
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Med. , 22 January 2025
Sec. Obstetrics and Gynecology
Volume 11 - 2024 | https://doi.org/10.3389/fmed.2024.1502969
This article is part of the Research Topic Reviews in Obstetrics and Gynecology 2024 View all 10 articles
 Mequanint Melesse Bicha1*
Mequanint Melesse Bicha1* Tewodros Zenabu Kebede1
Tewodros Zenabu Kebede1 Ayalew Lingerih Arefeaynie2
Ayalew Lingerih Arefeaynie2 Eden Woldegerima Meressa3
Eden Woldegerima Meressa3Although pulmonary tuberculosis is a common infectious disease, especially in low-and middle-income countries, female genital tract tuberculosis (TB) is rarely reported. Female genital TB might be asymptomatic or manifest clinically in an unusual way, making an early diagnosis challenging. The most often affected regions of the genital system are the fallopian tubes and endometrium. Menstrual abnormalities, infertility, and chronic pelvic pain are frequent presenting symptoms. Rare reports of vulvar and vaginal TB exist. This case report features a 35-year-old woman who had a bulging tumor in her vagina for a year before being identified with anterior vaginal wall TB, treated with anti-tuberculosis medication, and made improvements.
Tuberculosis (TB) is a communicable disease that is a major cause of morbidity and mortality. Its etiologic agent is a bacterium called Mycobacterium tuberculosis (1). The disease typically affects the lungs (pulmonary TB) but can affect other sites as well (2). A survey done in the national adult population in Ethiopia estimated that the prevalence of smear-positive TB was 108/100000 and that of bacteriologically confirmed TB was 277/100000 (3). Morgagni documented the first instance of female genital tuberculosis in 1744, following a post-mortem examination of a 20-year-old lady who died of tuberculosis and whose uterus and tubes were found to be packed with caseous contents (4, 5).
Female genital tuberculosis (FGTB) is a kind of extrapulmonary tuberculosis (EPTB) that affects the female reproductive organs, most commonly the fallopian tubes (90%), ovaries (10–30%), and endometrium (50%). The highest incidence of genital tuberculosis occurs in child-bearing age women. Because it is detected in approximately 10% of individuals with pulmonary tuberculosis, one may expect a high incidence of pelvic tuberculosis in areas where the incidence of pulmonary tuberculosis is high (6).
FGTB can present with chronic pelvic inflammatory disease, menstrual abnormalities, and infertility (7). The actual number of FGTB incidences cannot be estimated accurately, as it is often asymptomatic, and only 50% of cases are diagnosed without surgery (8). Vaginal tuberculosis is extremely rare (9) and may present as a differential of vaginal cancer (10). Vaginal tuberculosis was also found as a multifocal mass in the area of the vaginal introitus, with the main lesion reaching a diameter of 3 cm (11). This case report described an uncommon symptom of genital TB in the vagina, which has been rarely recorded in the literature.
A 35-year-old Para Five woman presented with a 1-year history of a progressively increasing bulging mass per vagina which was initially small but increased in size progressively. She also reported loss of appetite and a 30% weight loss. She had severe dyspareunia and discomfort during vaginal intercourse. She had five children, the youngest of whom was 4 years old. She delivered all of her children vaginally. After the last child, she was using Depo-Provera injection as a contraceptive method. She had no history of past TB treatment and no contact with a known TB patient. For these complaints, she visited a health center and was referred for further evaluation after she was told that her diagnosis was uterovaginal prolapse. She came to our hospital with these complaints, her history was taken, and she was examined. Her vital signs were all in the normal range, but she appeared emaciated; her weight was 35 kg, and her BMI was 13 kg/m2. On examination of the external genitalia, there was a 5 by 4 cm pink smooth protruded mass outside the introitus (Figure 1) which had a cystic consistency, was non-tender, and emerged from the mid-anterior vaginal wall. The urethral opening, the distal and proximal anterior vaginal walls, the lateral and posterior vaginal walls, the vaginal fornixes, and the cervix are all normal. Pelvic ultrasound revealed a normal size and outline of the urinary bladder, uterus, and adnexa (Figure 2). On laboratory evaluation, the erythrocyte sedimentation rate (ESR) was 100 mm/h, and a complete blood count showed lymphocytosis. The chest x-ray showed normal findings. Fine needle aspiration was done on the cystic mass (Figure 3) and using Ziehl Neelson Staining, microscopy showed Acid-Fast Bacilli (Figure 4). The sample was sent for culture, and tuberculosis was confirmed. The patient was given standard daily anti-tuberculosis therapy (isoniazid, rifampicin, ethambutol, and pyrazinamide) for the first 2 months and continued daily therapy with isoniazid and rifampicin for the next 4 months, and the anti-TB was given for a total of 6 months. She was counseled on drug adherence, put on a high-protein diet, and had an optimal follow-up in the hospital. After she completed the treatment, she was examined and the bulging mass per vagina disappeared (Figure 5), her BMI was corrected, and her overall wellbeing improved a lot.
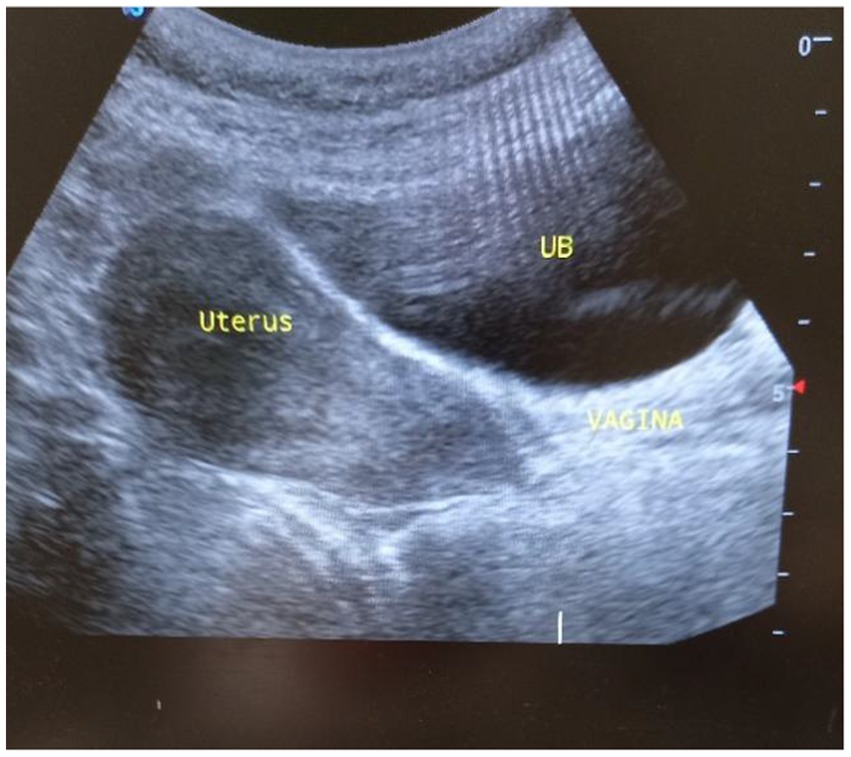
Figure 2. Pelvic ultrasound showing a sagittal view of a normal uterine and cervical outline, UB, Urinary bladder.
Genitourinary TB was reported to be responsible for 27.1 percent of cases of EPTB with genital TB being seen in 9 percent of cases (12). However, the exact incidence of FGTB is not known due to underreporting, asymptomatic cases, vague symptoms, and the lack of reliable and highly sensitive diagnostics (13, 14). The diagnosis of FGTB is made by detecting acid-fast bacilli under microscopy or culture on endometrial biopsy, or by detecting epithelioid granuloma during biopsy. The polymerase chain reaction is insufficient to make a diagnosis because of the higher rate of false positives. Laparoscopy and hysteroscopy can detect genital TB based on numerous findings (13). In our case, acid-fast bacilli were seen on a sample taken from the vaginal mass under microscopy, and tuberculosis was confirmed with culture.
Genital tract TB has been associated with up to 21% of infertility cases in low-and middle-income countries, due to tubal obstruction or adhesions in the uterine cavity (15, 16) and is even higher in patients with tubal factor infertility (17). Although the symptoms of genital TB are often absent, patients can present with infertility, pelvic/abdominal pain, or menstrual disturbances (18). Tuberculosis in the genital tract is usually secondary to tuberculosis elsewhere, most commonly in the lungs, but also in the kidneys, gastrointestinal tract, bones, or joints. (19). In our case, the chest x-ray was normal, and the patient did not have clinical evidence of tuberculosis in the internal female genital tract. Primary vaginal wall tuberculosis is highly likely.
Tuberculosis affecting the vagina and vulva is uncommon (20, 21) and is usually an extension from the endometrium or cervix, or very rarely primary due to transmission from an infected partner’s semen (22). Our case did not have menstrual abnormalities, infertility, or cervicitis. Her partner was not having tuberculosis. A hypertrophic ulcer or growth on the vulva or vagina may necessitate a biopsy and histological demonstration of granuloma, as well as the exclusion of cancer and other diseases such as syphilis and lymphogranuloma venereum (13, 14, 23). In our case, there was neither an ulcer nor hypertrophic mass, but it was just a cystic and soft anterior vaginal wall swelling protruding through the introitus. A giant vulval tumor has also been reported in FGTB (24). Even vesicovaginal and rectovaginal fistulas have also been reported (25). In this case, the vesicovaginal septum was normal before, during, and after treatment, and the mass disappeared with no sequelae.
Genital TB should be treated with anti-tuberculous therapy consisting of rifampin, isoniazid, pyrazinamide, ethambutol (RIPE) for 2 months followed by rifampin and isoniazid for 4 months (26). In this case, the standard anti-TB treatment was administered with proper follow-up for 6 months, and the patient improved.
In conclusion, it is always better to have a high index of suspicion in any mass arising from the female genital tract, particularly in areas where tuberculosis is rampant. Vaginal tuberculosis could be one of the differential diagnoses in women presenting with vaginal mass.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Our institution does not require ethical approval to report individual cases. Written informed consent was obtained from the patient for her anonymized information to be published in this article. Written informed consent was obtained from the patient for the publication of this case report.
MB: Conceptualization, Writing – original draft, Writing – review & editing. TK: Writing – review & editing. AA: Writing – review & editing. EM: Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
We appreciate the hard work and devotion of every employee at the University of Gondar Comprehensive Specialized Hospital throughout our client’s full course of treatment.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors declare that no Gen AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
AFB, Acid fast bacilli; BMI, Body mass index; EPTB, Extrapulmonary tuberculosis; FGTB, Female genital tuberculosis; Fig, Figure; Kg, Kilograms; Mm/h, Millimeter per hour; TB, Tuberculosis.
1. Chakaya, J, Khan, M, Ntoumi, F, Aklillu, E, Fatima, R, Mwaba, P, et al. Global tuberculosis report 2020–reflections on the global TB burden, treatment and prevention efforts. Int J Infect Dis. (2021) 113:S7–S12. doi: 10.1016/j.ijid.2021.02.107
2. World Health Organization. Global tuberculosis report 2021. Geneva: World Health Organization (2022).
3. Kebede, A, Alebachew, Z, Tsegaye, F, Lemma, E, Abebe, A, Agonafir, M, et al. The first population-based national tuberculosis prevalence survey in Ethiopia, 2010-2011. Int J Tuberc Lung Dis. (2014) 18:635–9. doi: 10.5588/ijtld.13.0417
4. Sharma, JB, Sharma, E, Sharma, S, and Dharmendra, S. Female genital tuberculosis: revisited. Indian J Med Res. (2018) 148:S71–83. doi: 10.4103/ijmr.IJMR_648_18
5. Mustafa, M, Amin, B, and Gayas, S. Female genital tuberculosis in infertile women. Arch Anesthesiol Crit Care. (2022) 8:226–9. doi: 10.18502/aacc.v8i3.9615
7. Bapna, N, Swarankar, M, and Kotia, N. Genital tuberculosis and its consequences on subsequent fertility. J Obstet Gynaecol India. (2005) 55:534–7.
8. Abebe, M, Lakew, M, Kidane, D, Lakew, Z, Kiros, K, and Harboe, M. Female genital tuberculosis in Ethiopia. Int J Gynecol Obstet. (2004) 84:241–6. doi: 10.1016/j.ijgo.2003.11.002
9. Nogales-Ortiz, F, Tarancón, I, and Nogales, FF Jr. The pathology of female genital tuberculosis. A 31-year study of 1436 cases. Obstet Gynecol. (1979) 53:422–8.
10. Carton, I, Balès, D, Bargain, A, and Lemoine, PLP. Vaginal tuberculosis as differential diagnosis of cancer: a case report. J Gynecol Obstet Hum Reprod. (2021) 50:101873. doi: 10.1016/j.jogoh.2020.101873
11. Alhakeem, M, and Schneider, A. Genital tuberculosis–a rare cause for vulvovaginal discharge and swelling. J Microbiol Infect Dis. (2013) 3:141–3. doi: 10.5799/ahinjs.02.2013.03.0097
12. Golden, MP, and Vikram, HR. Extrapulmonary tuberculosis: an overview. Am Fam Physician. (2005) 72:1761–8.
13. Sharma, JB. Current diagnosis and management of female genital tuberculosis. J Obstet Gynaecol India. (2015) 65:362–71. doi: 10.1007/s13224-015-0780-z
14. Neonakis, IK, Spandidos, DA, and Petinaki, E. Female genital tuberculosis: a review. Scand J Infect Dis. (2011) 43:564–72. doi: 10.3109/00365548.2011.568523
15. Aliyu, MH, Aliyu, SH, and Salihu, HM. Female genital tuberculosis: a global review. Int J Fertil Womens Med. (2004) 49:123–36.
16. Mondal, SK, and Dutta, T. A ten year clinicopathological study of female genital tuberculosis and impact on fertility. J Nepal Med Assoc. (2008) 48:202. doi: 10.31729/jnma.202
17. Fowler, ML, and Mahalingaiah, S. Case report of pelvic tuberculosis resulting in Asherman’s syndrome and infertility. Fertil Res Pract. (2019) 5:1–3. doi: 10.1186/s40738-019-0061-0
18. Sharma, JB, Roy, KK, Pushparaj, M, Gupta, N, Jain, SK, Malhotra, N, et al. Genital tuberculosis: an important cause of Asherman’s syndrome in India. Arch Gynecol Obstet. (2008) 277:37–41. doi: 10.1007/s00404-007-0419-0
19. Varma, T. Genital tuberculosis and subsequent fertility. Int J Gynecol Obstet. (1991) 35:1–11. doi: 10.1016/0020-7292(91)90056-B
20. Akhlaghi, F, and Hamedi, A. Postmenopausal tuberculosis of the cervix, vagina and vulva. Int J Gynaecol Obstet. (2004) 3:e6. doi: 10.5580/15e6
21. Manoj, K, Soma, M, Ajay, L, Ashish, A, Rakesh, S, and Paliwal, R. Tubercular sinus of labia majora: rare case report. Infect Dis Obstet Gynecol. (2008) 2008:1–3. doi: 10.1155/2008/817515
22. Parikh, FR, Nadkarni, SG, Kamat, SA, Naik, N, Soonawala, SB, and Parikh, RM. Genital tuberculosis—a major pelvic factor causing infertility in Indian women. Fertil Steril. (1997) 67:497–500. doi: 10.1016/S0015-0282(97)80076-3
23. Tiwari, P, Pal, DK, Moulik, D, and Choudhury, MK. Hypertrophic tuberculosis of vulva--a rare presentation of tuberculosis. Indian J Tuberc. (2010) 57:95–7.
24. Kumar, S, Kameshwarachari, P, and Ray, R. Giant vulval tumor due to tuberculosis. Int J Gynaecol Obstet. (2010) 110:69–70. doi: 10.1016/j.ijgo.2010.02.010
25. Sharma, J, Sharma, K, and Sarin, U. Tuberculosis: a rare cause of rectovaginal fistula in a young girl. J Obstet Gynaecol India. (2001) 51:176.
Keywords: female genital tract tuberculosis, vagina, tuberculosis, vaginal wall mass, case report
Citation: Bicha MM, Kebede TZ, Arefeaynie AL and Meressa EW (2025) Female genital tuberculosis presenting as a protruding anterior vaginal wall mass: a case report. Front. Med. 11:1502969. doi: 10.3389/fmed.2024.1502969
Received: 27 September 2024; Accepted: 20 December 2024;
Published: 22 January 2025.
Edited by:
Mattia Dominoni, San Matteo Hospital Foundation (IRCCS), ItalyReviewed by:
Sunil Joshi, University of Miami, United StatesCopyright © 2025 Bicha, Kebede, Arefeaynie and Meressa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mequanint Melesse Bicha, bWVxdW1hbi5tbUBnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.