- 1QU Health, Qatar University, Doha, Qatar
- 2Hamad Medical Corporation, Doha, Qatar
Introduction: Breaking bad news is a critical yet challenging aspect of healthcare that requires effective communication skills, empathy, and cultural sensitivity. Health professionals in the World Health Organization’s (WHO) Eastern Mediterranean Region face unique cultural and social factors distinct from other parts of the world. This scoping review aims to comprehensively explore the peer-reviewed literature on the health professionals’ experiences in delivering bad news within the WHO’s Eastern Mediterranean Region.
Methods: This scoping review was conducted according to the Joanna Brigg Institute’s scoping review methodology and reported utilizing the Preferred Reporting Items for Systematic Reviews extension for scoping review (PRISMA-ScR) guidelines. A search using a combination of keywords and MeSH terms related to “breaking bad news” and “health professionals” was performed in PubMed, Scopus, CINAHL, EBSCO, ERIC via Embase, and Dar Almandumah (Arabic) databases. Common themes were synthesized from studies conducted in the WHO’s Eastern Mediterranean Region.
Results: Out of 4,883 studies initially identified in the databases, 24 studies met the inclusion criteria, involving a total of 4,710 participants, including physicians, nurses, and residents. The studies were published between 2006 and 2022, predominantly from Iran (n = 12). The majority employed a cross-sectional design (n = 21) or mixed methods (n = 3), with a notable absence of qualitative studies. No studies used theoretical frameworks. More than half of the studies (n = 14) reported that participants had positive attitudes toward breaking bad news. This positivity was evident in their willingness to share bad news, perceived possession of adequate knowledge, positive attitudes, having received training, awareness of accepted approaches, and adherence to protocols. The lack of training and limited awareness of established protocols like SPIKES, ABCDE, and BREAKS for breaking bad news were major concerns among participants.
Conclusion: The scoping review reveals both positive and negative experiences of breaking bad news by health professionals in the WHO’s Eastern Mediterranean Region. Most studies highlight the need for culturally sensitive targeted education and training programs on breaking bad news. Further research, particularly using qualitative methodologies and theoretical frameworks is warranted.
1 Introduction
Breaking bad news to patients is widely recognized as a key aspect of clinical practice, yet it remains challenging for health professionals at all levels of experience (1–4). Acknowledging that the interpretation of what may be considered neutral, good, or bad is subjective, Ptacek and Eberhardt define “bad news” as, information that results in a cognitive, behavioral, and/or emotional deficit in the person receiving the news, which persists for a while (5). An individual’s response may be shaped by one’s life experiences, personality, spiritual beliefs, philosophical stance, perceived social support and/or emotional resilience (1, 6).
Breaking bad news can have devastating effects on patients and their families. Such disclosures may generate feelings of hopelessness and potentially adversely impact patient outcomes (7, 8). In addition, the manner in which bad news is delivered can exacerbate a patient’s emotional distress (9), and influence a patient’s perception of their condition and their adherence to the management plan (10).
For many health professionals, breaking bad news can be a daunting task. Evidence links this responsibility to exhaustion, fatigue, and burnout (4, 11–14); fear of making diagnostic errors and self-blame (12); poor practitioner self-care (12); and a reduced sense of personal accomplishment (13). Novice health professionals, in particular, may lack the experience to fully comprehend the myriad of patients’ concerns, and address these issues inadequately, fostering feelings of mistrust, anger, and fear (15). The challenges of breaking bad news may be compounded by factors beyond the patient-professional relationship, including family involvement, cultural influences, and institutional constraints (16).
Education and training at undergraduate and postgraduate levels, complemented with ongoing professional development, are essential to equip health professionals to break bad news effectively. Related interventions are associated with significant improvements in observer-rated news delivery skills and moderate improvements in confidence (17). Indeed, those who have not received formal education and training in this area often feel ill-prepared for the task (18). Although breaking bad news is recognized as an essential skill in undergraduate and graduate health programs (19), many health professionals report feeling ill-equipped and express the need for additional training (20, 21).
Protocols like SPIKES (Setting up, Perception, Invitation, Knowledge, Emotions with Empathy, and Strategy or Summary) (22) and the ABCDE model (Advanced preparation, Building therapeutic relationship, Communicating effectively, Dealing with reactions, and Encouraging emotions) (23, 24) are increasingly employed to provide a structure to breaking bad news with synthesized evidence of their effectiveness (25). Respect, support, and empathy are central to these approaches which aim to mitigate the negative impact of breaking bad news (26).
Effective communication of bad news has been studied extensively in Western medical contexts, which often emphasize secularism, individualism, and patient autonomy (27). In Western culture, patients expect to be provided with at least some information about their disease and an estimate of their prognosis (28). The gold standard for delivering bad news in the West is to speak directly to the patient and their family (29). Western ethics unequivocally supports disclosing bad news to patients. Concealing the truth can lead to a crisis of conscience and psychological exhaustion among healthcare workers (30). However, it is important to acknowledge that the Western emphasis on autonomy and truth is distinctive and not universally shared, with some cultures prioritizing harmony over truth (31). These cultural differences can lead to professional dilemmas. For instance, Malaysian medical students studying a Western curriculum noted a significant disparity: 64% of students in Malaysia reported that relatives are informed of a diagnosis before the patient, compared to only 2% of students in the UK (32). In contrast, in the UK, withholding a diagnosis from the patient would violate professional guidelines and would only be permissible within the legal framework in exceptional circumstances (33, 34).
Less is known, however, about disclosures of bad news in non-Western cultural milieus, such as the World Health Organization (WHO) Eastern Mediterranean Region (EMR) (28). This predominantly Arab-Muslim region comprises 21 countries with a population of 679 million (35). Healthcare professionals in this region navigate a complex landscape of social, religious, and linguistic factors when breaking bad news. The religious and paternalistic cultural values guiding behavior, decision-making, perception, delivery, and the experiences of the stakeholders in the EMR need examination (36–39). This scoping review aims to address this gap by synthesizing the peer-reviewed literature on health professionals’ experiences of breaking bad news within the Eastern Mediterranean region. The findings of this scoping review will help understand cultural aspects and practices regarding breaking bad news in the EMR.
2 Methods
The scoping review was conducted in accordance with the Joanna Brigg Institute’s (JBI) methodology for scoping reviews (40) and is reported following the Preferred Reporting Items for Systematic Reviews extension for scoping review (PRISMA-ScR) guidelines (41).
The study inclusion criteria were based on the population, concept, and context model. Studies reporting views and experiences of any health professional population were included, with “breaking bad news” as the review concept. The geographic context was the WHO Eastern Mediterranean Region, which includes the Gulf Cooperation Council (GCC) members (Qatar, Saudi Arabia, Bahrain, Oman, Kuwait, and the United Arab Emirates), Djibouti, Egypt, Iran, Iraq, Israel, Jordan, Libya, Lebanon, Morocco, Syria, Malta, Tunisia, West Bank and Gaza, and Yemen (35).
The search was conducted in PubMed, Scopus, Embase, Cumulative Index to Nursing and Allied Health Literature (CINAHL), EBSCO, Education Resources Information Center (ERIC), and Dar Almandumah (Arabic database) to identify the relevant literature. The key search terms were “breaking bad news,” “health professionals,” and “Eastern Mediterranean Region,” modified as necessary for each database (see Supplementary material 1). Databases were searched from inception until July 2023. No language limitations were applied, ensuring a comprehensive review across diverse linguistic sources such as English and Arabic. Review articles, letters, opinion papers, and editorials were excluded. All identified citations were collated and uploaded into EndNote Web (Clarivate Analytics, PA, USA) and duplicates were removed. The remaining citations were exported to Rayyan QCRI® (42). Two independent reviewers screened titles and abstracts followed by full text for eligibility, with disagreements resolved by discussion or consultation with a third reviewer.
Data extraction was conducted using a pre-piloted Microsoft Excel® spreadsheet. Extracted data included authors, year of publication, title, journal, country, study aim, design, professions of participants, number of participants (response rate), setting, method, any theory used, data collection tool development and validation, key findings, stated study strengths and weaknesses, and conclusion. As with the screening phase, data extraction was performed by two independent reviewers, with disagreements resolved by a third reviewer. Data synthesis was then conducted using a narrative approach to identify key themes and patterns in the data related to the review aim. Similarly, each article was reviewed by two independent reviewers to identify the key patterns and themes during data synthesis. However, five reviewers were involved in the process, with one reviewer reviewing all articles and the other four equally reviewing all articles. Disagreements were resolved with mutual discussion. Data was coded manually by each independent reviewer.
3 Results
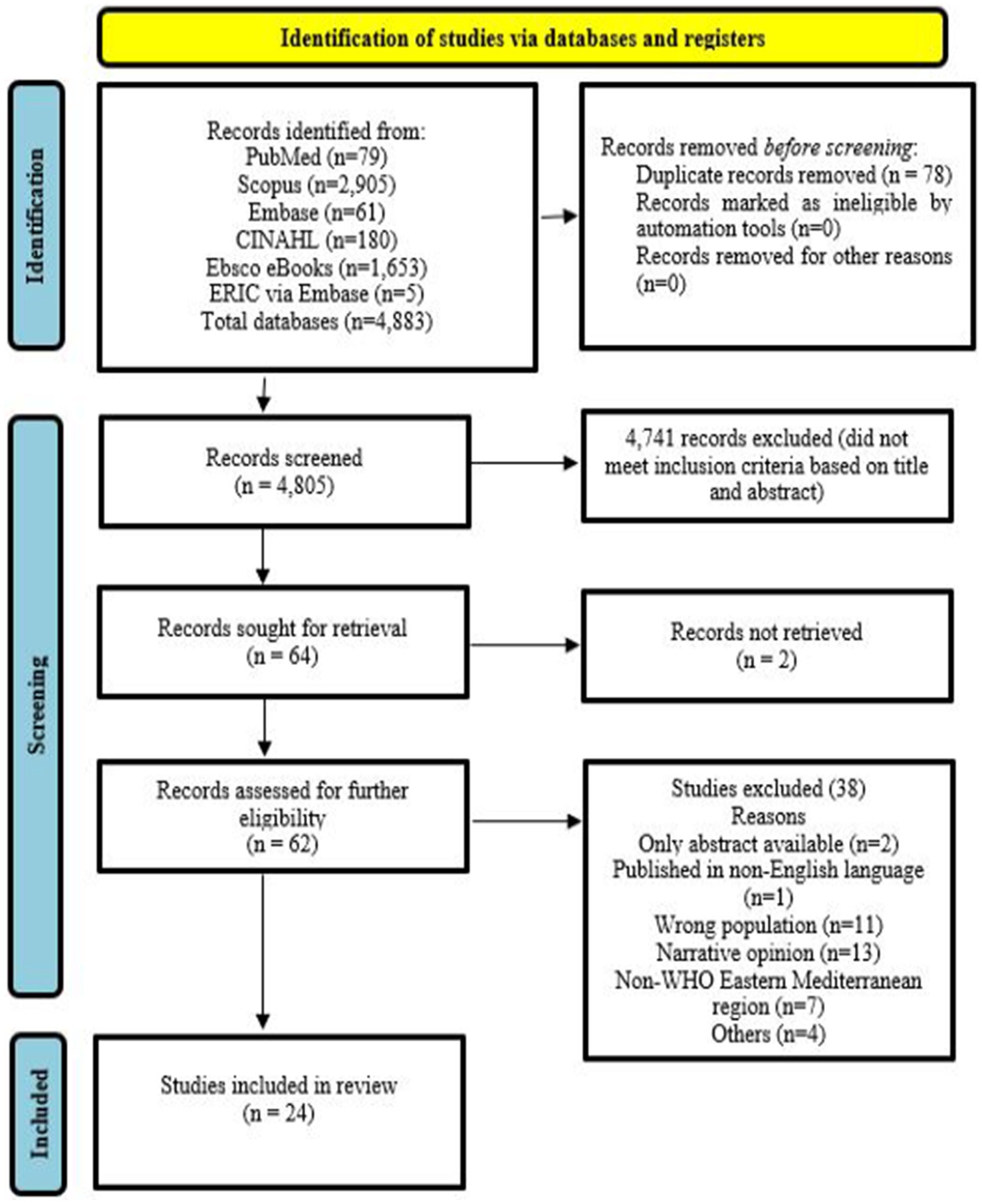
The search yielded 4,883 articles, of which 4,805 remained after removing duplicates. Dar Almandumah (Arabic database) produced no results. Title and abstract screening reduced the number to 64, with 24 retained for data extraction and mapping (Figure 1).
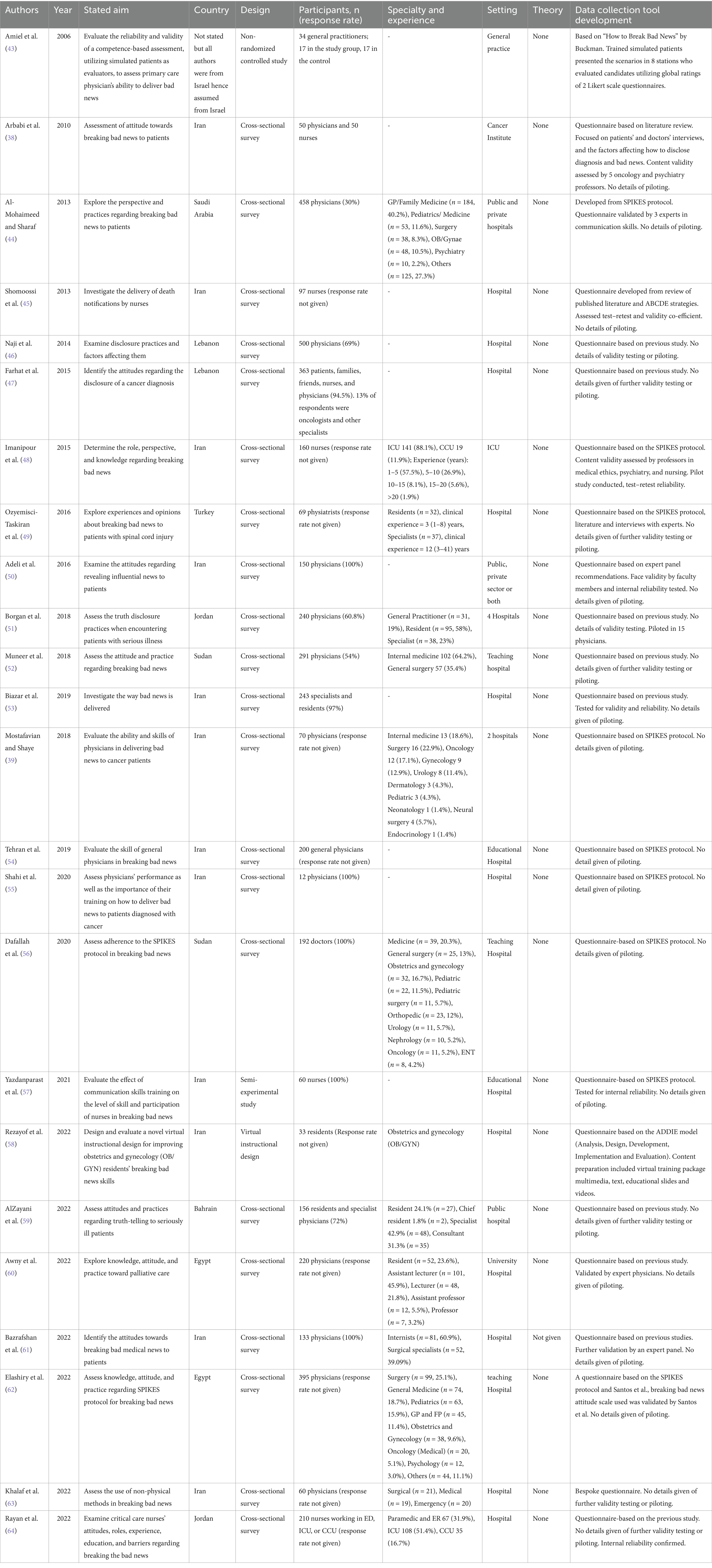
Study characteristics including aims, countries, study designs, participants, setting, use of theory, and data collection tool development are provided in Table 1.
Half of the studies were conducted in Iran (n = 12), with 2 studies each from Lebanon, Jordan, Egypt, and Sudan, and one each from Saudi Arabia, Bahrain, and Turkey (N.B. one study did not specify the region). Most studies (n = 21) were cross-sectional, with one non-randomized controlled study, one semi-experimental study, and one adopting a virtual instructional design. There were no qualitative studies exploring the phenomenon in-depth or using theoretical frameworks. Study participants included physicians (15 studies), nurses (4), physicians and nurses (2), physicians and residents (2), and residents only (1). Study settings spanned private/public hospitals and medical centers, private/public university hospitals, cancer centers, and intensive care departments.
A total of 4,710 participants were included in the 24 studies, with the largest study reporting data from 500 participants (a cross-sectional survey of physicians, with a response rate of 69%). The smallest study had only 12 participants (100% response rate). Cross-sectional survey studies reported response rates ranging from 30 to 100%. Nine studies employed the SPIKES protocol in questionnaire development, while another nine adopted questionnaires from previously published studies. In the remaining cross-sectional studies, little detail was provided on questionnaire development. No study reported the use of any theory in the development of data collection tools or data analysis and interpretation. Similarly, few studies provided details on questionnaire piloting prior to usage.
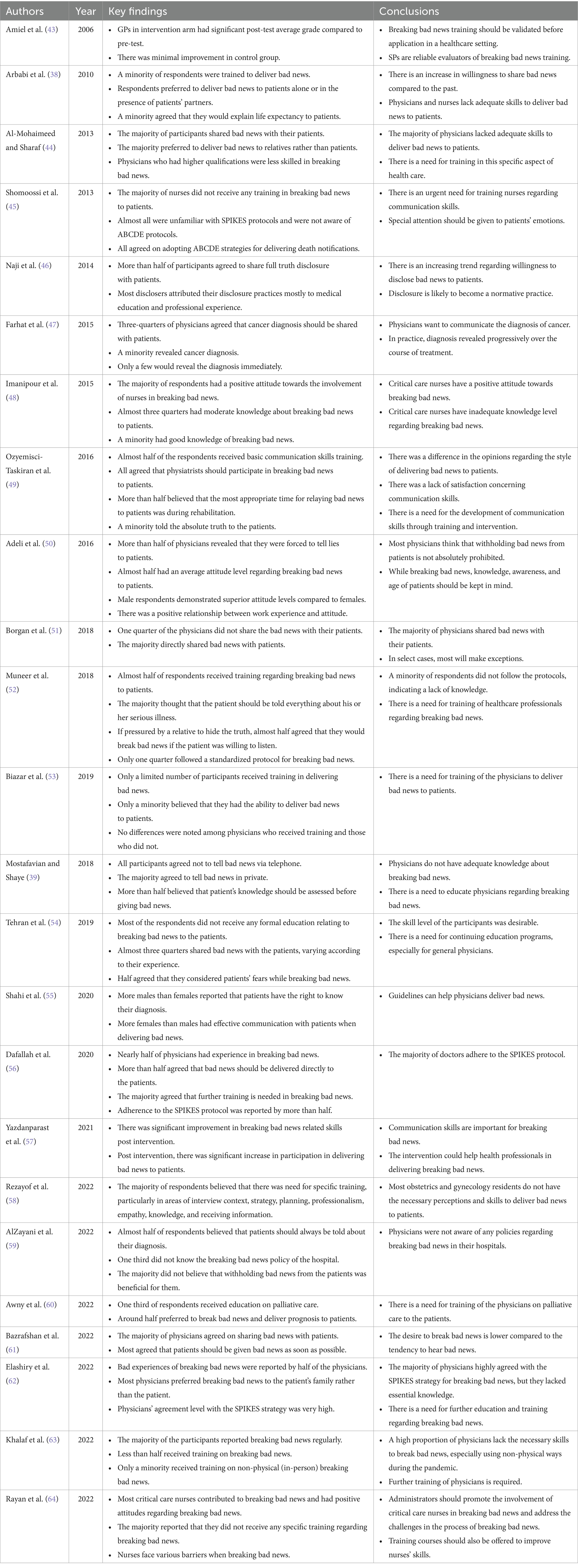
The key findings and conclusions derived from each study are given in Table 2. The most common findings were willingness to share bad news, inadequate training for breaking bad news, lack of formal education, experiences varying with participant demographics, and lack of awareness and adherence to SPIKES and ABCDE protocols.
Mapping identified themes of
i. Positive views and experiences
ii. Negative views and experiences
iii. Practice variation with demographics and experience
iv. Need for education or further training
Table 3 provides the synthesis relating to the mapping of each study to these themes, which are described in further detail.

Table 3. Synthesis mapping of key study findings, identifying positive and negative views and experience.
3.1 Positive views and experience
There were five themes of positive views and experiences: perceived adequate knowledge/skills, positive attitude towards breaking bad news, having received training, awareness of accepted approaches (e.g., SPIKES/ABCDE), and adherence to accepted approaches.
3.1.1 Perceived adequate knowledge/skills
Of the 24 studies reviewed, five reported positive aspects regarding perceived knowledge and skills being adequate. These studies were all cross-sectional, with the participants in three studies being nurses and in two being physicians. Naji et al. (46) reported an association between higher perceived knowledge/skills and younger physicians with a high number of weekly practice hours.
3.1.2 Positive attitude towards breaking bad news
Most studies (n = 14) reported participants’ positive attitudes regarding breaking bad news. Thirteen studies were cross-sectional, and one reported the development of a virtual instructional medium. Six of the studies included physicians, three included nurses, two each included physicians/nurses and physicians/residents, and one with residents only. Arbabi et al. (38) found an association between older age and experience and positive attitudes towards breaking bad news.
3.1.3 Received training
Four studies reported that participants had received formal training in breaking bad news. Two had a cross-sectional design, one a semi-experimental study, and one a non-randomized controlled study design. All studies involved physicians, with one also including nurses. The percentage of participants receiving training on breaking bad news ranged from 15.9 to 50.9%.
3.1.4 Awareness of accepted approaches (e.g., SPIKES/ABCDE)
Only one cross-sectional study of physicians explicitly reported that participants were aware of SPIKES/ABCDE approaches. In this study, Elashiry et al. (62) reported that 10% were aware of the SPIKES protocol. Dafallah et al. (56) and Muneer et al. (52) reported adherence to SPIKES/ABCDE protocols but did not assess the level of awareness among their participants.
3.1.5 Adherence to accepted approaches
Three studies reported that participants adhered to accepted protocols while breaking bad news. All were cross-sectional studies of physicians. Elashiry et al. (62) reported that 91.8% of physicians agreed with the SPIKES protocol. They further noted that adherence level was significantly higher among male participants and those who received training about breaking bad news. Dafallah et al. (56) reported adherence to the SPIKES protocol ranging from 35 to 79%. According to Muneer et al. (52), only 55.6% of participants followed the SPIKES protocol, with others following BREAKS (Background, Rapport, Explore, Announce, Kindling, Summarise; 25%) and ABCDE (11.1%).
3.2 Negative views and experiences
There were five themes of negative views and experiences: reported lack of training, unawareness of accepted approaches, lack of full disclosure to patients, unawareness of institutional policy, and practice variation with demographics and experience.
3.2.1 Reported lack of training
In nine studies, the respondents explicitly reported a lack of training in delivering bad news. These studies were largely cross-sectional, with five studies including physicians, two including physicians/residents, one including nurses, and one including both physicians and nurses. The remaining studies did not report any aspect of training.
3.2.2 Unaware of accepted approaches
One study reported that participants were unaware of the accepted approaches for breaking bad news. This cross-sectional study on nurses by Shomoossi et al. (45) reported that almost all participants were unaware of SPIKES and ABCDE protocols.
3.2.3 Lack of full disclosure to patients
Nine studies reported that participants did not disclose bad news in full. These cross-sectional studies were largely of physicians, with one study including nurses. Arbabi et al. (38) reported that a minority of physicians always discussed patients’ diagnoses, compared to two-thirds of nurses. Moreover, nurses mostly communicated with families rather than patients. Similarly, Al-Mohaimeed and Sharaf (44) reported that almost three-quarters of respondents delivered bad news to relatives rather than patients. Farhat et al. (47), also reported that a minority of physicians broke bad news to their patients. Only one-fifth of the respondents in a study by Ozyemisci-Taskiran et al. (49) told the “absolute truth” to patients, while the remainder conveyed a “partial truth”. Borgan et al. (51), and Muneer et al. (52) reported that most physicians complied with family requests for non-disclosure of bad news to patients. According to Elashiry et al. (62), most physicians preferred discussing bad news with family members rather than directly with patients.
3.2.4 Unaware of institutional policy
In a cross-sectional study, AlZayani et al. (59) reported that one-third of physicians and residents were not aware of the institutional policy on breaking bad news.
3.3 Practice variation with demographic characteristics
Five cross-sectional studies of physicians reported that breaking bad news practice varied based on participant characteristics and experience. For example, Al-Mohaimeed and Sharaf (44) demonstrated that primary healthcare physicians were more open when breaking bad news to patients. Naji et al. (46) reported that those who disclosed bad news were more involved in medical teaching compared to non-disclosers Tehran et al. (54) reported significant differences in practices among different age groups.
3.4 Need for education/training
Most studies (n = 17) emphasized the need for education and training in breaking bad news. Of these, 10 studies involved physicians, four involved nurses, two involved physicians/residents/nurses, and one involved residents only. Most studies (n = 15) were cross-sectional, with two being semi-experimental with a virtual instructional design.
4 Discussion
4.1 Key findings
Twenty-four studies were identified in this scoping review of the peer-reviewed literature on health professionals’ views and experiences of breaking bad news in the WHO Eastern Mediterranean region. The Dar Almandumah (Arabic database) reported no results. Half of these studies were from Iran and were cross-sectional, with no studies reporting the use of theory. Most studies included physicians with very few reporting data from nurses and none from other health professionals. Mapping of study results generated four major themes: positive views and experiences (perceived adequate knowledge/skills, positive attitude towards breaking bad news, received training, awareness of accepted approaches (e.g., SPIKES/ABCDE), adherence to accepted approaches); negative views and experiences (reported lack of training, unaware of accepted approaches, lack of full disclosure to patients, unaware of institutional policy); practice varying with demographics and experience; and the need for education/training.
4.2 Strengths and weaknesses
The JBI method for scoping reviews was adhered to throughout, and the review was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses extension (PRISMA-ScR). Despite searching in an Arabic database, all the papers included in the review were in English language. There was only one non-English study (Persian), which was excluded after screening. Despite a robust approach to the conduct and reporting of the review itself, the findings and conclusions are limited by the absence of qualitative studies and the absence of theory in data collection and analysis. Most studies provided limited details of the development of questionnaire domains and items. Response rates were also variable, with several studies not quantifying the response rate.
4.3 Interpretation
The findings of this scoping review align with existing literature on breaking bad news, emphasizing the global challenge of health professionals in effectively communicating bad news. Given that this is a key competency of clinical practice, it is evident that health professionals need appropriate education and training to develop and master this skill. Breaking bad news can have adverse consequences for patients and their families (7–10), and negatively impact those delivering the news (4, 11–16), underscoring the need for targeted education geared towards honing and enhancing these skills. Perhaps the most significant finding of this scoping review is healthcare providers’ articulation of the expressed need for specific training in this area. Of note were the reports of the absence of training, and a lack of awareness of accepted approaches and institutional policies pertaining to breaking bad news in this region. While several of these themes (i.e., perceived adequate knowledge and skills, having received training, awareness, and adherence to accepted protocols) were described as positive findings, they were only reported in a minority of studies.
These findings resonate with literature from other parts of the world, which report issues related to training and accepted models of practice (65). In a meta-synthesis of 40 studies, Bousquet et al. attributed the difficulty in breaking bad news to a lack of physician training (16). A similar finding was reported by Sharif et al. in an evidence synthesis of 14 studies of health professionals’ training in breaking bad news (14). There is convincing evidence that links training in breaking bad news to improvements in practice. A scoping review by Chow et al. reported that physicians who received training were more likely to experience personal accomplishment and less likely to feel emotional exhaustion and depersonalization (11). Similarly, a meta-analysis of 17 studies identified that training interventions were associated with large, significant improvements in observer-rated news delivery skills (17).
Despite the issues identified in the scoping review relating to specific aspects of training, the participants in most studies reported positive attitudes towards breaking bad news and accepted this as an important task. It is, therefore, of particular interest that many studies highlighted negative aspects in terms of the lack of full disclosure of bad news. In nine studies, the participants reported partial disclosure to patients or opted to discuss bad news with the families rather than patients themselves. While involving family members in the coping mechanism for patients receiving bad news is acknowledged (16), the findings of lack of full disclosure may reflect the cultural and religious context of the Eastern Mediterranean region. Unlike the Western emphasis on individualism, patient autonomy, full diagnosis disclosure, and litigiousness (27), there is a propensity within this region to conceal bad news in an effort to protect patients’ morale (66). Therefore, in some cases, cultural influences can take precedence over professional considerations. This can be the reason why in some studies physicians were willing to share the bad news with relatives rather than the patients (44). Another important aspect to consider in the Eastern Mediterranean region is the strong bonds between families and the patriarchic nature of families, with elders making the majority of the decisions without much consideration for an individual’s rights. This can significantly influence how bad news is delivered. Another aspect of this relationship is shared by Borgan et al. (51) who report that bad news carries a sense of dread and family, in a way, feels obligated to insulate the patient from such news. The discrepancy regarding gender roles in breaking bad news as reported by Elashiry et al. (62) can be explained by the fact that female doctors may avoid breaking bad news due to the fear of being harmed, while male doctors may be more respected in the community and thus are more courageous while breaking bad news. Due to these reasons, some authors advocate the use of the culture-based protocol for breaking bad news in each area, with physicians following their local guidelines (53).
There was a noticeable lack of the application of theory in all studies. The inclusion of theory (e.g., behavioral) in the development of data collection tools, data analysis, and interpretation enhances research robustness and rigor. Importantly, the use of behavioral theory allows consideration of all possible influences on and explanations for behavior and informs the design of effective interventions. The lack of theory in the studies may be one reason that few studies reported issues of negative impact on health professionals’ emotions, fatigue and burnout which have been reported in other related reviews (12, 13).
The studies captured were largely cross-sectional, which, while appropriate for quantifying views and experiences, lack the depth of data generated via qualitative research. It is also noticeable that half of the studies were from Iran with no uniform representation of the WHO Eastern Mediterranean region. Most studies reported the perspectives of physicians, with fewer nurses and none from other health professions. Given the multidisciplinary nature of healthcare and the increasingly clinical role of other health professionals, it is likely that the delivery of bad news may no longer be solely within the domain of physicians. Training and practice of other health professionals warrants further investigation.
The incorporation of structured training on this topic in health profession graduate programs globally is becoming increasingly recognized as essential to preparing the future workforce. For instance, in India, the AETCOM (Attitude, Ethics, and Communication) module is a comprehensive curriculum initiative aimed at enhancing medical students’ competencies in these areas (67). Similarly, in various other countries, there has been an increased emphasis on communication training in medical education (68, 69). For example, in Qatar, Hamad Medical Corporation has become mandatory for residents to complete their training (70). However, there is still a need for continuing education and training for breaking bad news.
4.4 Further research
Qualitative methods should be employed in future research to provide a deeper understanding of health professionals’ views and experiences when breaking bad news. Such qualitative studies should be designed with an underpinning theoretical framework and with greater consideration of the cultural factors influencing communication practices. There is also merit in conducting research that focuses on the development, implementation, and evaluation of novel approaches to health professional education and training in breaking bad news.
5 Conclusion
This scoping review provides a comprehensive mapping of existing literature on health professionals’ views and experiences of breaking bad news in the Eastern Mediterranean region. The findings revealed both positive and negative aspects while highlighting persistent challenges, with emphasis on the need for targeted education and training programs and the development of culturally sensitive communication protocols. Further research, particularly using qualitative methodologies, is warranted.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
AY: Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Resources, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. DS: Conceptualization, Formal analysis, Methodology, Project administration, Resources, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. TK: Writing – original draft, Writing – review & editing. ASo: Writing – original draft, Writing – review & editing, Data curation, Methodology. AA-K: Writing – original draft, Writing – review & editing. ASe: Conceptualization, Formal analysis, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, Data curation, Investigation.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The APC for this manuscript was covered by the Health Sector at Qatar University.
Conflict of interest
AY and AA-K were employed by Hamad Medical Corporation.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2024.1440867/full#supplementary-material
References
1. Fallowfield, L, and Jenkins, V. Communicating sad, bad, and difficult news in medicine. Lancet. (2004) 363:312–9. doi: 10.1016/S0140-6736(03)15392-5
2. Mirza, RD, Ren, M, Agarwal, A, and Guyatt, GH. Assessing patient perspectives on receiving bad news: a survey of 1337 patients with life-changing diagnoses. AJOB Emp Bioethics. (2019) 10:36–43. doi: 10.1080/23294515.2018.1543218
3. Paul, C, Clinton-McHarg, T, Sanson-Fisher, R, Douglas, H, and Webb, G. Are we there yet? The state of the evidence base for guidelines on breaking bad news to cancer patients. Eur J Cancer. (2009) 45:2960–6. doi: 10.1016/j.ejca.2009.08.013
4. Garnett, A, Hui, L, Oleynikov, C, and Boamah, S. Compassion fatigue in healthcare providers: a scoping review. BMC Health Serv Res. (2023) 23:1336. doi: 10.1186/s12913-023-10356-3
5. Ptacek, JT, and Eberhardt, TL. Breaking bad news. Rev Lit Jama. (1996) 276:496–502. doi: 10.1001/jama.1996.03540060072041
6. Choe, EK, Duarte, ME, Suh, H, Pratt, W, and Kientz, JA. Communicating bad news: insights for the Design of Consumer Health Technologies. JMIR Hum Factors. (2019) 6:e8885. doi: 10.2196/humanfactors.8885
7. Almansour, I, and Abdel Razeq, NM. Communicating prognostic information and hope to families of dying patients in intensive care units: a descriptive qualitative study. J Clin Nurs. (2021) 30:861–73. doi: 10.1111/jocn.15630
8. Beyraghi, N, Mottaghipour, Y, Mehraban, A, Eslamian, E, and Esfahani, F. Disclosure of Cancer information in Iran: a perspective of patients, family members, and health professionals. Iran J Cancer Prev. (2011) 4:130–4.
9. Anderson, B. Reflecting on the communication process in health care. Part 1: clinical practice—breaking bad news. Br J Nurs. (2019) 28:858–63. doi: 10.12968/bjon.2019.28.13.858
10. Kaplan, A, and Price, D. Treatment adherence in adolescents with asthma. J Asthma Allergy. (2020) 13:39–49. doi: 10.2147/JAA.S233268
11. Chow, E, and DBioethics, BH. The impact of breaking bad news on oncologist burnout and how communication skills can help: a scoping review. J Pain Manag. (2017) 10:89–97.
12. Francis, L, and Robertson, N. Healthcare practitioners’ experiences of breaking bad news: a critical interpretative meta synthesis. Patient Educ Couns. (2023) 107:107574. doi: 10.1016/j.pec.2022.107574
13. de Freitas Domingues, MJ. (2016). Psychological burden on physicians delivering bad news. University of Porto.
14. Sharif, N, Ibrahim, N, Don, Z, and Nur'ain, BH. Current research trends and research themes of breaking bad news: a systematic review. Educ Med J. (2023) 15:1–19. doi: 10.21315/eimj2023.15.4.1
15. Maguire, P, Faulkner, A, Booth, K, Elliott, C, and Hillier, V. Helping cancer patients disclose their concerns. Eur J Cancer. (1996) 32:78–81. doi: 10.1016/0959-8049(95)00527-7
16. Bousquet, G, Orri, M, Winterman, S, Brugière, C, Verneuil, L, and Revah-Levy, A. Breaking bad news in oncology: a Metasynthesis. J Clin Oncol. (2015) 33:2437–43. doi: 10.1200/JCO.2014.59.6759
17. Johnson, J, and Panagioti, M. Interventions to improve the breaking of bad or difficult news by physicians, medical students, and interns/residents: a systematic review and Meta-analysis. Acad Med. (2018) 93:1400–12. doi: 10.1097/ACM.0000000000002308
18. Narayanan, V, Bista, B, and Koshy, C. 'BREAKS' protocol for breaking bad news. Indian J Palliat Care. (2010) 16:61–5. doi: 10.4103/0973-1075.68401
19. Ochs, M, Mestre, D, De Montcheuil, G, Pergandi, J-M, Saubesty, J, Lombardo, E, et al. Training doctors’ social skills to break bad news: evaluation of the impact of virtual environment displays on the sense of presence. J Multimodal User Interfaces. (2019) 13:41–51. doi: 10.1007/s12193-018-0289-8
20. Ferraz Gonçalves, JA, Almeida, C, Amorim, J, Baltasar, R, Batista, J, Borrero, Y, et al. Family physicians' opinions on and difficulties with breaking bad news. Porto Biomed J. (2017) 2:277–81. doi: 10.1016/j.pbj.2017.04.004
21. Yi, J, Kim, MA, Choi, KH, and Bradbury, L. Oncologists’ experience of delivering bad news in Korea. OMEGA-J Death Dying. (2022) 85:285–302. doi: 10.1177/0030222820944087
22. Baile, WF, Buckman, R, Lenzi, R, Glober, G, Beale, EA, and Kudelka, AP. SPIKES-A six-step protocol for delivering bad news: application to the patient with cancer. Oncologist. (2000) 5:302–11. doi: 10.1634/theoncologist.5-4-302
23. Rabow, MW, and McPhee, SJ. Beyond breaking bad news: how to help patients who suffer. West J Med. (1999) 171:260–3.
24. Monden, KR, Gentry, L, and Cox, TR. Delivering bad news to patients. Proc (Baylor Univ Med Cent). (2016) 29:101–2. doi: 10.1080/08998280.2016.11929380
25. Mahendiran, M, Yeung, H, Rossi, S, Khosravani, H, and Perri, G-A. Evaluating the effectiveness of the SPIKES model to break bad news – a systematic review. Am J Hosp Palliat Med. (2023) 40:1231–60. doi: 10.1177/10499091221146296
26. Jalali, R, Jalali, A, and Jalilian, M. Breaking bad news in medical services: a comprehensive systematic review. Heliyon. (2023) 9:e14734. doi: 10.1016/j.heliyon.2023.e14734
27. Zhang, H, Zhang, H, Zhang, Z, and Wang, Y. Patient privacy and autonomy: a comparative analysis of cases of ethical dilemmas in China and the United States. BMC Med Ethics. (2021) 22:8. doi: 10.1186/s12910-021-00579-6
28. Block, KI, Bugno, TJ, Collichio, FA, Geffen, J, and Schapira, L. Breaking bad news. Integr Cancer Ther. (2003) 2:39–62. doi: 10.1177/1534735403251273
29. Holmes, SN, and Illing, J. Breaking bad news: tackling cultural dilemmas. BMJ Support Palliat Care. (2021) 11:128–32. doi: 10.1136/bmjspcare-2020-002700
30. Ong, WY, Yee, CM, and Lee, A. Ethical dilemmas in the care of cancer patients near the end of life. Singapore Med J. (2012) 53:11–6.
31. Claramita, M, Nugraheni, MD, van Dalen, J, and van der Vleuten, C. Doctor–patient communication in Southeast Asia: a different culture? Adv Health Sci Educ. (2013) 18:15–31. doi: 10.1007/s10459-012-9352-5
32. Holmes, S, Finch, W, Gilhespy, A, and Christopher, C. Cultural variation in attitudes to collusion in end of life care: A survey of medical students in Malaysia and the UK. Annual Scientific Meeting of Association for the Study of Medical Education: Newcastle, UK (2018).
34. Cave, E. The ill-informed: consent to medical treatment and the therapeutic exception. Common Law World Rev. (2017) 46:140–68. doi: 10.1177/1473779517709452
35. WHO (2023). World health organization (WHO) Eastern Mediterranean region. Available at: https://www.emro.who.int/countries.html (Accessed November 2023).
36. Rodriguez Del Pozo, P, Fins, JJ, Helmy, I, El Chaki, R, El Shazly, T, Wafaradi, D, et al. Truth-telling and cancer diagnoses: physician attitudes and practices in Qatar. Oncologist. (2012) 17:1469–74. doi: 10.1634/theoncologist.2012-0128
37. Khalil, RB. Attitudes, beliefs and perceptions regarding truth disclosure of cancer-related information in the Middle East: a review. Palliat Support Care. (2013) 11:69–78. doi: 10.1017/S1478951512000107
38. Arbabi, M, Roozdar, A, Taher, M, Shirzad, S, Arjmand, M, Mohammadi, MR, et al. How to break bad news: physicians' and nurses' attitudes. Iran J Psychiatry. (2010) 5:128–33.
39. Mostafavian, Z, and Shaye, ZA. Evaluation of physicians' skills in breaking bad news to cancer patients. J Family Med Prim Care. (2018) 7:601–5. doi: 10.4103/jfmpc.jfmpc_25_18
40. Peters, MDJ, Marnie, C, Tricco, AC, Pollock, D, Munn, Z, Alexander, L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. (2020) 18:2119–26. doi: 10.11124/JBIES-20-00167
41. Moher, D, Shamseer, L, Clarke, M, Ghersi, D, Liberati, A, Petticrew, M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. (2015) 4:1–9. doi: 10.1186/2046-4053-4-1
42. Ouzzani, M, Hammady, H, Fedorowicz, Z, and Elmagarmid, A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. (2016) 5:1–10. doi: 10.1186/s13643-016-0384-4
43. Amiel, GE, Ungar, L, Alperin, M, Baharier, Z, Cohen, R, and Reis, S. Ability of primary care physician's to break bad news: a performance based assessment of an educational intervention. Patient Educ Couns. (2006) 60:10–5. doi: 10.1016/j.pec.2005.04.013
44. Al-Mohaimeed, AA, and Sharaf, FK. Breaking bad news issues: a survey among physicians. Oman Med J. (2013) 28:20–5. doi: 10.5001/omj.2013.05
45. Shomoossi, N, Rad, M, Kooshan, M, and Ganjloo, J. Nurses as death notifiers: a report from nurses in Iran. Life Sci J. (2013) 10:26–31.
46. Naji, F, Hamadeh, G, Hlais, S, and Adib, S. Truth disclosure to Cancer patients: shifting attitudes and practices of Lebanese physicians. AJOB Emp Bioethics. (2014) 6:41–9. doi: 10.1080/23294515.2014.996265
47. Farhat, F, Othman, A, El Baba, G, and Kattan, J. Revealing a cancer diagnosis to patients: attitudes of patients, families, friends, nurses, and physicians in Lebanon-results of a cross-sectional study. Curr Oncol. (2015) 22:e264–72. doi: 10.3747/co.22.2351
48. Imanipour, M, Karim, Z, and Bahrani, N. Role, perspective and knowledge of Iranian critical care nurses about breaking bad news. Aust Crit Care. (2016) 29:77–82. doi: 10.1016/j.aucc.2015.07.003
49. Ozyemisci-Taskiran, O, Budakoglu, II, Coskun, O, and Demirsoy, N. Breaking bad news to patients with spinal cord injury in Turkey - physiatrists' perspective. J Spinal Cord Med. (2017) 40:423–31. doi: 10.1080/10790268.2016.1234735
50. Adeli, H, Aghaali, M, and Hashemi, M. An investigation of physicians’ attitudes to disclosure of bad news to patients in the City of Qom. Health Spirit Med Ethics. (2016) 3:25–9.
51. Borgan, SM, Amarin, JZ, Othman, AK, Suradi, HH, and Qwaider, YZ. Truth disclosure practices of physicians in Jordan. J Bioeth Inq. (2018) 15:81–7. doi: 10.1007/s11673-018-9837-x
52. Muneer, MS, Elhassan, AE, Osman, AM, Abdalla, AA, Abdelrahim, MA, Ali, SM, et al. Breaking bad news from the doctors' perspective in a paternalistic society: the case of Sudan. Trop Dr. (2018) 48:340–4. doi: 10.1177/0049475518795765
53. Biazar, G, Delpasand, K, Farzi, F, Sedighinejad, A, Mirmansouri, A, and Atrkarroushan, Z. Breaking bad news: a valid concern among clinicians. Iran J Psychiatry. (2019) 14:198–202. doi: 10.18502/ijps.v14i3.1321
54. Ahmari Tehran, H, Shirazi, M, Kachoie, A, and Khalajinia, Z. Evaluation of general physicians’ skills in breaking bad news to the patient based on the SPIKES questionnaire in Qom, 2016. Elect J General Med. (2018) 16:em103. doi: 10.29333/ejgm/102415
55. Shahi, F, Emami, A, Shirazi, M, Mokhtari, S, Moghimi, M, Gohari, S, et al. Assessing physicians’ performance when telling the truth to patients diagnosed with Cancer. J Adv Med Biomed Res. (2021) 29:68–73. doi: 10.30699/jambs.29.133.68
56. Dafallah, MA, Ragab, EA, Salih, MH, Osman, WN, Mohammed, RO, Osman, M, et al. Breaking bad news: awareness and practice among Sudanese doctors. AIMS Public Health. (2020) 7:758–68. doi: 10.3934/publichealth.2020058
57. Yazdanparast, E, Arasteh, A, Ghorbani, S, and Davoudi, M. The effectiveness of communication skills training on nurses' skills and participation in the breaking bad news. Iran J Nurs Midwifery Res. (2021) 26:337–41. doi: 10.4103/ijnmr.IJNMR_150_20
58. Rezayof, E, Akhavan, S, Afshar, L, Ghaemi, M, Sahebi, L, and Akbari, FS. A virtual instructional design improved breaking bad news in obstetrics and gynecology residents. J Family Reprod Health. (2022) 16:282–9. doi: 10.18502/jfrh.v16i4.11359
59. AlZayani, A, Jassim, G, Bakhiet, B, and Nurdin, H. Attitudes and practices of physicians towards truth-telling to patients. Ethics Med Public Health. (2022) 20:100737. doi: 10.1016/j.jemep.2021.100737
60. Awny, MM, Al-Touny, SA, and Gaafar, SEM. Physicians' knowledge, attitude and practice toward ethical and medical issues of palliative Care in Suez Canal University Hospital. Indian J Palliat Care. (2022) 28:391–7. doi: 10.25259/IJPC_65_2021
61. Bazrafshan, A, Zendehbad, A, and Enjoo, SA. Delivering bad news to patients: survey of physicians, patients, and their family members’ attitudes. Shiraz E-Med J. (2022) 23:e109016. doi: 10.5812/semj.109016
62. Elashiry, A, Abdel Wahed, W, and Elhady, G. Assessing Physicians' knowledge, attitude, and practice towards breaking bad news: a multicenter study in Egypt. Egyp J Hosp Med. (2022) 89:6305–12. doi: 10.21608/ejhm.2022.268973
63. Khalaf, H, Almothafar, B, and Alhalabi, N. Breaking bad news during COVID-19 time in surgical, emergency and medical specialties-what more we need to develop? Mediev Archaeol. (2022) 76:131–4. doi: 10.5455/medarh.2022.76.131-134
64. Rayan, A, Hussni Al-Ghabeesh, S, and Qarallah, I. Critical care Nurses' attitudes, roles, and barriers regarding breaking bad news. SAGE Open Nurs. (2022) 8:237796082210899. doi: 10.1177/23779608221089999
65. Warrier, V, and Pradhan, A. A narrative review of interventions to teach medical students how to break bad news. Med Sci Educ. (2020) 30:1299–312. doi: 10.1007/s40670-020-01015-x
66. Basheikh, M. Preferences of the Saudi population in breaking bad medical news: a regional study. Cureus. (2021) 13:e19525. doi: 10.7759/cureus.19525
67. Shrivastava, SR, and Shrivastava, PS. Implementation of AETCOM module in Indian settings: points to ponder. Med J Babylon. (2021) 18:287–90. doi: 10.4103/MJBL.MJBL_42_21
68. Ramseier, CA, Hübschi, C, Crnić, T, and Woelber, JP. Implementation of a communication curriculum in undergraduate dental education—students' opinions during a 5-year development phase. Eur J Dent Educ. (2024) 28:227–35. doi: 10.1111/eje.12940
69. Kienle, R, Freytag, J, Lück, S, Eberz, P, Langenbeck, S, Sehy, V, et al. Communication skills training in undergraduate medical education at Charité-Universitätsmedizin Berlin. GMS J Med Educ. (2021) 38:Doc56. doi: 10.3205/zma001452
Keywords: truth disclosure, Qatar, Middle East, MENA, breaking bad news
Citation: Yousuf AAAA, Stewart DC, Kane T, Soltani A, Al-Khal A and Sethi A (2024) Health professionals’ views and experiences of breaking bad news in the Eastern Mediterranean Region: a scoping review. Front. Med. 11:1440867. doi: 10.3389/fmed.2024.1440867
Edited by:
Ciraj Ali Mohammed, National University of Science and Technology (Muscat), OmanReviewed by:
Gagan Bajaj, Kasturba Medical College, Mangalore, IndiaYousef Ahmed Fouad, Ain Shams University, Egypt
Copyright © 2024 Yousuf, Stewart, Kane, Soltani, Al-Khal and Sethi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ahsan Sethi, YXNldGhpQHF1LmVkdS5xYQ==
 Abdulla Ahmad A. A. Yousuf1,2
Abdulla Ahmad A. A. Yousuf1,2 Derek Charles Stewart
Derek Charles Stewart Abderrezzaq Soltani
Abderrezzaq Soltani Ahsan Sethi
Ahsan Sethi