- 1Department of Plastic Surgery, Changzheng Hospital, Second Military Medical University, Shanghai, China
- 2Department of Cardiothoracic Surgery, Changzheng Hospital, Second Military Medical University, Shanghai, China
Aim: This analysis evaluates the efficacy and safety of different flap techniques for Autologous Breast Reconstruction by collecting all clinical trials employing these methods and applying a Bayesian network meta-analysis.
Materials and methods: We systematically searched PubMed, Embase, and Web of Science for relevant literature, focusing on outcomes such as total flap loss, donor site wound dehiscence, secondary corrections at the donor site, psychosocial well-being, satisfaction with breasts, and sexual well-being.
Results: Our analysis included 10 clinical studies involving 871 patients across six flap techniques. In terms of total flap loss, the TUG flap showed the highest SUCRA value (89.6%), followed by the TMG flap (64.8%). For donor site wound dehiscence, the DIEP flap ranked highest with a SUCRA value of 60.1%, followed by the PAP flap (48.6%). In secondary corrections at the donor site, the PAP flap was the leader (95.5%), followed by the DIEP flap (52.5%) and the TMG flap (41.4%). For outcomes related to psychosocial well-being, satisfaction with breasts, and sexual well-being, the Four-flap technique consistently ranked highest (81.3, 85.0, and 88.4%, respectively).
Conclusion: Various flap techniques in Autologous Breast Reconstruction each present distinct benefits and risks. The Four-flap technique shows significant advantages in patient satisfaction, while the TUG flap excels in reducing total flap loss.
1 Introduction
Breast cancer is a common malignancy and the leading cause of cancer-related death among women worldwide (1). In 2023, breast cancer accounted for 12.4% of all cancer cases and 23.8% of all female cancers, with over 2.3 million new diagnoses and approximately 660,000 deaths, representing 6.9% of all cancer deaths and 15.4% of female cancer fatalities (1). According to the American Cancer Society, an estimated 310,720 new cases of invasive breast cancer in women will be diagnosed in the United States in 2024, and the rise in incidence rates have increased by 0.6% per year (2, 3).
Surgical treatment remains the primary modality for managing breast cancer, with mastectomy being the most common surgical procedure utilized clinically (3). Mastectomy significantly impacts the psychological health and social functioning of female patients, as changes in physical appearance after surgery often lead to various negative emotions (4). Research by Skrzypulec et al. (5) showed significant increases in depression and anxiety levels post-mastectomy. Breast reconstruction plays a crucial role in breast cancer treatment, aiding patients in regaining their physical image and self-esteem, thereby enhancing their quality of life.
Breast reconstruction is extremely important in the treatment of breast cancer, as it helps patients regain their physical image and self-esteem, thereby improving their quality of life (6). Autologous Breast Reconstruction, which uses the patient’s own tissues to create a new breast, is widely adopted. This method minimizes the risks associated with implants and provides a more natural appearance and feel. Current popular techniques for breast reconstruction include the Deep Inferior Epigastric Perforator (DIEP) flap, Profunda Artery Perforator (PAP) flap, muscle-sparing Transverse Rectus Abdominis Myocutaneous (TRAM) flap, Inferior Gluteal Artery Perforator (IGAP) flap, Transverse Myocutaneous Gracilis (TMG) flap, and the free Transverse Upper Gracilis (TUG) flap (7–10).
The DIEP flap is a reliable breast reconstruction technique commonly chosen by patients due to fewer complications at the donor site (11). However, absolute contraindications include prior abdominal surgery or liposuction, and smoking within 1 month before surgery (12). The PAP flap, considered an alternative to the DIEP flap, is better suited for patients with severe abdominal scarring, insufficient soft tissue volume, those who prefer to avoid a prominent abdominal scar, or those planning for pregnancy soon (10, 13). However, it is generally considered that donor site complications in the PAP flap are higher than in the DIEP flap.
Although these breast reconstruction techniques improve patient quality of life postoperatively, high-quality randomized controlled trials assessing postoperative outcomes like flap loss rate, donor site wound healing, psychological health, and patient satisfaction with surgical results are lacking (14). This study aims to evaluate the outcomes of all breast reconstruction techniques following mastectomy, indirectly comparing the efficacy and safety of treatment options based on a Bayesian framework, and determining the optimal breast reconstruction strategy through systematic review and meta-analysis.
2 Materials and methods
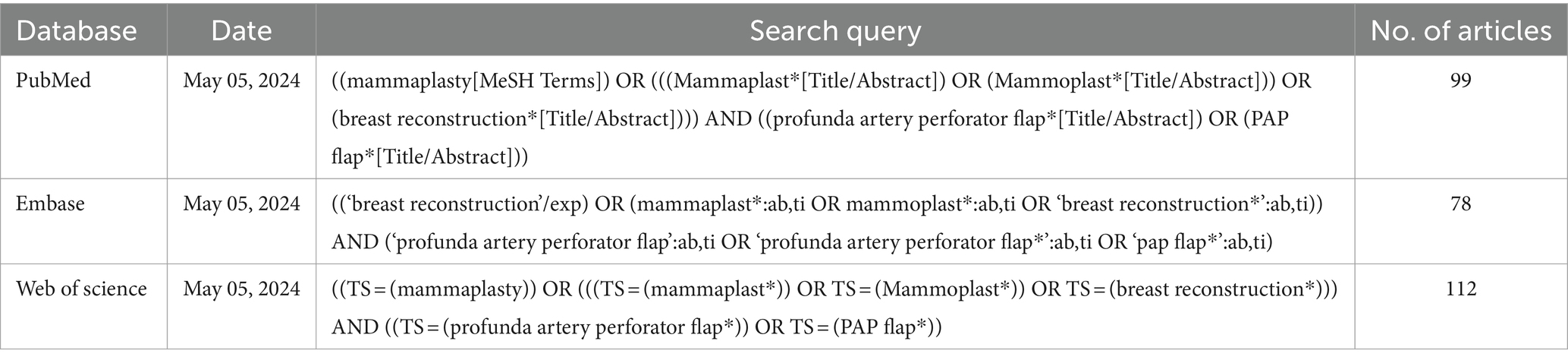
2.1 Literature search
A systematic review of literature was performed on May 05, 2024, following PRISMA guideline (15). English databases, including PubMed, Embase, and Web of science, were searched for articles. Our search strategy used the following Mesh terms and keywords: “mammaplasty,” “breast reconstruction,” “profunda artery perforator flap,” “PAP flap,” and “PAPF,” linked with Booleans operators (Table 1). Additionally, we performed manual searches by examining all references, exploring gray literature, and reviewing theses, government documents, letters, abstracts, minutes of meetings, and research reports to mitigate potential publication bias.
2.2 Selection criteria
Eligibility studies in our meta-analysis satisfied the following criteria: (1) Study design: clinical trials, including randomized controlled trial, cohort study, case–control study, or comparative study; (2) Patients: adults undergoing breast reconstruction; (3) Interventions and controls: different flaps; (4) Outcomes: measuring at least one of the following outcomes: total flap loss, donor site wound dehiscence, secondary corrections at the donor site, psychosocial well-being, satisfaction with breasts, and sexual well-being. Exclusion Criteria: (1) Trials based on the same group of patients at different times; (2) Trials that do not include the required outcome measures; (3) Reviews, case reports, or animal studies.
All included studies were double-checked by two reviewers to ensure that the data from the included trials were up-to-date.
2.3 Data extraction and quality assessment
Relevant articles retrieved from the database search were independently scrutinized by title and abstract by two investigators. Subsequently, data were independently collected using a standardized Excel data extraction sheet. In cases of disagreement, the article was reviewed by a third investigator, and a resolution was reached following a discussion among the three authors.
Demographic variables, primary outcomes, and secondary outcomes were recorded. Demographic variables included the authors, publication date, country of origin, mean body mass index (BMI), average flap weight, and pedicle length. Additionally, the required outcome measures were extracted.
For non-randomized trials, we employed the modified Newcastle-Ottawa Scale (NOS) to assess the methodological quality (16). This method comprised of three items to evaluate the quality of a non-RCT trial. The total score of this method was 9 points, and higher points indicated high quality. Studies with a score of more than 5 points were regarded as high quality.
2.4 Statistical analysis
Bayesian network meta-analysis was conducted using STATA 17. For dichotomous outcome measures, odds ratios (OR) and their 95% confidence intervals (95% CI) were calculated to estimate the pooled effect sizes. For continuous outcomes with non-uniform measurement units, the standardized mean difference (SMD) and its 95% CI were used to compute the pooled effect sizes, thereby eliminating bias caused by unit differences. Network graphs were drawn, and if a closed loop structure was present within the network, loop inconsistency tests were conducted to assess the consistency of the outcomes. If the p-value was greater than 0.05, indicating good consistency between direct and indirect evidence, a consistency model was used. Otherwise, sources of heterogeneity were explored through subgroup analysis and regression analysis. For open loop structures within the network graph, a consistency model was chosen. Subsequently, cumulative ranking curves (SUCRA) (17) were plotted to determine the best flap techniques in Autologous Breast Reconstruction. Lastly, comparison-adjusted funnel plots were utilized to detect publication bias and small-study effects.
3 Results
3.1 Literature search
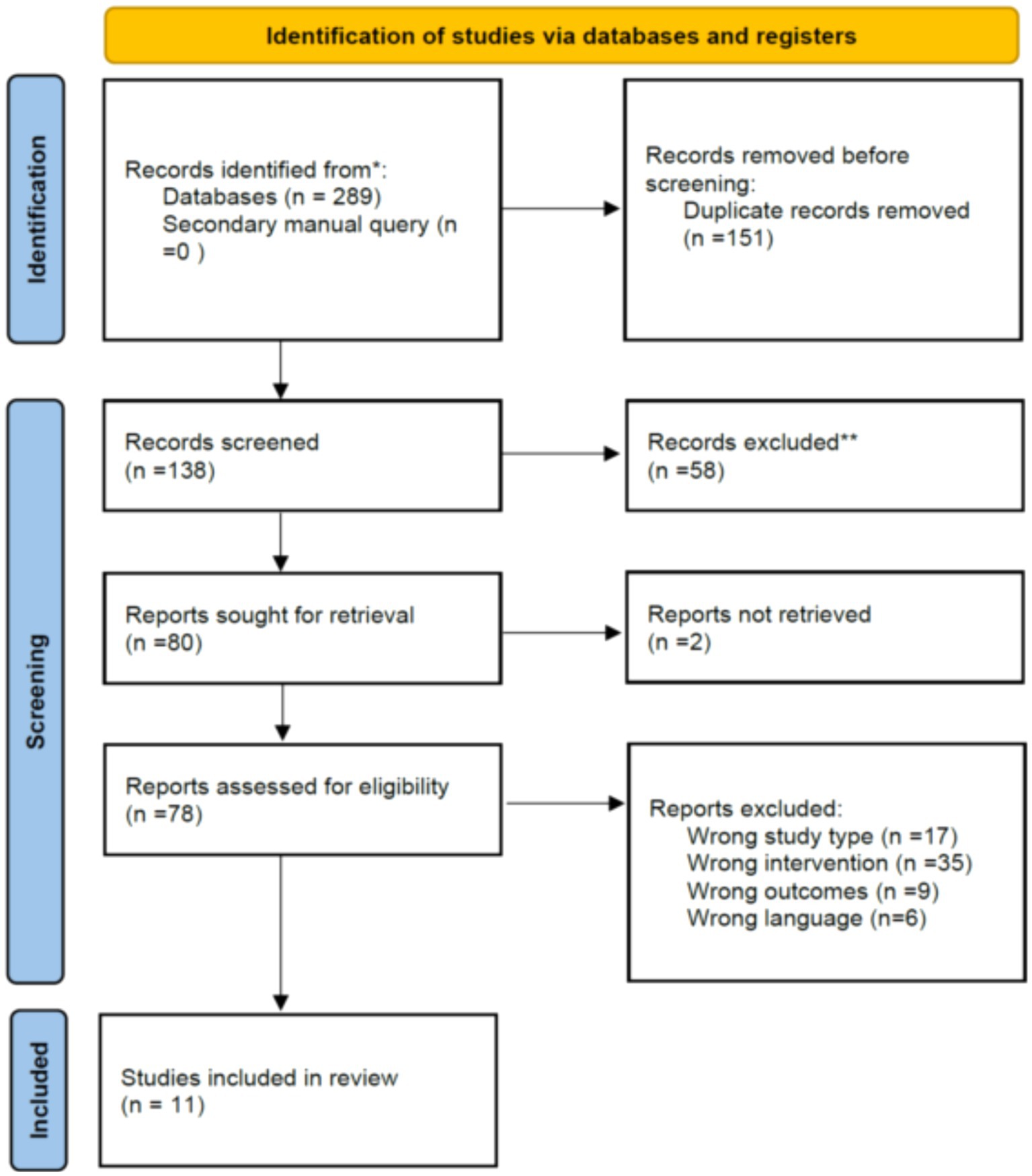
A total of 289 studies were identified through database searches. After removing 151 duplicate records, 138 studies remained for title and abstract review. Of these, 58 were excluded for various reasons. Subsequently, the remaining 78 studies were fully read for eligibility assessment, and then a total of 11 studies that fully met the inclusion criteria (10, 18–27) (Figure 1).
3.2 Clinical characteristics of included studies
Table 2 provides summaries of the key features of the studies included in the meta-analysis. Across these 11 studies, a total of 871 patients were enrolled, each undergoing one of six different flap techniques: PAP flap, DIEP flap, TMG flap, IGAP flap, Four-flap, and TUG flap. Two of the studies were conducted in the United States, United Kingdom, Austria, and Korea, respectively, while two additional studies were conducted in Germany and China, respectively. The mean age of patients using PAP flaps ranged from 39.1 to 51.4 years, compared to 41.3 to 51.5 years for those using other flaps. The mean BMI for patients using PAP flaps ranged from 20.6 to 25 kg/m2, whereas for those using other flaps, it ranged from 19.6 to 40 kg/m2.
3.3 Literature quality assessment
The methodological assessment for cohort studies showed that, the NOS score in each study was greater than 5 points, indicating that they were of high quality (Table 2).
3.4 Network evidence graph
The network evidence graph presented by the network meta-analysis consists of nodes, each representing a different intervention. The size of a node corresponds to the sample size of the intervention, with larger nodes indicating larger sample sizes. Lines between the nodes represent direct comparisons between interventions, with the thickness of the lines reflecting the number of direct comparison studies. Thicker lines indicate more evidence from direct comparisons, whereas thinner lines suggest fewer studies. The absence of a line between two nodes indicates that there are no direct comparisons between those interventions, necessitating the use of network meta-analysis to derive indirect evidence. A network comparison diagram showing the relationships between studies for six different outcome measures can be seen in Figure 2.
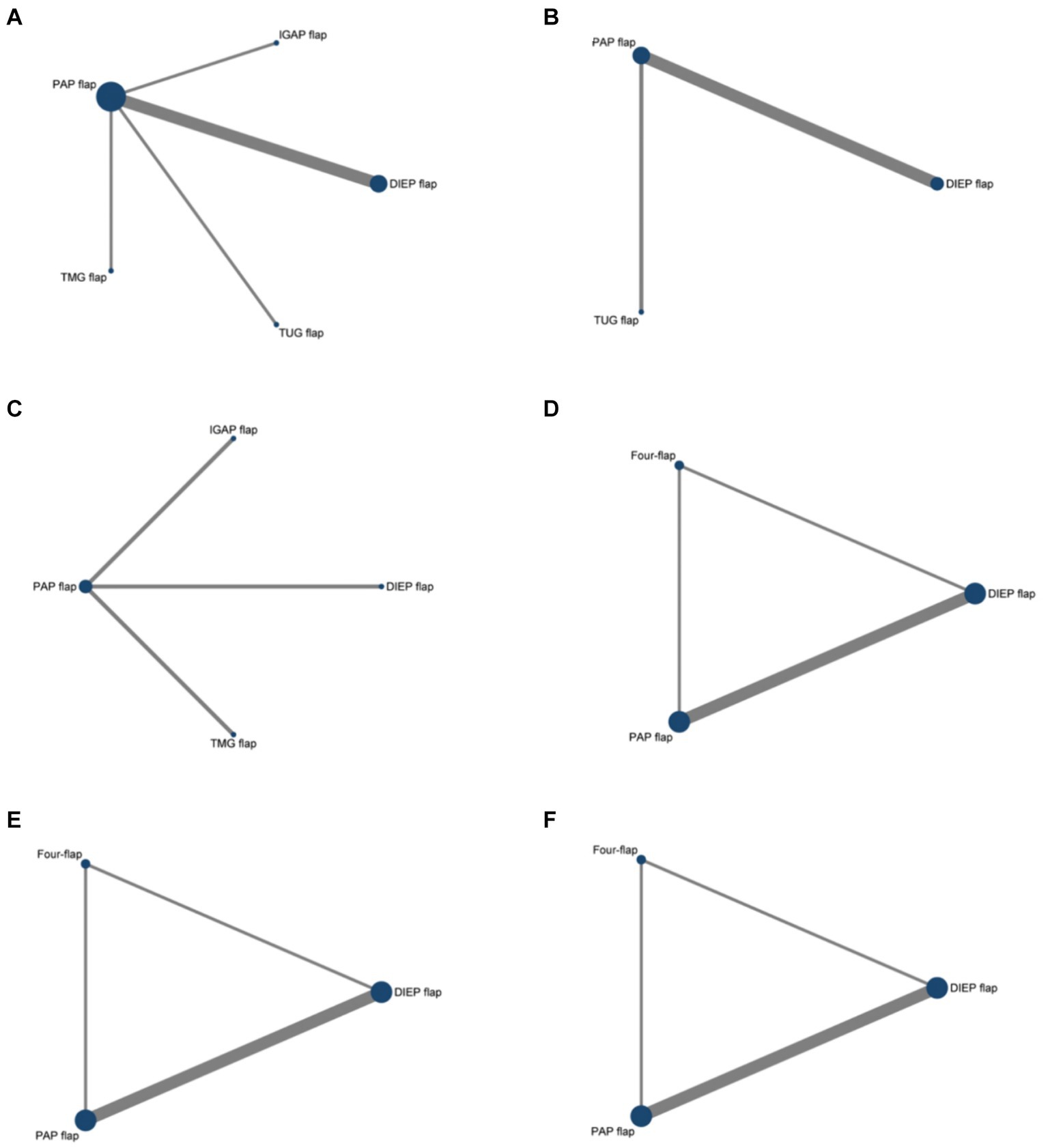
Figure 2. Network graph comparing the efficacy and safety of various flaps in Autologous Breast Reconstruction. (A) Total flap loss, (B) donor site wound dehiscence, (C) secondary corrections donor site, (D) psychosocial well-being, (E) satisfaction with breasts, (F) sexual well-being.
3.5 Efficacy
Since the network evidence graphs for psychosocial well-being, satisfaction with breasts, and sexual well-being are all open loop, a consistency model was applied for the network meta-analysis.
3.5.1 Psychosocial well-being
Four studies included psychosocial well-being as an outcome, involving three types of flaps. Compared to the PAP flap, the Four-flap showed the least reduction in psychosocial well-being scores (SMD = 0.76, 95% CI: −0.38, 1.90), though the difference was not statistically significant (Figure 3A).
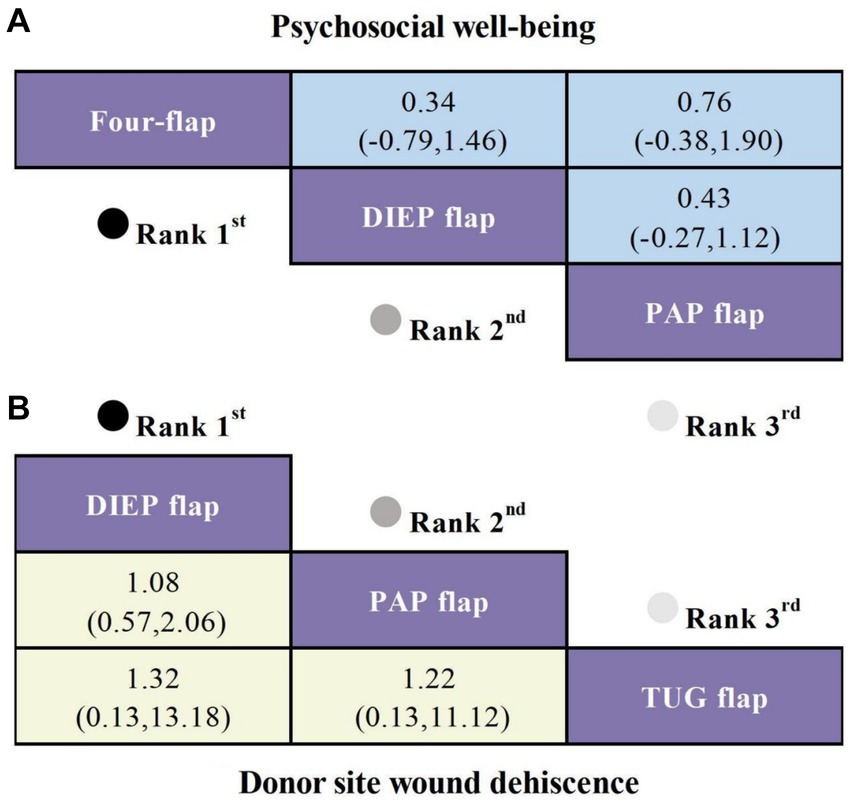
Figure 3. SUCRA curves based on Bayesian network meta-analysis comparing the efficacy and safety of different flaps in Autologous Breast Reconstruction. (A) SMD and 95% CI for psychosocial well-being (depicted in the blue upper triangular area). (B) OR and 95% CI for donor site wound dehiscence (depicted in the yellow lower triangular area).
3.5.2 Sexual well-being
Four studies reported on sexual well-being as an outcome, involving three different types of flaps. Compared to the PAP flap, the Four-flap showed the smallest reduction in sexual well-being scores (SMD = 0.56, 95% CI: −0.02, 1.14), followed by the DIEP flap (SMD = 0.32, 95% CI: −0.08, 0.71), although these differences were not statistically significant (Figure 4A).
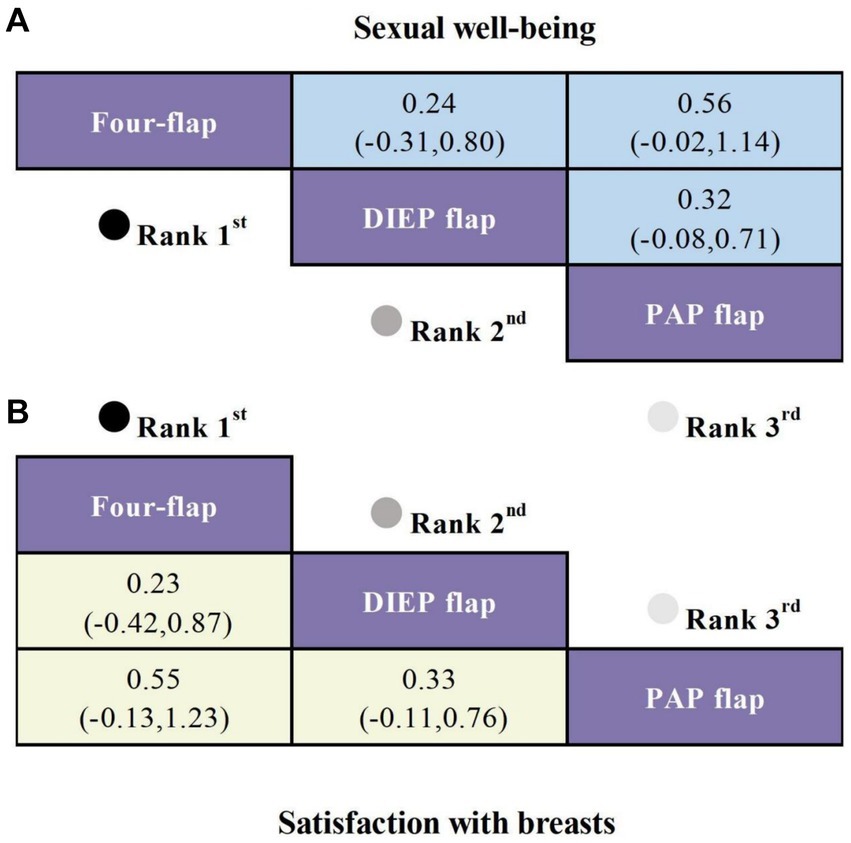
Figure 4. SUCRA curves from Bayesian network meta-analysis comparing the efficacy of different flaps in Autologous Breast Reconstruction. (A) SMD and 95% CI for sexual well-being (shown in the blue upper triangular area). (B) SMD and 95% CI for satisfaction with breasts (shown in the yellow lower triangular area).
3.5.3 Satisfaction with breasts
Four studies reported on satisfaction with breasts as an outcome, involving three different types of flaps. Compared to the PAP flap, the Four-flap demonstrated the smallest decrease in satisfaction (SMD = 0.55, 95% CI: −0.13, 1.23), followed by the DIEP flap (SMD = 0.33, 95% CI: −0.11, 0.76), although these differences were not statistically significant (Figure 4B).
3.6 Safety
The network graphs for psychosocial well-being, satisfaction with breasts, and sexual well-being are all closed loops. An inconsistency model was employed for testing, with results showing p > 0.05, thus confirming consistency in the studies. A consistency model was used for the network meta-analysis.
3.6.1 Total flap loss
Seven studies included total flap loss as an outcome, covering five types of flaps. Compared to the IGAP flap, the TUG flap exhibited the lowest risk of total flap loss (OR = 155.39, 95% CI: 2.46, 9832.27), which was statistically significant. This was followed by the TMG flap (OR = 36.2, 95% CI: 0.51, 2572.75) and DIEP flap (OR = 18.85, 95% CI: 0.84, 425.44), though these findings did not reach statistical significance (Figure 5).
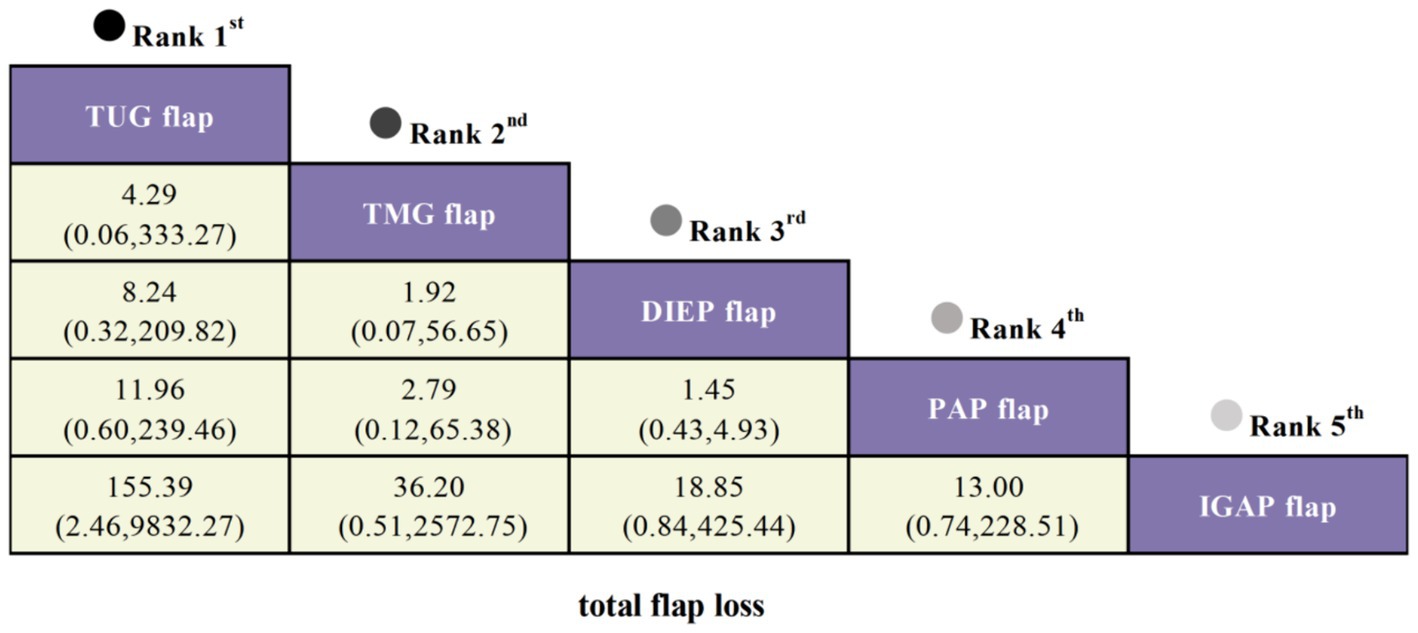
Figure 5. SUCRA curves from Bayesian network meta-analysis comparing total flap loss among different flaps in Autologous Breast Reconstruction.
3.6.2 Donor site wound dehiscence
Four studies reported donor site wound dehiscence as an outcome, involving three different types of flaps. Compared to the TUG flap, the DIEP flap exhibited the lowest risk of donor site wound dehiscence (OR = 1.32, 95% CI: 0.57, 2.06), followed by another flap (OR = 1.22, 95% CI: 0.13, 11.12), although these differences were not statistically significant (Figure 3B).
3.6.3 Secondary corrections at donor site
Three studies reported secondary corrections at the donor site as an outcome, involving four types of flaps. Compared to the IGAP flap, the PAP flap had the lowest risk of secondary corrections (OR = 15.36, 95% CI: 0.89, 265.05), followed by the DIEP flap (OR = 6.14, 95% CI: 0.27, 140.70) and the TMG flap (OR = 4.74, 95% CI: 0.22, 103.77), though none showed statistically significant differences (Figure 6).
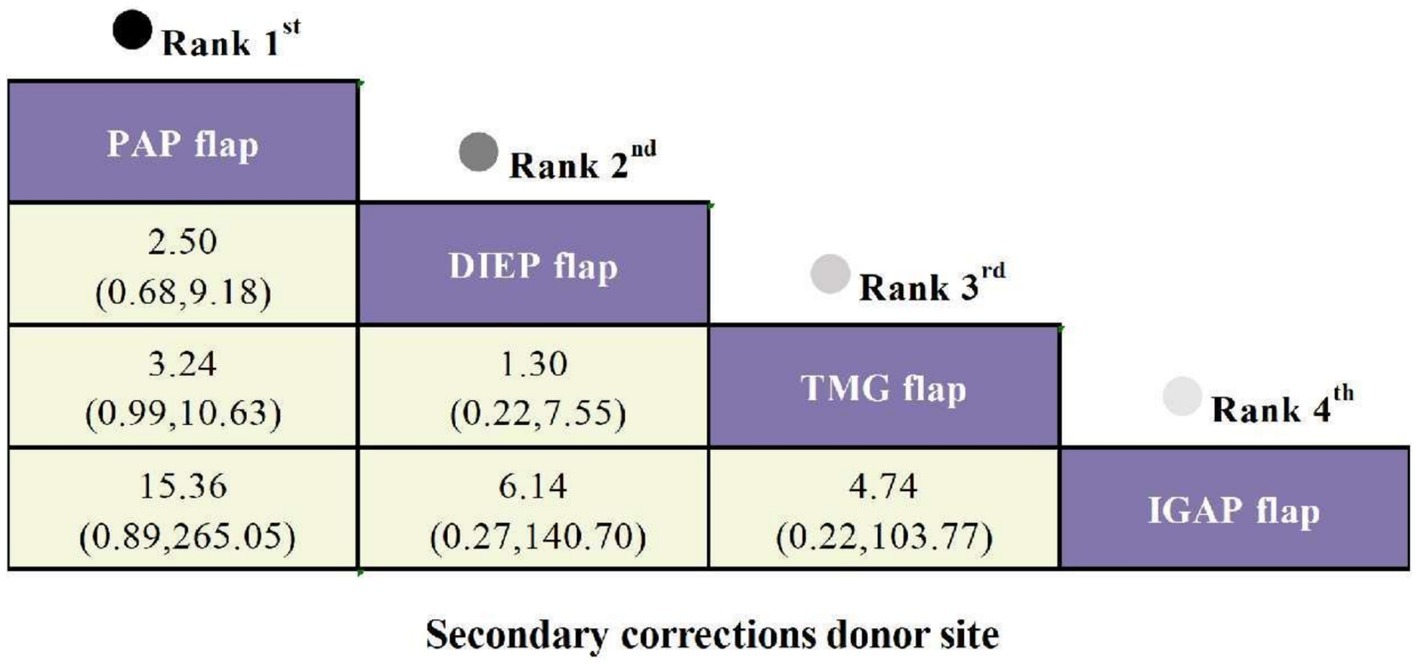
Figure 6. SUCRA curves from Bayesian network meta-analysis comparing secondary corrections at donor site among different flaps in Autologous Breast Reconstruction.
3.7 Rankings
Rankings were determined by comparing the Surface Under the Cumulative Ranking Curve (SUCRA), where the SUCRA values range from 0 to 100% (Table 3). A higher SUCRA value indicates better performance of the flap.
Results show that in the outcome measure of Total Flap Loss, the TUG flap had the highest SUCRA value at 89.6%, followed by the TMG flap at 64.8% (Table 3). For the outcome measure of Donor Site Wound Dehiscence, the DIEP flap had the highest SUCRA value at 60.1%, followed by the PAP flap at 48.6%. In the outcome measure of Secondary Corrections at Donor Site, the PAP flap ranked first with a SUCRA value of 95.5%, followed by the DIEP flap at 52.5% and the TMG flap at 41.4%. For the outcome measures of Psychosocial Well-being, Satisfaction with Breasts, and Sexual Well-being, the Four-flap consistently ranked first (81.3, 85.0, and 88.4%).
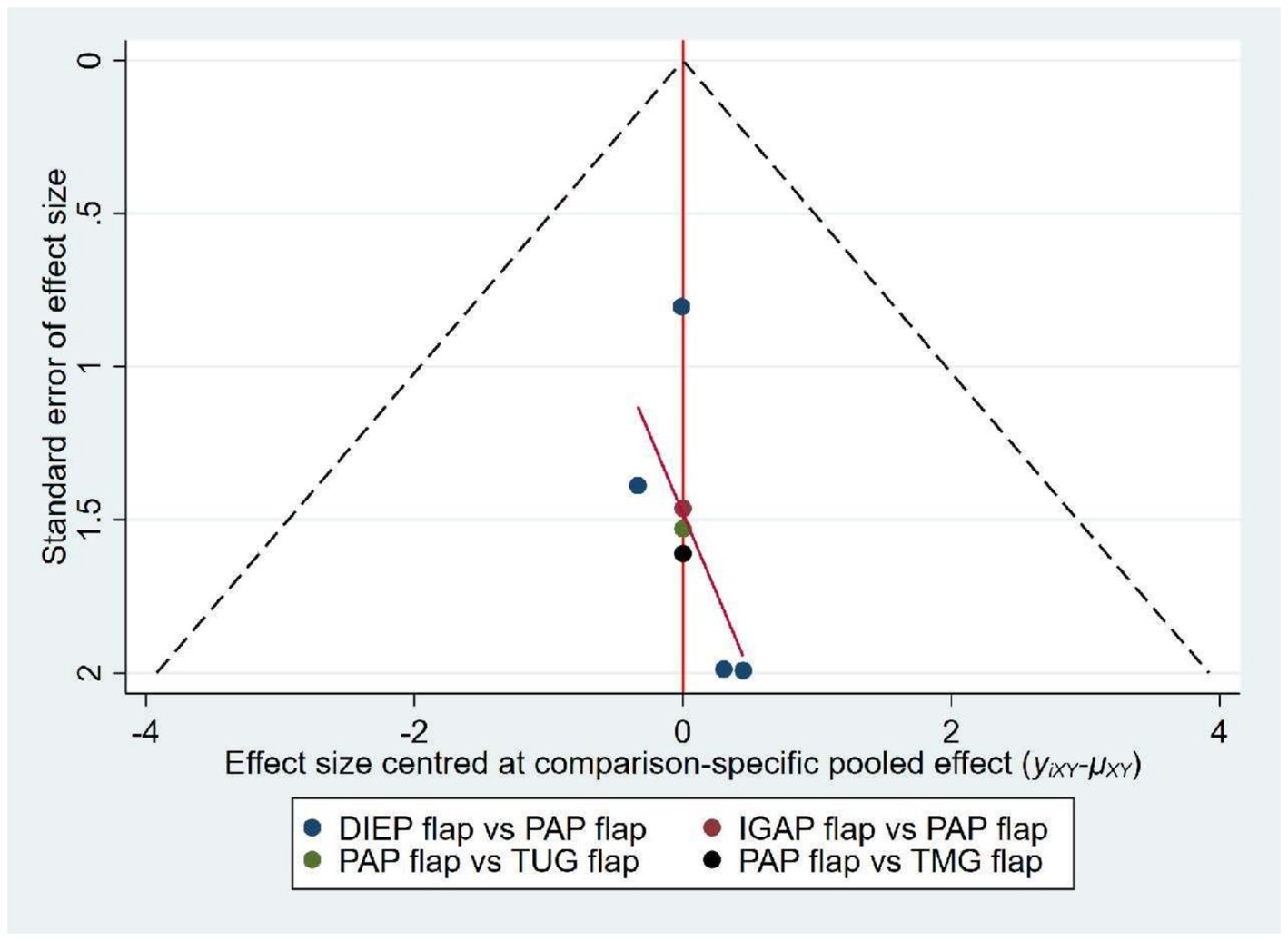
3.8 Publication bias
The funnel plot, as illustrated, shows that the data points are symmetrically and uniformly distributed within the funnel plot. The overall results indicate no significant publication bias, suggesting that the findings are robust and reliable (Figure 7).
4 Discussion
To our knowledge, this Bayesian network meta-analysis is the first to simultaneously evaluate the efficacy and safety of multiple types of flaps, including PAP, DIEP, TMG, TUG, IGAP, and Four-flap. Each flap type has its unique benefits and risks. Our study conducted a quantitative synthesis, revealing the efficacy and safety of different flap types, including the following: (1) The TUG flap exhibited the lowest risk of total flap loss, indicating higher reliability in certain patient populations. (2) Patients with the Four-flap reported the highest satisfaction levels. (3) The PAP flap excelled in secondary corrections at the donor site. (4) Patients with PAP flaps scored lower in psychological well-being, breast satisfaction, and sexual satisfaction compared to other groups.
The four-flap technique typically utilizes the patient’s own adipose and skin tissue for breast reconstruction, resulting in a breast that closely mimics the natural appearance and feel (28). This method allows for precise adjustments to the breast’s shape and size, enhancing symmetry with the contralateral breast and thereby improving aesthetic harmony (29). By avoiding the use of foreign implants, such as prostheses, the four-flap technique reduces the risk of complications associated with implants, including rejection reactions and implant rupture (30). Although the four-flap surgery May involve a more complex procedure and longer recovery time, the reduced use of foreign materials May contribute to a more positive postoperative self-perception in patients (31). This explains why patient satisfaction is highest with four-flap procedures.
Breast reconstruction patients often experience significant psychological stress. The use of autologous tissue, particularly when it achieves an outcome that closely resembles a natural breast, can provide substantial psychological comfort and boost the patient’s confidence, which supports the conclusions of our study. Compared to existing meta-analyses, which often focus on fewer flap types or non-autologous methods—sometimes overlooking the PAP flap—our study identifies its particular benefits for patients with prior abdominal surgeries (8). In terms of psychosocial well-being, satisfaction with breasts, and sexual well-being, patients with the PAP flap scored lower than other groups, possibly because those choosing the PAP flap tend to be slimmer, and the tissue volume provided by the PAP flap is somewhat limited (32). Breast reconstruction is more than just physical restoration; it profoundly affects a woman’s self-esteem, body image, and overall quality of life. Our findings indicate that selecting the appropriate breast reconstruction flap technique can significantly enhance life satisfaction after mastectomy.
The TUG flap Autologous Breast Reconstruction primarily utilizes the gracilis muscle from the inner thigh along with its associated skin and adipose tissue, making it suitable for patients lacking sufficient abdominal tissue (17). The gracilis muscle used in the TUG flap is supplied by branches of the deep artery, which reduces the risk of postoperative flap ischemia and consequently lowers the flap loss rate (33). The skin and fat from the inner thigh have a texture similar to that of breast tissue, making the TUG flap aesthetically more compatible with the natural breast. Additionally, the good elasticity and softness of the inner thigh tissue enhance the adaptability of the transplanted flap, promoting its survival (34). Compared to other methods requiring substantial tissue transfer, such as the DIEP flap, the TUG flap requires less tissue, thereby reducing surgical invasiveness and associated complication risks, ultimately decreasing the overall flap loss rate (35).
Despite the comprehensiveness of our analysis and discussion, there are limitations to this study. Firstly, although an extensive search of English-language databases was conducted, clinical trials focusing on patient satisfaction outcomes were limited to only three types of flaps. Secondly, seven of the 11 included studies were conducted in Europe, reducing the general applicability of the results, which May not be as relevant to populations in Asia and Africa. Thirdly, due to the limited number of studies and the minor differences between various flap techniques, some outcomes showed no statistically significant differences. Future research should include more uniform and rigorous study designs and long-term follow-up data to further validate our findings. Fourthly, some outcomes were analyzed using data from only one or two studies, which May introduce bias due to the small sample size. Consequently, these results should be interpreted with caution. Additional studies are necessary to validate our findings and ensure their reliability. Lastly, not all included studies reported flap volume or degrees of patient satisfaction. The absence of these important variables limits our ability to fully assess the outcomes of different flap techniques. Future studies should aim to include detailed reporting on flap volume and comprehensive measures of patient satisfaction to provide a more complete understanding of the effectiveness of these techniques.
While our Bayesian network meta-analysis highlights the relative strengths and weaknesses of each flap technique, we acknowledge that the results do not definitively establish the superiority of any single technique. This is due to the inherent variability in patient characteristics and clinical circumstances that influence the choice of flap. However, we have provided practical guidelines based on the findings to assist clinicians in selecting the most appropriate flap technique for individual patients.
In conclusion, various flap techniques in Autologous Breast Reconstruction each present distinct benefits and risks. The Four-flap technique shows significant advantages in patient satisfaction, while the TUG flap excels in reducing total flap loss.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
LL: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Project administration, Methodology, Investigation, Formal analysis, Data curation. DW: Conceptualization, Writing – review & editing, Writing – original draft, Validation, Supervision, Software, Resources, Project administration, Methodology, Investigation, Data curation. XZ: Visualization, Formal analysis, Writing – review & editing, Writing – original draft, Validation, Supervision, Software, Resources, Project administration, Methodology, Investigation, Data curation, Conceptualization.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Siegel, RL, Miller, KD, Wagle, NS, and Jemal, A. Cancer statistics, 2023. CA Cancer J Clin. (2023) 73:17–48. doi: 10.3322/caac.21763
3. Luo, N, Qu, Y, and Dong, R. The treatment progress of the breast cancer. Prog Modern Biomed. (2015) 15:160–6.
4. Ganz, PA. Quality of life across the continuum of breast cancer care. Breast J. (2000) 6:324–30. doi: 10.1046/j.1524-4741.2000.20042.x
5. Skrzypulec, V, Tobor, E, Drosdzol, A, and Nowosielski, K. Biopsychosocial functioning of women after mastectomy. J Clin Nurs. (2009) 18:613–9. doi: 10.1111/j.1365-2702.2008.02476.x
6. Eltahir, Y, Werners, LL, Dreise, MM, van Emmichoven, IAZ, Jansen, L, Werker, PM, et al. Quality-of-life outcomes between mastectomy alone and breast reconstruction: comparison of patient-reported BREAST-Q and other health-related quality-of-life measures. Plast Reconstr Surg. (2013) 132:201e–9e. doi: 10.1097/PRS.0b013e31829586a7
7. Semple, JL, Viezel-Mathieu, A, Alshaqsi, S, and Armstrong, K. A safe and efficient technique for Pedicled TRAM flap breast reconstruction. Plast Reconstr Surg. (2023) 151:1022e–34e. doi: 10.1097/PRS.0000000000010174
8. Martineau, J, Scampa, M, Viscardi, JA, Giordano, S, Kalbermatten, DF, and Oranges, CM. Inferior gluteal artery perforator (IGAP) flap in autologous breast reconstruction: a proportional meta-analysis of surgical outcomes. J Plast Reconstr Aesthet Surg. (2023) 84:147–56. doi: 10.1016/j.bjps.2023.05.018
9. Vollbach, FH, Neuss, C, Siegwart, LC, Bigdeli, AK, Kneser, U, Fansa, H, et al. The transverse myocutaneous gracilis flap (TMG) for breast reconstruction: ipsi vs. contralateral harvest—aesthetic outcome and refinement procedures. Breast Cancer. (2023) 30:845–55. doi: 10.1007/s12282-023-01478-x
10. Hunter, J, Lardi, A, Dower, D, and Farhadi, J. Evolution from the TUG to PAP flap for breast reconstruction: comparison and refinements of technique. J Plast Reconstr Aesthet Surg. (2015) 68:960–5. doi: 10.1016/j.bjps.2015.03.011
11. Macadam, SA, Zhong, T, Weichman, K, Papsdorf, M, Lennox, PA, Hazen, A, et al. Quality of life and patient-reported outcomes in breast cancer survivors: a multi-center comparison of four abdominally-based autologous reconstruction methods. Plast Reconstr Surg. (2015) 136:86–7. doi: 10.1097/01.prs.0000472386.80855.11
12. O'Neill, AC, Haykal, S, Bagher, S, Zhong, T, and Hofer, SO. Predictors and consequences of intraoperative microvascular problems in autologous breast reconstruction. J Plast Reconstr Aesthet Surg. (2016) 69:1349–55. doi: 10.1016/j.bjps.2016.07.006
13. Haddock, NT, Gassman, A, Cho, M-J, and Teotia, SS. 101 consecutive profunda artery perforator flaps in breast reconstruction: lessons learned with our early experience. Plast Reconstr Surg. (2017) 140:229–39. doi: 10.1097/PRS.0000000000003553
14. Chang, EI. Latest advancements in autologous breast reconstruction. Plast Reconstr Surg. (2021) 147:111e–22e. doi: 10.1097/PRS.0000000000007480
15. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
16. Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta analyses. Eur J Epidemiol. (2010). 25:603–5.
17. Salanti, G, Ades, AE, and Ioannidis, JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. (2011) 64:163–71. doi: 10.1016/j.jclinepi.2010.03.016
18. Augustin, A, Morandi, EM, Winkelmann, S, Schoberleitner, I, Egle, D, Ritter, M, et al. Long-term results after autologous breast reconstruction with DIEP versus PAP flaps based on quality of life and aesthetic outcome analysis. J Clin Med. (2023) 12:737. doi: 10.3390/jcm12030737
19. Augustin, A, Pülzl, P, Morandi, EM, Winkelmann, S, Schoberleitner, I, Brunner, C, et al. Donor-site morbidity and quality of life after autologous breast reconstruction with PAP versus TMG flap. Curr Oncol. (2022) 29:5682–97. doi: 10.3390/curroncol29080448
20. Chan, SY, Kuo, WL, Cheong, DC, Chang, FC, and Huang, JJ. Small flaps in microsurgical breast reconstruction: selection between the profunda artery perforator and small deep inferior epigastric artery perforator flaps and associated outcomes and complications. Microsurgery. (2024) 44:e31046. doi: 10.1002/micr.31046
21. Haddock, NT, Dickey, RM, Perez, K, Garza, R, Liu, Y, and Teotia, SS. BREAST-Q and donor site comparison in bilateral stacked autologous breast reconstruction. Plast Reconstr Surg Glob Open. (2022) 10:413. doi: 10.1097/GOX.0000000000004413
22. Jo, T, Jeon, DN, and Han, HH. The PAP flap breast reconstruction: a practical option for slim patients. J Reconstr Microsurg. (2022) 38:27–33. doi: 10.1055/s-0041-1727200
23. Kim, HB, Han, SJ, Kim, EK, Eom, JS, and Han, HH. Comparative study of DIEP and PAP flaps in breast reconstruction: reconstructive outcomes and fat necrosis. J Reconstr Microsurg. (2023) 39:627–32. doi: 10.1055/a-2040-1368
24. Lee, ZH, Chu, CK, Asaad, M, Liu, J, Selber, JC, Butler, CE, et al. Comparing donor site morbidity for autologous breast reconstruction: thigh vs. abdomen. Plast Reconstr Surg Glob Open. (2022) 10:e4215. doi: 10.1097/GOX.0000000000004215
25. Murphy, DC, Razzano, S, Wade, RG, Haywood, RM, and Figus, A. Inferior gluteal artery perforator (IGAP) flap versus profunda artery perforator (PAP) flap as an alternative option for free autologous breast reconstruction. J Plast Reconstr Aesthet Surg. (2022) 75:1100–7. doi: 10.1016/j.bjps.2021.09.043
26. Teotia, SS, Dumestre, DO, Jayaraman, AP, Sanniec, KJ, and Haddock, NT. Revisiting anastomosis to the retrograde internal mammary system in stacked free flap breast reconstruction: an algorithmic approach to recipient-site selection. Plast Reconstr Surg. (2020) 145:880–7. doi: 10.1097/PRS.0000000000006712
27. Varnava, C, Klietz, ML, Hirsch, T, Wiebringhaus, P, and Kueckelhaus, M. Comparison of surgical and patient-reported outcomes between 85 profunda artery perforator flaps and 122 deep inferior epigastric perforator flaps as first-choice treatment for breast reconstruction. J Plast Reconstr Aesthet Surg. (2023) 80:168–77. doi: 10.1016/j.bjps.2023.02.018
28. Toyserkani, NM, Jørgensen, MG, Tabatabaeifar, S, Damsgaard, T, and Sørensen, JA. Autologous versus implant-based breast reconstruction: a systematic review and meta-analysis of breast-Q patient-reported outcomes. J Plast Reconstr Aesthet Surg. (2020) 73:278–85. doi: 10.1016/j.bjps.2019.09.040
29. Nahabedian, MY, and Patel, K. Autologous flap breast reconstruction: surgical algorithm and patient selection. J Surg Oncol. (2016) 113:865–74. doi: 10.1002/jso.24208
31. Champaneria, MC, Wong, WW, Hill, ME, and Gupta, SC. The evolution of breast reconstruction: a historical perspective. World J Surg. (2012) 36:730–42. doi: 10.1007/s00268-012-1450-2
32. Atzeni, M, Salzillo, R, Haywood, R, Persichetti, P, and Figus, A. Breast reconstruction using the profunda artery perforator (PAP) flap: technical refinements and evolution, outcomes, and patient satisfaction based on 116 consecutive flaps. J Plast Reconstr Aesthet Surg. (2022) 75:1617–24. doi: 10.1016/j.bjps.2021.11.085
33. Arnež, Z, Pogorelec, D, Planinšek, F, and Ahčan, U. Breast reconstruction by the free transverse gracilis (TUG) flap. Br J Plast Surg. (2004) 57:20–6. doi: 10.1016/j.bjps.2003.10.007
34. Pantelides, NM, Romulus, C, Patel, NG, Morgan, M, and Ramakrishnan, VV. Unilateral breast reconstruction using double transverse upper gracilis (TUG) flaps. J Plast Reconstr Aesthet Surg. (2022) 75:1164–70. doi: 10.1016/j.bjps.2021.11.010
Keywords: Autologous Breast Reconstruction, flap, network meta-analysis, efficacy, safety
Citation: Li L, Wu D and Zhu X (2024) Evaluating the efficacy and safety of various flaps in Autologous Breast Reconstruction: a Bayesian network meta-analysis. Front. Med. 11:1440139. doi: 10.3389/fmed.2024.1440139
Edited by:
Andrea Lisa, Humanitas Research Hospital, ItalyReviewed by:
Yong Miao, Southern Medical University, ChinaManuela Bottoni, European Institute of Oncology (IEO), Italy
Copyright © 2024 Li, Wu and Zhu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaohai Zhu, ZHJ6eGhAcXEuY29t
†These authors have contributed equally to this work
 Ling Li1†
Ling Li1† Xiaohai Zhu
Xiaohai Zhu