- 1Faculty of Pharmaceutical Sciences, University of British Columbia, Vancouver, BC, Canada
- 2Faculty of Medicine, University of British Columbia, Vancouver, BC, Canada
- 3Centre for Advancing Health Outcomes, Providence Health Care Research Institute, Vancouver, BC, Canada
- 4Edwin S.H. Leong Centre for Healthy Aging, Faculty of Medicine, University of British Columbia, Vancouver, BC, Canada
Background: General medical practitioners are responsible for promoting and prescribing lifestyle modification and serve as role models for healthy behaviors. We aimed to assess self-reported knowledge, adherence, barriers and time spent on all recommended health behaviors among medical students.
Methods: A cross-sectional online survey of eight behavioral domains among undergraduate medical students in The University of British Columbia, Canada, was analysed using descriptive statistics and visual display.
Results: Between March and April 2023, 137 medical students participated in the survey (74% female). Over 80% had knowledge of five health behavior recommendations, but lacked knowledge of specific dietary recommendations in particular. Over 60% reported meeting guideline-recommended levels for tobacco, weekly alcohol, daily alcohol (females only), and physical activity (males only). Large gaps existed between knowledge and adherence for physical activity, sleep, sedentariness, screen time, and dietary recommendations. Sex differences in knowledge and adherence to recommended health behaviors were identified. Time spent on wellness focused on sleep (47–49 h/week), diet (9.6 h/week), exercise (5.8 h/week), and hobbies (6.1 h/week). Forgetting recommendations (69% of females, 71% of males), and lack of time (72% of females, 52% of males) were principal barriers to knowledge and adherence.
Conclusion: Most medical students in Western Canada reported not meeting multiple recommended health behaviors. Time was the largest barrier to adherence and free time was spent on sleep. Medical education may require protected time and dedicated content for health behaviors to ensure future physicians can be role models of health promotion for patients.
Introduction
It is widely accepted that adherence to health recommendations is essential for the prevention and management of diseases. Medical professionals serve as role models for healthful behaviors to their patients, with most patients expecting to be prescribed health behavior recommendations (“lifestyle modification”) by their physicians (1–5). Thus, students of medicine are expected to both know and adhere to key health recommendations through the achievement of physician competencies set by the Royal College of Physicians and Surgeons: namely, professional competency 4 (demonstrate a commitment to physician health and wellbeing to foster optimal patient care), leader competency 2 (engage in the stewardship of health care resources) and medical expert competency 1 (apply knowledge from the social/behavioral sciences) and 2 (select appropriate cost-effective interventions for health promotion in patient care) (6).
Current medical curriculum content on recommended behaviors for health promotion and disease prevention is, however, limited and patchy. There is inadequate coverage around Public Health and Preventive Medicine as important areas of knowledge for physicians, and the medical curriculum does not emphasize the scope, importance, or sources of public health recommendations in Canada. Instead, the syllabus introduces weekly disease themes wherein specific lifestyle modifications are mentioned piecemeal. For example, dietary recommendations for sodium intake are introduced during weeks focused on hypertension and heart failure, yet sodium is also relevant for kidney care and overall health. Similarly, recommended daily water intake is mentioned during a week focused on acute kidney injury but drinking adequate water is vital to many bodily functions including getting rid of wastes, protecting joints and organs and maintaining body temperature. Moderate intensity exercise is highlighted during weeks focused on hypertension, type II diabetes, and cardiovascular disease, although exercise is also important for sleep, mood, cancer, bone health and obesity. Since the medical education program structure teaches selected health behavior recommendations exclusively through a patient pathology lens, it lacks a holistic health maintenance framework to educate medical students on the comprehensive set of health behavior recommendations from Health Canada. In addition, the medical program structure provides little to no personal time for extracurricular activities of medical students including self-care and health-promoting behaviors; this deficit is highlighted by the rising prevalence of burnout among Canadian physicians and medical residents from a third in 2018 to more than half in 2021 (7, 8). It is a public health and occupational imperative that medical students learn about and develop protective and sustainable health behaviors for their future health, the sustainability of the healthcare system and most importantly for their role modelling for patients.
Globally, a body of literature suggests that a significant proportion of medical students fail to meet important health behavior recommendations. For example, one study showed that about a quarter of all medical students surveyed reporting sleeping less than recommended levels (9), and multiple studies reported that a majority of medical students did not achieve the evidence-based recommendations for sleep (10, 11). Several studies have also shown the high prevalence of tobacco use and alcohol consumption among medical students, contrary to health guidelines (12–14). Medical students in the US, however, appear to meet or exceed recommendations for physical activity (15–19). One study in Canada also showed that medical students engaged in more strenuous physical activity when compared to the general population (20). Despite some research on this topic, no research has comprehensively assessed knowledge, barriers, adherence and time-burden of all health-promoting behaviors, including dietary recommendations, among medical students. Prevalence studies on specific behaviors also rarely consider the reasons medical students fail to meet health guidelines even when students possess clear knowledge of recommended health behaviors.
In a departure from literature, this study aimed to fill a knowledge gap by comprehensively assessing self-reported knowledge, adherence, barriers, and time spent on all recommended health behaviors among medical students in Western Canada. This research expands current evidence on the prevalence of all health behaviors among physicians-in-training and adds new data on the estimated time burden and barriers of adherence.
Materials and methods
Subjects and data collection
A cross-sectional survey was administered between March and April 2023 to University of British Columbia (UBC) medical students in all 4 years of the undergraduate Medical Program from the classes of 2023–2026 across all Medical Program sites of UBC (n = 1,152): the medical student population is 59% female and 80% aged 21–26 years. The online semi-structured survey collected anonymous data from 137 respondents through the institutionally approved Qualtrics platform, and included predetermined and free-text response categories. The questionnaire administered 30 items across demographics, self-reported knowledge of recommendations for personal application, achievement of recommendations, and hours per week spent on 8 behavioral domains (Supplementary Methods). Health behavior guidelines often vary by individual, depending on factors such as age (as with sleep) and body mass (as with water) (21, 22). For this reason, students’ knowledge of their health behavior recommendations could not be directly tested. Instead, students were asked to self-report whether they felt they knew how each recommendation applied to them. The questionnaire was developed based on clinical guidelines and government websites with health behavior recommendations (e.g., https://www.healthlinkbc.ca/), and was piloted with 2 medical students and 1 health professional known to the research team. This research was approved for minimal risk by the UBC Behavioral Research Ethics Board (H16-00044), and written informed consent was obtained from survey participants.
Data cleaning and analysis
Responses were excluded if participants answered fewer than four survey questions beyond the demographics section (n = 20), resulting in a final sample size of 117 for analysis (about 10% of the medical student population in the province; Supplementary Figure S1). Open-text data were coded for quantitative content analysis and frequencies (proportions) were used to analyze knowledge and adherence. Surveys were analyzed in Microsoft Excel v16.72. Responses to the hours per week section were analyzed using MATLAB vR2022b. The frequency of the knowledge and achievement of barriers was summarised in bar graphs by sex; results for average hours per week spent on a recommended health behavior were reported by medical year.
Results
The majority of survey respondents were medical students who self-identified as female (74%), with an even distribution across medical year 1 (19%), year 2 (30%), year 3 (32%) and year 4 (20%). Most survey respondents were from the Vancouver Fraser Site (39%) or the Southern Site (38%), with respondents from the Interior Site (9%) and Northern Site (15%) accounting for around a fifth of all respondents (Supplementary Table S1).
The prevalence of self-reported knowledge of health behavior recommendations varied widely by behavior, with similar proportions of male and female medical students reporting having knowledge of nearly two-thirds of the measured behaviors (Figure 1). More males than females skipped questions about knowledge of physical activity, sleep, sedentariness and screen time. Most respondents reported having knowledge of recommendations for weekly alcohol (96% of females, 97% of males), physical activity (94% of females, 90% of males), daily alcohol (88% of females, 84% of males), tobacco (93% of females, 84% of males), sleep (92% of females, 84% of males), and Canada’s Food Guide (86% of females, 81% of males). Some notable sex/gender differences were seen for specific dietary recommendations. A majority of female medical students reported knowing the recommendation for Vitamin D (80%), but less than half of male medical students reported knowing the recommendation (42%). Most of the female and male medical students reported having knowledge of recommended daily water intake (72% of females, 71% of males), more female (69%) than male (52%) medical students reported knowing about sodium recommendations. Less than half of respondents reported knowing the recommendations for caffeine and added sugar, again with notable sex/gender differences: 45% of males reported knowing the recommendation for added sugar (45%) but only 20% of female respondents reported knowing the recommendation. Knowledge was also reported to be less prevalent among medical students for dietary guidelines on calcium (45% of females, 68% of males), fiber (38% of females, 39% of males), fats (29% of females, 32% of males), and potassium (23% of females, 19% of males).
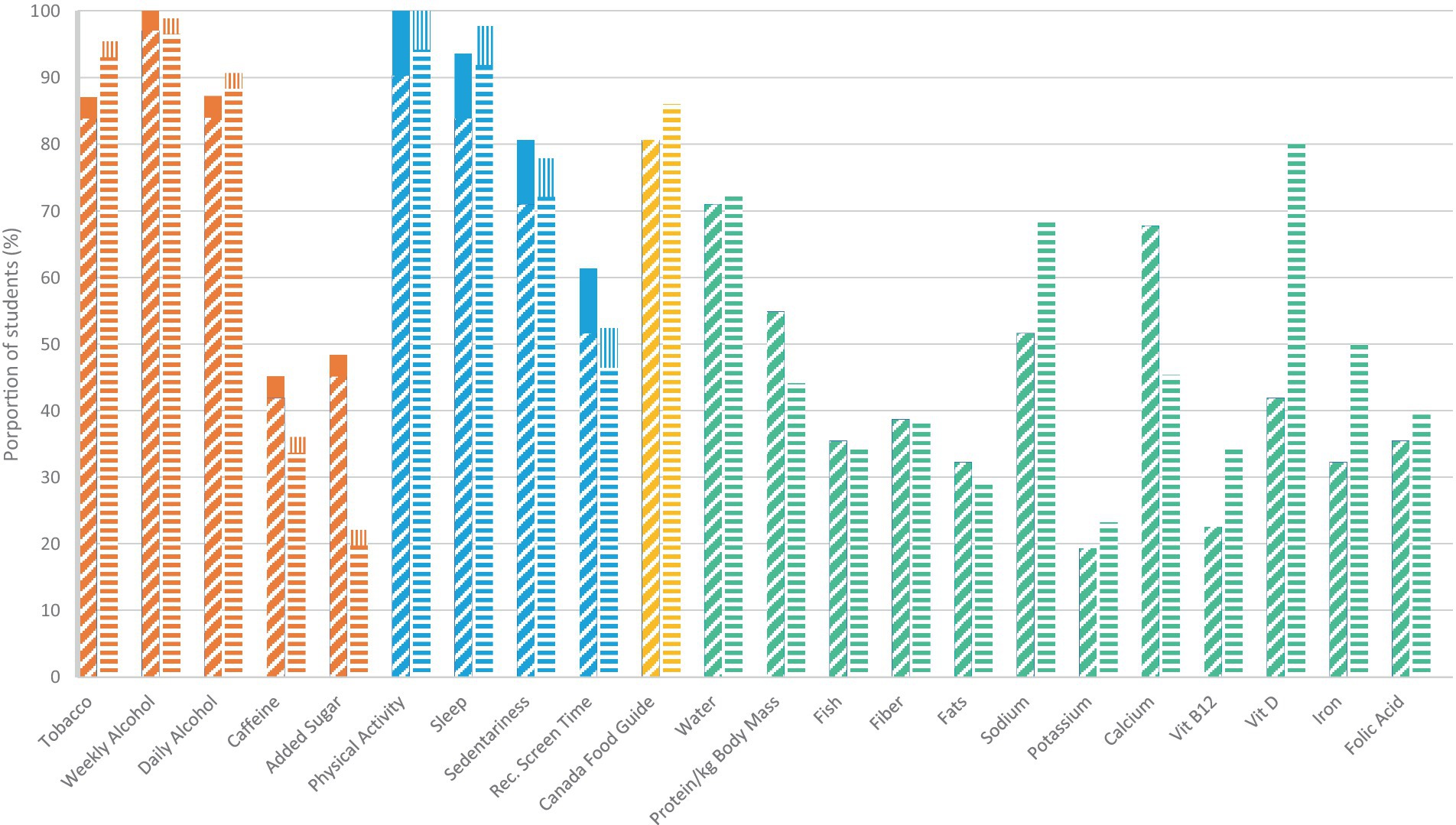
Figure 1. Prevalence of self-reported behaviors of health behavior recommendations among medical students in Western Canada, by sex. Hash, male respondent; solid, male no response/skipped; horizontal stripe, female; vertical stripe, female no response/skipped; n = 117.
As shown in Figure 2, over 60% of male medical students met the health recommendations for tobacco, weekly alcohol intake and physical activity and over 60% of female medical students met the recommendations for tobacco, weekly and daily alcohol intake; less than half of female medical students met the recommended physical activity levels. About half of male medical students (52%) met the recommendation for water, whereas a third of female medical students achieved this health behavior (34%). Adherence of respondents to the other non-dietary behaviors was generally low across male and female respondents, with some differences by sex/gender in meeting the recommendations for sleep (34% of females, 29% of males), sedentariness (13% of females, 19% of males), recreational screen time (5% of females, 16% of males). In free-text responses, medical students reported that they did a behavior when it gave them a noticeable positive effect: females most often listed exercise and sleep and males most often listed as exercise and hobbies (e.g., “I take time for hobbies because I think it prevents burnout”).
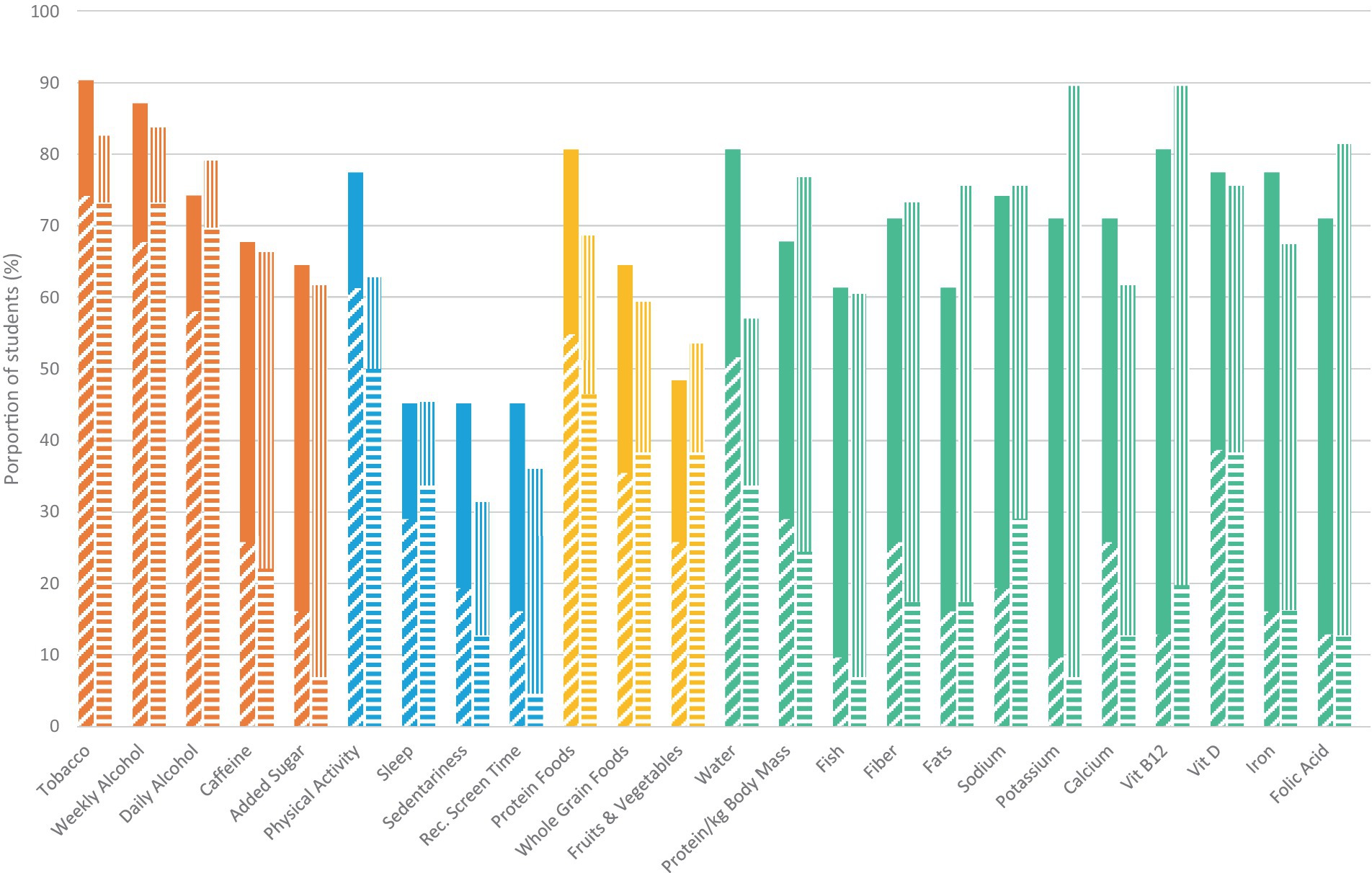
Figure 2. Prevalence of meeting recommended health behaviors among medical students in Western Canada, by sex. Hash, male; solid, male no response/skipped; horizontal stripe, female; vertical stripe, female no response/skipped.
There was wide variation in the proportion of medical students meeting dietary recommendations. Female and male medical students were similar in meeting the recommendations for whole grain foods (38% of females, 35% of males), fish (7% of females, 10% of males), fats (17% of females, 16% of males), potassium (7% of females, 10% of males), vitamin D (38% of females, 39% of males), iron (16% of females, 16% of males), and folic acid (13% of females, 13% of males). However, other dietary recommendations were not met equally: fruits and vegetables (38% of females, 26% of males), protein (47% of females, 55% of males), fiber (17% of females, 26% of males), calcium (13% of females, 26% of males), and sodium (29% of females, 19% of males).
As Figure 3 illustrates, respondents spent the most time on achieving sleep recommendations. Females reported spending an average of 49.29 h per week on sleeping, while males reported spending an average of 47.54 h per week on sleeping. Students reported spending an average of around 10 h a week adhering to dietary guidelines (10.03 h for females, 8.87 h for males) and around 6 h a week adhering to exercise guidelines (5.86 h for females, 6.07 h for males). Male respondents reported spending almost double the average amount of time (8.98 h) on hobbies when compared to female respondents (5.19 h). Students spent significantly less time on spirituality (approximately 1 h/week) and personal health (approximately 1 h/week).
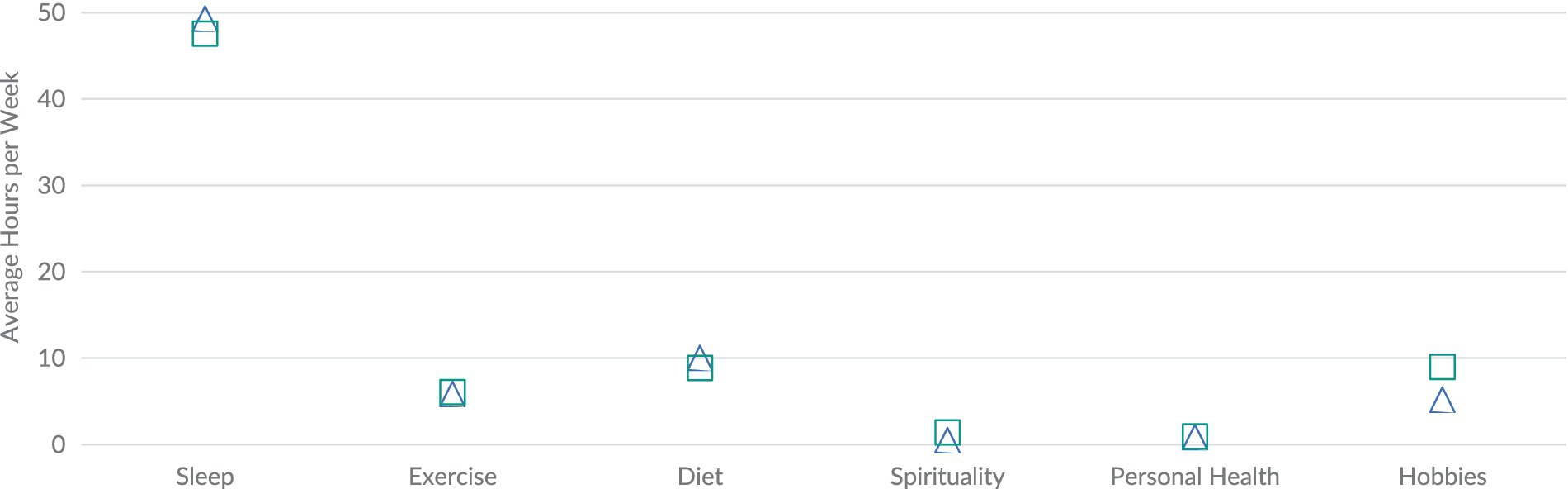
Figure 3. Reported time spent to achieve recommended health behaviors among medical students in Western Canada, by sex. Triangle, female; square, male.
Figure 4 shows some variations across medical years in the time spent on achieving recommended health behaviors. In particular, year 1 medical students (Panel A) spent more time on sleeping (49.64 h/week) and hobbies (7.18 h/week) than year 4 medical students (respectively, 46.83 h/week and 5.89 h/week) (Panel D). By contrast, year 1 medical students spent less time on diet (8.60 h/week), spirituality (0.50 h/week) and personal health (0.72 h/week) than did year 4 medical students (10.11 h/week; 1.00 h/week; 1.33 h/week). Differences in time spent on activities across medical years was not statistically significant (ANOVA p = 0.566).
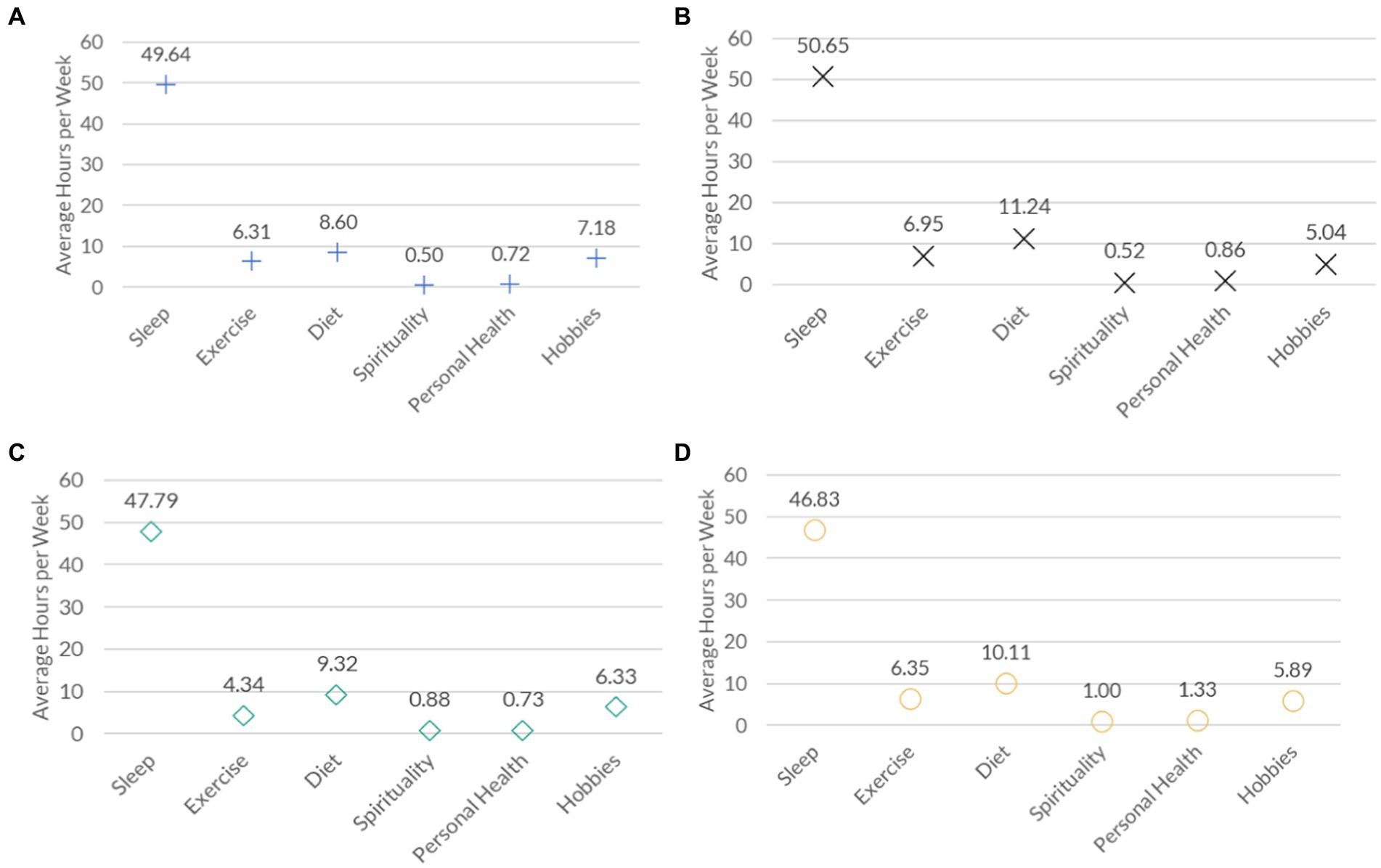
Figure 4. Reported time spent to achieve recommended health behaviors among medical students in Western Canada, by year. Panel A, year 1; Panel B, year 2; Panel C, year 3; Panel D, year 4.
About 10% of respondents reported that they had achieved the recommendations for diet but were unable to estimate the time, but less than 5% of medical students reported meeting recommendations without estimating the time spent on each behavior (Supplementary Figure S2). Between 20 and 30% of medical students did not respond to questions about time spent on health behaviors.
The most common barrier to knowledge of recommended health behaviors was forgetting the recommendation in both female (69%) and male (71%) medical students (Figure 5). Around half of female medical students reported they were unaware of the recommendation (48%) or it was unclear (53%), whereas 29% of male medical students were unaware of the recommendation or indicated it was unclear. A small proportion of respondents indicated that the recommendation was not important (7% of females, 16% of males). Achieving recommended health behaviors was time-prohibitive for 72% of female medical students and 52% of male medical students. A higher proportion of female medical students reported a range of barriers to achieving recommended health behaviors than males. Key barriers to achieving health behaviors included: being too overwhelmed (55% of females, 32% of males), the behavior was important but not a priority (44% of females, 39% of males), and the behavior was not practical (37% of females, 16% of males). Both females and males shared other barriers to the recommended health behavior such as a fear of academic decline (33% of females, 32% of males), cost (12% of females, 13% of males) and lack of cultural relevancy (3% of females, 6% of males). In free-text responses asking about barriers to health behavior adherence, female respondents specifically identified two time-consuming themes of being a caregiver/parent and being responsible for housework that male respondents did not report as time constraints. Table 1 provides examples of free-text written responses from female and male medical students about the barriers to meeting recommended behaviors.
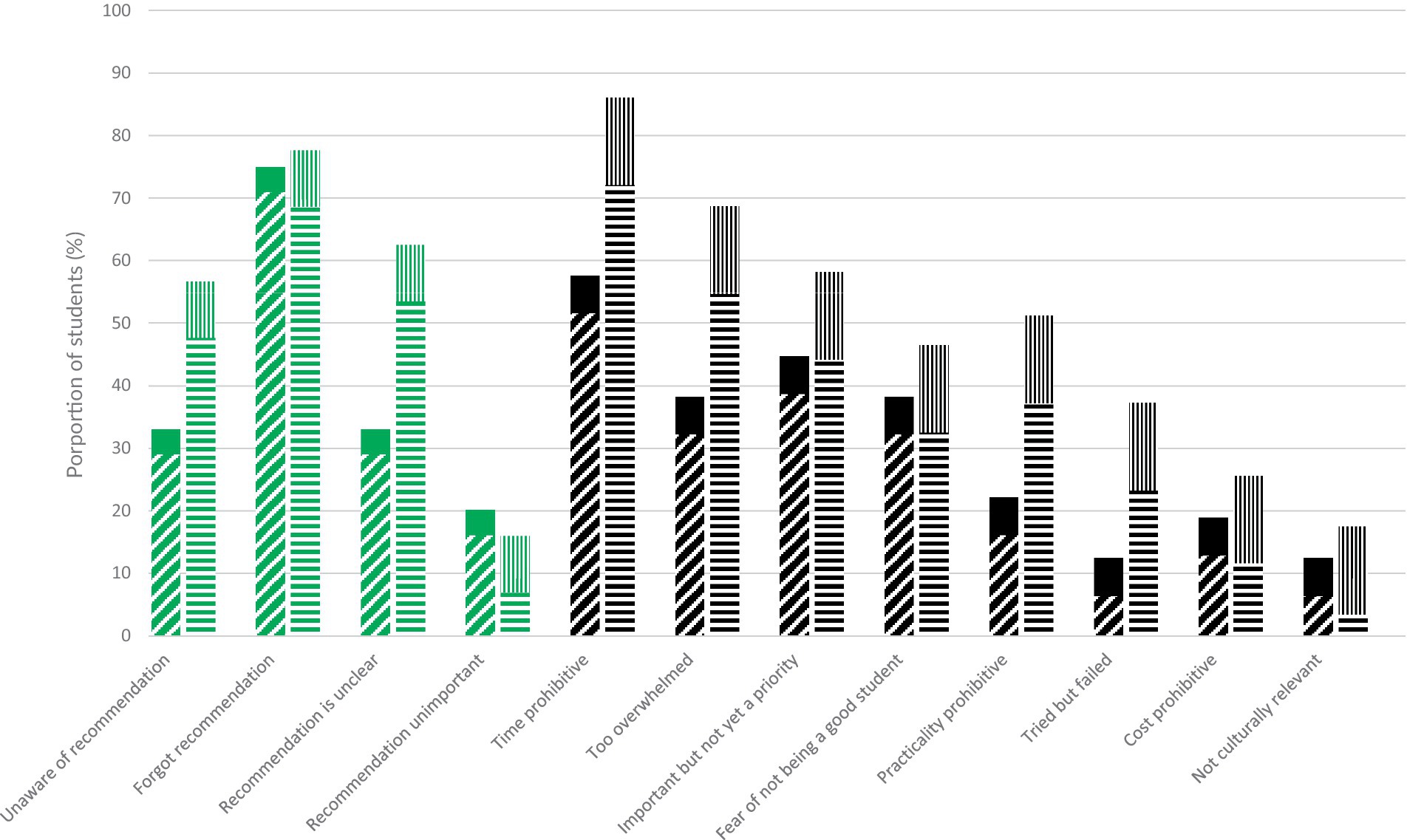
Figure 5. Prevalence of barriers to knowledge (green) and behaviors (black) among medical students in Western Canada, by sex. Hash, male; solid, male no response/skipped; horizontal stripe, female; vertical stripe, female no response/skipped.
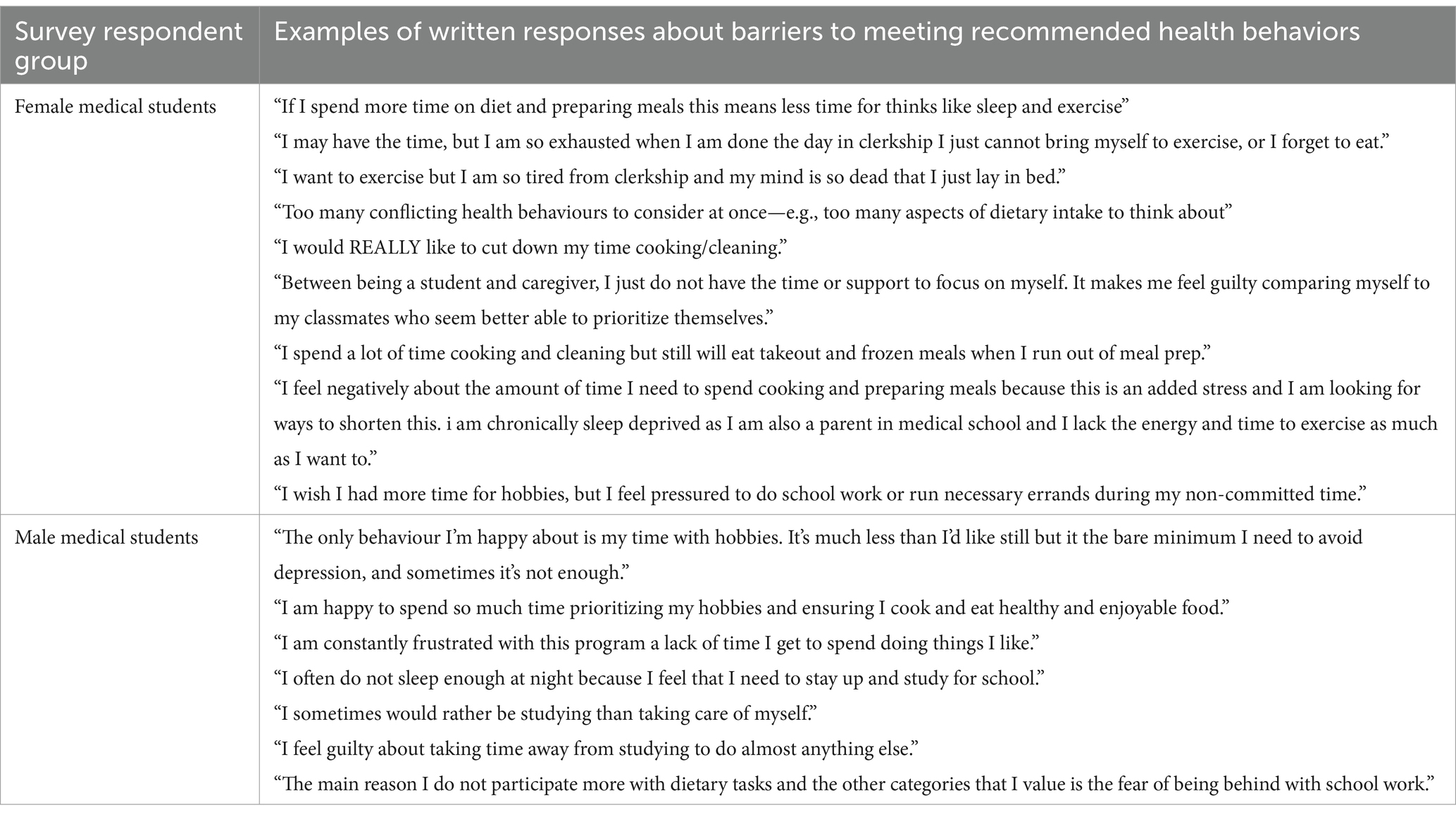
Table 1. Narrative responses to free-text questions about barriers to meeting recommended health behaviors.
Discussion
This cross-sectional study aimed to survey the self-reported knowledge, adherence, and barriers of health behaviors among medical students studying in Canadian institutions. We found that a large proportion of medical students reported having knowledge of five health behaviors but reported lacking knowledge of recommended levels for most other health behaviors, especially specific dietary factors. The prevalence of meeting the recommendations varied across health behaviors and large gaps were seen between knowledge and adherence for physical activity, sleep, sedentariness, screen time, and healthy eating practices in line with Canada’s Food Guide. Differences between the proportion of male and female respondents that reported knowledge of, and adherence to certain health recommendations were identified. Apart from sleep, the most amount of time spent on health behaviors was reported for diet and physical activity in both males and females. Across medical years, time spent on some behaviors decreased while other increased. Forgetting recommendations was identified to be the most prevalent barrier to knowledge, while lack of time was the most prevalent barrier to achieving the recommended behavior.
Findings in relation to other work
We found that a large majority of respondents reported knowledge of guidelines for alcohol, tobacco, physical activity, healthy eating and sleep for their personal use. Our finding of high prevalence of reported knowledge on sleep recommendations in both male and female medical students is similar to, and higher than, other survey data from the United States which showed that 72% of medical students had correct knowledge about the recommended amount of 7–9 h a day for adults from guidelines of both the Canadian Society for Exercise Physiology and the American National Sleep Foundation (9, 21, 23). It is not surprising that we found over 85% of medical students in Western Canada reported having knowledge of recommendations for both tobacco or alcohol which are substances that have strong national and provincial public health campaigns over many decades, and have known harms (24–28). Equally, knowledge of physical activity recommendations and the new Canada Food Guide was also reported to be prevalent in BC medical students which has also been reported elsewhere in limited literature on the dietary and physical activity knowledge of healthcare providers in Canada and internationally (29–31). However, we found a reported lack of knowledge of the guidelines for other stimulants such as added sugar and caffeine, and specific dietary factors such as fish, fiber, fats and key micronutrients. One study found that between 8 and 26% of Australian postgraduate medical students surveyed had knowledge of the guidelines for sodium, mirroring the low reported prevalence of knowledge about sodium guidelines recorded in this present study (19% of male respondents, 29% of female respondents) (32).
The majority of respondents reported meeting recommendations for tobacco and weekly alcohol, with sex differences in adhering to recommended daily alcohol (female only) or physical activity (males only). These results are comparable to a similar study that found the large majority of surveyed American medical students reported never having smoked a cigarette (15). However, despite the fact that almost all medical students in Western Canada reported knowledge of physical activity and sleep guidelines, only around a half reported meeting physical activity recommendations and a about a third reported they achieved the recommendations for sleep. It is possible that respondents had a high level of self-reported knowledge for both behaviors due to wider public health campaigns aiming to increase awareness of recommended physical activity (ParticipACTION) and sleep (the Canadian 24-Hour Movement Guidelines, 24HMG) (23). A Public Health Agency of Canada paper found that 82% of Canadians surveyed recognized the ParticipACTION campaign when prompted while another group of researchers found a third of Canadians surveyed were aware of the 24HMG campaign (33, 34). However, the practical implementation of this knowledge did not match the level of knowledge which is likely to do the multiple barriers that medical students identified. Another reason for this large gap between knowledge and adherence of respondents in this present investigation is that behavior change requires more than awareness and information; it needs motivation and skills to perform the behavior in the context of a system of structured support (35, 36). Notably, Canada lacks physical activity and sleep interventions that provide behavioral skills or target barriers to guideline adherence. Motivation alone is complex and involves inter-linked factors (risk perception, action self-efficacy and outcome expectancies) that lead to intention for and maintenance of a recommended behavior (37). Some of the responses suggested that the gap between knowledge and behavior may simply be a consequence of a lack of any observable positive result.
Overall, medical student reported a low level of meeting the recommendations for fruits and vegetables (FV) which is national statistics and existing literature. Several studies concluded that medical students consume less than the World Health Organization (WHO) recommendation of five daily servings (38–40). Our study found that a third of medical students met FV guidelines, which is higher than previous research showing about one-tenth of medical and pharmacy students in California met the recommendations for FV (41). Notably, we also observed a sex/gender difference in this dietary behavior with 39% of females but 26% of males consuming the recommended levels of FV, which was also reflected in the other California survey of 12% of female and 8% of male respondents meeting FV recommendations (41). It is known that there are sex/gender differences in dietary intake, particularly FV, which may be attributed to a difference in attitudes towards FV consumption between males and females (42–46). Although about 40% of medical students reported knowledge of recommended fiber levels, we found that it was less common for medical students to meet fiber recommendations with some sex/gender differences. Previous qualitative research shows adherence to fiber guidelines of medical students is generally low (41, 47). One study surveying the nutrient intake of medical students in Greece found the mean daily consumption of fiber to be 16.9 grams in males and 13.7 grams in females, falling below the WHO/Food and Agriculture Organization and European Food Safety Authority recommendations of 25 grams a day fiber intake for adults (47–49). These results corroborate our study showing a higher proportion of male medical students (26%) than female medical students (17%) met the Canadian guidelines for fiber. Similarly, although about a third of medical students reported having knowledge of fish guidelines (35% of females and males), less than 10% reported being able to achieve recommended fish intakes (8% of all students), particularly female medical students (7%). The low rates of adherence to fish intake guidelines is reflective of the trend in the fish consumption of Canadians, with one study finding that the average Canadian failed to meet the recommendations for daily fish intake (50). However, the findings of this present study were surprising as British Columbia’s geographical location bordering the Pacific Ocean supports a large seafood industry that accounted for $1.4 billion in exports in 2018 (51, 52).
Achievement of recommendations for healthy behaviors can be particularly challenging to medical students due to logistics alone. Some examples include daily physical activity recommendations, daily sedentary time, sleep and nutrition. In addition to 150 min per week of moderate to vigorous aerobic physical activities, Canada’s 24-h movement guidelines recommend “several hours per day of light physical activity, including standing” as well as “limiting sedentary time to 8 h or less” which includes “no more than 3 h of recreational screen time” and “breaking up long periods of sitting as often as possible” (53). Medical training can require 3 to 5 days per week spent in traditional classroom or small-group lessons for 4 to 8 h. This program structure is particularly concentrated in the earlier, less-clinical years of training, and presents both physical and social constraints to engaging in disease-preventing physical activity and reducing large amounts of sedentary time. Requirements in the later, more clinical years of training present their own logistical barriers to Canada’s 24-h movement guidelines (54, 55). For example, “getting 7 to 9 h of good-quality sleep on a regular basis, with consistent bed and wake-up times” is not compatible with compulsory rotations requiring student availability on hospital wards for 27.5-h periods. These requirements also increase barriers to recommended caffeine intake and healthy eating choices.
As this study aimed to understand the feasibility of medical students achieving all the recommendations for health behaviors, our survey showed that medical students spend an average of 72 to 73 h per week on all health behaviors in their extra-curricular time. The most time was spent on sleep which had a non-significant decline by 2.8 h/week between year 1 and year 4. About 10 h per week were spent on average on achieving dietary recommendations and around 6 h per week were spent on physical activity and on hobbies. Both male and female medical students reported similar amounts of time spent on each of the behaviors. One study surveying the leisure-time physical activity of Canadian medical students has found students spend at least 15 min on exercise an average of 16.2 times per week, that is, that students spend an average of at least 4.05 h per week on physical activity. In comparison, our findings showed a slightly higher average of 6 h per week on physical activity (56). This inconsistency can likely be attributed to a difference in the method used to measure time spent on physical activity as Babenko and colleagues recorded the average number of times a week that students spent at least 15 min on exercise while this study measured the average time in hours per week directly (56).
Finally, a number of different barriers to both knowledge and adherence of multiple recommended health behaviors were identified. Forgetting recommendations was reported as the most prevalent barrier to knowledge, while lack of time was the most prevalent barrier to achieving the behavior. As reported by Nelson and colleagues 47% of American medical students surveyed found time to be a barrier to meeting physical activity guidelines while 17% of respondents found cost to be barrier to meeting recommended food guidelines (57). These findings mirrored our results with time representing a major barrier to recommended behaviors and cost representing a less common barrier to meeting recommendations for both female (12%) and male (13%) medical students. The current medical school policy schedules students for 40 h of curricular time per week, similar to that of a regular work week. Of these 40 h, 4–8 h of unstructured time is included for students to use at their discretion. However, medical students are also expected to commit a significant amount of time outside the aforementioned 40 h to study curricular work. One group of researchers found that working more than 40 h was associated with a negative impact on healthy eating in young adults (58).
An important finding was the sex difference in the reported barriers to adherence of recommended behaviors. Nearly three quarters of female respondents reported time as a barrier whereas only about half of male respondents noted time as a barrier to achieving health behaviors. In sum, female written responses indicated that sleep and exercise were already prioritised and, despite knowing other recommended behaviors are important, their bandwidth was full because they spend much of their time cooking/cleaning/running errands/being a caretaker; that is, females would have to trade off sleep and exercise in order to implement any other health behaviors in the context of non-curricular housework. Globally, time poverty is a gendered phenomenon whereby women are more time poor than men due to the gendered division of domestic labour (59). Among young workers it is shown that young females are responsible for greater amounts of housework than are young males (60). The barrier of time constraint may also explain the observed sex difference in other barriers to adherence, with more females reporting being too overwhelmed and being impractical to implement behaviors. The narrative responses showed that female medical students faced time barriers to adherence due to being a caregiver/parent and being responsible for housework such as cooking, cleaning and shopping. Research shows that not only do women spend more of their time on unpaid labour, but also that unpaid labour is correlated with negative mental health effects (61). Thus, our study results corroborate the broader literature on the uneven distribution of housework and reveal that both time and being overwhelmed are unique barriers to achieving health behaviors for female medical students who must balance the competing demands of both their curricular work and disproportionate housework, with the recommended health behaviors. These findings have implications for embedding gender equity in the physician competencies of the medical program and may require gender-specific considerations and structural interventions for more protected time for female medical students to serve as future role models for their patients.
Methodological considerations
Limitations of our study warrant discussion. Our survey is limited by sample size and possibly volunteer selection bias that may underestimate the knowledge and adherence of health behaviors among Canada’s future clinicians from the West Coast. Our study did not offer incentives nor protected time for completion which likely affected the response rate; also, recruitment for our a two-month survey included only one reminder and was done through the newsletter of the Medicine Undergraduate Learner Access Advisory Council. Notably, medical students in Canada are known to have the lowest response rates to surveys relative to medical residents and practising physicians (62, 63). Additionally, our survey respondents in [redacted for review] were mostly female and thus findings may not be generalizable to male physicians-in-training or to other settings in Canada. However, our sample largely reflects the overall medical student pool as about 60% of all undergraduate medical students in the classes of 2023–2026 self-reported as female. While our collection method was expected to select females and males with equal sampling probability, it is well-known that females have higher survey response rates than males. To rebalance the under-representation of males in survey responses, future work may need to employ techniques such as a dual-frame sampling design to oversample males as a minority population of medical students in Western Canada.
A major strength of this study is the comprehensive inclusion of all recommended health behaviors, including water, sleep and sedentary behavior. To the best of our knowledge, this is the first study investigating the self-reported knowledge of, adherence to, time spent and barriers to the full breadth of health behaviors among future doctors in Canada. Another strength of this study is the focus on medical students who are an under-studied population of healthcare providers. This focus is imperative not only as physician burnout rates are increasing, but also as physicians should strive to serve as positive health role models for their patients (7, 8). Emphasized in physician competencies outlined by the Royal College of Physicians and Surgeons, Canadian medical students are expected to know and adhere to health behaviors by engaging in the stewardship of health care resources (leader competency); demonstrating a commitment to physician health and wellbeing to foster optimal patient care (professional competency); and, applying knowledge of social/ behavioral sciences and selecting interventions for prevention and health promotion in patient care (medical expert competency) (6). Of significance, the study’s novelty is the new data generated on estimated time spent on recommended health behaviors by way of assessing feasibility of medical students achieving health and wellness for themselves and modeling for their patients. Finally, another major strength of this study was a survey sample that consisted of a relatively equal balance of respondents from all 4 years of medical school, allowing results to be more representative of the general medical student population in Canada.
Conclusion
The knowledge of and adherence to health behaviors are requirements for medical students who are expected to serve as role models for their future patients. This study demonstrated that medical students in Western Canada reported having knowledge of some but not all recommended health behaviors and that most did not achieve health promotion guidelines. This research also illustrated the average time required to achieve recommended health behaviors as well as identified a range of barriers to both knowledge and adherence, with forgetfulness and time being key barriers of each. There is great scope to improve the knowledge and adherence of recommended health behaviors among medical students, and a need to address relevant barriers.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The study involving humans were approved by UBC Behavioural Research Ethics Board Class Project Certificate H16-00044. The study was conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
NI: Formal Analysis, Visualization, Writing – original draft. KS: Conceptualization, Writing – review & editing, Data curation, Formal analysis, Investigation. AC: Conceptualization, Methodology, Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
AIC acknowledges salary support from the Michael Smith Health Research BC Scholar award (SCH-2020-0581).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2024.1468990/full#supplementary-material
Abbreviations
FV, Fruit and vegetable; MD, Doctor of Medicine; BC, British Columbia.
References
1. Thornton, JS, Frémont, P, Khan, K, Poirier, P, Fowles, J, Wells, GD, et al. Physical activity prescription: a critical opportunity to address a modifiable risk factor for the prevention and management of chronic disease: a position statement by the Canadian Academy of Sport and Exercise Medicine: Table 1. Br J Sports Med. (2016) 50:1109–14. doi: 10.1136/bjsports-2016-096291
2. Lobelo, F, and De Quevedo, IG. The evidence in support of physicians and health care providers as physical activity role models. Am J Lifestyle Med. (2016) 10:36–52. doi: 10.1177/1559827613520120
3. La Torre, G, Saulle, R, Unim, B, Angelillo, IF, Baldo, V, Bergomi, M, et al. Knowledge, attitudes, and smoking Behaviours among physicians specializing in public health: a multicentre study. Biomed Res Int. (2014) 2014:1–8. doi: 10.1155/2014/516734
4. Truswell, AS, Hiddink, GJ, and Blom, J. Nutrition guidance by family doctors in a changing world: problems, opportunities, and future possibilities. Am J Clin Nutr. (2003) 77:1089S–92S. doi: 10.1093/ajcn/77.4.1089S
5. Falskog, F, Landsem, AM, Meland, E, Bjorvatn, B, Hjelle, OP, and Mildestvedt, T. Patients want their doctors’ help to increase physical activity: a cross sectional study in general practice. Scand J Prim Health Care. (2021) 39:131–8. doi: 10.1080/02813432.2021.1910670
6. Frank, JR, Snell, L, and Sherbino, J, (2015). CanMEDS 2015 physician competency framework [internet]. Royal College of Physicians and Surgeons of Canada. Available at: https://canmeds.royalcollege.ca/uploads/en/framework/CanMEDS%202015%20Framework_EN_Reduced.pdf (Accessed April 17, 2024).
7. Canadian Medical Association (2018). CMA National Physician Health Survey: A National Snapshot [internet]. Ottawa: Canadian Medical Association. p. 30. Available at: https://www.cma.ca/sites/default/files/2018-11/nph-survey-e.pdf (Accessed June 19, 2023).
8. Canadian Medical Association (2021). National Physician Health Survey [internet]. Ottawa: Canadian Medical Association. p. 122. Available at: https://www.cma.ca/sites/default/files/2022-08/NPHS_final_report_EN.pdf (Accessed June 19, 2023).
9. Ahmed, N, Sadat, M, and Cukor, D. Sleep knowledge and behaviors in medical students: results of a single center survey. Acad Psychiatry. (2017) 41:674–8. doi: 10.1007/s40596-016-0655-3
10. Fan, LM, Collins, A, Geng, L, and Li, JM. Impact of unhealthy lifestyle on cardiorespiratory fitness and heart rate recovery of medical science students. BMC Public Health. (2020) 20:1012. doi: 10.1186/s12889-020-09154-x
11. Ayala, EE, Berry, R, Winseman, JS, and Mason, HR. A cross-sectional snapshot of sleep quality and quantity among US medical students. Acad Psychiatry. (2017) 41:664–8. doi: 10.1007/s40596-016-0653-5
12. Kanikowska, D, Sikorska, D, Kuczyńska, B, Grzymisławski, M, Bręborowicz, A, and Witowski, J. Do medical students adhere to advice regarding a healthy lifestyle? A pilot study of BMI and some aspects of lifestyle in medical students in Poland. Adv Clin Exp Med. (2017) 26:1391–8. doi: 10.17219/acem/65783
13. Rodakowska, E, Kierklo, A, and Jamiołkowski, J. Self-reported Oral health behaviour among Scandinavian and polish medical students studying in Poland. Cent Eur J Public Health. (2016) 24:68–75. doi: 10.21101/cejph.a4084
14. Jackson, ER, Shanafelt, TD, Hasan, O, Satele, DV, and Dyrbye, LN. Burnout and alcohol abuse/dependence among U.S. medical students. Acad Med. (2016) 91:1251–6. doi: 10.1097/ACM.0000000000001138
15. Frank, E, Carrera, J, Elon, L, and Hertzberg, V. Basic demographics, health practices, and health status of U.S. medical students. Am J Prev Med. (2006) 31:499–505. doi: 10.1016/j.amepre.2006.08.009
16. FitzGerald, LZ, and Boland, D. The impact of behavioral and psychological factors on physical fitness in medical and nursing students. Holist Nurs Pract. (2018) 32:125–32. doi: 10.1097/HNP.0000000000000265
17. Greco, L, Gindi, M, Yusupov, E, Niwagaba, L, and Pino, MA. Are medical students prepared to model healthy behaviors for their future patients? A survey comparing aged-matched peers. Med Sci Educ. (2020) 30:843–8. doi: 10.1007/s40670-020-00960-x
18. Rye, PL, Reeson, ME, Pekrul, CM, Asfour, NA, Kundapur, R, Wilson, MP, et al. Comparing health behaviours of internal medicine residents and medical students: an observational study. CIM. (2012) 35:40–E44. doi: 10.25011/cim.v35i1.16105
19. Howie, EK, Cannady, N, Messias, EL, McNatt, A, and Walter, CS. Associations between physical activity, sleep, and self-reported health with burnout of medical students, faculty and staff in an academic health center. Sport Sci Health. (2022) 18:1311–9. doi: 10.1007/s11332-022-00902-7
20. Holtz, KA, Kokotilo, KJ, Fitzgerald, BE, and Frank, E. Exercise behaviour and attitudes among fourth-year medical students at the University of British Columbia. Can Fam Physician. (2013) 59:e26–32.
21. Hirshkowitz, M, Whiton, K, Albert, SM, Alessi, C, Bruni, O, DonCarlos, L, et al. National Sleep Foundation’s updated sleep duration recommendations: final report. Sleep Health. (2015) 1:233–43. doi: 10.1016/j.sleh.2015.10.004
22. Popkin, BM, D’Anci, KE, and Rosenberg, IH. Water, hydration, and health: nutrition reviews©. Nutr Rev. (2010) 68:439–58. doi: 10.1111/j.1753-4887.2010.00304.x
23. Ross, R, Chaput, JP, Giangregorio, LM, Janssen, I, Saunders, TJ, Kho, ME, et al. Canadian 24-Hour movement guidelines for adults aged 18–64 years and adults aged 65 years or older: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. (2020) 45:S57–S102. doi: 10.1139/apnm-2020-0467
24. Walser, T, Cui, X, Yanagawa, J, Lee, JM, Heinrich, E, Lee, G, et al. Smoking and lung Cancer: the role of inflammation. Proc Am Thorac Soc. (2008) 5:811–5. doi: 10.1513/pats.200809-100TH
25. Youlden, DR, Cramb, SM, and Baade, PD. The international epidemiology of lung Cancer: geographical distribution and secular trends. J Thorac Oncol. (2008) 3:819–31. doi: 10.1097/JTO.0b013e31818020eb
26. Wood, AM, Kaptoge, S, Butterworth, AS, Willeit, P, Warnakula, S, Bolton, T, et al. Risk thresholds for alcohol consumption: combined analysis of individual-participant data for 599 912 current drinkers in 83 prospective studies. Lancet. (2018) 391:1513–23. doi: 10.1016/S0140-6736(18)30134-X
27. Griswold, MG, Fullman, N, Hawley, C, Arian, N, Zimsen, SRM, Tymeson, HD, et al. Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet. (2018) 392:1015–35. doi: 10.1016/S0140-6736(18)31310-2
28. Statistics Canada, Health Canada (2017). Canadian tobacco, alcohol and drugs survey (CTADS): summary of results for 2017 [internet]. Health Canada. Available at: https://www.canada.ca/en/health-canada/services/canadian-alcohol-drugs-survey/2017-summary.html (Accessed November 19, 2023).
29. Solmundson, K, Koehle, M, and McKenzie, D. Are we adequately preparing the next generation of physicians to prescribe exercise as prevention and treatment? Residents express the desire for more training in exercise prescription. Can Med Educ J. (2016) 7:e79–96. doi: 10.36834/cmej.36702
30. Mota, IB, Castelo, I, Morais, J, Anjos, M, Costa, JP, Dias, M, et al. Nutrition education in Portuguese medical students: impact on the attitudes and knowledge. Acta Medica Port. (2020) 33:246–51. doi: 10.20344/amp.11817
31. Sahlqvist, S, Rees, B, Hoffmann, S, McCoombe, S, Santoro, G, and Kremer, P. Physical activity knowledge, attitudes and behaviours of pre-clinical medical students attending an Australian university. BMC Med Educ. (2022) 22:642. doi: 10.1186/s12909-022-03695-y
32. Perlstein, R, McCoombe, S, Macfarlane, S, Bell, AC, and Nowson, C. Nutrition practice and knowledge of first-year medical students. J Biomed Educ. (2017) 2017:1–10. doi: 10.1155/2017/5013670
33. Spence, JC, Faulkner, G, Lee, EY, Berry, T, Cameron, C, Deshpande, S, et al. Awareness of ParticipACTION among Canadian adults: a seven-year cross-sectional follow-up. Health Promot Chronic Dis Prev Can. (2018) 38:179–86. doi: 10.24095/hpcdp.38.4.04
34. Kauffeldt, KD, Varkul, O, Latimer-Cheung, AE, Faulkner, G, Brouwers, MC, Chulak-Bozzer, T, et al. Awareness and knowledge of the Canadian 24-Hour movement guidelines for adults among adults living in Canada. Appl Physiol Nutr Metab. (2024) 49:405–10. doi: 10.1139/apnm-2023-0255
35. Masana, L, Ros, E, Sudano, I, Angoulvant, D, Ibarretxe Gerediaga, D, Murga Eizagaechevarria, N, et al. Is there a role for lifestyle changes in cardiovascular prevention? What, when and how? Atheroscler Suppl. (2017) 26:2–15. doi: 10.1016/S1567-5688(17)30020-X
36. Zurynski, Y, Smith, C, Siette, J, Nic Giolla Easpaig, B, Simons, M, and Knaggs, GT. Identifying enablers and barriers to referral, uptake and completion of lifestyle modification programmes: a rapid literature review. BMJ Open. (2021) 11:e045094. doi: 10.1136/bmjopen-2020-045094
37. Schwarzer, R . Modeling health behavior change: how to predict and modify the adoption and maintenance of health behaviors. Appl Psychol. (2008) 57:1–29. doi: 10.1111/j.1464-0597.2007.00325.x
38. Vibhute, N, Baad, R, Belgaumi, U, Kadashetti, V, Bommanavar, S, and Kamate, W. Dietary habits amongst medical students: an institution-based study. J Family Med Prim Care. (2018) 7:1464–6. doi: 10.4103/jfmpc.jfmpc_154_18
39. Cefai, C, and Camilleri, L. The dietary habits of Maltese university students. Malta Med J. (2011) 23:7–12.
40. AL-Otaibi, HH . The pattern of fruit and vegetable consumption among Saudi university students. GJHS. (2013) 6:p155. doi: 10.5539/gjhs.v6n2p155
41. Bergeron, N, Al-Saiegh, S, and Ip, EJ. An analysis of California pharmacy and medical students’ dietary and lifestyle practices. Am J Pharm Educ. (2017) 81:5956. doi: 10.5688/ajpe5956
42. Emanuel, AS, McCully, SN, Gallagher, KM, and Updegraff, JA. Theory of planned behavior explains gender difference in fruit and vegetable consumption. Appetite. (2012) 59:693–7. doi: 10.1016/j.appet.2012.08.007
43. Kähäri, A . Gender differences in fresh vegetable intake from 1979 to 2017 in Finland. BFJ. (2022) 124:53–65. doi: 10.1108/BFJ-09-2021-1004
45. Baker, AH, and Wardle, J. Sex differences in fruit and vegetable intake in older adults. Appetite. (2003) 40:269–75. doi: 10.1016/S0195-6663(03)00014-X
46. Wardle, J, Haase, AM, Steptoe, A, Nillapun, M, Jonwutiwes, K, and Bellisie, F. Gender differences in food choice: the contribution of health beliefs and dieting. Ann Behav Med. (2004) 27:107–16. doi: 10.1207/s15324796abm2702_5
47. Mammas, I, Bertsias, G, Linardakis, M, Moschandreas, J, and Kafatos, A. Nutrient intake and food consumption among medical students in Greece assessed during a clinical nutrition course. Int J Food Sci Nutr. (2004) 55:17–26. doi: 10.1080/09637480310001642448
48. Nishida, C, Uauy, R, Kumanyika, S, and Shetty, P. The joint WHO/FAO expert consultation on diet, nutrition and the prevention of chronic diseases: process, product and policy implications. Public Health Nutr. (2004) 7:245–50. doi: 10.1079/PHN2003592
49. EFSA Panel on Dietetic Products, Nutrition, and Allergies (NDA) . cientific opinion on dietary reference values for carbohydrates and dietary fibre. EFS2 [Internet]. (2010) 8. Available from: https://data.europa.eu/doi/10.2903/j.efsa.2010.1462
50. Hu, XF, and Chan, HM. Seafood consumption and its contribution to nutrients intake among Canadians in 2004 and 2015. Nutrients. (2020) 13:77. doi: 10.3390/nu13010077
51. Government of British Columbia (2018). British Columbia seafood industry YEAR IN REVIEW 2018 [internet]. British Columbia Ministry of Agriculture. p. 17. Available at: https://www2.gov.bc.ca/assets/gov/farming-natural-resources-and-industry/agriculture-and-seafood/statistics/industry-and-sector-profiles/year-in-review/bcseafood_yearinreview_2018.pdf (Accessed November 19, 2023).
52. Gibson, D, and Sumaila, UR. Determining the degree of “small-scaleness” using fisheries in British Columbia as an example. Mar Policy. (2017) 86:121–6. doi: 10.1016/j.marpol.2017.09.015
53. Canadian Society of Exercise Physiology (2021), Public Health Agency of Canada, Queen’s University, PARTICIPATION. CANADIAN 24-HOUR MOVEMENT GUIDELINES FOR ADULTS AGED 18-64 YEARS: an integration of physical activity, sedentary behaviour, and sleep [internet]. Canadian Society of Exercise Physiology. Available at: https://csepguidelines.ca (Accessed April 17, 2024).
54. Hill, MR, Goicochea, S, and Merlo, LJ. In their own words: stressors facing medical students in the millennial generation. Med Educ Online. (2018) 23:1530558. doi: 10.1080/10872981.2018.1530558
55. Malau-Aduli, BS, Roche, P, Adu, M, Jones, K, Alele, F, and Drovandi, A. Perceptions and processes influencing the transition of medical students from pre-clinical to clinical training. BMC Med Educ. (2020) 20:279. doi: 10.1186/s12909-020-02186-2
56. Babenko, O, Mosewich, A, Abraham, J, and Lai, H. Contributions of psychological needs, self-compassion, leisure-time exercise, and achievement goals to academic engagement and exhaustion in Canadian medical students. J Educ Eval Health Prof. (2018) 15:2. doi: 10.3352/jeehp.2018.15.2
57. Nelson, B, Petushek, E, and Teising, S. Knowledge and barriers to a healthy lifestyle in medical students. Am J Lifestyle Med. (2023):15598276231199057. doi: 10.1177/15598276231199057
58. Escoto, KH, Laska, MN, Larson, N, Neumark-Sztainer, D, and Hannan, PJ. Work hours and perceived time barriers to healthful eating among young adults. Am J Health Behav. (2012) 36:786–96. doi: 10.5993/AJHB.36.6.6
59. Hyde, E, Greene, ME, and Darmstadt, GL. Time poverty: obstacle to women’s human rights, health and sustainable development. J Glob Health. (2020) 10:020313. doi: 10.7189/jogh.10.020313
60. Loughlin, C, and Barling, J. Young workers’ work values, attitudes, and behaviours. J Occupat Organ Psychol. (2001) 74:543–58. doi: 10.1348/096317901167514
61. Ervin, J, Taouk, Y, Alfonzo, LF, Hewitt, B, and King, T. Gender differences in the association between unpaid labour and mental health in employed adults: a systematic review. Lancet Public Health. (2022) 7:e775–86. doi: 10.1016/S2468-2667(22)00160-8
62. Grava-Gubins, I, and Scott, S. Effects of various methodologic strategies: survey response rates among Canadian physicians and physicians-in-training. Can Fam Physician. (2008) 54:1424–30.
Keywords: health behaviors, healthcare professionals, medical students, knowledge, adherence, barriers, time, prevalence
Citation: Ip N, Scarrott K and Conklin AI (2024) Multiple recommended health behaviors among medical students in Western Canada: a descriptive study of self-reported knowledge, adherence, barriers, and time use. Front. Med. 11:1468990. doi: 10.3389/fmed.2024.1468990
Edited by:
Sebastian Schnaubelt, Medical University of Vienna, AustriaReviewed by:
Nina Pereza, University of Rijeka, CroatiaMeshal Sultan, Mohammed Bin Rashid University of Medicine and Health Sciences, United Arab Emirates
Copyright © 2024 Ip, Scarrott and Conklin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Annalijn I. Conklin, YW5uYWxpam4uY29ua2xpbkB1YmMuY2E=
 Nathanael Ip
Nathanael Ip Kendra Scarrott2
Kendra Scarrott2 Annalijn I. Conklin
Annalijn I. Conklin