- 1Department of Intensive Care Unit, Shanxi Bethune Hospital, Shanxi Academy of Medical Sciences, Tongji Shanxi Hospital, Third Hospital of Shanxi Medical University, Taiyuan, Shanxi, China
- 2Department of Intensive Care Unit, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, Hubei, China
- 3Heping Hospital Affiliated to Changzhi Medical College, Changzhi, Shanxi, China
- 4Linfen Central Hospital, Linfen, Shanxi, China
Background: Sepsis management in the Intensive Care Unit (ICU) presents a significant challenge within contemporary healthcare. The primary challenge lies in ensuring the timely and appropriate utilization of antibiotics. Inappropriate antibiotic use in sepsis management can result in a multitude of adverse outcomes. There has been insufficient focus on thoroughly understanding and resolving the issues related to the improper application of antibiotics in sepsis treatment by physicians and pharmacists. This gap in research is concerning, considering its potential implications for patient outcomes and public health. This study aimed to assess the knowledge, attitudes and practices (KAP) among physicians and pharmacists toward antibiotic use in sepsis.
Methods: This web-based cross-sectional study was conducted at Shanxi Bethune Hospital between June 2023 and October 2023. A self-designed questionnaire was developed to collect demographic information of physicians and pharmacists, and to assess their knowledge, attitudes and practices toward antibiotic use in sepsis.
Results: A total of 200 valid questionnaires were collected. Among the participants, 115 (57.5%) were female and 118 (59%) had experience with ICU patient management. The mean knowledge, attitudes and practices scores were 10.2 ± 1.14 (possible range: 0–12), 45.88 ± 4.00 (possible range: 10–50) and 48.38 ± 5.84 (possible range: 11–55), respectively. Multivariate logistic regression showed that attitudes (OR = 1.59, 95%CI: 1.34–1.87, p < 0.001), work experience of 15 years and above (OR = 7.17, 95%CI: 2.33–22.0, p = 0.001) were independently associated with proactive practices. For physicians, the structural equation model (SEM) demonstrated that attitudes directly affects practices, as indicated by a path coefficient of 0.91 (p < 0.001). For pharmacist, SEM showed that knowledge directly affect attitudes, with a path coefficient of 0.75 (p < 0.024), moreover, attitudes directly affect practices, with a path coefficient of 0.87 (p < 0.001).
Conclusion: The findings revealed that physicians and pharmacists have sufficient knowledge, active attitudes, and proactive practices toward the antibiotic use in sepsis. Nonetheless, the findings also reveal the persistence of certain misconceptions, alongside notable shortcomings in both attitudes and practices. Comprehensive training programs are imperative for enhancing the practices of physicians and pharmacists in this field.
Introduction
Sepsis in the intensive care unit (ICU) presents a significant challenge in modern healthcare (1). The mortality associated with sepsis varies from 15% in patients with sepsis without shock to 56% in those with sepsis accompanied by shock (2). The primary pathogens associated with sepsis include Pseudomonas aeruginosa, Staphylococcus aureus, and Candida albicans, all of which exhibit serious multi-drug resistance (3), and the management of sepsis in the ICU is heavily reliant on the use of antibiotics (4).
In recent years, sepsis management has emphasized early identification and prompt antibiotic administration as key strategies to improve outcomes. Guidelines now recommend initiating antibiotics within 1 h for patients with septic shock or a high likelihood of sepsis, as early antibiotic use has been linked to reduced mortality, particularly in septic shock cases (5). To optimize treatment, the choice of antibiotics should consider patient history, comorbidities, and local resistance patterns, with adjustments as culture results become available (6).
Challenge lies in the timely and appropriate use of these antibiotics. Inappropriate use of antibiotics in sepsis management can lead to several adverse outcomes. Previous research highlights that these adverse effects encompass detrimental drug interactions, escalated toxicity, the emergence of antibiotic resistance, and the liberation of endotoxins, which are crucial in the pathogenesis of sepsis and septic shock (7, 8). Subsequent studies have established a correlation between the inappropriate administration of antibiotics and an increase in both mortality and adverse clinical events (9). Moreover, the emergence of multi-drug resistant strains complicates the choice of empirical antibiotic therapy, making it crucial to consider local microbial and resistance patterns (10).
Despite the indispensable role antibiotics play in sepsis management, a noteworthy gap persists in the current research landscape. Inadequate attention has been devoted to a comprehensive understanding and resolution of the inappropriate application of antibiotics in the treatment of sepsis by medical practitioners and pharmacists. This research deficit raises significant concerns, given the potential repercussions for patient outcomes and public health (11, 12). Consequently, a meticulous examination of the knowledge and attitudes of these professional groups regarding antibiotic utilization in sepsis becomes imperative to cultivate judicious clinical practices. While numerous studies have explored antibiotic perceptions, none are specific to this critical area of sepsis management (13–15).
The conceptual framework of knowledge, attitudes, and practices (KAP) research serves as a valuable lens for exploring the intricate dynamics surrounding antibiotic utilization in sepsis (16, 17). Thus, this study aimed to address the current knowledge gap by elucidating the complexities of attitudes and identifying the actual practices influencing antibiotic usage in the critical context of sepsis. This study aims to support the development of targeted clinical interventions.
Materials and methods
Study design and participants
This cross-sectional survey was conducted at Shanxi Bethune Hospital between June 2023 and October 2023. Participants in the study comprised physicians and clinical pharmacists affiliated with this institution, with a total of 200 valid responses collected. In the study population, 127 participants were classified as physicians. In the context of the Chinese medical system, fully licensed physicians may hold bachelor’s or master’s degrees in medicine. No nurse practitioners, physician assistants, or other roles were included in this study. This classification aligns with the standard definitions of medical practice in China. Notably, only participants in direct patient care roles were included, while other roles, such as nurse practitioners or physician assistants, were excluded. This study was approved by the Ethic Committee of Shanxi Bethune Hospital (No. YXLL-2023-107), which functions as an Institutional Review Board (IRB) at the hospital. Comprehensive review and approval were conducted based on the submitted protocol, including the Application Form for Medical Ethics Review, Sample Informed Consent Form, and Clinical Research Protocol. All participants provided written informed consent prior to participation.
Questionnaire
The questionnaire was formulated with guidance derived from Sepsis Guidelines (18) and relevant literature on antibiotics management of sepsis (19, 20). The initial draft underwent refinements incorporating feedback from three senior experts, each holding the title of associate professor and specializing in ICU and Clinical Pharmacy. Following these expert revisions, a preliminary trial was conducted on a limited scale (n = 41), resulting in a Cronbach’s alpha coefficient value of 0.895, indicating good internal consistency.
The final questionnaire, administered in Chinese, encompassed four dimensions: demographic information, knowledge, attitudes, and practices. Demographic information comprised 11 items, while the knowledge, attitudes, and practices dimensions included 12, 11, and 11 items, respectively. Knowledge items were scored 1 point for a correct answer and 0 points otherwise, resulting in a possible score range of 0–12. The attitude items scored on a five-point Likert scale ranging from very positive (5 points) to very negative (1 point), wherein questions A11 are designated exclusively for descriptive analysis purposes, with a possible score range of 10 to 50. Similarly, practice items were scored on a five-point Likert scale, varying from very consistent (5 points) to very inconsistent (1 point), with a possible score range of 11 to 55 (see Supplementary material).
Data collection was conducted using an online questionnaire hosted on Sojump.1 Prior to accessing the questionnaire, participants were required to select the option “I agree to participate in this study,” thereby providing their consent. While no personally identifiable information was collected, a temporary IP restriction was implemented to prevent duplicate submissions. The IP addresses were stored temporarily during the submission process but were not retained after data collection was completed. This approach aligns with ethical practices outlined in previous studies (21, 22).
Sample size calculation
The sample size calculation was based on a ratio of 5–20 times the number of questionnaire items, as recommended (23). The KAP questionnaire includes 34 items (12 for Knowledge, 11 for Attitude, and 11 for Practice). To account for a potential 10% missing data rate, the target sample size was set to exceed 189 questionnaires.
Statistical analysis
STATA 17.0 (Stata Corporation, College Station, TX, USA) was employed for statistical analysis. Continuous variables were presented as mean ± SD, while categorical variables were expressed as n (%). Continuous variables conforming to a normal distribution were assessed using the t-test or ANOVA. For multivariate analysis, the median (50% distribution) of the total score was used as the threshold value. Pearson correlation was used to analyze the correlation between knowledge, attitudes, and practices. The structural equation model (SEM) of knowledge, attitudes and practices among physicians and pharmacists toward antibiotic use in sepsis was constructed with AMOS 24.0 (IBM, NY, United States). The hypotheses as following: (1) knowledge had direct effects on attitude, (2) knowledge had direct effects on practice, and (3) attitude had direct effects on practice. The model fitting was evaluated with CMIN/DF (Chi-square fit statistics/degree of freedom), RMSEA (root mean square error of approximation), IFI (incremental fix index), TLI (Tucker-Lewis index) and CFI (comparative fix index). Two-sided p < 0.05 were considered statistically significant.
Results
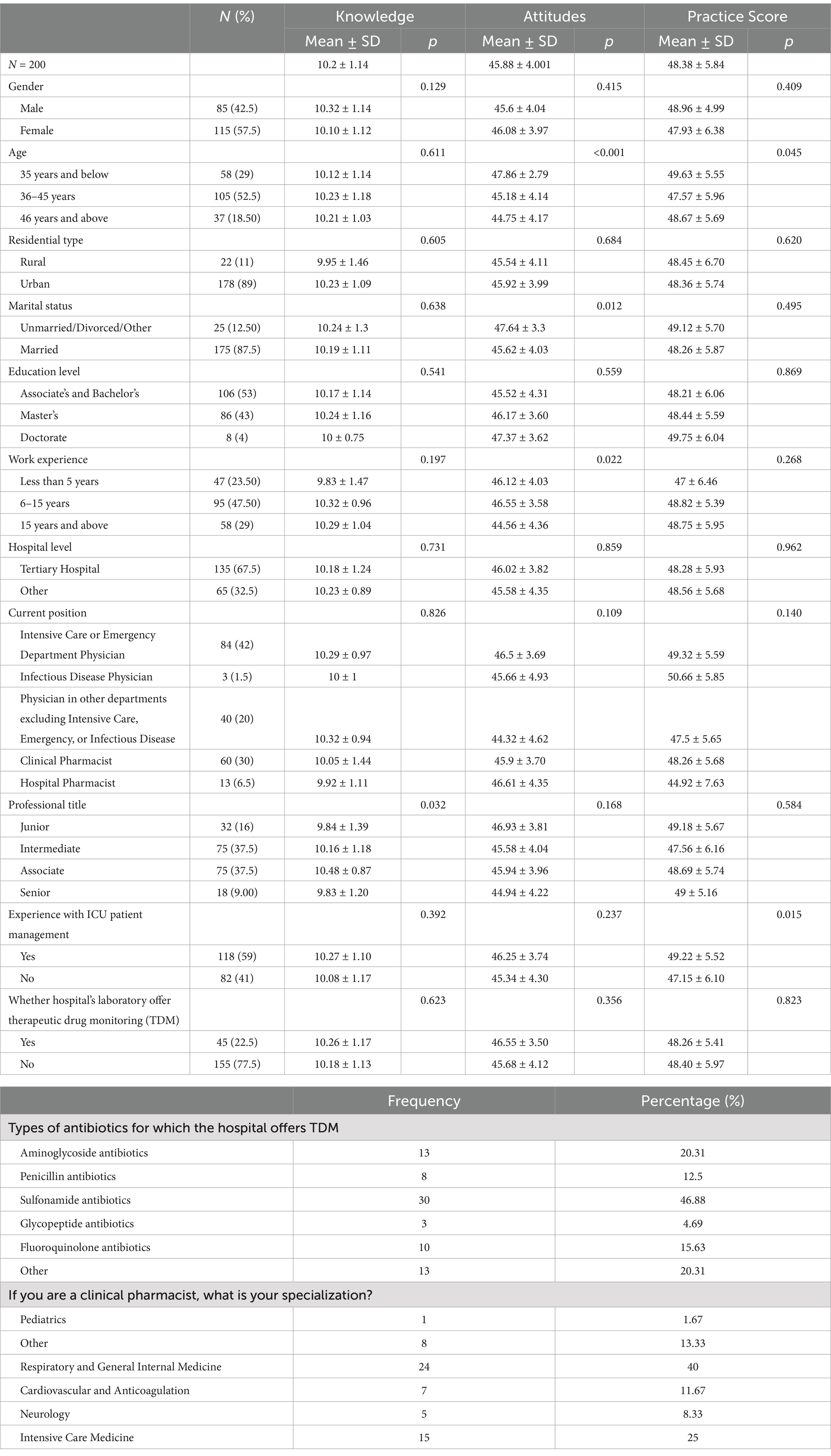
A total of 200 valid questionnaires were collected. Among the participants, 115 (57.5%) were female, 105 (52.5%) aged 36–45 years, 106 (53%) had graduated from college and undergraduate program, 95 (47.50%) had work experience of 6–15 years, 135 (67.5%) in tertiary hospitals, and 118 (59%) had experience in managing ICU patients. Significant demographic differences, including age (p < 0.001), marital status (p = 0.012), work experience (p = 0.022), professional title (p = 0.032), and ICU management experience (p = 0.015), were observed among participants, which may influence knowledge, attitudes, and practices scores. Therapeutic drug monitoring (TDM) for antibiotics was conducted in hospitals where 45 (22.5%) of the respondents were employed, with sulfonamide antibiotics comprising 46.88% of the TDM. Furthermore, 24 (40%) of the clinical pharmacists were affiliated with the respiratory and general internal medicine departments.
The mean knowledge, attitudes and practices scores were 10.2 ± 1.14 (possible range: 0–12), 45.88 ± 4.001 (possible range: 10–50) and 48.38 ± 5.84 (possible range: 11–55), respectively. The knowledge varied from those with different Professional Title (p = 0.032). As for the attitudes, there were difference among physicians and pharmacists with different age (p < 0.001), marital status (p = 0.012) and work experience (p = 0.022). The difference of practices scores were found among physicians and pharmacists with different age (p = 0.045) and ICU patient management experience (p = 0.015) (Table 1).
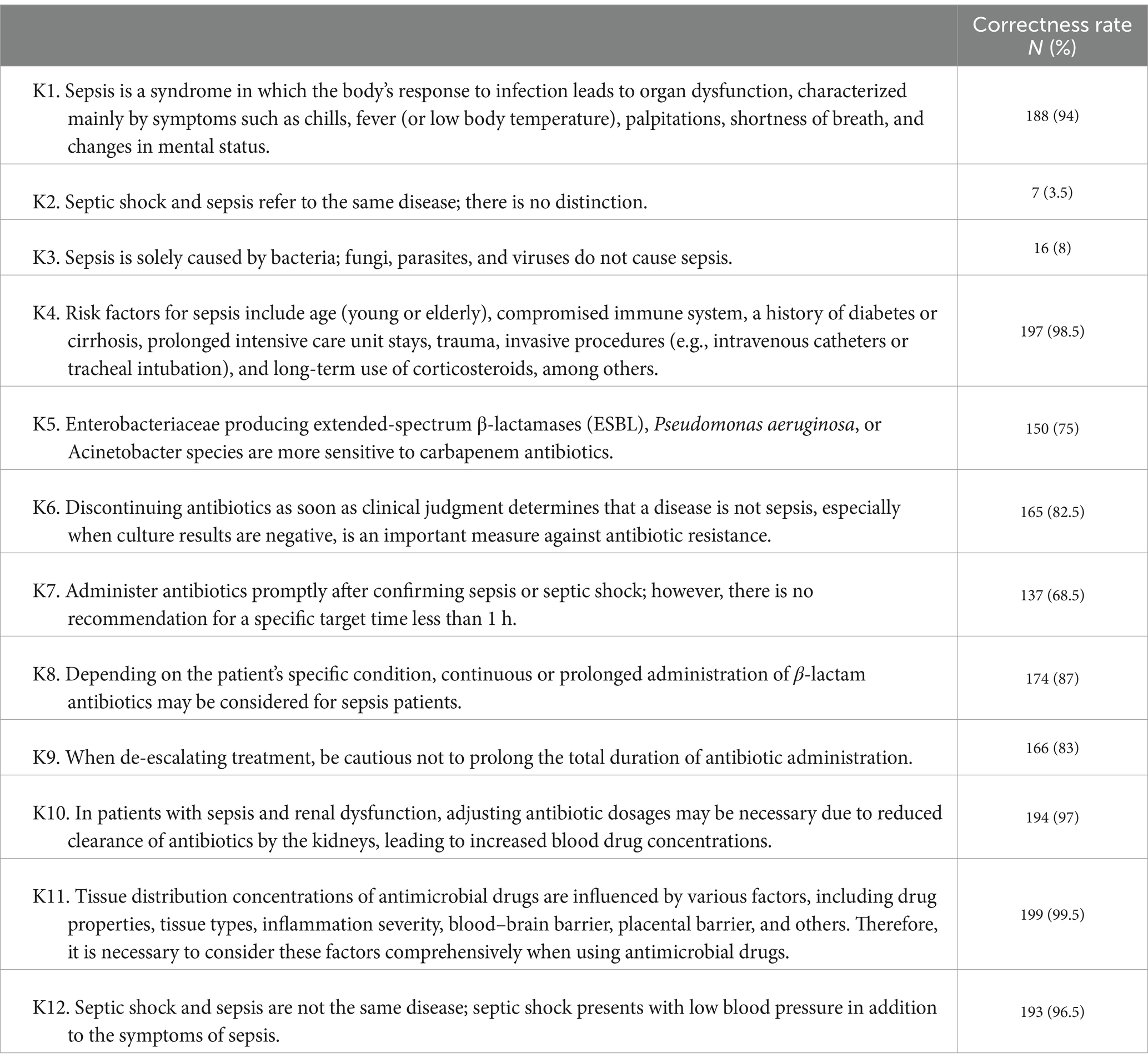
Most participants recognized the syndrome’s complexity and the distinction between sepsis and septic shock, with high correctness rates of 94% (K1) and 96.5% (K12), respectively. However, 31.5% of them were still unclear about the timing of using antibiotics to treat sepsis (K7). 25% were unable to clearly recongnize that Enterobacteriaceae bacteria, Pseudomonas aeruginosa, or Acinetobacter that express ESBLs are more sensitive to carbapenem antibiotics (K5). Moreover, there was a notable misconception that sepsis is only caused by bacteria, with a correctness rate of only 8% (K3) and that septic shock and sepsis refer to the same disease, with a correctness rate of 3.5% (K2) (Table 2).
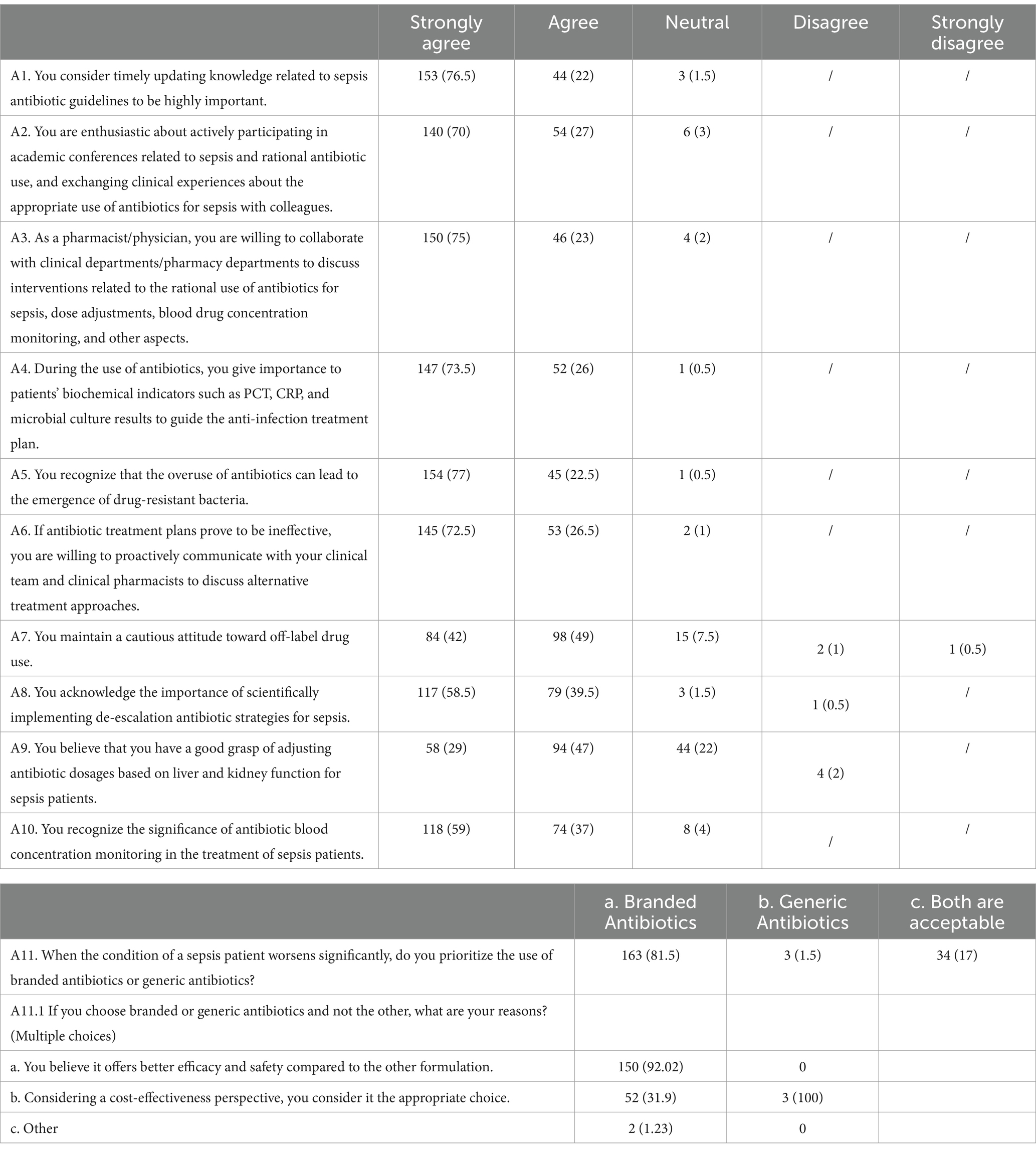
Attitudes toward antibiotic use in sepsis were generally proactive, with a majority agreeing on the importance of timely knowledge updates, active participation in academic conferences, and collaborative interventions for rational antibiotic use. A significant majority of participants (76.5%) strongly agreed on the importance of timely updating knowledge on sepsis antibiotic guidelines. Moreover, 81.5% of the respondents preferred branded antibiotics when the condition of a sepsis patient worsened significantly, mainly due to perceived better efficacy and safety (Table 3).
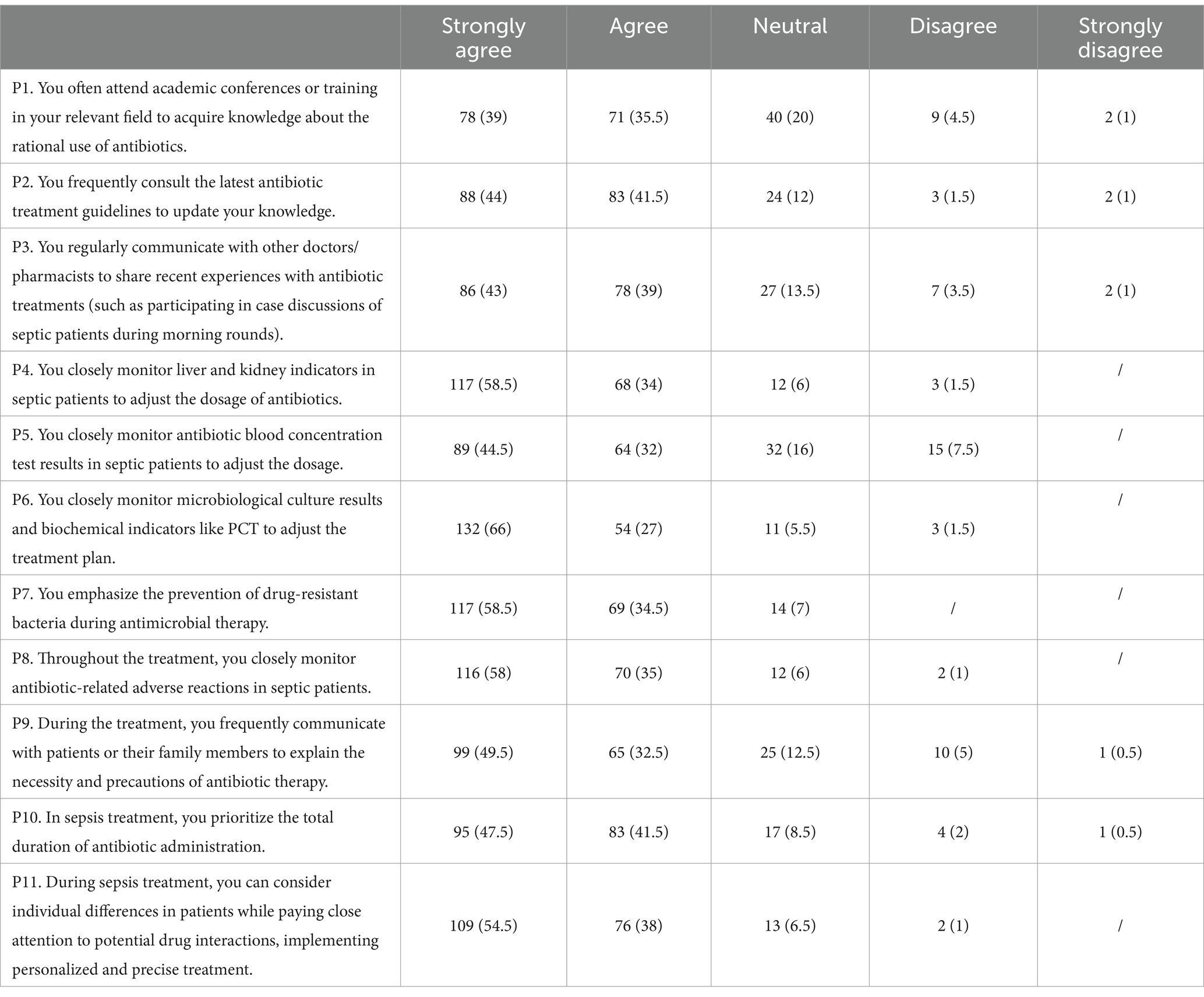
In practice, a significant number of participants reported regular attendance at relevant academic conferences (39%) and consultation of the latest guidelines (44%). There was also a strong emphasis on monitoring biochemical indicators (P4&P6) and drug concentrations to guide treatment in sepsis patients (P11) (Table 4).
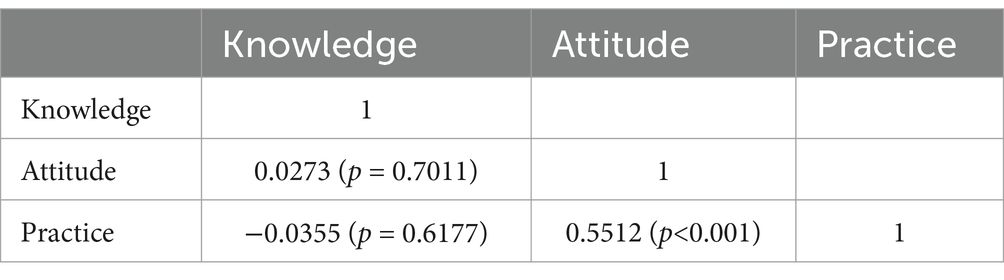
Pearson’s analysis was performed to assess the relationship between knowledge, attitudes and practices. It was shown that attitudes and practices were positively correlated (r = 0.5512, p < 0.001) (Table 5).
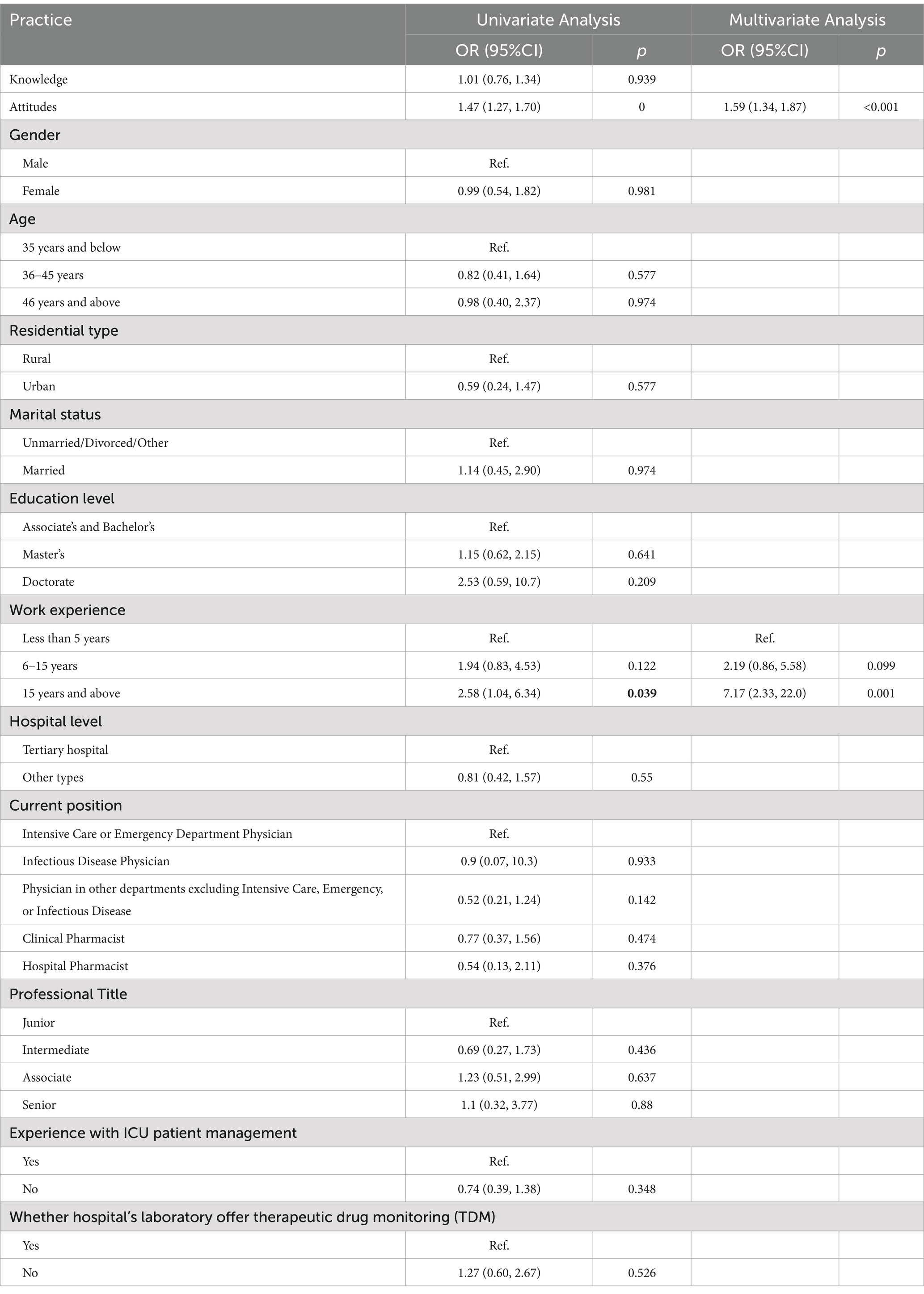
Multivariate logistic regression showed that attitudes (OR = 1.59, 95% CI: 1.34–1.87, p < 0.001), work experience of 15 years and above (OR = 7.17, 95% CI: 2.33–22.0, p = 0.001) were independently associated with practices (Table 6).
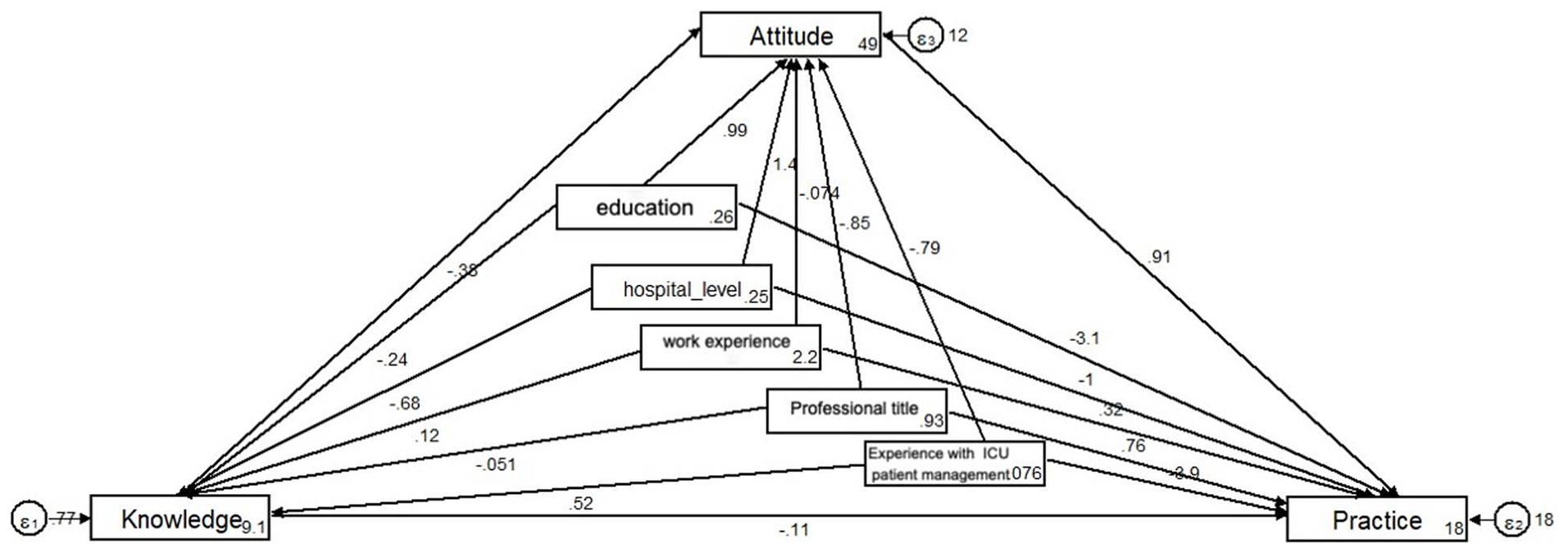
The structural equation model was established to further investigate whether physicians’/pharmacists’ knowledge and attitude toward antibiotic use in sepsis affect their practice, whether attitude plays an intermediary role between knowledge and practice, and whether knowledge can directly affect their practice. The hypotheses underlying this study are as follows: (1) knowledge directly affects attitudes, (2) knowledge directly affects practices, and (3) attitudes directly affect practices (24).
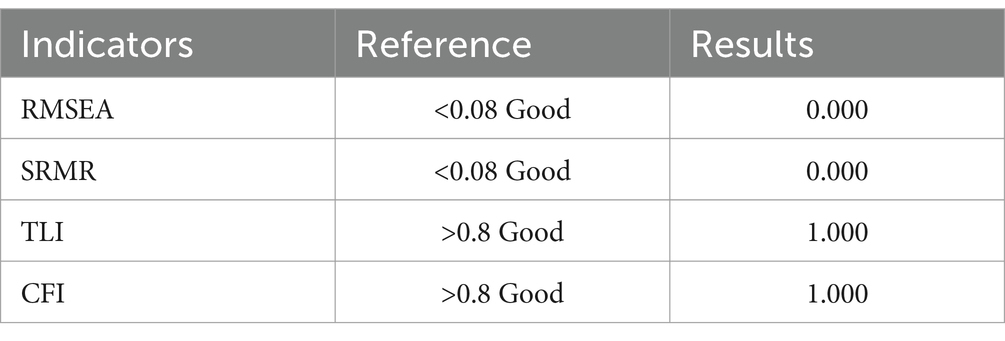
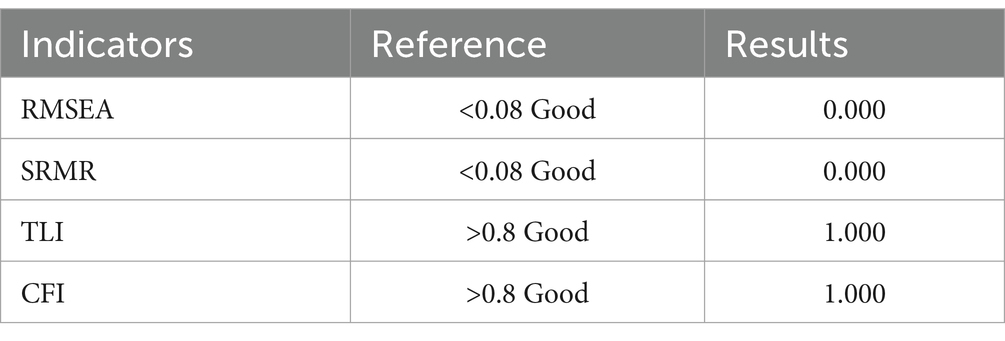
For physicians, the fitting index of the structural model (RMSEA = 0.000; SRMR = 0.000; TLI = 1.000; CFI = 1.000) outperformed the respective threshold value, signifying that the data satisfactorily fit the structural model (Table 7). The SEM results support hypothesis (3), showing that attitudes directly affect practices, as indicated by a path coefficient of 0.91 (p < 0.001) (Figure 1 and Table 8). However, the SEM did not show a significant direct effect of knowledge on practices, suggesting that while knowledge is essential, its influence on practices may be mediated through attitudes (Figure 1; Table 8).
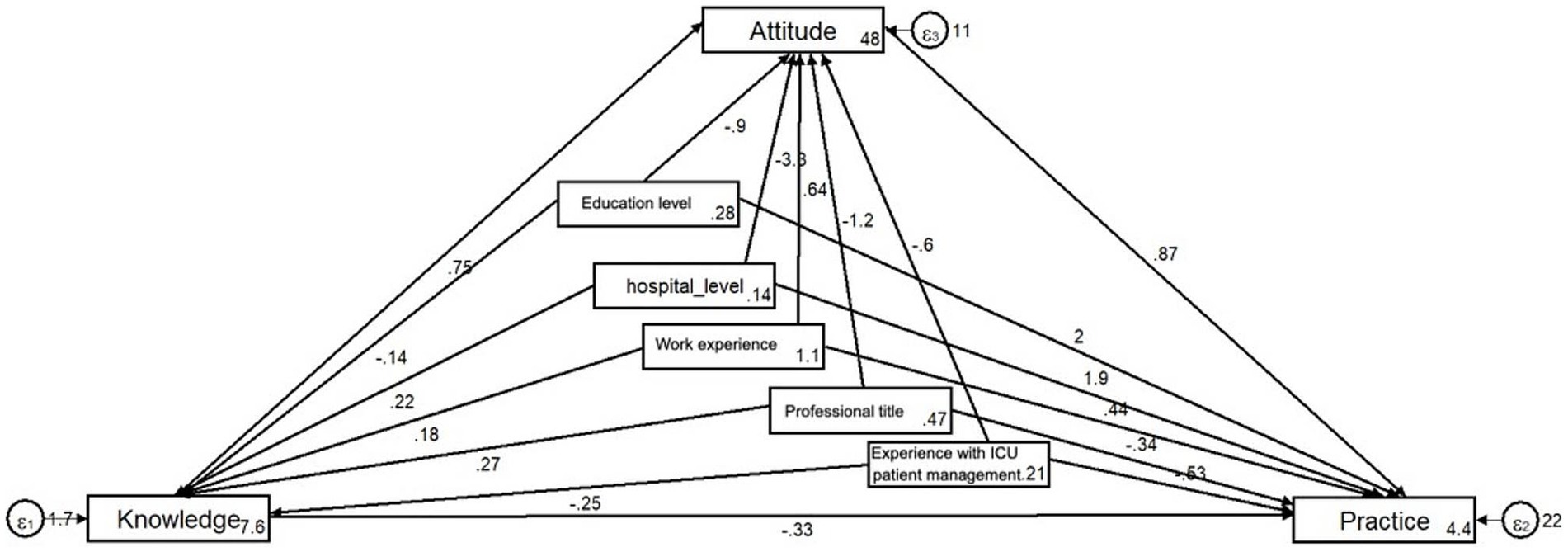
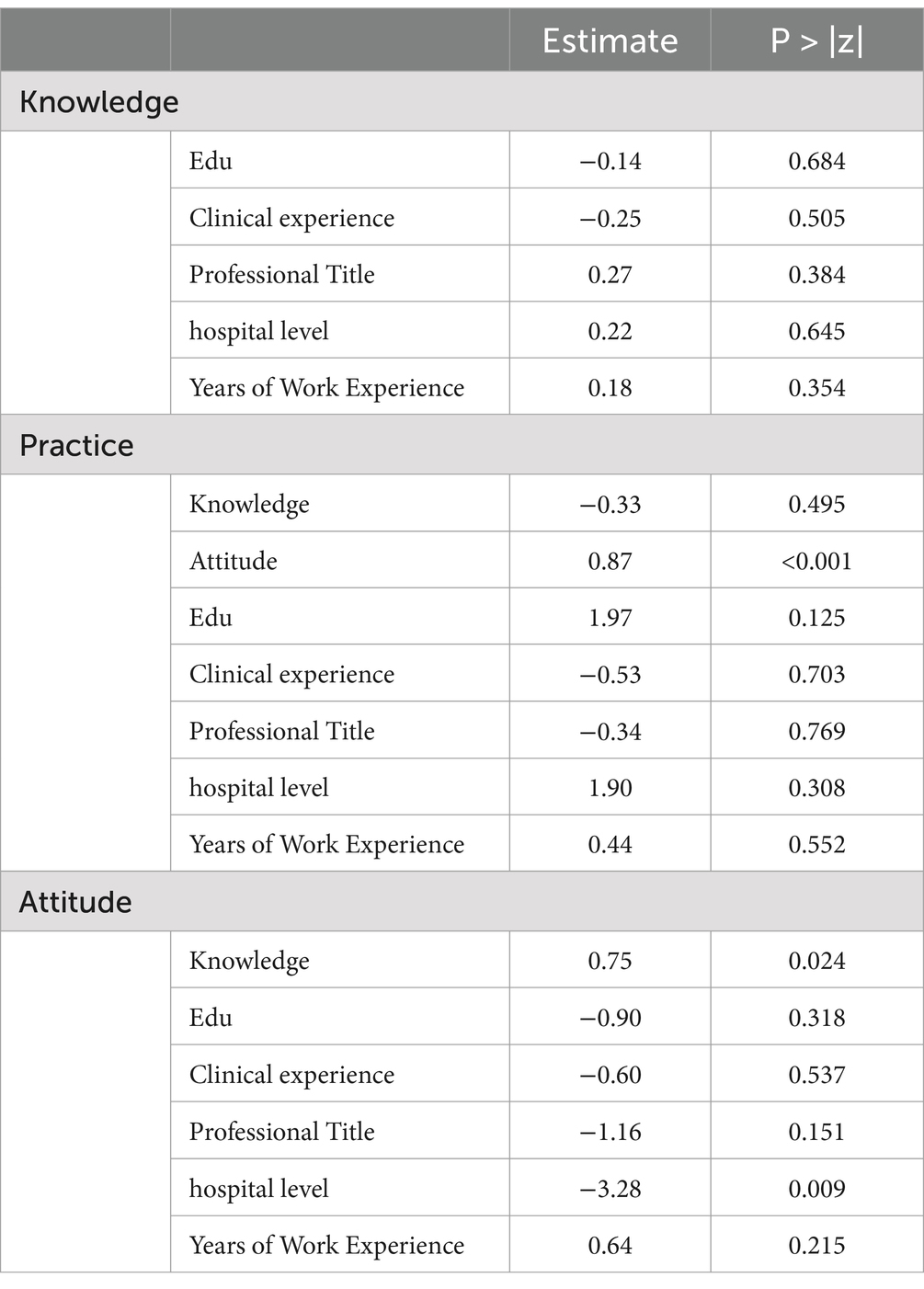
For pharmacists, the same satisfactory structural model was also fitted (Table 9). SEM showed that knowledge directly affects attitudes, supporting hypothesis (1), with a path coefficient of 0.75 (p = 0.024). Moreover, attitudes have a strong direct effect on practices, supporting hypothesis (3), with a path coefficient of 0.87 (p < 0.001) (Figure 2; Table 10).
Discussion
The findings revealed that physicians and pharmacists have sufficient knowledge, active attitudes, and proactive practices toward antibiotic use in sepsis. Nonetheless, the results also reveal the persistence of certain misconceptions, alongside notable shortcomings in both attitudes and practices, indicating that comprehensive training programs are imperative for enhancing the practices of physicians and pharmacists in this field.
The results of this study indicate a generally positive orientation of physicians and pharmacists toward appropriate antibiotic use in sepsis, as evidenced by high mean scores in knowledge, attitude, and practice. However, certain demographic factors were found to influence these scores, and targeted educational interventions based on professional status and demographic characteristics could address these variations (25, 26).
The results of the knowledge assessment revealed a generally high correct rate among participants, indicating a solid understanding of key concepts related to sepsis and antibiotic management. However, certain deficiencies were identified, particularly in the recognition of distinctions between sepsis and septic shock. A notable proportion of respondents incorrectly asserted that septic shock and sepsis are synonymous, overlooking the crucial distinction of low blood pressure in septic shock. Educational interventions should prioritize emphasizing the unique clinical features of septic shock, ensuring accurate differentiation from sepsis. Additionally, interventions should focus on reinforcing the understanding of prompt antibiotic administration while considering patient-specific conditions, such as renal dysfunction, to avoid suboptimal dosing and potential adverse outcomes (27, 28). These targeted educational efforts can contribute to a more comprehensive and accurate knowledge base among healthcare professionals involved in sepsis management.
The assessment of attitudes toward sepsis management and antibiotic use revealed generally positive inclinations among healthcare professionals. However, certain deficiencies were identified, particularly in the prioritization of branded antibiotics over generics in the event of a significant worsening of a sepsis patient’s condition. A substantial percentage of respondents expressed a preference for branded antibiotics, citing perceived better efficacy and safety. This finding suggests a potential inclination toward a preference for brand names that may not always align with evidence-based practices or cost-effectiveness considerations. Previous studies have highlighted the importance of promoting rational antibiotic use, considering both efficacy and cost-effectiveness, to address concerns related to antibiotic resistance and healthcare costs (29). To improve clinical practice, interventions should focus on antibiotic stewardship principles, emphasizing evidence-based decision-making and cost-effectiveness without compromising patient safety. Additionally, collaborative efforts between healthcare professionals, clinical pharmacists, and pharmacy departments, as expressed in the positive attitude toward collaboration, can be leveraged to enhance antibiotic management strategies. This underscores the need for multifaceted interventions that address knowledge gaps and promote a balanced approach to antibiotic selection in sepsis management.
The evaluation of clinical practices related to antibiotic use in sepsis management indicates a generally positive adherence to evidence-based practices among healthcare professionals. However, certain areas of improvement were identified, such as the prioritization of the total duration of antibiotic administration, which exhibited a lower agreement rate. Previous research has emphasized the importance of individualizing antibiotic duration based on patient response and clinical indicators, rather than adhering strictly to fixed durations, to optimize patient outcomes and minimize the risk of antibiotic resistance (30). To address this deficiency, interventions should focus on reinforcing the principles of antibiotic stewardship, incorporating flexible duration strategies that align with patient-specific factors. Additionally, the practices of monitoring antibiotic-related adverse reactions, communicating with patients or their family members, and considering individual differences should be further promoted (31). These recommendations underscore the need for continuous education and awareness programs to further optimize clinical practices in antibiotic use during sepsis treatment.
One limitation of this study is that the study relies on self-reported data from physicians and pharmacists, which could introduce response bias or social desirability bias. The cross-sectional design provides a snapshot of the participants’ knowledge, attitudes, and practices at a specific point in time, but it does not allow for the examination of causality or changes over time. The use of a web-based questionnaire may also introduce a selection bias, as participants with internet access and familiarity with online surveys may differ from those without. Additionally, as a single-site study conducted within the ICU of Shanxi Bethune Hospital, the findings may be limited in generalizability. Only three infectious disease physicians were included due to the ICU team configuration at this hospital. Thus, they were grouped within the broader physician cohort rather than analyzed separately. Furthermore, significant demographic differences among participants, including age, marital status, work experience, professional title, and ICU management experience, may influence knowledge, attitudes, and practices scores. These discrepancies could limit the conclusions to the major demographic categories represented, and findings should be interpreted with caution when generalizing to broader populations. Despite these limitations, the study offers valuable insights into the current state of knowledge, attitudes, and practices among physicians and pharmacists in the specified setting.
Overall, the results underscore the need for tailored educational interventions that specifically address identified knowledge gaps and misconceptions. Such interventions would promote optimal antibiotic stewardship in sepsis care, improving both clinical decision-making and patient outcomes.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Ethic Committee of Shanxi Bethune Hospital (No. YXLL-2023-107). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JZ: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. HS: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Writing – original draft, Writing – review & editing. YX: Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. ZZ: Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. YZ: Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by TLR4/NF-KB signaling pathway regulation of mitochondrial function on acute kidney injury in sepsis mechanism (202203021222350).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2024.1454521/full#supplementary-material
Footnotes
References
1. Zhang, L, Huang, T, Xu, F, Li, S, Zheng, S, Lyu, J, et al. Prediction of prognosis in elderly patients with sepsis based on machine learning (random survival forest). BMC Emerg Med. (2022) 22:26. doi: 10.1186/s12873-022-00582-z
2. Pieroni, M, Olier, I, Ortega-Martorell, S, Johnston, BW, and Welters, ID. In-hospital mortality of Sepsis differs depending on the origin of infection: an investigation of predisposing factors. Front Med. (2022) 9:915224. doi: 10.3389/fmed.2022.915224
3. Niederman, MS, Baron, RM, Bouadma, L, Calandra, T, Daneman, N, DeWaele, J, et al. Initial antimicrobial management of sepsis. Crit Care. (2021) 25:307. doi: 10.1186/s13054-021-03736-w
4. Rhee, C, Kadri, SS, Dekker, JP, Danner, RL, Chen, HC, Fram, D, et al. Prevalence of antibiotic-resistant pathogens in culture-proven Sepsis and outcomes associated with inadequate and broad-Spectrum empiric antibiotic use. JAMA Netw Open. (2020) 3:e202899. doi: 10.1001/jamanetworkopen.2020.2899
5. Evans, L, Rhodes, A, Alhazzani, W, Antonelli, M, Coopersmith, CM, French, C, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. (2021) 47:1181–247. doi: 10.1007/s00134-021-06506-y
6. Kamath, S, Hammad Altaq, H, and Abdo, T. Management of Sepsis and septic shock: what have we learned in the last two decades? Microorganisms. (2023) 11:2231. doi: 10.3390/microorganisms11092231
7. Ahmed, H, Farewell, D, Francis, NA, Paranjothy, S, and Butler, CC. Choice of empirical antibiotic therapy and adverse outcomes in older adults with suspected urinary tract infection: cohort study. Open Forum Infect Dis. (2019) 6:ofz039. doi: 10.1093/ofid/ofz039
8. Liang, CY, Yang, YY, Hung, CC, Wang, TH, and Hsu, YC. Prognostic values of the timing of antibiotic administration and the Sepsis bundle component in elderly patients with septic shock: a retrospective study. Shock. (2022) 57:181–8. doi: 10.1097/SHK.0000000000001854
9. Nadig, NR, and Ford, DW. A consensus: everyone agrees collectively but no one believes individually. Crit Care Med. (2019) 47:1470–2. doi: 10.1097/CCM.0000000000003939
10. Lertwattanachai, T, Montakantikul, P, Tangsujaritvijit, V, Sanguanwit, P, Sueajai, J, Auparakkitanon, S, et al. Clinical outcomes of empirical high-dose meropenem in critically ill patients with sepsis and septic shock: a randomized controlled trial. J Intensive Care. (2020) 8:26. doi: 10.1186/s40560-020-00442-7
11. Chang, Y, Chusri, S, Sangthong, R, McNeil, E, Hu, J, Du, W, et al. Clinical pattern of antibiotic overuse and misuse in primary healthcare hospitals in the southwest of China. PLoS One. (2019) 14:e0214779. doi: 10.1371/journal.pone.0214779
12. Diamant, M, Baruch, S, Kassem, E, Muhsen, K, Samet, D, Leshno, M, et al. A game theoretic approach reveals that discretizing clinical information can reduce antibiotic misuse. Nat Commun. (2021) 12:1148. doi: 10.1038/s41467-021-21088-5
13. Al-Halawa, DA, Seir, RA, and Qasrawi, R. Antibiotic resistance knowledge, attitudes, and practices among pharmacists: a cross-sectional study in West Bank, Palestine. J Environ Public Health. (2023) 2023:1–11. doi: 10.1155/2023/2294048
14. Kosiyaporn, H, Chanvatik, S, Issaramalai, T, Kaewkhankhaeng, W, Kulthanmanusorn, A, Saengruang, N, et al. Surveys of knowledge and awareness of antibiotic use and antimicrobial resistance in general population: a systematic review. PLoS One. (2020) 15:e0227973. doi: 10.1371/journal.pone.0227973
15. Rahbi, FA, Salmi, IA, Khamis, F, Balushi, ZA, Pandak, N, Petersen, E, et al. Physicians' attitudes, knowledge, and practices regarding antibiotic prescriptions. J Global Antimicrobial Resist. (2023) 32:58–65. doi: 10.1016/j.jgar.2022.12.005
16. Mallah, N, Rodríguez-Cano, R, Badro, DA, Figueiras, A, Gonzalez-Barcala, FJ, and Takkouche, B. Development and validation of a knowledge, attitude and practice questionnaire on antibiotic use in Arabic and French languages in Lebanon. Int J Environ Res Public Health. (2022) 19:687. doi: 10.3390/ijerph19020687
17. Wang, J, Sheng, Y, Ni, J, Zhu, J, Zhou, Z, Liu, T, et al. Shanghai Parents' perception and attitude towards the use of antibiotics on children: a cross-sectional study. Infect Drug Resist. (2019) 12:3259–67. doi: 10.2147/IDR.S219287
18. Chen, AX, Simpson, SQ, and Pallin, DJ. Sepsis Guidelines. N Engl J Med. (2019) 380:1369–71. doi: 10.1056/NEJMclde1815472
19. Esposito, S, De Simone, G, Boccia, G, De Caro, F, and Pagliano, P. Sepsis and septic shock: new definitions, new diagnostic and therapeutic approaches. J Global Antimicrobial Resist. (2017) 10:204–12. doi: 10.1016/j.jgar.2017.06.013
20. Liu, VX, Fielding-Singh, V, Greene, JD, Baker, JM, Iwashyna, TJ, Bhattacharya, J, et al. The timing of early antibiotics and hospital mortality in Sepsis. Am J Respir Crit Care Med. (2017) 196:856–63. doi: 10.1164/rccm.201609-1848OC
21. Gong, P, Shen, J, Yang, Y, Xue, D, Lu, H, Zhuang, Q, et al. Knowledge, attitude, and practice toward varicocele in patients with varicoceles: a cross-sectional study in Chinese patients. Int J Gen Med. (2024) 17:3423–32. doi: 10.2147/IJGM.S471004
22. Luo, Z, Guo, W, Zhou, H, and Chen, Z. Knowledge, attitude, and practice toward lung cancer risk among offspring of lung cancer patients: a cross-sectional study. Sci Rep. (2024) 14:18003. doi: 10.1038/s41598-024-69142-8
23. Naqvi, AA, Hassali, MA, Rizvi, M, Zehra, A, Nisa, ZU, Islam, MA, et al. Validation of the general medication adherence scale in Pakistani patients with rheumatoid arthritis. Front Pharmacol. (2020) 11:1039. doi: 10.3389/fphar.2020.01039
24. Khalid, A, Haque, S, Alvi, S, Ferdous, M, Genereux, O, Chowdhury, N, et al. Promoting health literacy about Cancer screening among Muslim immigrants in Canada: perspectives of imams on the role they can play in community. J Prim Care Community Health. (2022) 13:21501319211063051. doi: 10.1177/21501319211063051
25. Michaelidou, M, Karageorgos, SA, and Tsioutis, C. Antibiotic use and antibiotic resistance: public awareness survey in the Republic of Cyprus. Antibiotics. (2020) 9:759. doi: 10.3390/antibiotics9110759
26. Walker, SV, Steffens, B, Sander, D, and Wetsch, WA. Implementation of antibiotic stewardship improves the quality of blood culture diagnostics at an intensive care unit of a university hospital. J Clin Med. (2022) 11:3675. doi: 10.3390/jcm11133675
27. Nakayama, I, Izawa, J, Mouri, H, Kitamura, T, and Shiotsuka, J. Mortality and detailed characteristics of pre-ICU qSOFA-negative patients with suspected sepsis: an observational study. Ann Intensive Care. (2018) 8:44. doi: 10.1186/s13613-018-0389-3
28. Yao, L, Yin, J, Huo, R, Yang, D, Shen, L, Wen, S, et al. The effects of the primary health care providers' prescription behavior interventions to improve the rational use of antibiotics: a systematic review. Global Health Res Policy. (2020) 5:45. doi: 10.1186/s41256-020-00171-2
29. Huemer, M, Mairpady Shambat, S, Brugger, SD, and Zinkernagel, AS. Antibiotic resistance and persistence-implications for human health and treatment perspectives. EMBO Rep. (2020) 21:e51034. doi: 10.15252/embr.202051034
30. Kim, MS, Kim, JH, Ryu, S, Lee, SW, Yon, DK, Kim, E, et al. Comparative efficacy and optimal duration of first-line antibiotic regimens for acute otitis media in children and adolescents: a systematic review and network meta-analysis of 89 randomized clinical trials. World J Pediatrics. (2023) 20:219–29. doi: 10.1007/s12519-023-00716-8
Keywords: knowledge, attitudes, practices, antibiotic, sepsis, cross-sectional study
Citation: Zhang J, Shi H, Xia Y, Zhu Z and Zhang Y (2025) Knowledge, attitudes, and practices among physicians and pharmacists toward antibiotic use in sepsis. Front. Med. 11:1454521. doi: 10.3389/fmed.2024.1454521
Edited by:
Theodore Pak, Massachusetts General Hospital and Harvard Medical School, United StatesReviewed by:
Yaser Alahmadi, University of Taibah, Saudi ArabiaFauna Herawati, University of Surabaya, Indonesia
Copyright © 2025 Zhang, Shi, Xia, Zhu and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Haipeng Shi, U2hwaWN1QDE2My5jb20=
 Jingmin Zhang1,2
Jingmin Zhang1,2 Haipeng Shi
Haipeng Shi