- 1Internal Medicine Department, College of Medicine, King Faisal University, Al-Ahsa, Saudi Arabia
- 2Family and Community Medicine Department, College of Medicine, King Faisal University, Al-Ahsa, Saudi Arabia
- 3Internal Medicine Department, King Fahad Specialist Hospital, Dammam, Saudi Arabia
- 4Department of Pediatric, King Fahad Medical City, Riyadh, Saudi Arabia
- 5Pathology Department, King Fahad Specialist Hospital, Dammam, Saudi Arabia
- 6Internal Medicine Department, Prince Saud Bin Jalawi Hospital, Al-Ahsa, Saudi Arabia
Background: COVID-19 poses a significant threat to global public health. As the severity of SARS-CoV-2 infection varies among individuals, elucidating risk factors for severe COVID-19 is important for predicting and preventing illness progression, as well as lowering case fatality rates. This work aimed to explore risk factors for developing severe COVID-19 to enhance the quality of care provided to patients and to prevent complications.
Methods: A retrospective study was conducted in Saudi Arabia’s eastern province, including all COVID-19 patients aged 18 years or older who were hospitalized at Prince Saud Bin Jalawi Hospital in July 2020. Comparative tests as well as both univariate and multivariate logistic regression analyses were performed to identify risk factors for developing severe COVID-19 and poor outcomes.
Results: Based on the comparative statistical tests patients with severe COVID-19 were statistically significantly associated with older age and had higher respiratory rate, longer hospital stay, and higher prevalence of diabetes than non-severe cases. They also exhibited statistically significant association with high levels of potassium, urea, creatinine, lactate dehydrogenase (LDH), D-dimer, and aspartate aminotransferase (AST). The univariate analysis shows that having diabetes, having high severe acute respiratory infection chest X-ray scores, old age, prolong hospitalization, high potassium and lactate dehydrogenase, as well as using insulin, heparin, corticosteroids, favipiravir or azithromycin were all statistically significant associated with severe COVID-19. However, after adjustments in the multivariate analysis, the sole predictor was serum LDH (p = 0.002; OR 1.005; 95% CI 1.002–1.009). In addition, severe COVID-19 patients had higher odds of being prescribed azithromycin than non-severe patients (p = 0.001; OR 13.725; 95% CI 3.620–52.043). Regarding the outcomes, the median hospital stay duration was statistically significantly associated with death, intensive care unit admission (ICU), and mechanical ventilation. On the other hand, using insulin, azithromycin, beta-agonists, corticosteroids, or favipiravir were statistically significantly associated with reduced mortality, ICU admission, and need of mechanical ventilation.
Conclusion: This study sheds light on numerous parameters that may be utilized to construct a prediction model for evaluating the risk of severe COVID-19. However, no protective factors were included in this prediction model.
Introduction
In December 2019, the first case of COVID-19 was reported in Wuhan, a Chinese city in the province of Hubei (1). Its causative agent, SARS-CoV-2, is among the deadliest coronaviruses, alongside SARS-CoV-1, which causes severe acute respiratory syndrome (SARS), and MERS-CoV, which causes Middle East respiratory syndrome (MERS) (2, 3). However, the morbidity and mortality of COVID-19 are far greater than those of SARS and MERS (3).
COVID-19 has a wide spectrum of clinical manifestations, from asymptomatic to critical and life-threatening (4). Severe cases usually require artificial ventilation and intensive care unit (ICU) admission. Additionally, the disease’s case fatality rate is estimated to range from 3.4 to 11% (5, 6). Because certain populations have a higher chance of developing adverse outcomes, uncovering the risk factors that promote severe disease is important for predicting and preventing illness progression, as well as lowering the case fatality rate (6). Previous studies have constructed predictive models using various risk factors to identify high-risk groups that may develop severe COVID-19 infection. These factors range from demographic factors such as age, sex, and ethnicity to comorbidities and laboratory results (7). However, only a few published papers have investigated risk factors for severe SARS-CoV-2 specifically among the Saudi population in the Eastern province (8, 9). According to Al Dossary’s study, age, gender, and ethnicity are key predictors of COVID-19 severity; however, this study did not look at the relationship between laboratory parameters and COVID-19 severity or prognosis (8). Moreover, Ansari et al., who studied 1,444 hospitalized COVID-19 patients, found that old age, the presence of underlying cardiovascular conditions, an abnormal white blood count, and abnormal blood urea nitrogen levels are independent predictors of mortality, but his study did not account for disease severity or other outcomes such as ICU admission and mechanical ventilation requirement (9). Despite having larger sample sizes and statistically significant results, these studies had some limitations and still there is no conclusive data available.
Geographic variation may potentially contribute to differences in COVID-19 risks and severity (10). The reasons behind these differences are unknown, although they have been linked to a complex and interconnected patterning of several elements (10). Furthermore, in Saudi Arabia, the existence of religious sites that attract millions of people each year raises the risk of possible outbreaks (11). Population-based data could aid the identification of risk factors, which could then be used to optimize COVID-19 case management, provide more individualized guidance to patient groups, and reduce case fatalities (12, 13). Therefore, this work aimed to explore risk factors for developing severe COVID-19 as well as look at determinants of mortality, ICU admission and mechanical ventilation requirement to enhance the quality of care provided to patients and to prevent complications.
Materials and methods
Study design and participants
A retrospective cohort study was conducted in Saudi Arabia’s eastern province, including all COVID-19 patients aged 18 years or older who were hospitalized at Prince Saud Bin Jalawi Hospital in July 2020. Diagnoses were confirmed by polymerase chain reaction (PCR) testing. Patients who did not have an electronic medical record were excluded.
Data collected from the medical record system included sociodemographic data of the patient, basic clinical and laboratory data, medication history, and hospital course (length of hospital stay, severe COVID-19, and clinical outcome), with all patients being tracked until discharge or death.
Definitions
Chest X-ray clinical findings were graded based on the severe acute respiratory infection (SARI) chest X-ray severity scoring system as 1: normal; 2: patchy atelectasis and/or hyperinflation and/or bronchial wall thickening; 3: focal consolidation; 4: multifocal consolidation; and 5: diffuse alveolar changes (14). Then patients were divided into two groups based on their SARI score; low score (1-3) and high score (4-5).
Patients were categorized according to disease severity into severe and non-severe cases. Severe COVID-19 was defined as per the Saudi Ministry of Health Protocol for COVID-19, particularly taking an oxygen saturation below 93% in room air or a respiratory rate above 30/min as the determining criteria (15).
Clinical outcome was assessed in terms of percent mortality, mechanical ventilation, and ICU admission.
Statistical analysis
Data were analyzed using the Statistical Package for Social Sciences (SPSS) for Windows, version 22 (SPSS Inc. Chicago, IL, USA). Shapiro–Wilk and Kolmogorov–Smirnov tests were used to assess the normality of continuous data. Continuous variables were expressed as mean and standard deviation and categorical data as numbers and percentages. The comparative tests (Chi-square (χ2) and Fisher’s exact tests for categorical variables, and independent t-test and Mann–Whitney U test for quantitative variables) were used to identify significant factors for COVID-19 disease severity as well as clinical outcome (mortality, mechanical ventilation, and ICU admission). The following independent variables were interpreted as continuous data; age, length of hospitalization, hemoglobin, leukocyte, platelets, potassium, sodium, AST, albumin, urea, creatinine, lactate dehydrogenase, creatine Kinase, and d-dimer, while other data interpreted as categorical data; Sex, ICU admission, Mechanical ventilation, DM, HTN, Respiratory diseases, Cardiovascular disease, Chronic kidney disease, SARI CXR Severity, Insulin, Heparin, Corticosteroids, Favipiravir, and Azithromycin. These variables were chosen based on the literature review and their clinical relevance. Then both univariate and multivariate logistic regression analyses were performed to identify COVID-19 disease severity predictors. Variables with clinical relevance and statistical significance from the comparative tests were included in a univariate analysis. However, even if a variable is statistically significant in comparative analysis, it may be excluded from further analysis based on clinical judgment, data quality issues, or if it is deemed redundant or highly collinear with other variables. Furthermore, variables with statistically significant association on univariate analysis were included in a multivariable regression model. This step-by-step strategy aims to refine relevant predictors for future multivariate modelling, hence improving the robustness of our findings. All statistical analyses were based on two-sided hypothesis tests with a significance level of p < 0.05.
Ethical consideration
The Institutional Review Board at The King Fahad Hospital approved this study (IRB KFHH No. H-05-HS-065) and waived patient consent due to the study’s retrospective nature. The study was performed according to the Helsinki Declaration, and all data were collected, coded, and analyzed to ensure data integrity and patient privacy.
Results
Epidemiological and clinical characteristics
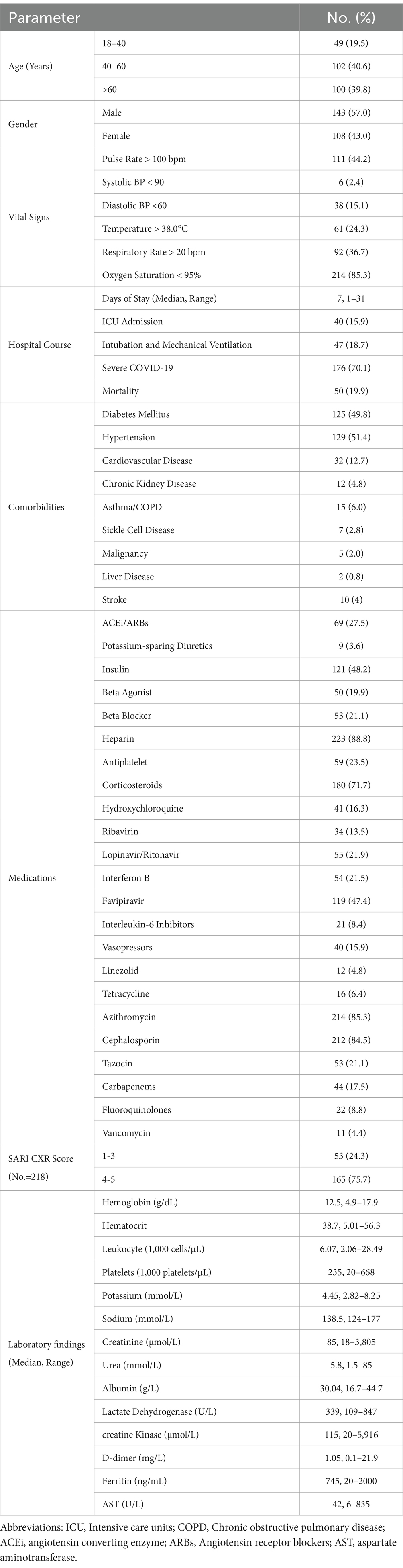
A total of 251 COVID-19 patients were included in this study. The majority (57%) were male, and 39.8% were over the age of 60 years. Hypertension and diabetes mellitus constituted the most common comorbidities (51.4 and 49.8% respectively). Hospital admission periods ranged 1–31 days with a median of 7 days; in addition, 15.9% of patients were admitted to the ICU, 19.9% suffered mortality, 18.7% required mechanical ventilation, and around two-thirds (70.1%) had severe COVID-19. Heparin (88.8%), azithromycin (85.3%), cephalosporin (84.5%), corticosteroids (71.7%), and favipiravir (47.4%) were the most common prescribed drugs (Table 1).
Regarding radiology, more than 75% of patients had score 4–5 on the SARI CXR system. In laboratory results, the median levels of hemoglobin, white blood cells, and platelets were 12.5 gm/dL, 6.07 × 109/L, and 235 × 109/L respectively, while median levels of potassium, urea, and creatinine were 4.45 mmol/L, 5.8 mmol/L, and 85 μmol/L, respectively, (Table 1).
Factors associated with the severity of COVID-19
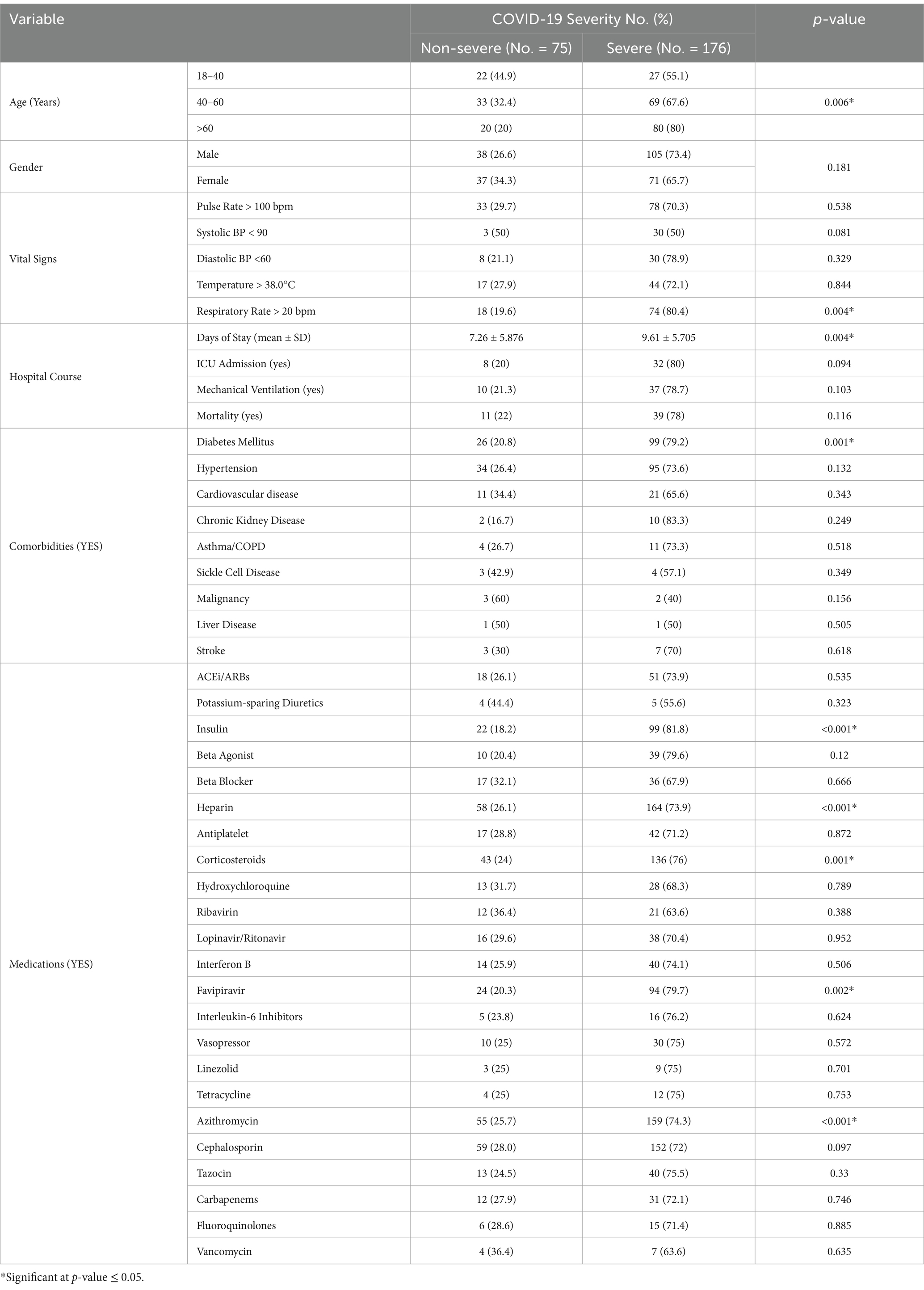
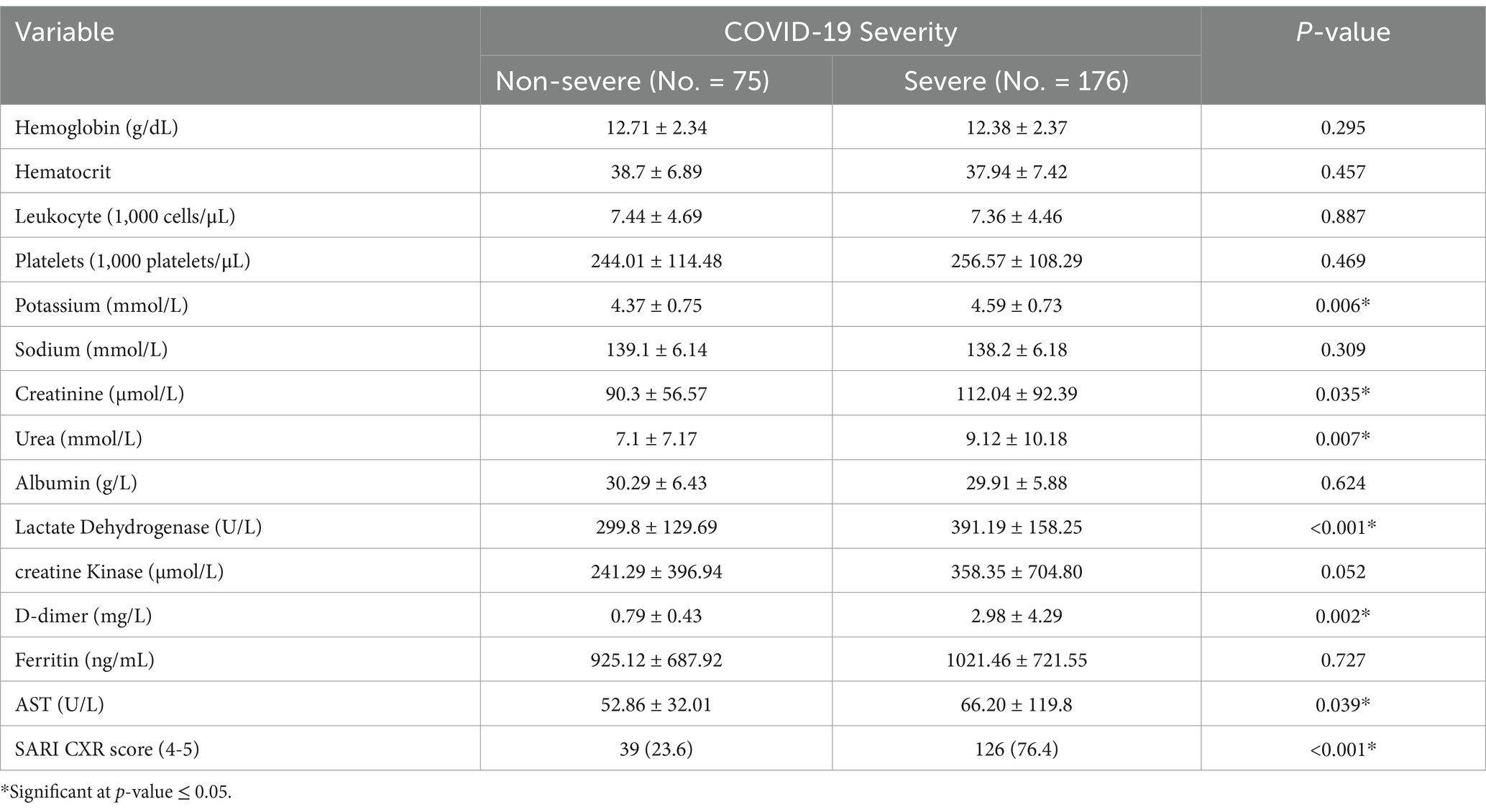
Based on comparative statistical tests, severe COVID-19 was statistically significantly associated with older age, high respiratory rate, prolonged hospital stay, and diabetes mellitus; the use of insulin, heparin, corticosteroids, favipiravir, or azithromycin; and higher levels of potassium, urea, creatinine, lactate dehydrogenase (LDH), D-dimer, and aspartate aminotransferase (AST), as well as high SARI CXR scores (Tables 2, 3). Of note, respiratory rate was eliminated from the univariate analysis, although being statistically significant in the comparative analysis, because it is used to assess illness severity and is related to mechanical ventilation.
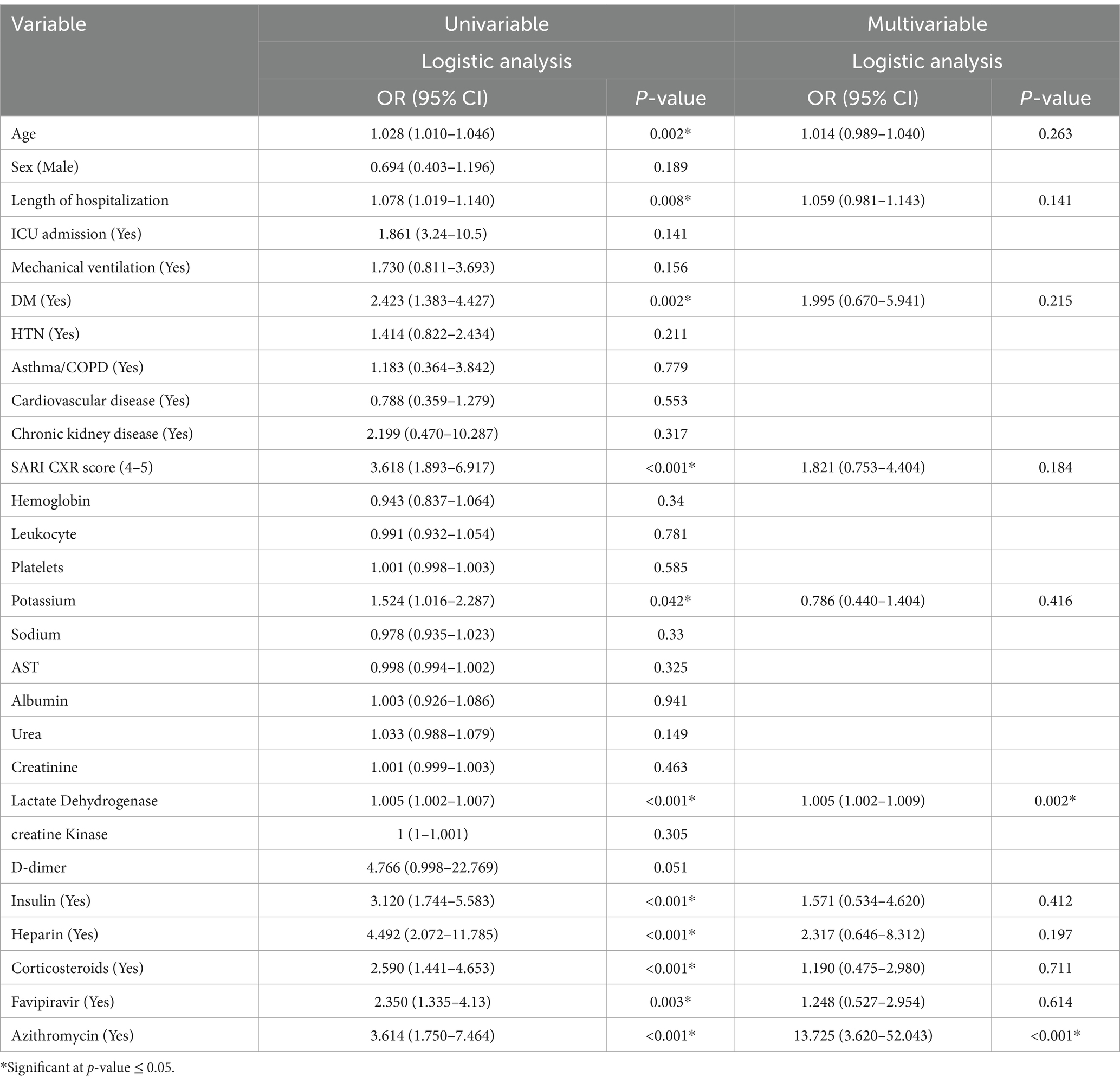
The univariate analysis shows that patients with diabetes mellitus had 2.423 times higher odds of developing severe COVID-19 compared to those without diabetes. Similarly, those with high SARI CXR scores had 3.618 times higher odds of having severe COVID-19. Moreover, old age, prolong hospitalization, high potassium and lactate dehydrogenase, as well as using insulin, heparin, corticosteroids, favipiravir or azithromycin were all significantly associated with severe COVID-19 (Table 4). However, after adjustments in the multivariate analysis, the sole predictor was serum LDH (p = 0.002; OR 1.005; 95% CI 1.002–1.009). Additionally, azithromycin was statistically significantly more prescribed in severe COVID-19 cases (p = 0.001; OR 13.725; 95% CI 3.620–52.043) (Table 4).
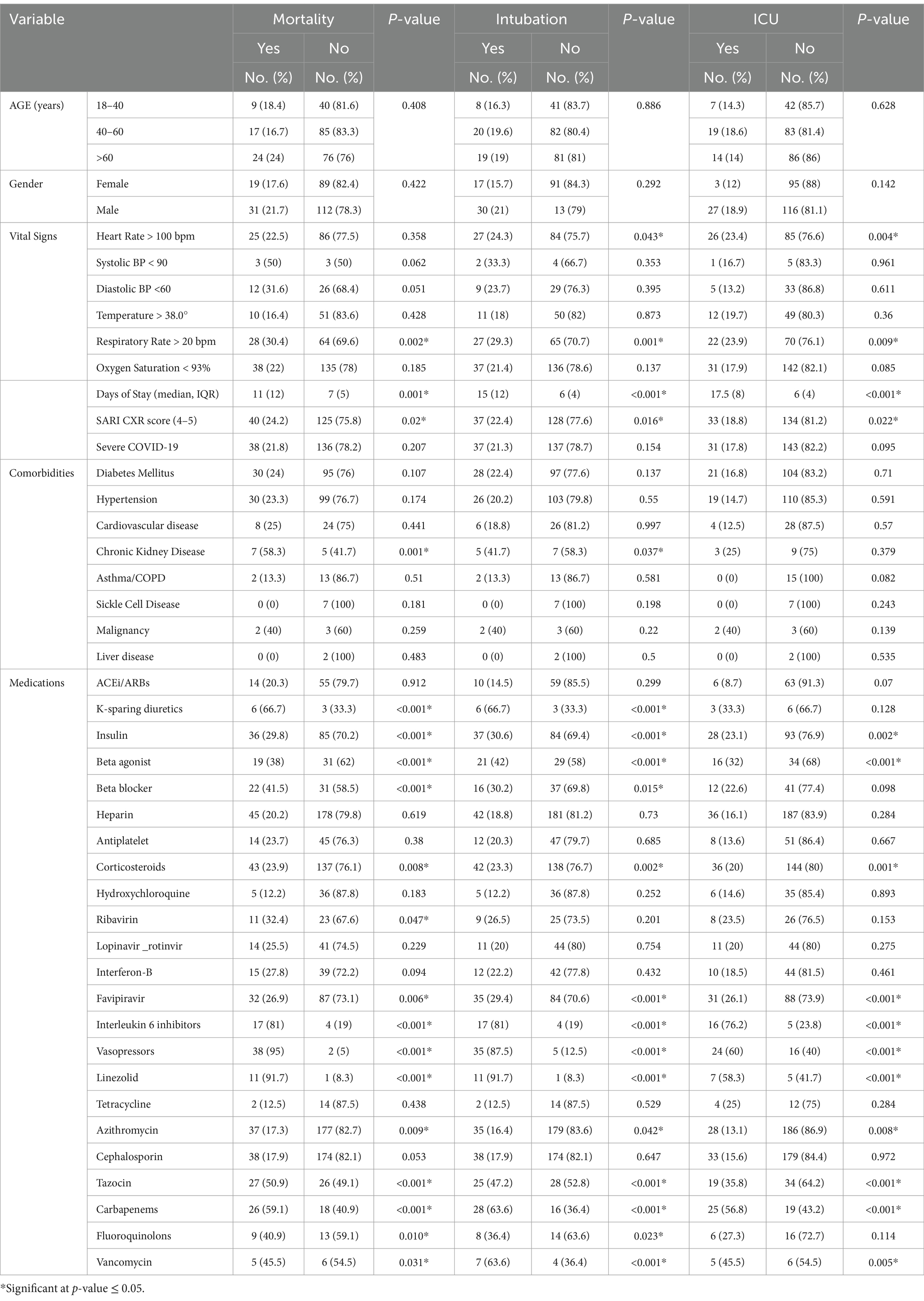
The comparative statistical analysis for demographic and clinical factors with COVID-19 outcomes (mortality, mechanical ventilation, and ICU admission) is presented in Table 5. The median hospital stay duration was statistically significantly associated with all three outcomes. Patients who died had a median stay of 11 days, compared to 7 days for those who survived (p = 0.001). Similarly, patients requiring intubation had a median stay of 15 days, compared to 6 days for those who did not require intubation (p < 0.001). Those admitted to the ICU had a median stay of 17.5 days, while those not admitted to the ICU had a median stay of 6 days (p < 0.001). Regarding patients’ comorbidities, chronic kidney disease was statistically significantly associated with increase mortality (p = 0.001).
Patients treated with Interleukin 6 inhibitors, Vasopressors, Carbapenems, or Linezolid had a statistically significant association with increased poor outcomes, including death, intubation, and ICU admission (p < 0.001). Moreover, using K-sparing diuretics was statistically significantly associated with increased mortality and need of intubation (p < 0.001). On the other hand, using insulin, azithromycin, beta-agonists, corticosteroids, or favipiravir was statistically significantly associated with reduced all these poor outcomes. Tazocin was statistically significantly associated with increased mortality but reduced intubation and ICU admission (p < 0.001). Furthermore, patients on Vancomycin were statistically significantly associated with increased intubation, although they had decreased mortality and ICU admission. Using beta blockers was statistically significantly associated with decreased mortality and the requirement for intubation.
Discussion
The COVID-19 pandemic has challenged healthcare systems in both developed and developing countries, with a wide spectrum of clinical symptoms and consequences (16). Currently based on the WHO, COVID-19 is an established health concern that requires long-term care, rather than a worldwide health emergency (17). This study shed light on different demographic and clinical characteristics associated with severe COVID-19 which might assist in minimizing adverse consequences. Findings from this study found that old age, high respiratory rate, long hospital stay, and diabetes as well as high levels of potassium, urea, creatinine, LDH, D-dimer, and AST all were statistically significantly associated with severe COVID-19. However, when these factors were merged for further analysis, the sole predictor was serum LDH, possibly due to multicollinearity and confounding. In addition, azithromycin was more prescribed in severe cases, which is likely associated with severe COVID-19. Regarding the clinical outcomes, the median hospital stay duration was statistically significantly associated with increased mortality, ICU admission, and mechanical ventilation requirements. However, using azithromycin, corticosteroids, or favipiravir was statistically significantly associated with reduced mortality, ICU admission, and need for mechanical ventilation.
In the current study, the median period of hospital stay was seven days, which aligns with a recent Saudi study (18). Additionally, approximately two-thirds (70.1%) of our patients had severe disease, 15.9% were admitted to the ICU, and the mortality was 19.9%. In a previous Chinese study, 81% of cases were mild, 14% were severe and required ventilation in the ICU, 5% were critical and involved respiratory failure, septic shock, and/or multiple organ dysfunction and the overall case-fatality rate was 2.3% (19). The greater percentage of severe cases in the present study may be attributed to it exclusively including hospitalized patients. Another study in New York assessed the outcome of 2,634 patients who were discharged or had died at their study end point. Of the 2,634 patients; 14.2% were treated in the ICU, 12.2% received invasive mechanical ventilation, and 21% died (20). Likewise, in a 2020 study of hospitalized patients in Germany, 22% died (21).
Numerous factors contribute to poor outcomes in patients with COVID-19-infection. This study found COVID-19 severity to be higher in older patients, consistent with the findings of Wang et al. and Zhang et al., who reported increased age to be one of the most commonly stated demographic factors that increases the probability of a severe course of disease and poor outcomes (22, 23). These findings could be attributed to the greater likelihood of comorbidities and weakening of the immune system as people age (24).
Regarding gender, most COVID-19 patients in this study were male (57%), which may confirm earlier reports that male sex is a risk factor for a positive SARS-CoV-2 test (25–27). This difference in viral attachment between men and women may be due to biological variances, differences in immunological responses, sex hormones, or a confluence of risky behaviors or lifestyle choices (28). Notably, Assiri et al. observed the conflicting finding that women were more likely to have a positive SARS-CoV-2 test than men. This discrepancy is expected because of the greater recruitment of female patients from the affiliated women’s university (Princess Nourah bint Abdulrahman University) in that study (18). On the other hand, our study, found no sex disparity in the severity and outcome of COVID-19 patients which aligns with Albishi et al. study in Jeddah, Saudi Arabia (29).
The most prevalent comorbidities among COVID-19 participants in our study were hypertension (51.4%) and diabetes (49.8%). These findings agree with earlier reports in Saudi Arabia and elsewhere (18, 30–32). Moreover, diabetic patients in this study population were at higher risk of severe disease, consistent with previous studies (33, 34). According to Palaiodimos et al., risk of death is elevated among hospitalized diabetic patients with COVID-19 compared to non-diabetic individuals (35). The pathophysiology of this elevated risk could be attributed to a compromised immune system caused by chronic or transient hyperglycemia as well as chronic inflammation (36, 37).
Laboratory parameters can be important indicators and predictors of disease severity. In this study, high levels of urea, creatinine, potassium, LDH, D-dimer, and AST were all statistically significantly associated with severe cases of COVID-19. Several prior reports have indicated a link between low renal function and poor COVID-19 prognosis (38–41). In addition, D-dimer was recognized to be a key predictor of COVID-19 prognosis, with high D-dimer most likely being caused by acute lung damage or increased risk of thromboembolic consequences (42, 43). The effect of COVID-19 on the liver has been controversial, with some research linking elevated liver enzyme levels to infection severity, whereas others found no difference between mild and severe infections (44). Our results also highlighted serum LDH as an independent risk factor associated with severe cases of COVID-19. Similar results have been reported by previous studies (45–48); collectively, these findings emphasize the importance of monitoring serum LDH levels in COVID-19 patients upon admission.
The SARI chest X-ray severity scoring system was proposed by Taylor et al. in 2015 as a validated CXR scoring method that non-radiologists may use to assess patients with acute respiratory infections. Despite having lower sensitivity than a CT scan, this system can be used to radiologically assess a severe acute respiratory infection (14). Our study demonstrated that the early evaluation of patients with COVID-19 was statistically significantly aided by chest imaging. Notably, 75% of patients had a high SARI chest X-ray score (4-5), and this high score was statistically significantly associated with severe COVID-19 cases (p < 0.001). It has been reported previously that the radiologic severity index can be used to describe disease severity and aid in therapy planning (49). Thus, a modified grading method based on chest X-rays can be of benefit in determining COVID-19 severity, particularly in places with limited resources and expertise.
Antibiotics have been used to treat COVID-19 in up to 72% of cases worldwide (50–52). In the current study, the antibiotics most commonly used during hospital stays were azithromycin and cephalosporins, while the most frequently prescribed antiviral medication was favipiravir. Similar findings were reported previously among Bangladeshi patients with COVID-19 (52). Notably, one of the most interesting findings of the current study was the relationship between the administration of azithromycin and considerably reduced rates of mortality, ICU admission, and mechanical ventilation; in addition, azithromycin was more prescribed in severe COVID-19. The potential efficacy of azithromycin against SARS-CoV-2 infection is hypothesized to stem from multiple mechanisms of action, including increasing cellular pH to prevent virus entry, binding to and inhibiting the SARS-CoV-2 spike protein, reducing several inflammatory cytokines that have been shown to be major drivers of COVID-19 mortality, and finally treating secondary bacterial infections (53–55). Despite these facts, an Italian study with a large sample size (4,861) and propensity-matched controls of the same number, found that azithromycin was ineffective in treating SARS-CoV-2 infection, and raised concerns about the hazards associated with its inappropriate use (53).
In addition to azithromycin, this study found favipiravir and corticosteroids to be more utilized in patients with severe disease (p < 0.05). Moreover, these medications were reported with lower mortality, intubation, and ICU admission. Favipiravir has been identified as one of the most effective COVID-19 treatments when provided early in the disease’s course, since it can increase viral clearance and improve clinical outcome (56). Meanwhile, corticosteroids are recommended for patients with severe or critical COVID-19 (60). Notably, while steroids are helpful and lower mortality because of their beneficial regulatory effects against hyper-inflammation, they could also increase mortality by allowing more secondary infections (57–59). Moreover, since interleukin-6 inhibitors, vasopressors, carbapenems, and linezolid are frequently administered to critically ill COVID-19 patients who are already at a higher risk of poor outcomes, the observed associations between these drugs and poor outcomes may be due to their conditions rather than a direct effect of the treatments.
Our study’s strengths include data only from confirmed hospitalized COVID-19 patients in Saudi Arabia’s eastern province where there has been limited study among this community. Also, a three-step analysis ending in multivariate analysis was used which enhanced the methodological value and contribution. Furthermore, our study addressed the limitations of previously published papers by including the missing parameters such as laboratory parameters (8). It also looked at determinants of COVID-19 severity as well as other outcomes like ICU admission and mechanical ventilation requirement, rather than only death (9). As a result, this study sheds light on numerous parameters that may be utilized to construct a prediction model for evaluating the risk of severe COVID-19 and might assist healthcare practitioners manage patients, especially in locations with limited resources such as using the SARI chest X-ray scoring system which supported Satoto et al. finding (49). Despite these, there are some limitations that might affect the results of our study. First, data were collected from a single center over a short time and did not include pregnant women; as such, the generalizability of the results to the broader population is limited. Second, cross-validation was not conducted to overcome the overfitting problem; thus, future studies should consider using it to improve the robustness of model evaluations. Third, COVID-19 vaccinations had not yet been approved at the time of data collection, and new strains had not yet been detected, thus the association reported in this study may be altered. Moreover, no protective factors such as healthy diet, supplementation, or atopic conditions were included in a COVID-19 severity prediction model. Finally, we acknowledge the possibility that additional factors were not examined in this study which may also influence the severity of COVID-19. On this basis, further replication with independent cohorts is required.
Conclusion
This study identified hypertension and diabetes mellitus as the most common comorbidities among COVID-19 patients in the eastern province of Saudi Arabia. The results highlighted a number of factors that can help predict the possibility of severe COVID-19, such as old age, diabetes mellitus, and high values for the laboratory parameters including urea, creatinine, potassium, LDH, D-dimer, and AST. After adjustment, only serum LDH was found to be an independent risk factor associated with severe COVID-19 infection. Finally, using azithromycin, corticosteroids, or favipiravir was statistically significantly associated with reduced mortality, ICU admission, and need for mechanical ventilation. These indicators can potentially be combined into a scoring system to identify high-risk individuals, identify priority groups for COVID-19 vaccination, facilitate better outcomes, and potentially develop preventative strategies.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The Institutional Review Board at the King Fahad Hospital approved this study (IRB KFHH No. H-05-HS-065) and waived patient consent due to the study’s retrospective nature. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because Informed consent was not applicable.
Author contributions
HAA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. ED: Conceptualization, Data curation, Project administration, Validation, Visualization, Writing – original draft. ZA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AmA: Conceptualization, Data curation, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing – review & editing. AbA: Data curation, Investigation, Methodology, Resources, Validation, Visualization, Writing – review & editing. FA: Data curation, Investigation, Formal analysis, Resources, Validation, Visualization, Writing – review & editing. MA: Data curation, Investigation, Methodology, Resources, Validation, Visualization, Writing – review & editing. AE: Conceptualization, Data curation, Investigation, Methodology, Validation, Supervision, Writing – review & editing. EA: Conceptualization, Investigation, Methodology, Project administration, Resources, Validation, Writing – review & editing. KMAE: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Validation, Visualization, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Deanship of Scientific Research, Vice Presidency for Graduate Studies and Scientific Research, King Faisal University, Saudi Arabia [KFU242904].
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. WHO. (2020). WHO Statement regarding cluster of pneumonia cases in Wuhan, China. Available online at: https://www.who.int/hongkongchina/news/detail/09-01-2020-who-statement-regarding-cluster-of-pneumonia-cases-in-wuhan-china
2. Liu, B, Li, M, Zhou, Z, Guan, X, and Xiang, Y. Can we use interleukin-6 (IL-6) blockade for coronavirus disease 2019 (COVID-19)-induced cytokine release syndrome (CRS)? J Autoimmun. (2020) 111:102452. doi: 10.1016/j.jaut.2020.102452
3. Costela-Ruiz, VJ, Illescas-Montes, R, Puerta-Puerta, JM, Ruiz, C, and Melguizo-Rodríguez, L. SARS-CoV-2 infection: the role of cytokines in COVID-19 disease. Cytokine Growth Factor Rev. (2020) 54:62–75. doi: 10.1016/j.cytogfr.2020.06.001
4. Zhou, F, Yu, T, Du, R, Fan, G, Liu, Y, Liu, Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retro- spective cohort study. Lancet. (2020) 395:1054–62. doi: 10.1016/S0140-6736(20)30566-3
5. Rajgor, DD, Lee, MH, Archuleta, S, Bagdasarian, N, and Quek, SC. The many estimates of the COVID-19 case fatality rate. Lancet Infect Dis. (2020) 20:776–7. doi: 10.1016/S1473-3099(20)30244-9
6. Wolff, D, Nee, S, Hickey, NS, and Marschollek, M. Risk factors for Covid-19 severity and fatality: a structured literature review. Infection. (2021) 49:15–28. doi: 10.1007/s15010-020-01509-1
7. Wong, KC, Xiang, Y, Yin, L, and So, HC. Uncovering clinical risk factors and predicting severe COVID-19 cases using UK biobank data: machine learning approach. JMIR Public Health Surveill. (2021) 7:e29544. doi: 10.2196/29544
8. Al Dossary, R, Alnimr, A, Aljindan, R, Alkharsah, KR, Al-Qurayn, AK, Eltreifi, O, et al. Predictors of illness severity in COVID-19 cases in Saudi Arabia. Infect Drug Resist. (2021) 14:4097–105. doi: 10.2147/IDR.S333300
9. Ansari, KA, Alwazzeh, MJ, Alkuwaiti, FA, Farooqi, FA, Al Khathlan, N, Almutawah, H, et al. Early determinants of mortality in hospitalized COVID-19 patients in the Eastern Province of Saudi Arabia. Int J Gen Med. (2022) 15:1689–701. doi: 10.2147/IJGM.S349598
10. Magesh, S, John, D, Li, WT, Li, Y, Mattingly-App, A, Jain, S, et al. Disparities in COVID-19 outcomes by race, ethnicity, and socioeconomic status: a systematic-review and Meta-analysis. JAMA Netw Open. (2021) 4:e2134147. doi: 10.1001/jamanetworkopen.2021.34147
11. Sheerah, HA, Almuzaini, Y, and Khan, A. Public health challenges in Saudi Arabia during the COVID-19 pandemic: a literature review. Healthcare (Basel). (2023) 11:1757. doi: 10.3390/healthcare11121757
12. Booth, A, Reed, AB, Ponzo, S, Yassaee, A, Aral, M, Plans, D, et al. Population risk factors for severe disease and mortality in COVID-19: a global systematic review and meta-analysis. PLoS One. (2021) 16:e0247461. doi: 10.1371/journal.pone.0247461
13. Lipsitch, M, Swerdlow, DL, and Finelli, L. Defining the epidemiology of Covid-19—studies needed. N Engl J Med. (2020) 382:1194–6. doi: 10.1056/NEJMp2002125
14. Taylor, E, Haven, K, Reed, P, Bissielo, A, Harvey, D, McArthur, C, et al. A chest radiograph scoring system in patients with severe acute respiratory infection: a validation study. BMC Med Imaging. (2015) 15:61. doi: 10.1186/s12880-015-0103-y
15. Saudi Ministry of Health. (2023). Protocol for patients suspected of/confirmed with COVID-19 (version 3.9) Saudi Ministry of Health. Saudi Ministry of Health Protocol for Patients Suspected of/Confirmed with COVID-19. 3.; pp. 1–12.
16. Subhani, F, Chhotani, AA, Waheed, S, Zahid, RO, Azizi, K, and Buksh, AR. Development of COVID-19 severity assessment score in adults presenting with COVID-19 to the emergency department. BMC Infect Dis. (2022) 22:576. doi: 10.1186/s12879-022-07535-8
17. WHO. (2023). Statement on the fifteenth meeting of the IHR (2005) Emergency Committee on the COVID-19 pandemic. Available online at: https://www.who.int/news/item/05-05-2023-statement-on-the-fifteenth-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-coronavirus-disease-(covid-19)-pandemic
18. Assiri, RA, Bepari, A, Patel, W, Hussain, SA, Niazi, SK, Alshangiti, A, et al. Exploration of sex and age-based associations in clinical characteristics, predictors of severity, and duration of stay among COVID-19 patients at the University Hospital of Saudi Arabia. Healthcare (Basel). (2023) 11:751. doi: 10.3390/healthcare11050751
19. Wu, Z, and McGoogan, JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA. (2020) 323:1239–42. doi: 10.1001/jama.2020.2648
20. Richardson, S, Hirsch, JS, Narasimhan, M, Crawford, JM, McGinn, T, Davidson, KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the new York City area. JAMA. (2020) 323:2052–9. doi: 10.1001/jama.2020.6775
21. Karagiannidis, C, Mostert, C, Hentschker, C, Voshaar, T, Malzahn, J, Schillinger, G, et al. Case characteristics, resource use, and outcomes of 10 021 patients with COVID-19 admitted to 920 German hospitals: an observational study. Lancet Respir Med. (2020) 8:853–62. doi: 10.1016/S2213-2600(20)30316-7
22. Wang, D, Hu, B, Hu, C, Zhu, F, Liu, X, Zhang, J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. (2020) 323:1061–9. doi: 10.1001/jama.2020.1585
23. Zhang, J-J, Dong, X, Cao, Y-Y, Yuan, Y-D, Yang, Y-B, Yan, Y-Q, et al. Clinical characteristics of 140 patients infected with SARSCoV-2 in Wuhan, China. Allergy. (2020) 75:1730–41. doi: 10.1111/all.14238
24. Barnett, K, Mercer, SW, Norbury, M, Watt, G, Wyke, S, and Guthrie, B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. (2012) 380:37–43. doi: 10.1016/S0140-6736(12)60240-2
25. de Lusignan, S, Dorward, J, Correa, A, Jones, N, Akinyemi, O, Amirthalingam, G, et al. Risk factors for SARS-CoV-2 among patients in the Oxford Royal College of general practitioners research and surveillance Centre primary care network: a cross-sectional study. Lancet Infect Dis. (2020) 20:1034–42. doi: 10.1016/S1473-3099(20)30371-6
26. Pijls, BG, Jolani, S, Atherley, A, Derckx, RT, Dijkstra, JIR, Franssen, GHL, et al. Demographic risk factors for COVID-19 infection, severity, ICU admission and death: a meta-analysis of 59 studies. BMJ Open. (2021) 11:e044640. doi: 10.1136/bmjopen-2020-044640
27. Chen, N, Zhou, M, Dong, X, Qu, J, Gong, F, Han, Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. (2020) 395:507–13. doi: 10.1016/S0140-6736(20)30211-7
28. Kelada, M, Anto, A, Dave, K, and Saleh, SN. The role of sex in the risk of mortal- ity from COVID-19 amongst adult patients: a systematic review. Cureus. (2020) 12:e10114. doi: 10.7759/cureus.10114
29. Albishi, WK, Ramadan, IK, Abulkalam, SMMD, Alsaab, HA, Hayd, MYB, AL-Ghamdi, MA, et al. Factors associated with the severity of Covid19 in Jeddah, Saudi Arabia: a retrospective cohort study. AMJ. (2023) 16:822–41.
30. Meister, T, Pisarev, H, Kolde, R, Kalda, R, Suija, K, Milani, L, et al. Clinical characteristics and risk factors for COVID-19 infection and disease severity: a nationwide observational study in Estonia. PLoS One. (2022) 17:e0270192. doi: 10.1371/journal.pone.0270192
31. Bajgain, KT, Badal, S, Bajgain, BB, and Santana, MJ. Prevalence of comorbidities among individuals with COVID-19: a rapid review of current literature. Am J Infect Control. (2021) 49:238–46. doi: 10.1016/j.ajic.2020.06.213
32. Shi, Y, Yu, X, Zhao, H, Wang, H, Zhao, R, and Sheng, J. Host susceptibility to severe COVID-19 and establishment of a host risk score: findings of 487 cases outside Wuhan. Crit Care. (2020) 24:108. doi: 10.1186/s13054-020-2833-7
33. Shoaib, N, Noureen, N, Munir, R, Shah, FA, Ishtiaq, N, Jamil, N, et al. COVID-19 severity: studying the clinical and demographic risk factors for adverse outcomes. PLoS One. (2021) 16:e0255999. doi: 10.1371/journal.pone.0255999
34. Manalu, BPS, Leonard, E, Paramita, C, and Tendean, M. Factors affecting the disease severity of COVID-19 patients in an emergency setting. Family Medicine & Primary Care. Review. (2022) 24:56–60. doi: 10.5114/fmpcr.2022.113014
35. Palaiodimos, L, Chamorro-Pareja, N, Karamanis, D, Li, W, Zavras, PD, Chang, KM, et al. Diabetes is associated with increased risk for in-hospital mortality in patients with COVID-19: a systematic review and meta-analysis comprising 18,506 patients. Hormones. (2021) 20:305–14. doi: 10.1007/s42000-020-00246-2
36. Figueroa-Pizano, MD, Campa-Mada, AC, Carvajal-Millan, E, Martinez-Robinson, KG, and Chu, AR. The underlying mechanisms for severe COVID-19 progression in people with diabetes mellitus: a critical review. AIMS Public Health. (2021) 8:720–42. doi: 10.3934/publichealth.2021057
37. Huang, I, Lim, M, and Pranata, R. Diabetes mellitus is associated with increased mortality and severity of disease in COVID-19 pneumonia – a systematic review, meta-analysis, and meta-regression. Diabetes Metab Syndr. (2020) 14:395–403. doi: 10.1016/j.dsx.2020.04.018
38. Trabulus, S, Karaca, C, Balkan, II, Dincer, MT, Murt, A, Ozcan, SG, et al. Kidney function on admission predicts in-hospital mortality in COVID-19. PLoS One. (2020) 5:1–14. doi: 10.1371/journal.pone.0238680
39. Cheng, Y, Luo, R, Wang, K, Zhang, M, Wang, Z, Dong, L, et al. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. (2020) 97:829–38. doi: 10.1016/j.kint.2020.03.005
40. Uribarri, A, Núñez-Gil, IJ, Aparisi, A, Becerra-Muñoz, VM, Feltes, G, Trabattoni, D, et al. Impact of renal function on admission in COVID-19 patients: an analysis of the international HOPE COVID-19 (health outcome predictive evaluation for COVID 19) registry. J Nephrol. (2020) 33:737–45. doi: 10.1007/s40620-020-00790-5
41. Tao, Z, Xu, J, Chen, W, Yang, Z, Xu, X, Liu, L, et al. Anemia is associated with severe illness in COVID-19: a retrospective cohort study. J Med Virol. (2021) 93:1478–88. doi: 10.1002/jmv.26444
42. Gao, Y, Li, T, Han, M, Li, X, Wu, D, Xu, Y, et al. Diagnostic utility of clinical laboratory data determinations for patients with the severe COVID-19. J Med Virol. (2020) 92:791–6. doi: 10.1002/jmv.25770
43. Lehmann, A, Prosch, H, Zehetmayer, S, Gysan, MR, Bernitzky, D, Vonbank, K, et al. Impact of persistent D-dimer elevation following recovery from COVID-19. PLoS One. (2021) 16:e0258351. doi: 10.1371/journal.pone.0258351
44. Fadl, N, Ali, E, and Salem, TZ. COVID-19: risk factors associated with infectivity and severity. Scand J Immunol. (2021) 93:e13039. doi: 10.1111/sji.13039
45. Kojima, K, Yoon, H, Okishio, K, Tsuyuguchi, K, et al. Increased lactate dehydrogenase reflects the progression of COVID-19 pneumonia on chest computed tomography and predicts subsequent severe disease. Sci Rep. (2023) 13:1012. doi: 10.1038/s41598-023-28201-2
46. Han, Y, Zhang, H, Mu, S, Wei, W, Jin, C, and Tong, C. Lactate dehydrogenase, an independent risk factor of severe COVID-19 patients: a retrospective and observational study. Aging (Albany NY). (2020) 12:11245–58. doi: 10.18632/aging.103372
47. Huang, Y, Guo, L, Chen, J, Wu, M, Zhang, C, Liu, Z, et al. Serum lactate dehydrogenase level as a prognostic factor for COVID-19: a retrospective study based on a large sample size. Front Med. (2022) 8:671667. doi: 10.3389/fmed.2021.671667
48. Li, C, Ye, J, Chen, Q, Hu, W, Wang, L, Fan, Y, et al. Elevated lactate dehydrogenase (LDH) level as an independent risk factor for the severity and mortality of COVID-19. Aging (Albany NY). (2020) 12:15670–81. doi: 10.18632/aging.103770
49. Satoto, B, Handoyo, T, Sari, MNW, Santoso, AG, and Prasetyo, NE. The chest X-ray radiologic severity index as a determinant of the severity of COVID-19 pneumonia: study based on the duration of treatment and inpatient rooms. Chin J Acad Radiol. (2023) 6:10–7. doi: 10.1007/s42058-022-00109-2
50. Rawson, TM, Moore, LSP, Zhu, N, Ranganathan, N, Skolimowska, K, Gilchrist, M, et al. Bacterial and fungal coinfection in individuals with coronavirus: a rapid review to support COVID-19 antimicrobial prescribing. Clin Infect Dis. (2020) 71:2459–68. doi: 10.1093/cid/ciaa530
51. Townsend, L, Hughes, G, Kerr, C, Kelly, M, O'Connor, R, Sweeney, E, et al. Bacterial pneumonia coinfection and antimicrobial therapy duration in SARS-CoV-2 (COVID-19) infection. JAC Antimicrob Resist. (2020) 2:dlaa071. doi: 10.1093/jacamr/dlaa071
52. Mah-E-Muneer, S, Hassan, MZ, Biswas, MAAJ, Rahman, F, Akhtar, Z, Das, P, et al. Use of antimicrobials among suspected COVID-19 patients at selected hospitals, Bangladesh: findings from the first wave of COVID-19 pandemic. Antibiotics. (2021) 10:738. doi: 10.3390/antibiotics10060738
53. Antonazzo, IC, Fornari, C, Rozza, D, Conti, S, di Pasquale, R, Cortesi, P, et al. Azithromycin use and outcomes in patients with COVID-19: an observational real-world study. Int J Infect Dis. (2022) 124:27–34. doi: 10.1016/j.ijid.2022.09.005
54. Echeverría-Esnal, D, Martin-Ontiyuelo, C, Navarrete-Rouco, ME, De-Antonio Cuscó, M, Ferrández, O, Horcajada, JP, et al. Azithromycin in the treatment of COVID-19: a review. Expert Rev Anti-Infect Ther. (2021) 19:147–63. doi: 10.1080/14787210.2020.1813024
55. Sultana, J, Cutroneo, PM, Crisafulli, S, Puglisi, G, Caramori, G, and Trifirò, G. Azithromycin in COVID-19 patients: pharmacological mechanism, clinical evidence and prescribing guidelines. Drug Saf. (2020) 43:691–8. doi: 10.1007/s40264-020-00976-7
56. Manabe, T, Kambayashi, D, Akatsu, H, and Kudo, K. Favipiravir for the treatment of patients with COVID-19: a systematic review and meta-analysis. BMC Infect Dis. (2021) 21:489. doi: 10.1186/s12879-021-06164-x
57. Piccica, M, Lagi, F, Trotta, M, Spinicci, M, Zammarchi, L, Bartoloni, A, et al. High-dose steroids for the treatment of severe COVID-19. Intern Emerg Med. (2021) 16:1395–9. doi: 10.1007/s11739-021-02707-x
58. RECOVERY Collaborative GroupHorby, P, Lim, WS, Emberson, JR, Mafham, M, Bell, JL, et al. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med. (2021) 384:693–704. doi: 10.1056/NEJMoa2021436
59. Sari, A, Aslan, M, and Ekinci, O. The effect of steroids used in the treatment of coronavirus disease 2019 on infections in intensive care. North Clin Istanb. (2022) 9:131–9. doi: 10.14744/nci.2022.43827
60. Agarwal, A, Hunt, B, Stegemann, M, Rochwerg, B, Lamontagne, F, Siemieniuk, RA, et al. A living WHO guideline on drugs for covid-19. BMJ. (2020) 4:m3379. doi: 10.1136/bmj.m3379, Update in: BMJ. 2020 Nov 19;371:m4475. doi: 10.1136/bmj.m4475. Update in: BMJ. 2021 Mar 31;372:n860. doi: 10.1136/bmj.n860. Update in: BMJ 2021;374:n1703
Keywords: COVID-19, SARS-CoV-2, severe, risk factors, outcome, epidemiology
Citation: Alkhalifa HA, Darwish E, Alsalman Z, Alfaraj A, Alkhars A, Alkhalifa F, Algaraash M, Elshebiny AM, Alkhoufi E and Elzorkany KMA (2025) Predictors of developing severe COVID-19 among hospitalized patients: a retrospective study. Front. Med. 11:1494302. doi: 10.3389/fmed.2024.1494302
Edited by:
Zhongshan Cheng, St. Jude Children’s Research Hospital, United StatesReviewed by:
Smruti Karale, Rajarshee Chhatrapati Shahu Maharaj Government Medical College and CPR Hospital Kolhapur, IndiaXin Liu, University of Houston, United States
Pui Yeung Lee, Yale University, United States
Copyright © 2025 Alkhalifa, Darwish, Alsalman, Alfaraj, Alkhars, Alkhalifa, Algaraash, Elshebiny, Alkhoufi and Elzorkany. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zaenb Alsalman, QWxzYWxtYW4uemFpbmFiQGhvdG1haWwuY29t; WmFsc2FsbWFuQGtmdS5lZHUuc2E=
†ORCID: Hussain Abduljaleel Alkhalifa orcid.org/0000-0002-4709-5030
Ehab Darwish orcid.org/0000-0001-5063-2792
Zaenb Alsalman orcid.org/0000-0002-1008-7977
Aman Alfaraj orcid.org/0009-0009-4410-0680
Abdullah Alkhar orcid.org/0009-0002-9635-7268
Fatimah Alkhalifa orcid.org/0000-0003-4853-571X
Mohammed Algaraash orcid.org/0009-0004-2849-7693
Ahmed Mohammed Elshebiny orcid.org/0000-0001-9215-7088
Emad Alkhoufi orcid.org/0000-0002-4427-8579
Khaled Mohamed Amin Elzorkany orcid.org/0000-0003-4632-891X
 Hussain Abduljaleel Alkhalifa
Hussain Abduljaleel Alkhalifa Ehab Darwish
Ehab Darwish Zaenb Alsalman
Zaenb Alsalman Aman Alfaraj
Aman Alfaraj Abdullah Alkhars
Abdullah Alkhars Fatimah Alkhalifa
Fatimah Alkhalifa Mohammed Algaraash
Mohammed Algaraash Ahmed Mohammed Elshebiny
Ahmed Mohammed Elshebiny Emad Alkhoufi
Emad Alkhoufi Khaled Mohamed Amin Elzorkany
Khaled Mohamed Amin Elzorkany