- 1Department of Respiratory and Critical Care Medicine, The Affiliated Hospital of Qingdao University, Qingdao, China
- 2Department of Gastroenterology, The Affiliated Hospital of Qingdao University, Qingdao, China
- 3Department of Anesthesiology, The Affiliated Hospital of Qingdao University, Qingdao, China
Background: Capsule endoscopy (CE) is widely used for intestinal examination; however, capsule aspiration into the airway is a serious complication that requires urgent intervention. We present a management case report and review 39 cases from 2003 to 2023, providing insights into the prevention and treatment of capsule aspiration.
Case presentation: A 69-year-old man with chronic bronchitis and emphysema presented with 7 months of intermittent melena. After swallowing a capsule endoscope (PillCam™ SB 3), he had a brief cough and chest tightness. Imaging confirmed aspiration in the right intermediate bronchus, and non-invasive removal procedures were unsuccessful.
Methods: Real-time imaging confirmed the lodged capsule. Non-invasive methods, such as coughing and chest percussion, were unsuccessful. Therefore, flexible bronchoscopy was performed under general anesthesia to retrieve the capsule using a snare, which was then placed into the duodenum using a gastroscope.
Results: The capsule was successfully retrieved, and the patient recovered well, completing the endoscopy without further issues.
Conclusion: Our case study and literature review highlight the need for careful attention to high-risk groups in CE, including the elderly and individuals with neurological or swallowing difficulties. A thorough history review and real-time monitoring are essential for preventing complications. Bronchoscopy is preferred for CE retrieval due to its advantages. Manufacturers are urged to improve CE safety, with respiratory physicians helping internists in managing this potentially life-threatening complication.
Introduction
Capsule endoscopy (CE) is a primary diagnostic tool for small bowel diseases due to its non-invasiveness and safety in diagnosing mucosal diseases. It has pioneered a new mode of examination for the entire digestive tract (1, 2). This innovative technique involves swallowing a small, pill-sized capsule containing a camera that captures images as it traverses the digestive tract. Capsule endoscopy is very useful for investigating obscure gastrointestinal bleeding (3), diagnosing Crohn’s disease (4), assessing small bowel disorders (5), and detecting abnormalities, such as polyps or tumors in the small intestine (6). Its non-invasive nature makes it a valuable tool for patients who may find traditional endoscopic procedures uncomfortable or challenging. In addition, capsule endoscopy is an effective diagnostic tool when conventional imaging methods fail to identify the underlying causes of gastrointestinal symptoms. However, adverse events such as CE retention, difficulty swallowing, aspiration, and missed diagnosis can still occur in clinical applications (1).
Despite occasional instances in previously documented cases where patients were able to naturally expel aspirated capsules from the respiratory tract and later re-ingest them into the digestive system (7), capsule aspiration remains a serious complication requiring prompt intervention. While spontaneous resolution is possible in some cases, the unpredictable nature of this response underscores the need for vigilance and intervention to mitigate potential adverse outcomes. Therefore, clinicians must remain alert to the severity of capsule aspiration as a serious complication, emphasizing the need for timely and appropriate medical management. CE aspiration is an emergent complication that requires immediate intervention. Previous studies have reported several methods for managing CE aspiration, including the use of rigid or flexible bronchoscopy with various tools to aid in manipulation (8). We further conducted a detailed analysis of previous studies documenting cases of CE aspiration to identify common clinical features and effective management strategies to provide valuable references for future instances.
However, as of now, standardized treatment strategies for this potentially fatal complication have not been established. This report examines the causes of capsule aspiration and suggests preventive measures, emphasizing the importance of physicians familiarizing themselves with management options.
Case presentation
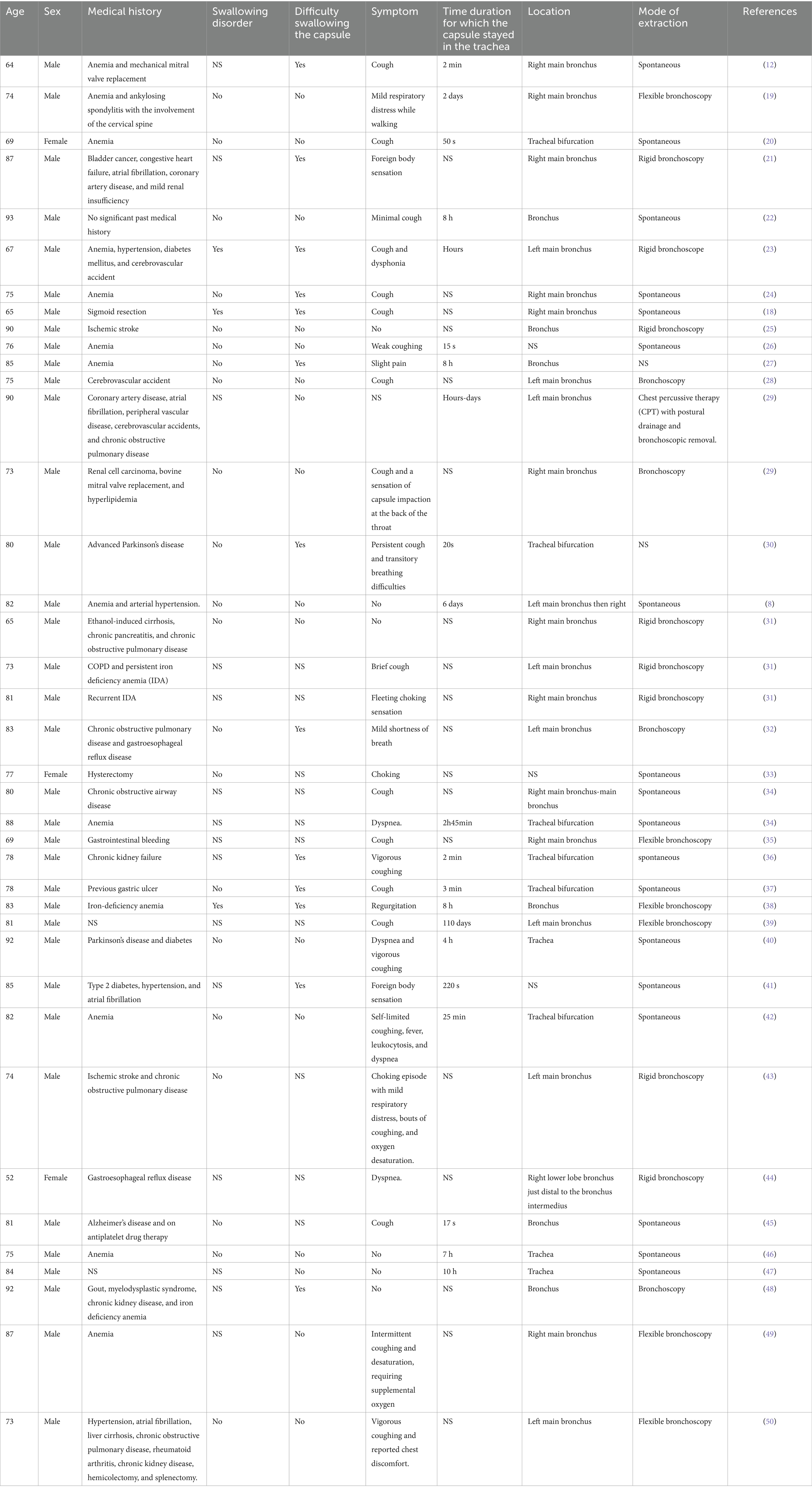
A 69-year-old man with a history of chronic bronchitis and emphysema presented to our hospital with intermittent melena for 7 months. Previous endoscopy revealed chronic atrophic gastritis and multiple colon polyposis. Upon swallowing a capsule endoscope (PillCam™ SB 3 Capsule Endoscopy System, Medtronic), the patient immediately experienced coughing and chest tightness lasting approximately 1 min. The physical examination revealed decreased inspiratory sounds and expiratory wheezing in the central part of the right lung, indicating capsule aspiration. Meanwhile, the CE image showed a real-time recording of the tracheal cartilage ring and typical airways, supporting this diagnosis (Figure 1a). As the capsule was lodged in the right intermediate bronchus, the symptoms of cough and dysphagia were not evident. We encouraged the patient to cough actively and performed postural drainage and chest percussion therapy in an attempt to remove the capsule spontaneously. Unfortunately, the capsule remained lodged in the right intermediate bronchus.

Figure 1. Removal process of the capsule endoscope (a) real-time capsule endoscopic images showing the tracheal cartilage ring and typical airways. (b,c) Bronchoscopic view shows the capsule lodged in the bronchus intermedius. (b) Tracheal carina and (c) right main bronchus. (d) Capsule endoscopy successfully removed the capsule from the airway.
As previously reported, flexible bronchoscopy or hard endoscopy examination is the most preferred approach to retrieve the capsule. Given the patient’s history of pulmonary disease and the unpredictable timing of the surgery, we opted to perform the procedure with general anesthesia, using a laryngeal mask airway for ventilation support. The bronchoscopy revealed that the capsule was located in the right intermediate bronchus (Figures 1b,c). Despite the challenge posed by the capsule’s smooth surface coated with mucus, we were able to successfully retrieve it with the use of a snare (Figure 1d).
Given the patient’s high risk of aspiration, we decided to bypass the esophagus and directly place the capsule into the duodenum using a gastroscope. However, during the procedure, we encountered several obstacles, such as difficulty in accurately entering the esophagus with the gastroscope and the capsule falling back into the trachea. This occurred because the capsule in front of the gastroscope obstructed the endoscope’s view of its progression. Fortunately, by adjusting the patient’s position and modifying the method of securing the capsule to the gastroscope, we successfully implanted the capsule into the duodenum (Figure 2). The patient recovered well and completed the video capsule endoscopy the following day.
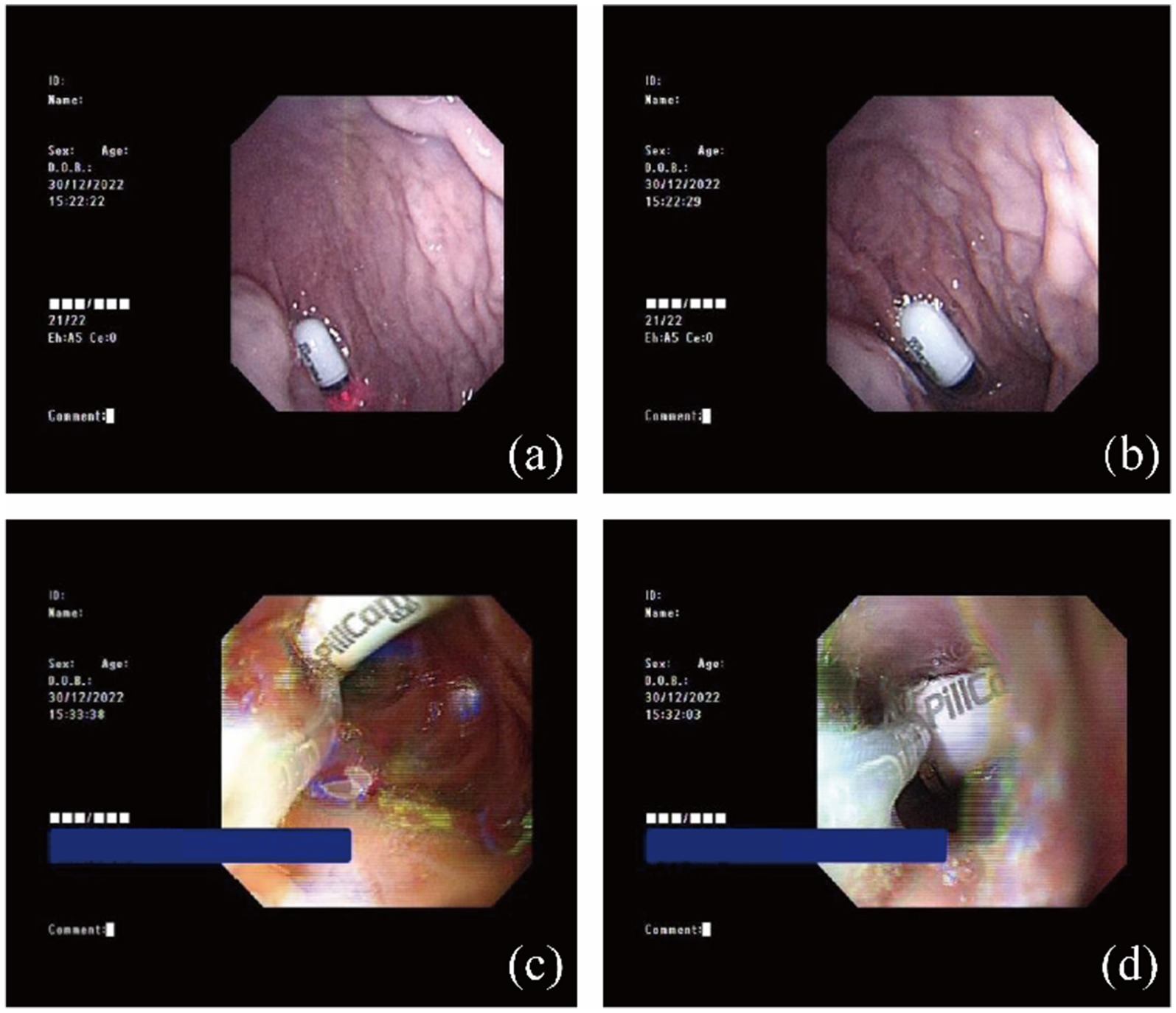
Figure 2. Successfully pushed the capsule endoscope into the duodenum. (a,b) The capsule endoscope in the stomach. (c,d) The capsule endoscope in the duodenum.
Discussion and literature review
CE, as an effective tool for directly evaluating the intestinal lumen via a video, has become widely accepted in recent clinical gastrointestinal investigations. With high patient acceptance and safety, the indications for CE have expanded to include obscure gastrointestinal bleeding, inflammatory bowel diseases without ileus, and other abnormalities that cannot be confirmed by gastrointestinal endoscopy or colonoscopy (9, 10). The overall complication rate of CE is low, with CE retention occurring in approximately 2% of all cases (11). However, one isolated but emergent complication that requires multi-departmental effort is capsule aspiration into the trachea or bronchial tree. Schneider et al. published the first case of M2A capsule aspiration since the diagnostic method became available in general clinical practice in 2003. The patient aspirated the capsule into the right main bronchus on the fourth attempt, but coughed it out after 2 min. The subsequent evaluation confirmed appropriate swallowing and small-bowel visualization (12).
While the case had a relatively benign outcome, a broader review of the literature revealed a more varied and complex picture of capsule aspiration events. Using “capsule endoscopy” and “aspiration” as keywords, a search on PubMed identified a total of 39 cases reported between 2003 and 2023 (Table 1). The majority of the patients were over 60 years old (38/39, 97.4%), with most being male (36/39, 92.3%). All patients had underlying conditions; however, only three cases (7.7%) had a documented history of swallowing difficulties. One-third of the patients (13/39) experienced difficulties swallowing the capsule. After aspiration, except for a few patients (8/39, 20.5%) who remained asymptomatic, the majority of them experienced coughing, a sensation of a foreign body in the throat, and respiratory difficulties. The capsules mostly lodged into the right main bronchus. Following aspiration, a subset of patients (18/39) either spontaneously coughed out the capsule or re-swallowed it into their digestive tract. Bronchoscopy has emerged as the most commonly used method for managing capsule endoscopy aspiration, and in this case, the capsule was successfully retrieved using a flexible bronchoscope. Notably, in one case involving a 77-year-old man, despite briefly expelling the capsule after aspiration, the patient succumbed to a cerebrovascular accident. In addition, another patient suffered atelectasis following capsule retrieval, while the remaining patients had good post-extraction outcomes. A logistic regression analysis was conducted to assess whether factors such as age, sex, and the presence of coughing symptoms had a significant effect on poor prognosis. The results indicated that these variables did not have any statistically significant impact (p > 0.05, Table 2). The small sample size of 39 cases might have limited the ability to detect meaningful associations. Patient variability, such as comorbidities and symptom severity, might have obscured the impact of the analyzed variables. Unmeasured factors, such as individual responses to aspiration or medical management, could also have played a larger role, making age, sex, and coughing symptoms less predictive. In addition, with only two poor outcomes, it was difficult to identify clear predictors.
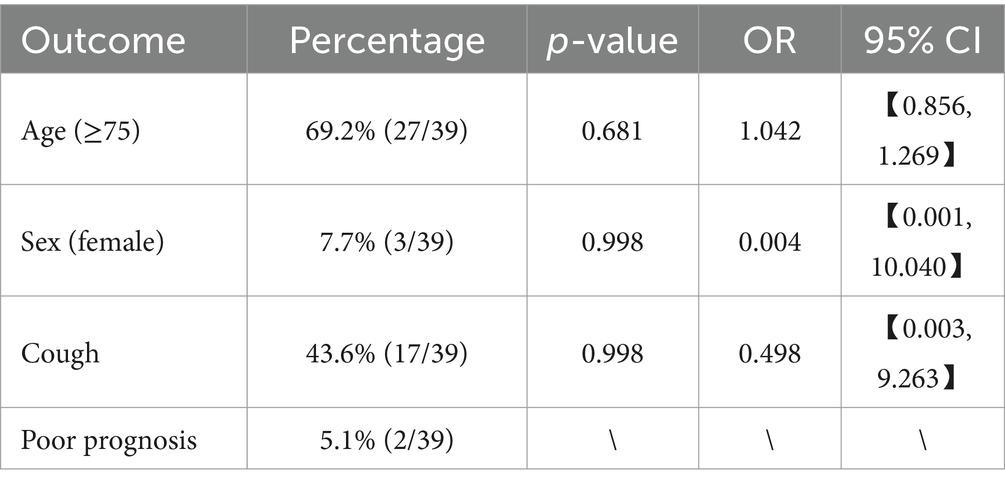
Table 2. Statistical analysis of the demographics and cough symptoms impacting the prognosis after capsule endoscopy retrieval.
In summary, capsule aspiration primarily occurs in elderly patients, with key risk factors including depressed mental status, impaired cough reflex, esophageal sphincter relaxation, and reduced laryngopharyngeal sensitivity. These factors have shifted the high-risk group toward this population (13, 14). Interestingly, recent research has shown an increase in iatrogenic causes of aspiration, including intubation, tracheostomy tube changes, dental procedures, and CE. Although few patients reported difficulty swallowing, the majority reported coughing, as well as symptoms such as transient choking, a foreign body sensation, and dyspnea, which varied based on the position of the capsule in the airway. A multicenter study revealed that the right bronchial tree, particularly the right bronchus intermedius and right lower lobe basal segment, is the most common site for capsule aspiration (15). In addition, insights from the study by Ulas et al. indicate that foreign body aspiration (FBA) presents significant diagnostic challenges, especially in children, where non-opaque foreign bodies complicate radiological evaluations and may lead to delays in diagnosis. Their findings suggest that immediate interventions, such as rigid bronchoscopy, are crucial for managing these cases (16).
In terms of aspiration treatment, in some cases, it can be resolved through active cough, chest percussion therapy, and postural drainage. However, CE aspiration often warrants an invasive procedure, with bronchoscopic retrieval preferred to avoid long-term sequelae. Previous bronchoscopic techniques for CE removal included rigid and flexible bronchoscopy, with assistant devices for manipulation, such as foreign body forceps, expandable basket foreign body retrieval devices, and balloon catheters. From the present case and previous case reports, we summarized several experiences and suggestions for improvement, as follows: ① when conducting CE, gastroenterologists should raise their awareness of the above-mentioned high-risk population. All medical histories should be evaluated, especially concerning neurological disorders, degenerative conditions, and swallowing difficulties. To timely localize the capsule, they must pay attention to the endoscopic return image in real time and, if necessary, perform additional auxiliary examinations, such as chest X-ray or CT scan. Next, while managing patients at risk of aspiration, selecting a suitable postural position and providing instructions to modify swallowing techniques are useful. ② Due to the large size and smooth surface of the capsule, the retrieval process is prone to slippage, making the timing of the procedure unpredictable. Therefore, it is recommended to use general anesthesia with the assistance of a laryngeal mask airway for ventilation. ③ As there is no grip point on the surface of capsule endoscopes, using a snare or stone retrieval basket is more advantageous for the retrieval process.④ When aspiration has already occurred and the patient is under general anesthesia, it is recommended that the capsule be directly delivered into the duodenum with gastroscope assistance (17, 18) during the procedure to avoid further aspiration due to active swallowing.⑤ During the process of pushing the capsule into the gastrointestinal tract, it is difficult to accurately guide a gastroscope into the esophagus because the capsule in front of the endoscope blocks the view of its progression. Therefore, adopting a position with the neck flexed and the head bowed or performing tracheal intubation can help prevent the capsule from falling back into the trachea. ⑥ Flexible bronchoscopy should be attempted first in cases where the patient is not in respiratory distress as it carries lower risks and has a high success rate of approximately 90% for foreign body removal. If necessary, early conversion to rigid bronchoscopy is crucial to avoid complications from excessive manipulation. Finally, a surgical thread can be wrapped around the capsule to facilitate emergency retrieval in high-risk patients. ⑦ For manufacturers, it would be beneficial to incorporate a grip point on the surface of the capsule, such as carving a groove in the middle or designing a textured surface that aligns with commonly used retrieval tools, such as snare loops. This would allow for easier and more secure retrieval in cases of aspiration. In addition, modifying the capsule’s size and weight could help reduce the risk of it becoming lodged in the airway. Exploring biocompatible materials with both flexibility and firmness would also enhance the capsule’s maneuverability during its passage through the esophagus and digestive tract, potentially minimizing the risk of accidental aspiration. Another design consideration could be incorporating a retractable safety mechanism or sheath to prevent the capsule from entering the airway during swallowing, further reducing the risk of aspiration in high-risk patients.
The cases detailed above involve elderly male patients who, after inadvertent ingestion, presented with typical symptoms such as persistent cough and chest discomfort. In line with the patterns observed in the majority of cases documented in the literature, the capsule became lodged in the right main bronchus. CE aspiration is specific to the medical device used for gastrointestinal examination, primarily affecting patients with predisposing factors. Its prevention relies on a thorough risk assessment before the procedure. To address this, we opted for the conventional approach of using a flexible bronchoscope for the extraction of the capsule. Subsequently, with the assistance of a gastroscope, we carefully maneuvered the capsule directly into the duodenum, thereby mitigating the potential risk of recurrent aspiration. Our intention in presenting these cases is to raise the awareness of internal medicine practitioners regarding the potential complications associated with capsule aspiration. By sharing our experiences, we aimed to provide valuable insights and serve as a reliable reference for effectively managing this serious complication. It is our fervent hope that this report will prove beneficial in guiding medical professionals on the nuances of dealing with capsule aspiration and underscore the importance of preventive measures to minimize the associated risks.
Conclusion
In conclusion, more information is needed to tackle aspiration during CE practices. Elderly patients and those with neurological or swallowing disorders and spinal abnormalities should be regarded as a high-risk population for CE aspiration. Performing routine investigations of the related medical history, taking precautionary measures, and monitoring in real-time is essential. Bronchoscopy stands out for its dual functionality, excelling in both meticulous inspection and effective treatment, making it the preferred method for the retrieval of capsule endoscopes. This multifaceted capability not only facilitates successful capsule extraction but also allows for immediate intervention if any complications arise during the procedure. As we navigate the evolving landscape of medical technology, we look forward to advancements from manufacturers in developing capsule endoscopes that are not only scientifically advanced but also equipped with enhanced safety features. By fostering continuous innovation in this field, we can ensure the development of more reliable and secure capsule endoscopy devices for the benefit of both clinicians and patients.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
YZ: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. HW: Writing – review & editing, Visualization, Validation, Supervision, Software, Resources, Project administration, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization. MZ: Writing – review & editing. HL: Writing – review & editing, Supervision, Software, Methodology, Investigation, Conceptualization. LQ: Writing – review & editing. LZ: Writing – review & editing. JS: Writing – review & editing, Writing – original draft.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was funded by the Health Science and Technology Development Program of Shandong Province, as well as the Medical and Health Research in Qingdao Mentoring Project (grant numbers 202203020560 and 2022-WJZD183).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
FBA, Foreign body aspiration; OGIB, obscure gastrointestinal bleeding; CE, capsule endoscopy.
References
1. Rondonotti, E, Herrerias, JM, Pennazio, M, Caunedo, A, Mascarenhas-Saraiva, M, and de Franchis, R. Complications, limitations, and failures of capsule endoscopy: a review of 733 cases. Gastrointest Endosc. (2005) 62:712–716; quiz 752, 754.
2. Melson, J, Trikudanathan, G, Abu Dayyeh, BK, Bhutani, MS, Chandrasekhara, V, Jirapinyo, P, et al. Video capsule endoscopy. Gastrointest Endosc. (2021) 93:784–96. doi: 10.1016/j.gie.2020.12.001
3. Hirata, I, Tsuboi, A, Matsubara, Y, Sumioka, A, Takasago, T, Tanaka, H, et al. Long-term outcomes of patients with obscure gastrointestinal bleeding after negative capsule endoscopy. J Gastroenterol Hepatol. (2023) 39:165–71. doi: 10.1111/jgh.16379
4. da Silva Júnior, RT, Apolonio, JS, de Souza Nascimento, JO, da Costa, BT, Malheiro, LH, Silva Luz, M, et al. Crohn’s disease and clinical management today: how it does? World J Methodol. (2023) 13:399–413. doi: 10.5662/wjm.v13.i5.399
5. De Simone, F, Machado, P, and Guzmán Calderon, E. Diagnostic and therapeutic approach to small bowel disorders through capsule endoscopy and double-balloon endoscopy. Revista de gastroenterologia del Peru. (2017) 37:58–64.
6. Kim, HJ, Gong, EJ, Bang, CS, Lee, JJ, Suk, KT, and Baik, GH. Computer-aided diagnosis of gastrointestinal protruded lesions using wireless capsule endoscopy: a systematic review and diagnostic test accuracy meta-analysis. J Pers Med. (2022) 12:644. doi: 10.3390/jpm12040644
7. Yung, DE, Plevris, JN, and Koulaouzidis, A. Short article: aspiration of capsule endoscopes: a comprehensive review of the existing literature. Eur J Gastroenterol Hepatol. (2017) 29:428–34. doi: 10.1097/MEG.0000000000000821
8. Lucendo, AJ, González-Castillo, S, Fernández-Fuente, M, and De Rezende, LC. Tracheal aspiration of a capsule endoscope: a new case report and literature compilation of an increasingly reported complication. Dig Dis Sci. (2011) 56:2758–62. doi: 10.1007/s10620-011-1666-2
9. Moglia, A, Pietrabissa, A, and Cuschieri, A. Capsule endoscopy. BMJ. (2009) 339:b3420. doi: 10.1136/bmj.b3420
10. Akpunonu, B, Hummell, J, Akpunonu, JD, and Ud Din, S. Capsule endoscopy in gastrointestinal disease: evaluation, diagnosis, and treatment. Cleve Clin J Med. (2022) 89:200–11. doi: 10.3949/ccjm.89a.20061
11. Rezapour, M, Amadi, C, and Gerson, LB. Retention associated with video capsule endoscopy: systematic review and meta-analysis. Gastrointest Endosc. (2017) 85:1157–1168.e2. doi: 10.1016/j.gie.2016.12.024
12. Schneider, AR, Hoepffner, N, Rösch, W, and Caspary, WF. Aspiration of an M2A capsule. Endoscopy. (2003) 35:713. doi: 10.1055/s-2003-41527
13. Benjelloun, H, Zaghba, N, Bakhatar, A, Yassine, N, and Bahlaoui, A. Tracheobronchial foreign bodies in adults. Pan Afr Med J. (2014) 19:220. doi: 10.11604/pamj.2014.19.220.4952
14. Limper, AH, and Prakash, UB. Tracheobronchial foreign bodies in adults. Ann Intern Med. (1990) 112:604–9. doi: 10.7326/0003-4819-112-8-604
15. Jang, G, Song, JW, Kim, HJ, Kim, EJ, Jang, JG, and Cha, SI. Foreign-body aspiration into the lower airways in adults; multicenter study. PLoS One. (2022) 17:e0269493. doi: 10.1371/journal.pone.0269493
16. Ulas, AB, Aydin, Y, and Eroglu, A. Foreign body aspirations in children and adults. Am J Surg. (2022) 224:1168–73. doi: 10.1016/j.amjsurg.2022.05.032
17. Toth, E, Fork, FT, Almqvist, P, and Thorlacius, H. Endoscopy-assisted capsule endoscopy in patients with swallowing disorders. Endoscopy. (2004) 36:746–7; author reply 747-748. doi: 10.1055/s-2004-825685
18. Bredenoord, AJ, Stolk, MF, and Al-toma, A. Unintentional video capsule bronchoscopy. Eur J Gastroenterol Hepatol. (2009) 21:593. doi: 10.1097/MEG.0b013e328326cae2
19. Buchkremer, F, Herrmann, T, and Stremmel, W. Mild respiratory distress after wireless capsule endoscopy. Gut. (2004) 53:472. doi: 10.1136/gut.2003.033845
20. Sinn, I, Neef, B, and Andus, T. Aspiration of a capsule endoscope. Gastrointest Endosc. (2004) 59:926–7. doi: 10.1016/S0016-5107(04)00291-3
21. Tabib, S, Fuller, C, Daniels, J, and Lo, SK. Asymptomatic aspiration of a capsule endoscope. Gastrointest Endosc. (2004) 60:845–8. doi: 10.1016/S0016-5107(04)02032-2
22. Nathan, SR, and Biernat, L. Aspiration - an important complication of small-bowel video capsule endoscopy. Endoscopy. (2007) 39:E343. doi: 10.1055/s-2007-995327
23. Sepehr, A, Albers, GC, and Armstrong, WB. Aspiration of a capsule endoscope and description of a unique retrieval technique. Otolaryngology. (2007) 137:965–6.
24. Shiff, AD, Leighton, JA, and Heigh, RI. Pulmonary aspiration of a capsule endoscope. Am J Gastroenterol. (2007) 102:215–6.
25. Guy, T, Jouneau, S, D'Halluin, PN, and Lena, H. Asymptomatic bronchial aspiration of a video capsule. Interact Cardiovasc Thorac Surg. (2009) 8:568–70. doi: 10.1510/icvts.2008.190058
26. Koulaouzidis, A, Pendlebury, J, Douglas, S, and Plevris, JN. Aspiration of video capsule: rare but potentially life-threatening complication to include in your consent form. Am J Gastroenterol. (2009) 104:1602–3. doi: 10.1038/ajg.2009.93
27. Leeds, JS, Chew, TS, Sidhu, R, Elliot, CA, Sanders, DS, and McAlindon, ME. Asymptomatic bronchial aspiration and retention of a capsule endoscope. Gastrointest Endosc. (2009) 69:561–2. doi: 10.1016/j.gie.2008.09.044
28. Choi, HS, Kim, JO, Kim, HG, Lee, TH, Kim, WJ, Cho, WY, et al. A case of asymptomatic aspiration of a capsule endoscope with a successful resolution. Gut Liver. (2010) 4:114–6. doi: 10.5009/gnl.2010.4.1.114
29. Depriest, K, Wahla, AS, Blair, R, Fein, B, and Chin, R Jr. Capsule endoscopy removal through flexible bronchoscopy. Respiration. (2010) 79:421–4. doi: 10.1159/000255763
30. Kurtz, LE, Devito, B, and Sultan, K. Electronic image of the month. Small bowel video capsule aspiration with bronchoscopic-assisted extraction. Clin Gastroenterol Hepatol. (2010) 8:e37–8. doi: 10.1016/j.cgh.2009.10.024
31. Pezzoli, A, Fusetti, N, Carella, A, and Gullini, S. Asymptomatic bronchial aspiration and prolonged retention of a capsule endoscope: a case report. J Med Case Rep. (2011) 5:341. doi: 10.1186/1752-1947-5-341
32. Girdhar, A, Usman, F, and Bajwa, A. Aspiration of capsule endoscope and successful bronchoscopic extraction. J Bronchol Interven Pulmonol. (2012) 19:328–31. doi: 10.1097/LBR.0b013e31826e3b53
33. Parker, C, Davison, C, and Panter, S. Tracheal aspiration of a capsule endoscope: not always a benign event. Dig Dis Sci. (2012) 57:1727–8. doi: 10.1007/s10620-012-2173-9
34. Ding, NS, Hair, C, De Cruz, P, and Watson, J. Education and imaging. Gastrointestinal: symptomatic bronchial aspiration of capsule endoscope - a significant complication. J Gastroenterol Hepatol. (2013) 28:761. doi: 10.1111/jgh.12173
35. Hall, JJ, Fischer, UM, Shah, SK, and Wilson, TD. Video endoscope removal from the right main bronchus using a flexible esophagogastroduodenoscope. Am Surg. (2013) 79:E185–6. doi: 10.1177/000313481307900503
36. Pereira, B, Santos, A, Leitão, C, and Banhudo, A. Aspiration of capsule endoscope. Rev Esp Enferm Dig. (2013) 105:438–9. doi: 10.4321/S1130-01082013000700015
37. Sánchez-Chávez, X, and Martínez-García, CL. Capsule endoscope aspiration: a common complication? Revista de gastroenterologia de Mexico. (2013) 78:257–8. doi: 10.1016/j.rgmx.2013.04.003
38. Hussan, H, Paradowski, TJ, and Prather, CM. Unexpected capsule endoscopy images reveal aspiration. ACG Case Rep J. (2014) 1:69. doi: 10.14309/crj.2014.2
39. Amarna, M, Vanlandingham, A, Brahmbhatt, P, Roy, TM, and Byrd, RP Jr. Late presentation of capsule endoscope aspiration with successful extraction by flexible bronchoscopy utilizing a snare wire loop. Endoscopy. (2015) 47:E6–7. doi: 10.1055/s-0034-1377543
40. Magalhães-Costa, P, Bispo, M, and Chagas, C. Aspiration of capsule endoscopy. GE Port J Gastroenterol. (2015) 22:178–9. doi: 10.1016/j.jpge.2015.03.004
41. Mannami, T, Ikeda, G, Seno, S, Sonobe, H, Fujiwara, N, Komoda, M, et al. Capsule endoscope aspiration after repeated attempts for ingesting a patency capsule. Case Rep Gastroenterol. (2015) 9:347–52. doi: 10.1159/000441382
42. Juanmartiñena Fernández, JF, Fernández-Urien, I, and Vila Costas, JJ. Asymptomatic bronchial aspiration of capsule endoscope: a significant complication. Rev Esp Enferm Dig. (2016) 108:605. doi: 10.17235/reed.2016.4363/2016
43. Buscot, M, Leroy, S, Pradelli, J, Chaabane, N, Hebuterne, X, Marquette, CH, et al. Bronchial aspiration of capsule endoscope. Respiration. (2017) 93:122–5. doi: 10.1159/000453587
44. Haseeb, A, Lateef, N, Bilal, M, Gaurav, K, Prudom, J, and Musani, A. Bravo® capsule aspiration: a rare case report. Cureus. (2017) 9:e 1556. doi: 10.7759/cureus.1556
45. Juanmartiñena Fernández, JF, Fernández-Urién Sainz, I, Zabalza Ollo, B, Lizarbe Larrea, A, Gomez Salvador, B, Montañes Guimera, M, et al. Transient tracheo-bronquial aspiration of capsule endoscope. Acta Gastro-Enterol Belg. (2017) 80:441.
46. Ribaldone, DG, Bruno, M, Solidoro, P, and De Angelis, C. Real time visualization may be advisable to exclude aspiration in patients undergoing capsule endoscopy examination. Rev Esp Enferm Dig. (2017) 109:878–9. doi: 10.17235/reed.2017.5244/2017
47. Keil-Ríos, D, Angulo-Molina, D, and Farca-Belsaguy, A. Ten-hour asymptomatic bronchoaspiration of a capsule endoscopy camera. Revista de gastroenterologia de Mexico. (2018) 83:451–2. doi: 10.1016/j.rgmx.2018.01.002
48. Gaisinskaya, P, Yoshinaga, K, and Hernandez, OL. Necessity of swallow evaluations in the elderly prior to capsule endoscopy. Cureus. (2022) 14:e24138. doi: 10.7759/cureus.24138
49. Tamang, S, and Mitnovetski, S. Capsule endoscopy in airway: a difficult extraction. J Surg Case Rep. (2022) 2022:rjac385. doi: 10.1093/jscr/rjac385
Keywords: capsule endoscope, complication, aspiration, bronchoscope, case report
Citation: Zhou Y, Wang H, Zhuang M, Liu H, Qi L, Zhang L and Sun J (2024) Capsule endoscopy aspiration and respiratory physician’s treatment insights: a case report and literature review. Front. Med. 11:1442245. doi: 10.3389/fmed.2024.1442245
Edited by:
Angel Lanas, University of Zaragoza, SpainCopyright © 2024 Zhou, Wang, Zhuang, Liu, Qi, Zhang and Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiaxing Sun, amlheGluZzIwMDIyMDAxQDE2My5jb20=
 Yinxue Zhou
Yinxue Zhou Hongmei Wang
Hongmei Wang Min Zhuang1
Min Zhuang1 Hua Liu
Hua Liu Lingyun Zhang
Lingyun Zhang Jiaxing Sun
Jiaxing Sun