- Mayo Clinic, Rochester, MN, United States
Background: Nearly 30% of patients with COVID-19 infection develop post-COVID Syndrome. Knowledge of post-COVID Syndrome is evolving, creating the need for adaptable curricula. Flipped classrooms (FC) are flexible and dynamic with demonstrated utility in continuing medical education (CME), yet there has been no research on application of FCs, or comparisons between livestream and in-person learning, in post-COVID CME.
Methods: We implemented a novel post-COVID curriculum using FCs for in-person and livestream participants at four Mayo Clinic CME conferences. Outcomes were validated measures of knowledge; perceptions of FCs and CME teacher effectiveness; and learner engagement. Pre-conferences surveys were a post-COVID knowledge test and the Flipped Classroom Perception Inventory (FCPI). Post-conference surveys were a post-COVID knowledge test, the FCPI, the CME Teaching Effectiveness Instrument (CMETE), and the Learner Engagement Inventory (LEI). Pre-post knowledge and FCPI scores were analyzed using linear mixed models. CMETE and LEI were compared for in-person versus livestream participants using the Wilcoxon rank-sum test.
Results: Overall, 59 participants completed the pre-test, and 72 participants completed the post-test, surveys. Participants were predominantly female (58%), were in nonacademic group practices (65%), and lacked prior experience with flipped classrooms (83%). Following the presentations, participants showed significant improvements in post-COVID knowledge (47% correct precourse to 54% correct postcourse, p-value = 0.004), and a trend toward improved FCPI scores. Teaching effectiveness, learner engagement, and pre-post change in COVID knowledge did not differ significantly between participants of in-person versus livestream sessions.
Conclusion: This post-COVID FC curriculum was feasible and associated with improved knowledge scores among a diverse population of physician learners in CME, without any apparent compromise in learner engagement, or in perceptions of teaching effectiveness and FCs, among livestream versus in-person participants.
Background
Amidst the COVID pandemic there is an increased need for novel methods to disseminate rapidly evolving medical information effectively and safely (1–3). Post-COVID syndrome (PoCoS) is a constellation of symptoms persisting greater than three months after initial onset of acute COVID symptoms (4). PoCoS is characterized by fatigue, orthostatic intolerance, or diffuse pain disproportionate to objectively measured markers of tissue damage. In addition to being significantly function limiting, PoCoS is common, affecting an estimated 10–30% of patients with COVID (5, 6). Barriers to disseminating information on PoCoS include lack of standardized information, rapidly evolving data and treatment recommendations, and limited existing curricula.
There is growing interest in flipped classroom (FC) models as a flexible, dynamic, and accessible teaching modality to disseminate information safely, effectively, and rapidly during in the setting of the COVID pandemic. As opposed to traditional models, FC models require that course attendees prepare before class participation and then use face-to-face learning time to apply key concepts. FC models incorporate higher order Bloom’s taxonomy functions such as application, analysis, and evaluation in the face-to-face settings, which enhances opportunities for feedback and knowledge assessments (7–10).
Previously, FC models have been successfully studied and implemented at the Mayo Clinic through a QI curriculum for residents and in a CME setting primarily involving academic faculty members (11, 12). To our knowledge, utilization of FC methodologies in the setting of PoCoS curricula has not been studied.
Project design/methods
Setting: We conducted a cross-sectional survey with pre/post-test analyses of all participants at the post-COVID talks at the following Mayo Clinic CME events: The Practice of Internal Medicine Conference (POIM) on 3 May 2022, the Medically Unexplained Symptoms Conference on 18 August 2022, the Updates in Internal Medicine Conference on 22 October 2022, and the Medically Unexplained Symptoms Conference on 10 August 2023. These courses are all accredited by the Mayo School of Continuous Professional Development, range in attendance from 60 to 220 attendees, and qualify for between 19.5 and 26.25 h of CME credit. Each course consisted of 30 to 60-min podium presentations and small-group breakout sessions, and all courses were offered in both in-person and livestream formats. This study was deemed exempt by the Mayo Clinic Institutional Review Board (ID 21-012865).
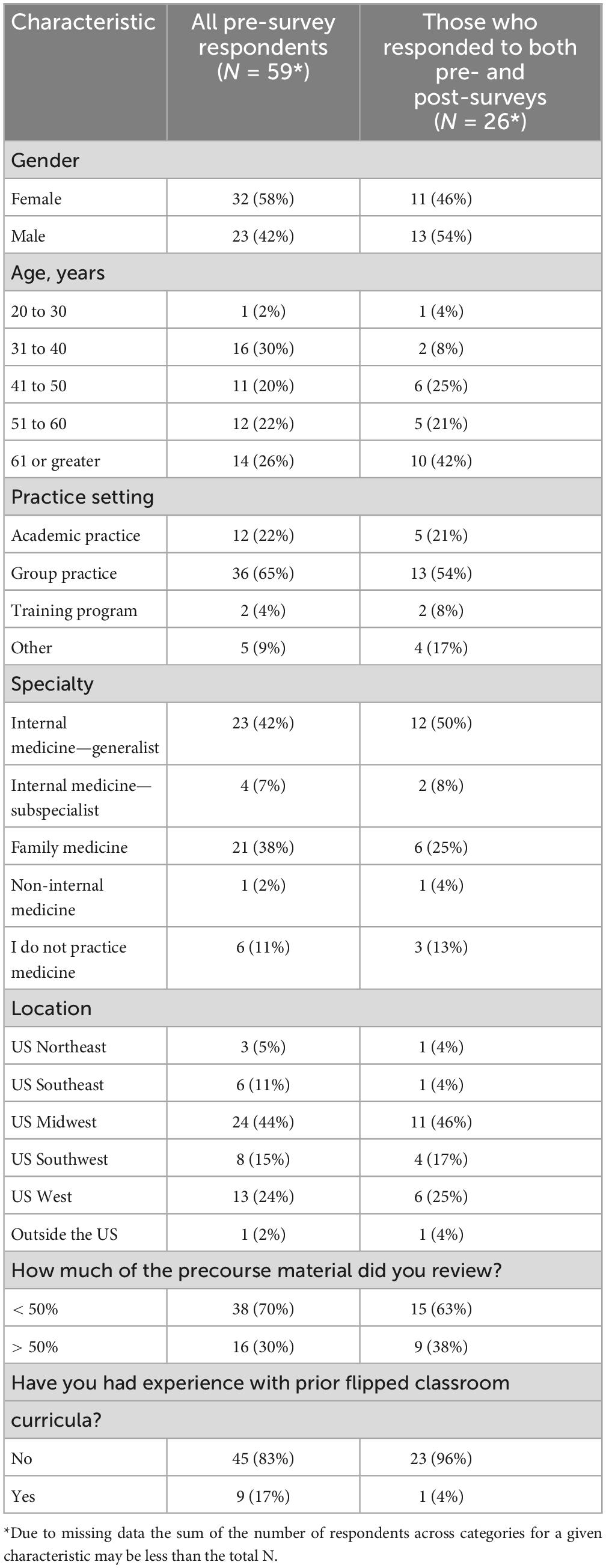
Study variables: Demographic variables of course participants, collected on the pre-survey, included age (years: 20–30, 31–40, 41–50, 51–60, ≥ 61), sex (M/F), practice setting (academic, group, training program, other), specialty (internal medicine, family medicine, medical specialty, non-medical specialty), practice location (northeast, southeast, midwest, southwest, west, international), pre-FC module completion (< 50%, ≥ 50%), and prior FC experience (Y/N). The outcome variables were a 10-item multiple choice post-COVID knowledge questionnaire, the 8-item Flipped Classroom Perception Inventory (FCPI), the 8-item CME Teaching Effectiveness Instrument, and the 8-item Learner Engagement Inventory (11, 13–15). Please see Supplementary Addendums 1–4 for the actual instruments.
Before the conference, participants received the multiple choice post-COVID knowledge questionnaire which was reviewed, revised, and updated for accuracy prior to each CME course. In addition, participants received the Flipped Classroom Perception Inventory (FCPI), which was designed to measure baseline knowledge and perceptions of flipped classroom curricula. After the conference, participants again received the multiple choice questionnaire. They also received the FCPI, the CME Teaching Effectiveness instrument, and Learner Engagement Inventory, all of which have been validated and published by Mayo authors (11, 13).
Study design: This was a two-group group, pre/post-test comparison study of a post-COVID curriculum using FCs among attendees at four Mayo Clinic CME courses.
Study intervention: Before the conference, participants were given access to online didactic materials reviewing key concepts to understanding post-COVID syndrome (see Supplementary Addendum 5 for a copy of the didactic material used). Modules were developed, reviewed, and revised by experts who designed and staff the Mayo Clinic Post COVID Care Clinic, and they were updated for accuracy prior to each CME course. The in-person conference presentation for post-COVID syndrome consisted of case-based presentations by the experts listed above, followed by a 30-s “think, pair, share” discussion among conference participants. Livestream participants were given a 30-s pause for reflection prior to proceeding to the next case.
Data analysis: Categorical data are presented as numbers and percentages. Continuous data are summarized as mean and SD. Knowledge and FCPI scores were analyzed using linear mixed models with time (pre vs. post) as the explanatory variable of interest and participant included as a random effect to account for the repeated measures design. These analyses were performed using all available data and also using data only for those who completed both the pre- and post-surveys. In order to assess whether changes from pre to post differed between those who attended in person versus livestream, a secondary analysis was performed which included mode of attendance (in person vs. livestream) and the mode of attendance—by—time interaction. CMETE and LEI were available for those who completed the post-survey and were compared for in-person versus livestream participants using the Wilcoxon rank-sum test. Statistical Significance was set at α < 0.05. Statistical analyses were conducted with SAS version 9.4 software (SAS Institute Inc., Cary, NC, USA).
Results
The pre-survey was completed by 59 participants and the post-survey was completed by 72 participants; with 26 participants completing both surveys. Demographics of those who completed the pre-survey are presented in Table 1. The majority of participants were from a group practice (65%), and most reported their specialty as internal medicine generalist (42%) or family medicine (38%).
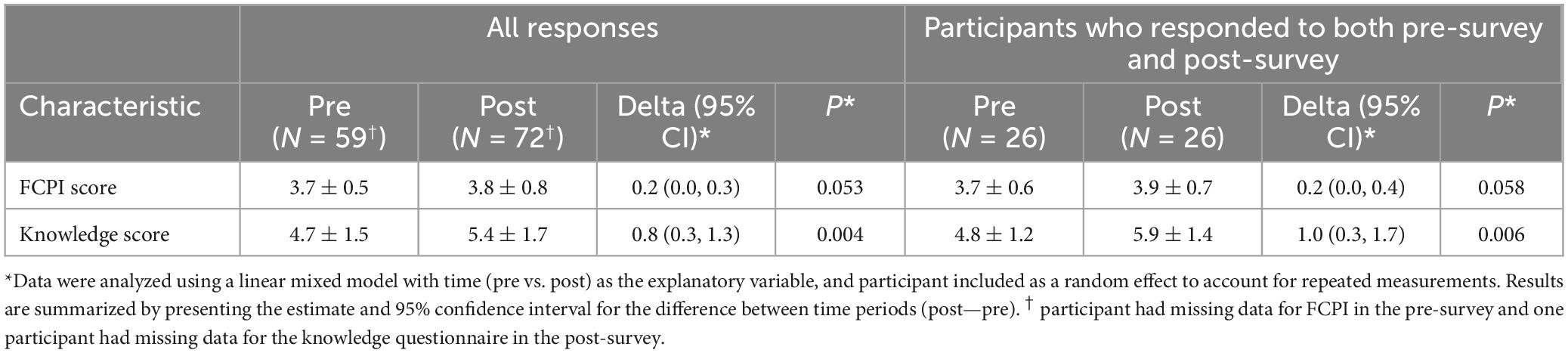
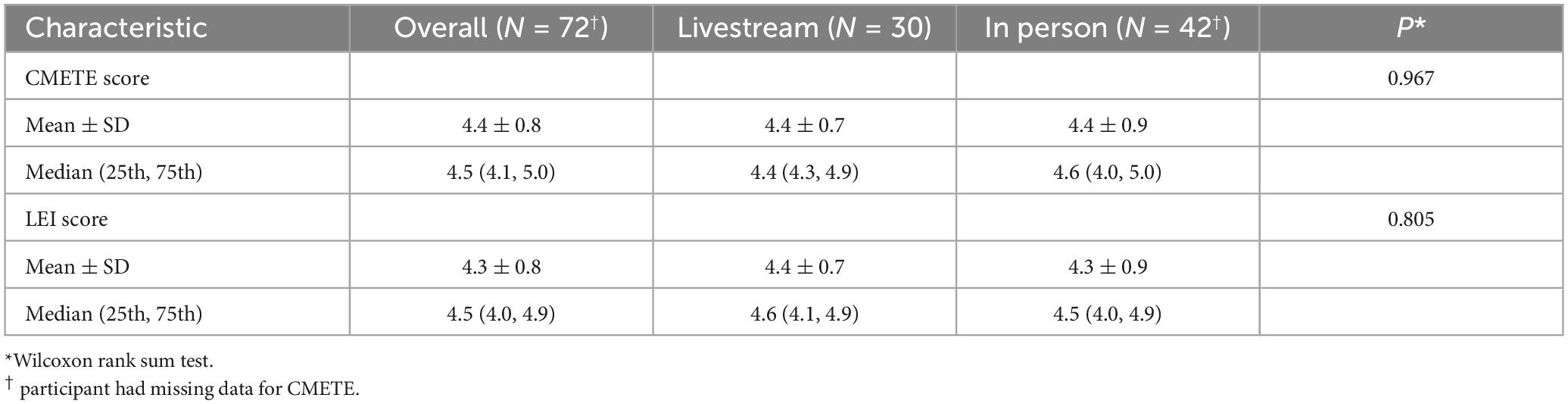
Results of the analyses of the FCPI and knowledge scores are summarized in Table 2. From the analysis which included all available data, the mean knowledge score increased significantly from pre to post (mean change = 0.8, 95% CI 0.3 to 1.3, p = 0.004), and the FCPI score was also observed to increase (mean change = 0.2, 95% CI 0.0 to 0.3, p = 0.053). Similar results were obtained from the analysis which was restricted to participants who completed both the pre- and post-surveys. From supplemental analysis, the changes from pre to post were not found to differ significantly between those who attended in person versus livestream (interaction p = 0.932 and p = 0.458 for knowledge and FCPI, respectively). For participants who completed the post-survey the CMETE and LEI scores are summarized in Table 3. For these outcomes, there were no significant differences found between those who attended in person versus livestream (P = 0.967 for CMETE score, p = 0.805 for LEI score).
Discussion
To our knowledge, this is the first study to demonstrate the feasibility and effectiveness of a post-COVID FC curriculum among postgraduate clinicians. The FC curriculum was associated with improved knowledge scores for both in person and livestream attendees. Furthermore, teaching effectiveness scores were not significantly different for in person versus livestream attendees, suggesting that this post-COVID FC curriculum is equally effective for distance learners.
Approximately 10 to 30% of patients with COVID-19 develop post-COVID Syndrome, which results in 2 to 4 million unemployed and $170 billion in lost wages annually in the United States (16–18). Few post-COVID curricula exist, and developing these curricula is challenging due to lack of standardization and rapidly evolving treatment recommendations (16), which highlights a need for post-COVID curricula that are effective, adaptable, and feasible.
We are unaware of previous curricula—let alone with the incorporation of FC methodology—for the management of post-COVID Syndrome. This curriculum was associated with similar knowledge gains for both in person and livestream models, and for attendees at multiple CME courses over 16 months, which speaks to the curriculum’s adaptability. Prior experience with FC models did not impact on knowledge gains. Finally, there was nonsignificant trend toward pre-post course perceptions of the FC approach, which is consistent with prior FC research (12).
Studies have suggested that learner engagement and teaching effectiveness are strongly correlated (13), and that in-person flipped classroom sessions are generally favored over online sessions (11, 12). However, this study did not reveal significant differences between in person versus livestream attendees with respect to teaching effectiveness or learner engagement scores, which indicates that, at least for this post-COVID FC curriculum, livestream attendance may be just as feasible and effective as the more resource intensive, in person sessions. Moreover, CME Teaching Effectiveness scores for this curriculum compared favorably with what was previously reported in the literature (15).
This study has several limitations. According to some traditional models, flipped classroom teachers interact with their students to check in, confirm understanding, and/or correct mistakes. A limitation of this study is that the instructors were teaching large audiences from the podium within strict time constraints, which precluded any informal interaction with the learners. Decreased learner engagement may have hampered the effectiveness of the extensive, precourse, FC learning materials. Future research should endeavor to improve learner engagement and satisfaction by implementing more streamlined course materials, and by offering greater incentives (19, 20). Participants were primarily older and practiced in nonacademic settings, which may limit the generalizability of flipped classroom data to other populations. The study relied on self-reporting of precourse material review, which could not be verified objectively. Moreover, although there were significant improvements in knowledge scores following the curriculum intervention, the absolute percentages correct on the knowledge assessments were not very high. Another potential explanation for the low knowledge scores is that that post-COVID syndrome is a very new and recent disorder; therefore, there remains little experience with this topic among general clinicians, and the pathophysiological mechanisms are still being determined. Finally, the surveys had generally low response rates.
In summary, we present the results of research on a novel post-COVID FC curriculum. The curriculum intervention was associated with increased pre-post knowledge scores, and with CME Teaching Effectiveness scores that compared favorably with prior CME research. Validated outcome measures for knowledge acquisition, teaching effectiveness, and learner engagement were similar for in person and livestream participants, suggesting that distance learning, which is less resource intensive, may be a feasible option for content delivery. We anticipate that future endeavors to streamline the precouse FC material will lead to further enhancements in knowledge acquisition and learner engagement.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Mayo Clinic Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
MM: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Visualization, Writing – original draft, Writing – review & editing. RG: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Visualization, Writing – original draft, Writing – review & editing. DS: Data curation, Formal analysis, Software, Writing – original draft, Writing – review & editing. TJB: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Visualization, Writing – original draft, Writing – review & editing.
Funding
The authors declare that financial support was received for the research, authorship, and/or publication of this article. Financial support for the development of this study and subsequent manuscript preparation was received from the Division of General Internal Medicine, Mayo Clinic, Rochester, Minnesota.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2024.1438068/full#supplementary-material
References
1. He L, Yang N, Xu L, Ping F, Li W, Sun Q, et al. Synchronous distance education vs traditional education for health science students: A systematic review and meta-analysis. Med Educ. (2021) 55:293–308. doi: 10.1111/medu.14364
2. Dedeilia A, Sotiropoulos M, Hanrahan J, Janga D, Dedeilias P, Sideris M. Medical and surgical education challenges and innovations in the COVID-19 era: A systematic review. In Vivo. (2020) 34:1603–11. doi: 10.21873/invivo.11950
3. Papapanou M, Routsi E, Tsamakis K, Fotis L, Marinos G, Lidoriki I, et al. Medical education challenges and innovations during COVID-19 pandemic. Postgrad Med J. (2021) 98:321–7. doi: 10.1136/postgradmedj-2021-140032
4. Bierle D, Aakre C, Grach S, Salonen B, Croghan I, Hurt R, et al. Central sensitization phenotypes in post acute sequelae of SARS-CoV-2 infection (PASC): Defining the post COVID syndrome. J Prim Care Community Health. (2021) 12:21501327211030826. doi: 10.1177/21501327211030826
5. Ganesh R, Grach S, Bierle D, Bierle D, Salonen B, Collins N, et al. The female predominant persistent immune dysregulation of the post COVID syndrome: A cohort study. medRxiv [Preprint] (2021). doi: 10.1101/2021.05.25.21257820 medRxiv:2021.05.25.21257820.
6. Ganesh R, Ghosh A, Nyman M, Croghan I, Grach S, Anstine C, et al. PROMIS scales for assessment of persistent post-COVID symptoms: A cross sectional study. J Prim Care Commun Health. (2021) 12:21501327211030413. doi: 10.1177/21501327211030413
7. Tolks D, Schäfer C, Raupach T, Kruse L, Sarikas A, Gerhardt-Szép S, et al. An introduction to the inverted/flipped classroom model in education and advanced training in medicine and in the healthcare professions. GMS J Med Educ. (2016) 33:Doc46. doi: 10.3205/zma001045
8. Chen F, Lui A, Martinelli SM. A systematic review of the effectiveness of flipped classrooms in medical education. Med Educ. (2017) 51:585–97. doi: 10.1111/medu.13272
9. Hernández-Guerra M, Quintero E, Morales-Arráez D, Carrillo-Pallarés A, Nicolás-Pérez D, Carrillo-Palau M, et al. Comparison of flipped learning and traditional lecture method for teaching digestive system diseases in undergraduate medicine: A prospective non-randomized controlled trial. Med Teach. (2021) 43:463–71. doi: 10.1080/0142159x.2020.1867312
10. de Vries T. Making confident and competent readers of cell, nature and science papers using a flipped classroom approach to introduce protein detection techniques. Front Educ. (2023) 8:1144010. doi: 10.3389/feduc.2023.1144010
11. Stephenson C, Wang A, Szostek J, Bonnes S, Ratelle J, Mahapatra S, et al. Flipping the continuing medical education classroom: Validating a measure of attendees’ perceptions. J Contin Educ Health Prof Fall. (2016) 36:256–62. doi: 10.1097/ceh.0000000000000113
12. Bonnes S, Ratelle J, Halvorsen A, Carter K, Hafdahl L, Wang A, et al. Flipping the quality improvement classroom in residency education. Acad Med. (2017) 92:101–7. doi: 10.1097/acm.0000000000001412
13. Stephenson C, Bonnes S, Sawatsky A, Richards L, Schleck C, Mandrekar J, et al. The relationship between learner engagement and teaching effectiveness: A novel assessment of student engagement in continuing medical education. BMC Med Educ. (2020) 20:403. doi: 10.1186/s12909-020-02331-x
14. Palmer B, Frye M, Vickers Douglas K, Staab J, Bright R, Schleck C, et al. Validation of a teaching effectiveness assessment in psychiatry continuing medical education. Acad Psychiatry. (2018) 42:458–63. doi: 10.1007/s40596-017-0763-8
15. Ratelle J, Wittich C, Yu R, Newman J, Jenkins S, Beckman T. Associations between teaching effectiveness scores and characteristics of presentations in hospital medicine continuing education. J Hosp Med. (2015) 10:569–73. doi: 10.1002/jhm.2391
16. Mueller M, Ganesh R, Hurt R, Beckman T. Post-COVID conditions. Mayo Clin Proc. (2023) 98:1071–8. doi: 10.1016/j.mayocp.2023.04.007
17. Logue J, Franko N, McCulloch D, McDonald D, Magedson A, Wolf C, et al. Sequelae in adults at 6 months after COVID-19 infection. JAMA Netw Open. (2021) 4:e210830. doi: 10.1001/jamanetworkopen.2021.0830
18. Bach K. New data shows long COVID is keeping as many as 4 million people out of work. Washington, DC: Brookings Institution (2022).
19. Nematollahi S, St John P, Adamas-Rappaport W. Lessons learned with a flipped classroom. Med Educ. (2015) 49:1143. doi: 10.1111/medu.12845
Keywords: flipped classroom, post-COVID “long-haulers,” in person learning, livestream learning, continuing medical education (CME)
Citation: Mueller M, Ganesh R, Schroeder D and Beckman TJ (2024) A post-COVID syndrome curriculum for continuing medical education (CME): in-person versus livestream. Front. Med. 11:1438068. doi: 10.3389/fmed.2024.1438068
Received: 24 May 2024; Accepted: 05 August 2024;
Published: 27 August 2024.
Edited by:
Ana L. S. Da Silva, Swansea University Medical School, United KingdomReviewed by:
Teun J. De Vries, VU Amsterdam, NetherlandsMenna Brown, Swansea University, United Kingdom
Copyright © 2024 Mueller, Ganesh, Schroeder and Beckman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Michael Mueller, bXVlbGxlci5taWNoYWVsQG1heW8uZWR1
 Michael Mueller
Michael Mueller Ravindra Ganesh
Ravindra Ganesh Thomas J. Beckman
Thomas J. Beckman