- School of Pharmacy and Pharmacology, College of Health and Medicine, University of Tasmania, Hobart, TAS, Australia
Background: At the University of Tasmania (UTAS), pharmacy education traditionally relies on placements to provide students with hands-on experience. However, these placements have become increasingly limited due to logistical challenges and growing student numbers. Computer-based simulation (CBS) has the potential to offer a scalable, effective alternative to enhance learning and critical thinking. However, integrating CBS in pharmacy education faces several barriers that must be addressed for successful implementation.
Objective: To gain insight into pharmacy educators’ and students’ views regarding the barriers, and potential solutions, to integrating CBS in pharmacy practice education.
Methods: This mixed-methods case study involved semi-structured interviews with pharmacy educators and quantitative surveys with pharmacy students. The data underwent thematic coding for interview transcripts and statistical analysis for survey responses. The findings were integrated by examining convergence, complementarity, and discrepancy, revealing insights into how pharmacy students and educators perceive implementation barriers and improvement strategies for CBS.
Results: Ten interviews were conducted, and 75 survey responses were collected, with a 62.5% response rate. Key barriers to CBS integration included educators’ heavy workload, scepticism about CBS’s educational value, and general integration challenges. Students, however, showed high acceptance of CBS, with 70.7% agreeing that CBS could assess their knowledge, 69.3% emphasising its role in developing problem-solving skills, and 80% viewing CBS as a complement to classroom study. Proposed solutions for enhancing CBS uptake included additional institutional support by appointing dedicated simulation technicians, leveraging champions to advocate for CBS, and aligning CBS with educational objectives.
Conclusion: A significant gap between students’ readiness and educators’ hesitancy to use CBS in pharmacy education was identified. While students are eager to adopt new technologies, educators expressed reservations, primarily due to workload concerns and uncertainties about the efficacy of CBS. The feedback from educators suggests that institutions may see improved uptake by employing dedicated support personnel and initiating targeted training programs. Future research should focus on exploring barriers and facilitators, using larger and more diverse samples, and gaining deeper insights into decision-makers’ perspectives to enhance the integration and efficacy of CBS in pharmacy education.
1 Introduction
In pharmacy education, students typically participate in workplace-integrated learning placements, which immerse them in supervised, real-world pharmacy practice scenarios. Although the educational value of these placements is widely recognised (1, 2), their availability is constrained by an increase in student numbers and the rising difficulties and costs associated with facilitating such experiences, leading to challenges in offering enough high-quality clinical placements (3). With reduced placement opportunities, increased emphasis on preparatory exercises seems prudent, but traditional classroom exercises such as paper-based cases and standardised patients (role-play) have a significant cost associated with marking and delivery on a per-student basis, which impacts the ability to scale up. This predicament underscores the importance of integrating complementary training methods, like computer-supported learning, which has demonstrated significant advantages in knowledge acquisition through its interactive and engaging approach, and which can be scaled up without a significant increase in delivery cost per student (4). Computer-supported learning aligns with Kolb’s experiential learning cycle by simulating real-life challenges in a safe environment, thus enhancing students’ critical thinking and collaborative skills, which are essential for their professional competency (1, 5).
At the University of Tasmania (UTAS), the demand for quality workplace-integrated learning placements in pharmacy is intensifying, exacerbated by growing student populations and logistical challenges across diverse campus locations. These issues pose a risk to maintaining educational standards and preparing a competent healthcare workforce, potentially impacting patient safety (2, 6). Innovative new educational tools such as computer-based simulation (CBS) and virtual patient training, present promising solutions that aim to enhance teaching and learning experiences by making them more engaging, efficient, and accessible, thereby enriching experiential learning opportunities and bridging the gap between theoretical knowledge and practical skills (4, 7–9). CBS, in particular, has been identified as a key tool in advancing pharmacy students’ competencies in critical areas where hands-on experience may be limited (10, 11).
Despite the local development of ‘Pharmacy Simulator’ by the School of Pharmacy and Pharmacology at UTAS (12), which was designed to be used across several subjects within the pharmacy curriculum, including pharmacotherapy, clinical pharmacy, and pharmaceutical care. The simulator is designed to replicate various pharmacy practice scenarios, allowing students to apply theoretical knowledge in a controlled, virtual environment. It enables students to practice decision-making, patient counselling, and medication management in both community and hospital pharmacy settings, without the risks associated with real-life errors (13, 14). However, there is limited engagement with this simulation tool among educators. This reflects a broader trend where advancements like CBS are not being fully integrated into pharmacy education, especially compared to other health disciplines (13, 14). As a result, this study investigated the perceptions of pharmacy educators and students at UTAS regarding the barriers to integrating CBS into pharmacy practice education.
2 Methods
A mixed-methods case-study design was selected for its ability to provide in-depth contextual insights and actively engage stakeholders, which is crucial for understanding the intricate dynamics between technology, pedagogy, and institutional culture (15, 16). This case study aimed to address any potential challenges to the uptake of ‘Pharmacy Simulator’ and other CBS systems at the School of Pharmacy and Pharmacology, University of Tasmania, Australia. ‘Pharmacy Simulator’ is an in-house simulator specifically designed to enhance pharmacy education by providing a realistic and interactive learning environment (12). This CBS allows students to engage in simulated clinical scenarios, fostering critical thinking and soft skills essential for pharmacy practice.
The study involved surveys and interviews conducted between March to September 2023 to gather diverse stakeholder perspectives. Surveys were administered to students, while interviews were conducted with educators. The mixed-methods approach allowed for a comprehensive understanding of both quantitative and qualitative data, providing a holistic view of the perceptions of CBS. Given the small population size, we employed a total population sampling approach, inviting all members of the study population to participate.
All UTAS pharmacy students were eligible to participate. A link to the online survey was distributed via emails, and the institution’s learning management system. Participation was voluntary, with incentives including a chance to win one of ten $50 AUD gift vouchers. Implied consent was obtained at the survey’s start. The survey included questions designed to assess students’ opinions on the use of CBS technology, perceived implementation barriers, and their general interest in the adoption of this technology within the curriculum. The online survey was developed and administered using LimeSurvey® (LimeSurvey GmbH, Hamburg, Germany. URL http://www.limesurvey.org).
The initial constructs of the survey questions and overall design were identified based on a relevant literature search (13, 14) and scoping team meetings. Items were drafted and finalised using an iterative approach. The draft survey underwent independent content validation by two postgraduate pharmacy students and two pharmacy educators. Additionally, the survey was pre-tested with a small group of volunteers to assess its clarity and relevance, further supporting its face validity. These steps ensured that the survey was both comprehensive and aligned with the study’s objectives. The survey consisted of 20 questions, primarily close-ended for quantitative analysis, along with a 6-point Likert scale to measure respondents’ attitudes. The data were extracted from LimeSurvey® to IBM Statistical Package for Social Sciences (IBM SPSS® Statistics for Windows, version 26.0; IBM Corp, Armonk, NY, United States). Descriptive analysis was primarily used for the quantitative part of the study. Chi-square test was applied to make comparisons between groups, and a p-value <0.05 was considered statistically significant.
2.1 Design of the qualitative phase—educators interview
An email invitation, which included a participant information sheet and consent form, was sent to all pharmacy practice educators (n = 16) to participate in a semi-structured interview. These interviews aimed to examine their perspectives on CBS, discussing both the opportunities and challenges associated with its practical implementation. The interviews also explored educators’ views on possible approaches to enhance the integration and use of CBS at the institution. An online 30-min interview was conducted with each educator who agreed to participate and provided written consent. The semi-structured interviews were conducted using an open-ended script to explore the participants’ views on CBS and experiences with existing models. The interview format employed a ‘funnel-shaped’ approach, narrowing down from broad to specific inquiries (17). The script was developed based on a literature review (13, 14) and team discussions, and was pre-tested with three educators. The interview guide was designed to address several key constructs, including general perceptions of CBS, the adequacy of institutional and educator support, student engagement with CBS, and strategies for optimizing CBS implementation. Specific questions included, for instance, “What are pharmacy educators’ views on incorporating CBS into pharmacy practice education?” and “Are pharmacy educators adequately skilled and willing to integrate CBS into curricula?”. The full interview guide is available in Appendix B.
At the completion of each interview, the audio recording was transcribed using Zoom (18), and de-identified by assigning unique codes to remove personal identifiers. The interview transcripts were analysed thematically following Braun and Clarke’s (19) approach. The coding process, guided by an initial codebook, was manually conducted using NVivo (version 12.4, 2020, QSR) (20). This iterative process combined inductive and deductive strategies, allowing themes to emerge naturally while applying theoretical frameworks for depth. Researchers (AG, MS) conducted the coding, engaging in regular discussions to refine the codebook and resolve discrepancies through consensus, thereby enhancing thematic reliability. Contextual reflexivity was used to critically assess how the educational environment at UTAS and the researchers’ positionality influenced the findings on CBS integration barriers. To mitigate potential biases, independent researchers cross-validated the themes, and an audit trail of analytical decisions was maintained to ensure the trustworthiness of the findings.
Ethical approval was granted from the University of Tasmania’s (UTAS) Human Research Ethics Committee (Project ID: 26897).
3 Results
3.1 Student survey
The survey had a response rate of 62.5%, with 75 out of 120 enrolled students participating. The participants represented different study years of the Bachelor of Pharmacy program, as seen in Supplementary Table S1. The survey data highlighted students’ access to technology resources, their positive perspectives on the integration of CBS in the curriculum, the importance of a user-friendly and engaging CBS design, and their training preferences. However, there were concerns about the expected support levels from educators and institution for CBS implementation.
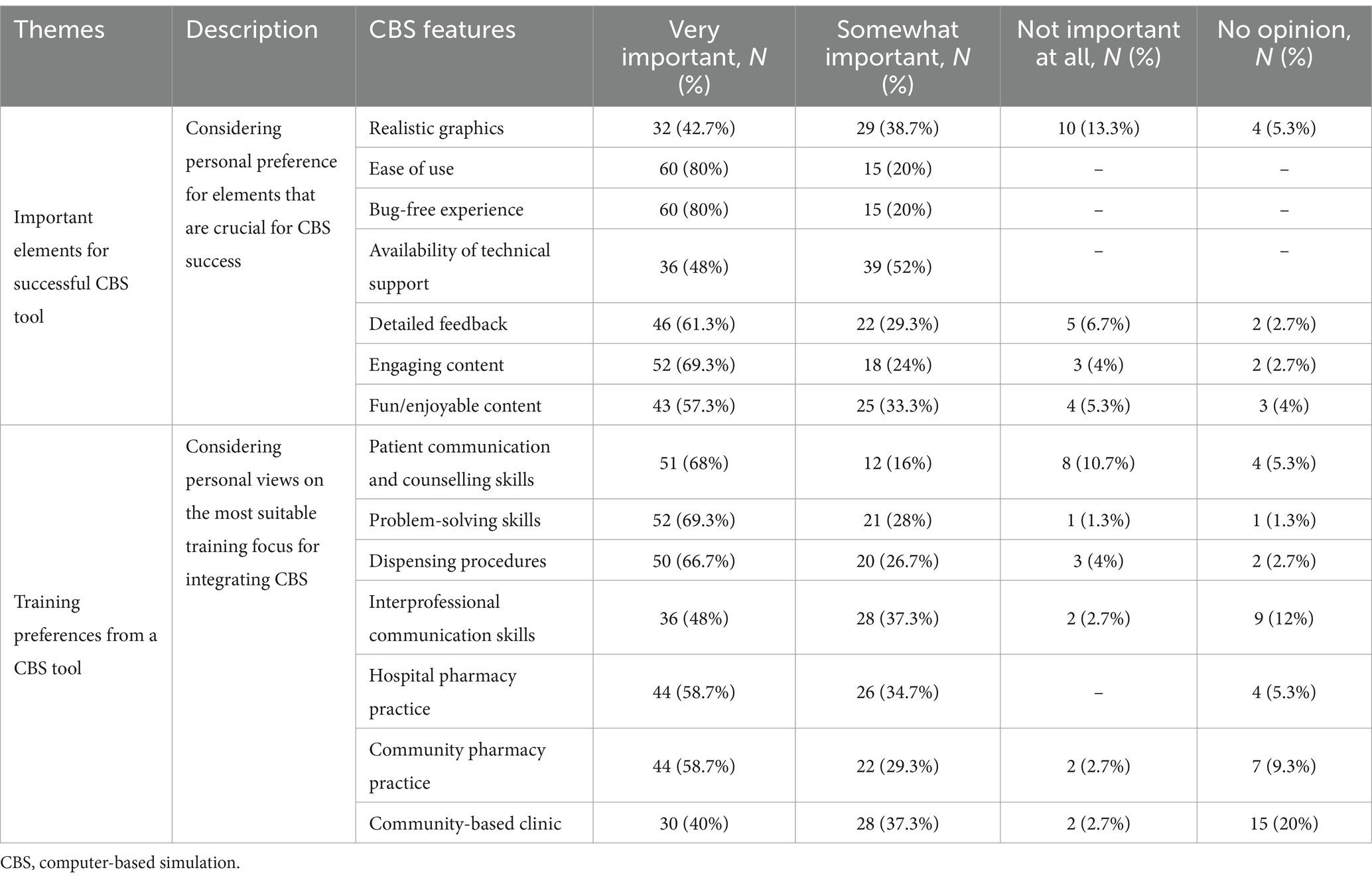
Regarding the role of CBS in curriculum, a significant proportion agreed that CBS could be utilised for assessing their knowledge (70.7%), in the classroom (62.7%), and as a supplement to classroom study (80%). The students expressed strong interest in developing patient communication and counselling skills (68%), problem-solving skills (69.3%), and dispensing procedures (66.7%) through CBS (as seen in Table 1). These preferences align with the practical and interpersonal competencies required in the pharmacy profession, indicating that students recognised the potential of CBS in enhancing these essential skills.
Table 2 shows students’ views on perceived support for CBS integration from different stakeholder groups. A chi-square test (p-value = 0.0002) confirmed significant differences in these perceptions. Notably, 37.3% of students believed their peers were very likely to support CBS, and 52% considered it somewhat likely. In contrast, only 16% perceived strong support from educators, with 33.3% seeing it as unlikely. Institutional support was also viewed critically, with only 20% seeing strong support and 40% considering it somewhat likely. These results highlight a gap in perceived support from educators and institutions compared to their peers.
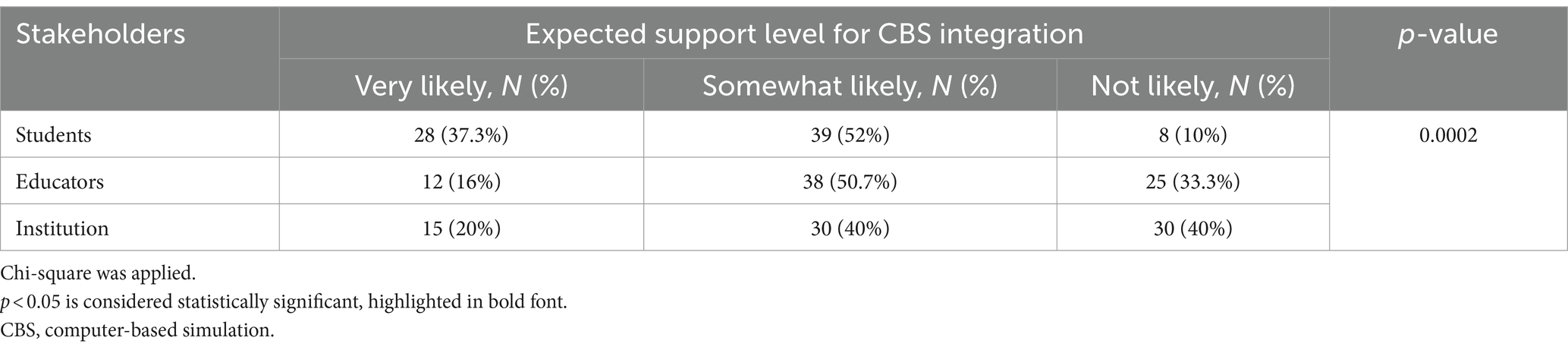
Table 2. Students’ views on the expected support level for CBS integration from different stakeholder groups.
3.2 Educator interviews
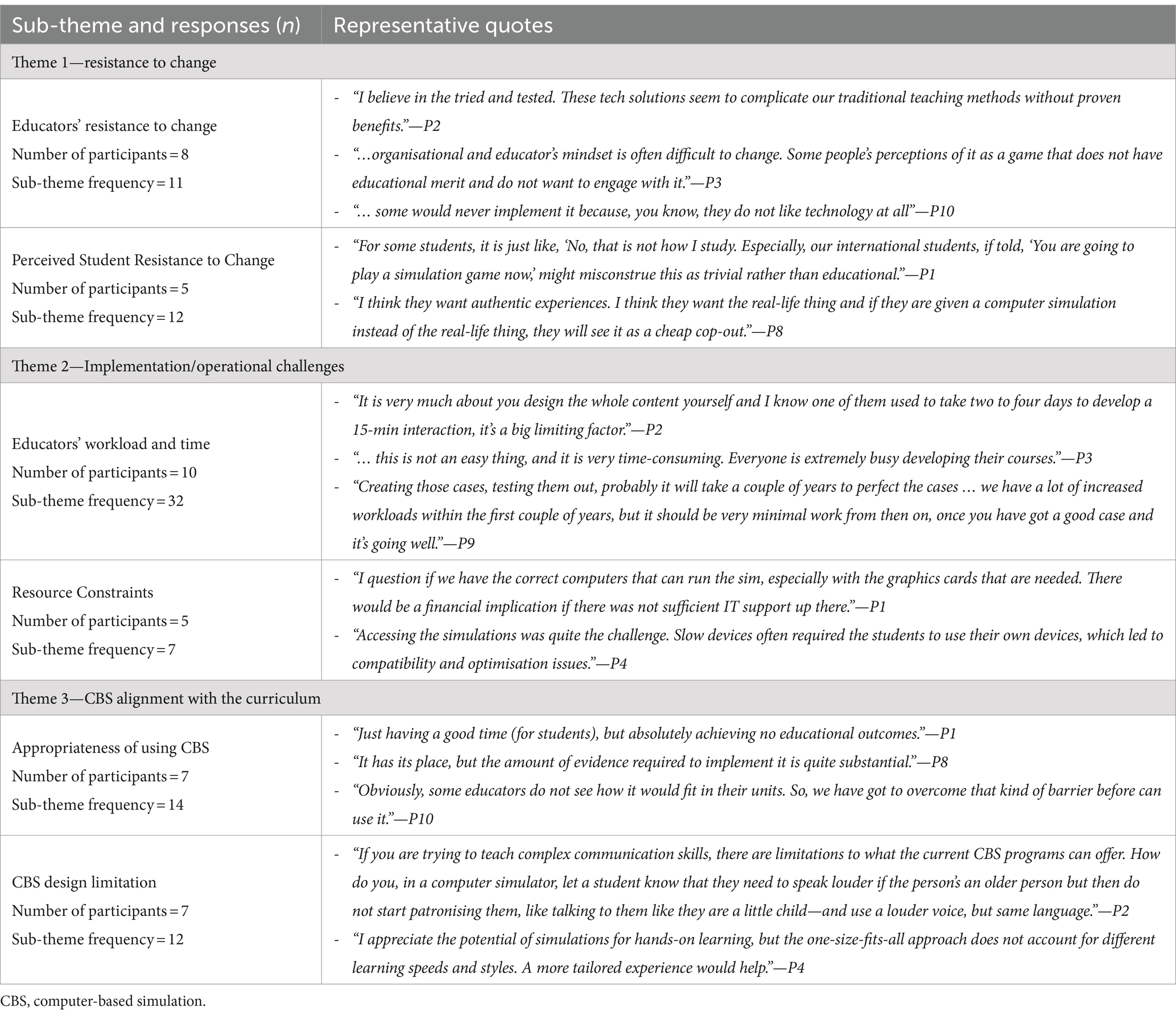
Of the 16 invited, 10 pharmacy practice educators were interviewed, achieving saturation-level with no new themes or insights emerging after the tenth interview. The educators had diverse pharmacy practice teaching experience, academic roles and exposure to CBS, as summarised in Supplementary Table S3. Regarding their experience with CBS, only two of the interviewees were actively using CBS in their teaching at the time of the interview. Additionally, eight educators had previous exposure to CBS, having trialled or used it in the past, but were not actively using it currently and were not necessarily updated on the changes that have occurred in CBS design features (some had not used CBS for several years). Data saturation was achieved after conducting 10 interviews, as no new themes emerged. The analysis identified three main themes: resistance to change, implementation and operational challenges, and CBS alignment with the curriculum. Additionally, several subthemes emerged within these broader categories, each highlighting specific aspects of the educators’ experiences and concerns. The emerging themes and insights are described in Tables 3, 4.
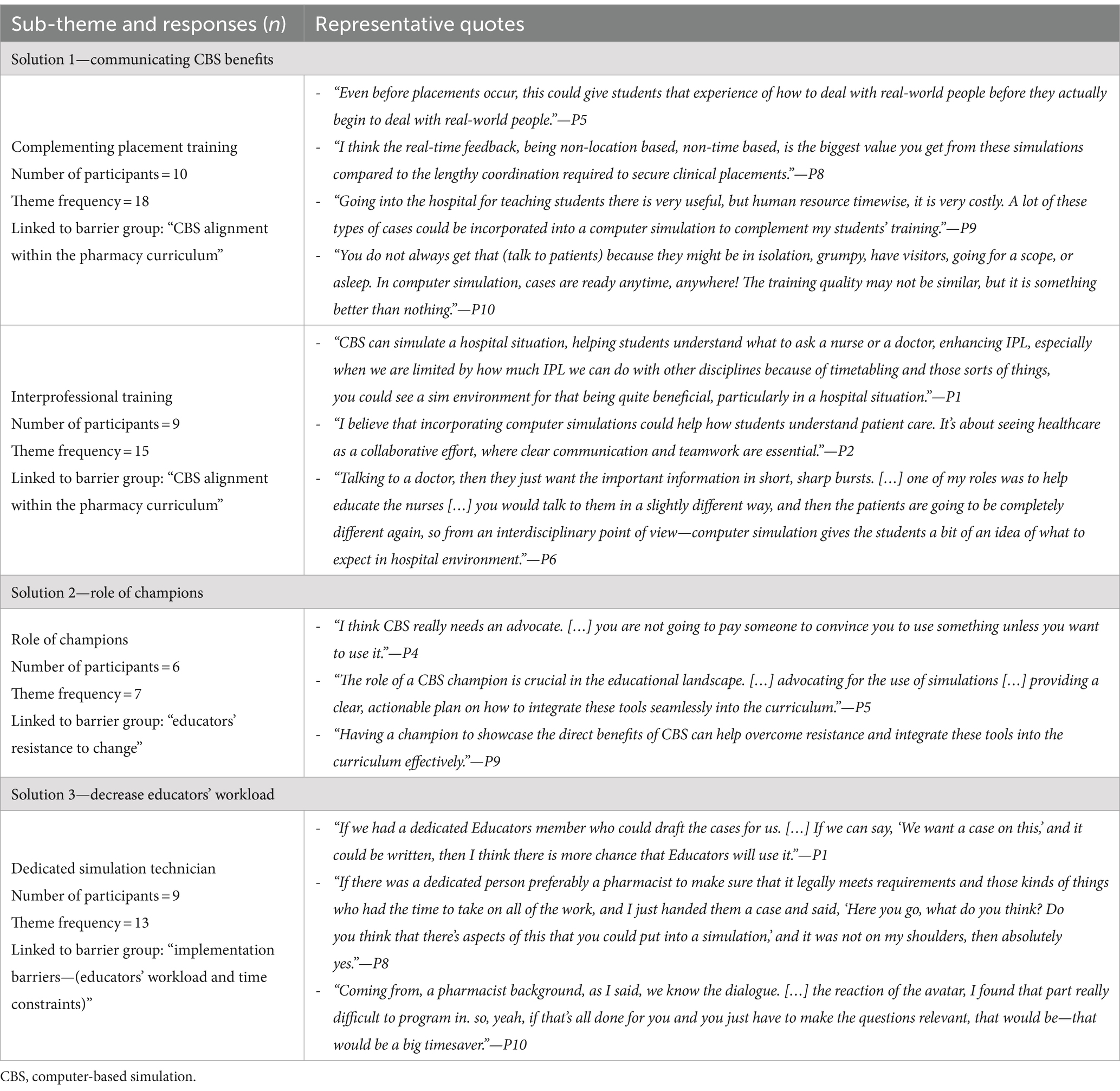
Table 4. Selected quotes on proposed solutions themes and its linkage to the corresponding barriers from educators’ interviews.
3.2.1 Theme 1: resistance to change
One of the most significant barriers to CBS uptake identified in the interviews was resistance to change, which manifested in two primary subthemes: educator resistance and student resistance.
Educators expressed a preference for traditional teaching methods and scepticism towards CBS. This reluctance to embrace new technologies reflects a broader cultural resistance within the educational environment, where innovation is often met with caution and the need for extensive testing before adoption. Additionally, some educators view CBS as lacking educational merit and perceive them as games rather than legitimate educational tools.
In addition to educator resistance, the interviews revealed concerns about student resistance, particularly among international students. Some educators noted that these students tended to view CBS as less formal and less valuable compared to traditional methods. This highlights the importance of considering cultural perceptions and learning preferences when introducing new educational tools. Students who are accustomed to more conventional forms of instruction may find CBS challenging to accept, perceiving it as a departure from the rigour and structure they associate with effective learning.
3.2.2 Theme 2: implementation and operational challenges
The second major theme was the implementation and operational challenges associated with integrating CBS into the curriculum. This theme encompasses several subthemes, including workload and time constraints and resource limitations.
Educators cited significant time constraints and increased workload required for developing case scenarios and adapting to CBS use. Balancing the initial setup of CBS with existing educational duties was highlighted as a major challenge, as it was seen as labour-intensive, involving the creation of complex case scenarios, testing, and refinement. Some educators expressed concerns that these demands could detract from other important responsibilities, making CBS a daunting addition to their teaching duties. However, many acknowledged that once CBS is fully integrated, it could reduce the ongoing workload compared to traditional methods, such as standardised patients and paper-based solutions, which need to be re-implemented annually. Despite recognising the potential long-term benefits of CBS, many felt that the upfront investment in time and resources could be a significant deterrent, particularly during the early stages of adoption. Another significant subtheme was the lack of adequate resources to support CBS implementation. Educators cited issues such as underpowered or malfunctioning computers, compounded by logistical challenges when institutions have multiple sites or campuses.
3.2.3 Theme 3: CBS alignment with the curriculum
This theme includes subthemes such as curriculum integration and pedagogical effectiveness.
Some educators questioned the alignment of CBS with the existing pharmacy curriculum and its effectiveness in achieving learning objectives. They highlighted perceived gaps between the potential of CBS as an engaging tool and its actual effectiveness in delivering educational outcomes. Concerns were raised about whether CBS, in its current form, could be seamlessly integrated into the curriculum without compromising the quality of education. Educators were particularly worried that CBS might disrupt the flow of the curriculum and whether it could effectively complement other teaching methods. Additionally, design limitations were noted, such as difficulties in replicating real-life natural communication and a lack of customisation in CBS, which some educators felt could hinder the development of critical thinking and problem-solving skills.
3.3 Proposed solutions
Participants proposed several solutions that may facilitate overcoming these challenges. They emphasised the importance of communicating the benefits of CBS to stakeholders, fostering interprofessional learning opportunities through simulation, leveraging champions to advocate for technology integration, and alleviating educators’ workload by employing dedicated simulation technicians. Specifically, the solutions included promoting the benefits of CBS in complementing clinical placement training (18 instances, 10 participants) and employing dedicated CBS support staff, such as specialist simulation technicians (13 instances, 9 participants), to ease educator workloads.
3.3.1 Solution 1: communicating CBS benefits
One of the proposed solutions focused on communicating the benefits of CBS more effectively, particularly in how CBS can complement existing training methods and foster interprofessional learning (IPL).
Educators suggested that CBS could play a critical role in complementing clinical placements, particularly by providing students with opportunities to practice and refine their skills in a controlled environment before interacting with real patients. This would help bridge the gap between theoretical knowledge and practical application, giving students confidence in their abilities. Additionally, CBS could offer real-time feedback, allowing students to learn from their mistakes in a safe setting. This approach would be especially valuable when traditional placements are limited or challenging to coordinate, as CBS can simulate scenarios that students might not otherwise encounter. The ability of CBS to supplement clinical placements was seen as a key factor in aligning it more closely with the pharmacy curriculum.
Another solution proposed was the use of CBS to enhance interprofessional training. By simulating real-life healthcare scenarios that involve multiple disciplines, CBS can help students understand the importance of communication and collaboration in patient care. Educators noted that IPL through CBS could overcome the logistical challenges of coordinating in-person IPL activities across different disciplines, making it a practical and effective tool for developing these essential skills. This solution directly addresses the subtheme of CBS alignment within the curriculum by integrating CBS as a means to achieve broader educational objectives beyond the scope of traditional, discipline-specific training.
3.3.2 Solution 2: role of champions
To address resistance to change, educators proposed introducing champions—key individuals who advocate for CBS and guide its integration. Champions are seen as crucial in addressing the educators’ resistance to change. By demonstrating the benefits of CBS and offering practical support, champions can help shift the cultural attitudes within the educational environment. They would lead by example, showcasing successful CBS implementations and providing mentorship to other educators who are hesitant to adopt the technology. Champions could also play a pivotal role in aligning CBS with educational goals, ensuring that its integration is seamless and effective. This approach would help build confidence in CBS and foster a more supportive environment for its adoption.
3.3.3 Solution 3: decreasing educators’ workload
A final proposed solution involves reducing the workload associated with CBS by employing dedicated simulation technicians. Educators suggested that this role could alleviate their burden by managing the technical aspects of CBS, such as scenario development, system maintenance, and troubleshooting. This approach would allow educators to concentrate on the pedagogical integration of CBS without being overwhelmed by operational demands. Having a team member who understands both the technical and educational aspects of CBS would also ensure its effective use, enhancing its value as a teaching tool. This solution addresses barriers related to educators’ workload and time constraints, making CBS a more viable option for curriculum integration.
4 Discussion
This case study explored the perceptions of students and educators towards using CBS in pharmacy education, uncovering several barriers impacting CBS uptake. These barriers encompassed cultural challenges, such as educators’ resistance to change, and operational challenges, including limited resources and substantial workload and time constraints faced by educators. Participants proposed several solutions to mitigate these barriers and enhance the uptake of CBS.
The combined insights from students and educators revealed both challenges and benefits to the broader adoption of CBS. There was strong student support for CBS, with 70.7% affirming its value for assessing knowledge and 80% endorsing its assistive role in education. These findings align with other educational contexts where technological readiness and positive perceptions towards digital learning tools have been increasingly noted. Studies have shown that digital natives, such as the current generation of students, are generally more receptive and adaptive to using technology for learning purposes (21).
However, only 16% of students believed that strong educator support for CBS integration was likely. The interviews with educators largely supported this view, exhibiting a notable resistance to change, potentially rooted in a preference for traditional teaching methods and concerns over the educational efficacy of new technologies. This resistance is compounded by practical barriers such as resource constraints and workload, hindering the effective deployment and integration of CBS into the curriculum. This phenomenon is well-documented in educational research, which underscores a natural hesitancy towards change (22–24). Introducing CBS requires an upfront investment and may be perceived as burdensome rather than enriching. Without adequate support, this workload can lead to burnout and resistance, despite the potential benefits for learning outcomes and longer-term workload reductions. Previous research has found that while students quickly adapt to new learning technologies, educators often lag due to factors such as resistance to change, lack of training, and perceived increase in workload (25).
This divergence in perspectives on the role of CBS in pharmacy education highlights a cultural gap that needs bridging. Overcoming faculty resistance and boosting institutional support are likely required to realise the full potential of CBS in pharmacy education. Students perceived CBS as highly valuable for improving patient communication, problem-solving abilities, and dispensing procedures. In contrast, educators expressed reservations about CBS’s ability to replicate complex real-world scenarios effectively and its alignment with educational outcomes. This limited active use suggests that their practical experience might not fully reflect CBS capabilities. Their feedback should be contextualised within their hands-on experience, highlighting the need for ongoing training and support to help educators integrate and utilise CBS effectively. The literature supports the positive views of students and refutes educators’ scepticism, with evidence that CBS can improve skills and knowledge, including clinical reasoning, procedural skills, and team skills (26). By integrating CBS more deeply into the curriculum, educational institutions can better prepare students for real-world clinical scenarios, enhancing their readiness for professional practice. Furthermore, the effective use of CBS can help bridge the gap between theoretical knowledge and practical application.
All interviewees supported CBS to complement placement training, recognising its value in addressing educational gaps. This support is reinforced by professional organisations such as the American Association of Colleges of Pharmacy (AACP) and the Accreditation Council for Pharmacy Education (ACPE), which advocate for using technologies like CBS as complementary teaching tools (27). CBS is also seen as having the potential to foster collaborative learning experiences and promote a culture of (IPL) within pharmacy education (28).
Our study revealed significant shortcomings in local institutional support, with nearly 40% of students questioning its adequacy. This underscores a critical gap in perceived support systems within the institution. Educators reported substantial challenges, notably heavy workloads and limited time, which hindered their ability to explore and adopt innovative teaching methods like CBS. To fully leverage the potential of CBS, schools must invest in infrastructure and provide ongoing training for educators. Such investments not only address current resistance but also empower educators with the skills and confidence needed to innovate in their teaching practices. As educators become more proficient with CBS, they can enhance the school’s overall development by creating more engaging and effective learning environments, which, in turn, can attract and retain students.
The literature consistently underscores the essential role of institutional support in successfully integrating new technologies in educational settings (29). One key suggested intervention is appointing a dedicated technician for CBS integration. This technician would provide essential technical support, facilitate smooth implementation, and allow educators to focus on pedagogical innovation rather than technical matters. By doing so, educators believed that educational institutions could ensure, CBS content is expertly managed and updated, enhancing both the quality and functionality of the simulations. Other targeted support measures identified in the literature may help address implementation challenges effectively (29). These include specialised training sessions for educators to grasp new technologies quickly without overwhelming them. Practical resources like customisable CBS templates and digital resource libraries can further streamline the time educators spend creating new content and integrating it into existing courses.
5 Study implications
Our study highlights the need for a strategic approach to equip both students and educators to engage effectively with CBS in pharmacy education.
For students, while their enthusiasm for CBS is evident, it is crucial to ensure they are not merely passive users but are actively developing the critical thinking and problem-solving skills that CBS can enhance. This requires carefully designed instructional strategies that integrate CBS into the curriculum in ways that align with professional practice expectations.
For educators, the study underscores the necessity of targeted faculty development initiatives. These should go beyond technical training to include pedagogical strategies for seamlessly incorporating CBS into teaching. The goal is to shift the perception of CBS from being an additional burden to a valuable tool that enhances educational outcomes. This shift can be facilitated by creating platforms for educators to share their experiences and successes with CBS, fostering a community of practice that supports continuous learning and adaptation.
Furthermore, the study suggests that institutional support plays a pivotal role in the successful adoption of CBS. This support includes not only providing the necessary infrastructure but also ensuring that educators have access to ongoing professional development and technical support. Such support structures are essential to overcoming the cultural and operational barriers identified in our study, enabling educators to innovate with confidence and effectiveness.
By addressing these implications, educational institutions can better prepare both students and educators to leverage CBS fully, ultimately enhancing the quality and effectiveness of pharmacy education. This will equip future pharmacists with the skills and knowledge needed to excel in an increasingly complex and technology-driven healthcare environment.
6 Limitations
The mixed-methods approach, combining qualitative interviews and quantitative surveys for two key stakeholders, ensured a comprehensive understanding of CBS uptake at UTAS and enhanced the reliability of the findings. Furthermore, the high response rate and detailed thematic analysis further strengthen the study’s credibility and relevance. However, the study sample, drawn from a single institution, may limit the generalisability of the findings. Nevertheless, the results are applicable in a broader context. The identified barriers and proposed solutions, such as dedicated support personnel and fostering interprofessional learning, address common issues in pharmacy education globally. These insights into overcoming challenges contribute to the wider adoption of CBS, benefiting pharmacy programs worldwide.
Additionally, the inclusion of students from different academic years may introduce bias due to uneven representation and varying levels of experience and familiarity with CBS. Moreover, there is a risk that participants might have provided socially desirable responses rather than their true perceptions, as the reliance on self-reported data from interviews and surveys may be subject to response bias. To mitigate this, we ensured the anonymity of responses, designed questions to maintain anonymity, and guaranteed that participation had no impact on students’ grades or study progress.
7 Recommendations for future research
Future research should incorporate larger, more diverse samples from multiple universities. This approach would enhance the accuracy and generalisability of the findings, providing a more comprehensive understanding of the barriers and facilitators to CBS adoption in pharmacy education. Additionally, gaining deeper insights into the perspectives of decision-makers would be useful for identifying potential barriers and developing strategies to overcome them.
8 Conclusion
This mixed-methods case study reveals a complex interplay of factors influencing the adoption of CBS in pharmacy education at our university, highlighting student enthusiasm and educator reservations. Despite students valuing the adoption of CBS, educators expressed concerns over practical implementation challenges, including infrastructure needs, workloads, and the impact on traditional teaching methods. Proposed solutions emphasised the need for dedicated support personnel, targeted training, and strategic curriculum integration.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Tasmanian Human Research Ethics Committee (reference: H0026897), Australia. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
AG: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Validation, Writing – original draft, Writing – review & editing. GP: Conceptualization, Investigation, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. IB: Conceptualization, Investigation, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. MS: Conceptualization, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. AG gratefully acknowledges the University of Tasmania for awarding a Tasmania Graduate Research Scholarship. The open access article-processing charge has been funded by the UTAS Pharmacy Appeal Fund.
Acknowledgments
We acknowledge all participants in our study (both educators and students) for sharing their views and insights.
Conflict of interest
The University of Tasmania owns the underlying Intellectual Property for Pharmacy Simulator and makes use of it in their Bachelor of Pharmacy program. This technology has been out-licensed for commercialisation and is being actively sold as Pharmacy Simulator by Imitated Environments Pty Ltd., Hobart, Australia. ABN 71625288575. One of the authors, Ivan Bindoff is the director and major shareholder of Imitated Environments Pty Ltd.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board members of Frontiers, (MS and GP) at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2024.1448893/full#supplementary-material
References
1. Jaber, AAS. Computer-based simulation in pharmacy education In: YM Al-worafi, editor. Comprehensive healthcare simulation: pharmacy education, practice and research comprehensive healthcare simulation. Switzerland: Springer International Publishing (2023). 23–9.
2. Australian Pharmacy Council Ltd. Accreditation Standards for Pharmacy Programs (2020) (Updated October 2022). Available at: https://www.pharmacycouncil.org.au/resources/pharmacy-program-standards/accreditation-standards-2020.pdf
3. Choi, M. Communities of practice: an alternative learning model for knowledge creation. Br J Educ Technol. (2006) 37:143–6. doi: 10.1111/j.1467-8535.2005.00486.x
4. Mai, C-W, Lee, E-L, Wong, P-S, and Er, H-M. Evaluation of computer-based simulation learning on knowledge, learning approaches and motivation among pharmacy students. Indian J Pharma Educ Res. (2019) 53:595–602. doi: 10.5530/ijper.53.4.120
5. Looyestyn, J, Kernot, J, Boshoff, K, Ryan, J, Edney, S, and Maher, C. Does gamification increase engagement with online programs? A systematic review. PLoS One. (2017) 12:e0173403. doi: 10.1371/journal.pone.0173403
6. Stupans, I, and Owen, S. Planning and scaffolding for learning in experiential placements in Australian pharmacy schools. Asia-Pacific J Cooperat Educ. (2009) 10:29.
7. Cook, DA, Hatala, R, Brydges, R, Zendejas, B, Szostek, JH, Wang, AT, et al. Technology-enhanced simulation for health professions education: a systematic review and Meta-analysis. JAMA J Am Med Assoc. (2011) 306:978–88. doi: 10.1001/jama.2011.1234
8. Benedict, N, and Schonder, K. Patient simulation software to augment an advanced pharmaceutics course. Am J Pharm Educ. (2011) 75:21. doi: 10.5688/ajpe75221
9. Duff, E, Miller, L, and Bruce, J. Online virtual simulation and diagnostic reasoning: a scoping review. Clin Simul Nurs. (2016) 12:377–84. doi: 10.1016/j.ecns.2016.04.001
10. Shin, J, Tabatabai, D, Boscardin, C, Ferrone, M, and Brock, T. Integration of a community pharmacy simulation program into a therapeutics course. Am J Pharm Educ. (2018) 82:6189. Epub 2018/03/02. doi: 10.5688/ajpe6189
11. Seybert, AL, Smithburger, PL, Benedict, NJ, Kobulinsky, LR, Kane-Gill, SL, and Coons, JC. Evidence for simulation in pharmacy education. JACCP: journal of the American college of. Clin Pharm. (2019) 2:686–92. doi: 10.1002/jac5.1167
12. PharmacySim. Pharmacy Simulator (2023) (Accessed December 09, 2023). Available at: https://www.pharmacysim.com/
13. Gharib, AM, Peterson, GM, Bindoff, IK, and Salahudeen, MS. Potential barriers to the implementation of computer-based simulation in pharmacy education: a systematic review. Pharmacy. (2023) 11:86. doi: 10.3390/pharmacy11030086
14. Gharib, AM, Bindoff, IK, Peterson, GM, and Salahudeen, MS. Computer-based simulators in pharmacy practice education: a systematic narrative review. Pharmacy. (2023) 11:8. doi: 10.3390/pharmacy11010008
15. Yin, RK. Case study research and applications, Thousand Oaks, California: Design and methods SAGE Publications, Inc., (2017).
16. Creswell, JW, and Poth, CN. Qualitative inquiry and research design. Los Angeles: Choosing among five approaches SAGE Publications (2017).
17. Brod, M, Tesler, LE, and Christensen, TL. Qualitative research and content validity: developing best practices based on science and experience. Qual Life Res. (2009) 18:1263–78. doi: 10.1007/s11136-009-9540-9
18. Gray, LM, Wong-Wylie, G, Rempel, GR, and Cook, K. Expanding qualitative research interviewing strategies: zoom video communications. Qual Rep. (2020) 25:1292–301. doi: 10.46743/2160-3715/2020.4212
19. Braun, V, and Clarke, V. Using thematic analysis in psychology. Qual Res Psychol. (2006) 3:77–101. doi: 10.1191/1478088706qp063oa
20. Chatzopoulou, E. Qualitative data analysis: using Nvivo. Researching and Analysing business. Routledge. (2024):146–64. doi: 10.4324/9781003107774-12
21. Culp-Roche, A, Hampton, D, Hensley, A, Wilson, J, Thaxton-Wiggins, A, Otts, JA, et al. Generational differences in faculty and student comfort with technology use. SAGE Open Nursing. (2020) 6:2377960820941394. doi: 10.1177/2377960820941394
22. Stone-Johnson, C. Possibility and persistence of educational change research: concluding remarks to the twentieth anniversary issue of the journal of educational change (2020) 21:511–5. doi: 10.1007/s10833-020-09395-y
23. Garcia-Huidobro, JC, Nannemann, A, Bacon, CK, and Thompson, K. Evolution in educational change: a literature review of the historical Core of the journal of educational change. J Educ Chang. (2017) 18:263–93. doi: 10.1007/s10833-017-9298-8
24. Lomba-Portela, L, Domínguez-Lloria, S, and Pino-Juste, MR. Resistances to educational change: teachers&Rsquo; perceptions. Educ Sci. (2022) 12:359. doi: 10.3390/educsci12050359
25. Haleem, A, Javaid, M, Qadri, MA, and Suman, R. Understanding the role of digital Technologies in Education: a review. Sustain Operat Comput. (2022) 3:275–85. doi: 10.1016/j.susoc.2022.05.004
26. Kononowicz, AA, Woodham, LA, Edelbring, S, Stathakarou, N, Davies, D, Saxena, N, et al. Virtual patient simulations in health professions education: systematic review and Meta-analysis by the digital health education collaboration. J Med Internet Res. (2019) 21:e14676. doi: 10.2196/14676
27. Silva, ROS, Pereira, AM, Araújo, DCSA, Rocha, KSS, Serafini, MR, and de Lyra Jr, DP. Effect of digital serious games related to patient Care in Pharmacy Education: a systematic review. Simul Gaming. (2021) 52:554–84. doi: 10.1177/1046878120988895
28. Korayem, GB, Alshaya, OA, Kurdi, SM, Alnajjar, LI, Badr, AF, Alfahed, A, et al. Simulation-based education implementation in pharmacy curriculum: a review of the current status. Adv Med Educ Pract. (2022) 13:649–60. doi: 10.2147/AMEP.S366724
Keywords: computer-based simulation, pharmacy education, educational technology, interprofessional learning, curriculum integration, simulation-based learning, mixed-methods, virtual patients
Citation: Gharib AM, Peterson GM, Bindoff IK and Salahudeen MS (2024) Exploring barriers to the effective use of computer-based simulation in pharmacy education: a mixed-methods case study. Front. Med. 11:1448893. doi: 10.3389/fmed.2024.1448893
Edited by:
Ardi Findyartini, University of Indonesia, IndonesiaReviewed by:
Melanie Stephens, University of Salford, United KingdomDaisy Volmer, University of Tartu, Estonia
Muna Barakat, Applied Science Private University, Jordan
Copyright © 2024 Gharib, Peterson, Bindoff and Salahudeen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ahmed M. Gharib, YWhtZWQuZ2hhcmliQHV0YXMuZWR1LmF1
 Ahmed M. Gharib
Ahmed M. Gharib Gregory M. Peterson
Gregory M. Peterson Ivan K. Bindoff
Ivan K. Bindoff Mohammed S. Salahudeen
Mohammed S. Salahudeen