abnormally dilated and tortuous arc of Buhler and pancreaticoduodenal arteries in the absence of celiac trunk stenosis. Surg Radiol Anat. (2022) 44:1343–7. doi: 10.1007/s00276-022-03018-2
30. Tokura, M, and Kawasaki, S. A case of pancreaticoduodenal artery aneurysm without stenosis or obstruction of celiac artery. Nihon Rinshō Geka Igakkai Zasshi. (2002) 63:1203–7. doi: 10.3919/jjsa.63.1203
31. Padar, M, Rieseberg, A, and Ratnayake, S. Unexpected finding of arc of Buhler with celiac artery stenosis during workup for a suspected pancreatic lesion. J Surg Case Rep. (2023) 2023:rjad178. doi: 10.1093/jscr/rjad178
32. Ong, DY, and Pua, U. Coil embolization of arc of Buhler aneurysm rupture. Case Rep Radiol. (2020) 2020:8855946. doi: 10.1155/2020/8855946
33. Baz, RO, Scheau, C, Baz, RA, and Niscoveanu, C. Buhler's arc: an unexpected finding in a case of chronic abdominal pain. J Gastrointestin Liver Dis. (2020) 29:304. doi: 10.15403/jgld-2639
34. Biswas, S, and Gogna, S. Arc of Buhler Pseudoaneurysm causing fatal retroperitoneal Hemorrhage; a rare case report and discussion of relevant literature. Bull Emerg Trauma. (2019) 7:183–6. doi: 10.29252/beat-070215
35. Schumacher, L, Albrecht, HC, and Gretschel, S. A significant vascular variant in oncologic pancreaticoduodenectomy: the arc of Buhler. Surg Case Rep. (2022) 8:37. doi: 10.1186/s40792-022-01387-9
36. Kageyama, Y, Kokudo, T, Amikura, K, Miyazaki, Y, Takahashi, A, and Sakamoto, H. The arc of Buhler: special considerations when performing pancreaticoduodenectomy. Surg Case Rep. (2016) 2:21. doi: 10.1186/s40792-016-0149-2
37. Shah, N, Chen, O, and Cohen, GS. Arc of Buhler catheterization for tumor therapy: case report. J Interv Radiol. (2010) 3:28–30. doi: 10.2310/6650.2010.060003
38. Nikolaos, S, Vasilios, P, Niki, L, Argyriou, EO, Theodoros, K, and Mihalis, A. Arc of Buhler: a lifesaving anatomic variation. A case report. J Vasc Bras. (2020) 19:e20200045. doi: 10.1590/1677-5449.200045
39. Quaretti, P, Corti, R, D'Agostino, AM, Bozzani, A, Moramarco, LP, and Cionfoli, N. Covered stent assisted coil embolization of large Buhler aneurysm in setting of chronic celiac trunk occlusion. CVIR Endovasc. (2024) 7:9. doi: 10.1186/s42155-023-00416-4
40. Abouzaid, KA, Lichtenberg, AB, Karim, AY, Stack, ER, Algoul, M, Imam, A, et al. A unique arc of Bühler variant connecting the arteries of the foregut, Midgut, and hindgut and its surgical significance. Cureus. (2023) 15:e42611. doi: 10.7759/cureus.42611
41. Ehemann, J, and Kim, JJY. Rare vascular complication of ESWL pseudoaneurysm of arc of Buhler. BMJ Case Rep. (2023) 16:e256089. doi: 10.1136/bcr-2023-256089
42. Tomaszewski, KA, Henry, BM, Kumar Ramakrishnan, P, Roy, J, Vikse, J, Loukas, M, et al. Development of the anatomical quality assurance (AQUA) checklist: guidelines for reporting original anatomical studies. Clin Anat. (2017) 30:14–20. doi: 10.1002/ca.22800
43. Ottone, NE, Sandoval, C, Cid-Gutierrez, P, Vásquez-Balboa, ML, Tubbs, RS, and Fuentes, R. Systematic review and meta-analysis of the anatomy of the maxillary artery using the anatomical quality assurance (AQUA) checklist. Surg Radiol Anat. (2021) 43:1875–86. doi: 10.1007/s00276-021-02825-3
44. Manta, BA, Rusu, MC, Jianu, AM, and Ilie, AC. Hexafurcated coeliac trunks, trifurcated common hepatic artery, and a new variant of the arc of Bühler. Folia Morphol (Warsz). (2022) 81:365–71. doi: 10.5603/FM.a2021.0025
Keywords: arc of Bühler, computed tomography angiography, digital subtraction angiography, meta-analysis, systematic review
Citation: Yan G, Li Y, He S, Li H, McClure MA, Li Q, Yang J, Wang H, Zhao L, Fan X, Yan J, Wu S and Guo W (2025) Prevalence and clinical implications of the rare arc of Bühler using computed tomography angiography and digital subtraction angiography: a systematic review and meta-analysis. Front. Med. 11:1522292. doi: 10.3389/fmed.2024.1522292
Edited by:
Pradeep Kumar Shukla, University of Tennessee Health Science Center (UTHSC), United StatesReviewed by:
Zheng Liu, National Cancer Center of China, ChinaDaming Zhang, First Affiliated Hospital of Harbin Medical University, China
Copyright © 2025 Yan, Li, He, Li, McClure, Li, Yang, Wang, Zhao, Fan, Yan, Wu and Guo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Suyu He, MTM4OTA4OTMwNTdAMTYzLmNvbQ==
†These authors have contributed equally to this work
 Gaowu Yan
Gaowu Yan Yong Li1†
Yong Li1† Hongwei Li
Hongwei Li Morgan A. McClure
Morgan A. McClure