- 1School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran
- 2Endocrinology and Metabolism Research Center, Hormozgan University of Medical Sciences, Bandar Abbas, Iran
- 3School of Medicine, Isfahan University of Medical Sciences, Isfahan, Iran
- 4Student Research Committee, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
- 5Faculty of Medicine, Georgian National University SEU, Tbilisi, Georgia
- 6Student Research Committee, Tabriz University of Medical Sciences, Tabriz, Iran
- 7Student Research Committee, School of Medicine, Zanjan University of Medical Sciences, Zanjan, Iran
- 8Student Research Committee, School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Background: Marital status is among the factors influencing type 2 diabetes mellitus (T2DM). However, the precise relationship remains incompletely understood. This meta-analysis aims to evaluate the association between marital status and the incidence of T2DM.
Methods: A review and meta-analysis of observational studies were conducted to investigate the relationship between marital status and diabetes incidence. We searched three databases, including PubMed, Google Scholar, and Scopus, for relevant studies published up to August 16th, 2023. In our initial search, we identified a total of 358 articles. After a demanding screening process involving evaluating titles, abstracts, and full-text content, we ultimately included six studies for our meta-analysis.
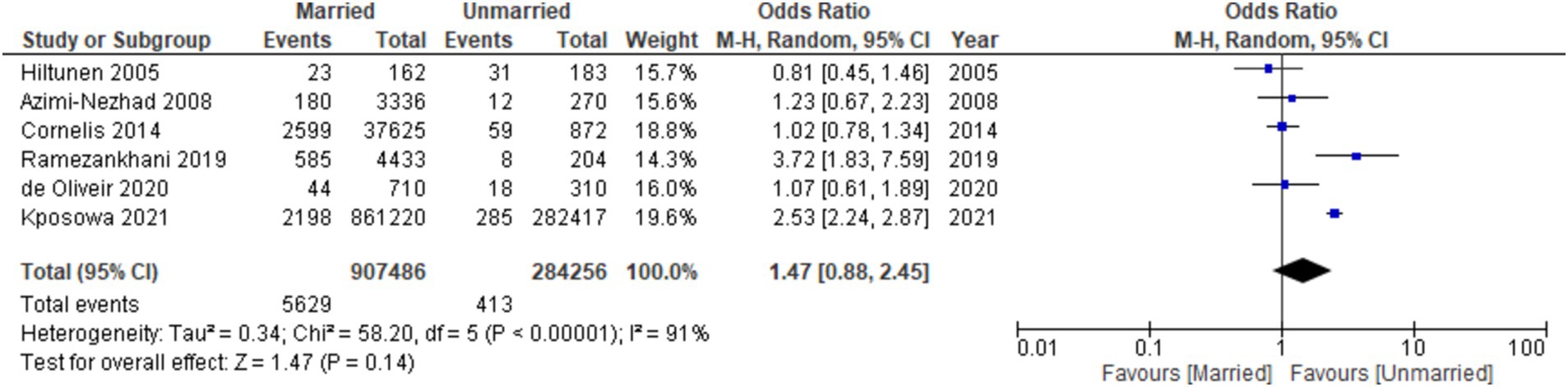
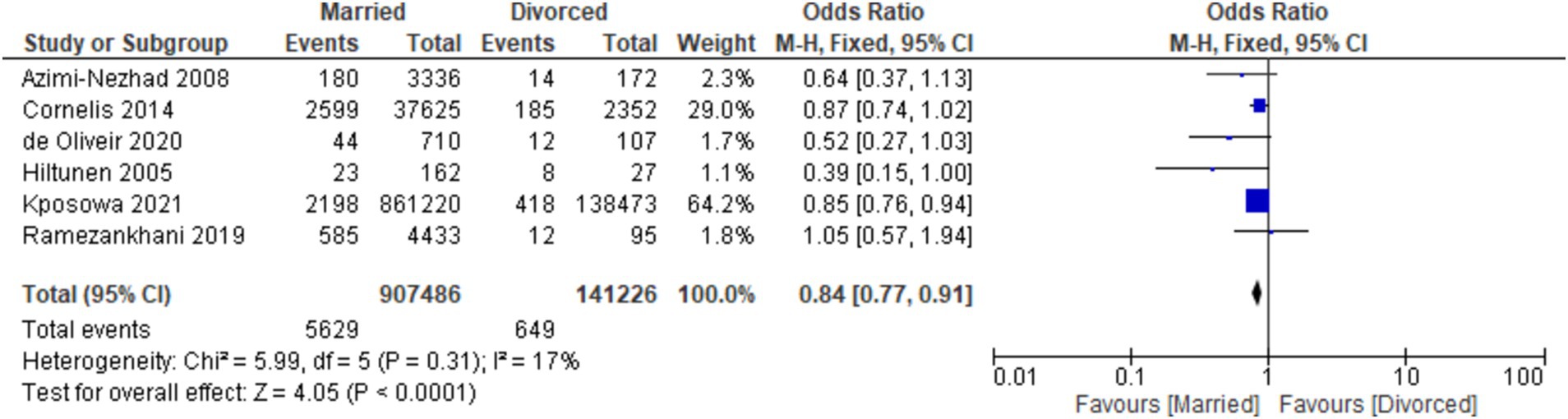
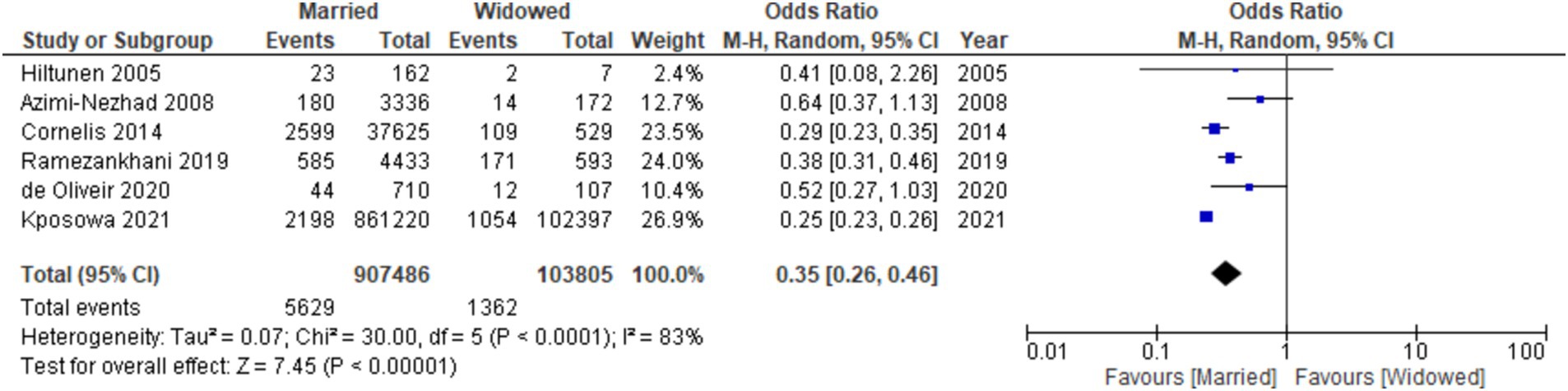
Result: Comprising a total of 1,440,904 participants, our study found that in comparison to married individuals, unmarried participants exhibited a higher likelihood of developing diabetes [odds ratio (OR): 1.47, 95% confidence interval (CI): 0.88–2.45, I2: 91%, p-value = 0.14]. Divorced participants had a reduced likelihood of developing diabetes compared to married participants (OR: 0.84, 95% CI: 0.77–0.91, I2: 17%, p < 0.001). Similarly, widowed participants showed a lower risk of developing diabetes compared to divorced participants (OR: 0.35, 95% CI: 0.26–0.46, I2: 83%, p < 0.00001).
Conclusion: This study provides strong evidence of links between marital status and type 2 diabetes risk. Unmarried individuals are more susceptible to T2DM, divorced individuals have a lower risk, and widowed individuals exhibit reduced T2DM risk. Further research should investigate underlying mechanisms and confounding factors.
Introduction
One of the world’s most prevalent chronic diseases is diabetes mellitus (DM), which ranks among the top 10 causes of mortality in the USA (1). Based on the World Health Organization (WHO) definition, DM is characterized by enduring metabolic dysfunction, leading to elevated blood glucose levels and adverse impacts on various bodily organs such as the cardiovascular, eyes, kidneys, and nervous systems. Most patients diagnosed with diabetes mellitus present as type 2 diabetes mellitus (T2DM). This condition is developed by insufficient insulin secretion from the pancreatic cells, tissue insensitivity to insulin, and limited compensatory insulin release (2–4). The increasing prevalence of T2DM can be attributed to lifestyle changes and overall health status improvements. Studies showed that nearly 300 million individuals could be affected by this condition by 2025 (5).
Moreover, it has been proved that diabetes was responsible for nearly 4 million fatalities among individuals aged 20 to 79 in 2019, accounting for roughly 11% of the total global mortality. Furthermore, more than 46% or about 2 million of these deaths occurred in individuals under 60 (6). Additionally, T2DM has been definitively linked to heightened risks of cardiovascular disease (CVD) (7), renal dysfunction (8), and increased mortality rates resulting from infections (9), as well as an elevated susceptibility to certain cancers, including pancreatic, hepatic, renal, thyroid, breast, and uterine corpus cancers (10).
One of the most important psychological factors influencing many aspects of a person’s health state is their marital relationship and its quality. The word “marital relationship” refers to a system for evaluating the overall marriage quality using positive and negative traits (11). Numerous studies have established that marital status significantly influences health outcomes, including the development and progression of chronic diseases such as cancer (12, 13), hypertension (14), and cardiovascular diseases (15). The relationship between marital status with a particular spotlight on T2DM has been the main point of multiple investigations (16–20). Specific studies have illuminated constructive consequences concomitant with marital status (21, 22). Notably, research among males has spotlighted the correlation between suboptimal marital quality, solitary marital status, and enhanced susceptibility to T2DM, especially among widowers (16). Furthermore, marital status has been identified as an independent risk factor for T2DM within the male demographic. Conversely, widowhood has been associated with a decreased T2DM risk in the female population (23). Another study showed that spousal participation is very important in improving teamwork in diabetes management and leads to better patient blood glucose control (24).
Consequently, due to heterogeneity and disagreement among the results of earlier studies, the effect of marital status on any component of T2DM and associated health effects continues to be a challenging issue despite the vast number of studies conducted. To the best of our knowledge, this study is the first to examine the relationship between T2DM and each marital status, including married, never married, widowed, and divorced.
Methods
Protocol and registration
This study was conducted in strict accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, ensuring methodological rigor and transparency. The study protocol has been meticulously developed and registered with the Open Science Framework (OSF), available at https://osf.io/a86vp
Search strategy
This meta-analysis searched three international databases: PubMed, Scopus, and Google Scholar. The search was performed in these databases from the beginning to August 16th, 2023, without any limitations or filters. The search terms consisted of the terms “diabetes OR diabetes mellitus” AND “marital status OR marital OR married OR marriage OR spouse OR widow OR widowed divorced” and MeSH terms (for PubMed). Supplementary Table S1 contains information on the search queries and the number of records in each database.
Screening and inclusion and exclusion criteria
We employed EndNote software to conduct the initial screening of records sourced from multiple databases. To ensure data integrity, duplicate database entries were eliminated utilizing the “Find Duplicates” function in EndNote. Subsequently, studies unrelated to marital status and those lacking diabetic populations were excluded through a meticulous screening of titles and abstracts. The full texts of the studies identified in the prior phase underwent a comprehensive evaluation to determine the final set of studies meeting the pre-defined inclusion and exclusion criteria for incorporation into this review.
We included observational studies (cross-sectional, cohort, case reports, and case series) that met the following inclusion criteria: observational studies on the correlation between marital status and the susceptibility to T2DM. The exclusion criteria encompassed review papers, editorials, comments, in vivo and in vitro investigations, and randomized clinical trial studies. In addition, several pertinent research were identified by manually examining the references cited in the articles from the original search.
Quality assessment
The Newcastle–Ottawa Scale (NOS) for non-randomized studies was used to assess the risk of bias in included studies (25). NOS evaluates studies according to pre-specified items, including selection, comparability, and exposure. Studies with a total NOS ≥8 are considered high quality.
Study selection and data extraction
After removing duplicate entries, two reviewers (MAK and SH) independently examined each title and abstract. Disagreements were resolved by utilizing a third reviewer or achieving a consensus (SB). The studies that met the inclusion criteria were obtained in their entirety and underwent an independent analysis by two authors (MAK and ElO). When the reviewers could not reach a consensus, a third author (RY) was consulted. Studies that did not meet the specified criteria for inclusion were finally excluded.
Two reviewers (MAK and ElO) independently extracted the following data from the included papers using a pre-existing standardized template: author and publication year, nation, study design, follow-up period, population and gender, age, and marital status. In instances of disagreement between reviewers, a third author (RY) was consulted.
Statistical analysis
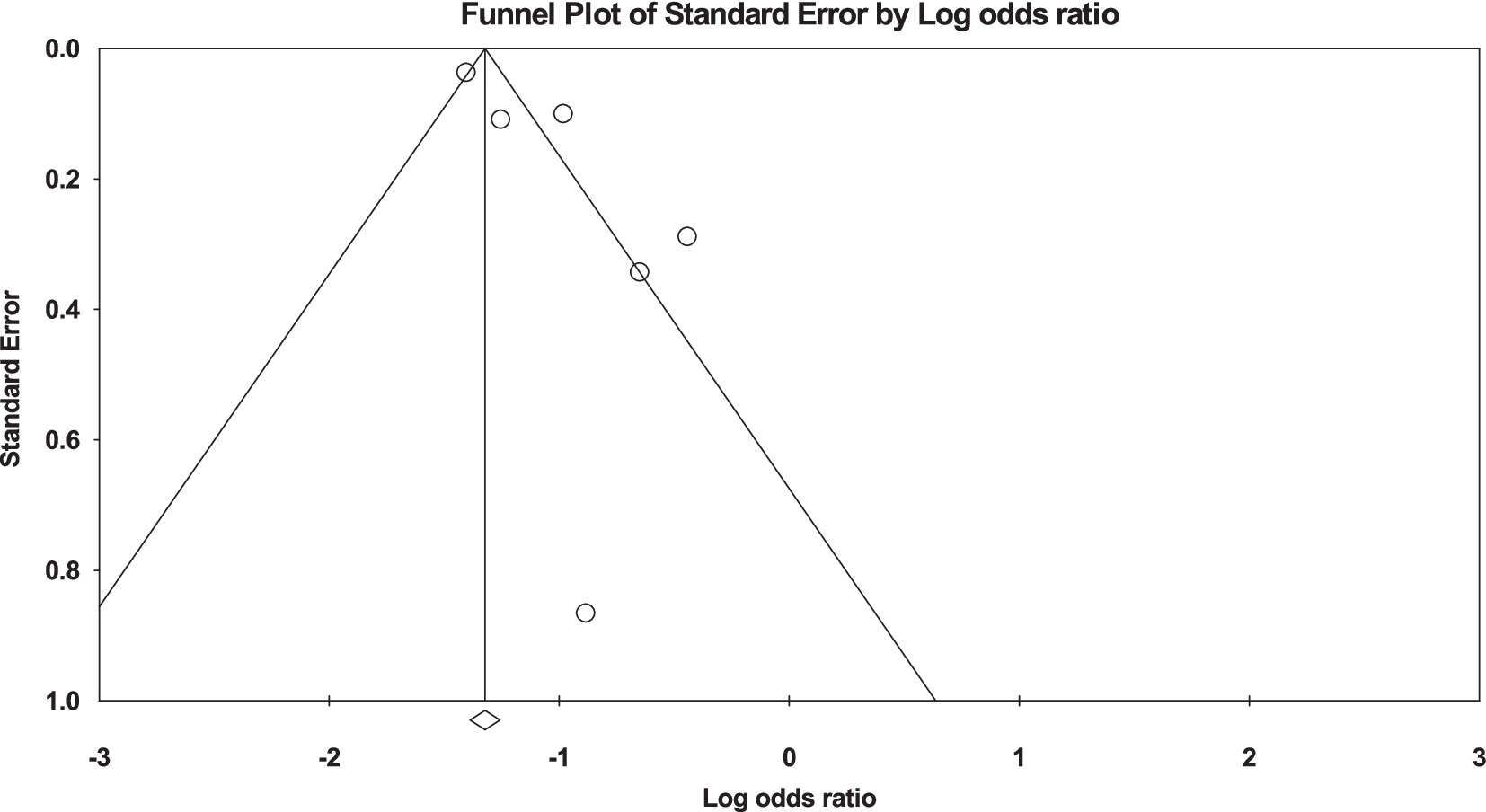
We employed the STATA 13.1 software, developed by StataCorp LP in College Station, TX, United States, to conduct our data analysis. The findings were reported as combined odds ratios (ORs) with a 95% confidence interval (CIs) and shown in a forest plot. In order to measure the differences between the studies that met the criteria, we employed the I2 statistic (26) and applied the random effects model when we found substantial variation (I2 is greater than 50%) (27). Following a thorough examination of the symmetry of the funnel plot and Egger’s regression analysis, we explored the possibility of publication bias (28).
Results
Study selection
A total of 489 studies were discovered for this analysis by conducting a primary literature search in Scopus, PubMed, and Google Scholar. Three hundred fifty-eight studies remained after removing the duplicates. Out of the total, 312 cases were deemed irrelevant to the study’s objective and were consequently removed through title/abstract screening. Afterward, a total of 46 records that could potentially be relevant were carefully examined in a full-text review. Out of them, 40 cases were also excluded due to the presence of irrelevant data. The selection and screening process for our study, encompassing identification, eligibility assessment, and final inclusion of studies, is comprehensively depicted in Figure 1.
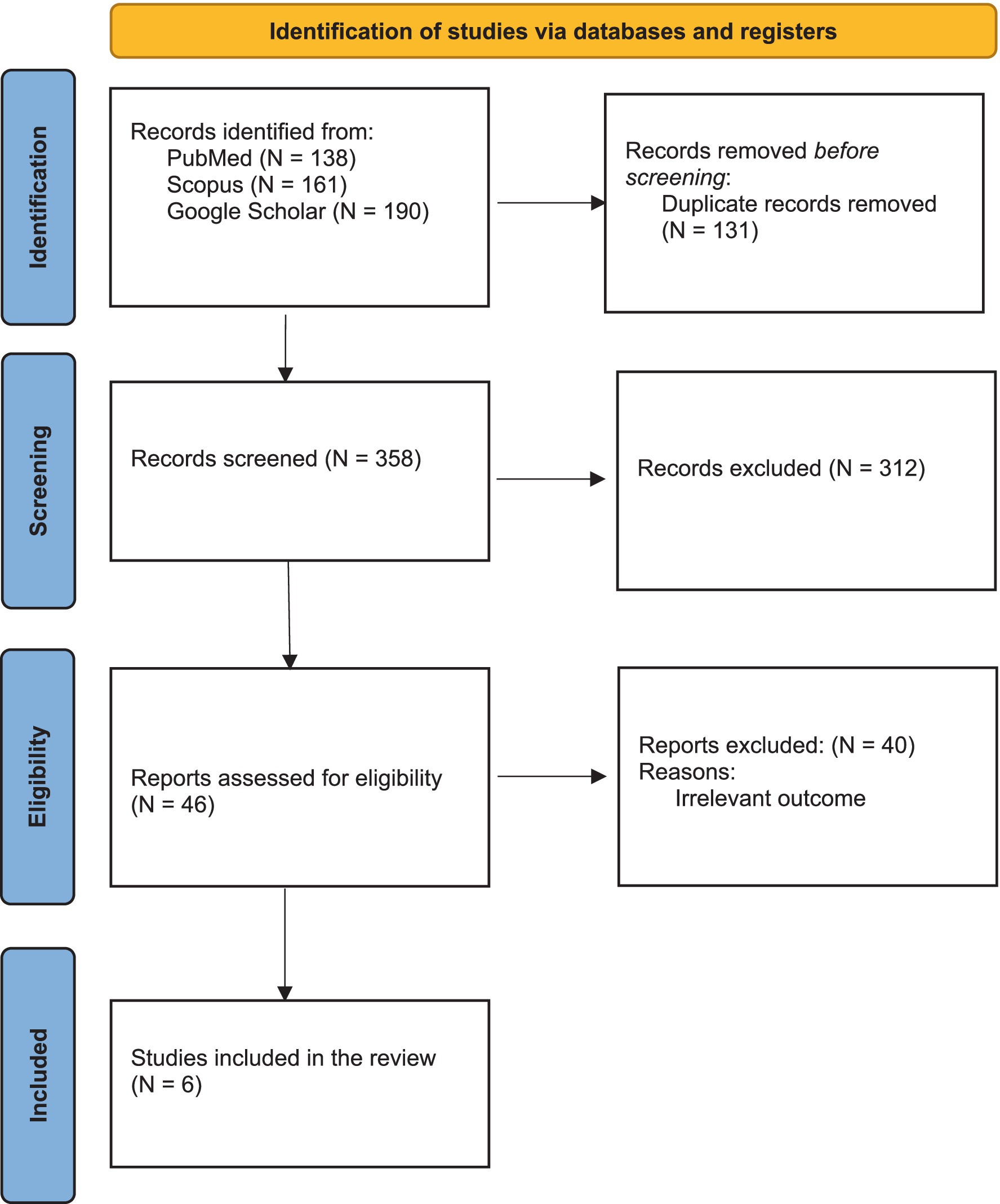
Figure 1. PRISMA flow diagram outlining the systematic review process. The figure illustrates the identification, screening, eligibility, and inclusion stages of the systematic review. A total of 489 records were initially identified from three databases: PubMed (n = 138), Scopus (n = 161), and Google Scholar (n = 190). After removing duplicates (n = 131), 358 unique records were screened based on titles and abstracts, excluding 312 irrelevant studies. Full-text assessments were conducted on 46 reports, with 40 excluded due to irrelevant outcomes. Ultimately, six studies meeting the inclusion criteria were selected for the final review and meta-analysis.
Baseline characteristics
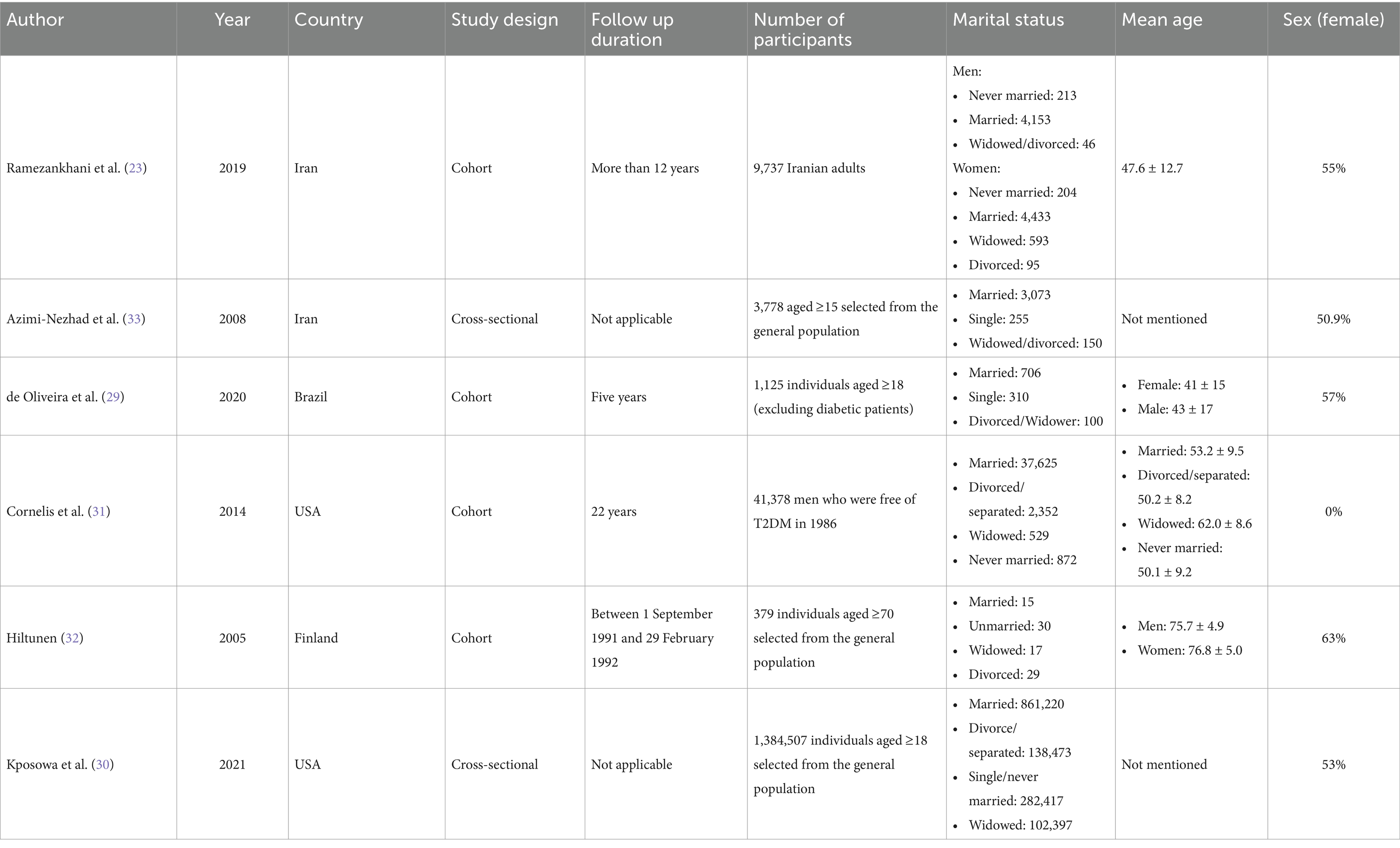
Finally, six articles with a total population of 1,440,904 were reviewed. Five of these six observational were cohort research (23, 29–32), and one was cross-sectional (33). These examinations were performed in Iran (23, 33), Brazil (29), the USA (30, 31), and Finland (32). The average age of those involved in these studies varied from 41 to 77 years. The follow-up duration of cohort studies ranged from 1 to 22 years. The years of investigation were 2002 through 2023. In each of the six incorporated studies, all reported the prevalence of marriage among individuals diagnosed with diabetes (23, 29–33), two out of the six studies addressed the status of being unmarried in diabetic patients (29, 32), while five out of the six studies examined the prevalence among widowed or divorced individuals within the diabetic population (23, 30–33). Additionally, four of the six studies investigated the occurrence of diabetes among individuals categorized as single or never married (23, 30, 31, 33).
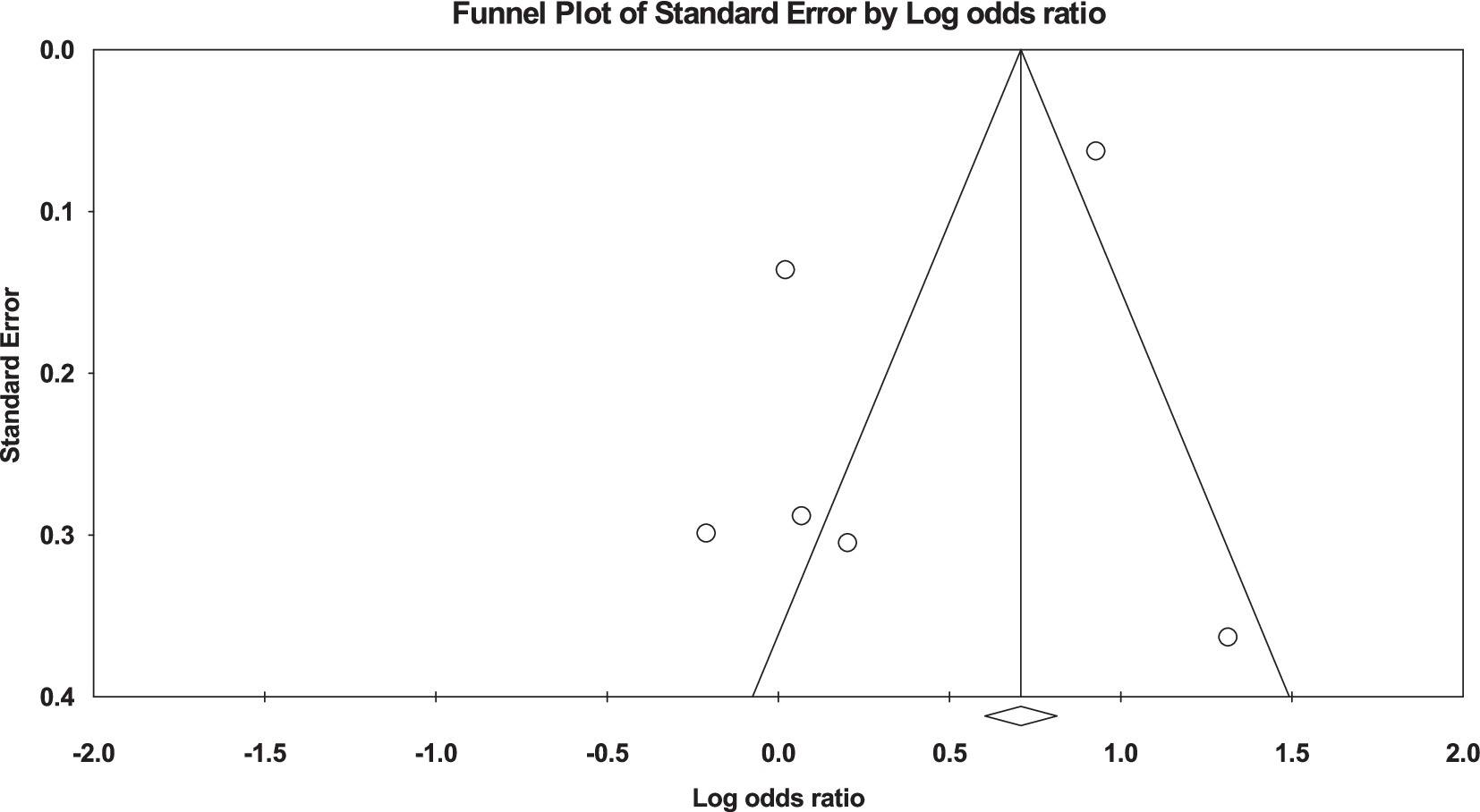
Married vs. unmarried
In the conducted analysis, it was observed that unmarried participants exhibited a higher propensity for developing diabetes in comparison to their married counterparts (OR: 1.47, 95% CI: 0.88 to 2.45, I2: 91%, p = 0.14) (Figure 2). Additionally, in evaluating publication bias, the funnel plots that were conducted displayed no discernible asymmetry in the distribution pattern of the studies (Figure 3).
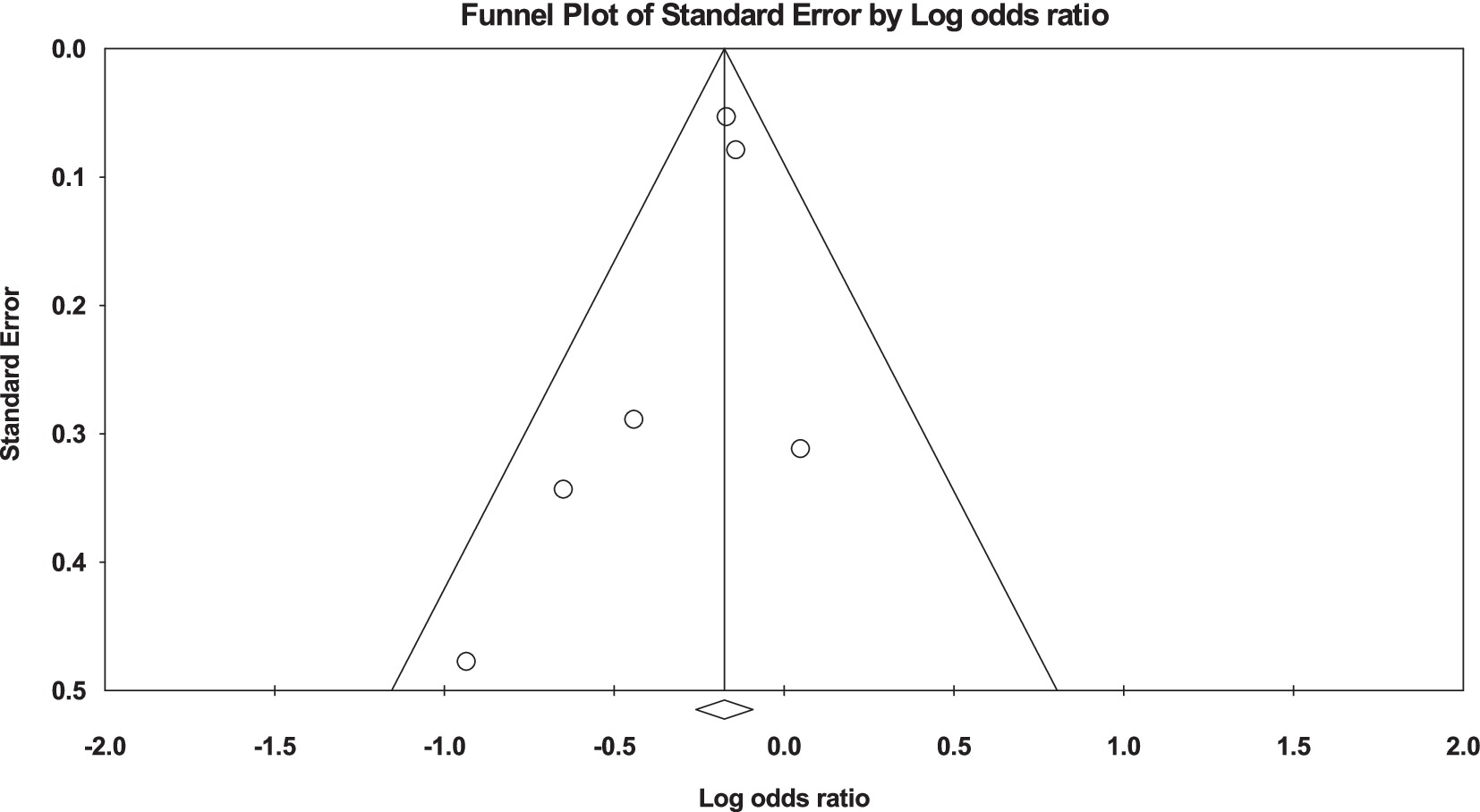
Married vs. divorced
The analysis revealed noteworthy findings in the context of marital status and the risk of developing diabetes. When comparing divorced individuals to their married counterparts, a lower likelihood of diabetes development was observed among the divorced group [OR: 0.84, 95% CI (0.77, 0.91), I2: 17%, p < 0.001] (Figure 4). Assessment for publication bias through funnel plots indicated no significant asymmetry in the distribution pattern of studies (Figure 5).
Married vs. widowed
Similarly, when evaluating the risk in widowed individuals compared to divorced individuals, a significantly lower likelihood of developing diabetes was evident among the widowed participants [OR: 0.35, 95% CI (0.26, 0.46), I2: 83%, p < 0.00001] (Figure 6). Furthermore, examination via funnel plots did not exhibit any substantial asymmetry in study distribution, signifying no evident publication bias (Figure 7).
Discussion
This systematic review and meta-analysis aimed to examine the relationship between marital status and the risk of T2DM. Our objective was to determine whether marital status significantly affects an individual’s susceptibility to type 2 diabetes, filling a critical void in the existing literature. The present study comprehensively analyzed six eligible research, encompassing 1,440,904 participants. The findings of this analysis have revealed that unmarried individuals exhibited a higher propensity for the development of diabetes in comparison to their married counterparts. Furthermore, divorced participants demonstrated a lower likelihood of developing diabetes when contrasted with their married counterparts. Similarly, widowed participants also displayed a reduced likelihood of diabetes development compared to their married counterparts (see Table 1).
Numerous studies have extensively explored the association between T2DM and marital status. The precise mechanisms contributing to the influence of marital status on T2DM remain incompletely understood. Previous research has proposed various hypotheses for these effects, encompassing psychopathological aspects, neuroendocrine pathways, health behaviors (including physical activity, dietary habits, and adherence), biological mediators, incorporating social cognitive processes, mental health outcomes, and immunological pathways (16, 34–36). Also, two principal theories have elucidated the health benefits attributed to marriage. The initial one relates to the “selection”: individuals in better health are more likely to enter into and maintain marriages. The second hypothesis reflects the post-marriage effect: tension reduction and adoption of healthful behaviors (37–39).
We have found that unmarried individuals were more likely to develop diabetes than married individuals [OR: 1.47, 95% CI (0.88, 2.45), I2: 91%, p = 0.14]. Cornelis et al. (31) revealed that unmarried males exhibited a 16% elevated susceptibility to developing T2DM compared to their married counterparts. They conducted a prospective analysis on male health professionals to investigate the probability of developing incident T2DM concerning their present marital status. Following a 22-year period of follow-up, it was determined that there exists a notable elevation in the likelihood of developing T2DM among males who are not married. Our findings are in agreement with Hiltunen’s (32) results, which showed that the prevalence of diabetes was lower among individuals who were married, in contrast to those who were unmarried. However, Azimi-Nezhad et al. (33) discovered that the prevalence of T2DM does not differ significantly between married and unmarried individuals.
Our analysis has shown that divorced participants were less likely to develop diabetes than married participants [OR: 0.84, 95% CI (0.77, 0.91), I2: 17%, p < 0.001]. Our finding is in contrast to the results of de Oliveira et al. (29) results. Their research findings showed a significant increase in body weight in individuals who stayed married or got married during the 5-year follow-up period. However, individuals who maintained their marital status despite experiencing substantial weight gain exhibited a notably reduced risk of developing diabetes compared to those who had gone through a divorce. Furthermore, Kposowa et al. (30) conducted a study revealing that men who had experienced divorce or separation had an increased risk of mortality due to diabetes mellitus. On the contrary, findings from Cornelis et al. (31) indicated no statistically significant elevation in the risk of M among men who were divorced, separated, or never married compared to their married counterparts. Also, Azimi-Nezhad’s et al. (33) investigation demonstrated that the prevalence of T2DM did not exhibit a significant difference between married, unmarried, bereaved, or divorced individuals.
Several studies have shown that those who are unmarried, divorced, or widowed may have negative health consequences. A survey conducted in Brazil showed that the incidence of diabetes was 60% higher among those who were widowed than those who were married (40). Our findings show that widowed participants were also less likely to develop diabetes compared to married participants [OR: 0.35, 95% CI (0.26, 0.46), I2: 83%, p < 0.00001]. These findings are in accordance with the research conducted by Ramezankhani et al. (23). The study revealed a substantial correlation between widowhood and a 31% diminished susceptibility to the development of T2DM in the female population. The results of this investigation further elucidated that, spanning 12 years, widowed women exhibited a reduced likelihood of developing Type T2DM compared to their married counterparts. Importantly, this association retained its statistical significance even after meticulous adjustment for confounding variables. However, these findings are incongruent with the results obtained by Cornelis et al. (31) and Kposowa et al. (30); individuals who have experienced the loss of a spouse are more susceptible to developing diabetes mellitus.
This systematic review and meta-analysis represents the first comprehensive investigation into the association between all major marital statuses—married, unmarried, divorced, and widowed—and the risk of T2DM, drawing on data from high-quality studies with a combined sample size exceeding 1.4 million participants. In contrast to prior studies, such as Leong et al. (41), which examined spousal diabetes and its relationship with shared socio-environmental factors, or Nikolic Turnic et al. (42), which assessed marital status in relation to obesity as an indirect risk factor for T2DM, this meta-analysis focuses directly on T2DM as the primary outcome. Furthermore, it differs from Ramezankhani et al. (23), which included T2D as part of a broader analysis of cardiovascular and metabolic outcomes but did not provide an in-depth examination of this condition. By incorporating a wide range of marital statuses and addressing underexplored categories such as divorced and widowed individuals, this study resolves inconsistencies in previous research and provides rough insights into marital status as a determinant of T2DM risk. These results contribute significantly to diabetes prevention research by addressing a previously overlooked factor and advocating for targeted public health interventions tailored to vulnerable marital groups.
Nonetheless, this research has limitations. The included studies exhibited considerable heterogeneity, and the limited availability of investigations in this field further restricts the generalizability of the findings. As this study is based on an observational design, it is limited in its ability to establish causal relationships between marital status and T2DM risk, as is typical of descriptive studies that rely on associations rather than direct cause-effect mechanisms. Additionally, demographic factors such as age, race, and participants’ backgrounds were not accounted for in the analysis, which might influence the observed associations. Future research is necessary to address these gaps and refine our understanding of the intricate relationships between marital status and T2DM risk. Despite these limitations, this study underscores the importance of considering marital status as a determinant of T2DM and lays the groundwork for future research and targeted public health strategies.
Conclusion
This study reveals consistent associations between marital status and T2DM risk, with unmarried individuals displaying a higher susceptibility to T2DM, divorced individuals having a lower likelihood, and widowed individuals exhibiting reduced T2DM risk. These findings underscore the importance of considering marital status as a potential factor in assessing T2DM risk. However, this study has some drawbacks, such as the heterogeneity and the shortage of studies. To better understand the association between marital status and T2DM, future research should look into the underlying mechanisms and consider potential confounding factors.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
MAK: Conceptualization, Formal analysis, Writing – original draft, Writing – review & editing, Investigation, Methodology, Validation. SB: Formal analysis, Writing – original draft, Validation. SH: Data curation, Investigation, Writing – original draft. PR: Data curation, Investigation, Writing – original draft. EnO: Data curation, Investigation, Writing – original draft. ElO: Data curation, Writing – original draft. AM: Investigation, Resources, Writing – original draft. RY: Formal analysis, Validation, Writing – original draft. MP: Writing – original draft, Writing – review & editing. ND: Writing – original draft, Writing – review & editing, Validation, Conceptualization.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2024.1485490/full#supplementary-material
References
1. American Diabetes Association. Economic costs of diabetes in the U.S. in 2017. Diabetes Care. (2018) 41:917–28. doi: 10.2337/dci18-0007
2. Roden, M, and Shulman, GI. The integrative biology of type 2 diabetes. Nature. (2019) 576:51–60. doi: 10.1038/s41586-019-1797-8
3. Stumvoll, M, Goldstein, BJ, and van Haeften, TW. Type 2 diabetes: principles of pathogenesis and therapy. Lancet. (2005) 365:1333–46. doi: 10.1016/S0140-6736(05)61032-X
4. Weyer, C, Bogardus, C, Mott, DM, and Pratley, RE. The natural history of insulin secretory dysfunction and insulin resistance in the pathogenesis of type 2 diabetes mellitus. J Clin Invest. (1999) 104:787–94. doi: 10.1172/JCI7231
5. Ebrahim, S, and Smith, GD. Exporting failure? Coronary heart disease and stroke in developing countries. Int J Epidemiol. (2001) 30:201–5. doi: 10.1093/ije/30.2.201
6. Saeedi, P, Salpea, P, Karuranga, S, Petersohn, I, Malanda, B, Gregg, EW, et al. Mortality attributable to diabetes in 20–79 years old adults, 2019 estimates: results from the international diabetes federation diabetes atlas, 9th edition. Diabetes Res Clin Pract. (2020) 162:108086. doi: 10.1016/j.diabres.2020.108086
7. Sarwar, N, Gao, P, Seshasai, SR, Gobin, R, Kaptoge, S, Di Angelantonio, E, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. (2010) 375:2215–22. doi: 10.1016/S0140-6736(10)60484-9
8. Saran, R, Robinson, B, Abbott, KC, Agodoa, LYC, Bragg-Gresham, J, Balkrishnan, R, et al. US renal data system 2018 annual data report: epidemiology of kidney disease in the United States. Am J Kidney Dis. (2019) 73:A7–a8. doi: 10.1053/j.ajkd.2019.01.001
9. Zoppini, G, Fedeli, U, Schievano, E, Dauriz, M, Targher, G, Bonora, E, et al. Mortality from infectious diseases in diabetes. Nutr Metab Cardiovasc Dis. (2018) 28:444–50. doi: 10.1016/j.numecd.2017.12.007
10. Linkeviciute-Ulinskiene, D, Patasius, A, Zabuliene, L, Stukas, R, and Smailyte, G. Increased risk of site-specific cancer in people with type 2 diabetes: a national cohort study. Int J Environ Res Public Health. (2019) 17:246. doi: 10.3390/ijerph17010246
11. Fincham, FD, and Bradbury, TN. The assessment of marital quality: a reevaluation. J Marriage Fam. (1987) 49:797–809. doi: 10.2307/351973
12. Liang, Y, Wu, X, Lu, C, and Xiao, F. Impact of marital status on the prognosis of liver cancer patients without surgery and the critical window. Ann Palliat Med. (2021) 10:2990–9. doi: 10.21037/apm-20-1885
13. Ai, L, Li, N, Tan, HL, Wei, B, Zhao, YX, Chen, P, et al. Effects of marital status on survival of medullary thyroid cancer stratified by age. Cancer Med. (2021) 10:8829–37. doi: 10.1002/cam4.4388
14. Son, M, Heo, YJ, Hyun, HJ, and Kwak, HJ. Effects of marital status and income on hypertension: the Korean Genome and Epidemiology Study (KoGES). J Prev Med Public Health. (2022) 55:506–19. doi: 10.3961/jpmph.22.264
15. Humbert, X, Rabiaza, A, Fedrizzi, S, Alexandre, J, Menotti, A, Touzé, E, et al. Marital status and long-term cardiovascular risk in general population (Gubbio, Italy). Sci Rep. (2023) 13:6723. doi: 10.1038/s41598-023-33943-0
16. Whisman, MA, Li, A, Sbarra, DA, and Raison, CL. Marital quality and diabetes: results from the health and retirement study. Health Psychol. (2014) 33:832–40. doi: 10.1037/hea0000064
17. Pieper, BA, Kushion, W, and Gaida, S. The relationship between a couple’s marital adjustment and beliefs about diabetes mellitus. Diabetes Educ. (1990) 16:108–12. doi: 10.1177/014572179001600206
18. Choi, H, Yorgason, JB, and Johnson, DR. Marital quality and health in middle and later adulthood: dyadic associations. J Gerontol B. (2016) 71:154–64. doi: 10.1093/geronb/gbu222
19. Trief, PM, Himes, CL, Orendorff, R, and Weinstock, RS. The marital relationship and psychosocial adaptation and glycemic control of individuals with diabetes. Diabetes Care. (2001) 24:1384–9. doi: 10.2337/diacare.24.8.1384
20. McBride, RAR. Association between marital status, family size, and diabetes among Asian-American women In: Walden dissertations and doctoral studies. Minneapolis, MN: Walden University (2024)
21. Metsä-Simola, N, and Martikainen, P. The short-term and long-term effects of divorce on mortality risk in a large Finnish cohort, 1990–2003. Popul Stud. (2013) 67:97–110. doi: 10.1080/00324728.2012.746386
22. Tuoyire, DA, and Ayetey, H. Gender differences in the association between marital status and hypertension in Ghana. J Biosoc Sci. (2019) 51:313–34. doi: 10.1017/S0021932018000147
23. Ramezankhani, A, Azizi, F, and Hadaegh, F. Associations of marital status with diabetes, hypertension, cardiovascular disease and all-cause mortality: a long term follow-up study. PLoS One. (2019) 14:e0215593. doi: 10.1371/journal.pone.0215593
24. Pratiwi, IN, Nursalam, N, Widyawati, IY, and Ramoo, V. Spousal involvement in collaborative management and glycemic behavior change among patients with diabetes mellitus: a systematic review. SAGE Open Nurs. (2024) 10:23779608241245196. doi: 10.1177/23779608241245196
25. Wells, GA, Shea, B, O’Connell, D, Peterson, J, Welch, V, Losos, M, et al. (2000). The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses.
26. Higgins, JP, and Thompson, SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58. doi: 10.1002/sim.1186
27. DerSimonian, R, and Kacker, R. Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials. (2007) 28:105–14. doi: 10.1016/j.cct.2006.04.004
28. Sterne, JA. Funnel plots in meta-analysis. Stata J. (2004) 4:127–41. doi: 10.1177/1536867X0400400204
29. de Oliveira, CM, Viater Tureck, L, Alvares, D, Liu, C, Horimoto, A, Balcells, M, et al. Relationship between marital status and incidence of type 2 diabetes mellitus in a Brazilian rural population: the Baependi Heart Study. PLoS One. (2020) 15:e0236869. doi: 10.1371/journal.pone.0236869
30. Kposowa, AJ, Aly Ezzat, D, and Breault, K. Diabetes mellitus and marital status: evidence from the National Longitudinal Mortality Study on the effect of marital dissolution and the death of a spouse. Int J Gen Med. (2021) 14:1881–8. doi: 10.2147/IJGM.S307436
31. Cornelis, MC, Chiuve, SE, Glymour, MM, Chang, SC, Tchetgen Tchetgen, EJ, Liang, L, et al. Bachelors, divorcees, and widowers: does marriage protect men from type 2 diabetes? PLoS One. (2014) 9:e106720. doi: 10.1371/journal.pone.0106720
32. Hiltunen, LA. Are there associations between socio-economic status and known diabetes in an elderly Finnish population? Cent Eur J Public Health. (2005) 13:187–90.
33. Azimi-Nezhad, M, Ghayour-Mobarhan, M, Parizadeh, MR, Safarian, M, Esmaeili, H, Parizadeh, SM, et al. Prevalence of type 2 diabetes mellitus in Iran and its relationship with gender, urbanisation, education, marital status and occupation. Singapore Med J. (2008) 49:571–6.
34. Causland, FR, Sacks, FM, and Forman, JP. Marital status, dipping and nocturnal blood pressure: results from the dietary approaches to stop hypertension trial. J Hypertens. (2014) 32:756–61. doi: 10.1097/HJH.0000000000000107
35. Schwandt, HM, Coresh, J, and Hindin, MJ. Marital status, hypertension, coronary heart disease, diabetes, and death among African American women and men: incidence and prevalence in the Atherosclerosis Risk in Communities (ARIC) study participants. J Fam Issues. (2010) 31:1211–29. doi: 10.1177/0192513X10365487
36. Rastkar, M, and Jalalifar, E. The association between marital quality and diabetes mellitus: a systematic review. Health Sci Rep. (2023) 6:e1106. doi: 10.1002/hsr2.1106
37. Espinosa, J, and Evans, WN. Heightened mortality after the death of a spouse: marriage protection or marriage selection? J Health Econ. (2008) 27:1326–42. doi: 10.1016/j.jhealeco.2008.04.001
38. Wyke, S, and Ford, G. Competing explanations for associations between marital status and health. Soc Sci Med. (1992) 34:523–32. doi: 10.1016/0277-9536(92)90208-8
39. Umberson, D. Gender, marital status and the social control of health behavior. Soc Sci Med. (1992) 34:907–17. doi: 10.1016/0277-9536(92)90259-S
40. de Almeida Busch Mendes, T, Goldbaum, M, Segri, NJ, Barros, MB, Cesar, CL, Carandina, L, et al. Diabetes mellitus: factors associated with prevalence in the elderly, control measures and practices, and health services utilization in São Paulo, Brazil. Cad Saude Publica. (2011) 27:1233–43. doi: 10.1590/s0102-311x2011000600020
41. Leong, A, Rahme, E, and Dasgupta, K. Spousal diabetes as a diabetes risk factor: a systematic review and meta-analysis. BMC Med. (2014) 12:12. doi: 10.1186/1741-7015-12-12
Keywords: diabetes, divorced, married, relationship, single, widow, T2DM, meta-analysis
Citation: Karimi MA, Binaei S, Hashemi SH, Refahi P, Olama E, Olama E, Mohammadpour A, Yonjali RM, Poudineh M and Deravi N (2025) Marital status and risk of type 2 diabetes among middle-aged and elderly population: a systematic review and meta-analysis. Front. Med. 11:1485490. doi: 10.3389/fmed.2024.1485490
Edited by:
Philip M. Gallagher, University of Kansas, United StatesReviewed by:
Carlos Manuel Zapata-Martín del Campo, National Institute of Cardiology Ignacio Chavez, MexicoLubia Velázquez López, Instituto Mexicano del Seguro Social, Mexico
Copyright © 2025 Karimi, Binaei, Hashemi, Refahi, Olama, Olama, Mohammadpour, Yonjali, Poudineh and Deravi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mohadeseh Poudineh, bW8ucG91ZGluZWhAZ21haWwuY29t; Niloofar Deravi, bmlsb29mYXJkZXJhdmlAc2JtdS5hYy5pcg==
†These authors have contributed equally to this work
 Mohammad Amin Karimi
Mohammad Amin Karimi Sara Binaei
Sara Binaei Seyed Hadi Hashemi3
Seyed Hadi Hashemi3 Mohadeseh Poudineh
Mohadeseh Poudineh Niloofar Deravi
Niloofar Deravi