- Department of Dermatology, The First Affiliated Hospital of Shantou University Medical College, Shantou, Guangdong, China
Background: While several studies have noted a higher SII correlates with multiple diseases, research on the association between SII and atopic dermatitis remains limited. Our cross-sectional study seeks to examine the association between SII and atopic dermatitis among outpatient US adults.
Methods: This compensatory cross-sectional study utilized NHANES data from 2001–2006 cycles, conducting sample-weighted multivariate logistic regression and stratified analysis of sub-groups.
Results: Higher levels of SII were positively associated with an increased risk of atopic dermatitis in adults with BMI <30 (OR, 1.44; 95% CI, 1.10–1.90) (p = 0.010).
Conclusion: Our findings suggested SII higher than 330 × 109/L was positively associated with a high risk of atopic dermatitis in US adults with BMI <30. To our knowledge, this is the first study focused on the risk of higher SII on atopic dermatitis in the outpatient US population. Currently, there are differences in the standards used to diagnose atopic dermatitis across countries, and our study may have implications.
1 Introduction
Atopic dermatitis is a common and chronic inflammatory dermatological condition that affects more than 200 million people worldwide, including 15 to 20% of children and 10% of adults (1, 2). It leads to substantial costs and accounts for the largest global burden of disability owing to skin diseases (3). Currently, there are many effective medications for the treatment of atopic dermatitis, such as JAK1 inhibitors and dupilumab. The mechanisms of action of these drugs involve the inhibition of inflammatory substances, which significantly control the condition of atopic dermatitis (4, 5). This represents a milestone compared to the effects achieved by traditional treatments.
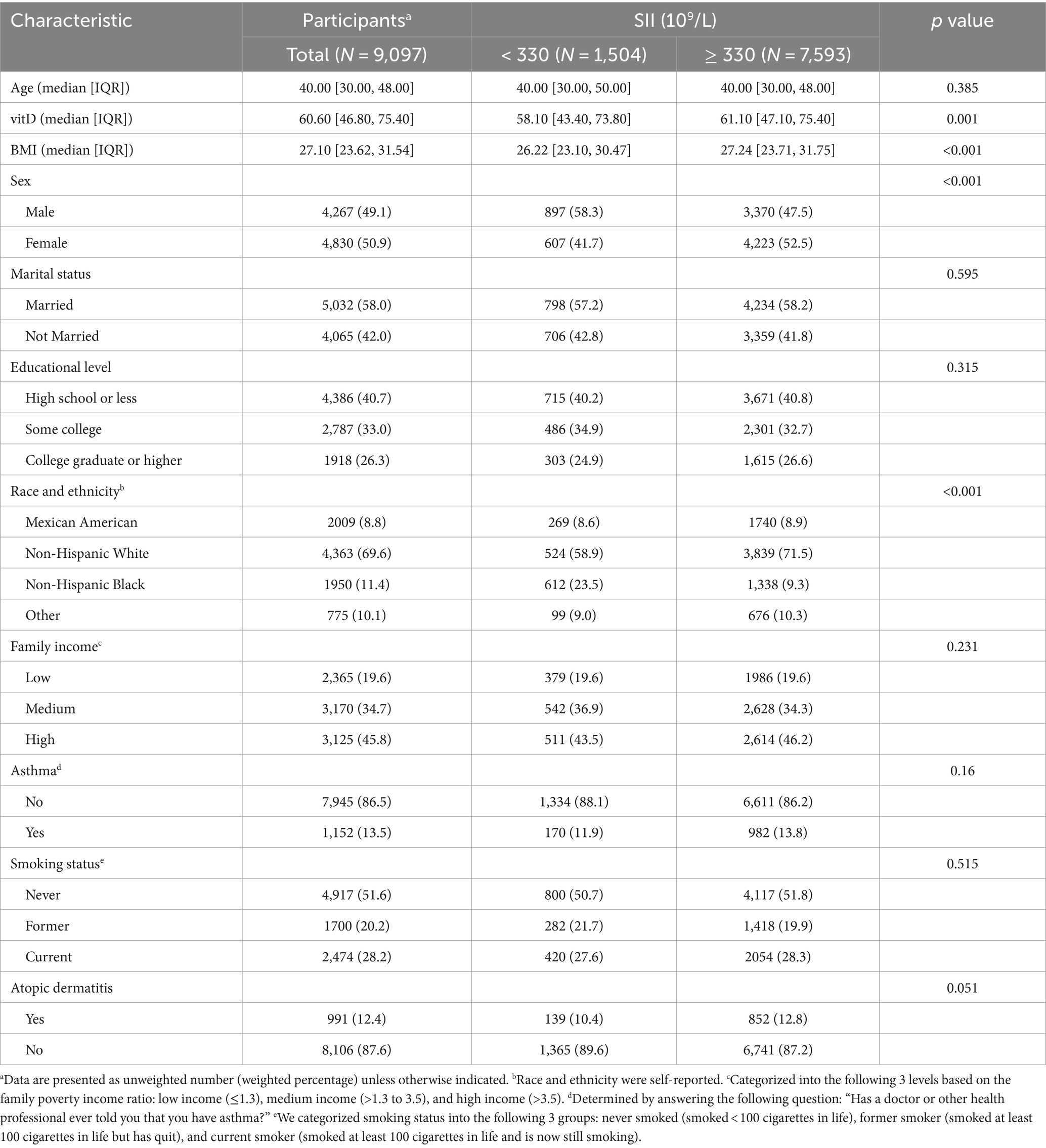
Within the systemic inflammatory system of the human body, immune cells play a critical role in multiple diseases. Scientists have found that combined counts of lymphocytes, neutrophils, and platelets in the peripheral blood may be a better predictor of inflammatory status. Importantly, SII was calculated by counting three types of circulating immune cells: neutrophils, lymphocytes, and platelets. Moreover, SII was initially identified as a prognosis of kidney stones, hepatic steatosis, and others (6, 7). Atopic dermatitis has been reported to be associated with inflammatory responses (8–10). However, the impact of SII on atopic dermatitis in the outpatient US population is not fully elucidated, and little is known about its prognostic ability for atopic dermatitis. In this cross-sectional study using NHANES data, we tried our best to find the association between SII and atopic dermatitis among outpatient US adults (Table 1).
2 Methods
2.1 Data sources
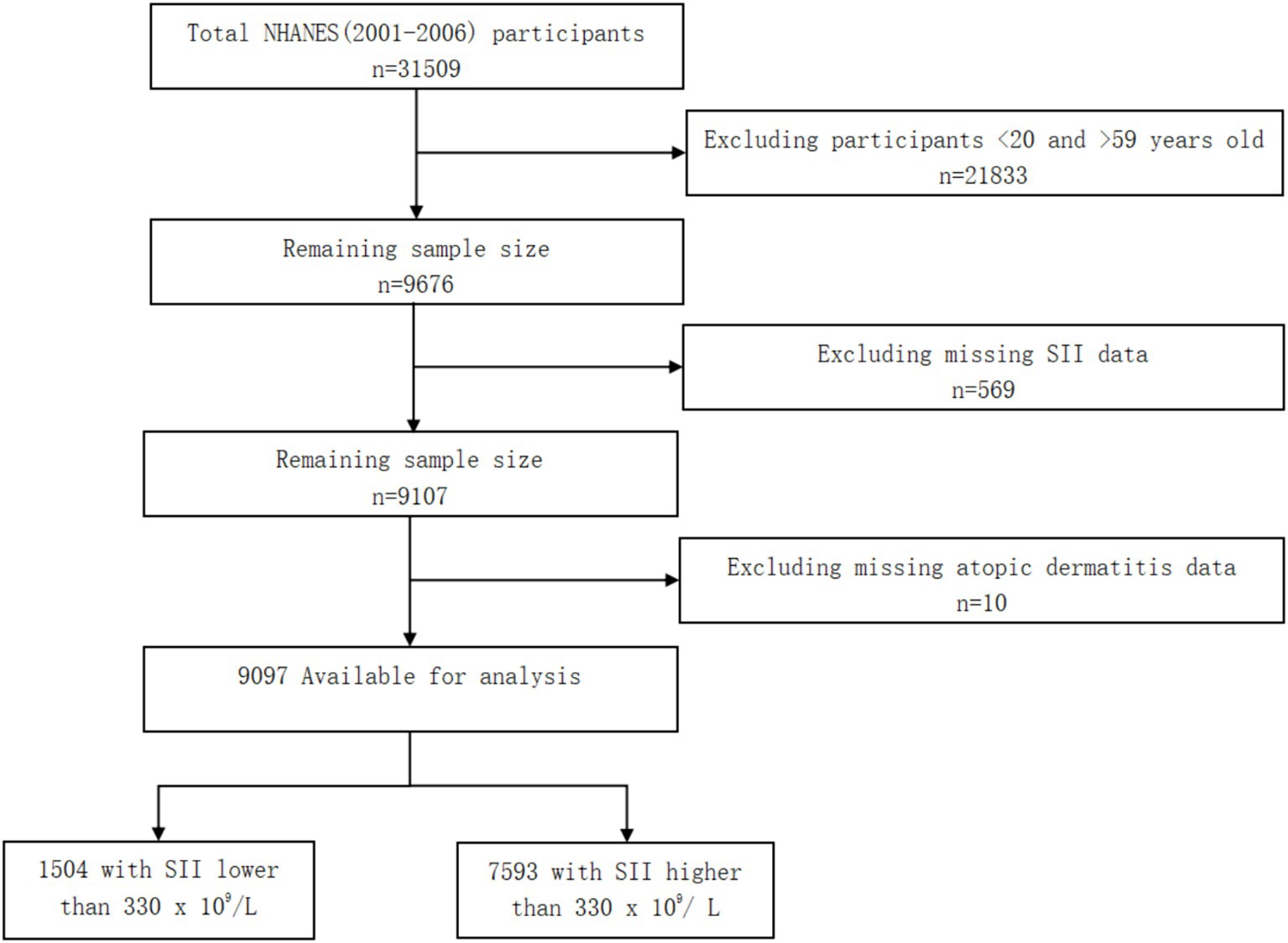
Information on atopic dermatitis was only provided in the NHANES 2001–2006 cycles for adults 20 to 59 years of age. In this cross-sectional study, deidentified data for participants 20 to 59 years of age were extracted from the 2001–2006 NHANES cycles. This cross-sectional study was deemed exempt as it used publicly available data, and informed consent was waived. This study followed the STROBE reporting guideline. Data were analyzed from July to November 2023 (Figure 1).
2.2 Study design and population
Because information on atopic dermatitis was only provided in the NHANES 2001–2006 cycles for adults 20 to 59 years of age, we selected a total of 9,676 adults within this age range. Moreover, we excluded 569 participants who had missing SII data, 10 participants who had missing atopic dermatitis data. Finally, a total of 9,097 participants were involved. Of the 9,097 participants, there were 1,504 participants with SII lower than 330 × 109/L and 7,593 participants with SII higher than 330 × 109/L.
2.3 Assessment of SII and atopic dermatitis
SII was defined as (platelet x neutrophil)/lymphocyte (11). Throughout the analysis, we set the cutoff value at 330 × 109/L based on previous studies of the NHANES (12, 13).
Atopic dermatitis was assessed by the question “Has a doctor ever told you that you have eczema?” (NHANES 2001–2004 cycles, Variable Name: DED061 and NHANES 2005–2006 cycle, Variable Name: AGQ180) (14) We refer to this inclusion criteria based on an article titled ‘Association between atopic dermatitis and thyroid disease among US adults in the 2001–2006 NHANES’ published in JAAD.
2.4 Covariates
The following covariates were included: sociodemographic variables (age, sex, race and ethnicity, family income, educational level, and marital status), NHANES cycles, BMI, serum 25(OH)D, asthma, and smoking status (15, 16). Races and ethnicities was categorized into 4 groups. Based on the family poverty income ratio, family income was categorized into the following 3 levels: low income (≤1.3), medium income (>1.3 to 3.5), and high income (>3.5). Educational level was categorized into 3 levels. Marital status was categorized into the following 2 groups: married, not married. We categorized smoking status into the following 3 groups: smoked <100 cigarettes in life, smoked at least 100 cigarettes in life but has quit now, and smoked at least 100 cigarettes in life and is now still smoking (17).
2.5 Statistical analysis
In accordance with NHANES analytic guidelines, our analyses considered the complex sampling design and sampling weights (18). The sampling weight was calculated using the following formula: fasting subsample 6-year mobile examination center (MEC) weight = fasting subsample 2-year MEC weight/3. Moreover, we used quartiles to describe the continuous variables with non-normal distribution and described the categorical variables using unweighted frequency and weighted percentage in this cross-sectional study.
We checked for multicollinearity using the VIF method. If the VIF was 5 or higher, it meant there was multicollinearity present (19). Model 1 was adjusted for sociodemographic variables and NHANES cycles. Model 2 was adjusted for sociodemographic variables, NHANES cycles, BMI (only for overall), serum 25(OH)D, asthma, and smoking status. We conducted a subgroup analysis on BMI to assess the possible influence of BMI on the association between SII and atopic dermatitis.
We used R version 4.3.1 for all the statistical analyses and we considered a significance level of p < 0.05 to show that the results were statistically significant.
3 Results
There were 31,509 participants from 2001–2006 included in this study. 21,833 participants <20 and > 59 years old were excluded, and 569 participants were excluded for missing SII data. After removing 10 participants missing atopic dermatitis data, 9,097 participants were finally enrolled. Compare with SII lower than 330 × 109/L, participants with SII higher than 330 × 109/ L were more non-Hispanic White (p < 0.001).
As shown in Table 2, logistic regression analysis found no significant difference between SII and atopic dermatitis after adjusting for covariates in the whole population. In the subgroup with BMI <30, the univariate and multivariate analyses demonstrated high SII over 330 × 109/L was associated with a higher risk of atopic dermatitis in the crude model (OR, 1.53; 95% CI, 1.17–1.99; p = 0.002) and model 1 (OR, 1.47; 95% CI, 1.12–1.93; p = 0.006). After adjusting for all confounding factors, high SII over 330 × 109/L was still positively associated with atopic dermatitis in the population with BMI <30 (OR, 1.44; 95% CI, 1.10–1.90; p = 0.010). The difference was not found in participants with BMI ≥30. Stratified logistic regression analysis in the subgroup with BMI <30 suggested no potential modifiers in the relationship between SII and atopic dermatitis in the population with BMI <30.
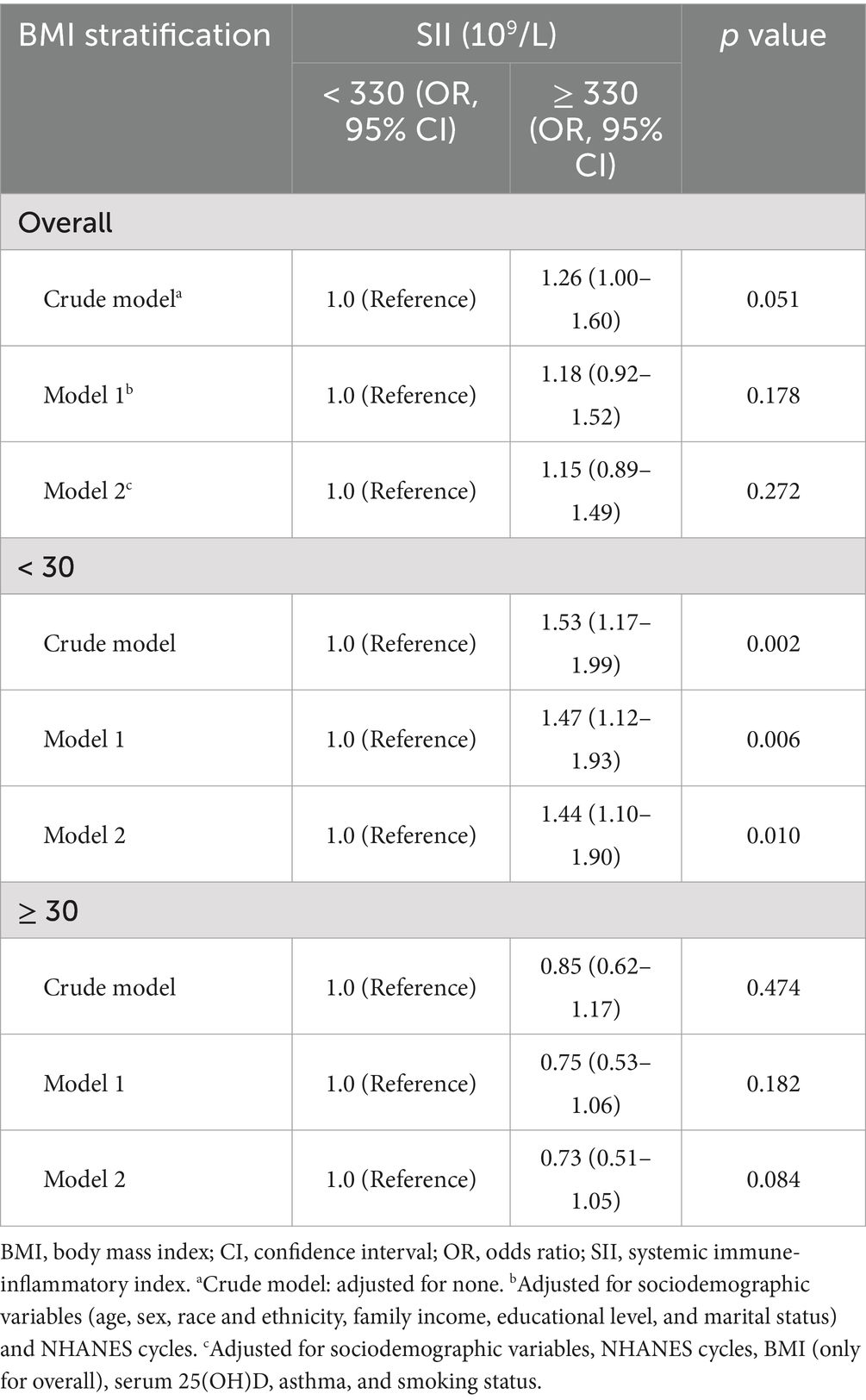
Table 2. Univariate and multivariate analyses by the activity-stratified logistic regression model, weighted.
Because the percentage of missing data was small (missing rate varied from 0 to 4.8%) for any variable, no imputation method was used.
4 Discussion
Chronic inflammation is important in the development of atopic dermatitis (20, 21). SII was calculated by neutrophils, lymphocytes, and platelets (22). It reflects the inflammatory reactions and may be a useful diagnostic biomarker for systemic inflammatory activity. In this cross-sectional study, we identified higher SII level was independently associated with atopic dermatitis in participants with BMI <30. But, we did not find such an association in adults with BMI ≥30. Moreover, SII is a widely available method with a non-intrusive methodology, low cost, and easy accessibility. Therefore, SII can be identified as a biomarker for atopic dermatitis in participants with BMI <30. Currently, there are differences in the standards used to diagnose atopic dermatitis across countries, and our study may have implications.
Interestingly, our findings only demonstrated the association between SII and atopic dermatitis in participants with BMI <30. Because there are more risk factors in participants with BMI ≥30, the impact of SII on atopic dermatitis in participants with BMI ≥30 might be compensated by other confounding factors.
5 Conclusion
After adjusting for all confounding factors, high SII over 330 × 109/L was still positively associated with atopic dermatitis in the population with BMI <30. From the above results obtained through the rigorous analysis, we believe that incorporating SII into the diagnostic criteria of atopic dermatitis may improve the diagnostic rate of atopic dermatitis. Early clinical manifestations of atopic dermatitis are often subtle and can be easily overlooked during diagnosis. Therefore, including SII as part of the diagnostic criteria may facilitate earlier detection and enable preventive management of the condition. Currently, there are differences in the standards used to diagnose atopic dermatitis across countries, and our study may have implications.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found at: https://www.cdc.gov/nchs/nhanes/index.htm.
Ethics statement
The NCHS research ethics review board approved the NHANES study protocol, and participants provided written informed consent at enrollment. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
QD: Writing – original draft, Writing – review & editing. LL: Writing – original draft, Writing – review & editing. XL: Writing – original draft, Writing – review & editing. XX: Writing – original draft, Writing – review & editing. TL: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Schuler, CF, Billi, AC, Maverakis, E, Tsoi, L, and Gudjonsson, J. Novel insights into atopic dermatitis. J Allergy Clin Immunol. (2023) 151:1145–54. doi: 10.1016/j.jaci.2022.10.023
3. Bylund, S, Kobyletzki, LB, Svalstedt, M, and Svensson, Å. Prevalence and incidence of atopic dermatitis: a systematic review. Acta Derm Venereol. (2020) 100:adv00160. doi: 10.2340/00015555-3510
4. Miniotti, M, Ribero, S, Mastorino, L, Ortoncelli, M, Gelato, F, Bailon, M, et al. Long-term psychological outcome of patients with moderate-to-severe atopic dermatitis continuously treated with Dupilumab: data up to 3 years. Exp Dermatol. (2023) 32:852–8. doi: 10.1111/exd.14786
5. Mastorino, L, Cantafio Duò, VL, Vecco, C, Gelato, F, Giordano, S, Roccuzzo, G, et al. Impact of comorbidities in the response of atopic patients treated with dupilumab: a real-life study up to 36 weeks. J Eur Acad Dermatol Venereol. (2022) 36:e1021–3. doi: 10.1111/jdv.18427
6. di, X, Liu, S, Xiang, L, and Jin, X. Association between the systemic immune-inflammation index and kidney stone: a cross-sectional study of NHANES 2007-2018. Front Immunol. (2023) 14:1116224. doi: 10.3389/fimmu.2023.1116224
7. Song, Y, Guo, W, Li, Z, Guo, D, Li, Z, and Li, Y. Systemic immune-inflammation index is associated with hepatic steatosis: evidence from NHANES 2015-2018. Front Immunol. (2022) 13:1058779. doi: 10.3389/fimmu.2022.1058779
8. Sroka-Tomaszewska, J, and Trzeciak, M. Molecular mechanisms of atopic dermatitis pathogenesis. Int J Mol Sci. (2021) 22:4130. doi: 10.3390/ijms22084130
9. Weidinger, S, Beck, LA, Bieber, T, Kabashima, K, and Irvine, AD. Atopic dermatitis. Nat Rev Dis Primer. (2018) 4:1. doi: 10.1038/s41572-018-0001-z
10. Heratizadeh, A, and Werfel, T. Anti-inflammatory therapies in atopic dermatitis. Allergy. (2016) 71:1666–75. doi: 10.1111/all.13065
11. Guo, W, Song, Y, Sun, Y, du, H, Cai, Y, You, Q, et al. Systemic immune-inflammation index is associated with diabetic kidney disease in type 2 diabetes mellitus patients: evidence from NHANES 2011-2018. Front Endocrinol. (2022) 13:1071465. doi: 10.3389/fendo.2022.1071465
12. Hu, B, Yang, X-R, Xu, Y, Sun, YF, Sun, C, Guo, W, et al. Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin Cancer Res. (2014) 20:6212–22. doi: 10.1158/1078-0432.CCR-14-0442
13. Ding, Q, Li, X, Lin, L, Xie, X, Jing, W, Chen, X, et al. Association between systemic immunity-inflammation index and psoriasis among outpatient US adults. Front Immunol. (2024) 15:1368727. doi: 10.3389/fimmu.2024.1368727
14. Smith, B, Collier, MR, Devjani, S, Han, G, and Wu, JJ. Association between atopic dermatitis and thyroid disease among U.S. adults in the 2001-2006 National Health and Nutrition Examination Survey. J Am Acad Dermatol. (2023) 88:889–91. doi: 10.1016/j.jaad.2022.10.017
15. Liu, J, Martin, A, Thatiparthi, A, and Wu, JJ. Association between atopic dermatitis and osteoarthritis among US adults in the 1999-2006 NHANES. J Eur Acad Dermatol Venereol. (2021) 35:e375–7. doi: 10.1111/jdv.17147
16. Iranpour, S, and Sabour, S. Inverse association between caffeine intake and depressive symptoms in US adults: data from National Health and Nutrition Examination Survey (NHANES) 2005–2006. Psychiatry Res. (2019) 271:732–9. doi: 10.1016/j.psychres.2018.11.004
17. Zhao, L, Sun, Y, Liu, Y, Yan, Z, and Peng, W. A J-shaped association between dietary inflammatory index (DII) and depression: a cross-sectional study from NHANES 2007–2018. J Affect Disord. (2023) 323:257–63. doi: 10.1016/j.jad.2022.11.052
18. Kabadi, SM, Lee, BK, and Liu, L. Joint effects of obesity and vitamin D insufficiency on insulin resistance and type 2 diabetes: results from the NHANES 2001-2006. Diabetes Care. (2012) 35:2048–54. doi: 10.2337/dc12-0235
19. Ruan, Z, Lu, T, Chen, Y, Yuan, M, Yu, H, Liu, R, et al. Association between psoriasis and nonalcoholic fatty liver disease among outpatient US adults. JAMA Dermatol. (2022) 158:745–53. doi: 10.1001/jamadermatol.2022.1609
20. Bakker, D, de Bruin-Weller, M, Drylewicz, J, van Wijk, F, and Thijs, J. Biomarkers in atopic dermatitis. J Allergy Clin Immunol. (2023) 151:1163–8. doi: 10.1016/j.jaci.2023.01.019
21. Arkwright, PD, and Koplin, JJ. Impact of a decade of research into atopic dermatitis. J Allergy Clin Immunol Pract. (2023) 11:63–71. doi: 10.1016/j.jaip.2022.09.021
22. Tang, Y, Peng, B, Liu, J, Liu, Z, Xia, Y, and Geng, B. Systemic immune-inflammation index and bone mineral density in postmenopausal women: a cross-sectional study of the National Health and Nutrition Examination Survey (NHANES) 2007-2018. Front Immunol. (2022) 13:975400. doi: 10.3389/fimmu.2022.975400
Keywords: atopic dermatitis, systemic immune-inflammation index, cross-sectional study, National Health and Nutrition Examination Survey, outpatient US adults
Citation: Ding Q, Lin L, Li X, Xie X and Lu T (2024) Association between systemic immune-inflammation index and atopic dermatitis: a cross-sectional study of NHANES 2001–2006. Front. Med. 11:1461596. doi: 10.3389/fmed.2024.1461596
Edited by:
Simone Ribero, University of Turin, ItalyCopyright © 2024 Ding, Lin, Li, Xie and Lu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tao Lu, bHV0YW9paEAxMjYuY29t
 Qike Ding
Qike Ding Tao Lu
Tao Lu