- 1Intensive Care Unit, Changshu No. 2 People’s Hospital, Suzhou, China
- 2Changshu Medicine Examination Institute, Suzhou, China
Aeromonas dhakensis is an increasingly recognized human pathogen in recent years and was first isolated and reported in a sample of childhood diarrhea in Bangladesh. More and more cases of Aeromonas dhakensis infection have been reported in recent years. Here we report a case of severe pneumonia caused by Aeromonas dhakensis with severe atrial septal defect. The patient, a 56-year-old male, was admitted to the hospital with severe hypoxemia and severe septic shock. Detection of the patient’s bronchoalveolar lavage fluid (BALF) and peripheral blood by the metagenomic next generation sequencing (mNGS) indicated Aeromonas dhakensis infection.
Introduction
Aeromonas dhakensis is a highly pathogenic human pathogen discovered in recent years (1). Aeromonas dhakensis is a Gram-negative bacillus and widely distributed in water environments (1). Aeromonas dhakensis is extremely virulent and can cause severe sepsis and multiple organ failure in a short time (2), with a 14-day sepsis-related mortality rate of 25.5% (3). Aeromonas dhakensis has been reported to have multiple virulence factors and its strains have cytotoxic activity against human blood cell lines (4). Aeromonas dhakensis, for example, produces a cytotoxic enterotoxin (5) and also secretes a pathogenic exotoxin A (6). Clinically, it can lead to the most common intestinal infections in patients, but also can lead to extremely serious invasive parenteral infections, such as lung infections, biliary tract infections, and soft tissue infections. Patients with compromised immunity are more susceptible to infection of Aeromonas dhakensis, which can lead to severe sepsis and organ failure (7). Here, we report a case of a 56-year-old man diagnosed with Aeromonas dhakensis pneumonia with severe atrial septal defect.
Case report
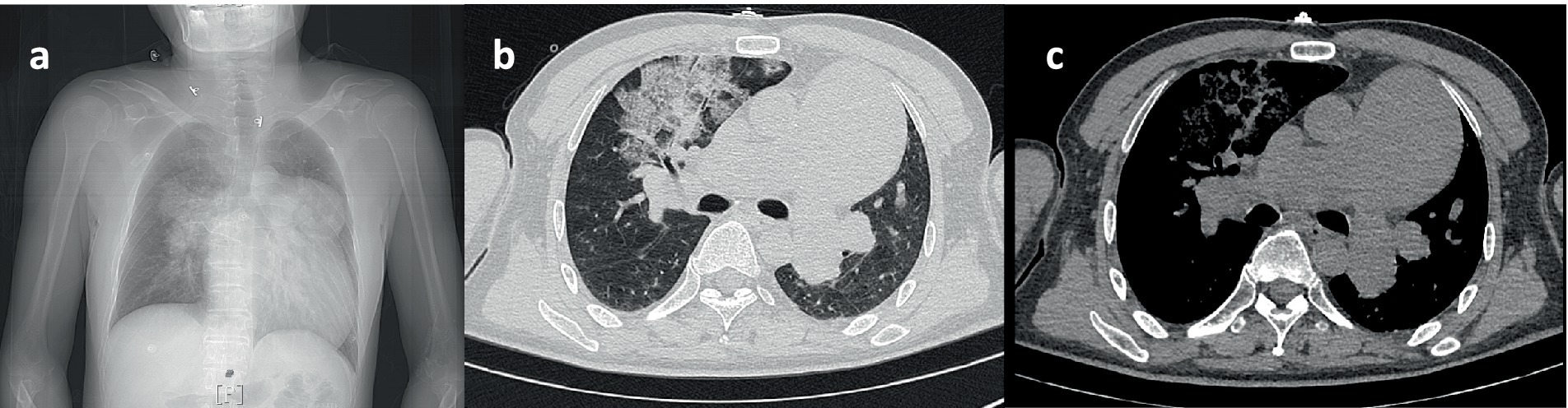
A 56-year-old male presented to the hospital due to fever with chest tightness and asthma for 1 day. The patient was admitted to ICU after endotracheal intubation with mechanical ventilation due to severe hypoxemia. The patient had a history of atrial septal defect for more than 30 years. A blood routine examination showed that white blood cell count was 2.0 × 109/L, the percentage of neutrophils was 85.8%, and platelet count was 43 × 109/L. C-reactive protein was 3.8 mg/L. Blood gas analysis showed that the oxygenation index was 39.5 mmHg. Procalcitonin was 91.8 ng/mL. The chest computer tomography (CT) scan displayed inflammation in both lungs, mainly in the upper lobe of the right lung (Figure 1). Cardiac ultrasound revealed that the atrial septal defect was 2.66 cm, and the pulmonary artery pressure is about 80 mmHg (Figure 2).
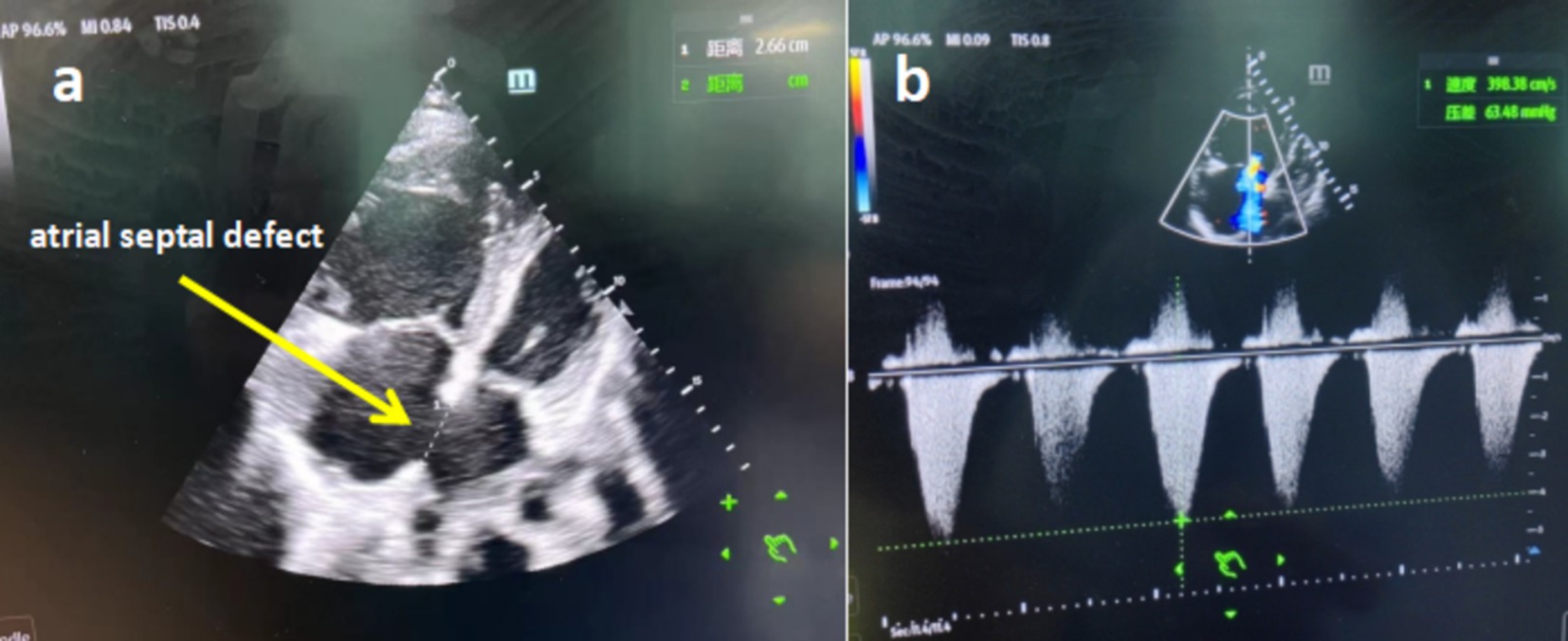
Figure 2. (a) Cardiac ultrasound showed the patient with severe atrial septal defect. (b) Cardiac ultrasound showed the patient with severe pulmonary hypertension.
The patient was diagnosed with severe pneumonia, severe acute respiratory distress syndrome (ARDS), septic shock, sepsis, severe atrial septal defect, and severe pulmonary hypertension. The patient’s empiric anti-infective therapy was omadacycline in combination with imipenem. The patient received the treatment of veno-arterio-venous extracorporeal membrane oxygenation (VAV-ECMO) immediately due to poor finger pulse oxygen and blood pressure. However, after ECMO treatment, the patient’s finger pulse oxygen was still poor. Sildenafil, ambrisentan and inhaled NO were given to reduce pulmonary arterial pressure, considering the patient had severe atrial septal defect and pulmonary hypertension, and severe pulmonary shunt. At the same time, the metagenomic next generation sequencing (mNGS) tested by the company Nanjing KingMed for clinical laboratory through Illumina MiSeq sequencing platform was used to detect the pulmonary alveolar lavage fluid (BALF) and peripheral blood to identify the infectious pathogen. Direct microscopic examination of BALF and peripheral blood showed Gram-negative bacteria.
On the third day of hospitalization, the results of the mNGS showed that Aeromonas dhakensis was positive and the relative abundance of Aeromonas dhakensis was 95.68%. According to the results of drug sensitivity test, Aeromonas dhakensis was sensitive to omoxycycline and imipenem. Therefore, the anti-infection treatment plan would not be adjusted. After active treatment for 2 weeks, the inflammatory index of the patient decreased significantly, and the patient’s consciousness became clear. However, due to pulmonary interstitial changes caused by infection and severe pulmonary hypertension, the patient still presented with moderate to severe respiratory failure and was unable to leave the ventilator (Figure 3). After 2 months of mechanical ventilation and rehabilitation exercise, the patient was successfully removed from the ventilator and transferred out of ICU (Figure 4). But the pulmonary interstitial changes caused by infection could not return to normal.
Discussion
Aeromonas is a Gram-negative bacterium. Human infections are usually caused by Aeromonas hydrophila, Aeromonas veronii biovar sobria, and Aeromonas caviae (8). Aeromonas is widely distributed in various kinds of freshwater waters, and the infection of Aeromonas in humans is usually through direct contact with water containing pathogenic bacteria (9). People with chronic underlying disease and low immunity are more susceptible to Aeromonas. Aeromonas can cause gastrointestinal tract, skin and soft tissue, respiratory infections, nervous system and biliary tract infections (10). The clinical manifestations of Aeromonas infection are usually rapid onset, severe symptoms and severe sepsis. It has been reported that the initial symptoms of Aeromonas infection may be diarrhea, cough, expectoration and hemoptysis (2).
Aeromonas dhakensis was previously considered a subspecies of Aeromonas hydrophila (11), which was first isolated from a sample of childhood diarrhea in Bangladesh (12). But according to the latest microbiology studies, whole genome sequence analyses unambiguously confirmed that Aeromonas dhakensis reached the level of species (13). Aeromonas dhakensis can also cause infections in the digestive, respiratory, urinary, hepatobiliary and skin and soft tissues (3). The mortality rate of Aeromonas dhakensis is much higher than other Aeromonas species (14), because Aeromonas dhakensis contains multiple pathogenic genes and can produce multiple exotoxins. Aeromonas dhakensis strains have toxic effects on human blood cell lines, which may result in a reduction in blood cell lines (15, 16). Up to now, the specific pathogenesis of Aeromonas dhakensis remains unclear (17).
Aeromonas dhakensis is sensitive to third or fourth generation cephalosporins, aminoglycosides, fluoroquinolones, and tetracyclines (18). Aeromonas dhakensis has been reported to produce a variety of β-lactamases resulting in resistance to a variety of penicillins, cephalosporins and even carbapenems (19). Clinicians should be cautious about the use of cephalosporins alone for anti-infective treatment if clinically suspected or confirmed Aeromonas dhakensis infection (20).
Conclusion
Clinically, we observed that the infection of Aeromonas dhakensis led to the rapid onset of severe septic shock and the possible complications of multiple organ failure Including heart failure, renal failure, respiratory failure, and decreased blood cell line. Aeromonas dhakensis is not a common pathogen in community-acquired pneumonia, but it can cause rapid onset, severe symptoms and multiple organ dysfunction in patients. At this time, clinicians should think of the possibility of a Aeromonas dhakensis infection. In this case, we used ECMO early to maintain the patient’s vital signs, which bought time and opportunity for effective treatment.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Ethics Review Committee of Changshu No. 2 People’s Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
JuS: Writing – original draft, Writing – review & editing. JiS: Project administration, Writing – review & editing. SL: Project administration, Writing – review & editing. MZ: Project administration, Writing – review & editing. CG: Project administration, Writing – review & editing. YD: Resources, Writing – review & editing. JZ: Project administration, Writing – review & editing. YF: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Chen, PL, Lamy, B, and Ko, WC. Aeromonas dhakensis, an increasingly recognized human pathogen. Front Microbiol. (2016) 7:793. doi: 10.3389/fmicb.2016.00793
2. Luo, D, and Dai, L. A 26-year-old man with multiple organ failure caused by Aeromonas dhakensis infection: a case report and literature review. Front Med. (2024) 11:1289338. doi: 10.3389/fmed.2024.1289338
3. Wu, CJ, Chen, PL, Hsueh, PR, Chang, MC, Tsai, PJ, Shih, HI, et al. Clinical implications of species identification in monomicrobial Aeromonas bacteremia. PLoS One. (2015) 10:e0117821. doi: 10.1371/journal.pone.0117821
4. Morinaga, Y, Yanagihara, K, Eugenin, FL, Beaz-Hidalgo, R, Kohno, S, and Figueras Salvat, MJ. Identification error of Aeromonas aquariorum: a causative agent of septicemia. Diagn Microbiol Infect Dis. (2013) 76:106–9. doi: 10.1016/j.diagmicrobio.2013.01.019
5. Chopra, AK, and Houston, CW. Enterotoxins in Aeromonas-associated gastroenteritis. Microbes Infect. (1999) 1:1129–37. doi: 10.1016/S1286-4579(99)00202-6
6. Ponnusamy, D, Kozlova, EV, Sha, J, Erova, TE, Azar, SR, Fitts, EC, et al. Cross-talk among flesh-eating Aeromonas hydrophila strains in mixed infection leading to necrotizing fasciitis. Proc Natl Acad Sci USA. (2016) 113:722–7. doi: 10.1073/pnas.1523817113
7. Patil, SM, and Hilker, ED. Aeromonas hydrophila community-acquired bacterial pneumonia with septic shock in a chronic lymphocytic leukemia patient due to absolute neutropenia and lymphopenia. Cureus. (2022) 14:e23345. doi: 10.7759/cureus.23345
8. Janda, JM, and Abbott, SL. The genus Aeromonas: taxonomy, pathogenicity, and infection. Clin Microbiol Rev. (2010) 23:35–73. doi: 10.1128/CMR.00039-09
9. Esteve, C, Alcaide, E, and Blasco, MD. Aeromonas hydrophila subsp. dhakensis isolated from feces, water and fish in Mediterranean Spain. Microbes Environ. (2012) 27:367–73. doi: 10.1264/jsme2.ME12009
10. Janda, JM. Recent advances in the study of the taxonomy, pathogenicity, and infectious syndromes associated with the genus Aeromonas. Clin Microbiol Rev. (1991) 4:397–410. doi: 10.1128/CMR.4.4.397
11. Figueras, MJ, Alperi, A, Saavedra, MJ, Ko, WC, Gonzalo, N, Navarro, M, et al. Clinical relevance of the recently described species Aeromonas aquariorum. J Clin Microbiol. (2009) 47:3742–6. doi: 10.1128/JCM.02216-08
12. Huys, G, Kämpfer, P, Albert, MJ, Kühn, I, Denys, R, and Swings, J. Aeromonas hydrophila subsp. dhakensis subsp. nov., isolated from children with diarrhoea in Bangladesh, and extended description of Aeromonas hydrophila subsp. hydrophila (Chester 1901) Stanier 1943 (approved lists 1980). Int J Syst Evol Microbiol. (2002) 52:705–12. doi: 10.1099/00207713-52-3-705
13. Beaz-Hidalgo, R, Martínez-Murcia, A, and Figueras, MJ. Reclassification of Aeromonas hydrophila subsp. dhakensis Huys et al. 2002 and Aeromonas aquariorum Martínez-Murcia et al. 2008 as Aeromonas dhakensis sp. nov. comb nov. and emendation of the species Aeromonas hydrophila. Syst Appl Microbiol. (2013) 36:171–6. doi: 10.1016/j.syapm.2012.12.007
14. Chen, PL, Wu, CJ, Tsai, PJ, Tang, HJ, Chuang, YC, Lee, NY, et al. Virulence diversity among bacteremic Aeromonas isolates: ex vivo, animal, and clinical evidences. PLoS One. (2014) 9:e111213. doi: 10.1371/journal.pone.0111213
15. Rasmussen-Ivey, CR, Figueras, MJ, McGarey, D, and Liles, MR. Virulence factors of Aeromonas hydrophila: in the wake of reclassification. Front Microbiol. (2016) 7:1337. doi: 10.3389/fmicb.2016.01337
16. Tomás, JM. The main Aeromonas pathogenic factors. ISRN Microbiol. (2012) 2012:256261–22. doi: 10.5402/2012/256261
17. Kitagawa, H, Ohge, H, Yu, L, Kayama, S, Hara, T, Kashiyama, S, et al. Aeromonas dhakensis is not a rare cause of Aeromonas bacteremia in Hiroshima, Japan. J Infect Chemother. (2020) 26:316–20. doi: 10.1016/j.jiac.2019.08.020
18. Chen, PL, Wu, CJ, Chen, CS, Tsai, PJ, Tang, HJ, and Ko, WC. A comparative study of clinical Aeromonas dhakensis and Aeromonas hydrophila isolates in southern Taiwan: A. dhakensis is more predominant and virulent. Clin Microbiol Infect. (2014) 20:O428–34. doi: 10.1111/1469-0691.12456
19. Wu, CJ, Chen, PL, Wu, JJ, Yan, JJ, Lee, CC, Lee, HC, et al. Distribution and phenotypic and genotypic detection of a metallo-β-lactamase, CphA, among bacteraemic Aeromonas isolates. J Med Microbiol. (2012) 61:712–9. doi: 10.1099/jmm.0.038323-0
Keywords: Aeromonas dhakensis , severe pneumonia, atrial septal defect, mNGS, ECMO
Citation: Sha J, Shao J, Lu S, Zhang M, Gu C, Deng Y, Zhang J and Feng Y (2024) A case report of severe pneumonia caused by Aeromonas dhakensis infection complicated with severe atrial septal defect. Front. Med. 11:1476864. doi: 10.3389/fmed.2024.1476864
Edited by:
Karolina Henryka Czarnecka-Chrebelska, Medical University of Lodz, PolandReviewed by:
Robson Leão, Rio de Janeiro State University, BrazilPo Lin Chen, National Cheng Kung University, Taiwan
Copyright © 2024 Sha, Shao, Lu, Zhang, Gu, Deng, Zhang and Feng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yufeng Feng, amlxaW1hb2tlQDE2My5jb20=
 Jun Sha
Jun Sha Jie Shao1
Jie Shao1