- 1Resident of Internal Department, Isfahan University of Medical Sciences, Isfahan, Iran
- 2Department of Internal Medicine, School of Medicine, Isfahan University of Medical Sciences, Isfahan, Iran
- 3Department of Community Medicine, School of Medicine, Isfahan University of Medical Sciences, Isfahan, Iran
- 4Isfahan Endocrine and Metabolism Research Center, Isfahan University of Medical Sciences, Isfahan, Iran
- 5Amin Hospital, Isfahan University of Medical Sciences, Isfahan, Iran
Background: Antimicrobial resistance (AMR) is one of the biggest threats to global public health systems. This study aimed to assess the knowledge, attitudes and practice about AMR, antimicrobial stewardship programs (ASPs) and multidrug-resistant (MDR) bacteria.
Methods: A web-based questionnaire survey was conducted among the residents of Isfahan University of Medical Sciences from May to November 2023. Data analysis was done using SPSS version 24.0 software.
Results: Overall, 400 out of 450 medical residents responded to the questionnaire, giving a response rate of 88.9%. The participants’ ages ranged from 26 to 54 years, and the majority were female (227/400 56.8%). Average scores for knowledge, attitudes, and practices were 53.70 ± 15.88, 36.97 ± 5.89 and 24.69 ± 4.24, respectively. In terms of knowledge, only 26.8% had heard the term “ASPs” and knew what it was. Most incorrect answers appeared to the treatment of infection caused by MDR bacteria including ESBL-producing Escherichia coli (27.8%) and carbapenem-resistant Klebsiella pneumoniae (30.8%), as well as the atypical bacteria (45.5%). Approximately, 50 and 71.7% said they had received no specific training in the fields of microbiological sampling methods and the appropriate time to prescribe antibiotics, respectively. Surprisingly, regarding practice, 81.8% of the respondents stated that antibiotics are used to treat flu or the common cold.
Conclusion: Residents considered their training on important issues including ASPs, MDR bacteria and the spectrum of antibiotics insufficient. This result highlights the need for targeted training interventions about antibiotic prescription in the curriculum at the university with more emphasis on ASPs to limit the development of resistance.
Introduction
Antimicrobial resistance (AMR) is one of the most serious public health concerns worldwide, posing a threat to the effective treatment of infectious diseases. AMR results in longer hospital stays, higher healthcare costs, higher mortality and higher medical resource consumption especially in low-income countries (1). It is estimated that a failure to address resistance to antibiotics would lead to approximately 10 million unnecessary deaths every year by 2050, resulting in projected economic costs as high as USD 100 trillion worldwide (2). The main factors associated with AMR in third-world countries include lack of sufficient knowledge and experience of clinicians, indeterminate diagnosis, inadequate dosage, use of antibiotics for non-bacterial infections, self-medication, over-prescription, incomplete treatment courses as well as poor infection control measures to prevent the spread of multidrug-resistant (MDR) bacteria in the hospitals (3, 4).
Iran has one of the highest rates of antibiotic consumption and resistance worldwide (5). The possible causes for this high consumption are related to the lack of knowledge about AMR, MDR pathogens and antimicrobial stewardship programs (ASPs), as well as the attitude and practices of physicians. Several knowledge, attitudes, and practices (KAP) surveys on antimicrobial resistance have been conducted among physicians, nurses and university students in both tertiary care and community settings (6–9). Understanding the KAP of the medical residents regarding antibiotics, antimicrobial stewardship and AMR is essential to developing targeted interventions and promoting appropriate antibiotic prescribing. Medical residents play a key role in the area of AMR when considering the inappropriate use or misuse of these agents. This is significantly more important when they are in charge of the administration and prescription of antibiotics in the hospitals and clinics where they work. Therefore, this population plays an important role in designing strategies that allow increasing awareness about the correct and rational use of antibiotics through communication and education.
In Iran, studies have shown high levels of antibiotic resistance in hospitals (10, 11), but published data assessing the KAP of medical residents toward AMR are absent. The present study aimed to investigate the medical residents’ KAP regarding antibiotics, antibiotic use and AMR in Iran to identify knowledge gaps and tailored educational interventions that could lead to wise use of antimicrobials and reduce the emergence of MDR organisms and their consequences.
Materials and methods
Study design and settings
A cross-sectional analytic online-based study was conducted to assess the KAP of medical residents toward AMR and MDR organisms and ASPs in academic hospitals (Isfahan University of Medical Sciences) in the center of Iran between May to November 2023. During this period, the medical residents are rotated through the different hospitals, which are relevant for their respective medical specializations. A web-based survey software (Google Forms) was used to collect data and that was voluntary and anonymous.
Study population
The Medical University of Isfahan (MUI) is one of the major public universities in Iran; every year, many specialists from all fields graduate from it. During the study period, the university had 450 medical residents. The sample size was determined by using Epi-info software. For a confidence level of 95%, the sample size equal to 450. The term “medical residents” referred to physicians after qualification from medical school who were still in their training years for a specialty. An electronic invitation letter including a link to the survey was sent to 450 residents from the first year to the fourth year in various specialties including Internal Medicine, Infectious Diseases, Orthopedic Surgery, General Surgery, Gynecology, Neurology, Neurosurgery, Urology, Cardiology, Pediatric, and ENT. During the period the survey remained open, medical residents received 3 reminders (email or call) to get the maximum number of participants. Due to the large number of subspecialties of residents and the meaningless analysis of each specialist separately, we had to categorize them into similar groups based on the amount of exposure of each resident’s group with antibiotic prescription. Our justification for such a division was our expectation of the similarity of antibiotic knowledge of these groups as follows:
Group 1 (Internalist, Infectious, Pediatric, N = 116): This group had the most exposure to the prescription of antibiotics. They were the group who visited many patients with medical problems every day. Group 2 (Cardiologist, Neurologist, N = 98): This group also faced medical problems in their patients, but they usually did not face the routine prescription of antibiotics. Group 3 (Orthopedist, Neurosurgeon, Urologist, ENT, N = 105): This group was the category of minor surgeries, which were usually faced with a limited field, and their patients experienced fewer complications from infection due to the limited surgical field. Group 4 (Gynecologist, Surgeon, N = 81): They were the group of major surgeries with extensive surgical sites.
Exclusion criteria
Due to the lack of antibiotic prescription during the residency, groups such as radiology, psychology, physical medicine and rehabilitation, skin, nuclear, emergency medicine, anesthesia, ophthalmology, radio-oncology, and pathology were excluded from the study.
Questionnaire design
A structured questionnaire was developed after a literature review of similar studies (12–14), and in consultation with relevant experts from the field of bacteriology and statistics. The questionnaire included two parts. In the first part, questions are about demographics and general information about residents, such as their Gender, year of study, and specialty. The second part had 31 questions including three sections: (1) 11 questions in a 2-level Likert scale to evaluate the knowledge of students about issues. In more detail, knowledge questions are related to identifying antibiotics, antibiotic role, antibiotic side effects, and awareness of antibiotic resistance. (2) The second section comprised 12 questions to assess the attitudes and perceptions toward AMR and MDR organisms and ASPs. (3) The last part of the questionnaire included eight questions on practices ranging from the participant’s awareness of the pattern of AMR at their workplace hospitals, proper use of international and local antibiotics guidelines, and consultation with infectious disease specialists. The attitude and practice questions have been designed on a 5-level Likert scale from 1 (completely disagree) to 5 (completely agree). The goal of the questionnaire was introduced to 450 voluntary participants and their agreement was reached before filling in the questionnaire. To evaluate the face validity of the questionnaire, five specialists assessed and commented on the appropriateness and clarity of the questions. The Content Validity Ratio (CVR) and the Content Validity Index (CVI) were used for the content validity analysis. The minimum acceptable value for CVR is 0.99 when the number of experts is five and the acceptable value for CVI is 0.79. The result of CVR and CVI shows all items are appropriate. The reliability of the questionnaire was assessed by calculating Cronbach’s alpha. The Cronbach’s alpha (0.711) demonstrated good reliability.
Data analysis
Each survey response was considered valid if more than 80% of questions (25 or more) had been answered. After collecting valid responses, Data were analyzed by using SPSS version 24 software. Statistical analysis, including the descriptive method, Chi-square and Fisher’s exact test was implemented on the total answers of respondents. The relation of participants’ knowledge, attitude, and practice with their sociodemographic features (age, gender, specialty) were compared and analyzed using the Mann–Whitney U test and Kruskall-Wallis H test.
Results
Demographic characteristics
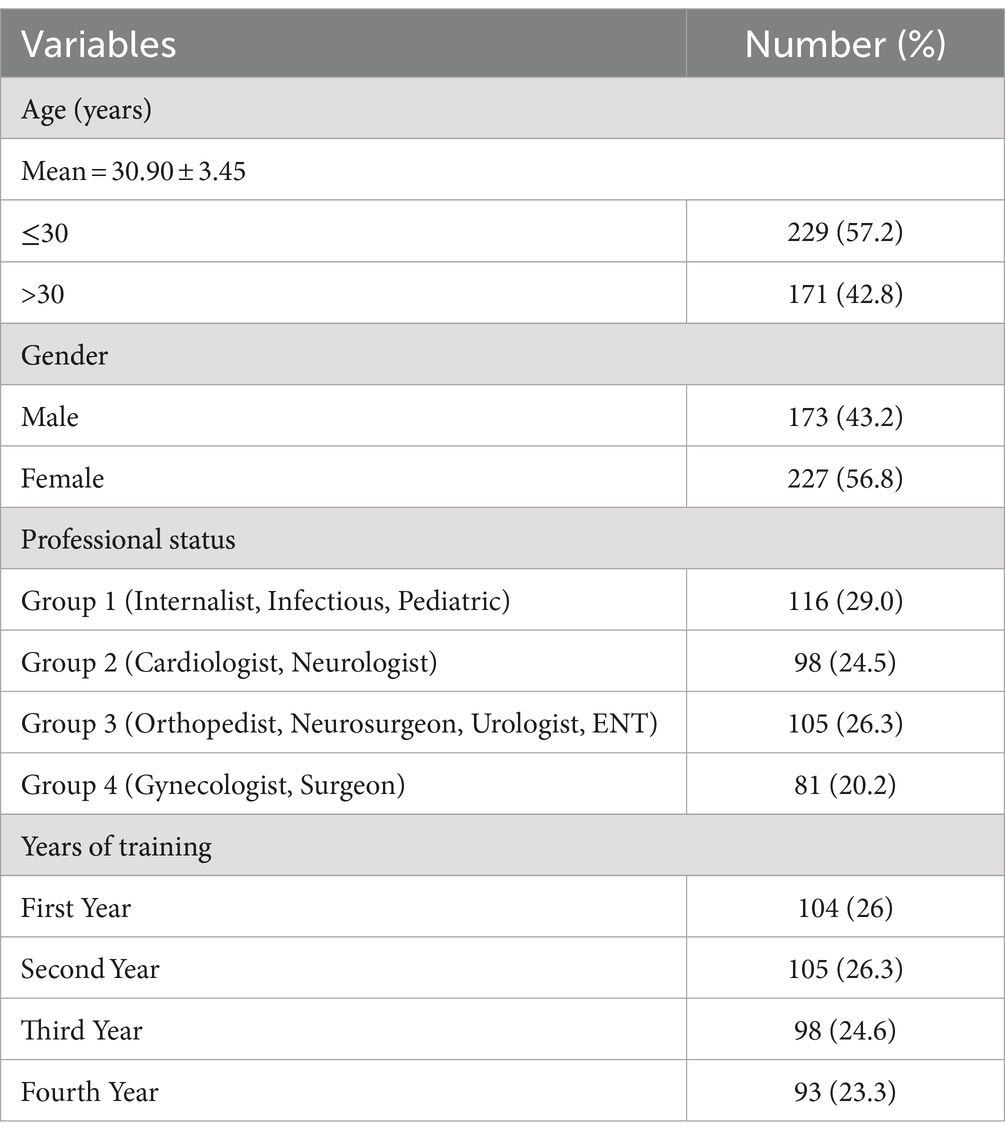
During the study period, out of 450 potential respondents, 400 responded and completed the questionnaires (response rate; 88.9%). Table 1 shows details on demographic characteristics of the study participants. Their age ranged from 26 to 54 years and 227 (56.8%) participants were females. The mean age of respondents was 30.90 ± 3.45 years and most of them, 229 (57.2%) were smaller or equal to 30 years. Participants were divided into four groups based on their field and the year of their university entrance, respectively. The largest group of respondents was group-1116 (29.0%), which included internal medicine, infectious, and pediatric residents. One hundred and four (26%) of the residents were in their first year of training, 105 (26.3%) in their second, 98 (24.6%) in their third, and 93 (23.3%) in their fourth or longer.
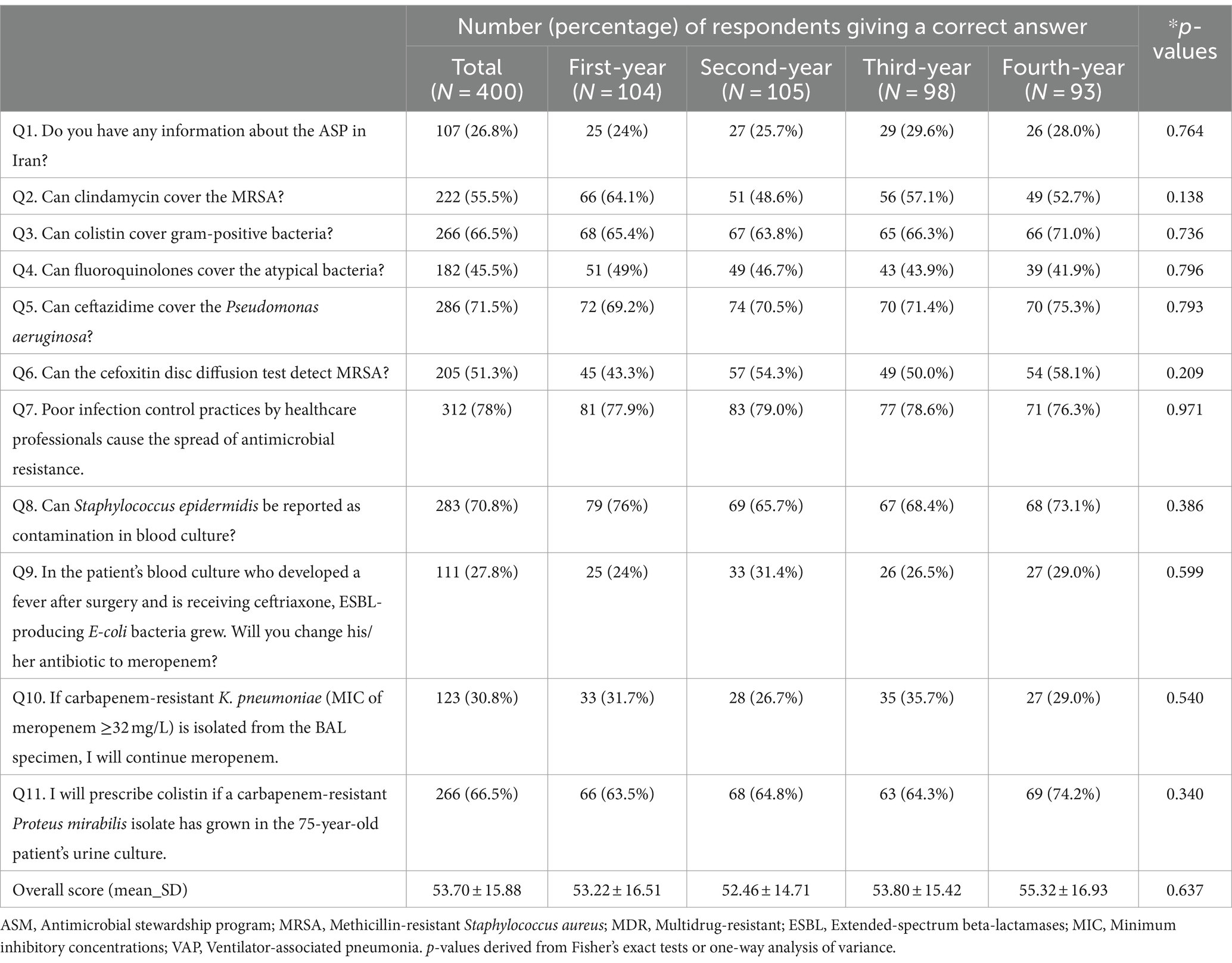
Medical residents’ knowledge
Data from 11 knowledge questions were analyzed according to two topics: (1) based on the professional status of participants, and (2) based on the participants’ years of entering the university. The responses to knowledge items were presented in Tables 1, 2. Overall, the average knowledge score among participants was 53.70 ± 15.88 in a 100-point scale. Approximately three-quarters of the participants (293/400, 73.2%) lacked awareness about the antimicrobial stewardship program in Iran.
The majority (286/400, 71.5%) of respondents correctly answered to appropriate coverage of ceftazidime to Pseudomonas aeruginosa. Nearly all the participants (312/400, 78%) expressed to importance of the infection control process in hospitals to decrease the spread of MDR bacteria. Most incorrect answers appeared to the treatment of blood infection caused by ESBL-producing Escherichia coli (Q9, 27.8%), followed by continuing the treatment of a patient with a lung infection caused by carbapenem-resistant Klebsiella pneumoniae with a MIC of meropenem ≥32 mg/L (Q10, 30.8%), and fluoroquinolone prescriptions for cover the atypical bacteria (Q4, 45.5%).
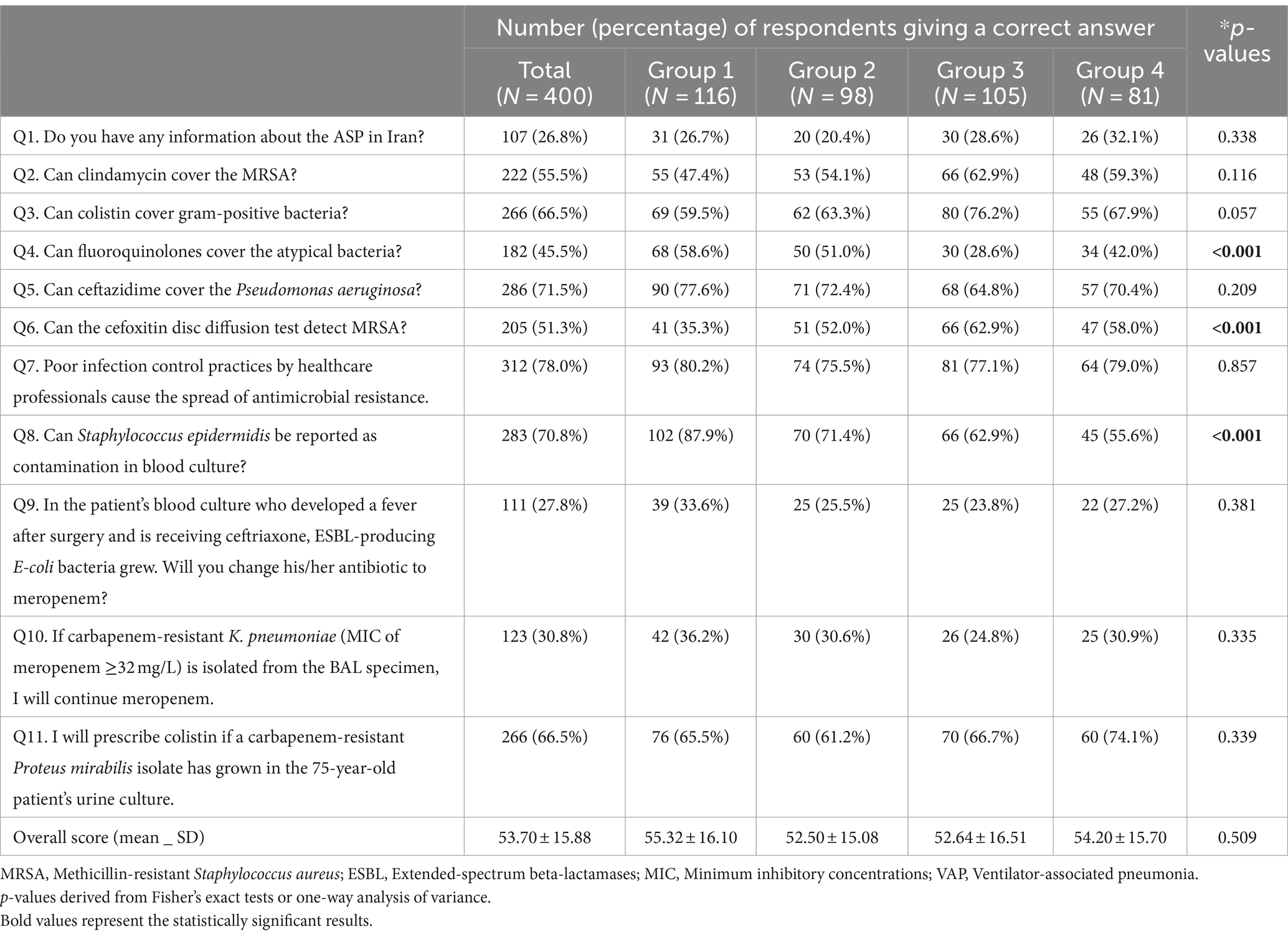
As it is described in Table 3, according to the p-values of Q4, 6 and 8, there is a remarkable difference between answers of four groups. Regarding the question of covering atypical bacteria with fluoroquinolones, the highest and lowest percentage of correct answers belonged to groups 1 (68/116, 58.6%) and 3 (30/105, 28.6%), respectively. Also, regarding the use of cefoxitin disc diffusion test to detect methicillin-resistant Staphylococcus aureus (MRSA), the lowest (35.3%) and highest (62.9%) correct answers were observed in groups 3 and 1, respectively. A notable percentage of group 1 (87.9%) selected the correct answer to the question about the possibility of blood culture contamination with Staphylococcus epidermidis, and the lowest percentage of correct answers to this question belonged to group 4 with 55%. More than half of the participants were mindful of the coverage of colistin and its intrinsic resistance to some bacterial strains like Proteus mirabilis.
Medical residents’ attitude
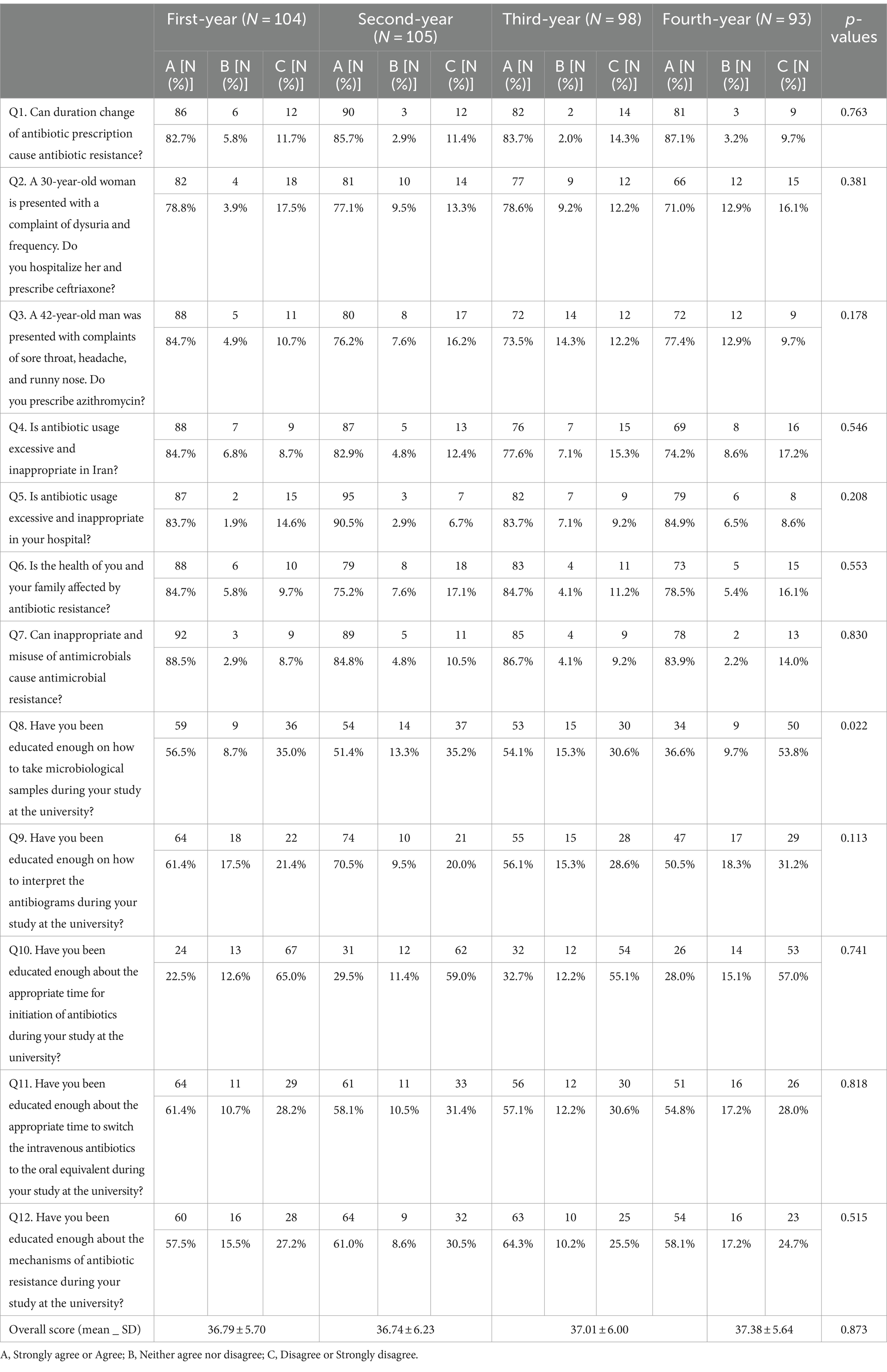
Data from 12 attitude questions were analyzed according to two topics: (1) based on the professional status of participants, and (2) based on the participants’ years of entering the university.
Tables 4, 5 present the levels of attitudes toward AMR and MDR organisms and ASPs among the study participants. The average attitude score among participants was 36.97 ± 5.89 on a 60-point scale.
Nearly 86% (344/400) of the respondents agreed or strongly agreed that an inappropriate use of antimicrobials could cause antimicrobial resistance. The great majority of respondents (85.8%, 343/400) admitted that antibiotic prescriptions are excessive and inappropriate in their workplace hospitals. When participants were asked about getting enough information about the appropriate time to start antibiotics at the university, only 28.3% (113/400) of respondents agreed or strongly agreed that they were given enough information. When respondents were asked about how to take microbiological samples, exactly 50% (200/400) stated that they had not learned about microbiological sampling during their degree courses. As it is shown in Table 4, only Q8 has a p-value<0.05 and so in this question, there is a remarkable difference between answers of different years. As can be depicted from Table 5, according to the p-values (<0.05) of Q2, 3, 4, 8 and 11, there is a remarkable difference between the answers of the four groups.
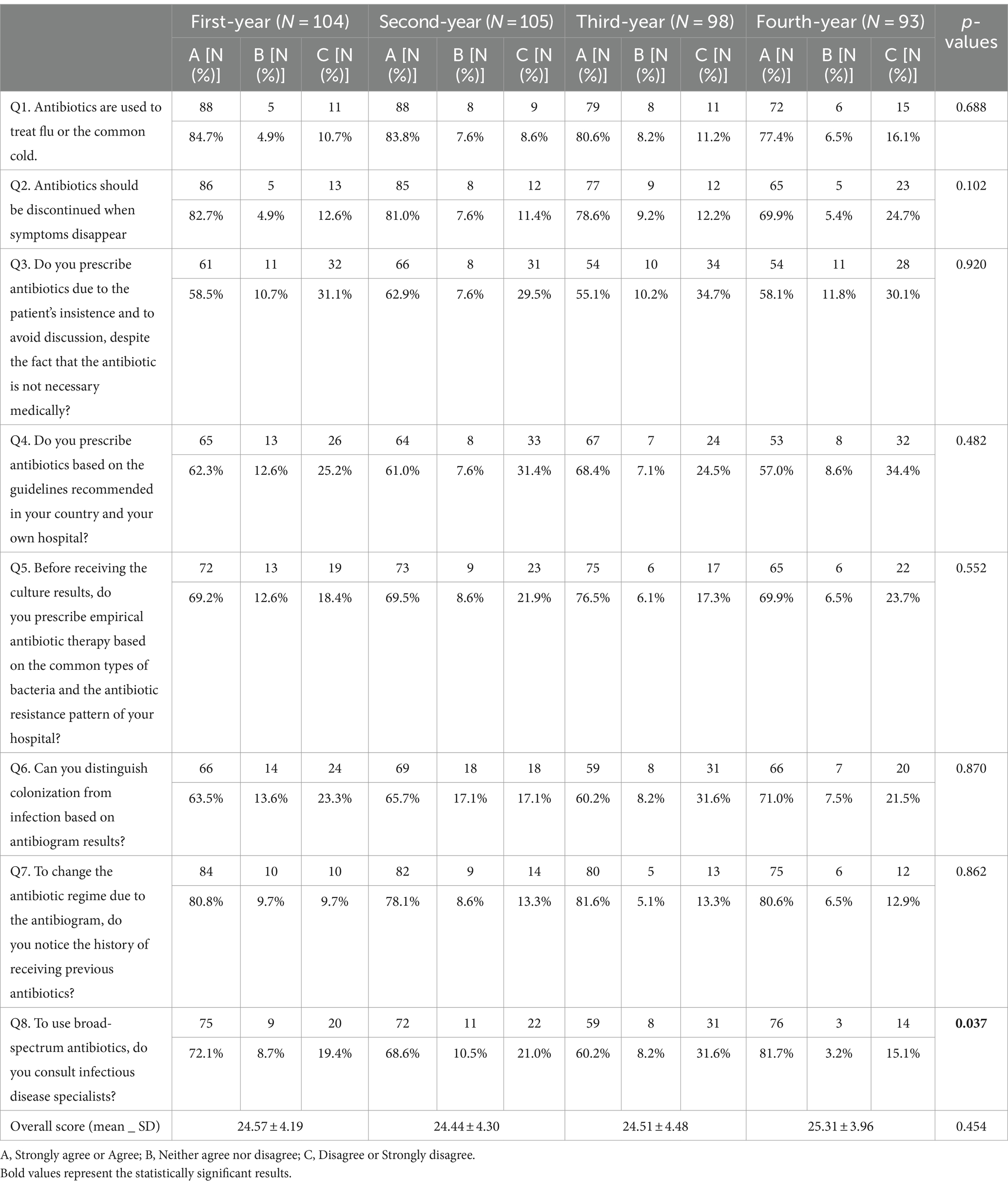
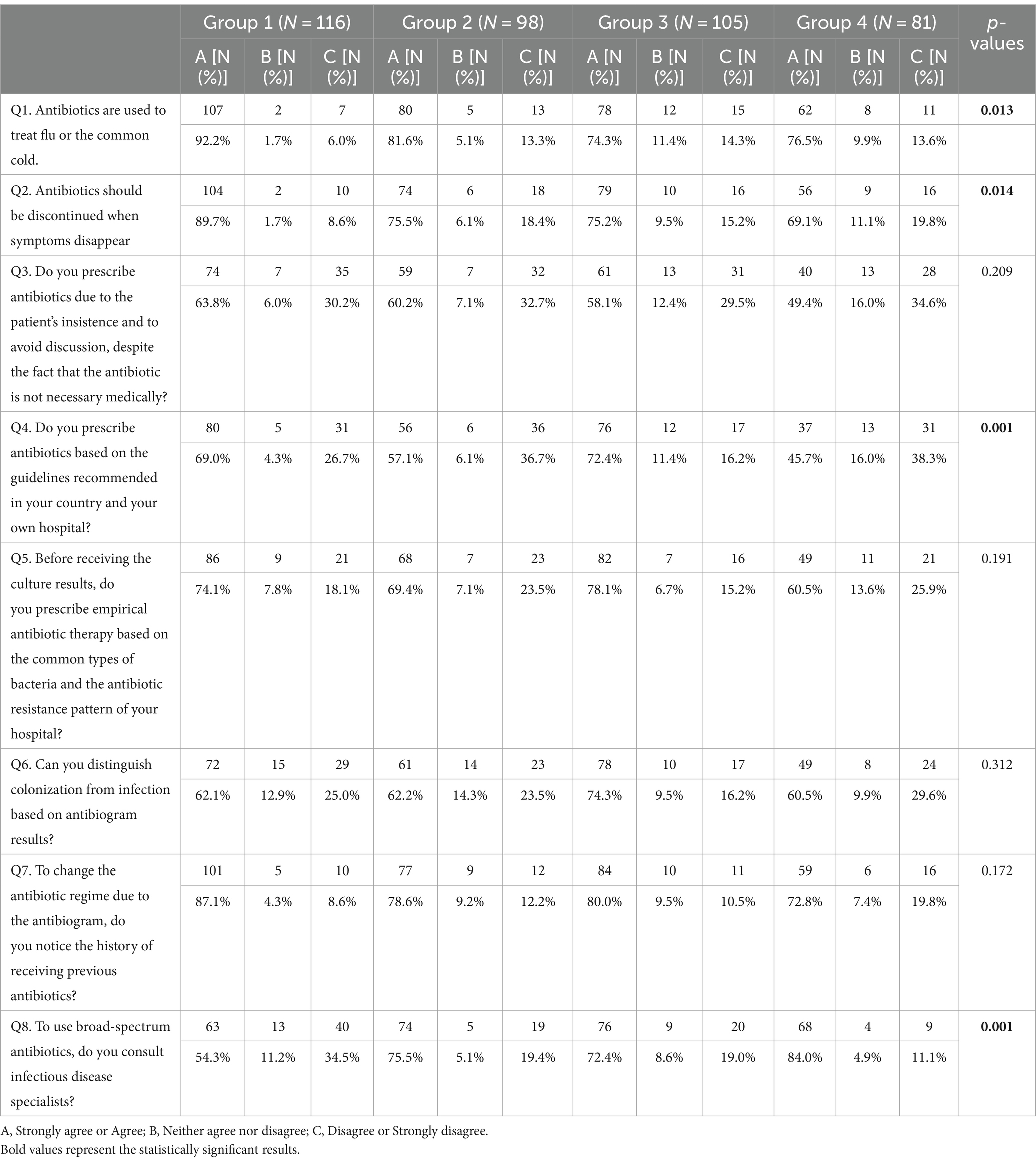
Medical residents’ practice
Data from eight practice questions were analyzed. Overall, the average practice score among participants was 24.69 ± 4.24 on a 40-point scale. Regarding practice, 81.8% (327/400) of the respondents stated that antibiotics are used to treat flu or the common cold, 78.3% (313/400) stated that antibiotics should be discontinued when symptoms disappear, 58.8% stated that they prescribe antibiotics because of the patient’s insistence, 62.3% (249/400) stated that they prescribe antibiotics according to the guidelines, 71.3% (285/400) stated that they prescribe antibiotics before preparing the microbiology culture results based on the local antibiotic resistance pattern, 65% (260/400) stated that before changing antibiotics, they differentiate colonization from infection based on the results of microbial culture, 80.3% (321/400) stated that before the antibiotic change, based on antibiogram result, they pay attention to the types of antibiotics the patient received previously and 70.5% they consult with infectious disease specialists to using of broad-spectrum antibiotics.
Table 6 shows only question 8 has a p-value <0.05 and so in this question, there is a significant difference between answers of different years of training. As shown in Table 7, questions 1, 2, 4, and 8 have p-value<0.05 and so in these questions there are significant differences between answers of different groups.
Discussion
The increase in AMR is a major threat to public health in the 21st century. Medical professionals are the key stakeholders in the prevention and control of AMR through strict and effective prescribing practices, promoting awareness of ASPs and antibiotic resistance mechanisms, as well as they are the cornerstone of good health systems.
To the best of our knowledge, this is the first such study conducted among Iranian medical residents. The present study was conducted among the medical residents of Isfahan University of Medical Sciences toward AMR and MDR organisms and ASPs, as they are the key prescribers of antibiotics during their studies in medical-educational centers of Iran. There are few published studies around the world about the KAP regarding these topics among medical residents (15, 16). However, some previous studies evaluated the KAP in general practitioners, medical students and specialists (6–8). To date, there is no other study that attempted to address this topic in the country except one (7). It should be noted that this study is different from that paper since it assesses other issues in addition to the prescription of antibiotics and includes only medical residents.
This report revealed low levels of knowledge in the study respondents. The respondents scored on average 53.70 ± 15.88% correct answers regarding AMR and MDR organisms and ASPs. Similarly, a study showed that 55% the Chinese medical doctors had low levels of knowledge about antibiotic prescriptions (12). On the other hand, proper knowledge was observed in a study conducted among South Indian medical students (17).
Although knowledge of the ASPs is necessary for the residents, the majority of our respondents (73.2%) declared that they did not know what antimicrobial stewardship meant and it was not taught during the 4 years of their study because the knowledge has not changed in years. The average age of our statistical population was 30.9-year-old physicians who worked in hospitals and clinics before starting residency and unfortunately, despite working in the clinical environment, they did not know the program. The gaps identified in knowledge among our residents regarding ASPs require heightened educational interventions and these activities could be targeted. Therefore, we recommended reinforcing the curriculum by introducing more lectures on ASPs. Some countries, such as France, the United States and Scotland, have developed a national recommendations program to improve antibiotic stewardship in their countries (4).
Amazingly, only 45.5% of the respondents answered correctly that quinolones provide exceptional coverage against atypical pathogens. Notably, 28.6% of group 3 were aware that fluoroquinolones can cover the atypical bacteria, which is very low compared to other groups. It was expected that the knowledge would increase based on the years of education and that the first group compared to other groups would be different due to their daily involvement with antibiotics. Low levels of knowledge about the levofloxacin spectrum were documented among the clinicians in Pakistan and only 20% correctly identified it to be effective against atypical bacteria (4). Our result revealed that there were no significant differences in the knowledge among the residents based on the professional status of participants and participants’ years of entering the university. This is probably due to the lack of AMR knowledge transfer from professors to residents. In fact, the knowledge transfer chain is incomplete because these same residents become professors after graduation.
MRSA is an important human pathogen that causes a wide variety of community-and health care-associated infections. Accuracy and promptness in the detection of meticillin resistance using disk diffusion testing with oxacillin or cefoxitin are of fundamental importance in ensuring correct antibiotic treatment in patients and control of MRSA in the hospital (18). The results of our study showed that only 51.3% of our residents knew that cefoxitin disc is used to identify bacteria.
In a review study (19), it has been shown that coagulase-negative staphylococci are the most commonly isolated bacteria in blood cultures, and is mostly regarded as contamination. Therefore, differentiating infection from contamination in blood culture leads to the correct decision to prescribe antibiotics for the patient. In the present study, 29.2% of the residents were not aware that the S. epidermidis isolated from the blood culture may be contamination, which will lead to the incorrect prescription of antibiotics.
In our study, the majority of respondents 80 and 85.8% stated that antibiotics were used inappropriately in Iran and their workplace hospitals, respectively. This is consistent with previous studies (20, 21). In contrast, in Ghana, the majority of the respondent physicians answered that antibiotics were used appropriately in their units or departments (13).
The inappropriate use and overprescribing of antibiotics are a serious and long-standing challenge in Iran’s health system. According to the annual report of the health department of Iran’s Health Ministry, our country has reported high resistance rates in the bacteria of international concern such as MRSA (49%), vancomycin-resistant enterococci (VRE; 59%), Escherichia coli [resistance to third-generation cephalosporins (41%), or fluoroquinolones (54%)], Klebsiella pneumoniae [resistance to third-generation cephalosporins (83%), or carbapenems (69%)] and Acinetobacter baumannii [resistance to carbapenems (93%)]. Despite the restrictions to the initial prescription of some antibiotics such as carbapenems, colistin, linezolid and vancomycin which is a common measure in Iranian hospitals, we are witnessing an increase in antibiotic resistance day by day. It seems that Iranian residents have significant gaps in knowledge regarding AMR, ASPs and MDR pathogens especially extended-spectrum β-lactamase (ESBL)- and carbapenemase-producing bacteria. Our participant believed they were taught acceptably during their study about the interpretation of the cultures, the change of intravenous antibiotics to the oral types, and the mechanism of bacterial resistance. This is although, from their point of view, their information about how to start antibiotics was less. According to the reported knowledge, it does not seem that their attitude about their education was correct.
Thus, as with many other countries (9, 22, 23), it is crucial to develop appropriate curricula to teach the goals of ASPs, antibiotic resistance mechanisms, correct and prudent and timely antibiotic use to university medical residents. The percentage of residents giving the right answer for the management of ESBL bacteremia was 27.8%. Also, the low percentage (30.8%) of awareness about carbapenems and their resistance may be due to a lack of adequate education programs regarding the mechanisms of antibiotic resistance. A greater proportion (78%) of our respondents stated that they would prescribe azithromycin to a patient with symptoms such as sore throat, headache, and runny nose. This finding is consistent with previous study conducted in Zambia (21) that reported antibiotics can be used to treat cough, sore throat and colds. Our study showed that our residents were significantly associated with antibiotic use for cold. Although ceftriaxone is not effective in the treatment of cystitis, nor is azithromycin in the treatment of the common cold, a large percentage of our participants agree with prescribing these two. The indiscriminate prescription of these two common drugs can be a sign of the inappropriate prescription of antibiotics by physicians, which has led to the ineffectiveness of these two in the treatment of the disease.
Regarding the knowledge, the study found that the majority of the population (80.8%) stated that antibiotic resistance can impact their health and that of their families. A similar finding was found in a study conducted among the public in Cyprus, where 76.4% of respondents were concerned about the impact of resistance on the health of individuals and their families (24). Interestingly, the majority of our residents (72%) agreed that they did not get the necessary information about the right time to prescribe antibiotics during their university courses. Therefore, these results showed that there is a lack of sufficient training on antibiotic prescribing during education and pharmaceutical promotional activities in Iranian universities. It seems that prescribing antibiotics is a concern for residents and the need for infectious consultation to prescribe is felt, and they also try to use national and hospital guidelines.
Our study has some potential limitations. At first, it was conducted only at the Medical University of Isfahan and may not be a representative sample. Secondly, as with most surveys, there is the possibility that respondent residents obtained answers to some of the knowledge questions through Internet searches or literature reviews. Because in reality, it seems that their knowledge about some questions is less than the reported values.
Conclusion
The present study highlighted the gaps in knowledge, attitude and practices of the residents regarding AMR, ASPs and MDR pathogens. The overall average knowledge score among residents was 53.70 ± 15.88. Group 1, which is the main antibiotic prescribing group, had an average score of 55.32 ± 16.10, which was not significantly different from the other three groups. As well, based on the year of entering the university, we see that the residents’ knowledge (Table 2) and attitude (Table 4) about the mentioned topics does not increase during 4 years, even in some cases, the knowledge has decreased. These findings indicate that education and intervention activities including reviewing the curricula and introducing the course of mechanisms of antibiotic resistance and ASPs in residents’ curricula are necessary to increase knowledge, promote responsible antibiotic use, and combat the growing threat of AMR.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The study was approved by the Research and Ethics Committee of MUI (IR.MUI.MED.REC.1401.323) and the guidelines of the Declaration of Helsinki. All participants were briefed and gave their verbal consent to participate in the study and confidentiality ensured. Informed consent was waived because our study was a descriptive, non-interventional one.
Author contributions
FK: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. GS: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. NM: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Writing – original draft, Writing – review & editing. MS: Methodology, Validation, Writing – original draft, Writing – review & editing. HS: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was funded by the Isfahan University of Medical Sciences (No. 3401403).
Acknowledgments
The authors express their gratitude to the respondents who participated in the survey by providing their valuable time.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Touat, M, Brun-Buisson, C, Opatowski, M, Salomon, J, Guillemot, D, Tuppin, P, et al. Costs and outcomes of 1-year post-discharge care trajectories of patients admitted with infection due to antibiotic-resistant bacteria. J Inf Secur. (2021) 82:339–45. doi: 10.1016/j.jinf.2021.02.001
2. O'Neill, J, and Grande-Bretagne,. Antimicrobial resistance: tackling a crisis for the health and wealth of nations; the review on antimicrobial resistance: London, UK. J Antimicrobial Resistance. (2014)
3. Precha, N, Sukmai, S, Hengbaru, M, Chekoh, M, Laohaprapanon, S, Makkaew, P, et al. Knowledge, attitudes, and practices regarding antibiotic use and resistance among health science and non-health science university students in Thailand. PLoS One. (2024) 19:e0296822. doi: 10.1371/journal.pone.0296822
4. Ashraf, S, Ashraf, S, Ashraf, M, Imran, MA, Choudhary, ZA, Hafsa, HT, et al. Knowledge, attitude, and practice of clinicians about antimicrobial stewardship and resistance among hospitals of Pakistan: a multicenter cross-sectional study. Environ Sci Pollut Res Int. (2022) 29:8382–92. doi: 10.1007/s11356-021-16178-2
5. Browne, AJ, Chipeta, MG, Haines-Woodhouse, G, Kumaran, EPA, Hamadani, BHK, Zaraa, S, et al. Global antibiotic consumption and usage in humans, 2000-18: a spatial modelling study. Lancet Planet Health. (2021) 5:e893–904. doi: 10.1016/S2542-5196(21)00280-1
6. Zainaghi, I, Cilluffo, S, and Lusignani, M. Knowledge, attitudes, and practices related to antibiotic resistance among physicians and nurses in Italian intensive care: a multicenter cross-sectional survey. J Glob Antimicrob Resist. (2024) 36:460–5. doi: 10.1016/j.jgar.2023.10.022
7. Sami, R, Sadegh, R, Fani, F, Atashi, V, and Solgi, H. Assessing the knowledge, attitudes and practices of physicians on antibiotic use and antimicrobial resistance in Iran: a cross-sectional survey. J Pharm Policy Pract. (2022) 15:82. doi: 10.1186/s40545-022-00484-2
8. Min, S, Zhou, Y, Sun, Y, Ye, J, Dong, Y, Wang, X, et al. Knowledge, attitude, and practice associated with antimicrobial resistance among medical students between 2017 and 2022: a survey in East China. Front Public Health. (2022) 10:1010582. doi: 10.3389/fpubh.2022.1010582
9. Lagadinou, M, Tsami, E, Deligakis, A, Paraskevas, T, Michailides, C, Velissaris, D, et al. Knowledge and attitudes of healthcare workers towards antibiotic use and antimicrobial resistance in two major tertiary hospitals in Western Greece. Antibiotics (Basel). (2023) 12:1–9. doi: 10.3390/antibiotics12111583
10. Sanikhani, R, Akbari, M, Hosseinzadeh, M, Siavash, M, Badmasti, F, and Solgi, H. Outbreak of colistin and carbapenem-resistant Klebsiella pneumoniae ST16 co-producing NDM-1 and OXA-48 isolates in an Iranian hospital. BMC Microbiol. (2024) 24:59. doi: 10.1186/s12866-024-03207-6
11. Khoshbakht, R, Kabiri, M, Neshani, A, Khaksari, MN, Sadrzadeh, SM, Mousavi, SM, et al. Assessment of antibiotic resistance changes during the Covid-19 pandemic in northeast of Iran during 2020–2022: an epidemiological study. Antimicrob Resist Infect Control. (2022) 11:121. doi: 10.1186/s13756-022-01159-y
12. Liu, C, Liu, C, Wang, D, and Zhang, X. Knowledge, attitudes and intentions to prescribe antibiotics: a structural equation modeling study of primary care institutions in Hubei, China. Int J Environ Res Public Health. (2019) 16:1–16. doi: 10.3390/ijerph16132385
13. Labi, AK, Obeng-Nkrumah, N, Bjerrum, S, Aryee, NAA, Ofori-Adjei, YA, Yawson, AE, et al. Physicians' knowledge, attitudes, and perceptions concerning antibiotic resistance: a survey in a Ghanaian tertiary care hospital. BMC Health Serv Res. (2018) 18:126. doi: 10.1186/s12913-018-2899-y
14. Nisabwe, L, Brice, H, Umuhire, MC, Gwira, O, Harelimana, JD, Nzeyimana, Z, et al. Knowledge and attitudes towards antibiotic use and resistance among undergraduate healthcare students at University of Rwanda. J Pharm Policy Pract. (2020) 13:7. doi: 10.1186/s40545-020-00207-5
15. Abbo, L, Sinkowitz-Cochran, R, Smith, L, Ariza-Heredia, E, Gómez-Marín, O, Srinivasan, A, et al. Faculty and resident physicians' attitudes, perceptions, and knowledge about antimicrobial use and resistance. Infect Control Hosp Epidemiol. (2011) 32:714–8. doi: 10.1086/660761
16. Navarro-San Francisco, C, Del Toro, MD, Cobo, J, De Gea-García, JH, Vañó-Galván, S, Moreno-Ramos, F, et al. Knowledge and perceptions of junior and senior Spanish resident doctors about antibiotic use and resistance: results of a multicenter survey. Enferm Infecc Microbiol Clin. (2013) 31:199–204. doi: 10.1016/j.eimc.2012.05.016
17. Khan, AKA, and Banu, G. Antibiotic resistance and usage-a survey on the knowledge, attitude, perceptions and practices among the medical students of a southern Indian teaching hospital. J Clin Diagn Res. (2013) 7:1613–6. doi: 10.7860/JCDR/2013/6290.3230
18. Bonjean, M, Hodille, E, Dumitrescu, O, Dupieux, C, Nkoud Mongo, C, Allam, C, et al. Disk diffusion testing for detection of methicillin-resistant staphylococci: does Moxalactam improve upon Cefoxitin? J Clin Microbiol. (2016) 54:2905–9. doi: 10.1128/JCM.01195-16
19. Dargère, S, Cormier, H, and Verdon, R. Contaminants in blood cultures: importance, implications, interpretation and prevention. Clin Microbiol Infect. (2018) 24:964–9. doi: 10.1016/j.cmi.2018.03.030
20. Marzan, M, Islam, DZ, Lugova, H, Krishnapillai, A, Haque, M, and Islam, S. Knowledge, attitudes, and practices of antimicrobial uses and resistance among public university students in Bangladesh. Infect Drug Resist. (2021) 14:519–33. doi: 10.2147/IDR.S289964
21. Mudenda, S, Chisha, P, Chabalenge, B, Daka, V, Mfune, RL, Kasanga, M, et al. Antimicrobial stewardship: knowledge, attitudes and practices regarding antimicrobial use and resistance among non-healthcare students at the University of Zambia. JAC Antimicrob Resist. (2023) 5:1–10. doi: 10.1093/jacamr/dlad116
22. Salcedo, S, Mora, L, Fernandez, DA, Marín, A, Berrío, I, Mendoza-Charris, H, et al. Knowledge, attitudes, and behavior regarding antibiotics, antibiotic use, and antibiotic resistance in students and health care professionals of the district of Barranquilla (Colombia): a cross-sectional survey. Heliyon. (2022) 8:e11378. doi: 10.1016/j.heliyon.2022.e11378
23. Higuita-Gutiérrez, LF, Roncancio Villamil, GE, and Jiménez Quiceno, JN. Knowledge, attitude, and practice regarding antibiotic use and resistance among medical students in Colombia: a cross-sectional descriptive study. BMC Public Health. (2020) 20:1861. doi: 10.1186/s12889-020-09971-0
Keywords: knowledge-attitude-practice, medical residents, antimicrobial stewardship (AMS), multidrug-resistant (MDR) bacteria, Iran
Citation: Kiani F, Sajadi G, Motamedi N, Salmasi M and Solgi H (2024) Medical residents’ knowledge, attitudes and practices regarding antibiotics, antimicrobial stewardship and multidrug-resistant bacteria: a cross-sectional study in a major university in Iran. Front. Med. 11:1435542. doi: 10.3389/fmed.2024.1435542
Edited by:
Steward Mudenda, University of Zambia, ZambiaReviewed by:
Abdulaziz Zorgani, National Center for Disease Control, LibyaFauna Herawati, University of Surabaya, Indonesia
Copyright © 2024 Kiani, Sajadi, Motamedi, Salmasi and Solgi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hamid Solgi, aGFtaWQuc29sZ2lAZ21haWwuY29t
†These authors have contributed equally to this work
 Fatemeh Kiani1†
Fatemeh Kiani1† Hamid Solgi
Hamid Solgi