- 1Institute for Regenerative Medicine (IRM), Graz, Austria
- 2Austrian Society of Regenerative Medicine (RegMed), Vienna, Austria
- 3Division of Orthopaedics and Traumatology, University Hospital Krems, Krems, Austria
Introduction
Osteoarthritis (OA) is the most common chronic joint disease and a leading cause of disability (1). Globally, the number of prevalent OA cases rises exponentially, with knee OA contributing the most to the overall burden (2). This will lead to substantial healthcare expenditures and an unmet demand for orthopedic surgeons in most Organization for Economic Co-operation and Development (OECD) countries (3, 4). Cell-based therapies are being utilized more frequently, and the outcomes of bone marrow aspirate concentrate (BMAC) or “stem cell therapy” demonstrate promising short- to mid-term results. With the use of BMAC, as discussed by Di Matteo and Kon in their study, “The Dilemma of Drink Selection for the Modern Orthopedic Surgeon,” the decision-making process is becoming increasingly complex, even for experienced practitioners. The question now is: “What should I inject into the patients with osteoarthritis (OA) of the knee? Platelet-rich martini or vodka hyaluronic acid?” (5).
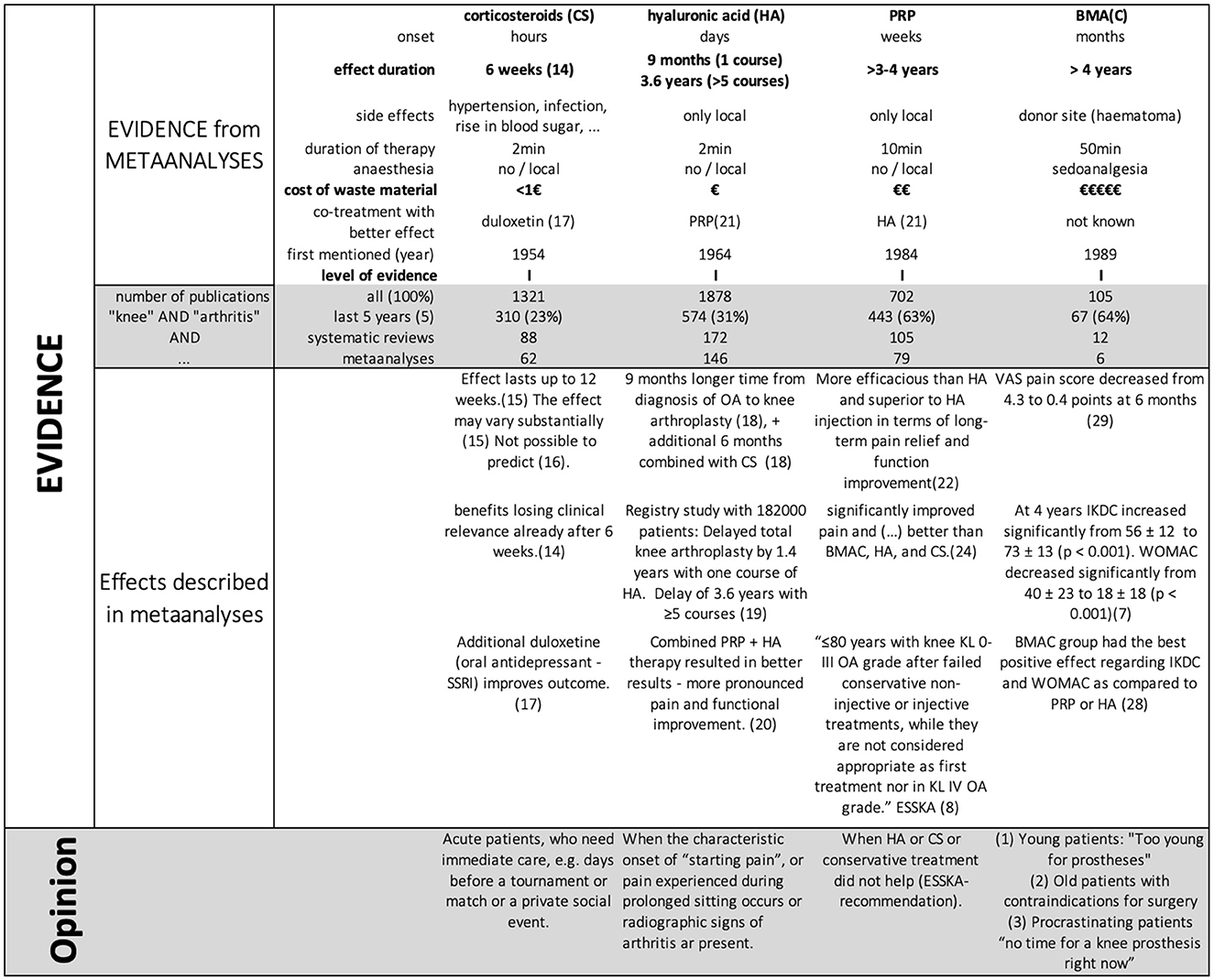
Our primary focus in this article will be on critically comparing various treatment options using published data. Second, we will emphasize addressing specific patient needs and share our perspective on personalized medicine for treating knee osteoarthritis. This opinion is informed by over 20 years of experience as the team doctor for the Austrian national soccer team and the Austrian national ski team, applying these insights to the treatment of regular patients.
Injection therapy
Injection therapy for knee OA is unquestionable, but the question of which type of injection is not easy. The currently used Kellgren–Lawrence (KL) classification for OA dates back to the year 1957 and is not of great help in decision-making (6).
Currently, we have evidence that BMAC injections even have excellent outcomes in patients with severe OA (7), and implants have become so good that the compound annual growth rate in knee arthroplasty in younger patients has exceeded the demand in the elderly for over 15 years (4). The European Society for Sports Traumatology, Knee Surgery, and Arthroscopy (ESSKA) also recommends platelet-rich plasma (PRP) in OA grades I–III (8). Furthermore, the discrepancy between radiological classification and patient-reported symptoms is well known.
The following key points have to be highlighted in our opinion:
• Conservative means (e.g., stretching, insoles, physio, weight reduction, and cycling) are the first choice of therapy and accompany every injection therapy.
• Mechanical errors, such as patellar malalignment, varus/valgus deviations more than 6°, and ligament or meniscal injuries, must be surgically corrected first—regardless of age—since they are significant risk factors for knee osteoarthritis (9–12).
• Total knee arthroplasty (TKA) is still the gold standard for severe osteoarthritis, not responding to conservative means, with 95% good and excellent results at 20 years (13).
Corticosteroids
Undoubtedly, intra-articular corticosteroid injections offer clinically perceivable pain relief and functional improvement higher than the placebo effect, but these benefits are typically short-term, often diminishing in clinical relevance after 6 weeks in patients with knee OA (14). The effect may vary substantially in different patient groups, and “appropriate patient” selection is important (15). However, it is not possible to predict which patients are most likely to benefit from intra-articular corticosteroid injections (16).
Patients receiving co-treatment with oral duloxetine (serotonin reuptake inhibitor) and CS injections experience considerable improvement in pain and knee function compared to those who receive a CS injection alone (17).
Hyaluronic acid
A registered study on 15,000 Medicare patients showed that the patients receiving hyaluronic acid (HA) were associated with a longer time to knee arthroplasty (KA) of 8.7 months (8.3–9.1, p < 0.001) as compared to patients without HA. Patients with both intra-articular HA and intra-articular CS had an additional 6.3 months (5.5–7.0, p < 0.001) to KA over those with only IA HA (18). In a registry study with 182,000 patients, it was evident that with one course of HA, the mean delay time to total knee arthroplasty was 1.4 years (p < 0.0001); patients who received ≥5 courses delayed total knee arthroplasty by 3.6 years (p < 0.0001) (19). A recent meta-analysis with 943 patients in 10 randomized controlled trials (RCTs) showed that PRP + HA therapy resulted in more pronounced pain and functional improvement in symptomatic KOA patients than HA treatments (20).
PRP (platelet-rich plasma)
One shot of PRP injection has been shown to reduce joint pain more effectively and for a longer duration, alleviate symptoms, and enhance the daily activities of living and quality of life compared to CS injections (21). In a meta-analysis comparing HA and PRP, intra-articular PRP injections appeared to be more efficacious than HA injections for the treatment of knee OA. PRP demonstrated superior short-term functional recovery (as measured by IKDC, WOMAC, Lequesne, and visual analog scale [VAS] scores) and long-term benefits (in terms of pain relief and function improvement). Additionally, PRP did not increase the risk of adverse events compared to HA (22).
Recent ESSKA guidelines consider PRP injections appropriate for patients aged ≤ 80 years with knee KL 0-III OA grade after failed conservative non-injective or injective treatments. However, PRP is not recommended as a first-line treatment or for patients with KL IV OA grade (8).
Bone marrow aspirate (concentrate)
One meta-analysis of 16 short-term studies with 875 patients receiving BMAC showed a significant pain reduction (VAS) from the third month onward (23). Another meta-analysis compared HA, PRP, and BMAC at 6 months and found that all led to a significant improvement in function scores when compared to placebo (24). A third meta-analysis of 27 studies and 1,042 patients with a mean 13-month follow-up compared PRP, BMAC, and HA for knee OA: these meta-analyses demonstrated significantly better postinjection WOMAC (p < 0.001), VAS (p < 0.01), and IKDC scores (p < 0.001) in patients who received PRP compared to patients who received HA. Similarly, other meta-analyses demonstrated significantly better postinjection WOMAC (p < 0.001), VAS (p = 0.03), and IKDC (p < 0.001) scores in patients who received BMAC compared to patients who received HA, but no significant differences when comparing PRP and BMAC (25). A further meta-analysis with a mean follow-up of 14 months, comprising 15 studies and 585 patients, found that bone marrow mesenchymal stem cells (BM-MSCs) therapy was most effective in improving VAS and ROM. In contrast, other types of mesenchymal stem cells (MSCs), such as those derived from umbilical cord and adipose tissue, were more effective in improving functional outcomes, including Whole-Organ Magnetic Resonance Imaging Score (WORMS) and Western Ontario McMaster Universities Osteoarthritis Index (WOMAC) scores (26).
To date, no further meta-analyses have been published comparing different sources of pluripotent stem cells or evaluating cell-based injections against established therapeutic options such as HA, CS, and PRP. However, all these meta-analyses have a follow-up of approximately 1 year. However, we know that the positive effect of BMAC is becoming statistically and clinically relevant from the second year onward (7).
Furthermore, a clinical study involving 175 patients directly comparing the outcomes of knee injections with BMAC, PRP, and HA over a 1-year follow-up found that the BMAC group had the best positive effect regarding IKDC and WOMAC at all time points (27). However, another single study reported that the effect of BMAC at 1 year was not superior to that of corticosteroids (28).
To our knowledge, there is only one study with a 4-year follow-up on BMAC therapy in patients with OA. In this study, 35 of 37 knees improved regarding IKDC and WOMAC scores from the first to the last follow-up. IKDC scores significantly increased from 56 ± 12 (range 34–81) to 73 ± 13 (range 45–100), p < 0.001. WOMAC scores decreased substantially from 40 ± 23 (range 6–96) to 18 ± 18 (range 0–67), p < 0.001 (7).
Discussion
Undoubtedly, the evolution in injection therapy from CS in 1964 to the current use of PRP and BMAC is impressive. This evidence-based evolution demonstrates that several HA injections can postpone knee arthroplasty by up to 4 years (19). Furthermore, PRP, when combined with HA, can produce even more substantial effects (20).
• CS injections are used in acute patients in our institution: for those who need immediate care, for example, days before a tournament, match, or private social event, we use Betamethasone 1 mL.
Regarding HA injections, we switched to the one-treatment 60-mg HA injection a decade ago instead of the 3 times 20 mg to minimize patients' traveling, infection risk, and pain.
• HA injections are administered when the characteristic onset of “starting pain” or pain experienced during prolonged sitting with a flexed knee (often referred to as the “cinema sign”) occurs.
We advise symptomatic patients that a renewal of an injection after 6–18 months has a better long-term effect (19). We never inject prophylactically in asymptomatic knees.
Regarding PRP, we currently use a one-treatment system that involves a 60-mL blood withdrawal to produce 4 mL of PRP. This approach seems better to us than the 4–5 times repetitive injections of 1–2 mL PRP, made out of 15 mL because the risk of infection and pain is minimized. The recent ESSKA statement on PRP clarifies its use:
• PRP injections are recommended when HA, CS, or conservative treatments are not effective.
Since all meta-analyses on BMAC showed at least equivalent results compared to PRP 1 year after the injection, and considering that the therapeutic effect of BMAC takes 2 years to occur fully, it is most likely that BMAC will outperform PRP in terms of results in the following years (7, 23, 25, 26).
• BMAC injections are therefore used in our institution when other injections have failed. We see impressive long-term effects: 35 of 37 patients benefit from this kind of treatment (7). These patient groups are best suited for this treatment:
1. Young patients (< 50 years) who are not yet suitable for knee prosthesis. We know that operating on these patients too early will not result in a “happy patient” (29). Thus, the goal is to gain several years until a prosthesis can be implanted.
2. Old patients (>80 years) with contraindications for surgery or severe comorbidities. Here, the goal is to avoid complications and surgical procedures.
3. “Procrastinating patients” (of all ages) with “no time for a knee prosthesis,” because they have to “take care of relatives,” or are “too much engaged in the jobs at the moment” can also be considered for BMAC injections.
Regarding the injection of intra-articular microfragmented adipose tissue (MF-AT, also known as (mesenchymal) stem cell therapy, stromal vascular fraction (SVF)-therapy), such types of injections have also been proposed for the treatment of knee OA. Several recent studies have shown that a single intra-articular injection of MF-AT is not superior to PRP, meta-analyses on this comparison are currently lacking (30–32). We want to emphasize that our stem cell research study group had significant trouble cultivating fat cells in an experimental setting. In contrast, we could quickly work with bone marrow cells. We, therefore, do not recommend this kind of fat-tissue-derived cell treatment.
We also use all the aforementioned injections in patients with rheumatoid arthritis as an additional option to their basic therapy with a similar outcome as compared to degenerative arthritis. However, the literature on injection therapy in rheumatoid arthritis with autologous PRP or BMA(C) is sparse, and the industry fosters small-molecule and biological therapies, devices, and gene therapy (33).
Based on the aforementioned meta-analyses, we can estimate that future publications will demonstrate the superior long-term effectiveness of BMAC injections as compared to PRP injections (7).
Currently, fluoroscopic guided subchondral injections (of BMAC) for knee osteoarthritis are being discussed, and few pilot study studies show promising results (34, 35). At the moment, a double-blind RCT is conducted, comparing bone marrow aspirate concentrate intra-articular injection combined with subchondral injection vs. intra-articular injection alone for the treatment of symptomatic knee osteoarthritis (36). This might be an option for patients with additional bone marrow edema.
Single studies also recommended the use of BMA instead of BMAC, which makes the procedure faster and cheaper, but this depends on the methodology of the harvesting procedure in order to gain a maximum cell yield (7, 37). This may become an option for the future when the harvesting procedure of BMA becomes standardized.
Transferring this evidence into daily clinical praxis, we developed a 1-page handout sheet that can help patients and doctors in choosing the right injection at the right point of time (Figure 1).
Author contributions
CP: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. GK: Formal analysis, Supervision, Validation, Writing – review & editing. DD: Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Hunter DJ, Bierma-Zeinstra S. Osteoarthritis. Lancet. (2019) 393:1745–59. doi: 10.1016/S0140-6736(19)30417-9
2. Long H, Liu Q, Yin H, Wang K, Diao N, Zhang Y, et al. Prevalence trends of site-specific osteoarthritis from 1990 to 2019: findings from the global burden of Disease Study 2019. Arthritis Rheumatol. (2022) 74:1172–83. doi: 10.1002/art.42089
3. Gagliardi AR, Ducey A, Lehoux P, Ross S, Trbovich P, Easty A, et al. Meta-review of the quantity and quality of evidence for knee arthroplasty devices. PLoS ONE. (2016) 11:e0163032. doi: 10.1371/journal.pone.0163032
4. Pabinger C, Lothaller H, Geissler A. Utilization rates of knee-arthroplasty in OECD countries. Osteoarthritis Cartilage. (2015) 23:1664–73. doi: 10.1016/j.joca.2015.05.008
5. Di Matteo B, Kon E. Editorial commentary: platelet-rich martini or vodka hyaluronate? The dilemma of drink selection for the modern orthopaedic surgeon. Arthroscopy. (2021) 37:916–8. doi: 10.1016/j.arthro.2020.11.016
6. Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. (1957) 16:494–502. doi: 10.1136/ard.16.4.494
7. Pabinger C, Lothaller H, Kobinia GS. Intra-articular injection of bone marrow aspirate concentrate (mesenchymal stem cells) in KL grade III and IV knee osteoarthritis: 4 year results of 37 knees. Sci Rep. (2024) 14:2665. doi: 10.1038/s41598-024-51410-2
8. Kon E, de Girolamo L, Laver L, Andriolo L, Andia I, Bastos R, et al. Platelet-rich plasma injections for the management of knee osteoarthritis: the ESSKA-ICRS consensus. Recommendations using the RAND/UCLA appropriateness method for different clinical scenarios. Knee Surg Sports Traumatol Arthrosc. (2024). doi: 10.1002/ksa.12320
9. Park JY, Kim JH, Cho JW, Kim MS, Choi W. Clinical and radiological results of high tibial of osteotomy over the age of 65 are comparable to that of under 55 at minimum 2-year follow-up: a propensity score matched analysis. Knee Surg Relat Res. (2024) 36:10. doi: 10.1186/s43019-024-00214-9
10. Goshima K, Sawaguchi T, Sakagoshi D, Shigemoto K, Hatsuchi Y, Akahane M. Age does not affect the clinical and radiological outcomes after open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. (2017) 25:918–23. doi: 10.1007/s00167-015-3847-6
11. Saito T, Kumagai K, Akamatsu Y, Kobayashi H, Kusayama Y. Five- to ten-year outcome following medial opening-wedge high tibial osteotomy with rigid plate fixation in combination with an artificial bone substitute. Bone Joint J. (2014) 96-B:339–44. doi: 10.1302/0301-620X.96B3.32525
12. Whittaker JL, Losciale JM, Juhl CB, Thorlund JB, Lundberg M, Truong LK, et al. Risk factors for knee osteoarthritis after traumatic knee injury: a systematic review and meta-analysis of randomised controlled trials and cohort studies for the OPTIKNEE Consensus. Br J Sports Med. (2022) 56:1406–21. doi: 10.1136/bjsports-2022-105496
13. SKAR. The Swedish Knee Arthoplasty Register. Lund: Lund University Department of Clinical Sciences, Orthopedics Skåne University Hospital. (2020).
14. Bensa A, Albanese J, Boffa A, Previtali D, Filardo G. Intra-articular corticosteroid injections provide a clinically relevant benefit compared to placebo only at short-term follow-up in patients with knee osteoarthritis: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. (2024) 32:311–22. doi: 10.1002/ksa.12057
15. Saltychev M, Mattie R, McCormick Z, Laimi K. The magnitude and duration of the effect of intra-articular corticosteroid injections on pain severity in knee osteoarthritis: a systematic review and meta-analysis. Am J Phys Med Rehabil. (2020) 99:617–25. doi: 10.1097/PHM.0000000000001384
16. Shekleton FE, Donovan RL, Wylde V, Whitehouse MR. Is it possible to predict which patients are most likely to benefit from intra-articular corticosteroid injections? A systematic review. Int J Rheum Dis. (2024) 27:e15005. doi: 10.1111/1756-185X.15005
17. Li D, Hang R, Meng L, Zhao Z, Zhao C, Luo F. Co-treatment with oral duloxetine and intraarticular injection of corticosteroid plus hyaluronic acid reduces pain in the treatment of knee osteoarthritis. Pain Physician. (2024) 27:E45–53.
18. Ong KL, Anderson AF, Niazi F, Fierlinger AL, Kurtz SM, Altman RD. Hyaluronic acid injections in medicare knee osteoarthritis patients are associated with longer time to knee arthroplasty. J Arthroplasty. (2016) 31:1667–73. doi: 10.1016/j.arth.2016.01.038
19. Altman R, Lim S, Steen RG, Dasa V. Hyaluronic acid injections are associated with delay of total knee replacement surgery in patients with knee osteoarthritis: evidence from a large U. S. health claims database. PLoS ONE. (2015) 10:e0145776. doi: 10.1371/journal.pone.0145776
20. Shaibe E, Metzer E, Halpern YS. Control of utilization of L-arginine, L-ornithine, agmatine, and putrescine as nitrogen sources in Escherichia coli K-12. J Bacteriol. (1985) 163:938–42. doi: 10.1128/jb.163.3.938-942.1985
21. Forogh B, Mianehsaz E, Shoaee S, Ahadi T, Raissi GR, Sajadi S. Effect of single injection of platelet-rich plasma in comparison with corticosteroid on knee osteoarthritis: a double-blind randomized clinical trial. J Sports Med Phys Fitness. (2016) 56:901–8.
22. Tang JZ, Nie MJ, Zhao JZ, Zhang GC, Zhang Q, Wang B. Platelet-rich plasma versus hyaluronic acid in the treatment of knee osteoarthritis: a meta-analysis. J Orthop Surg Res. (2020) 15:403. doi: 10.1186/s13018-020-01919-9
23. Xie RH, Gong SG, Song J, Wu PP, Hu WL. Effect of mesenchymal stromal cells transplantation on the outcomes of patients with knee osteoarthritis: a systematic review and meta-analysis. J Orthop Res. (2024) 42:753–68. doi: 10.1002/jor.25724
24. Jawanda H, Khan ZA, Warrier AA, Acuna AJ, Allahabadi S, Kaplan DJ, et al. Platelet-rich plasma, bone marrow aspirate concentrate, and hyaluronic acid injections outperform corticosteroids in pain and function scores at a minimum of 6 months as intra-articular injections for knee osteoarthritis: a systematic review and network meta-analysis. Arthroscopy. (2024) 40:1623–36 e1. doi: 10.1016/j.arthro.2024.01.037
25. Belk JW, Lim JJ, Keeter C, McCulloch PC, Houck DA, McCarty EC, et al. Patients with knee osteoarthritis who receive platelet-rich plasma or bone marrow aspirate concentrate injections have better outcomes than patients who receive hyaluronic acid: systematic review and meta-analysis. Arthroscopy. (2023) 39:1714–34. doi: 10.1016/j.arthro.2023.03.001
26. Chen X, Zheng J, Yin L, Li Y, Liu H. Transplantation of three mesenchymal stem cells for knee osteoarthritis, which cell and type are more beneficial? A systematic review and network meta-analysis. J Orthop Surg Res. (2024) 19:366. doi: 10.1186/s13018-024-04846-1
27. Dulic O, Rasovic P, Lalic I, Kecojevic V, Gavrilovic G, Abazovic D, et al. Bone marrow aspirate concentrate versus platelet rich plasma or hyaluronic acid for the treatment of knee osteoarthritis. Medicina. (2021) 57:1193. doi: 10.3390/medicina57111193
28. Mautner K, Gottschalk M, Boden SD, Akard A, Bae WC, Black L, et al. Cell-based versus corticosteroid injections for knee pain in osteoarthritis: a randomized phase 3 trial. Nat Med. (2023) 29:3120–6. doi: 10.1038/s41591-023-02632-w
29. Beverland D. Patient satisfaction following TKA: bless them all! Orthopedics. (2010) 33:657. doi: 10.3928/01477447-20100722-23
30. Zaffagnini S, Andriolo L, Boffa A, Poggi A, Cenacchi A, Busacca M, et al. Microfragmented adipose tissue versus platelet-rich plasma for the treatment of knee osteoarthritis: a prospective randomized controlled trial at 2-year follow-up. Am J Sports Med. (2022) 50:2881–92. doi: 10.1177/03635465221115821
31. Sgaglione NA. In patients with symptomatic knee osteoarthritis, a single intra-articular injection of microfragmented adipose tissue did not differ from platelet-rich plasma for clinical outcomes at up to 24 months. J Bone Joint Surg Am. (2023) 105:807. doi: 10.2106/JBJS.23.00158
32. Baria M, Pedroza A, Kaeding C, Durgam S, Duerr R, Flanigan D, et al. Platelet-rich plasma versus microfragmented adipose tissue for knee osteoarthritis: a randomized controlled trial. Orthop J Sports Med. (2022) 10:23259671221120678. doi: 10.1177/23259671221120678
33. Jones IA, Togashi R, Wilson ML, Heckmann N, Vangsness CT. Intra-articular treatment options for knee osteoarthritis. Nat Rev Rheumatol. (2019) 15:77–90. doi: 10.1038/s41584-018-0123-4
34. Kon E, Boffa A, Andriolo L, Di Martino A, Di Matteo B, Magarelli N, et al. Subchondral and intra-articular injections of bone marrow concentrate are a safe and effective treatment for knee osteoarthritis: a prospective, multi-center pilot study. Knee Surg Sports Traumatol Arthrosc. (2021) 29:4232–40. doi: 10.1007/s00167-021-06530-x
35. Kon E, Boffa A, Andriolo L, Di Martino A, Di Matteo B, Magarelli N, et al. Combined subchondral and intra-articular injections of bone marrow aspirate concentrate provide stable results up to 24 months. Knee Surg Sports Traumatol Arthrosc. (2023) 31:2511–7. doi: 10.1007/s00167-022-07195-w
36. Silva S, Andriolo L, Boffa A, Di Martino A, Reale D, Vara G, et al. Prospective double-blind randomised controlled trial protocol comparing bone marrow aspirate concentrate intra-articular injection combined with subchondral injection versus intra-articular injection alone for the treatment of symptomatic knee osteoarthritis. BMJ Open. (2022) 12:e062632. doi: 10.1136/bmjopen-2022-062632
Keywords: arthritis, OA, osteoarthritis, knee, BMA, mesenchymal stem cells, hyaluronic acid, PRP
Citation: Pabinger C, Kobinia GS and Dammerer D (2024) Injection therapy in knee osteoarthritis: cortisol, hyaluronic acid, PRP, or BMAC (mesenchymal stem cell therapy)? Front. Med. 11:1463997. doi: 10.3389/fmed.2024.1463997
Received: 12 July 2024; Accepted: 23 August 2024;
Published: 27 September 2024.
Edited by:
Benjamin Gesundheit, Cell-El Ltd., IsraelReviewed by:
Xiaolei Li, University of Pennsylvania, United StatesCopyright © 2024 Pabinger, Kobinia and Dammerer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Christof Pabinger, b2ZmaWNlQGlybS5jbGluaWM=
 Christof Pabinger
Christof Pabinger Georg Stefan Kobinia1,2
Georg Stefan Kobinia1,2