- 1Department of Gastroenterology, The First Hospital of Jilin University, Changchun, China
- 2Norman Bethune Health Science Center, Jilin University, Changchun, China
Introduction: Inflammatory bowel disease (IBD) is a multi-organ autoimmune disease that commonly affects the gastrointestinal tract, but can also affect other organs throughout the body. Less is known, however, about kidney involvement in IBD. Although IBD has been associated with chronic kidney disease (CKD) and end-stage renal disease (ESRD), these results have been inconsistent. The present study analyzed the prevalence of concurrent CKD and ESRD in patients with IBD.
Methods: PubMed, Cochrane, Web of Science, and Embase were searched for studies published through October 2023 on IBD patients with concurrent CKD or ESRD. Outcomes included the incidence rates and odds ratios (OR) of concurrent CKD and ESRD in IBD patients. The quality of included studies was assessed using the Newcastle-Ottawa Scale, and sequential sensitivity was analyzed. Publication bias was evaluated using Egger’s test.
Results: Nine studies were included in this meta-analysis. The combined results of eight studies, which included 239,042 IBD patients, showed that the prevalence of CKD in IBD patients was 5% (95% confidence interval [CI]: 1–9%). The combined results of two studies, which included 40,341 IBD patients, showed that the prevalence of ESRD in IBD patients was 0.2% (95% CI: −0.08–0.12%). The combined results of six case–control studies reported that the risk of CKD was significantly higher in patients with than without IBD (OR 1.36, 95% CI: 1.08–1.70, p = 0.008).
Conclusion: Although studies have shown an increased risk of CKD in IBD, due to the small number of included studies and high heterogeneity across studies, it is not enough to definitively conclude that CKD is more common in patients with IBD. But patients with IBD should be regularly monitored for CKD.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/.
1 Introduction
Inflammatory bowel disease (IBD), consisting mainly of Crohn’s disease (CD) and ulcerative colitis (UC), is characterized by chronic recurrent intestinal inflammation. The pathogenesis of IBD is thought to involve complex interactions among genetic, environmental, and microbial factors, as well as immune responses (1). Traditionally, the incidence rate of IBD is highest in North America and Western Europe. Many cohort studies have shown that the incidence of IBD in these geographic areas increased significantly during the latter half of the 20th century, as well as increasing in populations of emerging nations, including in Asian countries (2).
IBD is a systemic disease that not only affects the gastrointestinal tract but also involves many extraintestinal organs. The quality of life of IBD patients may be significantly influenced by these extraintestinal manifestations (EIMs). Up to 50% of IBD patients have been reported to develop at least one EIM affecting various systems throughout the body (3). EIMs in patients with CD and UC most commonly involve the musculoskeletal system (e.g., peripheral and axial arthritis, enthesitis), the skin (e.g., pyoderma gangrenosum, erythema nodosum, Sweet’s syndrome, aphthous stomatitis), the hepatobiliary system (e.g., primary sclerosing cholangitis), and the eyes (e.g., episcleritis, anterior uveitis, iritis) (4).
Although there are limited data on renal manifestations in IBD patients, up to 5–15% of adult IBD patients may develop chronic kidney disease (CKD) over time (5). CKD has been defined by the Kidney Disease: Improving Global Outcomes (KDIGO) and the National Kidney Foundation (NKF) Kidney Disease Outcomes Quality Initiative (K/DOQI) guidelines as kidney damage or a glomerular filtration rate (GFR) < 60 mL/min/1.73 m2 for more than 3 months. These guidelines have defined renal impairment as functional or structural abnormalities of the kidney (6, 7).
The pathophysiology of renal involvement in patients with IBD is complex and not yet fully understood, possibly leading to various renal disorders affecting the glomeruli and/or tubular structure. Furthermore, medications used to treat IBD may be potentially nephrotoxic, and metabolic complications caused by the disease itself may further lead to renal damage (5).
Important predictors of renal failure include age at diagnosis of kidney disease and the chronicity of the disease in kidney biopsies. Overall survival was found to be significantly better in patients who did than did not experience partial or complete resolution of kidney disease, and those who did than did not show stabilization or improvement of renal function (8).
The aim of this study was to quantify the prevalence of CKD and end-stage renal disease (ESRD) in patients with IBD and to assess their associations. Early identification of these renal diseases may improve long-term outcomes in these patients.
2 Methods
2.1 Literature search and selection of studies
This study follows the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement (9). The PubMed, Cochrane, Web of Science, and Embase databases were searched using relevant keywords for studies published through October 2023 on IBD patients with concurrent CKD or ESRD (Supplementary Table S1). Studies were included if they (a) reported the occurrence of CKD/ESRD in IBD patients and (b) were original studies written in English and available in full text. Studies were excluded if (a) study data were missing; (b) they duplicated data or papers; (c) were case reports, letters, editorials, or meta-analyses that did not include original data, or (d) were conference abstracts or review articles. The references cited by included articles were also reviewed to ensure study comprehensiveness and accuracy. If different publications provided data from the same population, only the latest or most comprehensive study was included.
2.2 Data extraction
The literature screening process was divided into three steps. Following the initial literature search by one researcher, duplicate papers were removed using EndNote X9 software, followed by manual elimination of any remaining duplicates. A second researcher subsequently read the titles and abstracts of the selected studies, identifying studies that potentially met the inclusion criteria. A third researcher subsequently read the full text of the selected studies, identifying those that met the original criteria. Data were extracted from these studies using a pre-designed standard set of parameters, which included author names, year of publication, country, study period, study design, number of IBD patients (including CD and UC), number of CKD/ESRD patients, and number of control group participants. Any disagreements were resolved through discussion with a fourth researcher.
2.3 Quality assessment
The quality of included studies was assessed using the Newcastle-Ottawa Scale (NOS), and scores of 7–9 indicating high-quality studies (10). Two researchers independently assessed the quality and level of evidence of eligible studies, with any differences resolved through discussion with a third researcher.
2.4 Statistical analysis
All data were analyzed using Stata software version 18.0. A random-effects model was used to calculate the prevalence of CKD/ESRD and its 95% confidence interval [CI]. The random (M-H heterogeneity) model was applied to estimate the odds ratio (OR) and 95% CI for the occurrence of CKD/ESRD in IBD patients. Study heterogeneity was evaluated using the I2 test. A random effects model was used when there was high heterogeneity among studies (I2 > 50%). whereas a fixed effects model was used when there was low heterogeneity among studies (I2 ≤ 50%). Heterogeneity was assessed by sequential sensitivity analysis, in which one study was sequentially removed in each scenario. Publication bias was analyzed using Egger’s test (11).
3 Results
3.1 Study selection and quality evaluation
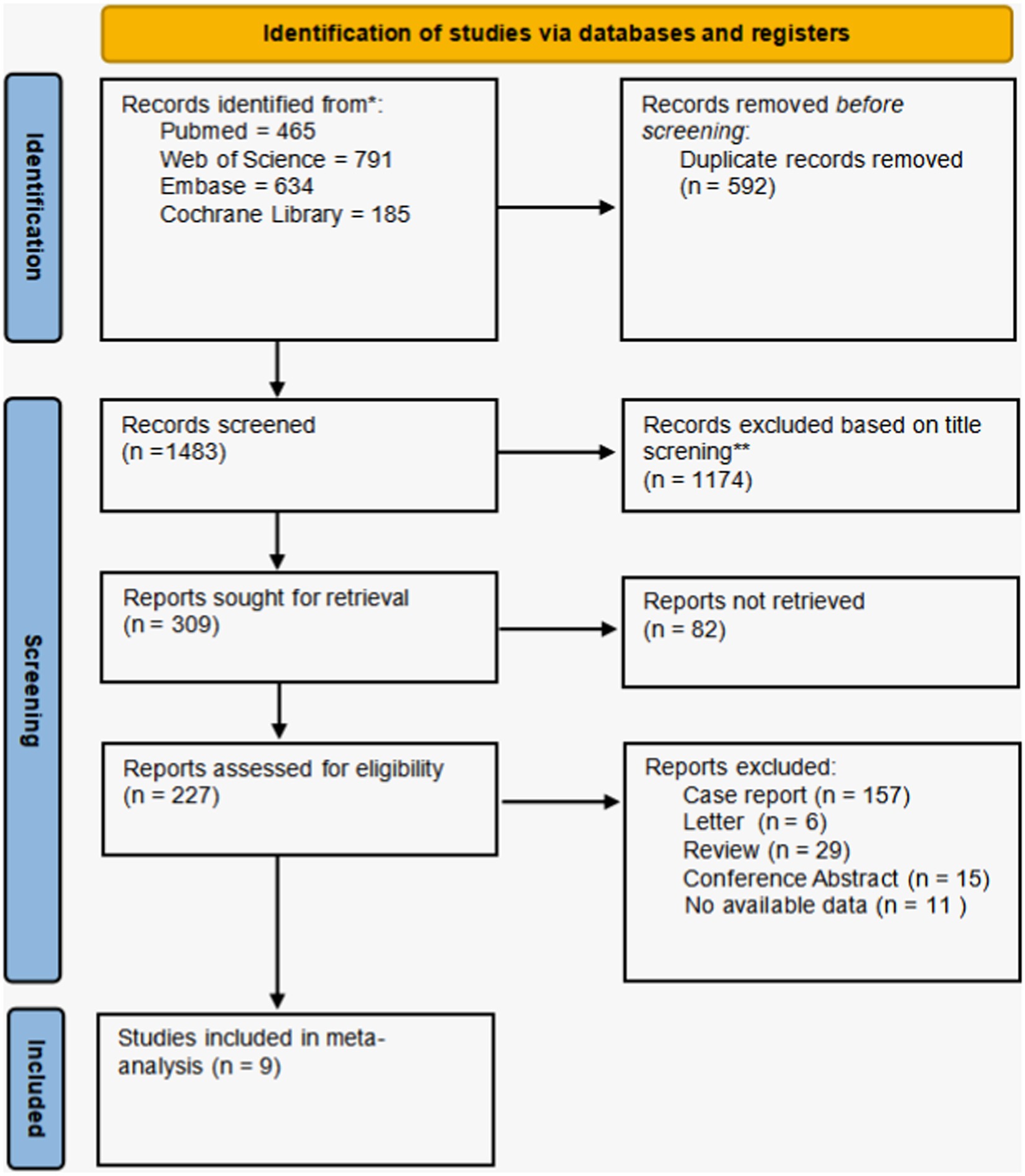
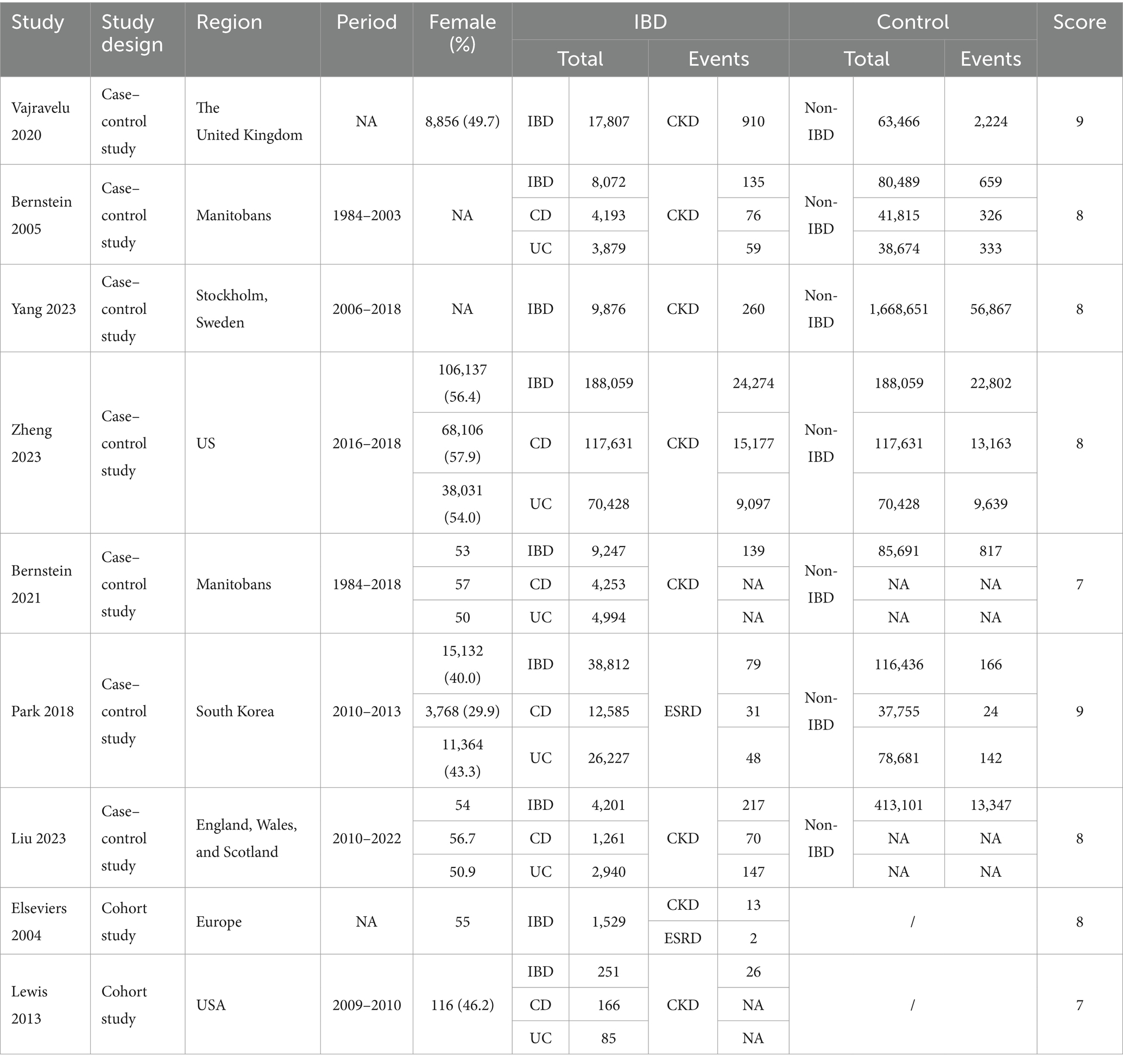
The original literature search identified a total of 2075 studies, 465 from PubMed, 634 from Embase, 791 from the Web of Science, and 185 from the Cochrane database. Of these, 592 duplicate studies were removed using EndNote X9 and manual screening, and 1,174 irrelevant studies were excluded by reviewing titles and abstracts. Of the 309 remaining studies, 82 could not be retrieved and were therefore excluded. Among the remaining 227 studies, 157 case reports, six letters, 29 reviews, 15 conference abstracts, and 11 studies with unavailable data were excluded, resulting in nine studies included in the meta-analysis. The flowchart of the search results and study selection process is shown in Figure 1. The main characteristics and quality assessment of the included studies are presented in Table 1. All nine included studies were of high quality.
3.2 Prevalence of CKD and ESRD in IBD patients
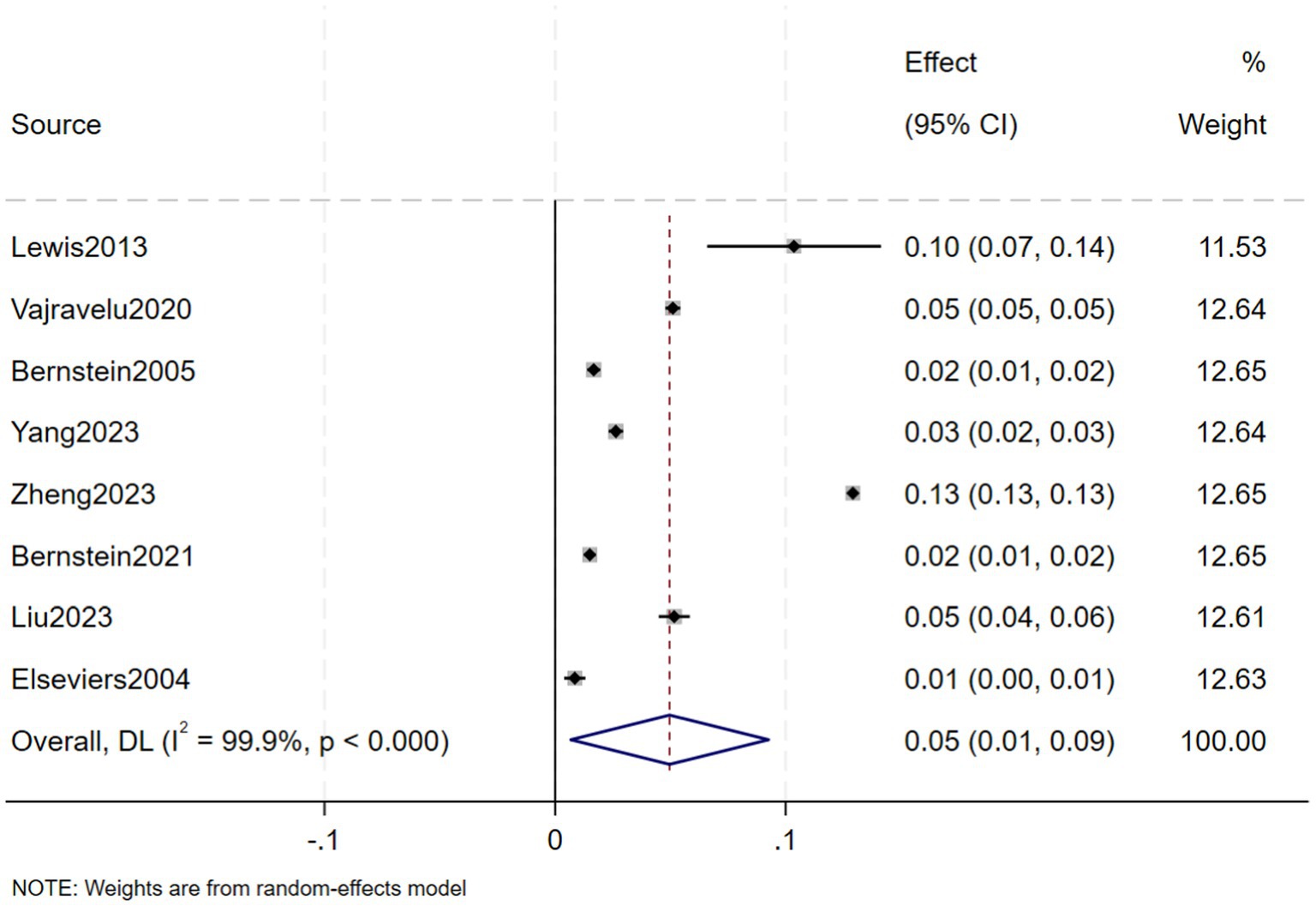
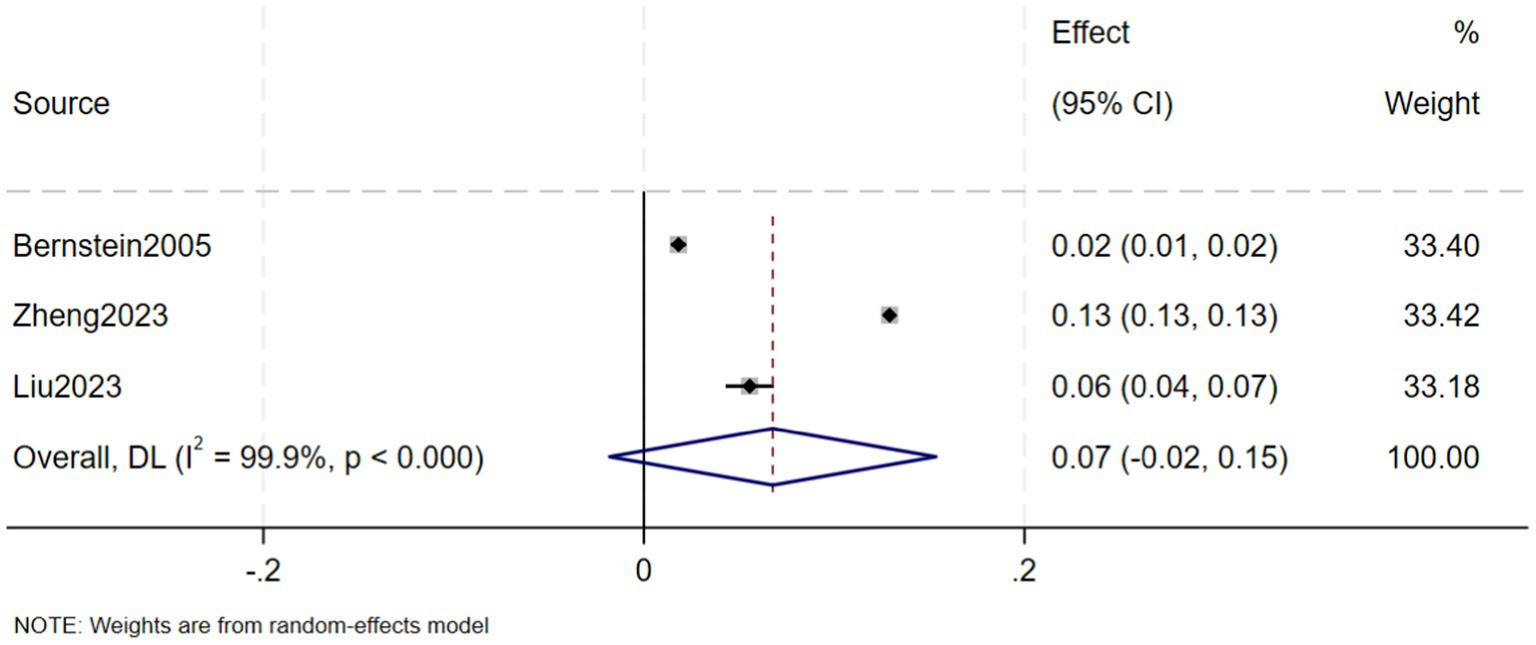
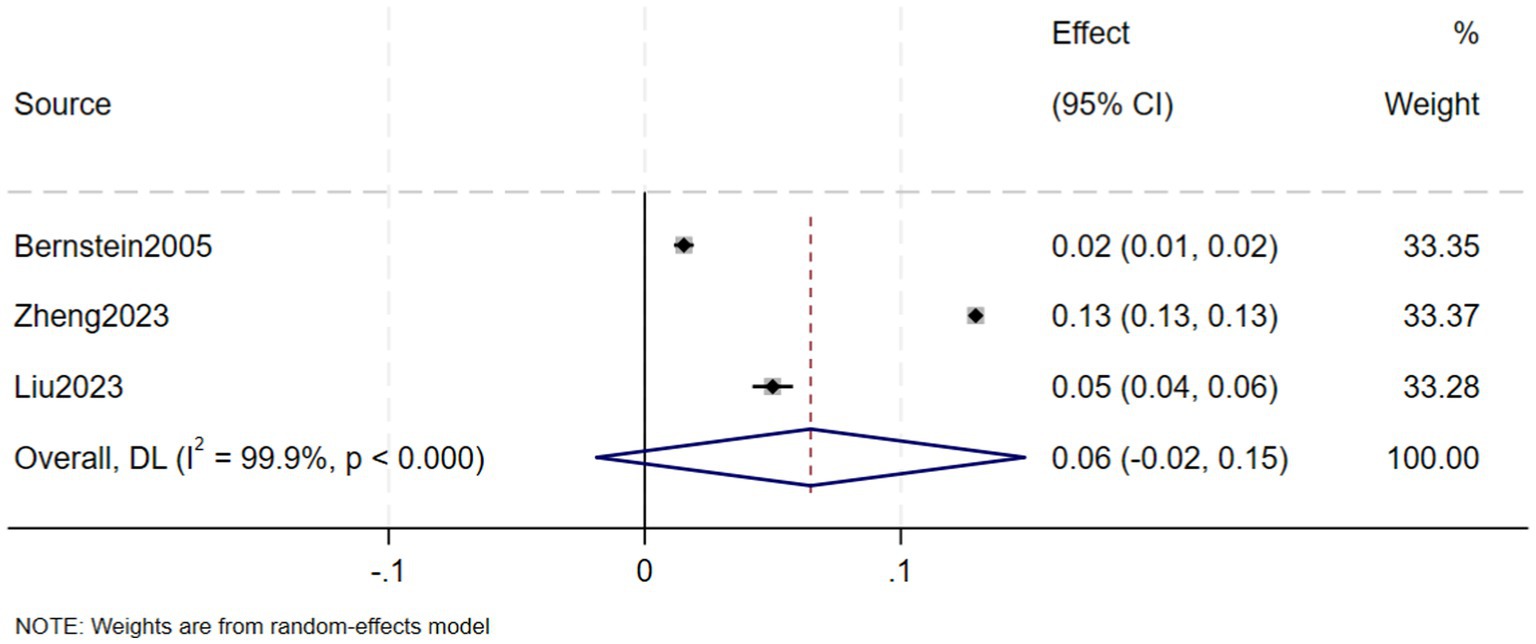
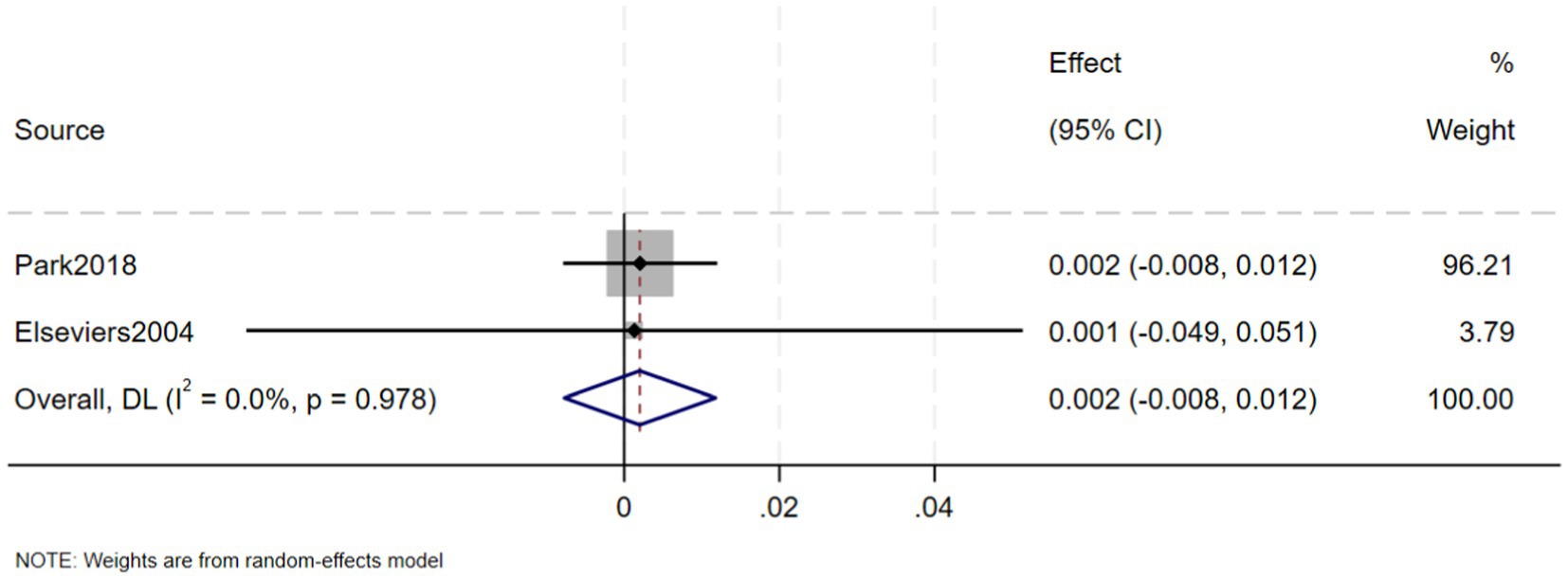
A total of eight studies, involving 239,042 patients with IBD, reported that the prevalence of CKD in in IBD patients was 5% (95% CI: 1–9%, I2 = 99.9%, heterogeneity p < 0.000) (Figure 2). Three of these studies reported the prevalence of CKD separately in CD and UC patients, finding that the prevalence of CKD in 123,085 CD patients was 7% (95% CI: −2–15%, I2 = 99.9%, heterogeneity p < 0.000) (Figure 3) and the prevalence of CKD in 77,247 UC patients was 6% (95% CI: −2–15%, I2 = 99.9%, heterogeneity p < 0.000) (Figure 4). Two studies, involving 40,341 patients with IBD, reported that the prevalence of ESRD was 0.2% (95% CI: −0.08–0.12%, I2 = 0.0%, heterogeneity p = 0.987) (Figure 5). Considering the single-group rate as a descriptive result, not a comparison of differences, sensitivity and publication bias analyses were not performed.
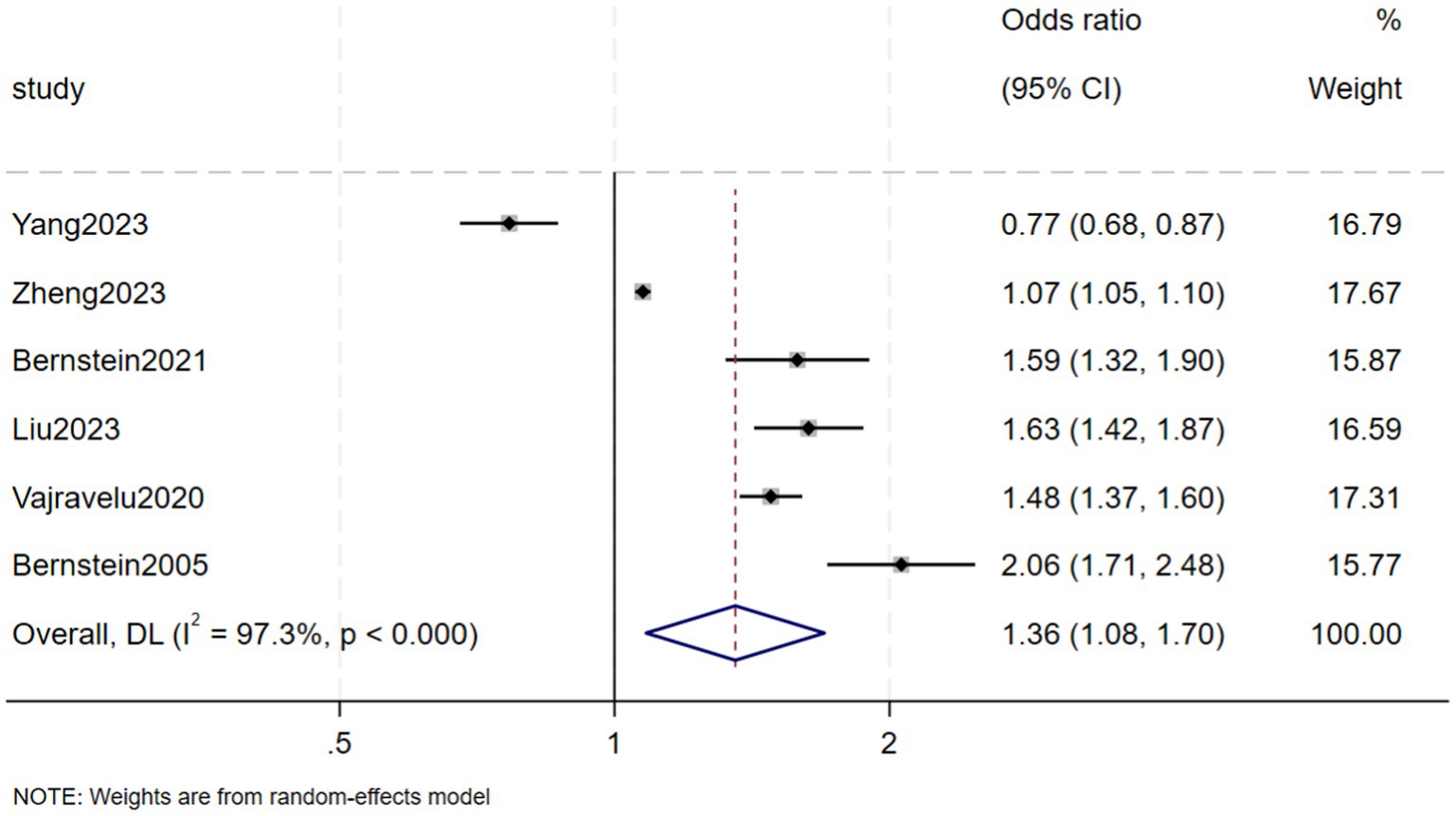
3.3 Association between IBD and CKD
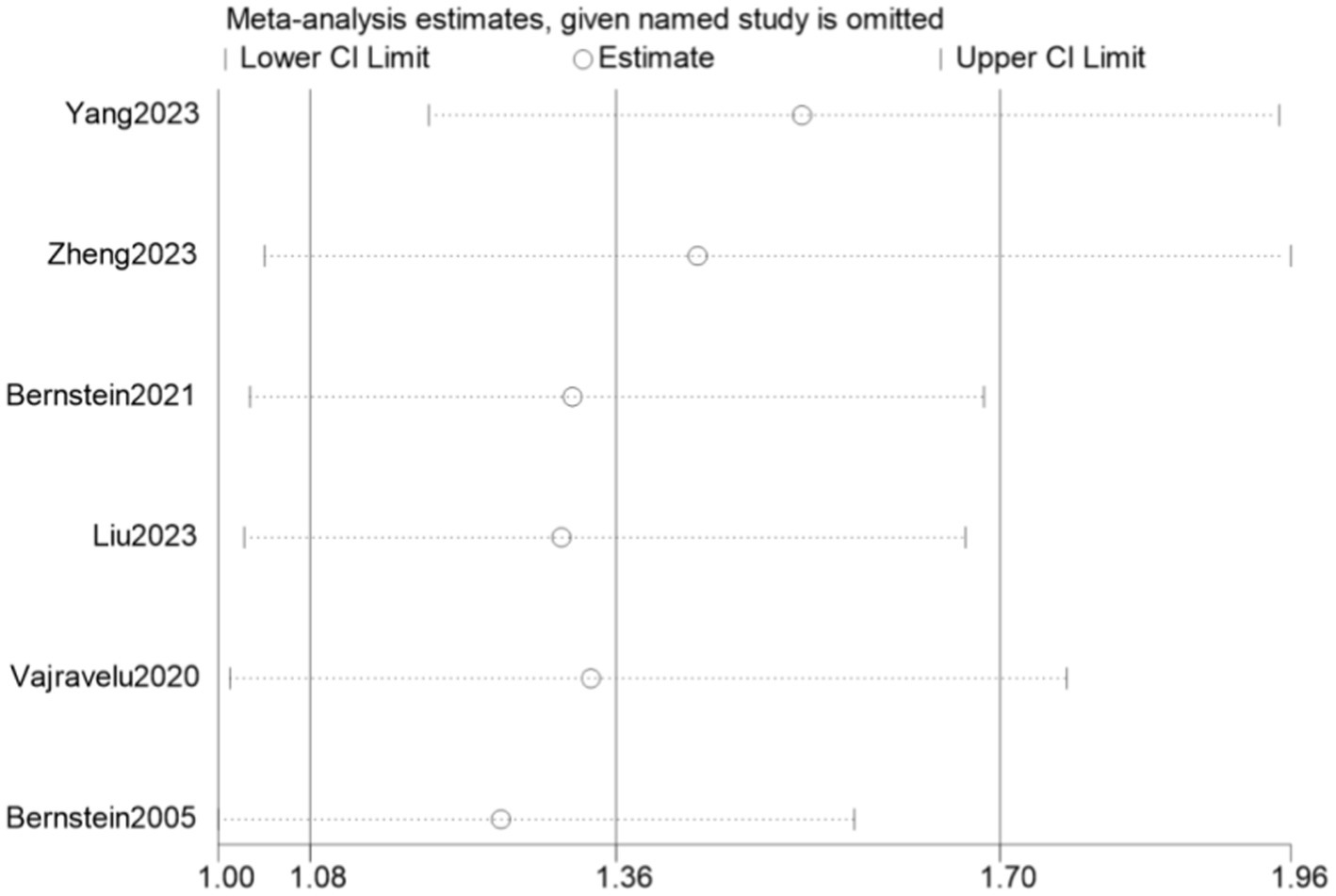
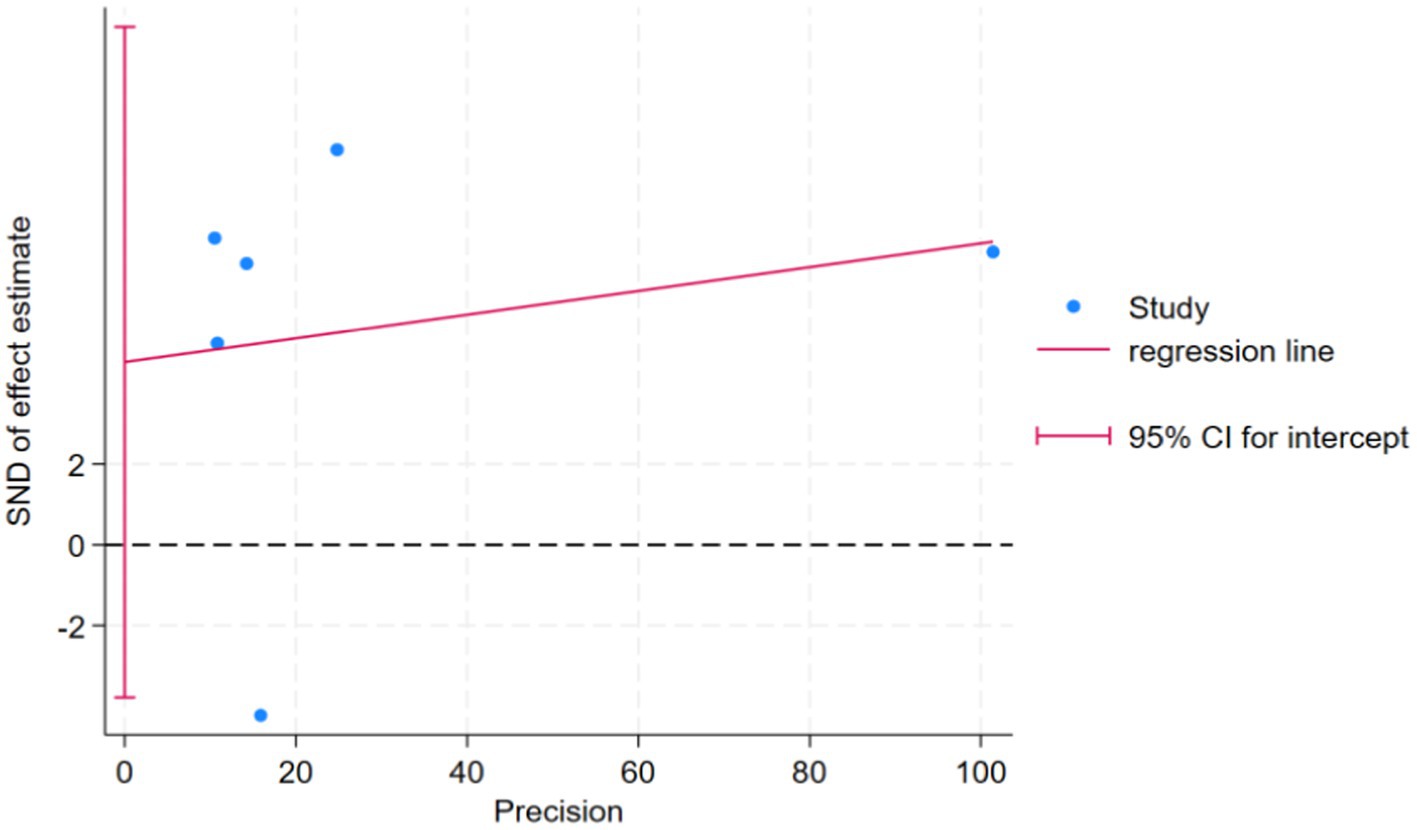
Six case–control studies reported the risk of CKD in patients with IBD compared with a control group, finding that the risk of CKD was significantly higher in patients with than without IBD had (OR = 1.36, 95% CI: 1.08–1.70, p = 0.008, I2 = 97.3%, heterogeneity p < 0.00) (Figure 6). Because I2 was >50%, this analysis utilized a random-effects model (M-H heterogeneity) and performed sensitivity analysis (Figure 7) by systematically excluding individual studies to evaluate their impact on the combined effect. After excluding any individual study, the combined results of the remaining studies were not statistically significant, indicating that the original meta-analysis results could easily change significantly and lacked stability due to variations in the number of studies. Egger’s test found no publication bias (p = 0.205) (Figure 8).
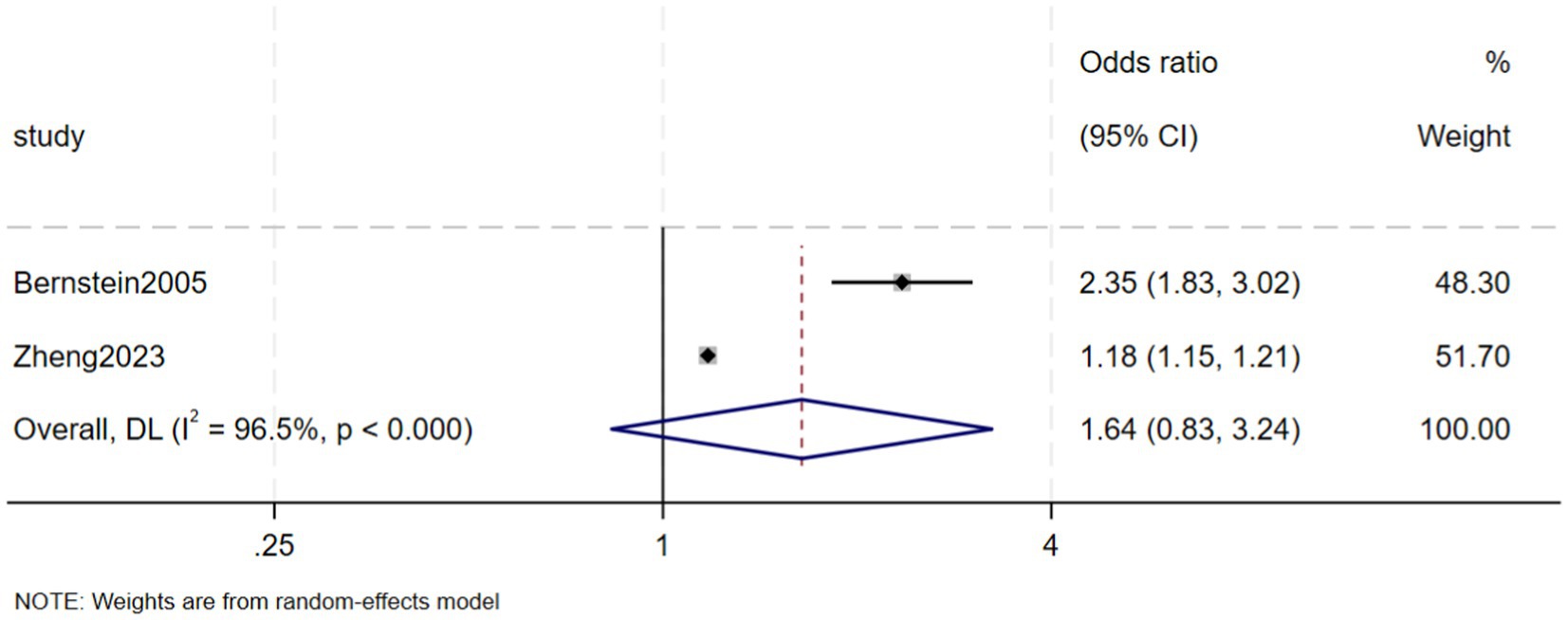
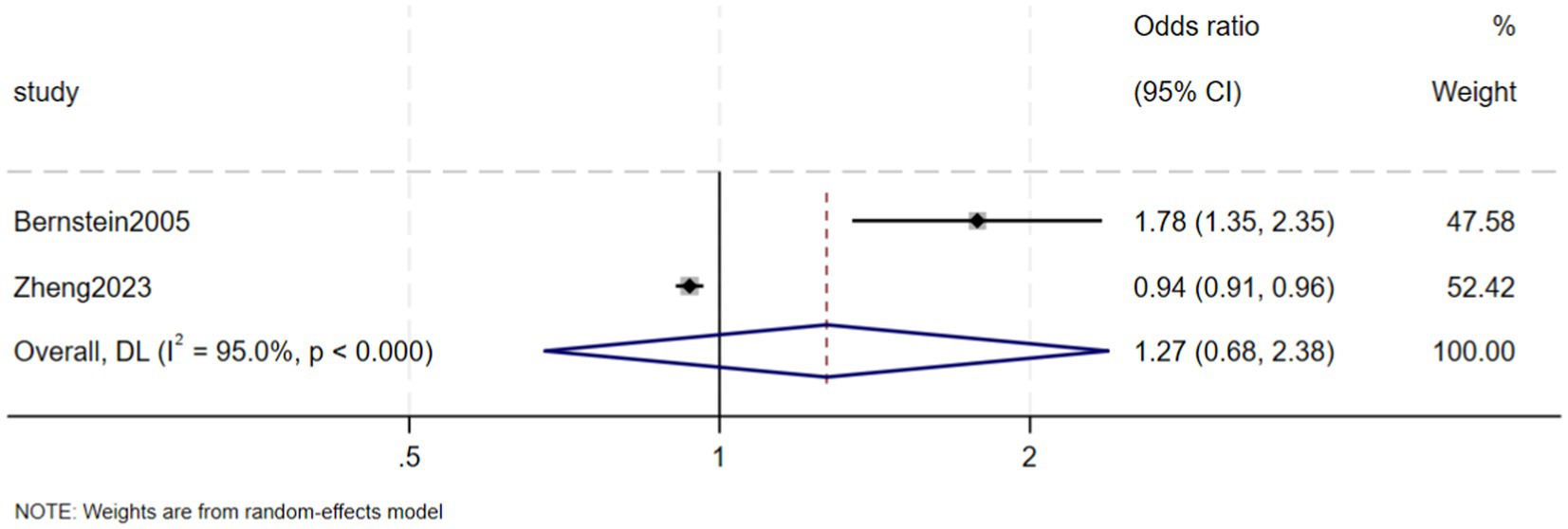
Two case–control studies separately reported the risk of CKD in CD and UC patients compared with a control group. Compared with control subjects, the ORs for CKD in CD and UC patients were 1.64 (95% CI 0.83–3.24, p = 0.151, I2 = 96.5%, heterogeneity p < 0.00) (Figure 9) and 1.27 (95% CI 0.68–2.38, p = 0.457, I2 = 95.0%, heterogeneity p < 0.00) (Figure 10), respectively.
Because only one case–control study reported the risk of ESRD in IBD patients compared with a control group, it was not subjected to a meta-analysis.
4 Discussion
This systematic review and meta-analysis found that the prevalence of CKD in patients with IBD was 5% (95% CI: 1–9%). Although the prevalence of CKD was higher in patients with CD (7%; 95% CI: −2–15%) than in patients with UC (6%; 95% CI: −2–15%), the difference was not statistically significant. The prevalence of ESRD in IBD patients was 0.2% (95% CI: −0.08–0.12%). The risk of CKD was found to be significantly higher in IBD patients than in a control group (OR = 1.36, 95% CI: 1.08–1.70, p = 0.008). Moreover, the ORs for CKD in CD and UC patients were 1.64 (95% CI: 0.83–3.24, p = 0.151) and 1.27 (95% CI: 0.68–2.38, p = 0.457), respectively.
Although studies have shown an increased risk of CKD in IBD, due to the small number of included studies and high heterogeneity across studies, it is not enough to definitively conclude that CKD is more common in patients with IBD. However, kidney function changes in IBD patients should still be of concern.
IBD is a systemic disease that primarily affects the intestines but is not limited to them. EIMs in IBD patients are caused by the same processes as intestinal inflammation but are located outside the intestines. The classic EIMs involve four organ systems: (1) the musculoskeletal system (e.g., arthritis and spondylitis); (2) the eyes (e.g., uveitis and episcleritis); (3) the skin (e.g., pyoderma gangrenosum, erythema nodosum, and oral ulcers); and (4) the liver-biliary system (e.g., primary sclerosing cholangitis) (12).
Although renal manifestations and complications are not rare in IBD patients, their direct correlation with intestinal diseases is not clear (13). Significant renal manifestations/complications in IBD include kidney stones, tubulointerstitial nephritis, glomerulonephritis, secondary amyloidosis, and medication-related complications (14), all of which can lead to impaired renal function, manifesting as acute or chronic renal insufficiency.
The risk of kidney stones has been reported higher in patients with than without IBD (15). Kidney stones are mainly caused by calcium oxalate or uric acid (16). The lifetime risk of kidney stones in IBD patients is approximately 18–20% (5), with this risk being higher in CD than in UC patients (5, 17). Patients with CD involving the colon are especially prone to oxalate stones, a condition known as enteric hyperoxaluria (EHO). EHO is thought to develop predominantly through three mechanisms: (1) increased absorption of oxalate salts, leading to increased excretion of oxalate salts in the urine and resulting in oxalate stone formation; (2) increased permeability of the colon to oxalate salts; and (3) decolonization of the gastrointestinal tract of IBD patients by the oxalate-degrading bacterium Oxalobacter formigenes, creating an ideal environment for promoting oxalate stone formation (18–20). Uric acid stones are common in patients with severe diarrhea or small intestine ostomies. The loss of intestinal fluid and bicarbonate leads to concentrated urine and increased acidity. Low urinary pH combined with low urine volume, especially in patients who have undergone colon surgery, promote the formation of uric acid stones (18, 21, 22). A single cohort study showed that recurrent urolithiasis was a major risk factor for renal insufficiency (23, 24). Therefore, complex IBD patients should be closely monitored, with regular urine analysis and upper urinary tract imaging (25).
Tubulointerstitial nephritis (TIN) in patients with IBD has been associated with exposure to 5-aminosalicylates (5-ASA) (26, 27), cyclosporine A, tumor necrosis factor-alpha (TNF-α) inhibitors (28) and vedolizumab (29). It is often challenging to determine whether renal dysfunction is a result of EIMs of IBD or drug therapy. Acute and chronic TIN have been reported to occur simultaneously with IBD, particularly CD, and in patients not exposed to nephrotoxic drugs (19). Kidney biopsies of untreated patients with CD have shown the presence of granulomas without eosinophilic infiltration. The co-occurrence in kidney biopsies of predominant lymphocytic infiltration with non-necrotizing granulomas further supports the diagnosis of TIN secondary to CD rather than drug-induced manifestations (30). Furthermore, TIN is most commonly associated with active intestinal disease, strongly suggesting that TIN is a true EIM of IBD (31, 32). Possible mechanisms of non-drug-related TIN include systemic immune dysregulation, cytokine activation, immune complexes targeting organ-specific epitopes shared by the colon and extracolonic sites (such as tubular basement membrane), and molecular mimicry (19).
Renal glomerular involvement in patients with IBD may be due to increased mucosal permeability, the deposition of intestinal-origin immune complexes following antigen exposure and the effects of drug therapy. The presence or worsening of glomerulonephritis has been reported consistent with the activity of intestinal diseases, indicating that renal glomerular injury is an EIM of IBD (19). Patients with IBD may have different histological types of glomerulonephritis, including IgA nephropathy, IgM nephropathy, membranous nephropathy, small vessel vasculitis, focal segmental glomerulosclerosis and anti-glomerular basement membrane glomerulonephritis (33). The most common diagnosis following kidney biopsy of these patients is IgA nephropathy, with the prevalence of IgA nephropathy being significantly higher than in kidney biopsy samples of all non-IBD patients (33, 34). Secondary IgA nephropathy in IBD may be a complex interaction involving mucosal inflammation, antigen rejection, chronic immune stimulation, and dysregulation of IgA production and transport (19). Furthermore, whole-genome association studies of IgA nephropathy have suggested a genetic cross-susceptibility between IBD and glomerular diseases (35). For example, HLA-DR1 has been associated with an increased risk of IgA nephropathy, whereas HLA-DR1/DQw5 has been associated with an increased risk of CD. Several loci associated with IgA nephropathy, such as CARD9 and HORMAD2, have also been associated with the risk of IBD. Other loci associated with IgA nephropathy, such as such as DEFA, TNFSF 13, VAV 3, ITGAM-ITGAX, and PSMB 8, encode proteins involved in maintaining the intestinal mucosal barrier or regulating mucosal immune responses (21). To date, however, there is no definitive information regarding the pathophysiology of other histological types of glomerulonephritis, such as IgM nephropathy, membranous nephropathy, small vessel vasculitis, focal segmental glomerulosclerosis, and anti-glomerular basement membrane glomerulonephritis (31).
Secondary amyloidosis (AA) is a rare but important complication of IBD. The most common clinical manifestation of AA is renal amyloidosis, typically presenting as proteinuria and nephrotic syndrome, which may progress to kidney failure (36). AA involves the deposition of amyloid fibrils derived from serum amyloid A (SAA) protein, an acute-phase reactant protein induced by chronic inflammation or infectious diseases that serves as a precursor to tissue amyloid proteins (37). In patients with CD and CD, the levels of SAA and acute-phase proteins correlate with disease activity (18). Early diagnosis of renal amyloidosis in IBD can improve patient prognosis.
Among the medications used to treat IBD, corticosteroids, azathioprine, metronidazole, low-dose methotrexate, and others have minimal or no renal toxicity (38). In contrast, ASAs, cyclosporine, tacrolimus, and TNF-α inhibitors may contribute to renal function impairment. However, the mechanisms by which these drugs participate in renal damage are generally unclear, making it difficult to determine whether renal impairment is due to EIMs or adverse drug reactions (31).
The ability of ASAs to cause renal damage is also unclear. Ulfasalazine, mesalazine, and olsalazine have been reported to induce renal toxicity, with the most common kidney alteration being interstitial nephritis (39). Systemic type I hypersensitivity reactions with fever and eosinophilia have also been observed (40).
Cyclosporine and tacrolimus are calcineurin inhibitors with immunosuppressive properties. The use of these drugs is often limited by severe adverse reactions, especially renal toxicity. Renal toxicity during treatment depends on the duration and dosage of treatment. The main features of chronic kidney damage are irreversible interstitial fibrosis and changes in small arteries (31).
TNF-α inhibitors, (including infliximab, adalimumab, certolizumab pegol, and golimumab) are increasingly used in the treatment of IBD (21). The anti-TNF-α produced by glomerular epithelial cells in patients with glomerulonephritis can lead to abnormal mucosal immune responses, such as the deposition of immune complexes of the drug itself or anti-drug antibodies, which can induce cell apoptosis and impair kidney function. Anti-TNF-α therapy can also shift the immune system to Th-2, upregulating the production of antibodies, including anti-nuclear, anti-dsDNA, and anti-neutrophil cytoplasmic antibodies, which may lead to the development of lupus-like and/or crescentic glomerulonephritis in susceptible individuals. Anti-TNF therapy can also increase the likelihood of viral or bacterial infections, which may promote different autoimmune reactions, such as molecular mimicry, bystander activation, or epitope spreading. In addition to anti-TNF drugs, other biologics that can cause this paradoxical effect. For example, adalimumab treatment of patients with refractory CD can lead to the development of tubulointerstitial nephritis (5, 31).
To our knowledge, this is the first study to analyze the incidence and risk of concurrent CKD in patients with IBD patients. However, this study had certain limitations. First, the number of studies included in the meta-analysis was limited, and there was significant heterogeneity among these studies, leading to the meta-analysis having insufficient robustness. Second, due to the limited number of studies included, this study did not perform stratified analyses based on factors such as patient gender and age.
5 Conclusion
Although studies have shown an increased risk of CKD in IBD, due to the small number of included studies and high heterogeneity across studies, it is not enough to definitively conclude that CKD is more common in patients with IBD. However, kidney function changes in IBD patients should still be of concern. Regular monitoring is crucial for early detection of kidney disease and prevention of progression to CKD. Early systematic diagnosis and management are recommended to reduce the burden of disease.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
XH: Writing – original draft, Software, Resources, Investigation, Conceptualization. ZX: Writing – original draft, Visualization, Project administration, Methodology, Formal analysis, Data curation. YC: Writing – original draft, Visualization, Project administration, Methodology, Formal analysis, Data curation. HL: Writing – original draft, Visualization, Project administration, Methodology, Formal analysis, Data curation. SH: Writing – original draft, Visualization, Project administration, Methodology, Formal analysis, Data curation. SC: Writing – review & editing, Validation, Supervision. YueL: Writing – review & editing, Validation, Supervision. CY: Writing – review & editing, Validation, Supervision. TT: Writing – review & editing. YuqL: Writing – review & editing, Validation, Supervision.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by Prospective clinical trial of efficacy and safety of infliximab in patients with moderate-to-severe Crohn’s disease (3R2240643428). The publication fee will be paid by this project.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2024.1485087/full#supplementary-material
References
1. Zhang, YZ, and Li, YY. Inflammatory bowel disease: pathogenesis. World J Gastroenterol. (2014) 20:91–9. doi: 10.3748/wjg.v20.i1.91
2. Ananthakrishnan, AN. Epidemiology and risk factors for IBD. Nat Rev Gastroenterol Hepatol. (2015) 12:205–17. doi: 10.1038/nrgastro.2015.34
3. Gordon, H, Burisch, J, Ellul, P, Karmiris, K, Katsanos, K, Allocca, M, et al. ECCO guidelines on extraintestinal manifestations in inflammatory bowel disease. J Crohns Colitis. (2024) 18:1–37. doi: 10.1093/ecco-jcc/jjad108
4. Rogler, G, Singh, A, Kavanaugh, A, and Rubin, DT. Extraintestinal manifestations of inflammatory bowel disease: current concepts, treatment, and implications for disease management. Gastroenterology. (2021) 161:1118–32. doi: 10.1053/j.gastro.2021.07.042
5. van Hoeve, K, and Hoffman, I. Renal manifestations in inflammatory bowel disease: a systematic review. J Gastroenterol. (2022) 57:619–29. doi: 10.1007/s00535-022-01903-6
6. Drawz, P, and Rahman, M. Chronic kidney disease. Ann Intern Med. (2015) 162:ITC1–ITC16. doi: 10.7326/AITC201506020
7. Stevens, PE, Ahmed, SB, Carrero, JJ, Foster, B, Francis, A, Hall, RK, et al. KDIGO 2024 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. (2024) 105:S117–314. doi: 10.1016/j.kint.2023.10.018
8. Yandian, F, Caravaca-Fontán, F, Herrera Hernandez, LP, Soler, MJ, Sethi, S, and Fervenza, FC. Kidney diseases associated with inflammatory bowel disease: impact of chronic histologic damage, treatments, and outcomes. Kidney Int Rep. (2024) 9:383–94. doi: 10.1016/j.ekir.2023.11.011
9. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
10. Kim, SR, Kim, K, Lee, SA, Kwon, SO, Lee, JK, Keum, NN, et al. Effect of red, processed, and white meat consumption on the risk of gastric cancer: an overall and dose(−)response meta-analysis. Nutrients. (2019) 11:826. doi: 10.3390/nu11040826
11. Egger, M, Smith, GD, Schneider, M, and Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
12. Greuter, T, and Vavricka, SR. Extraintestinal manifestations in inflammatory bowel disease - epidemiology, genetics, and pathogenesis. Expert Rev Gastroenterol Hepatol. (2019) 13:307–17. doi: 10.1080/17474124.2019.1574569
13. Oikonomou, K, Kapsoritakis, A, Eleftheriadis, T, Stefanidis, I, and Potamianos, S. Renal manifestations and complications of inflammatory bowel disease. Inflamm Bowel Dis. (2011) 17:1034–45. doi: 10.1002/ibd.21468
14. Lewis, B, Mukewar, S, Lopez, R, Brzezinski, A, Hall, P, and Shen, B. Frequency and risk factors of renal insufficiency in inflammatory bowel disease inpatients. Inflamm Bowel Dis. (2013) 19:1846–51. doi: 10.1097/MIB.0b013e31828a661e
15. Dimke, H, Winther-Jensen, M, Allin, KH, Lund, L, and Jess, T. Risk of urolithiasis in patients with inflammatory bowel disease: a nationwide Danish cohort study 1977-2018. Clin Gastroenterol Hepatol. (2021) 19:2532–40.e2. doi: 10.1016/j.cgh.2020.09.049
16. Abdulrhman, A, Alsweed, A, Alotaibi, MR, Aldakhil, AY, Alahmadi, SF, Albishri, SM, et al. Urolithiasis in patients with inflammatory bowel disease: a systematic review and meta-analysis of 13, 339, 065 individuals. Med. (2023) 102:e33938. doi: 10.1097/MD.0000000000033938
17. Zhang, H, Huang, Y, Zhang, J, Su, H, and Ge, C. Causal effects of inflammatory bowel diseases on the risk of kidney stone disease: a two-sample bidirectional mendelian randomization. BMC Urol. (2023) 23:162. doi: 10.1186/s12894-023-01332-4
18. Pardi, DS, Tremaine, WJ, Sandborn, WJ, and McCarthy, JT. Renal and urologic complications of inflammatory bowel disease. Am J Gastroenterol. (1998) 93:504–14. doi: 10.1111/j.1572-0241.1998.156_b.x
19. Ambruzs, JM, and Larsen, CP. Renal manifestations of inflammatory bowel disease. Rheum Dis Clin N Am. (2018) 44:699–714. doi: 10.1016/j.rdc.2018.06.007
20. Liu, M, and Nazzal, L. Enteric hyperoxaluria: role of microbiota and antibiotics. Curr Opin Nephrol Hypertens. (2019) 28:352–9. doi: 10.1097/MNH.0000000000000518
21. Kumar, S, Pollok, R, and Goldsmith, D. Renal and urological disorders associated with inflammatory bowel disease. Inflamm Bowel Dis. (2023) 29:1306–16. doi: 10.1093/ibd/izac140
22. Adler, M, Millar, EC, Deans, KA, Torreggiani, M, and Moroni, F. Dietary management of chronic kidney disease and secondary hyperoxaluria in patients with short bowel syndrome and type 3 intestinal failure. Nutrients. (2022) 14:1646. doi: 10.3390/nu14081646
23. Primas, C, Novacek, G, Schweiger, K, Mayer, A, Eser, A, Papay, P, et al. Renal insufficiency in IBD — prevalence and possible pathogenetic aspects. J Crohns Colitis. (2013) 7:e630–4. doi: 10.1016/j.crohns.2013.05.001
24. Wu, H, Liu, P, Gong, S, Liu, X, Hill, MA, Liu, Z, et al. Inflammatory bowel disease increases the levels of albuminuria and the risk of urolithiasis: a two-sample mendelian randomization study. Eur J Med Res. (2023) 28:167. doi: 10.1186/s40001-023-01128-0
25. Torricelli, FC, Reichard, C, and Monga, M. Urolithiasis in complicated inflammatory bowel disease: a comprehensive analysis of urine profile and stone composition. Int Urol Nephrol. (2021) 53:205–9. doi: 10.1007/s11255-020-02649-x
26. Moss, JG, Parry, CM, Holt, RCL, and McWilliam, SJ. 5-ASA induced interstitial nephritis in patients with inflammatory bowel disease: a systematic review. Eur J Med Res. (2022) 27:61. doi: 10.1186/s40001-022-00687-y
27. Vasanth, P, Parmley, M, Torrealba, J, and Hamdi, T. Interstitial nephritis in a patient with inflammatory bowel disease. Case Rep Nephrol. (2016) 2016:4260365–3. doi: 10.1155/2016/4260365
28. Sato, T, Kawasaki, Y, Ito, A, Izumi, H, Kawamorita, N, Yamashita, S, et al. Infliximab-induced tubulointerstitial nephritis with image findings of striated nephrogram in Crohn’s disease. Tohoku J Exp Med. (2018) 245:149–52. doi: 10.1620/tjem.245.149
29. Forss, A, Flis, P, Sotoodeh, A, Kapraali, M, and Rosenborg, S. Acute interstitial nephritis in patients with inflammatory bowel disease treated with vedolizumab: a systematic review. Scand J Gastroenterol. (2024) 59:821–9. doi: 10.1080/00365521.2024.2345383
30. Colvin, RB, Traum, AZ, Taheri, D, Jafari, M, and Dolatkhah, S. Granulomatous interstitial nephritis as a manifestation of Crohn disease. Arch Pathol Lab Med. (2014) 138:125–7. doi: 10.5858/arpa.2012-0224-CR
31. Corica, D, and Romano, C. Renal involvement in inflammatory bowel diseases. J Crohns Colitis. (2016) 10:226–35. doi: 10.1093/ecco-jcc/jjv138
32. Izzedine, H, Simon, J, Piette, AM, Lucsko, M, Baumelou, A, Charitanski, D, et al. Primary chronic interstitial nephritis in Crohn’s disease. Gastroenterology. (2002) 123:1436–40. doi: 10.1053/gast.2002.36613
33. Doumas, SA, Tsironis, C, Bolaji, AA, Garantziotis, P, and Frangou, E. Glomerulonephritis and inflammatory bowel disease: a tale of gut-kidney axis dysfunction. Autoimmun Rev. (2023) 22:103327. doi: 10.1016/j.autrev.2023.103327
34. Fernández-Castroagudín, J, Brage Varela, A, Lens Neo, XM, Martínez Castro, J, and Abdulkader, I. Renal amyloidosis as initial clinical manifestation of Crohn’s disease. Gastroenterol Hepatol. (2002) 25:395–7. doi: 10.1016/S0210-5705(02)70273-2
35. Kiryluk, K, Li, Y, Scolari, F, Sanna-Cherchi, S, Choi, M, Verbitsky, M, et al. Discovery of new risk loci for IgA nephropathy implicates genes involved in immunity against intestinal pathogens. Nat Genet. (2014) 46:1187–96. doi: 10.1038/ng.3118
36. Sattianayagam, PT, Gillmore, JD, Pinney, JH, Gibbs, SDJ, Wechalekar, AD, Gilbertson, JA, et al. Inflammatory bowel disease and systemic AA amyloidosis. Dig Dis Sci. (2013) 58:1689–97. doi: 10.1007/s10620-012-2549-x
37. Tosca Cuquerella, J, Bosca-Watts, MM, Anton Ausejo, R, Tejedor Alonso, S, Mora de Miguel, F, and Minguez Perez, M. Amyloidosis in inflammatory bowel disease: a systematic review of epidemiology, clinical features, and treatment. J Crohns Colitis. (2016) 10:1245–53. doi: 10.1093/ecco-jcc/jjw080
38. Park, S, Chun, J, Han, KD, Soh, H, Choi, K, Kim, JH, et al. Increased end-stage renal disease risk in patients with inflammatory bowel disease: a nationwide population-based study. World J Gastroenterol. (2018) 24:4798–808. doi: 10.3748/wjg.v24.i42.4798
39. Ambruzs, JM, Walker, PD, and Larsen, CP. The histopathologic spectrum of kidney biopsies in patients with inflammatory bowel disease. Clin J Am Soc Nephrol. (2014) 9:265–70. doi: 10.2215/CJN.04660513
Keywords: chronic kidney disease, inflammatory bowel disease, meta-analysis, Crohn disease, ulcerative colitis
Citation: Han X, Xu Z, Chang Y, Li H, Hu S, Chang S, Liu Y, Yu C, Tang T and Li Y (2024) Concurrent chronic kidney disease in patients with inflammatory bowel disease, a systematic review and meta-analysis. Front. Med. 11:1485087. doi: 10.3389/fmed.2024.1485087
Edited by:
Wolfgang Kruis, University of Cologne, GermanyReviewed by:
Jonathan Soldera, University of Caxias do Sul, BrazilSada Ghalib Taher, Thi Qar University, Iraq
Copyright © 2024 Han, Xu, Chang, Li, Hu, Chang, Liu, Yu, Tang and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuqin Li, bGl5dXFAamx1LmVkdS5jbg==
 Xiaoping Han1,2
Xiaoping Han1,2 Yu Chang
Yu Chang Chanjiao Yu
Chanjiao Yu Tongyu Tang
Tongyu Tang Yuqin Li
Yuqin Li