- National Clinical Research Center for Ocular Diseases, Eye Hospital, Wenzhou Medical University, Wenzhou, China
Background: While several studies have noted a higher SII correlates with multiple diseases, research on the association between SII and cataract remains limited. Our cross-sectional study seeks to examine the association between SII and cataract among outpatient US adults.
Methods: This compensatory cross-sectional study utilized NHANES data from 1999 to 2008 cycles, conducting sample-weighted multivariate logistic regression and stratified analysis of subgroups.
Results: Among 11,205 adults included in this study (5,571 [46.2%] male; 5,634 [53.8%] female), 2,131 (15.2%) had cataract and 9,074 (84.8%) did not have cataract. A fully adjusted model showed that SII higher than 500 × 109/L was positively correlated with an increased risk of cataracts among women (OR, 1.27; 95% CI, 1.02–1.59) (p = 0.036). However, no difference was found in the men subgroup, and there was no significant interaction between SII and sex.
Conclusion: Our results indicated that a SII higher than 500 × 109/L was positively correlated with an increased risk of cataracts in women. This study is the first to specifically investigate the impact of a high SII on cataract risk in outpatient adults in the United States. By effectively addressing inflammation, it is possible to mitigate cataract progression and significantly enhance patient outcomes.
1 Introduction
Cataract continues to pose a significant global concern for vision impairment and blindness, especially among the elderly population (1–3). In the United States, its prevalence rises from 24.4% in individuals aged 40 and above to over 50% in those aged 75 and older, predominantly due to aging (4). Risk factors such as smoking and alcohol contribute to its development (5–7). Cataract surgery is highly effective, but accessibility is often limited by economic challenges. This issue is particularly pronounced in developing countries (8). Addressing these modifiable risk factors is essential for reducing the health and socioeconomic burden of cataracts.
Research indicates that the SII is associated with pseudophakic cystoid macular edema (PCME) in patients without risk factors after uneventful phacoemulsification cataract surgery, suggesting that SII could serve as a predictive biomarker for PCME, thereby enhancing clinical assessment and risk stratification (9). Similarly, a study in Suzhou, China, found that while SII does not directly correlate with presenting visual impairment (PVI), uncorrected refractive error and cataracts remain the leading causes of PVI, with significant associations linked to older age and elevated fasting blood glucose (10). Furthermore, evidence from another study shows that a pro-inflammatory diet, as quantified by the dietary inflammatory index (DII), is associated with an increased risk of cataract and age-related macular degeneration (AMD), with the neutrophil-lymphocyte ratio (NLR) and other inflammatory markers mediating these effects (11).
In the human body’s systemic inflammatory system, immune cells play a crucial role in various diseases. Researchers have found that the combined counts of lymphocytes, neutrophils, and platelets in peripheral blood can provide a more accurate predictor of inflammatory status. Specifically, the SII is derived from these three types of circulating immune cells (12, 13). Recent studies suggest that systemic inflammation may contribute to photoreceptor cell death in patients with Retinitis Pigmentosa (RP). The NLR, calculated by dividing the total count of neutrophils by that of lymphocytes in a peripheral blood sample, has been proposed as a marker of systemic inflammation and a poor prognostic indicator for various chronic diseases. Additionally, the NLR is emerging as a potential inflammatory marker for several ocular conditions, including keratoconus, retinal vein occlusion (RVO), AMD, and dry eye (14). Cataracts, characterized by the clouding of the eye’s lens, lead to progressive visual impairment and are a major cause of blindness globally. The core features of cataracts include lens opacity, reduced light transmission, and compromised visual acuity. Inflammation and immune responses have been increasingly recognized as significant factors in cataract development. Chronic inflammation can induce oxidative stress and promote lens protein modification, which contributes to lens opacity (15). Additionally, immune responses involving cytokines and inflammatory mediators have been implicated in the cataractogenesis process. Given these insights, the SII, which integrates lymphocyte, neutrophil, and platelet counts, may offer a valuable tool for assessing systemic inflammation’s role in cataract formation.
The SII was initially identified as a prognostic marker for conditions such as kidney stones and hepatic steatosis (16, 17). However, its impact on cataracts within the outpatient U.S. population and its prognostic value for cataracts are not yet well established. In this cross-sectional study utilizing NHANES data from 1999 to 2008 cycles, we aimed to investigate the association between SII and cataract among outpatient US adults.
2 Methods
2.1 Data sources
Information on cataract was only provided in the NHANES 1999–2004 cycles for individuals aged 20 years or older and in the 2005–2008 cycles for individuals aged 50 years or older. In this cross-sectional study, deidentified data for participants aged 50 years or older were extracted from the NHANES 1999–2008 cycles. This study followed the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) reporting guideline. Data were analyzed from March to July 2024.
2.2 Study design and population
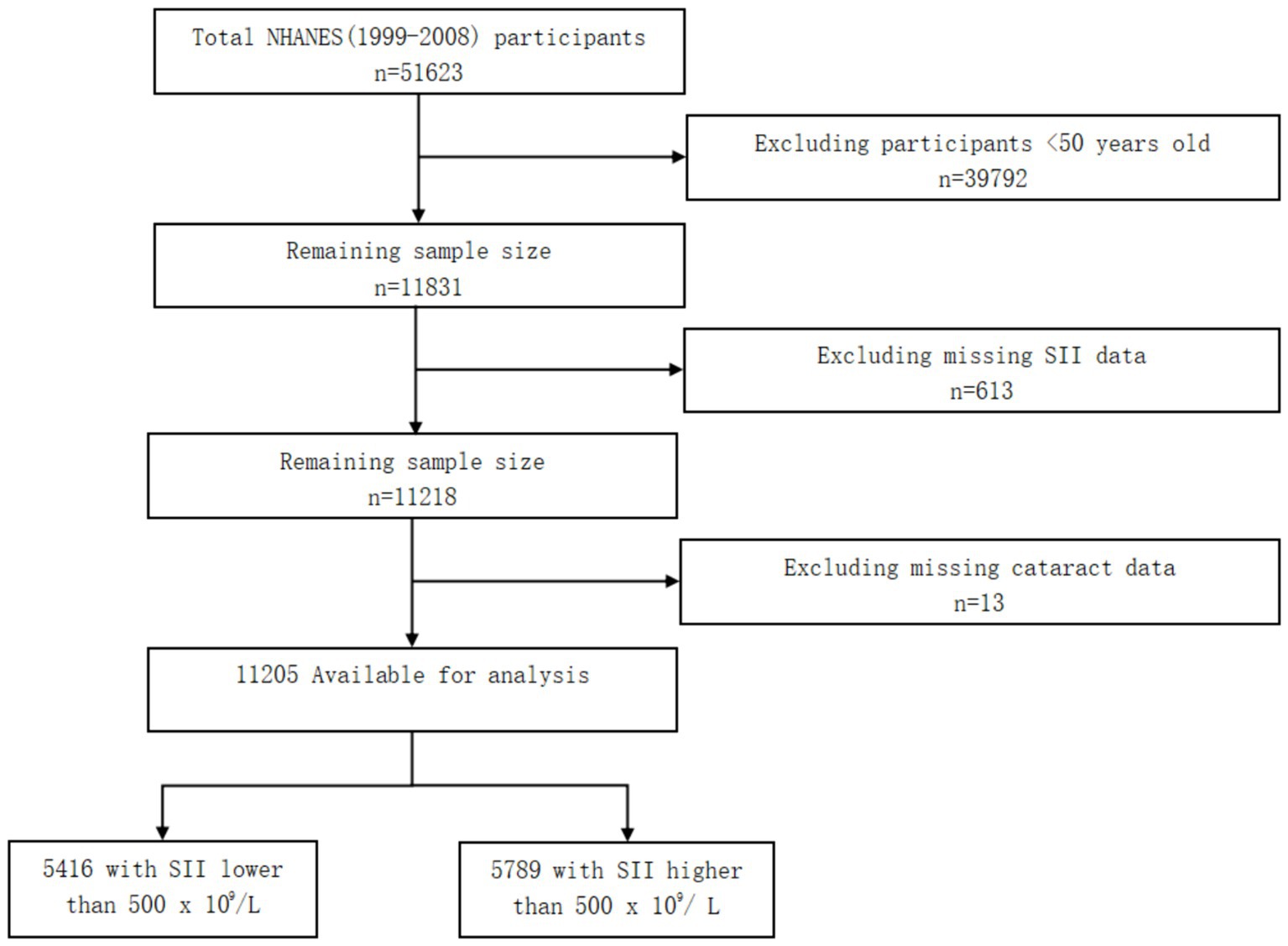
Because information on cataract was only provided in the NHANES 1999–2008 cycles for adults aged 50 years or older, we selected a total of 11,831 adults within this age range. Moreover, we excluded 613 participants who had missing SII data, 13 participants who had missing cataract data. Finally, a total of 11,205 participants were involved. Of the 11,205 participants, there were 5,416 participants with SII lower than 500 × 109/L and 5,789 participants with SII higher than 500 × 109/L (Figure 1).
2.3 Assessment of SII and cataract
SII was defined as (platelet x neutrophil)/lymphocyte (18–20). Throughout the analysis, an SII cutoff of 500 × 109/L was applied.
Cataract diagnosis was based on participants’ self-report of having undergone cataract surgery, as indicated by a positive response to the question “Have you ever had a cataract operation?” (VIQ070:1999–2002; VIQ071:2003–2008), with response options of “yes” or “no.” A positive response was considered indicative of a cataract (4, 21).
2.4 Covariates
According to previous studies concerning cataract, potential confounding factors studied in the current work included: sociodemographic variables (age, sex, race and ethnicity, family income, educational level, and marital status), NHANES cycles, BMI, lifestyle factors (alcohol drinking status, smoking status), and comorbidities (including hypertension, hyperlipidemia, and diabetes mellitus) (4, 21). Sociodemographic variables, lifestyle factors, and comorbidities were drawn from self-reported questionnaires.
2.5 Statistical analysis
Our analyses utilizing NHANES data from 1999 to 2008 cycles considered the complex sampling design and sampling weights and the sampling weight was calculated using the following formula: fasting subsample 10-year mobile examination center (MEC) weight = fasting subsample 2-year MEC weight/5 (22, 23). Moreover, we used quartiles to describe the continuous variables with non-normal distribution and described the categorical variables using unweighted frequency and weighted percentage in this cross-sectional study.
If the VIF was 5 or higher, it meant there was multicollinearity present (22). To investigate the association between SII and cataract, logistic regression models were established. Model 1 was adjusted for sociodemographic variables and NHANES cycles. Model 2 was adjusted for sociodemographic variables, NHANES cycles, BMI, lifestyle factors (alcohol drinking status, smoking status), and comorbidities (including hypertension, hyperlipidemia, and diabetes mellitus). Finally, we conducted a subgroup analysis on gender to assess the possible influence of sex on the association between SII and cataract.
We used R for all the statistical analyses and we considered a significance level of p < 0.05 to show that the results were statistically significant.
3 Results
There were 11,205 participants included in this study. 39,792 participants <50 years old were excluded, and 613 participants were excluded for missing SII data. After removing 13 participants missing cataract data, 11,205 participants were finally enrolled. Participants with SII levels higher than 500 × 109/L were found to have a higher prevalence of being non-Hispanic White compared to those with SII levels lower than 500 × 109/L (p < 0.001). Additionally, we have noted that individuals with higher SII levels are more likely to be current smokers (defined as having smoked at least 100 cigarettes in their lifetime and continuing to smoke), with statistical significance (p < 0.001) (see Table 1).
As shown in Table 2, logistic regression analysis found no significant difference between SII and cataract after adjusting for covariates in the whole population. In the women subgroup, the univariate and multivariate analyses demonstrated high SII over 500 × 109/L was associated with a higher risk of cataract in the crude model (OR, 1.40; 95% CI, 1.18–1.66; p < 0.001) and model 1 (OR, 1.27; 95% CI, 1.03–1.56; p = 0.024). After adjusting for all confounding factors, high SII over 500 × 109/L was still positively associated with cataract among women (OR, 1.27; 95% CI, 1.02–1.59; p = 0.036). No difference was found in the men subgroup, and there was no significant interaction between SII and sex (P for interaction = 0.198). Because the percentage of missing data was small for any variable in this cross-sectional study, no imputation method was used.
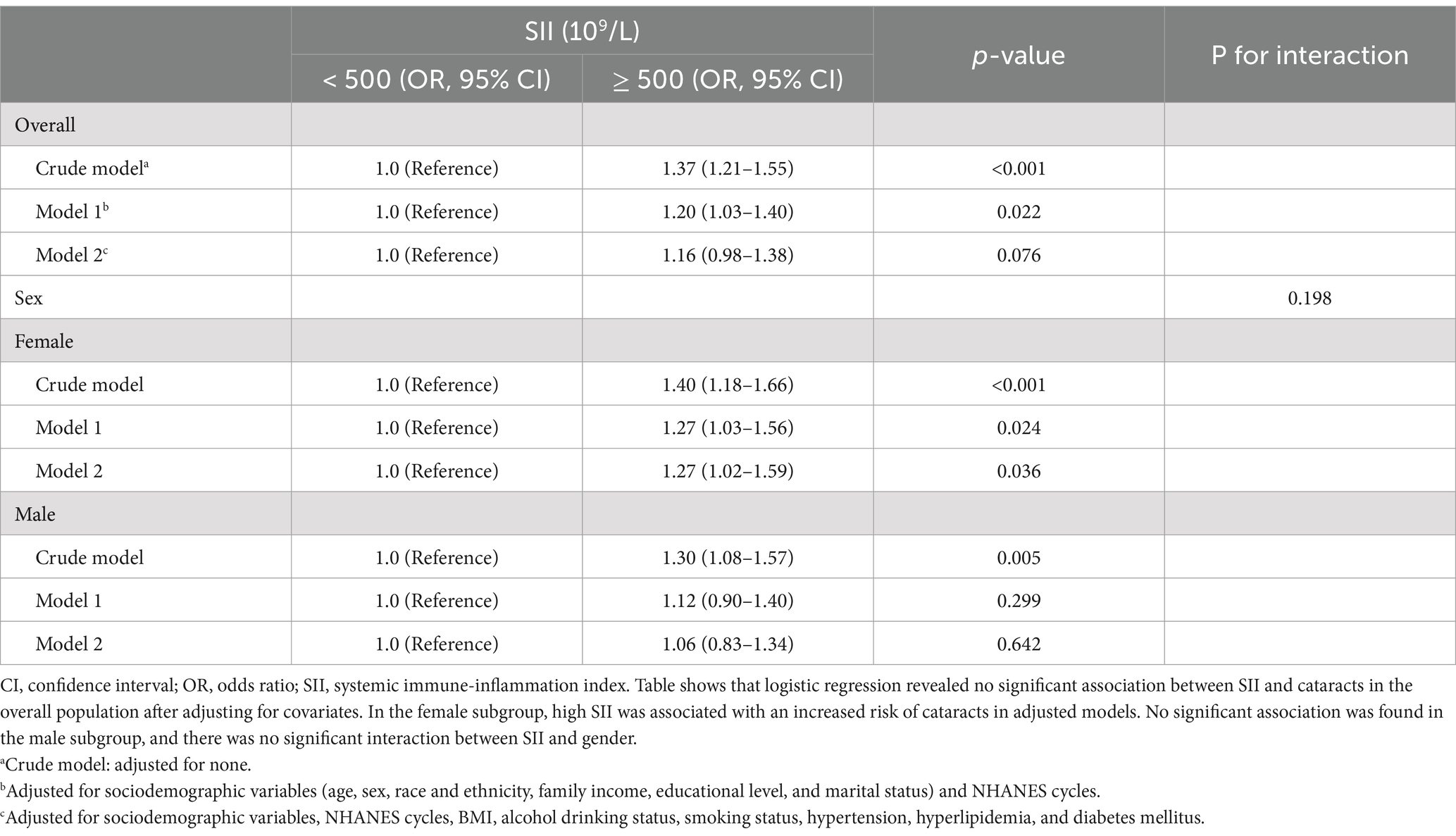
Table 2. Univariate and multivariate analyses by the activity-stratified logistic regression model, weighted.
4 Discussion
Cataract, a common cause of vision impairment worldwide, involves clouding of the eye’s lens. Apart from aging, research suggests a connection between cataract development and chronic inflammation (11). Studies have linked markers like C-reactive protein (CRP) and interleukin 6 (IL-6) to cataract risk, indicating their role in lens opacification (24). Inflammation and oxidative stress, typical in chronic inflammation, are positively associated with cataract formation (25–28). Conditions like systemic lupus erythematosus, linked to increased cataract risk, exhibit inflammatory processes that may contribute to cataract formation (29). Research has shown that cataracts are more prevalent in women than in men, with females exhibiting higher rates of lens opacities, especially cortical cataracts (30–32). This disparity is not solely due to higher cataract extraction rates among women in Western countries, and there is currently no definitive evidence linking lifestyle-related factors to this gender difference.
SII was calculated by neutrophils, lymphocytes, and platelets. It reflects the inflammatory reactions and may be a useful diagnostic biomarker for systemic inflammatory activity. Previous studies have found that the SII is associated with PCME in patients without risk factors following uneventful phacoemulsification cataract surgery, suggesting that SII could serve as a predictive biomarker for PCME (9). Additionally, research shows that a pro-inflammatory diet, as measured by the DII, is linked to an increased risk of cataract and AMD, with inflammatory markers such as the NLR mediating these associations (11). However, there is currently a gap in large-scale studies directly investigating the relationship between SII and cataracts. Our results indicated that a SII higher than 500 × 109/L was positively correlated with an increased risk of cataracts in women. Therefore, SII with a non-intrusive methodology and low cost can be identified as a biomarker for cataract among women.
Our study examined the link between SII and cataracts specifically in women and found that elevated SII levels were associated with cataracts. This suggests that anti-inflammatory therapies or lifestyle changes could be beneficial for those with chronic inflammation. The evidence highlights the need for further research to better understand this relationship and improve cataract prevention and treatment. Additionally, our findings indicate that higher SII levels are associated with current smoking, suggesting that smoking may contribute to elevated systemic inflammation. This underscores the importance of smoking cessation programs, as reducing smoking could potentially lower inflammation and mitigate associated health risks.
Our research employed a robust methodology with a large and diverse sample size drawn from NHANES data to investigate the relationship between SII and cataracts. By conducting subgroup analyses and carefully adjusting for confounding variables, we minimized bias and increased the statistical accuracy of our findings. This study contributes valuable insights to the existing knowledge base and sheds light on the correlation between elevated SII levels and cataract risk among adult outpatients in the United States.
Based on our findings, SII could be integrated into a broader risk assessment for cataracts, particularly for higher-risk populations. Routine screening might include measuring SII levels along with other established risk factors. For individuals with elevated SII, interventions could involve lifestyle changes such as improved diet, increased physical activity, and smoking cessation, as these can help manage inflammation and oxidative stress, which are modifiable risk factors for cataracts. Enhanced surveillance through more frequent eye examinations may also be recommended for those with high SII to facilitate early detection and management. Future research should investigate whether anti-inflammatory or antioxidant therapies could benefit individuals with elevated SII.
As a cross-sectional study, our ability to establish causal relationships is limited. To address this, future research should explore longitudinal or experimental designs. Additionally, we cannot fully eliminate the potential impact of residual confounding from unmeasured variables, including other inflammatory markers, lifestyle factors such as diet and physical activity, and exposure to environmental toxins. Although NHANES data provide national representativeness, the generalizability of our findings to other countries remains uncertain. Further research is needed to better understand the complexities of the link between chronic inflammation and cataracts, which could lead to innovative preventive measures and treatment options in cataract management.
5 Conclusion
In this cross-sectional study involving 11,205 participants from a large nationally representative survey, it was observed that a high SII over 500 × 109/L was positively associated with cataract development among women, even after adjusting for confounding factors. This study contributes valuable insights into the relationship between high SII levels and cataract risk in outpatient adults in the United States. Moving forward, larger prospective cohorts are needed to validate these results, emphasizing the importance of addressing inflammation to mitigate cataract progression and improve patient outcomes.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found at: https://www.cdc.gov/nchs/nhanes/index.htm.
Ethics statement
The studies involving humans were approved by The NCHS research ethics review board approved the NHANES study protocol, and participants provided written informed consent at enrollment. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JH: Writing – review & editing, Writing – original draft. HW: Writing – review & editing, Writing – original draft. FY: Writing – review & editing, Writing – original draft. FW: Writing – review & editing, Writing – original draft. CH: Writing – review & editing, Writing – original draft. XZ: Writing – review & editing, Writing – original draft. YH: Writing – review & editing, Writing – original draft. HF: Writing – review & editing, Writing – original draft. HX: Writing – review & editing, Writing – original draft. RL: Writing – review & editing, Writing – original draft. DC: Writing – review & editing, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by the Natural Science Foundation Project of Zhejiang Province (LWY20H120001), the Health Science and Technology Project of Zhejiang Province (2022PY073), Wenzhou Basic Medical Health Science and Technology Project (Y2020360).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Liu, Y-C, Wilkins, M, Kim, T, Malyugin, B, and Mehta, JS. Cataracts. Lancet Lond Engl. (2017) 390:600–12. doi: 10.1016/S0140-6736(17)30544-5
2. Delbarre, M, and Froussart-Maille, F. Signs, symptoms, and clinical forms of cataract in adults. J Fr Ophtalmol. (2020) 43:653–9. doi: 10.1016/j.jfo.2019.11.009
3. Lee, CM, and Afshari, NA. The global state of cataract blindness. Curr Opin Ophthalmol. (2017) 28:98–103. doi: 10.1097/ICU.0000000000000340
4. Zhang, Y, Zhou, J, Shen, W, Grzybowski, A, Jin, K, and Ye, J. Association between dietary inflammation index and cataract: a population-based study from NHANES 2005-2008. Front Nutr. (2024) 11:1379317. doi: 10.3389/fnut.2024.1379317
5. Ang, MJ, and Afshari, NA. Cataract and systemic disease: a review. Clin Experiment Ophthalmol. (2021) 49:118–27. doi: 10.1111/ceo.13892
6. Fukai, K, Terauchi, R, Furuya, Y, Sano, K, Nakazawa, S, Kojimahara, N, et al. Alcohol use patterns and risk of incident cataract surgery: a large scale case-control study in Japan. Sci Rep. (2022) 12:20142. doi: 10.1038/s41598-022-24465-2
7. Goutham, G, Manikandan, R, Beulaja, M, Thiagarajan, R, Arulvasu, C, Arumugam, M, et al. A focus on resveratrol and ocular problems, especially cataract: from chemistry to medical uses and clinical relevance. Biomed Pharmacother Biomedecine Pharmacother. (2017) 86:232–41. doi: 10.1016/j.biopha.2016.11.141
8. Lam, D, Rao, SK, Ratra, V, Liu, Y, Mitchell, P, King, J, et al. Cataract. Nat Rev Dis Primer. (2015) 1:15014. doi: 10.1038/nrdp.2015.14
9. Kocamış, Sİ, Boz, AAE, and Özdemir, İ. Systemic immune-inflammation index could be associated with pseudophakic cystoid macular edema after an uneventful phacoemulsification surgery in patients without risk factors. BMC Ophthalmol. (2022) 22:378. doi: 10.1186/s12886-022-02606-5
10. Sun, R, Huang, D, Liu, Z, Zhu, T, Gu, Z, Ma, G, et al. Prevalence, causes, and risk factors of presenting visual impairment and presenting blindness in adults presenting to an examination Center in Suzhou, China. J Ophthalmol. (2022) 2022:1–9. doi: 10.1155/2022/2885738
11. Vergroesen, JE, Thee, EF, de Crom, TOE, Kiefte-de Jong, JC, Meester-Smoor, MA, Voortman, T, et al. The inflammatory potential of diet is associated with the risk of age-related eye diseases. Clin Nutr Edinb Scotl. (2023) 42:2404–13. doi: 10.1016/j.clnu.2023.10.008
12. Mahemuti, N, Jing, X, Zhang, N, Liu, C, Li, C, Cui, Z, et al. Association between systemic immunity-inflammation index and hyperlipidemia: a population-based study from the NHANES (2015–2020). Nutrients. (2023) 15:1177. doi: 10.3390/nu15051177
13. Zhao, Y, Shao, W, Zhu, Q, Zhang, R, Sun, T, Wang, B, et al. Association between systemic immune-inflammation index and metabolic syndrome and its components: results from the National Health and nutrition examination survey 2011-2016. J Transl Med. (2023) 21:691. doi: 10.1186/s12967-023-04491-y
14. He, M, Wu, T, Zhang, L, Ye, W, Ma, J, Zhao, C, et al. Correlation between neutrophil-to-lymphocyte ratio and clinical manifestations and complications of retinitis pigmentosa. Acta Ophthalmol. (2022) 100:e278–87. doi: 10.1111/aos.14880
15. Lim, JC, Caballero Arredondo, M, Braakhuis, AJ, and Donaldson, PJ. Vitamin C and the Lens: new insights into delaying the onset of cataract. Nutrients. (2020) 12:3142. doi: 10.3390/nu12103142
16. Xie, R, Xiao, M, Li, L, Ma, N, Liu, M, Huang, X, et al. Association between SII and hepatic steatosis and liver fibrosis: a population-based study. Front Immunol. (2022) 13:925690. doi: 10.3389/fimmu.2022.925690
17. di, X, Liu, S, Xiang, L, and Jin, X. Association between the systemic immune-inflammation index and kidney stone: a cross-sectional study of NHANES 2007-2018. Front Immunol. (2023) 14:1116224. doi: 10.3389/fimmu.2023.1116224
18. Ding, Q, Li, X, Lin, L, Xie, X, Jing, W, Chen, X, et al. Association between systemic immunity-inflammation index and psoriasis among outpatient US adults. Front Immunol. (2024) 15:1368727. doi: 10.3389/fimmu.2024.1368727
19. Liu, B, Wang, J, Li, Y-Y, Li, KP, and Zhang, Q. The association between systemic immune-inflammation index and rheumatoid arthritis: evidence from NHANES 1999-2018. Arthritis Res Ther. (2023) 25:34. doi: 10.1186/s13075-023-03018-6
20. Song, Y, Guo, W, Li, Z, Guo, D, Li, Z, and Li, Y. Systemic immune-inflammation index is associated with hepatic steatosis: evidence from NHANES 2015-2018. Front Immunol. (2022) 13:1058779. doi: 10.3389/fimmu.2022.1058779
21. Zhou, J, Lou, L, Jin, K, and Ye, J. Association between healthy eating Index-2015 and age-related cataract in American adults: a cross-sectional study of NHANES 2005-2008. Nutrients. (2022) 15:98. doi: 10.3390/nu15010098
22. Ruan, Z, Lu, T, Chen, Y, Yuan, M, Yu, H, Liu, R, et al. Association between psoriasis and nonalcoholic fatty liver disease among outpatient US adults. JAMA Dermatol. (2022) 158:745–53. doi: 10.1001/jamadermatol.2022.1609
23. Ruan, Z, Xie, X, Yu, H, Liu, R, Jing, W, and Lu, T. Association between dietary inflammation and erectile dysfunction among US adults: a cross-sectional analysis of the National Health and nutrition examination survey 2001-2004. Front Nutr. (2022) 9:930272. doi: 10.3389/fnut.2022.930272
24. Sutkowy, P, Lesiewska, H, Woźniak, A, and Malukiewicz, G. Inflammation-involved proteins in blood serum of cataract patients-a preliminary study. Biomedicines. (2023) 11:2607. doi: 10.3390/biomedicines11102607
25. Ahmad, A, and Ahsan, H. Biomarkers of inflammation and oxidative stress in ophthalmic disorders. J Immunoassay Immunochem. (2020) 41:257–71. doi: 10.1080/15321819.2020.1726774
26. Selin, JZ, Lindblad, BE, Rautiainen, S, Michaëlsson, K, Morgenstern, R, Bottai, M, et al. Are increased levels of systemic oxidative stress and inflammation associated with age-related cataract? Antioxid Redox Signal. (2014) 21:700–4. doi: 10.1089/ars.2014.5853
27. Honisch, C, Rodella, U, Gatto, C, Ruzza, P, Tóthová, JD, et al. Oxidative stress and antioxidant-based interventional medicine in ophthalmology. Pharmaceuticals. (2023) 16:1146. doi: 10.3390/ph16081146
28. Tanito, M. Reported evidence of vitamin E protection against cataract and glaucoma. Free Radic Biol Med. (2021) 177:100–19. doi: 10.1016/j.freeradbiomed.2021.10.027
29. Dammacco, R. Systemic lupus erythematosus and ocular involvement: an overview. Clin Exp Med. (2018) 18:135–49. doi: 10.1007/s10238-017-0479-9
30. Zetterberg, M, and Celojevic, D. Gender and cataract – the role of estrogen. Curr Eye Res. (2015) 40:176–90. doi: 10.3109/02713683.2014.898774
31. Kanakamedala, A, Go, JA, Wendt, S, Ugoh, P, Khan, M, and al-Mohtaseb, Z. Systemic and ocular comorbidities of black, Hispanic, and white women with cataracts. J Women's Health. (2002) 31:117–24. doi: 10.1089/jwh.2020.8793
Keywords: cataract, systemic immune-inflammation index, cross-sectional study, National Health and Nutrition Examination Survey, outpatient US adults
Citation: Huang J, Wu H, Yu F, Wu F, Hang C, Zhang X, Hao Y, Fu H, Xu H, Li R and Chen D (2024) Association between systemic immune-inflammation index and cataract among outpatient US adults. Front. Med. 11:1469200. doi: 10.3389/fmed.2024.1469200
Edited by:
Wensi Tao, University of Miami Health System, United StatesReviewed by:
Nai-Kei Wong, Shantou University, ChinaYuan Liu, University of Miami Health System, United States
Copyright © 2024 Huang, Wu, Yu, Wu, Hang, Zhang, Hao, Fu, Xu, Li and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ding Chen, bmVjb2RpbmdAMTI2LmNvbQ==; Rong Li, MTM4NjgzMTUxMzZAbWFpbC5leWUuYWMuY24=
†These authors have contributed equally to this work
 Jin Huang†
Jin Huang† Hongjiang Wu
Hongjiang Wu Fangkun Wu
Fangkun Wu Ding Chen
Ding Chen