
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med., 30 January 2025
Sec. Obstetrics and Gynecology
Volume 11 - 2024 | https://doi.org/10.3389/fmed.2024.1509973
 Rüveyda Ölmez Yalazı1,2*†
Rüveyda Ölmez Yalazı1,2*† Nurdan Demirci3†
Nurdan Demirci3†Introduction: Urinary incontinence (UI) significantly affects women’s quality of life and may contribute to pelvic floor disorders. This study aimed to investigate the impact of UI on pelvic floor disorders through a mixed-methods approach.
Methods: A convergent parallel design was employed, integrating quantitative and qualitative data. Quantitative data were collected using the “Global Pelvic Floor Disorders Questionnaire,” and semi-structured interviews were conducted for qualitative insights. Quantitative data were analyzed using SPSS 26.0, while qualitative data underwent content analysis with MAXQDA Pro 22 software.
Results: Among the participants, 41.7% were diagnosed with stress urinary incontinence, which was associated with the highest level of discomfort. Qualitative findings revealed four main categories: effects on daily life, emotional and psychological effects, coping strategies, and treatment approaches and expectations. Participants reported that UI led to social isolation, reduced self-esteem, and increased anxiety.
Discussion: The findings highlight that UI adversely affects both the physical and psychosocial well-being of women. Addressing this condition requires a holistic approach combining medical treatment with psychosocial support to mitigate its multifaceted impact.
Urinary incontinence (UI), defined as the involuntary loss of urine, is classified into three types: stress, urge, and mixed UI, and is recognized as a significant social and health concern (1). The underlying causes of UI often involve dysfunction in the muscles and structures comprising the pelvic floor (2). UI affects 6–10% of women overall, approximately 10–25% of women over the age of 30, with prevalence increasing to 30–50% by the age of 50 (3, 4). Risk factors for UI include age, pregnancy, childbirth, and obesity (5–8). UI has a profound impact on women’s physical and mental health, disrupting daily activities and leading to morbidity and, in rare cases, mortality (9, 10). Consequently, early screening, assessment, intervention, and rehabilitation are essential components of managing UI effectively (11). Assessing the severity and discomfort caused by patients’ symptoms is critical for determining an appropriate treatment plan. This study aims to examine the effects of urinary incontinence on pelvic floor disorders and to evaluate the severity, frequency, and prevalence of these disorders using both quantitative and qualitative methods. By adopting this approach, the study seeks to gain a deeper understanding of the physical challenges faced by women diagnosed with UI and the extent of discomfort caused by these conditions.
The study employed a convergent parallel design, a mixed-methods approach in which qualitative and quantitative data, given equal importance, are collected simultaneously and independently, analyzed separately, and integrated during the interpretation phase (12). The findings were reported in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines (Supplementary File 1) and the Consolidated Criteria for Reporting Qualitative Research (COREQ) checklist (Supplementary File 2) (13, 14).
For the quantitative portion, a validated scale was used to assess the severity of pelvic floor symptoms in women with UI. Additionally, a questionnaire was employed to gather sociodemographic and obstetric information. For the qualitative portion, individual interviews were conducted via an online platform using Van Manen’s interpretive phenomenology model (15). The research was carried out between November 2023 and March 2024 after obtaining the necessary permissions.
In qualitative research, the sample size is determined by the principle of “saturation,” where data collection continues until concepts and themes begin to repeat and no new information emerges (12, 16). Accordingly, the qualitative portion of this study included 24 women. For the quantitative part, a power analysis conducted using G*Power 3.1.9.6 software, assuming 90% power and a Type I error of 0.05, determined the need for 240 participants.
Participants for both portions of the study were women aged 18–65, diagnosed with urinary incontinence, who had at least a primary school education, used the internet, and voluntarily agreed to participate. Quantitative data were collected using the “Personal Information Form” and the “Global Pelvic Floor Bother Questionnaire (GPFBQ),” while qualitative data were obtained through a semi-structured interview form designed specifically for women with UI.
The Personal Information Form was developed by the researchers based on the literature (17, 18). The GPFBQ, originally adapted into Turkish by Doğan and colleagues in 2016, measures symptoms and their severity related to stress, frequent and sudden urges to urinate, difficulty urinating, pelvic organ prolapse (POP), fecal incontinence, dyspareunia, and obstructive defecation (19). The GPFBQ includes nine items scored on a Likert scale, where women indicate symptom severity ranging from “not at all” (1) to “a great deal” (5). This practical and efficient tool is well-suited for both clinical and research settings. The Cronbach’s alpha value for the GPFBQ was 0.71 in the Turkish validity and reliability study and 0.82 in this study.
The semi-structured interview forms contained open-ended questions designed to guide the researchers during the interviews and capture participants’ views and experiences regarding pelvic floor health and related discomfort. A pilot study was conducted with five women diagnosed with UI to test the clarity of the data collection tools. Feedback from the pilot study informed adjustments to the interview forms. These participants were not included in the final sample.
The GPFBQ was digitized and distributed via an online survey platform. Researchers shared the online survey link with women meeting the study’s inclusion criteria, who were also invited to refer other women with UI and pelvic floor disorders fitting the criteria. Completing the forms took an average of 15 min.
The qualitative data were collected by researchers experienced and trained in qualitative methodologies. Informed consent was obtained prior to interviews, which were recorded and subsequently transcribed. Individual interviews were conducted face-to-face using the semi-structured interview form, with a moderator (ND) and a rapporteur (ROY) present. Each interview lasted approximately 30 min.
Qualitative and quantitative data were analyzed using distinct methods for each (12). Qualitative data were analyzed through content analysis. To ensure confidentiality, participants were coded with identifiers starting with “S” followed by their participant number. Researchers experienced in qualitative methodologies utilized MAXQDA Pro 22 software to code the data line by line and conduct content analysis. Themes and sub-themes were finalized during a collaborative meeting where researchers re-evaluated the data and reached a consensus.
Quantitative data were analyzed using SPSS 26.0. Descriptive statistics were employed to summarize the sociodemographic characteristics of the participants, and a p-value of <0.05 was considered statistically significant for all analyses. Logistic regression analysis was applied to account for the binary categorical structure of the dependent variable. Independent variables and other potential influencing factors were incorporated into the logistic regression model. The accuracy of the model was assessed using the Hosmer-Lemeshow test, with a significance level of p < 0.05 deemed acceptable. Odds ratio values and 95% confidence intervals were calculated to interpret the effect of independent variables on the dependent variable.
Additionally, Fleiss’s Kappa test was conducted to evaluate the agreement between responses on the GPFBQ scale. The chi-square test was also performed to assess relationships between categorical variables. Informed consent was obtained from participants prior to their inclusion in the study.
The average age of the women who participated in the qualitative interviews was 45.3 ± 10.2 years; 27.7% had a university degree, 79.2% had a history of pregnancy, 37.5% were overweight, and 41.7% were diagnosed with stress urinary incontinence (Table 1).
In the reliability analyses, the Fleiss Kappa values of the GPFBQ ranged from 0.65 to 0.92, and the average Fleiss Kappa value was calculated to be 0.81. This result indicates that interobserver agreement is at an ‘excellent’ level.
Table 2 presents a summary of the symptoms associated with pelvic floor disorders and their respective levels of bother. When considering moderate to severe levels of bother for any single symptom, SUI exhibited the highest bother scores. A total of 36% (n = 86) of women reported experiencing prolapse symptoms, yet only 15% (15 out of 118) reported experiencing moderate to severe bother. Approximately 32% (n = 76) of participants reported AI (anal incontinence), and 18% (n = 46) noted obstructive defecation. Additionally, 35% (n = 86) of participants reported urinary frequency issues.
The results of the stepwise regression analysis indicated that women’s age, number of births and stress were associated with the presence of incontinence (R2: 21.5%, p < 0.001, Durbin-Watson: 1.064; F: 13.755; Table 3).
A statistically significant correlation was identified between the number of births and the type of urinary incontinence (χ2 = 16.60, p < 0.05). Specifically, while stress urinary incontinence (SUI) was more prevalent in women who had one to two births, the incidence of mixed urinary incontinence (MUI) increased in women who had three or more births (Table 4). Additionally, the odds ratio (OR) analysis revealed that women who had one to two births were 1.6 times more likely to experience SUI compared to those with three or more births (95% CI: 0.81–3.15), though this result was not statistically significant.
A significant correlation was identified between body mass index (BMI) categories and urinary incontinence type (χ2 = 15.32, p < 0.05). SUI was more common in overweight and obese individuals, while a more balanced distribution between types was observed in normal-weight individuals (Table 4). SUI was more common in overweight and obese individuals, with the odds of experiencing SUI being higher in overweight individuals compared to those with normal weight. In contrast, a more balanced distribution between incontinence types was observed in normal-weight individuals (Table 4). However, further analysis is required to explore the magnitude of the effects and potential confounding variables.
As a result of the qualitative analysis of the data obtained from the interviews with women, 4 categories were identified from the interviews: (1) the impact of UI on daily life, (2) emotional and psychological effects, (3) coping strategies, and (4) treatment approach and expectations. These categories included 8 themes and 21 sub-themes (Table 5).
The impact on the daily lives of women with urinary incontinence (UI), their emotional and psychological states, their coping strategies and their perspectives on treatment were analyzed. The results were grouped into four main categories: ‘impact on daily life’, ‘emotional and psychological impact’, ‘coping strategies’ and ‘treatment approach and expectations’ (Table 6).
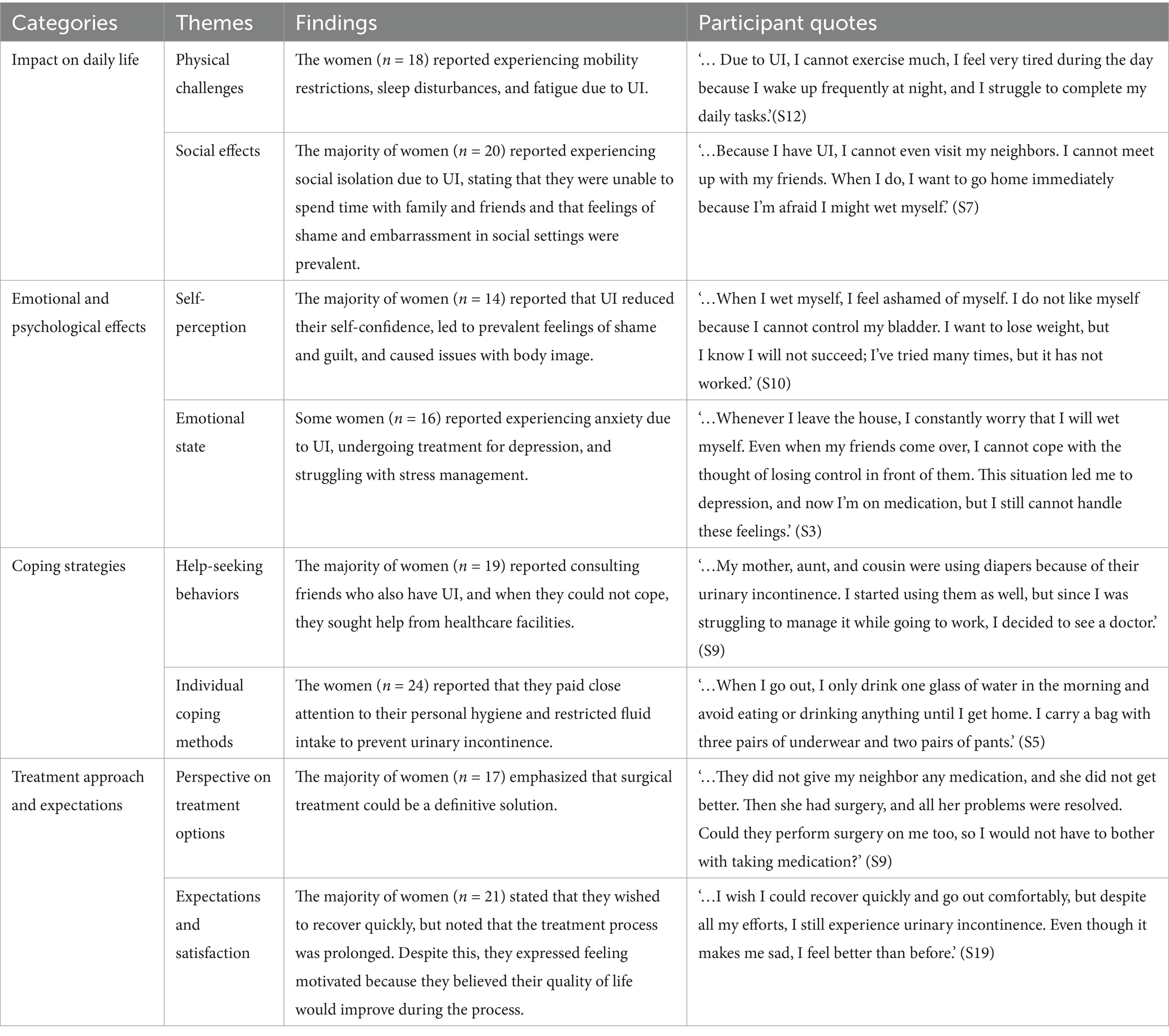
Table 6. The effects of urinary incontinence on women’s daily life, emotional states, coping strategies and treatment expectations.
This study provides an in-depth examination of both the physical and psychosocial effects of UI. Unlike most studies in the literature, which tend to focus on the physical symptoms of UI, this study comprehensively evaluates the impact of UI on women’s social lives, emotional well-being, and daily activities using both qualitative and quantitative methods. Particularly, the effects of social isolation and disruptions in self-perception, which are less emphasized in the literature, are thoroughly addressed in this study.
The quantitative findings reveal that SUI poses a significant burden on women. Approximately 36% of participants reported experiencing prolapse symptoms, though only 15% expressed moderate to severe discomfort from these symptoms. Similarly, the rates of participants experiencing anal incontinence and obstructive defecation are notable. These findings highlight the complexity of UI and its varying degrees of impact on individuals. Consistent with previous studies, this research confirmed the significant relationship between UI and factors such as age, number of births, and stress (20, 21). In line with other research, the regression analysis in this study found that these factors increase the risk of incontinence and explained 21.5% of the total variance (22, 23). Higher age and lower education levels were found to be associated with increased risk of UI, consistent with previous findings (24, 25). Our study also highlights that women with one to two births have a higher prevalence of SUI, while those with three or more births exhibit a greater incidence of MUI. In line with earlier research, factors such as mobility restrictions, obesity, and chronic conditions remain significant contributors to UI risk (22, 26).
The qualitative findings provide a deeper understanding of the negative impact of UI on women’s quality of life. Women reported experiencing social isolation, difficulty in daily activities, and loss of self-confidence due to UI. These findings emphasize that UI is not merely a physical issue but also a significant social and emotional burden. The decline in self-perception and psychological outcomes such as anxiety further illustrate the broad impact of UI on mental health. Previous studies have similarly supported the destructive effects of UI on individuals’ social lives and psychological well-being (26–28).
Regarding coping strategies and treatment approaches, the majority of participants expressed positive expectations toward surgical treatment. However, despite the long duration of the treatment process, women remained motivated due to the belief that their quality of life would improve. This is an important factor that enhances individuals’ commitment to the treatment process, and the influence of patient expectations on treatment outcomes in UI has been widely discussed in the literature (28, 29).
The results of this study demonstrate the multifaceted impact of UI on women’s lives and underline the necessity for a comprehensive treatment and support approach to address this condition. In particular, it is clear that social support systems and psychological assistance play a critical role in coping with UI (29, 30). Accelerating treatment processes and improving access to treatments have the potential to significantly enhance women’s quality of life (27, 31).
One of the strengths of this study is its use of the convergent parallel design, which enabled the integration of both qualitative and quantitative data for a comprehensive analysis. This method provided a broader perspective on the effects of UI on women and contributed to a deeper understanding of the findings. While the quantitative data helped elucidate the physical and symptomatic aspects of UI, the qualitative data detailed the social and psychological impacts. Furthermore, this study, conducted in the Turkish context, offers valuable contributions to the literature by considering regional and cultural differences in the effects of UI on women.
However, the study has some limitations. The sample size, particularly in the qualitative data, may limit the generalizability of the findings. Additionally, the high proportion of participants diagnosed with SUI may result in less information about other types of UI. Future studies with larger samples and examinations of different types of incontinence could help address these limitations.
This study highlights the importance of holistic approaches, including psychosocial support, in managing UI. Healthcare professionals must address the emotional needs of women with UI and develop inclusive, multidisciplinary programs. Revisiting health policies and treatment strategies is essential to implement effective support and rehabilitation for these individuals. UI is influenced by social determinants such as age, education, ethnicity, body mass index, and number of births. Our findings show that stress urinary incontinence is more prevalent among women with one to two births, while mixed urinary incontinence is common in those with three or more births. Overweight and obese women also face a higher risk of stress urinary incontinence, underscoring the need for personalized interventions. Public awareness campaigns should aim to reduce stigma and encourage women to seek care. Culturally sensitive messages and community-based support programs, including pelvic floor exercise workshops and counseling, could significantly improve the quality of life for women with UI.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Prior to data collection, ethical approval was obtained from the Ethics Committee of Çanakkale Onsekiz Mart university (26/10/2023–13/18). Before the application of the data collection instruments, the participants were informed about the purpose and scope of the research in online platform. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the individual(s), and minor(s)’ legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
RY: Data curation, Investigation, Writing – original draft. ND: Supervision, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors declare that no Gen AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2024.1509973/full#supplementary-material
1. Herdman, TH, and Lopes, CT. Supplement to NANDA international nursing diagnoses: Definitions and classification 2021–2023. 12th ed. Georg Thieme Verlag. (2023).
2. Wallace, SL, Miller, LD, and Mishra, K. Pelvic floor physical therapy in the treatment of pelvic floor dysfunction in women. Curr Opin Obstet Gynecol. (2019) 31:485–93. doi: 10.1097/GCO.0000000000000584
3. Weber-Rajek, M, Strączyńska, A, Strojek, K, Piekorz, Z, Pilarska, B, Podhorecka, M, et al. Assessment of the effectiveness of pelvic floor muscle training (PFMT) and extracorporeal magnetic innervation (ExMI) in treatment of stress urinary incontinence in women: a randomized controlled trial. Biomed Res Int. (2020) 2020:1–7. doi: 10.1155/2020/1019872
4. Derewiecki, T, Mroczek, M, Majcher, P, and Chruściel, P. Importance of urinary incontinence problem among women over 40 years of age. Hyg Publ Health. (2015) 50:219–25.
5. Baran, E, Akbayrak, T, Özgül, S, Nakip, G, Çinar, GN, Üzelpasacı, E, et al. Musculoskeletal and anthropometric factors associated with urinary incontinence in pregnancy. Physiother Theory Pract. (2022) 38:1789–98. doi: 10.1080/09593985.2021.1878568
6. Özgül, S, Gürşen, C, Toprak Çelenay, Ş, Baran, E, Üzelpasacı, E, Nakip, G, et al. Contributory effects of individual characteristics on pelvic floor distress in women with pelvic floor dysfunctions. Physiother Theory Pract. (2022) 40:625–36. doi: 10.1080/09593985.2022.2127137
7. Weintraub, AY, Glinter, H, and Marcus-Braun, N. Narrative review of the epidemiology, diagnosis and pathophysiology of pelvic organ prolapse. Int Braz J Urol. (2019) 46:5–14. doi: 10.1590/S1677-5538.IBJU.2018.0581
8. Dumoulin, C, Pazzoto Cacciari, L, and Mercier, J. Keeping the pelvic floor healthy. Climacteric. (2019) 22:257–62. doi: 10.1080/13697137.2018.1552934
9. Liu, Z, Zhou, C, Munoz, A, Zhang, Y, and Li, X. Validation of a Chinese version for the global pelvic floor bother questionnaire. Arch Gynecol Obstet. (2022) 305:1353–7. doi: 10.1007/s00404-021-06370-7
10. Astepe, BS, and Köleli, I. Translation, cultural adaptation, and validation of Australian pelvic floor questionnaire in a Turkish population. Eur J Obstet Gynecol Reprod Biol. (2019) 234:71–4. doi: 10.1016/j.ejogrb.2019.01.004
11. Molina-Torres, G, Amiano-López, L, Córdoba-Peláez, MM, Ibáñez-Vera, AJ, and Diaz-Mohedo, E. Analysis of the structural characteristics and psychometric properties of the pelvic floor bother questionnaire (PFBQ): a systematic review. J Clin Med. (2022) 11:7075. doi: 10.3390/jcm11237075
12. Plano Clark, VL. Mixed methods research. J Posit Psychol. (2017) 12:305–6. doi: 10.1080/17439760.2016.1262619
13. Von Elm, E, Altman, D, Egger, M, Pocock, S, Gøtzsche, P, and Vandenbroucke, J. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Rev Esp Salud Publica. (2019) 61:344–9. doi: 10.1016/j.jclinepi.2007.11.008
14. Tong, A, Sainsbury, P, and Craig, J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. (2007) 19:349–57. doi: 10.1093/intqhc/mzm042
15. Lorello, GR, Tewari, A, Sivagurunathan, M, Potter, E, Krakowsky, Y, Du Mont, J, et al. The lived experiences of transgender and gender-diverse people in accessing publicly funded penile-inversion vaginoplasty in Canada. CMAJ. (2024) 196:E816–25. doi: 10.1503/cmaj.231250
16. Constantinou, CS, Georgiou, M, and Perdikogianni, M. A comparative method for themes saturation (CoMeTS) in qualitative interviews. Qual Res. (2017) 17:571–88. doi: 10.1177/1468794116686650
17. Todhunter-Brown, A, Hazelton, C, Campbell, P, Elders, A, Hagen, S, and McClurg, D. Conservative interventions for treating urinary incontinence in women: an overview of Cochrane systematic reviews. Cochrane Database Syst Rev. (2022) 9:CD012337. doi: 10.1002/14651858.CD012337.pub2
18. Juhl, C, Thimm, MH, and Glavind, K. Impact on urinary incontinence after management of complications related to a retropubic midurethral sling. Int Urogynecol J. (2023) 34:2767–74. doi: 10.1007/s00192-023-05600-7
19. Doğan, H, Özengin, N, Bakar, Y, and Duran, B. Reliability and validity of a Turkish version of the global pelvic floor bother questionnaire. Int Urogynecol J. (2016) 27:1577–81. doi: 10.1007/s00192-016-3014-8
20. Liu, W, and Qian, L. Risk factors for postpartum stress urinary incontinence: a prospective study. BMC Urol. (2024) 24:42. doi: 10.1186/s12894-024-01430-x
21. Ganz, M, Alessandro, C, Jacobs, M, Miller, D, Diah, J, Winer, A, et al. The role of body mass index and waist circumference in gender-specific risk factors for stress urinary incontinence: a cross-sectional study. Cureus. (2023) 15:e38917. doi: 10.7759/cureus.38917
22. Campos, NC, de Carvalho, GM, de Santos, RA, de Brito Oliveira, RD, de Oliveira Sunemi, MM, and Figueiredo, EM. Prevalence, bother, and risk factors associated with occurrence of pelvic floor dysfunctions in young women: a cross-sectional survey. The Journal of Women's & Pelvic Health Physical Therapy. (2024) 48:194–201. doi: 10.1097/JWH.0000000000000305
23. Palmieri, S, De Bastiani, SS, Degliuomini, R, Ruffolo, AF, Casiraghi, A, Vergani, P, et al. Prevalence and severity of pelvic floor disorders in pregnant and postpartum women. Int J Gynecol Obstet. (2022) 158:346–51. doi: 10.1002/ijgo.14019
24. Mou, T, Brown, O, Dong, S, Abbasy, S, Leung, V, and Simon, M. Exploratory mixed methods study on care-seeking behaviors of Asian Americans with pelvic floor symptoms. Int Urogynecol J. (2023) 34:2557–64. doi: 10.1007/s00192-023-05574-6
25. Sundqvist, C, Li, X, Sundquist, K, and Jansåker, F. Sociodemographic disparities and parity in relation to urinary incontinence: a Nationwide primary healthcare cohort study (1997–2018). J Clin Med. (2022) 11:496. doi: 10.3390/jcm11030496
26. Peinado Molina, RA, Hernández Martínez, A, Martínez Vázquez, S, and Martínez Galiano, JM. Influence of pelvic floor disorders on quality of life in women. Front Public Health. (2023) 11:1180907. doi: 10.3389/fpubh.2023.1180907
27. Burzynski, B, Gibala, P, Soltysiak-Gibala, Z, Jurys, T, Przymuszala, P, Rzymski, P, et al. How urinary incontinence affects sexual activity in polish women: results from a cross-sectional study. Int J Environ Res Public Health. (2022) 19:13818. doi: 10.3390/ijerph192113818
28. Trinchieri, M, Perletti, G, Magri, V, Stamatiou, K, Montanari, E, and Trinchieri, A. Urinary side effects of psychotropic drugs: a systematic review and metanalysis. Neurourol Urodyn. (2021) 40:1333–48. doi: 10.1002/nau.24695
29. Ferrari, L, Gala, T, Igualada-Martinez, P, Brown, HW, Weinstein, M, and Hainsworth, A. Multidisciplinary team (MDT) approach to pelvic floor disorders. Continence. (2023) 7:100716. doi: 10.1016/j.cont.2023.100716
30. Monti, M, Fischetti, M, Santangelo, G, Giannini, A, D'Oria, O, Carbone, F, et al. Update on surgical treatment of female stress urinary incontinence. Minerva Obstetrics and Gynecology. (2020) 73:140–4. doi: 10.23736/S2724-606X.20.04658-4
Keywords: urinary incontinence, pelvic floor dysfunction, mixed methods, psychosocial impact, quality of life
Citation: Yalazı RÖ and Demirci N (2025) Determining the levels of pelvic floor disorders in women diagnosed with urinary incontinence: a mix-method study. Front. Med. 11:1509973. doi: 10.3389/fmed.2024.1509973
Received: 11 October 2024; Accepted: 26 December 2024;
Published: 30 January 2025.
Edited by:
Andrea Giannini, Umberto 1 Hospital, ItalyReviewed by:
Tullio Golia D’Augè, Sapienza University of Rome, ItalyCopyright © 2025 Yalazı and Demirci. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rüveyda Ölmez Yalazı, cnV2ZXlkYS5vbG1lenpAZ21haWwuY29t
†ORCID: Rüveyda Ölmez Yalazı, orcid.org/0000-0003-1826-2108
Nurdan Demirci, orcid.org/0000-0003-0489-186X
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.