- 1Research and Development Unit, Hammersmith and Fulham Primary Care Network, London, United Kingdom
- 2Faculty of Medicine, Imperial College London, London, United Kingdom
Introduction
The issue of diagnostic bias within primary care has profound implications for the early detection of cancer, particularly among younger patients. Diagnostic bias refers to the preconceived notions and assumptions that influence a clinician's judgment, potentially leading to misdiagnosis or delayed diagnosis (1). Early diagnosis of cancer is critical for effective treatment and improved prognostic outcomes, making the recognition and mitigation of diagnostic biases an essential component of primary care practice.
Cancer incidence and mortality in adults under 50 years of age has been rising globally in the decades since 1990, especially in more highly-developed countries (2). This trend has occurred in the UK, and 9% of new cancer cases are diagnosed in those aged 25–49 (a rise in incidence of 22% from 1993 to 2019, total incidence 164.6 per 100,000 25–49 year olds in 2019), predominantly affecting women (Tables 1, 2) (3). Whilst this trend may partially be due to increasing access to investigations and improved diagnostic capabilities, it has been suggested that the rising incidence is also partly attributable to the oncogenic effects of rising obesity, rising alcohol consumption, and new dietary and environmental exposures (4).
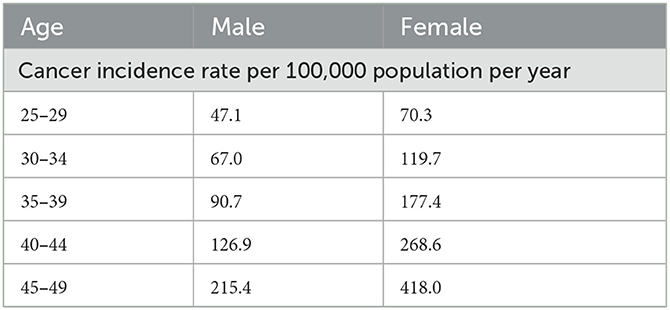
Table 1. Cancer incidence rates per 100,000 population per year, subdivided by age group, in males and females aged 25–49 in the UK, from 2017–2019.
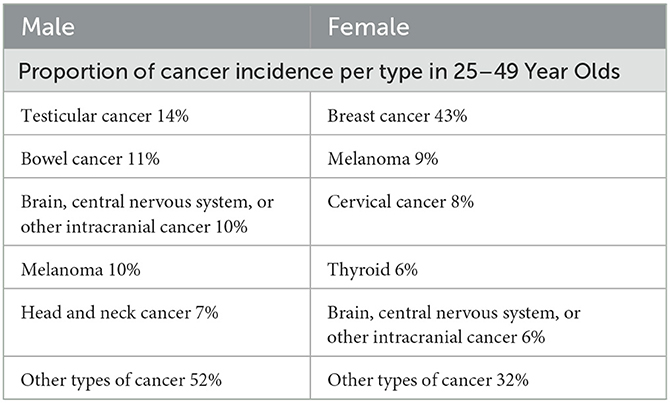
Table 2. Percentages of different types of cancer as a proportion of the total incidence of new cancer diagnoses, in males and females aged 25–49 in the UK, from 2017–2019 (data from Cancer Research UK; N.B. all data excludes non-melanoma skin cancer) (3).
Primary care physicians are often the first point of contact for patients, positioning them uniquely to detect early signs of cancer. However, the age-related bias that younger patients are less likely to have serious conditions such as cancer can lead to significant delays in diagnosis (1, 5). This is especially concerning given that certain cancers in young patients can be more aggressive and progress rapidly, such as in breast cancer (6). Therefore, the main argument posited in this view point is that primary care physicians must actively work to overcome diagnostic biases that impede the early detection of cancer in younger patients.
Diagnostic bias in younger patients
Diagnostic bias toward younger patients has the potential to lead to significant delays in identifying serious conditions such as cancer. Interviews with young adults with cancer, revealed that in many cases the patient and/or the clinician assumed it unlikely they would have cancer due to their age, resulting in delayed diagnosis in most cases (7). This bias is even noted in cancer investigation clinical guidance, with many guidelines having strict age cut-offs for investigating certain symptoms, such as under the UK's 2-week wait pathways (although some do contain overriding caveats for serious clinician concern) (8). Younger individuals presenting with atypical symptoms can be presumed by clinicians to have benign conditions (9), a presumption likely rooted in the significantly lower statistical prevalence of cancer within this demographic, (5, 10)something elsewhere termed epidemiological optimism bias (11). This bias is further exacerbated by the tendency of some primary care physicians to prioritize more common and less severe diagnoses (6). Studies have demonstrated that general practitioners are less likely to suspect malignancy in younger patients, which can result in delays in diagnosis and treatment (10, 12).
Research indicates that when younger patients present with symptoms such as unexplained weight loss, persistent pain, or unusual lumps, these signs are often attributed to benign causes like stress, infections, or minor injuries. For instance, a study by Dommett et al. (10) found that the likelihood of cancer being initially misdiagnosed in younger individuals was substantially higher compared to older adults. This misdiagnosis often leads to multiple consultations and a significant delay before appropriate investigations are conducted.
A notable example is the misdiagnosis of Hodgkin lymphoma in younger patients, which often presents with non-specific symptoms such as fatigue, fever, and lymphadenopathy. A delay in recognizing these symptoms as potential indicators of cancer can severely impact prognosis (10, 13). Similarly, younger patients with colorectal cancer often have a delay in diagnosis (14), due to both patient and doctor delay, and in some cases can also receive misdiagnosis as common benign conditions, such as hemorrhoids (15).
The tendency to overlook serious conditions in younger patients highlights the urgent need for heightened awareness and consideration of cancer as a differential diagnosis. Studies such as those by Lyratzopoulos et al. (16) have underscored the importance of considering a wider range of potential diagnoses to prevent delays that can compromise treatment outcomes. By recognizing and challenging these biases, we hope primary care physicians can improve diagnostic accuracy and ensure more timely intervention, ultimately enhancing patient care and survival rates.
Importance of differential diagnosis and appropriate investigation
The necessity of considering cancer as a potential diagnosis in younger patients cannot be overstated. When cancer is not included as a differential diagnosis, critical time may be lost, leading to more advanced disease stages at the time of diagnosis. This delay can diminish the efficacy of treatment and worsens patient prognosis, making early and accurate diagnosis paramount (10, 11, 17). For example, a study by Swann et al. (18) reflects that delayed cancer diagnosis in younger patients often results in more aggressive disease progression and reduced survival rates. Conducted as a clinical audit in English general practices, data was collected on 17,042 patients newly diagnosed with cancer in 2014, noting that diagnostic delays occurred in 22% of cases due to patient, clinician, or system factors.
The thoroughness of the diagnostic process is crucial in mitigating these delays. Primary care physicians must adopt a comprehensive and systematic approach to evaluating symptoms, irrespective of the patient's age. This involves maintaining a high index of suspicion and conducting appropriate investigations even when initial symptoms are non-specific. As noted by Black et al. (19), implementing a structured diagnostic protocol can enhance early detection rates and improve clinical outcomes.
Vigilance in identifying potential cancer signs is imperative. Whilst of course the majority of presentations in primary care are not due to cancer, we would propose a dual approach of working toward a most likely diagnosis, whilst also considering serious differential diagnoses. For instance, non-specific symptoms such as abdominal pain, or unexplained weight loss, should prompt consideration of malignancy and inclusion of appropriate investigations regardless of patient age and whether malignancy is the most likely diagnosis. The integration of decision support tools and evidence-based guidelines in primary care practice can aid clinicians in making more informed diagnostic decisions (20, 21, 27). Additionally, a proactive stance, as recommended by O'Sullivan et al. (22), involves routine updates to clinical guidelines and continuous professional development to keep abreast of emerging trends in cancer presentation and investigation.
Beyond challenging diagnostic biases to improve clinician recognition of potential cancers in younger patients, there must be better support for clinicians in then making further decisions about investigations. An investigation can be judged in terms of its appropriateness, which is the balance of risk and benefit of any investigation for a specific patient (23). Unfortunately, there is generally a lack of research into the appropriateness of investigations specifically for cancer in younger people presenting to primary care (24). Changing this is vital to better inform guidelines and decision support tools, so that clinicians are well supported in making decisions about the investigations needed to diagnose cancer.
Apart from the potential benefit of an accurate diagnosis, there are innumerable risks of an investigation a clinician will be weighing up, such as: false reassurance and patient disengagement following a false negative result; patient anxiety and further investigations resulting from either false positive results or non-symptomatic incidental findings; and the risks of direct harm from any investigation, for example radiation exposure. More broadly, clinicians will also be considering the wider implications of any investigation, including the costs to the healthcare system and the risk of lengthening waiting times for investigations for other patients. These risks are especially pronounced in younger patients presenting to primary care, as the vast majority of presentations, will not be due to cancer. To make more confident decisions about investigations, clinicians must be given enhanced guidelines for managing investigations for potential cancer in younger people, as well as better data to back-up their decisions. This research and guidance should also account for possible lead-time bias, which would be the potential for any increase in investigation in younger people for cancer, to lead to earlier detection but not necessarily truly enhanced survival (25).
Training and awareness programs
The implementation of comprehensive training and awareness programs for general practitioners (GPs) is critical in addressing diagnostic biases and improving the accuracy of cancer detection in younger patients. Such programs are designed to enhance clinicians' awareness of their biases, be they conscious or unconscious, and equip them with the necessary skills to recognize atypical presentations of cancer. These educational initiatives can significantly alter diagnostic practices and improve patient outcomes (Table 3). An excellent example of this is Bowel Cancer UK's “Never Too Young” initiative (26).
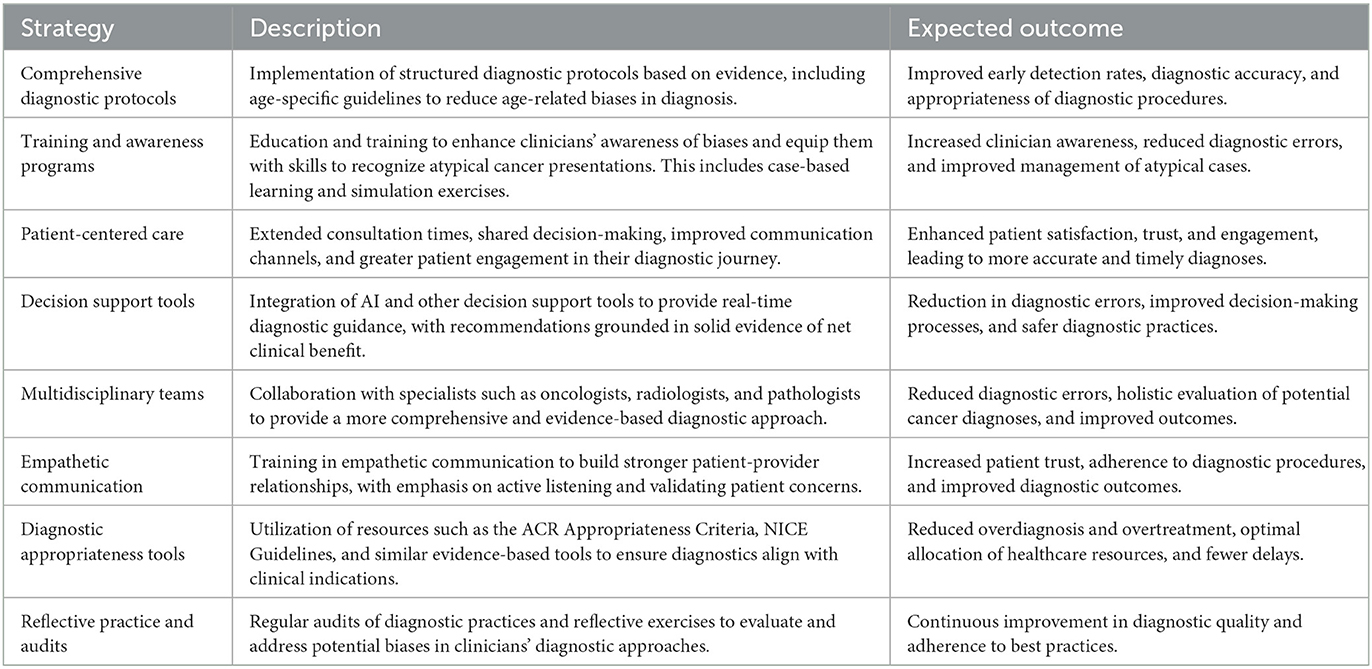
Table 3. Summary of key strategies to mitigate diagnostic bias in cancer detection among younger patients.
Effective training programs focus on several key areas. Firstly, they emphasize the importance of a thorough and systematic approach to diagnosis, encouraging GPs to consider a broad differential diagnosis that includes malignancies, regardless of the patient's age (19). According to a study by Walter et al. (28), training that incorporates case-based learning and simulation exercises can improve diagnostic accuracy by providing GPs with practical experience in identifying cancer symptoms in younger patients. These programs also highlight the significance of early detection and the potential consequences of delayed diagnosis, reinforcing the need for vigilance and overcoming diagnostic bias in clinical practice.
Furthermore, awareness initiatives that target diagnostic bias can help clinicians recognize and mitigate their own preconceived notions. A study by Staal et al. (29) examined the importance of fostering a broad differential diagnostic approach, as narrowing the focus prematurely can overlook potential key diagnoses. Incorporating reflective practice, where physicians regularly review and critically analyze their diagnostic decisions, can foster a culture of self-awareness, openness and continuous improvement.
In addition to formal training, ongoing professional development and access to updated clinical guidelines are essential. Regular workshops, educational courses, and peer-reviewed journals help keep GPs up to date with the latest evidence-based practices and emerging trends in cancer diagnosis. For instance, the integration of decision support tools, as recommended by Schmidt et al. (30), can assist GPs in making more informed decisions by providing contemporary guidance based on current clinical data.
Discussion
The necessity to overcome diagnostic biases in primary care to enhance early cancer detection in younger patients has been examined in the preceding sections. The central points underscored the detrimental impact of age-related biases, the importance of including cancer in differential diagnoses for younger patients, and the vital role of training and awareness programs (1, 10). Addressing these biases has significant implications for clinical practice, patient outcomes, and the broader healthcare system.
One of the primary implications for practice is the potential improvement in early cancer detection rates among younger patients (17). Early diagnosis is crucial as it often leads to better prognostic outcomes and more effective treatment options (5). By ensuring that cancer is considered as a possible diagnosis irrespective of patient age, primary care physicians can help mitigate the risks associated with delayed diagnosis (19, 21). Moreover, addressing diagnostic biases can enhance the overall quality of patient care. When physicians adopt a more inclusive diagnostic process, they are likely to conduct more thorough evaluations, thereby improving the accuracy of their diagnoses (20, 22). This comprehensive approach not only benefits the patients by providing timely and appropriate care but also reinforces trust in the healthcare system. To actively engage primary care physicians in mitigating diagnostic biases, ongoing education and awareness-raising must be emphasized. Professional development programs that focus on recognizing and overcoming diagnostic biases should be mandated (22).
Furthermore, implementing decision support algorithms in primary care settings can significantly aid in reducing diagnostic errors. Algorithms can provide evidence-based guidance and highlight potential malignancies based on presenting symptoms, regardless of patient age. The use of artificial intelligence (AI) in primary care is one area that may see future expansion and work alongside this. AI tools can analyze large datasets to identify patterns that may not be immediately apparent to human clinicians, which could offer enhanced diagnostics and in the future (31). However, this is dependent on the specifics of any AI development and implementation, and there are concerns being raised of AI amplifying and entrenching the existing human diagnostic biases of those designing and developing it (32, 33).
Primary care settings should also advocate for policy changes that support regular training and the integration of diagnostic support tools. Policymakers and healthcare administrators need to allocate resources (both in terms of finances and clinician time) toward these initiatives, recognizing their long-term benefits in improving patient outcomes and reducing healthcare costs associated with late-stage cancer treatments (28), alongside the important moral imperative to challenge factors that disadvantage younger people with cancer. Collaborations with academic institutions, professional organizations, and charities, can help facilitate the development and dissemination of effective training and policy changes (26, 27, 34, 35).
Future research should focus on several key areas of cancer diagnosis in younger people. Firstly, it is vital research looks to further develop and validate diagnostic algorithms that are tailored to younger patient populations, so that clinicians can be better supported in their decision making. Studies should also investigate the effectiveness of different training methodologies in reducing diagnostic biases and improving early detection rates (13, 18, 19, 36, 37). Emerging population-based evidence supports this trend as particularly urgent. Sifaki-Pistolla et al. (38) demonstrated a significant increase in the incidence of colorectal cancer among age groups below 50 years during the past 30 years in the Greek population, while further projection indicated that there is also a trend to be projected. These findings set the challenge for updating the guidelines by putting an accent on young age groups early in the course of interventions.
Additionally, research on patient outcomes following the implementation of bias reduction strategies can provide valuable insights into the practical benefits of these initiatives. There is a broader picture here as well, which has innumerable areas where future research would be helpful, including research looking to understand and intervene in patient factors related to delayed presentation in younger people with cancer, as well as research examining the underlying reasons for the rising incidence of cancer diagnosis in younger people. Besides, cultural and behavioral factors play an important role in the influence of delays in diagnosis. Oikonomidou et al. indicated that in rural Greece, patients often refused diagnostic procedures such as endoscopy due to fears, misconceptions, and competing life priorities. These barriers underline the need for culturally sensitive strategies to enhance compliance and early detection (39).
Patient-centered care strategies
Addressing diagnostic biases in primary care not only requires systemic and educational interventions but also necessitates a shift toward more patient-centered care strategies. These strategies place the patient at the heart of the diagnostic process, ensuring that their concerns and symptoms are thoroughly evaluated and addressed. One effective patient-centered strategy is the implementation of extended consultation times for complex cases, allowing GPs to conduct more comprehensive histories and examinations, and consider a wider range of differential diagnoses. Research by Epstein et al. (34) suggests that longer consultation times are associated with improved diagnostic accuracy, particularly in cases presenting with atypical symptoms.
Another crucial aspect of patient-centered care is the active involvement of patients in their diagnostic journey. This can be achieved through shared decision-making, where patients are encouraged to participate more actively in discussions about their symptoms, investigations, and differential diagnoses. Providing patients with detailed information about their symptoms can empower them to advocate for their own health. A study by Charles et al. (35) found that patient involvement in the diagnostic process leads to higher satisfaction and better health outcomes. Concurrently, improving communication channels between GPs and patients is essential. Timely follow-ups and open lines of communication can help in monitoring the progression of symptoms and making appropriate adjustments to the diagnostic approach. Implementing electronic health records (EHR) with patient portals can facilitate this communication.
Patient education is a critical public health and policy component of patient-centered care. Educating patients about the signs and symptoms of cancer, regardless of their age, can raise awareness and prompt earlier medical consultations. Community outreach programs and educational campaigns, as highlighted by Young and Robb (36) have been shown to improve public awareness of cancer symptoms, which can lead to more timely presentation and diagnosis.
Integrating multidisciplinary teams into primary care can also enhance patient-centered care. Collaboration with specialists such as oncologists, radiologists, and pathologists can provide a more comprehensive approach to diagnosis and treatment planning (35–37).
Lastly, fostering a supportive and empathetic clinical environment is paramount. Primary care physicians should be trained in empathetic communication, which involves actively listening to patients, validating their concerns, and expressing genuine care and understanding. Empathetic interactions have been shown to build stronger patient-provider relationships, increase patient trust, and improve adherence to recommended diagnostic procedures (37).
Conclusion
Addressing diagnostic biases in primary care is paramount for improving the detection of cancer in younger patients. Overcoming these biases requires a multifaceted approach, including comprehensive training programs to enhance clinical awareness, the integration of decision support tools, and systemic changes to support continuous professional development. Furthermore, adopting patient-centered care strategies, such as extended consultation times, shared decision-making, and improved communication, can significantly enhance diagnostic accuracy and patient outcomes. By challenging diagnostic biases, and fostering an environment of vigilance and empathy, we hope primary care physicians can better identify and diagnose cancer in younger patients, ultimately leading to more timely and effective treatments. This proactive and inclusive approach not only benefits patients but also wider healthcare systems.
Author contributions
WJ: Conceptualization, Data curation, Investigation, Resources, Validation, Visualization, Writing – original draft, Writing – review & editing. DH: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Maringe C, Spicer J, Morris M, Purushotham A, Nolte E, Sullivan R, et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol. (2020) 21:1023–34. doi: 10.1016/S1470-2045(20)30388-0
2. Zhao J, Xu L, Sun J, Song M, Wang L, Yuan S, et al. Global trends in incidence, death, burden and risk factors of early-onset cancer from 1990 to 2019. BMJ Oncol. (2023) 2:e000049. doi: 10.1136/bmjonc-2023-000049
3. Cancer Research UK. Cancer Incidence by Age. Cancer Research UK. CRUK (2024). Available at: https://www.cancerresearchuk.org/health-professional/cancer-statistics/incidence/age (accessed December 3, 2024).
4. Ugai T, Sasamoto N, Lee HY, Ando M, Song M, Tamimi RM, et al. Is early-onset cancer an emerging global epidemic? Current evidence and future implications. Nat Rev Clin Oncol. (2022) 19:1–18. doi: 10.1038/s41571-022-00672-8
5. Richards MA. The size of the prize for earlier diagnosis of cancer in England. Br J Cancer. (2009) 101:S125–9. doi: 10.1038/sj.bjc.6605402
6. Costa L, Kumar R, Villarreal-Garza C, Sinha S, Saini S, Jaynati Semwal, et al. Diagnostic delays in breast cancer among young women: An Emphasis on healthcare providers. The Breast. (2023) 73:103623. doi: 10.1016/j.breast.2023.103623
7. Miedema BB, Easley J, Hamilton R. Young adults' experiences with cancer: comments from patients and survivors. Canad Family Phys. (2006) 52:1446.
8. NICE. Recommendations organised by site of cancer | Suspected cancer: recognition and referral | Guidance | NICE. www.nice.org.uk (2023) Available at: https://www.nice.org.uk/guidance/ng12/chapter/Recommendations-organised-by-site-of-cancer (accessed December 3, 2024).
9. Hajdarevic S, Högberg C, Marzo-Castillejo M, Silina V, Sawicka-Powierza J, Esteva M, et al. Why do European primary care physicians sometimes not think of, or act on, a possible cancer diagnosis? A qualitative study. BJGP Open. (2023) 7:29. doi: 10.3399/BJGPO.2023.0029
10. Dommett RM, Redaniel MT, Stevens MC, Hamilton W, Martin RM. Features of cancer in teenagers and young adults in primary care: a population-based nested case-control study. Br J Cancer. (2013) 108:2329–33. doi: 10.1038/bjc.2013.191
11. Lyratzopoulos G, Vedsted P, Singh H. Understanding missed opportunities for more timely diagnosis of cancer in symptomatic patients after presentation. Br J Cancer. (2015) 112:S84–91. doi: 10.1038/bjc.2015.47
12. Unger-Saldaña K, Fitch-Picos K, Villarreal-Garza C. Breast cancer diagnostic delays among young mexican women are associated with a lack of suspicion by health care providers at first presentation. J Global Oncol. (2019) 23:1–12. doi: 10.1200/JGO.19.00093
13. White B, Renzi C, Barclay M, Lyratzopoulos G. Underlying cancer risk among patients with fatigue and other vague symptoms: a population-based cohort study in primary care. Br J Gen Pract. (2023) 73:e75–87. doi: 10.3399/BJGP.2022.0371
14. Rydbeck D, Asplund D, Bock D, Haglind E, Park J, Rosenberg J, et al. Younger age at onset of colorectal cancer is associated with increased patient's delay. Eur J Cancer. (2021) 154:269–76. doi: 10.1016/j.ejca.2021.06.020
15. Aaronson EL, Quinn GR, Wong CI, Murray AM, Petty CR, Einbinder J, et al. Missed diagnosis of cancer in primary care: Insights from malpractice claims data. J Healthcare Risk Manag. (2019) 39:19–29. doi: 10.1002/jhrm.21385
16. Lyratzopoulos G, Wardle J, Rubin G. Rethinking diagnostic delay in cancer: how difficult is the diagnosis? BMJ. (2014) 349:g7400. doi: 10.1136/bmj.g7400
17. White B, Rafiq M, Gonzalez-Izquierdo A, Hamilton W, Price S, Lyratzopoulos G. Risk of cancer following primary care presentation with fatigue: a population-based cohort study of a quarter of a million patients. Br J Cancer. (2022) 126:1627–36. doi: 10.1038/s41416-022-01733-6
18. Swann R, McPhail S, Witt J, Shand B, Abel GA, Hiom S, et al. Diagnosing cancer in primary care: results from the national cancer diagnosis audit. Br J Gen Pract. (2018) 68:e63–72. doi: 10.3399/bjgp17X694169
19. Black GB, Lyratzopoulos G, Vincent CA, Fulop NJ, Nicholson BD. Early diagnosis of cancer: systems approach to support clinicians in primary care. BMJ. (2023) 380:e071225. doi: 10.1136/bmj-2022-071225
20. Wulaningsih W. Putting the components back in the systems approach to early diagnosis of cancer. BMJ. (2023) 380:700. doi: 10.1136/bmj.p700
21. Dixon S, McNiven A, Perro D, Vincent K, Marečková M. Systems approach applies to diagnosis of other conditions. BMJ. (2023) 380:704. doi: 10.1136/bmj.p704
22. O'Sullivan JW, Muntinga T, Grigg S, Ioannidis JPA. Prevalence and outcomes of incidental imaging findings: umbrella review. BMJ. (2018) 361:k2387. doi: 10.1136/bmj.k2387
23. Cappelletti P. Appropriateness of diagnostics tests. Int J Lab Hematol. (2016) 38:91–9. doi: 10.1111/ijlh.12502
24. Walther F, Eberlein-Gonska M, Hoffmann RT, Schmitt J, Blum S. Measuring appropriateness of diagnostic imaging: a scoping review. Insights Imaging. (2023) 14:62. doi: 10.1186/s13244-023-01409-6
25. van Dam L, Bretthauer M. Ethical issues in colorectal cancer screening. Best Pract Res Clin Gastroenterol. (2014) 28:315–26. doi: 10.1016/j.bpg.2014.03.002
26. Bowel Cancer UK. Never Too Young. Bowel Cancer UK. (2020). Available at: https://www.bowelcanceruk.org.uk/campaigning/never-too-young/ (accessed December 3, 2024).
27. Chima S, Reece JC, Milley K, Milton S, McIntosh JG, Emery JD. Decision support tools to improve cancer diagnostic decision making in primary care: a systematic review. Br J Gen Pract. (2019) 69:e809–18. doi: 10.3399/bjgp19X706745
28. Walter FM, Emery JD, Mendonca S, Hall N, Morris HC, Mills K, et al. Symptoms and patient factors associated with longer time to diagnosis for colorectal cancer: results from a prospective cohort study. Br J Cancer. (2016) 115:533–41. doi: 10.1038/bjc.2016.221
29. Staal J, Speelman M, Brand R, Alsma J, Zwaan L. Does a suggested diagnosis in a general practitioners' referral question impact diagnostic reasoning: an experimental study. BMC Med Educ. (2022) 22:256. doi: 10.1186/s12909-022-03325-7
30. Schmidt HG, Van Gog T, Schuit SC, Van den Berge K, Van Daele PL, Bueving H, et al. Do patients' disruptive behaviours influence the accuracy of a doctor's diagnosis? A randomised experiment. BMJ Qual Saf. (2017) 26:19–23. doi: 10.1136/bmjqs-2015-004109
31. Topol EJ. High-performance medicine: the convergence of human and artificial intelligence. Nat Med. (2019) 25:44–56. doi: 10.1038/s41591-018-0300-7
32. Abràmoff MD, Tarver ME, Loyo-Berrios N, Trujillo S, Char D, Obermeyer Z, et al. Considerations for addressing bias in artificial intelligence for health equity. NPJ Digital Med. (2023) 6:1–7. doi: 10.1038/s41746-023-00913-9
33. Seyyed-Kalantari L, Zhang H, McDermott MBA, Chen IY, Ghassemi M. Underdiagnosis bias of artificial intelligence algorithms applied to chest radiographs in under-served patient populations. Nat Med. (2021) 27:2176–82. doi: 10.1038/s41591-021-01595-0
34. Epstein RM, Franks P, Shields CG, Meldrum SC, Miller KN, Campbell TL, et al. Patient-centered communication and diagnostic testing. Ann Fam Med. (2005) 3:415–21. doi: 10.1370/afm.348
35. Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango). Soc Sci Med. (1997) 44:681–92. doi: 10.1016/S0277-9536(96)00221-3
36. Young B, Robb KA. Understanding patient factors to increase uptake of cancer screening: a review. Future Oncol. (2021) 17:3757–75. doi: 10.2217/fon-2020-1078
37. Mercer SW, Zhou Y, Humphris GM, McConnachie A, Bakhshi A, Bikker A, et al. Multimorbidity and socioeconomic deprivation in primary care consultations. Ann Fam Med. (2018) 16:127–31. doi: 10.1370/afm.2202
38. Sifaki-Pistolla D, Poimenaki V, Fotopoulou I, Saloustros E, Mavroudis D, Vamvakas L, et al. Significant rise of colorectal cancer incidence in younger adults and strong determinants: 30 years longitudinal differences between under and over 50s. Cancers. (2022) 14:4799. doi: 10.3390/cancers14194799
Keywords: early-onset cancer, diagnostic bias, primary care, cancer detection, patient compliance
Citation: Jerjes W and Harding D (2025) Breaking barriers: enhancing cancer detection in younger patients by overcoming diagnostic bias in primary care. Front. Med. 11:1438402. doi: 10.3389/fmed.2024.1438402
Received: 25 May 2024; Accepted: 30 December 2024;
Published: 22 January 2025.
Edited by:
Christos D Lionis, University of Crete, GreeceReviewed by:
Cecilia Acuti Martellucci, University of Ferrara, ItalyCopyright © 2025 Jerjes and Harding. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Waseem Jerjes, d2FzZWVtLmplcmplc0BuaHMubmV0
 Waseem Jerjes
Waseem Jerjes Daniel Harding1,2
Daniel Harding1,2