- 1School of Public Health, College of Health Sciences, Arsi University, Asella, Ethiopia
- 2School of Nursing and Midwifery, College of health sciences, Arsi university, Asella, Ethiopia
- 3School of Nursing and Midwifery, College of Health and Medical sciences, Haramaya university, Harar, Ethiopia
Background: Every day throughout the world more than 4,000 infants and young children die because colostrum feeding was not initiated within an hour of birth as recommended by the World Health Organization (WHO)/United Nations Children’s Fund. Even though breastfeeding is common in Ethiopia, the widespread belief that colostrum feeding causes morbidity and mortality among neonates still exists.
Objective: To assess the colostrum feeding practice and It’s associated factors among mothers who come for Post-natal care at Asella Referral and Teaching Hospital, Asella Town, Southeast Ethiopia from November 20, 2023, to January 25, 2024.
Method: This study employed an institutional-based cross-sectional study among 301 surveyed postnatal care mothers from November 20, 2023, to January 25, 2024. Systematic random sampling was employed to select study participants. A pretest was performed to check the reliability and clarity of the study questionnaires. The tool to examine the practice of colostrum feeding and related aspects was modified from earlier studies. The collected data were input into Epi Info version 7.2.5.0 and exported to SPSS version 26 for analysis. Bivariate and multivariable logistic regression analyses were used to identify variables associated with the practice of colostrum feeding. The variables with significant association were identified based on p-value < 0.05.
Results: In this study, 301 study participants took part, with a 99% response rate. The mean age of mothers was found to be 27.13 ± 5.46. This study’s overall prevalence of practice was 57.8% (95% CI, 52.2–63.35). Being Urban residence (AOR = 4.05, 95%CI: 2.18–7.52), health education counseling (AOR = 4.31, 95%CI: 1.27–10.73), and favorable attitude toward colostrum milk (AOR = 6.64, 95% CI: 3.61–12.2) were factors significantly associated with colostrum feeding practice.
Conclusion and recommendations: In comparison to WHO recommendations, the study area had a low rate of colostrum feeding practice. Additionally, this study also identified factors associated with maternal colostrum feeding practice level such as urban residence, counseling on timely initiation of breastfeeding during antenatal care, and good maternal attitude toward colostrum feeding. Therefore, Health education dissemination should be given to postnatal mothers regarding the importance of colostrum feeding.
Introduction
Colostrum is the thick, yellowish fluid secreted by the breast beginning in midpregnancy and continuing for 3–4 days after delivery. It has a high concentration of antibodies and other protective elements essential for newborns (1). It contains antibodies which help the baby to fight against illness. Furthermore, early breastfeeding helps to forge the bond between mother and baby as well as enable a constant milk supply (2). Compared to regular milk, colostrum has much lower levels of lipids and potassium, but it is rich in proteins, carbohydrates, vitamin A, and sodium chloride. Its laxative properties, along with bioactive immune components, help protect newborns from various illnesses and allergic conditions (3). Besides being a pure food source, breast milk provides all the essential nutrients a baby needs during the first 6 months of life. The American Academy of Pediatrics recommends exclusive breastfeeding for the first 6 months (2).
The two main components of colostrum are also growth factors and immune factors. Colostrum nursing allows the baby to receive the mother’s passive immunity, which aids in the infant’s defense against bacteria, viruses, fungi, giardia, and other protozoan parasites. This comprehensive defense is something even antibiotics cannot offer. Moreover, unlike synthetic antibiotics, colostrum does not lead to bacterial resistance. As a result, it supports the infant’s healthy development, strength, and longevity (4, 5). Colostrum is also a great source of vital growth factors, which are important for promoting growth, promoting regeneration, and accelerating the repair of aging skin, muscles, collagen, bone cartilage, and nerve tissue (6). In addition, it contains high levels of sodium, chloride, and cholesterol, which collectively support the optimal development of the infant’s heart, brain, and central nervous system (7, 8).
Globally, less than half of newborns begin breastfeeding within the first hour of life. As a result of not receiving colostrum within this crucial time frame, over 4,000 infants die worldwide each day (9). In 2015, approximately 2.7 million newborns died globally within the first month of life (0–27 days), with more than a third of these deaths occurring on the first days (10). Southeast Asia and Sub-Saharan Africa together account for two-thirds of the nearly 3 million newborn deaths that occur annually (1). Sub-Saharan Africa continues to have the highest infant mortality rates in the world. In developing countries, 3,000–4,000 newborns die daily from acute respiratory diseases and diarrhea because they do not receive adequate breast milk and colostrum (11). According to the World Health Organization (WHO), neonatal deaths contribute to 45% of all deaths in children under the age of five (12). While three-quarters of newborn deaths happen within the first 7 days of life, over one-third of these deaths occur within the first 24 h after birth (13).
Numerous studies suggest that children who did not receive colostrum are at a higher risk of wasting, infections, stunting, and underweight (14–16). Avoiding colostrum also reduces a newborn’s intake of immunoglobulin and other vital nutrients, which impairs the gastrointestinal tract’s priming and raises the risk of infant morbidity and mortality (17). Despite the long-term health and immunological benefits that colostrum offers, it is often avoided in many countries, including Nepal, Pakistan, and Burkina Faso, where a significant number of mothers discard colostrum (18–20). In Ethiopia, discarding colostrum is a widespread nutritional malpractice across nearly all communities. For instance, in Afar, 35% of mothers reported discarding colostrum, in Debra Tabor, the rate was 25.6%, in Raya Kobo it was 13.5%, in Axum it was 6.3%, in Jinka Town it was 9.8%, and in Motta Town it was 20.3% (21–24).
In developing countries, among women who do not give colostrum feeds to their children, most of them avoid colostrum feeding based on traditional or cultural beliefs (14, 25, 26). Ethiopia has one of the highest infant mortality rates in the world that occur due to inappropriate neonatal feeding. Even though colostrum discarding hurts child health, little is known about the extent of the problem and its contributing factors in South Eastern Ethiopia (11). Furthermore, in Ethiopia, a substantial number of neonatal deaths occur within the first week of life, and many mothers hold the misconception that colostrum feeding is linked to neonatal morbidity and mortality. As a result, they believe that colostrum should be discarded. However, the reasons behind this misconception have not been thoroughly studied in Ethiopia, particularly in the study area. Therefore, this study aimed to assess the Colostrum feeding practice and identify its associated factors among mothers attending postnatal care at Asella Referral and Teaching Hospital, located in Asella Town in Southeast Ethiopia.
Objectives
General objective
To assess colostrum feeding practice and its associated factors among mothers attending post-natal care service in Asella Referral and Teaching Hospital from November 20, 2023, to January 25, 2024.
Specific objectives
To determine the colostrum feeding practice among mothers attending post-natal care service in Asella Referral and Teaching Hospital from November 20, 2023, to January 25, 2024.
To identify factors associated with colostrum feeding practice among mothers attending post-natal care service in Asella Referral and Teaching Hospital from November 20, 2023, to January 25, 2024.
Specific objectives
After reviewing different literature, the following theoretical framework is developed as indicated in Figure 1.
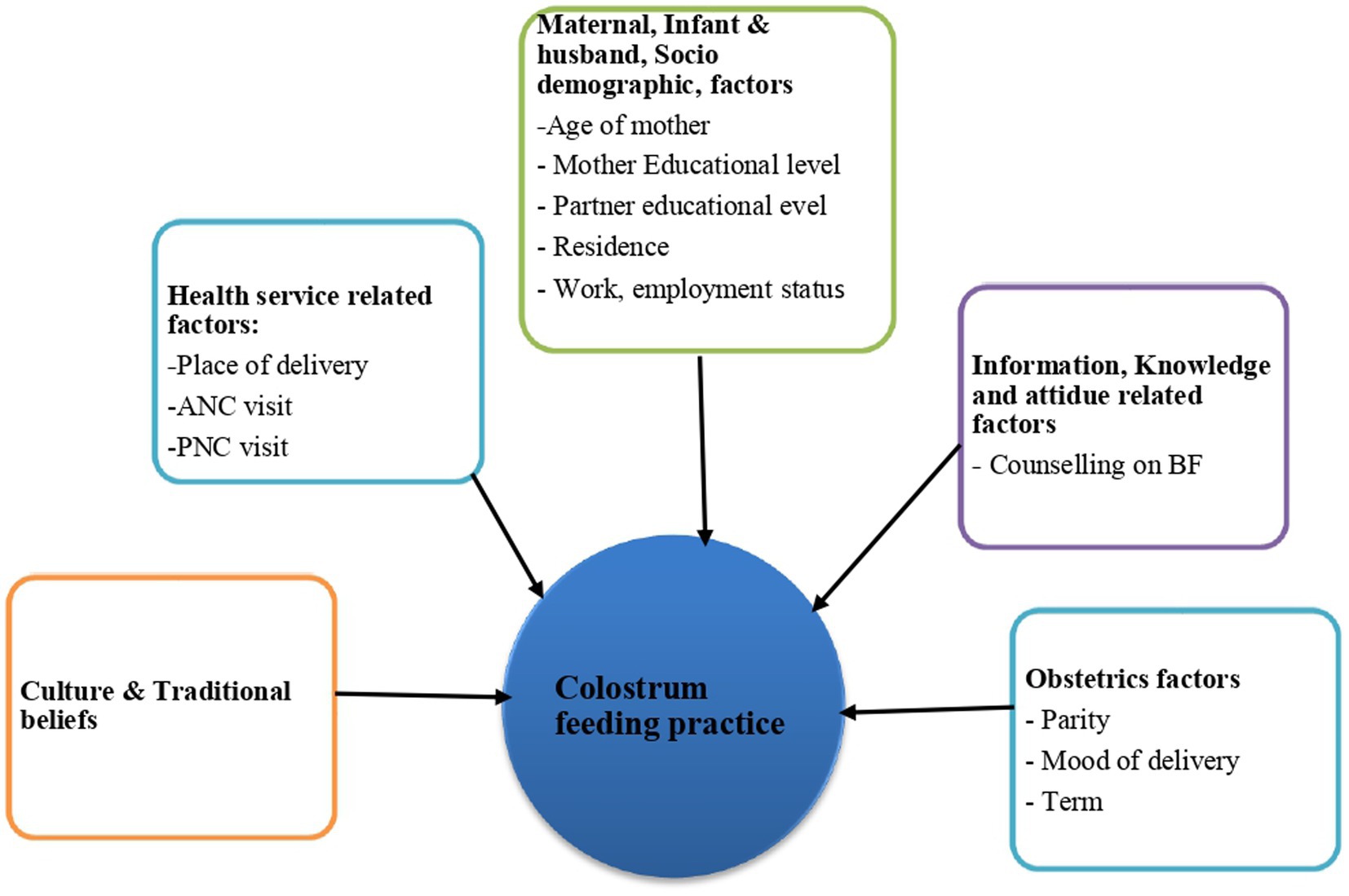
Figure 1. Theoretical framework for the colostrum feeding practice and its associated factors among Mothers Who Come for Postnatal Care to Asella Referral and Teaching Hospital, Arsi Zone, South-East Ethiopia, 2024.
Materials and methods
Study design and setting
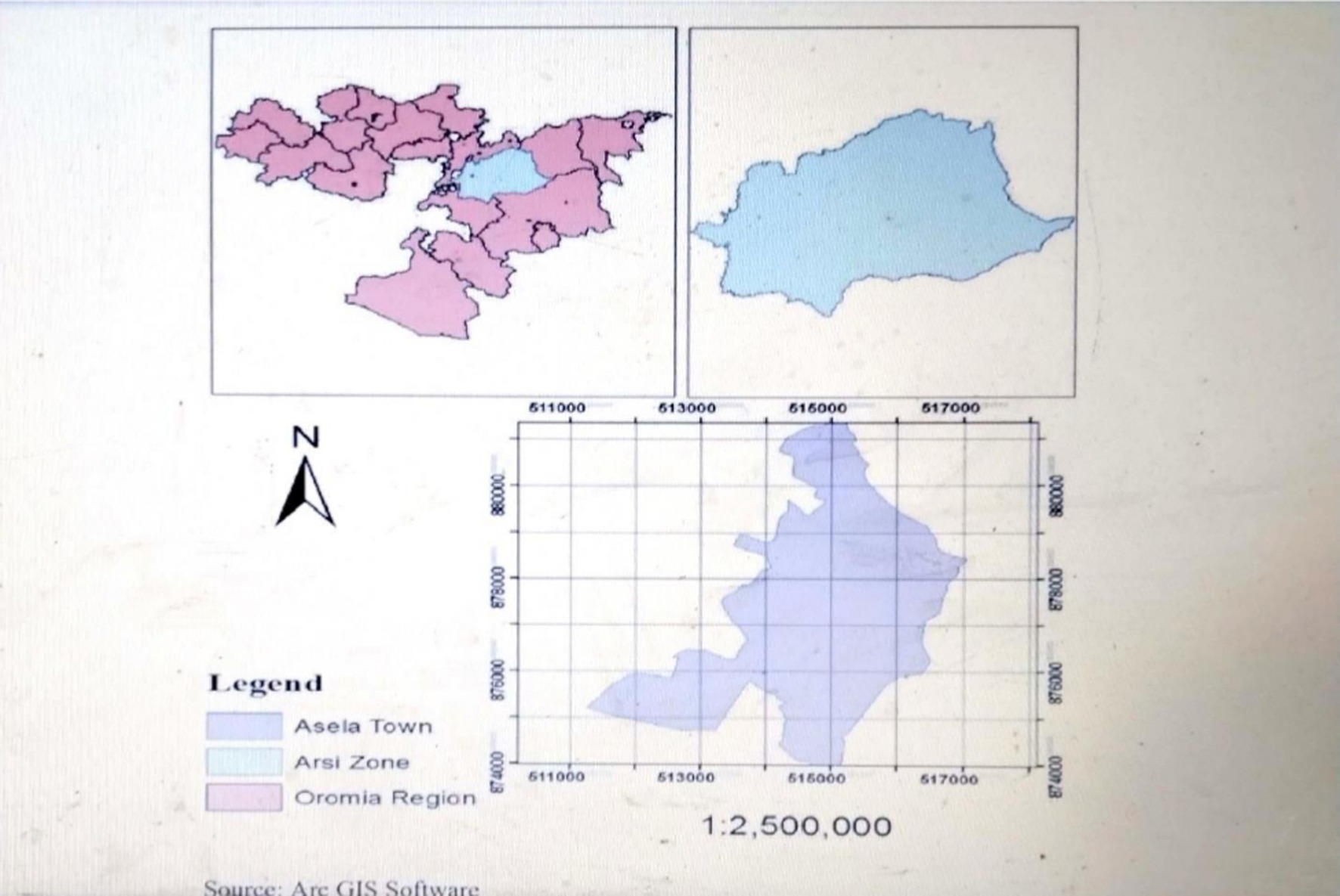
This study was conducted from November 20, 2023, to January 25, 2024, at Asella Referral and Teaching Hospital, located in Arsi Zone, Oromia Regional State (Figure 2). The hospital was established in 1964 and is situated about 175 kilometers southeast of the capital city, Addis Ababa. Currently, the zone has a total population of around 3,563,474 of which 1,767,483 were females. Of the total number of women, approximately 44.8% were in the reproductive age group. According to the hospital’s annual report provided by the administration, it has a total of 443 staff members. Asella Referral and Teaching Hospital offers preventive, curative, and diagnostic services to the population of approximately 3.5 million in Asella town and its surrounding areas. The hospital operates through three main departments: outpatient department (OPD), inpatient department, and emergency department. There are several services available for mothers and newborns at the hospital, such as antenatal care (including investigations and immunizations), delivery services, postnatal care (PNC) services, and an expanded program on immunization (EPI) services. According to the hospital’s quarterly report, around 1,254 mothers got care there. From these, 289 were from the obstetrics and gynecology follow-up department, 553 from the obstetric ward, and 412 from the EPI department.
Source and study populations
The source populations were all mothers who had children less than 6 months of age and who attended postnatal care at Asella Referral and Teaching Hospital. Mothers who had children less than 6 months of age, Attending Asella Referral and Teaching Hospital, and were eligible for the study were included in the study. However, mothers who had severe mental illnesses or were unable to participate in the study during data collection were excluded from the study.
Sample size determination
The required sample size was determined by a formula with a single population. The calculation was made assuming 95% confidence interval, 5% margin of error and the prevalence of 56.5% colostrum feeding practice reported in a study done in Ambo (26). In this study, the calculation for correctional formula was applied because the sample from which population drawn is less than 10,000 and by adding non-response rate of 10%, sample size final became 304. For the second objective (Factors associated with colostrum feeding practice), we used double population proportion formula in Epi info version 7 statistical calculation to determine a sample size as indicated in Table 1.
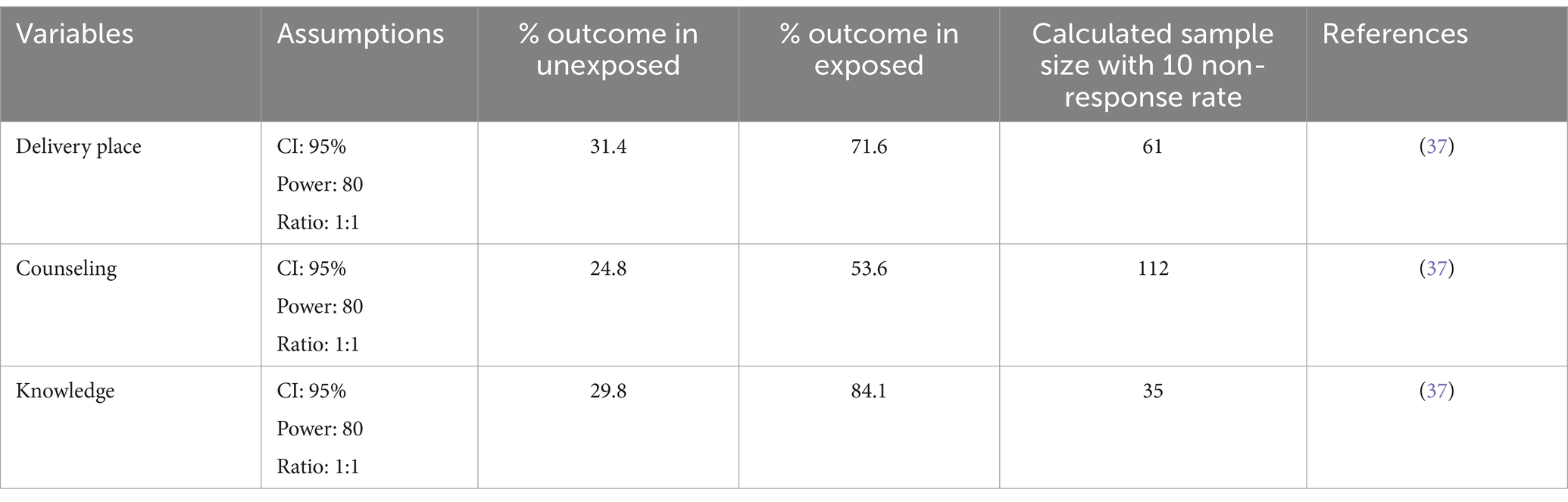
Table 1. Sample size determination for the study on the colostrum feeding practice and associated factors among mothers who come for Postnatal Care to Asella Referral and Teaching Hospital, Arsi Zone, South-East Ethiopia.
Therefore, we selected the higher result by comparing the result of two of the objectives and the final sample was 304.
Sampling procedure
To select the study participants, the quarterly report’s total number of mothers enrolled in the healthcare facility, 1,254 was determined. Once the K value had been calculated, respondents were selected by a systematic random sampling method. The first participant was randomly selected and further participants were recruited every four.
Data collection tools and methods
The questionnaires were developed by reviewing previous studies (1, 3, 8, 17, 26). Initially, the questionnaire was prepared in English, then translated into the local language, Afan Oromo, to facilitate data collection from the study participants. Finally, it was translated back into English by experts to ensure consistency. The tool comprised four sections: socio-demographic factors, knowledge-related factors, attitude-related factors, and practice-related factors. Data was collected by three BSc Nurses, using a structured face-to-face, interviewer-administered questionnaire and supervised by one MSc nurse.
Study variables and measurements
In this study, the outcome variable was colostrum feeding practice and the independent variables were socio-demographic characteristics, maternal health service utilization, knowledge of mothers about colostrum, and attitude of mothers toward colostrum. Colostrum is the breast milk women produce in the first few (3, 4) days after birth before the regular breast milk comes (17). Colostrum feeding practice is defined as the mothers who give colostrum (first thick and yellowish milk) to the newborn within the first 3 days of birth (26). Feeding colostrum was coded as “1” while avoiding colostrum feeding was coded as “0” for regression analysis.
Good knowledge among participants was defined as having responses equal to or greater than the mean value of the total knowledge-related questions, while those who scored below the mean were categorized as having poor knowledge (3). Similarly, a good attitude was determined by responses equal to or above the mean value for attitude-related questions, with responses below the mean coded as a poor attitude (3). Moreover, if the mother responded greater than or equal to the mean value to practice-related questions, it is coded as good practice, while if the mother responded less than the mean value, it is considered poor practice (3).
Data quality controls
To minimize bias, data collectors were recruited from outside the study area. The principal investigator provided 1 day of training to the data collectors and supervisors, covering the study’s objectives, components, participant recruitment, ethical considerations, and a general overview of the data collection procedure to ensure a common understanding. To enhance data quality, a pretest was conducted on 5% of the total sample outside the study setting prior to the actual data collection. Feedback from this pretest was incorporated into the survey. Every day, the supervisors rechecked the questionnaire’s completeness after data collection was completed.
Data processing and analysis procedure
Data were entered into Epi Info version 7.2.5.0 and exported to SPSS version 26 for analysis. Descriptive analysis results were presented in the form of tables and texts using frequencies and summary statistics such as standard deviation and percentage. A binary Logistic regression model was also used to identify factors associated with the practice of colostrum feeding practice. Then those variables with a p value of < 0.25 were entered into multivariable logistic regressions to control the effect of confounding variables. An adjusted odds ratio with a 95% Confidence Interval (C.I) was calculated to determine the strength of the association. The model goodness of fit was tested by the Hosmer-Lemeshow and Omnibus test. Accordingly in this study, Hosmer-lemshow and Omnibus test (p = 0.47 and p = 0.000) respectively. To check the presence of multicollinearity among independent variables variance inflation factors >10 and tolerance <0.1 were used. Finally, to declare statistical significance, a p-value of < 0.05 was considered.
Ethical considerations
To ensure ethical standards, necessary permissions were sought from Arsi University Asella Referral and Teaching Hospital, the Department of Public Health, as well as the administrative body of the hospital, to obtain cooperation for the study. The study, purpose, procedure, duration, possible risks, and benefits of participating in this study were clearly explained for each study participant using the local language (Afan Oromo). Verbal and informed consent was taken from each study participant before data collection and the right to withdraw was informed.
Results
Socio-demographic characteristics
In this study, a total of 301 study participants were surveyed, making a response rate of 99%.
The mean (±SD) age of study participants was 27.13 (±5.46) years. Of the total respondents, 189 (62.8%) aged from 25 to 34 years old and the majority of the respondents, 294 (97.7%) were married, 233 (77.4%) had formal education, and 159 (52.8%) of the respondents were Muslim religion followers. Of the total respondents, 208 (69.1%) of mothers were housewives, and 187 (62.1%) of mothers resided in rural areas (Table 2).
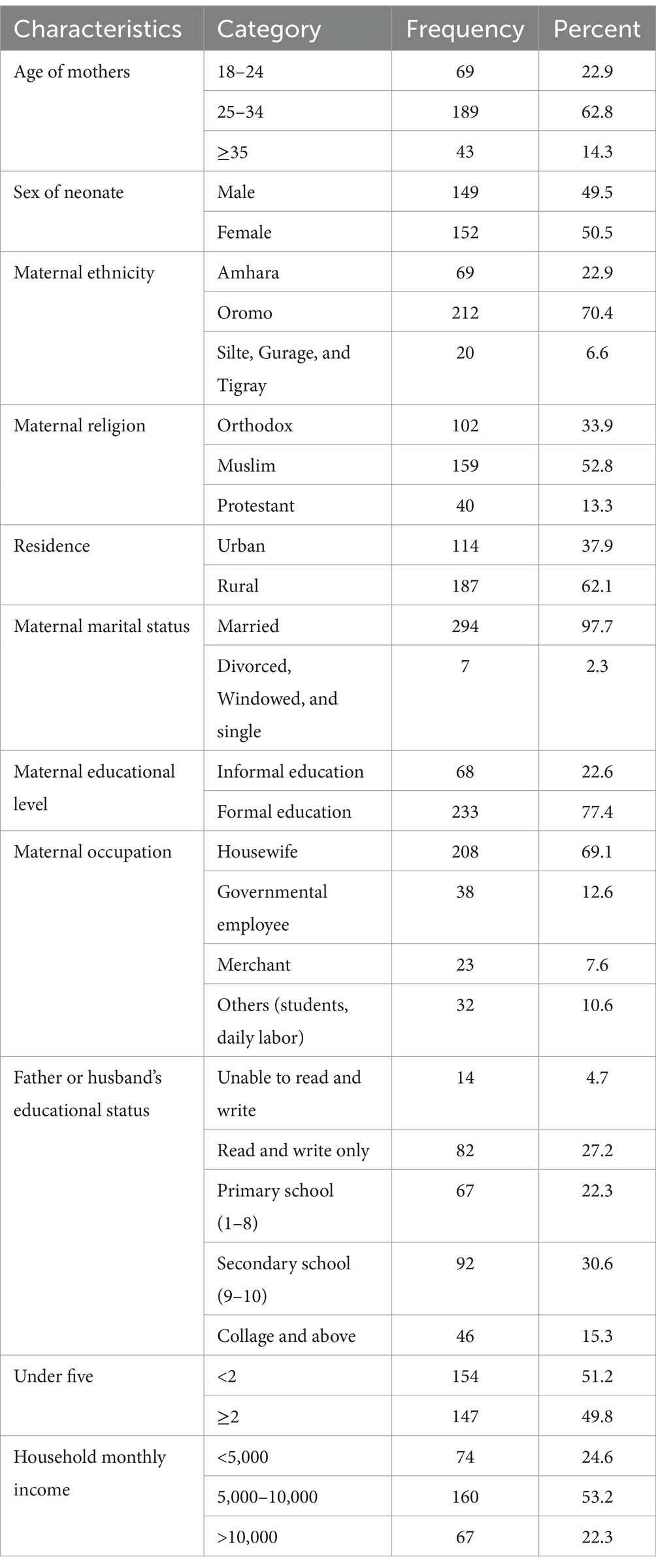
Table 2. Socio-demographic and economic-related characteristics of mothers who attended the PNC clinic at Asella Referral and Teaching Hospital, Southeast Ethiopia, 2024 (n = 301).
Obstetrics health service-related characteristics of mothers
This study showed that 283 (94%) of mothers, received antenatal care for their recent pregnancies. From these, 227 (80.2%) of these mothers attended ANC appointments four or more times, yet only 47 (16.6%) received health education regarding breastfeeding and colostrum. The majority of mothers chose to have deliveries at a health facility 294 (97.7%). Regarding the mode of delivery, 152 (50.5%) experienced vaginal delivery (Table 3).
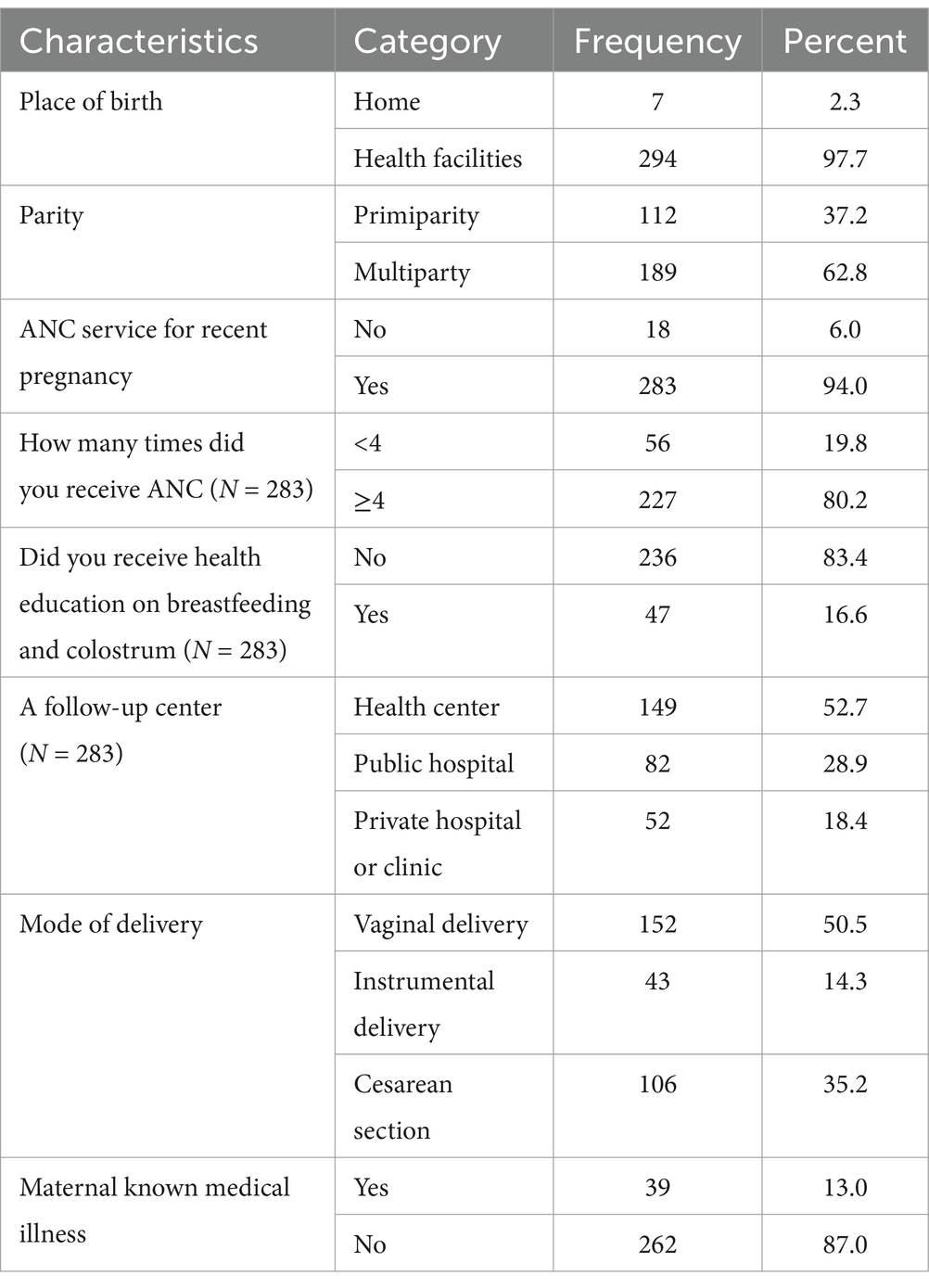
Table 3. Obstetric health services related to characteristics of mothers who attended PNC clinic at Asella referral and teaching hospital, Oromia regional state, Southeast Ethiopia, 2024 (n = 301).
Knowledge of colostrum feeding
Regarding knowledge about colostrum, 251 (83.4%) of mothers were generally aware of colostrum feeding. Additionally, 220 (73.1%) of the mothers recognized the color of colostrum. Of the total respondents, 195 (64.8%) of mothers were aware that colostrum milk serves as the first vaccine and 173 (57.5%) knew that initiating colostrum feeding immediately helps protect against maternal complications such as vaginal bleeding. In this study, the overall knowledge of mothers about colostrum feeding was 65.8% (95% CI, 60.46–71.19) (Table 4).
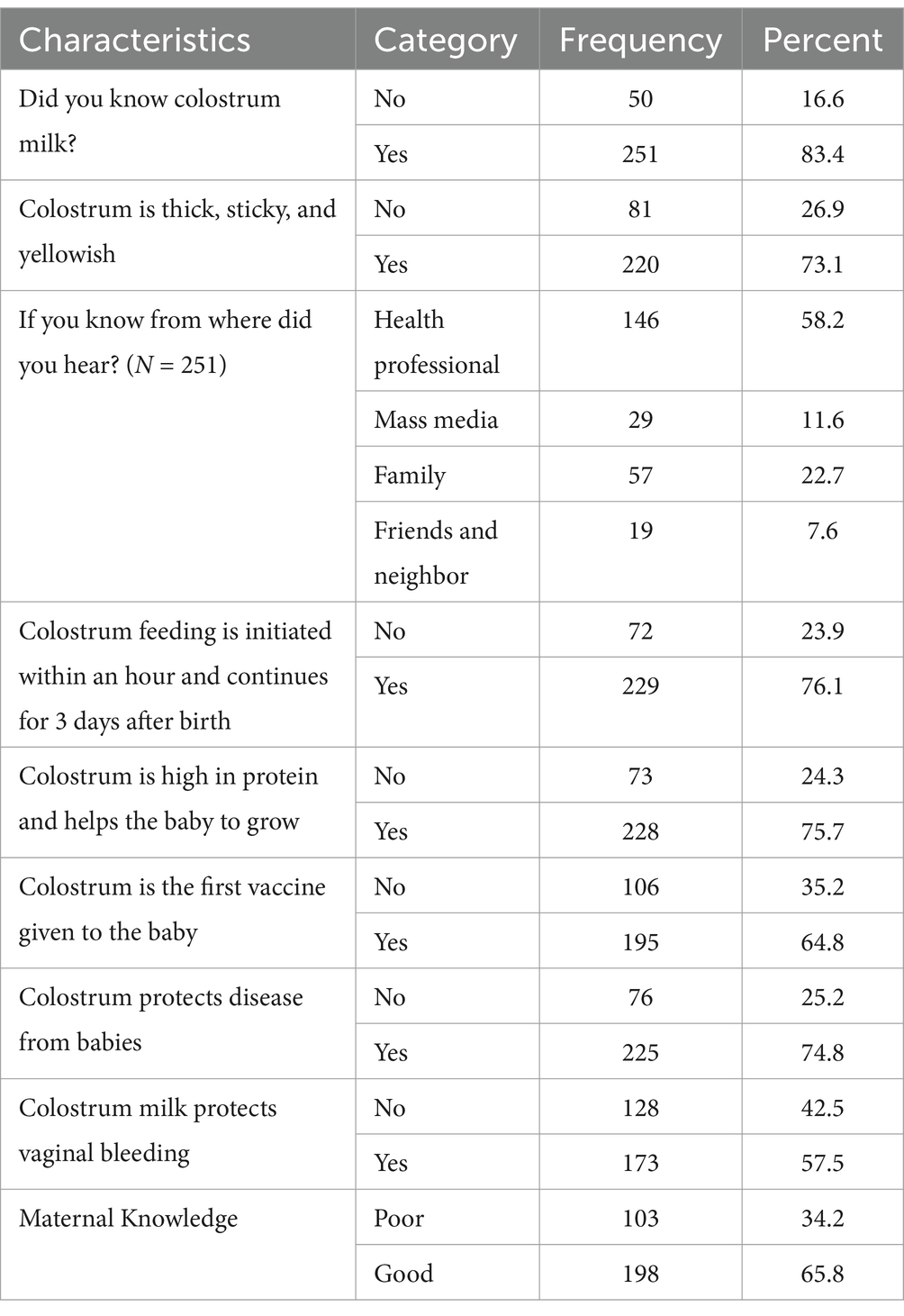
Table 4. Knowledge of colostrum feeding among mothers who attended PNC clinic at Asella referral and teaching hospital, Oromia regional state, southeast Ethiopia, 2024 (n = 301).
Attitude toward colostrum feeding
In this study, 181 (60.1%) of mothers agreed that colostrum is important for growth and mental development. About 70 (24.9%) of mothers believed that colostrum causes diarrhea and 69 (22.3%) thought that colostrum breast milk is dirty and looks like pus. The findings revealed that approximately 62.8% (95% CI: 57.36–68.23) of mothers had favorable attitudes toward colostrum feeding (Table 5).
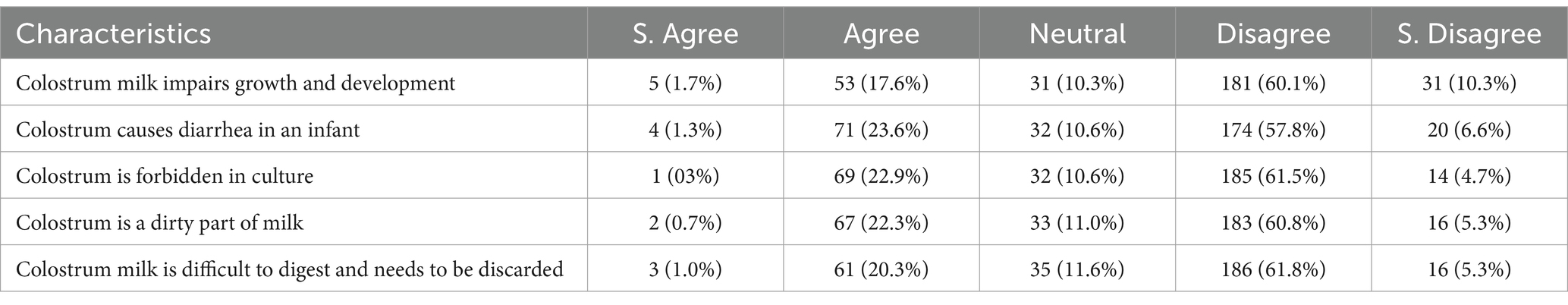
Table 5. Attitude toward colostrum feeding among mothers who attended PNC clinic at Asella referral and teaching hospital, Oromia regional state, Southeast Ethiopia, 2024 (n = 301).
The practice of colostrum feeding
The proportion of colostrum feeding practice among mothers who attend postnatal care was found to be 57.8% (95% CI: 52.2–63.35) as indicated in Figure 1.
Factors associated with colostrum feeding practice
The study employed both Bivariable and multivariable binary logistic regression analyses to identify the factors associated with colostrum feeding practice. In the bivariable analysis, factors with a p-value of less than 0.25 were maternal resident, the number under-five children, sex of neonate, ANC visiting, parity, place of birth, counseling on BF, and colostrum and maternal attitude. However, in the multivariable logistic regression analysis urban resident, health counseling on colostrum feeding, and good maternal attitude variables were found to be significantly associated with colostrum feeding at a p-value of < 0.05 (Table 6).
In multivariable logistic regression, the odds of practicing colostrum feeding were 4.05 times higher among mothers residing in urban areas compared to those living in rural areas (AOR = 4.05, 95% CI: 2.18–7.52). Mothers who received counseling on breastfeeding and colostrum had 4.3 times the odds of the practice of colostrum feeding compared to those who did not receive counseling (AOR = 4.31, 95% CI: 1.27–10.73). Those mothers with a favorable attitude toward colostrum milk had 6.6 times higher odds of colostrum feeding practice than mothers with an unfavorable attitude (AOR = 6.64, 95% CI: 3.61–12.22) (Table 6).

Table 6. Binary and multivariable logistic regression analysis of factors associated with colostrum feeding practice among mothers who attended the PNC clinic at Asella referral and teaching hospital, Oromia regional state, Southeast Ethiopia, 2024 (N = 301).
Discussion
This study examined colostrum feeding practices and associated factors among postnatal mothers at Asella Referral and Teaching Hospital. The prevalence of colostrum feeding in the study area was found to be 57.8%. This result aligns with findings from studies conducted in Debre Berhan town (56.2%) (27) and Ambo (56.5%) (26). However, the prevalence observed in this study is lower compared to findings from other locations, such as the three districts in Sindh province, Pakistan namely, Larkana, Qamber Shahdadkot, and Dadu (72.1%) (19), Pakistan’s Military Hospital Rawalpindi (86%) (7), Papua New Guinea (68.6%) (28), Kamrul, Assam in India (76%) (29), Bahir Dar city (83.3%) (30), Arba Minch Zuria (89.0%) (31), Mizan Tepi University Teaching Hospital, Bench Maji Zone, SNNPR (60.88%) (32), Gununo Health Center in the Wolaita Zone (83%) (1), Dubti town, Afar regional state (84.4%) (21), Motta town (79.8%) (24), Hula district of Sidama Region (96.1%) (33), and Samara-Logia city, Northeastern Ethiopia (88.0%) (34). This variation could be attributed to differences in maternal access to healthcare services and the sociocultural practices surrounding breastfeeding (Figure 3).
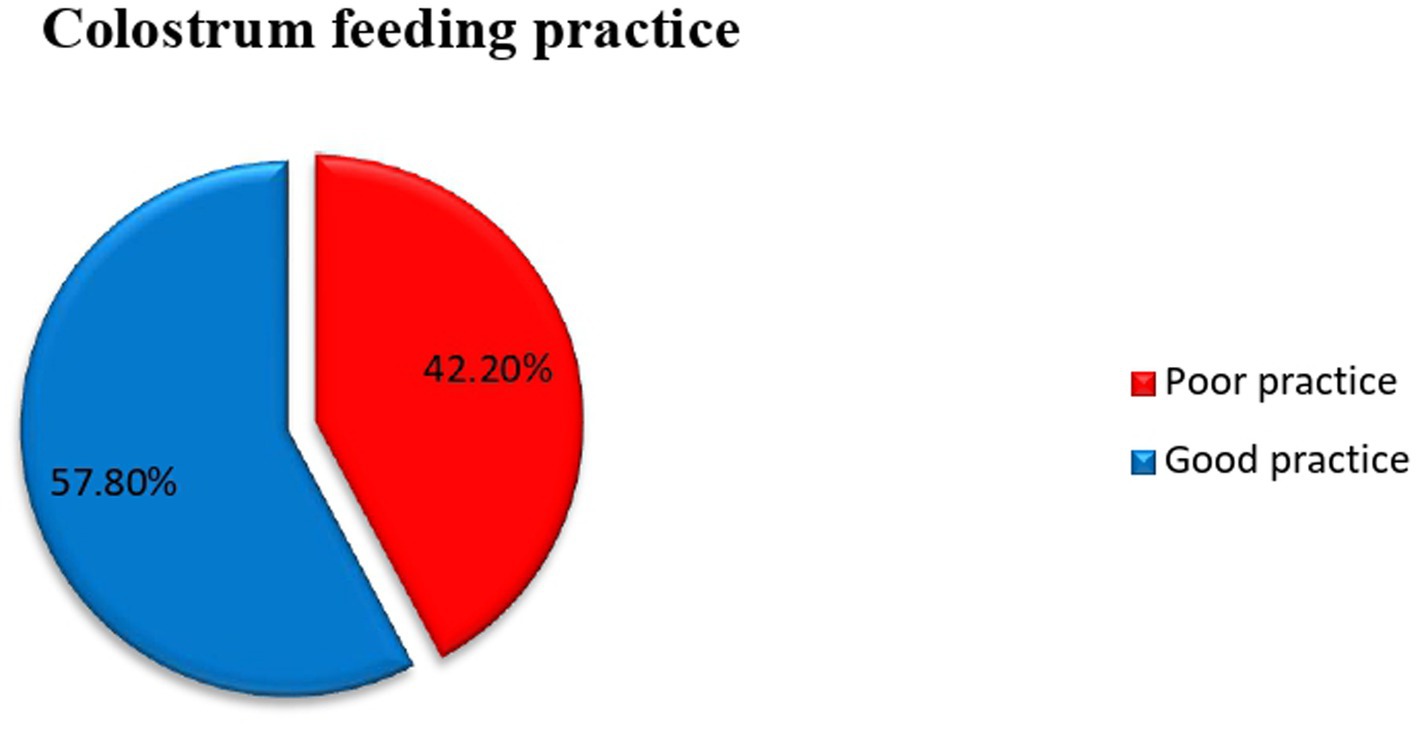
Figure 3. Prevalence of colostrum feeding practice among Mothers Who Come for Postnatal Care to Asella Referral and Teaching Hospital, Arsi Zone, South-East Ethiopia, 2024.
The findings of this study were higher than those of a study conducted in Egypt, which reported a colostrum feeding rate of 41.4% (35). This difference may be attributed to variations in the study area and socio-demographic factors. Additionally, cultural beliefs and practices related to breastfeeding, including colostrum feeding, can differ significantly across regions and countries. Cultural norms, traditions, and taboos around infant feeding practices can strongly influence maternal behaviors and attitudes toward colostrum feeding. For example, in some cultures, colostrum may be viewed as harmful or unnecessary, resulting in lower rates of colostrum feeding.
This study also identified several factors associated with maternal colostrum feeding practices, including participant residence, counseling on the timely initiation of breastfeeding during antenatal care, and maternal attitudes toward colostrum feeding. The findings indicated that mothers residing in urban areas were more likely to practice colostrum feeding compared to those living in rural areas. This result is consistent with studies conducted in Kombolcha, South Wollo Zone of Ethiopia (29), governmental health facilities in Dire Dawa administrative city (8), and Kamrup, Assam in India, which also showed that urban mothers were more likely to provide colostrum than their rural counterparts (36). The possible explanation for this finding is the difference in access to healthcare services and education between urban and rural areas. Urban areas generally have better access to healthcare facilities, including hospitals and clinics, where mothers may receive more comprehensive antenatal care, including counseling on the importance of colostrum feeding. In contrast, rural areas may experience challenges such as limited access to healthcare services, lower levels of education, and traditional beliefs that may discourage colostrum feeding. These factors likely contribute to the observed disparity in colostrum feeding practices between urban and rural mothers in the study.
The finding of this study indicated that mothers who received health education counseling during antenatal care follow-ups regarding colostrum feeding were more likely to practice colostrum feeding compared to those who did not receive counseling. This finding is consistent with the study conducted in Wolaita Sodo (17). This could be because health education counseling during antenatal care (ANC) follow-ups provides mothers with information about the importance and benefits of colostrum feeding. This counseling may cover topics such as the nutritional value of colostrum, its role in protecting newborns from infections, and its contribution to early bonding between mother and child. When mothers receive this education, they are more likely to understand the significance of colostrum feeding and feel empowered to initiate and continue the practice after childbirth.
Mothers with a favorable attitude toward colostrum milk were more likely to have higher odds of colostrum feeding practice compared to mothers with an unfavorable attitude. The result is consistent with the study conducted in Addis Ababa (9). This might be due to a positive attitude toward colostrum lead to a stronger intention to practice colostrum feeding. Essentially, when mothers have a favorable attitude toward colostrum, they are more likely to perceive it as valuable and important, which translates into a higher motivation to engage in the behavior of colostrum feeding.
Conclusion and recommendation
Conclusion
The study area had a low rate of colostrum feeding practice (57.8%) when compared with WHO recommendations. Additionally, this study identified factors associated with maternal colostrum feeding practice level such as participant residence, counseling on timely initiation of breastfeeding during antenatal care, and maternal attitude toward colostrum feeding. Therefore, the following recommendation was forwarded to different stakeholders;
Recommendations
Health care professionals
• Should conduct door-to-door campaigns in rural areas to educate expectant mothers about the importance of colostrum feeding.
• Provide Health education dissemination to all postnatal mothers on the importance of colostrum feeding to increase mothers’ attitude toward breast feeding.
• Should incorporate counseling on timely initiation of breastfeeding, including colostrum feeding, into their antenatal care consultations.
Community Leaders and Volunteers:
• Should work in collaboration with health care professionals and facilitate mobilization of rural community to enhance Health education on colostrum feeding to improve mothers Attitude.
Future researchers
• Consider conducting longitudinal studies to track maternal colostrum feeding practices over time. Longitudinal data can provide insights into changes in feeding behaviors and attitudes throughout pregnancy, childbirth, and the postpartum period, allowing for a more comprehensive understanding of the factors influencing colostrum feeding.
Limitations of the study
The study is only conducted at Asella Referral and Teaching Hospital, which may limit the generalizability of the findings to other healthcare settings with different patient populations and practices. Additionally, the study is cross-sectional design which does not allow for the establishment of causal relationships. Moreover, there was recall bias due to study participants being unable to remember what happened in the past.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Ethical permission was obtained from the Arsi University, College of Health Sciences. A formal letter of permission and support was provided to all hospitals where the study was conducted. Informed written consent was obtained from all study participants before data collection. For those who were unable to give written consent, we obtained fingerprints.
Author contributions
GH: Conceptualization, Data curation, Investigation, Methodology, Software, Writing – original draft. GA: Conceptualization, Data curation, Investigation, Methodology, Writing – original draft. AE: Formal analysis, Supervision, Validation, Writing – review & editing. AbH: Writing – review & editing, Supervision, Validation, Software. AhH: Formal analysis, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to express special thanks to Arsi University College of Health Sciences, School of Graduate Studies, for enabling us to conduct this study. Furthermore, we would like to thank the study’s participants, data collectors, and supervisors.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer MA declared a shared affiliation, with no collaboration, with one of the authors, AH to the handling editor at the time of the review.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2024.1487179/full#supplementary-material
References
1. Yeshambel Wassie, A, Atnafu Gebeyehu, N, and Abebe, GK. Knowledge, attitude, and associated factors towards colostrum feeding among antenatal care attendant mothers in Gununo health Centre, Wolaita zone, Ethiopia 2019: cross-sectional study. Int J Pediatr. (2020) 2020:1–10. doi: 10.1155/2020/3453502
2. Demographic, E. Health survey (EDHS) 2016: Key indicators report, central statistical agency Addis Ababa, Ethiopia. Rockville, Maryland: The DHS Program ICF (2016).
3. Zewde, GT. Assessment of knowledge, attitude, and practices of colostrum feeding among postnatal mothers in Harar town governmental hospital Harar, Ethiopia 2019. J Pediatr Res Rev Rep. (2020) 2:2–6. doi: 10.47363/JPRRR/2020(2)104
4. Liben, ML. Colostrum: the Golden Milk for Infants’ health. Glob J Intellect Dev Disabil. (2017) 1:59–60. doi: 10.19080/GJIDD.2017.01.555566
5. Legesse, M, Demena, M, Mesfin, F, and Haile, D. Factors associated with colostrum avoidance among mothers of children aged less than 24 months in Raya kobo district, North-Eastern Ethiopia: community based cross-sectional study. J Trop Pediatr. (2015) 61:357–63. doi: 10.1093/tropej/fmv039
6. Liben, ML, Abuhay, T, and Haile, Y. The role of colostrum feeding on the nutritional status of preschool children in Afambo District, Northeast Ethiopia: a descriptive cross-sectional study. Eur J Clin Biomed Sci. (2016) 2:87–91. doi: 10.11648/j.ejcbs.20160206.15
7. Aisha, R, Batool, F, and Sultana, S. Knowledge, attitude and practices about colostrum feeding among pregnant women in military hospital Rawalpindi of Pakistan. Open J Nurs. (2016) 6:309–13. doi: 10.4236/ojn.2016.64032
8. Natnael, D. Practice of colostrum feeding and associated factors among mothers who attended child immunization Clinic in Governmental Health Facilities of Dire Dawa Administrative City, Eastern Ethiopia 2021 (2021).
9. Teketel, A. Assessment of colostrum feeding practice and associated factors among postnatal mothers in selected health facilities in Addis Abeba, Ethiopia. (2020).
10. Reid, G, Kumar, H, Khan, A, Rautava, S, Tobin, J, and Salminen, S. The case in favor of probiotics before, during and after pregnancy: insights from the first 1,500 days. Benef Microbes. (2016) 7:353–62. doi: 10.3920/BM2015.0140
11. Amaje, E, Gebremeskel, F, Tufa, G, Gelchu, M, and Wayessa, ZJ. Colostrum avoidance practices and its associated factors among mothers of children aged less than 12 months in Jinka town, South Ethiopia, 2020. A community-based cross-sectional study. Health Serv Res Manag Epidemiol. (2022) 9:23333928221106056. doi: 10.1177/23333928221106056
12. WHO. Neonatal mortality. Available at: https://www.who.int/gho/child_health/mortality/neonatal/en/ (Accessed September 20, 2017).
13. Akter, T, Dawson, A, and Sibbritt, D. What impact do essential newborn care practices have on neonatal mortality in low and lower-middle-income countries? Evidence from Bangladesh. J Perinatol. (2016) 36:225–30. doi: 10.1038/jp.2015.181
14. Menchetti, L, Traina, G, Tomasello, G, Casagrande Proietti, P, Leonardi, L, Barbato, O, et al. Potential benefits of colostrum in gastrointestinal diseases. Front Biosci. (2016) 8:331–51. doi: 10.2741/s467
15. Liben, ML, and Yesuf, EM. Determinants of early initiation of breastfeeding in Amibara district, northeastern Ethiopia: a community-based cross-sectional study. Int Breastfeed J. (2016) 11:1–7. doi: 10.1186/s13006-016-0067-8
16. Yirgu, R, Molla, M, and Sibley, L. Determinants of neonatal mortality in rural northern Ethiopia: a population-based nested case-control study. PLoS One. (2017) 12:e0172875. doi: 10.1371/journal.pone.0172875
17. Gargamo, DB. Colostrum feeding practices and associated factors among mothers having children less than 12 months of age in Wolaita Sodo City, Wolaita, Ethiopia 2019. Biomed Sci. (2020) 6:17. doi: 10.11648/j.bs.20200602.11
18. Bhandari, S, Thorne-Lyman, AL, Shrestha, B, Neupane, S, Nonyane, BAS, Manohar, S, et al. Determinants of infant breastfeeding practices in Nepal: a national study. Int Breastfeed J. (2019) 14:1–17. doi: 10.1186/s13006-019-0208-y
19. Sohail, J, and Khaliq, A. Knowledge, attitude and practice of mothers regarding colostrum feeding to newborns in rural Pakistan: a cross-sectional study. Khyber Med Univ J. (2017) 9:192–6.
20. Munos, MK, Mullany, LC, Maïga, A, Baya, B, and Bryce, J. Coverage and determinants of newborn feeding practices in rural Burkina Faso. J Perinatol. (2014) 34:369–74. doi: 10.1038/jp.2014.13
21. Liben, ML, Gemechu, YB, Adugnew, M, Asrade, A, Adamie, B, Gebremedin, E, et al. Factors associated with exclusive breastfeeding practices among mothers in Dubti town, afar regional state, Northeast Ethiopia: a community-based cross-sectional study. Int Breastfeed J. (2016) 11:1–6. doi: 10.1186/s13006-016-0064-y
22. Abie, BM, and Goshu, YA. Early initiation of breastfeeding and colostrum feeding among mothers of children aged less than 24 months in Debre Tabor, Northwest Ethiopia: a cross-sectional study. BMC Res Notes. (2019) 12:65. doi: 10.1186/s13104-019-4094-6
23. Weldesamuel, GT, Atalay, HT, Zemichael, TM, Gebre, HG, Abraha, DG, Amare, AK, et al. Colostrum avoidance and associated factors among mothers having children less than 2 years of age in Aksum town, Tigray, Ethiopia: a cross-sectional study 2017. BMC Res Notes. (2018) 11:1–7. doi: 10.1186/s13104-018-3712-z
24. Tewabe, T. Timely initiation of breastfeeding and associated factors among mothers in Motta town, east Gojjam zone, Amhara regional state, Ethiopia, 2015: a cross-sectional study. BMC Pregnancy Childbirth. (2016) 16:1–7. doi: 10.1186/s12884-016-1108-4
25. Paithran, K, Aalinkeel, A, and Payora, R. Infant feeding practices in a well-baby clinic of a tertiary hospital in North Kerala. J Med Sci Clin Res. (2016) 4:10886–92. doi: 10.18535/jmscr/v4i6.34
26. Gela, JD, Minase, D, Teferi, E, and Tesfaye, T. Knowledge, attitude, practices and associated factors towards colostrum feeding among mothers of infants in Ambo District of west Shewa zone, Oromiya region, Ethiopia. (2020).
27. Tadese, M, Kebede, W, and Mulu, G. Assessment of knowledge, attitude, and practice of colostrum feeding among lactating women in Northeast Ethiopia. Clin Case Rep Int. (2022) 6:100.
28. Kuzma, J. Knowledge, attitude and practice related to infant feeding among women in rural Papua New Guinea: a descriptive, mixed method study. Int Breastfeed J. (2013) 8:1–5. doi: 10.1186/1746-4358-8-16
29. Kakati, R, Rahman, SJ, Borah, M, and Borah, H. Colostrum feeding practices and its determinants among urban and rural mothers in Kamrup, Assam, India. Int J Res Med Sci. (2016) 4:4567–72. doi: 10.18203/2320-6012.ijrms20163331
30. Seid, AM, Yesuf, ME, and Koye, DN. Prevalence of exclusive breastfeeding practices and associated factors among mothers in Bahir Dar City, Northwest Ethiopia: a community-based cross-sectional study. Int Breastfeed J. (2013) 8:1–8. doi: 10.1186/1746-4358-8-14
31. Tamiru, D, and Mohammed, S. Maternal knowledge of optimal breastfeeding practices and associated factors in rural communities of Arba Minch Zuria. Int J Nutr Food Sci. (2013) 2:122–9. doi: 10.11648/j.ijnfs.20130203.15
32. Shewasinad, S, Manjura, M, Bolesh, A, Sisay, D, and Negash, S. Assessment of knowledge, attitude, and practice towards colostrum feeding among antenatal care attendant pregnant mothers in Mizan Tepi university teaching hospital, bench Maji zone, SNNPR, south West Ethiopia, 2016/2017 GC. J Preg Child Health. (2017) 4:1–8. doi: 10.4172/2376-127X.1000348
33. Hoche, S, Meshesha, B, and Wakgari, N. Sub-optimal breastfeeding and its associated factors in rural communities of Hula District, southern Ethiopia: a cross-sectional study. Ethiop J Health Sci. (2018) 28:49–62. doi: 10.4314/ejhs.v28i1.7
34. Beyene, AM, Liben, ML, and Arora, A. Factors associated with the early termination of exclusive breastfeeding among mother-infant dyads in Samara-logia, Northeastern Ethiopia. BMC Pediatrics. (2019) 19:428. doi: 10.1186/s12887-019-1803-1
35. Abdelmenam, NA, Youness, EM, and Arief, AF. Knowledge and practices among immediate post-partum women about colostrum at Women's health hospital. Assiut Sci Nurs J. (2018) 6:92–100. doi: 10.21608/asnj.2018.58968
36. Gebreyesus, H, Girma, E, and Cherie, N. Colostrum avoidance and associated factors among mothers of children aged less than 12 months in Kombolcha town, south Wollo zone. Ethiopia Med Res Chronicles. (2017) 4:545–59.
Keywords: colostrum feeding, practice, post-Natal, Asella, Southeast Ethiopia
Citation: Haji G, Agero G, Eshete A, Hasan A and Hiko A (2025) Colostrum feeding practice and associated factors among mothers who come for postnatal care to Asella referral and teaching hospital, Arsi Zone, South-East Ethiopia. Front. Med. 11:1487179. doi: 10.3389/fmed.2024.1487179
Edited by:
Alessandro Iellamo, FHI 360, United StatesReviewed by:
Hemant Khuntia, Siksha O Anusandhan University, IndiaMohammed Ahmed, Haramaya University, Ethiopia
Lalitchandra Sorathiya, Kamdhenu University, India
Copyright © 2025 Haji, Agero, Eshete, Hasan and Hiko. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gisha Haji, Z2lzaGhhamlAZ21haWwuY29t
 Gisha Haji1*
Gisha Haji1* Ahmed Hiko
Ahmed Hiko