- 1Department of Intensive Care Unit, Shenzhen Guangming District People's Hospital, Shenzhen, Guangdong, China
- 2Department of Pulmonary and Critical Care Medicine, Shenzhen Guangming District People's Hospital, Shenzhen, Guangdong, China
- 3Department of Stomatology, Shenzhen Guangming District People's Hospital, Shenzhen, Guangdong, China
Background: As a novel indicator of inflammation, the relationship between the systemic immune-inflammation index (SIRI) and mortality in patients with asthma remains uncertain. Our study aimed to explore the association between SIRI and mortality in asthma patients.
Methods: Data from the National Health and Nutrition Examination Survey (NHANES) for US adults from 2001 to 2018 were included in this study. Then, we divided all patients into three groups based on SIRI tertiles and used multivariable weighted Cox regression analysis, smoothing curve fitting, survival curve analysis, and subgroup analysis to investigate the relationship between SIRI and asthma.
Results: A total of 6,156 participants were included in the study, with each SIRI tertile consisting of 2052 individuals. Asthma patients with higher SIRI levels were older, had a higher level of education, were more likely to be married, and had a higher chance of being smokers. In Cox proportional-hazards models, the highest SIRI group showed higher hazard ratios (HRs) for all-cause mortality in individuals with asthma after adjusting for potential confounders. The restricted cubic spline analysis indicated a non-linear relationship between SIRI and all-cause mortality. The Kaplan–Meier survival curves showed that patients with higher SIRI levels had a higher risk of all-cause mortality. Subgroup analyses revealed SIRI’s association with all-cause mortality across various demographics, including age, sex, race, education levels, smoking status, and marital status.
Conclusion: Our study provides evidence for the relationship between SIRI and mortality in asthma patients. SIRI may potentially serve as a predictive tool for evaluating asthma mortality rates.
1 Introduction
Asthma, a chronic inflammatory disease of the airways, is characterized by reversible constriction and hyperresponsiveness of the airways. The disease presents a considerable global healthcare burden, affecting an estimated 334 million people worldwide and increasing every year (1). Exacerbations of asthma result in large numbers of emergency department visits, while improved control of the disease reduces healthcare expenses. Therefore, it is important to understand the causes of asthma.
The systemic immune-inflammation index (SIRI), as an inflammation index, is composed of peripheral blood neutrophil, monocyte, and lymphocyte counts (2). SIRI is widely used for the survival and mortality of various diseases as a predictive indicator in many studies. In a prospective study including 298 postoperative colorectal patients, compared to other serum inflammatory biomarkers, SIRI had a higher predictive ability for survival outcomes (3). In a prospective study including 52 patients diagnosed with advanced lung adenocarcinoma, Wang et al. found that the low SIRI level had a prolonged progression-free survival (4). A meta-analysis revealed that high SIRI levels could predict adverse survival outcomes in breast cancer patients (5). Furthermore, SIRI can provide better prognostic discrimination correlating with mortality risk not only in chronic heart failure patients (6) but also in cardiovascular and cerebrovascular disease patients (7–10). In addition, elevated SIRI levels are also associated with the incidence and mortality rates of chronic kidney disease (CKD) (11).
Although there is emerging evidence that the risk of all-cause mortality in asthma depends on the highest quartile of SIRI compared to the lowest quartile of SIRI (12), the research on the relationship between SIRI and mortality risk in asthma has not been evaluated as far as we know. Therefore, to investigate the relationship between SIRI and mortality rates in asthma patients, we use data from the National Health and Nutrition Examination Survey (NHANES) spanning from 2001 to 2018, aiming to find new valuable prognostic indicators.
2 Research design and methods
2.1 Study population
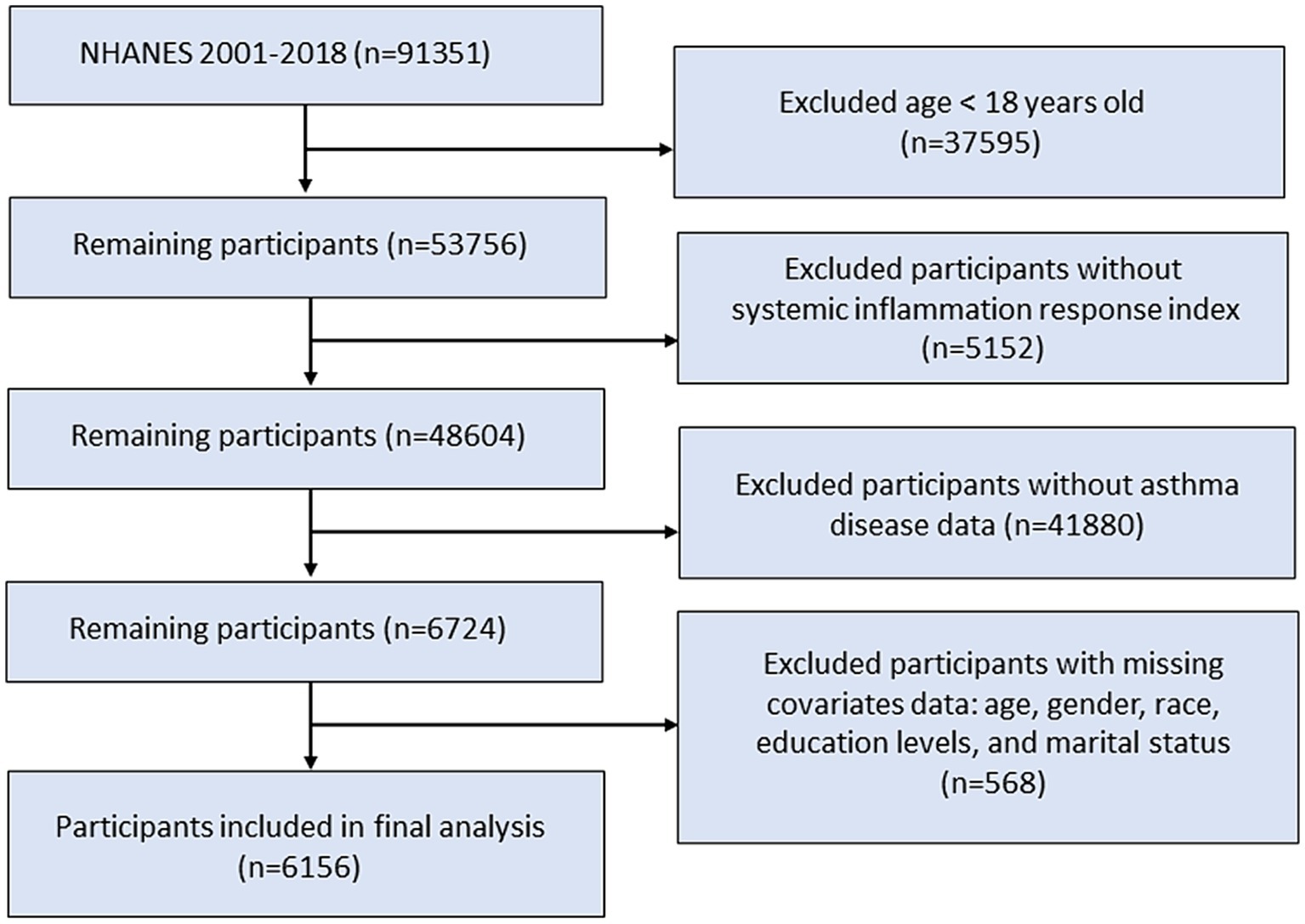
The NHANES provided cross-sectional data to assess the nutritional and health status of the non-institutionalized civilian population of the United States. Our study utilized data from the continuous NHANES survey, spanning 11 survey cycles conducted between 2001 and 2018, with a total of 91,351 participants. A total of 53,756 eligible participants aged 18 years and older were included in the study population. We excluded patients without SIRI or asthma disease data. Additionally, participants without records of age, sex, race, marital status, or education level were excluded from the study. Finally, 6,156 participants were included in this study (Figure 1).
2.2 Assessment of mortality
All-cause mortality data were obtained by linking to the National Death Index as of April 26, 2022.
2.3 Statistical analysis
SIRI was calculated using the formula (neutrophil count × monocyte count)/lymphocyte count. Participants were equally classified into three groups based on the values of SIRI. The adjusted hazard ratios (HRs) and 95% confidence intervals (95% CIs) were calculated using the Cox proportional-hazards regression model. This observational study used three models based on the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines (13). Model I was adjusted for none. Model II was adjusted for age, sex, and race. Model III was adjusted for all variables in Model II and included other risk factors such as marital status, education level, and smoking status. Furthermore, the Kaplan–Meier survival curves for all-cause mortality stratified by the values of the SIRI index were generated. Smooth curve fitting (penalized spline method) examined the non-linearity association between the SIRI index and all-cause mortality. All data analyses were performed using R version 4.2.2, and p-values less than 0.05 indicated statistical significance.
3 Results
3.1 Subject characteristics
The baseline characteristics of the cohort were analyzed based on the changes in SIRI tertiles, as shown in Table 1. This analysis included 6,156 patients, with each tertile based on 2,052 individual observations. Compared to the lowest SIRI tertile group, patients in the highest SIRI tertile group had a higher average age, were more likely to be married, had a higher level of education, and had a higher chance of being smokers. Additionally, the male-to-female ratio was similar in all SIRI groups, but the patients in the highest SIRI tertile group were predominantly non-Hispanic white. Furthermore, all baseline variables showed statistically significant differences between the SIRI groups (p < 0.05).
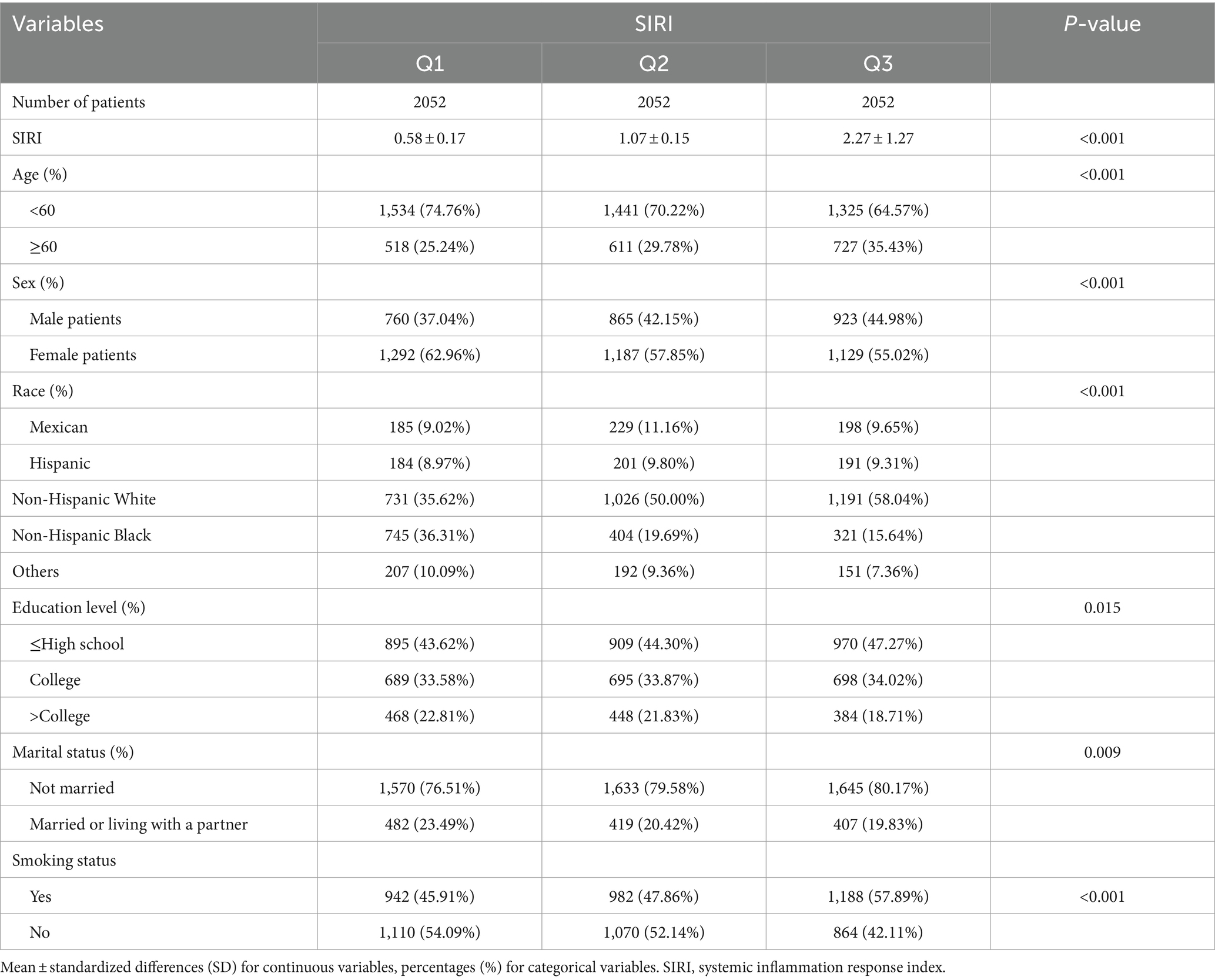
Table 1. Demographic and clinical characteristics according to systemic inflammation response index (SIRI).
3.2 Association between the SIRI index and mortality
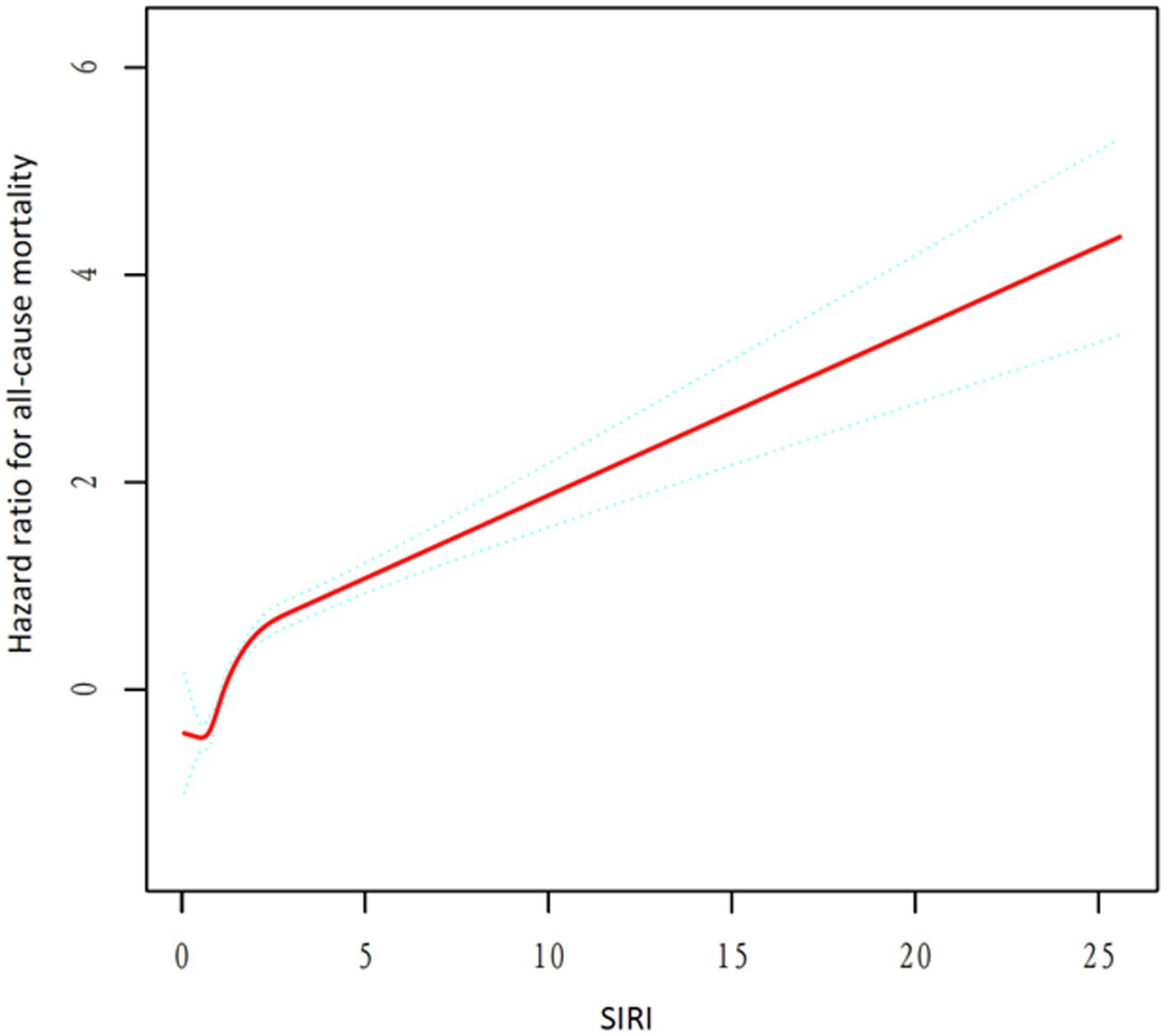
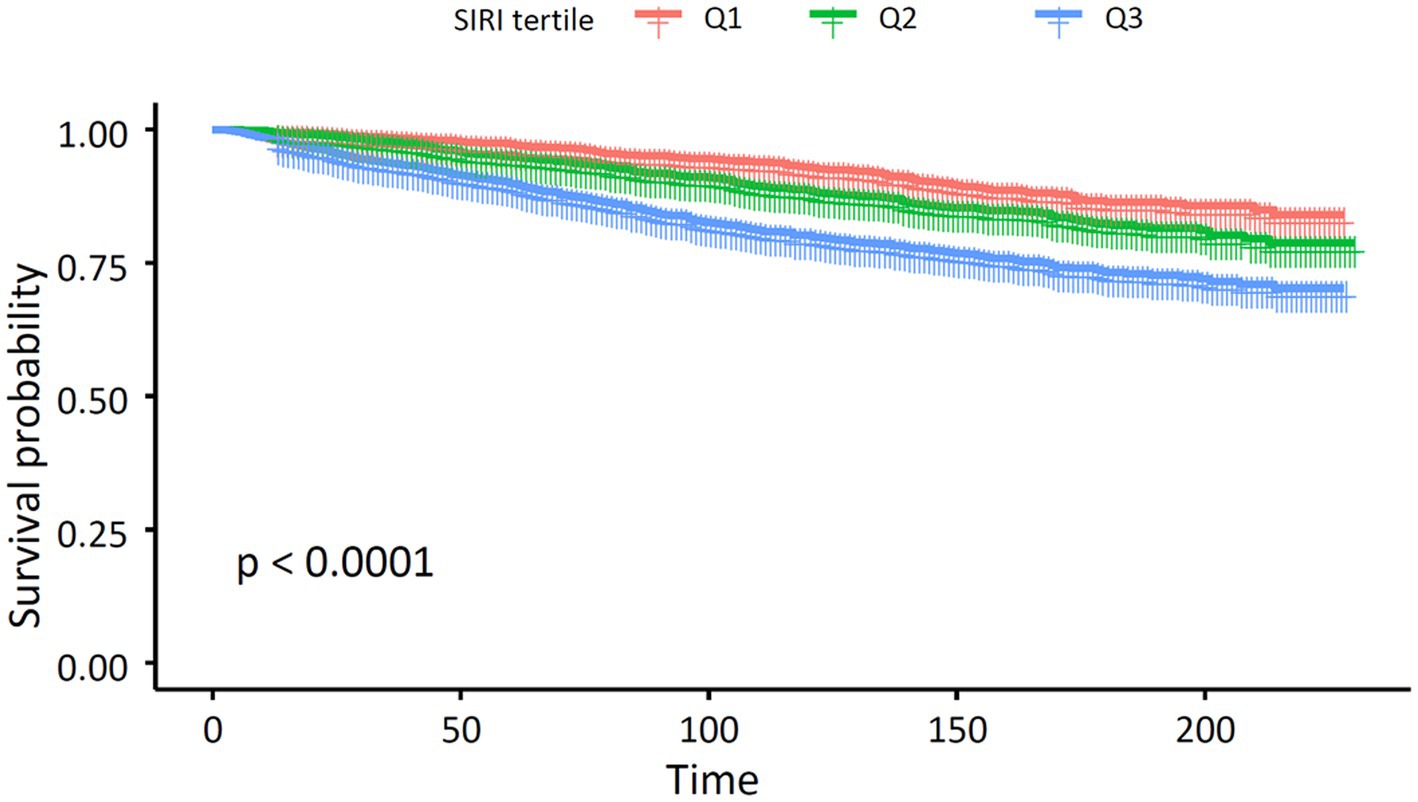
Table 2 displays the three quartiles of all-cause mortality rates in asthma patients at different levels of SIRI. In the unadjusted Model 1, the hazard ratios (HRs) from the lowest SIRI tertile group to the highest SIRI tertile group were 1.00 (reference), 1.46 (1.20, 1.78), and 2.59 (2.16, 3.11), with a p-value of <0.001, indicating a significant association between SIRI levels and increased overall mortality risk in asthma patients. In Model 2, after further adjusting for age, sex, and race, the HRs for the SIRI tertile groups were 1.00 (reference), 1.26 (1.03, 1.54), and 2.19 (1.81, 2.65), with a p-value of <0.001. The risk of overall mortality gradually increased with increasing SIRI. In Model 3, after further adjusting for marital status, education level, and smoking status based on Model 2, the results of Model 3 were similar to those of Model 2. The HRs for the SIRI tertile groups were 1.00 (reference), 1.24 (1.01, 1.52), and 2.08 (1.71, 2.51), with a p-value of <0.001. Thus, the relationship between SIRI and overall mortality in asthma patients remained consistent in different models of our study. We then used a smoothing curve to plot the relationship between SIRI levels and mortality risk in asthma patients. We found an approximately linear relationship between SIRI and overall mortality risk, and the risk of overall mortality increased with an increase in SIRI (Figure 2). Furthermore, we conducted a Kaplan–Meier survival analysis for the overall mortality rates among the SIRI tertile groups. The curves showed that, compared to the higher SIRI tertile groups, the lowest SIRI tertile group was associated with the lowest lifetime risk of overall mortality. As the SIRI tertiles increased, the risk of overall mortality also increased (Figure 3). Finally, we performed a subgroup analysis on the association between SIRI and asthma and found that higher SIRI levels were significantly associated with an increased risk of all-cause mortality, regardless of age (<60 or ≥60), sex (male or female), race, education level, smoking status, and marital status (p < 0.001) (Figure 4).
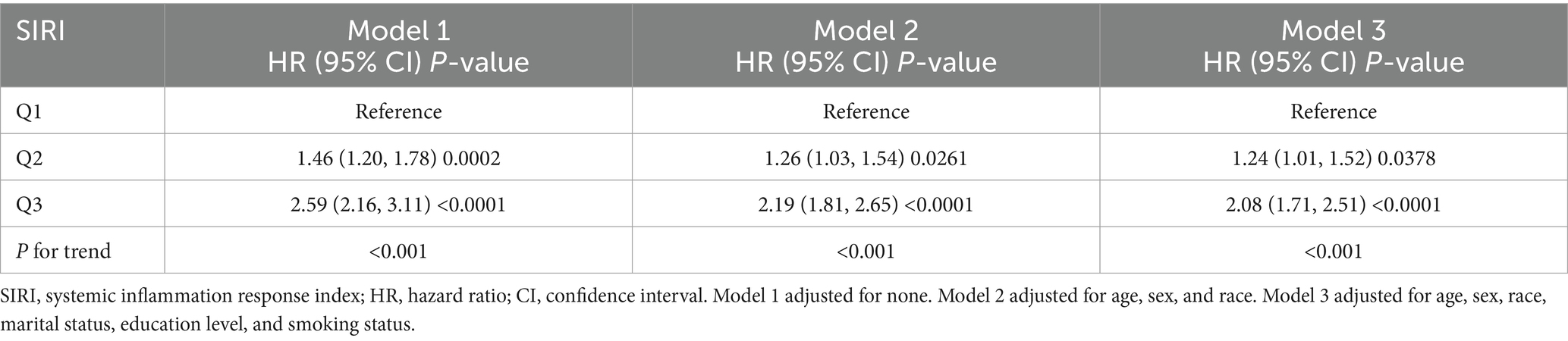
Table 2. Multivariate Cox regression analysis of systemic inflammation response index with all-cause mortality.
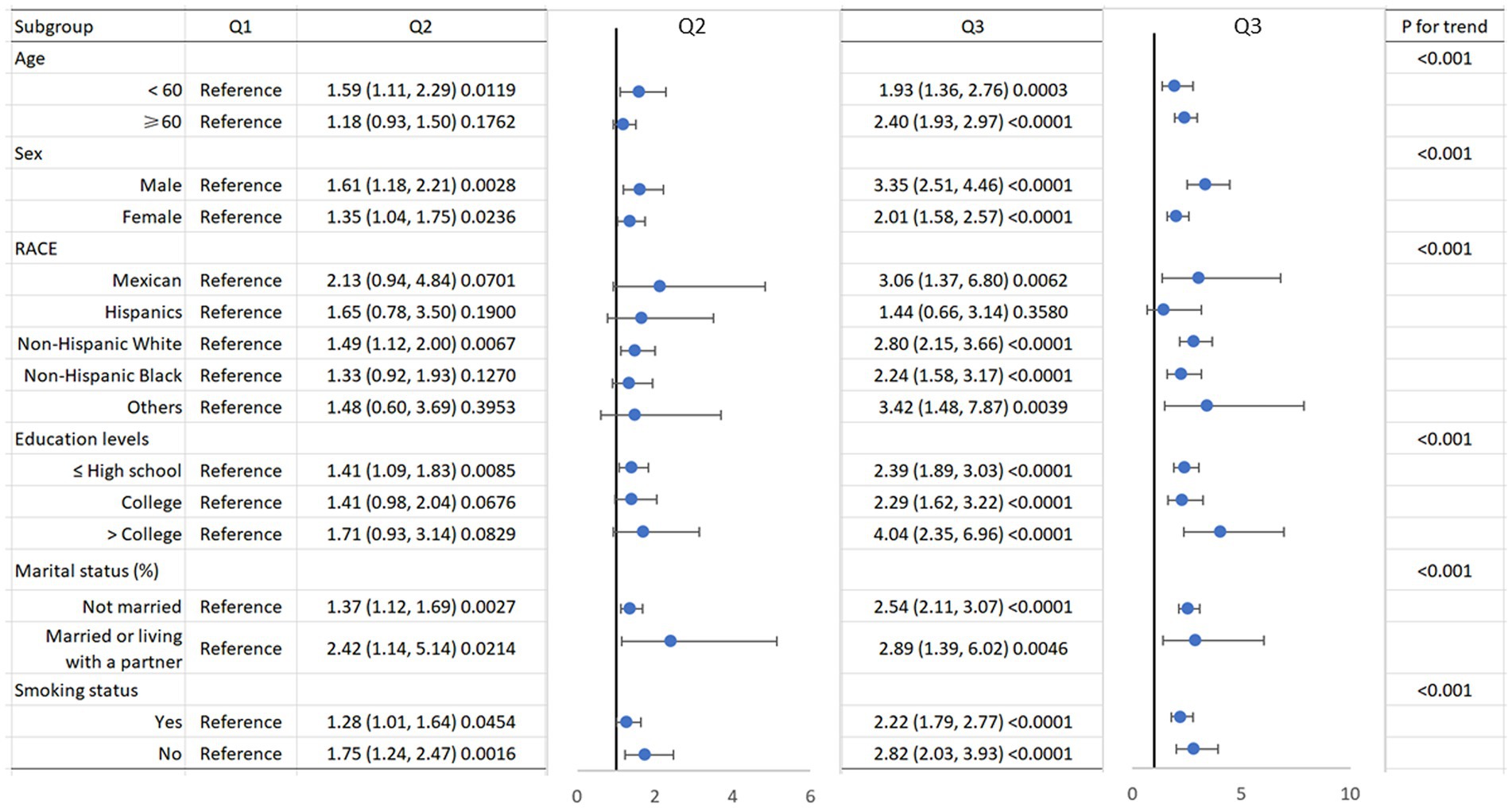
Figure 4. Subgroup of the association between systemic inflammation response index and all-cause mortality.
4 Discussion
By analyzing the NHANES data from 2001 to 2018, we discovered a significant linear correlation between SIRI levels and all-cause mortality rates in patients with asthma. Even after considering potential confounding factors, our analysis results remained robust, indicating that SIRI levels may be independently associated with all-cause mortality rates in asthma patients. This finding introduces an innovative predictive indicator for predicting mortality in asthma patients, offering a fresh perspective for a more comprehensive assessment of their survival risk.
In recent years, inflammatory biomarkers derived from complete blood cell counts, such as neutrophil-to-lymphocyte ratio (NLR), monocyte-to-lymphocyte ratio (MLR), platelet-to-lymphocyte ratio (PLR), systemic immune-inflammation index (SII), and SIRI, have increasingly garnered attention as predictors of asthma. These indices are all based on parameters related to neutrophils, lymphocytes, monocytes, and platelets (12). Zhu et al. found that elevated NLR levels were associated with higher all-cause mortality in asthma in a cross-sectional study from the NHANES database (14). Shi et al. confirmed a correlation between NLR levels and the severity and prognosis of adult asthma and childhood asthma (15, 16). Xuanqi et al. proved that PLR can predict the frequency of acute exacerbations in patients during stable periods with chronic obstructive pulmonary disease (COPD) (17). Additionally, NLR and PLR levels have also been shown to be predictive indices of mortality rates in COPD (18). Moreover, a population-based study has shown that the higher the SII, the poorer the prognosis for middle-aged and elderly patients with COPD and asthma (19). There is evidence to suggest that elevated and activated neutrophil levels are linked to symptom relief and treatment outcomes in symptomatic asthma patients (20), and to the activation of monocytes in the peripheral blood in asthma patients (21). On the one hand, these monocytes can change into macrophages or dendritic cells to promote the inflammatory process and destroy lung function (22–24). On the other hand, lymphocytes, which play a regulatory role in allergic inflammation associated with asthma, may decrease their response due to the increase in neutrophil and monocyte counts (25). According to these findings, utilizing the SIRI to predict the mortality rate of asthma patients is suitable.
Other complete blood count (CBC) parameters, such as eosinophil count and red cell distribution width (RDW), have been suggested to play a significant role in asthma pathobiology. The study by Wenzel et al. indicated that eosinophils are critical in the inflammatory processes of asthma, particularly in patients with severe, corticosteroid-resistant asthma (26). Additionally, other CBC parameters such as RDW have been suggested as markers of hypoxia in COPD. According to a study by Karampitsakos et al., increased RDW is a negative prognostic marker in COPD patients (27). Preliminary findings have also shown promising data regarding the role of RDW in asthma (28). These findings suggest that RDW could potentially be used as a marker of hypoxia and systemic inflammation in asthma, providing a broader perspective on the utility of CBC parameters in managing and understanding asthma.
Asthma and COPD are distinct respiratory conditions with overlapping symptoms, making the differentiation between these diseases and the asthma-COPD overlap syndrome (ACOS) challenging. ACOS represents a condition where patients exhibit clinical features of both asthma and COPD, often leading to more severe symptoms and complications. The diagnosis and management of ACOS are complex due to the lack of standardized criteria and biomarkers. Karampitsakos et al. proposed fractional exhaled nitric oxide (FeNO) as a potential biomarker to aid in distinguishing these conditions (29). Thus, identifying clinically applicable biomarkers of inflammation in asthma, specifically mentioning the role of FeNO and other potential biomarkers such as eosinophil count and RDW, is important for further research in these areas.
The strengths of this study are as follows: First, our study is the first to investigate the association between SIRI levels and mortality risk in patients with asthma. Second, our research included 6,156 participants, providing a large dataset for statistical analysis. Third, we also covered potential risk factors, which make our statistical results more credible. However, there are limitations to consider in our study. The NHANES database is based on cross-sectional survey data; this type of survey data focuses on specific time points but does not establish causality or track the long-term relationship between asthma and mortality. Accordingly, future studies using longitudinal data will provide stronger evidence for this evaluation. Although we had adjusted for several potential confounding factors, there were still some unmeasured confounders we missed. The biological mechanisms that potentially link SIRI to increased mortality in asthma remain unclear. Therefore, future research aimed at exploring these mechanisms is necessary.
In summary, our study provides evidence that higher SIRI levels are relevant to the increased all-cause mortality in patients with asthma. However, further research is warranted to confirm our findings.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: Publicly available datasets were analyzed in this study. This data can be found at: https://www.cdc.gov/nchs/nhanes/index.htm.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the patients/ participants was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
FX: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. HJ: Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Software, Validation, Writing – review & editing. FL: Conceptualization, Formal analysis, Project administration, Resources, Supervision, Writing – review & editing. YW: Conceptualization, Methodology, Project administration, Visualization, Writing – review & editing. PJ: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. FC: Formal analysis, Investigation, Methodology, Project administration, Writing – review & editing. YF: Formal analysis, Investigation, Methodology, Project administration, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Enilari, O, and Sinha, S. The global impact of asthma in adult populations. Ann Glob Health. (2019) 85:2. doi: 10.5334/aogh.2412
2. Jin, Z, Wu, Q, Chen, S, Gao, J, Li, X, Zhang, X, et al. The associations of two novel inflammation indexes, SII and SIRI with the risks for cardiovascular diseases and all-cause mortality: a ten-year follow-up study in 85,154 individuals. J Inflamm Res. (2021) 14:131–40. doi: 10.2147/JIR.S283835
3. Cao, Y, Zheng, X, Hu, Y, Li, J, Huang, B, Zhao, N, et al. Levels of systemic inflammation response index are correlated with tumor-associated bacteria in colorectal cancer. Cell Death Dis. (2023) 14:69. doi: 10.1038/s41419-023-05602-9
4. Wang, H, and Li, W. Prognostic significance of SIRI in patients with late-stage lung adenocarcinoma receiving EGFR-TKI treatment. Curr Probl Cancer. (2024) 50:101099. doi: 10.1016/j.currproblcancer.2024.101099
5. Zhang, S, and Cheng, T. Prognostic and clinicopathological value of systemic inflammation response index (SIRI) in patients with breast cancer: a meta-analysis. Ann Med. (2024) 56:2337729. doi: 10.1080/07853890.2024.2337729
6. Zhu, D, Wang, C, Zhou, Y, Che, H, Wang, R, Cheng, L, et al. The associations of two novel inflammation biomarkers, SIRI and SII, with mortality risk in patients with chronic heart failure. J Inflamm Res. (2024) 17:1255–64. doi: 10.2147/JIR.S451190
7. Zhao, S, Dong, S, Qin, Y, Wang, Y, Zhang, B, and Liu, A. Inflammation index SIRI is associated with increased all-cause and cardiovascular mortality among patients with hypertension. Front Cardiovasc Med. (2022) 9:1066219. doi: 10.3389/fcvm.2022.1066219
8. Zhang, Y, Xing, Z, Zhou, K, and Jiang, S. The predictive role of systemic inflammation response index (SIRI) in the prognosis of stroke patients. Clin Interv Aging. (2021) 16:1997–2007. doi: 10.2147/CIA.S339221
9. Wang, RH, Wen, WX, Jiang, ZP, Du, ZP, Ma, ZH, Lu, AL, et al. The clinical value of neutrophil-to-lymphocyte ratio (NLR), systemic immune-inflammation index (SII), platelet-to-lymphocyte ratio (PLR) and systemic inflammation response index (SIRI) for predicting the occurrence and severity of pneumonia in patients with intracerebral hemorrhage. Front Immunol. (2023) 14:1115031. doi: 10.3389/fimmu.2023.1115031
10. Xia, Y, Xia, C, Wu, L, Li, Z, Li, H, and Zhang, J. Systemic immune inflammation index (SII), system inflammation response index (SIRI) and risk of all-cause mortality and cardiovascular mortality: a 20-year follow-up cohort study of 42,875 US adults. J Clin Med. (2023) 12:1128. doi: 10.3390/jcm12031128
11. Huang, P, Mai, Y, Zhao, J, Yi, Y, and Wen, Y. Association of systemic immune-inflammation index and systemic inflammation response index with chronic kidney disease: observational study of 40,937 adults. Inflamm Res. (2024) 73:655–67. doi: 10.1007/s00011-024-01861-0
12. Ke, J, Qiu, F, Fan, W, and Wei, S. Associations of complete blood cell count-derived inflammatory biomarkers with asthma and mortality in adults: a population-based study. Front Immunol. (2023) 14:1205687. doi: 10.3389/fimmu.2023.1205687
13. von Elm, E, Altman, DG, Egger, M, Pocock, SJ, Gøtzsche, PC, and Vandenbroucke, JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. (2007) 147:573–7. doi: 10.7326/0003-4819-147-8-200710160-00010
14. Zhu, N, Lin, S, Yu, H, Liu, F, Huang, W, and Cao, C. Naples prognostic score as a novel prognostic prediction indicator in adult asthma patients: a population-based study. World Allergy Organ J. (2023) 16:100825. doi: 10.1016/j.waojou.2023.100825
15. Wawryk-Gawda, E, Żybowska, M, and Ostrowicz, K. The neutrophil to lymphocyte ratio in children with bronchial asthma. J Clin Med. (2023) 12:6869. doi: 10.3390/jcm12216869
16. Huang, WJ, Huang, GT, Zhan, QM, Chen, JL, Luo, WT, Wu, LH, et al. The neutrophil to lymphocyte ratio as a novel predictor of asthma and its exacerbation: a systematic review and meta-analysis. Eur Rev Med Pharmacol Sci. (2020) 24:11719–28. doi: 10.26355/eurrev_202011_23819
17. Liu, X, Ge, H, Feng, X, Hang, J, Zhang, F, Jin, X, et al. The combination of Hemogram indexes to predict exacerbation in stable chronic obstructive pulmonary disease. Front Med (Lausanne). (2020) 7:572435. doi: 10.3389/fmed.2020.572435
18. Zinellu, A, Zinellu, E, Mangoni, AA, Pau, MC, Carru, C, Pirina, P, et al. Clinical significance of the neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in acute exacerbations of COPD: present and future. Eur Respir Rev. (2022) 31:220095. doi: 10.1183/16000617.0095-2022
19. Benz, E, Wijnant, SRA, Trajanoska, K, Arinze, JT, de Roos, EW, de Ridder, M, et al. Sarcopenia, systemic immune-inflammation index and all-cause mortality in middle-aged and older people with COPD and asthma: a population-based study. ERJ Open Res. (2022) 8:00628–2021. doi: 10.1183/23120541.00628-2021
21. Eguíluz-Gracia, I, Malmstrom, K, Dheyauldeen, SA, Lohi, J, Sajantila, A, Aaløkken, R, et al. Monocytes accumulate in the airways of children with fatal asthma. Clin Exp Allergy. (2018) 48:1631–9. doi: 10.1111/cea.13265
22. Han, P, Chen, L, Chen, D, Yang, R, Wang, W, Liu, J, et al. Upregulated expression of substance P and NK1R in blood monocytes and B cells of patients with allergic rhinitis and asthma. Clin Exp Immunol. (2022) 210:39–52. doi: 10.1093/cei/uxac074
23. Rastogi, D, Fraser, S, Oh, J, Huber, AM, Schulman, Y, Bhagtani, RH, et al. Inflammation, metabolic dysregulation, and pulmonary function among obese urban adolescents with asthma. Am J Respir Crit Care Med. (2015) 191:149–60. doi: 10.1164/rccm.201409-1587OC
24. Zhang, M, Yu, Q, Tang, W, Wu, Y, Lv, J, Sun, L, et al. Epithelial exosomal contactin-1 promotes monocyte-derived dendritic cell-dominant T-cell responses in asthma. J Allergy Clin Immunol. (2021) 148:1545–58. doi: 10.1016/j.jaci.2021.04.025
25. Schuijs, MJ, Willart, MA, Hammad, H, and Lambrecht, BN. Cytokine targets in airway inflammation. Curr Opin Pharmacol. (2013) 13:351–61. doi: 10.1016/j.coph.2013.03.013
26. Wenzel Sally, E . Eosinophils in asthma — closing the loop or opening the door? N Engl J Med. (2009) 360:1026–8. doi: 10.1056/NEJMe0900334
27. Karampitsakos, T, Dimakou, K, Papaioannou, O, Chrysikos, S, Kaponi, M, Bouros, D, et al. The role of increased red cell distribution width as a negative prognostic marker in patients with COPD. Pulm Pharmacol Ther. (2020) 60:101877. doi: 10.1016/j.pupt.2019.101877
28. Bozkurt, B, and Kizilirmak, D. Relation of hemogram parameters with asthma. Eur Respir J. (2015) 46:PA1102. doi: 10.1183/13993003.congress-2015.PA1102
Keywords: systemic immune-inflammation index, mortality, asthma, NHANES, association
Citation: Xu F, Jiang H, Li F, Wen Y, Jiang P, Chen F and Feng Y (2024) Association between the systemic inflammation response index and mortality in the asthma population. Front. Med. 11:1446364. doi: 10.3389/fmed.2024.1446364
Edited by:
Harissios Vliagoftis, University of Alberta, CanadaReviewed by:
Su-Boon Yong, China Medical University, TaiwanOurania Papaioannou, General University Hospital of Patras, Greece
Copyright © 2024 Xu, Jiang, Li, Wen, Jiang, Chen and Feng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yongwen Feng, ZmVuZ3lvbmd3ZW4yMDA4QDEyNi5jb20=; Feng Chen, MTIzMzgyOTY2QHFxLmNvbQ==; Pan Jiang, amlhbmdwYW5wcml2YXRlQDE2My5jb20=
†These authors have contributed equally to this work
 Feng Xu
Feng Xu Hui Jiang2†
Hui Jiang2†