- 1Department of Obstetrics and Gynecology, Women and Children's Hospital of Chongqing Medical University (Chongqing Health Center for Women and Children), Chongqing, China
- 2Department of Ultrasound, Women and Children's Hospital of Chongqing Medical University (Chongqing Health Center for Women and Children), Chongqing, China
- 3Department of Radiology, Women and Children's Hospital of Chongqing Medical University (Chongqing Health Center for Women and Children), Chongqing, China
Background: Robert’s uterus combined with transverse uterine septum is a rare uterine malformation. Only one case has been reported to date, and it is challenging to diagnose and treat.
Case presentation: Here we report the case of a 19-year-old female had undergone multiple treatments at a previous hospital for primary amenorrhea and periodic lower abdominal pain, with the cause remaining unclear. Ultrasonography and magnetic resonance imaging conducted at our hospital displayed the presence of uterine dysplasia with an incomplete septum. Following a multidisciplinary discussion, a preliminary diagnosis of Robert’s uterus combined with transverse uterine septum was made. Following this, laparoscopic exploration and ultrasound-guided hysteroscopic metroplasty were performed. The patient experienced periodic menstruation postoperatively and did not manifest periodic lower abdominal pain.
Conclusion: Robert’s uterus combined with transverse uterine septum is a very rare uterine malformation, with hysteroscopic metroplasty being the preferred surgical option. Nevertheless, preoperative diagnosis is extremely difficult, and there are also many difficulties in the surgical process. This case outlines the diagnostic and treatment process of a patient with Robert’s uterus and transverse uterine septum. It is of great significance to fill the gap in clinical diagnosis and treatment of this special uterine malformation.
Introduction
Robert’s uterus (asymmetric septate uterus) is a rare complex Müllerian malformation first described by French gynecologists in 1970 with an incidence <3% (1, 2). Indeed, only a few cases have been reported. Robert’s uterus is anatomically characterized by asymmetric uterine separation with unilateral menstrual blood retention in the uterus. This separation extends from the fundus to the upper part of the internal opening of the cervix, inclining to one side of the uterine cavity, and completely closes the uterine cavity on the ipsilateral side. This results in a blind hemicavity that does not communicate with the contralateral uterine cavity and vagina. On the other hand, the blind hemicavity is connected with the ipsilateral side of the fallopian tube. Notwithstanding, the uterine silhouette is unremarkable (3, 4). The lack of communication between the two uterine hemicavities leads to menstrual blood retention and reflux, hematometra, ipsilateral hematosalpinx, severe dysmenorrhea, pelvic endometriosis, and secondary reproductive dysfunction, encompassing infertility, abortion, premature delivery, and malpresentation-induced dystocia (5). Of note, only one case of Robert’s uterus combined with a transverse uterine septum was documented in 2017 (6).
Patients with Robert’s uterus combined with transverse septum do not discharge menstrual blood due to the complete obstruction of the reproductive tract, thereby exacerbating dysmenorrhea, which can be detected via Ultrasonography and magnetic resonance imaging (MRI) examinations (7). Ascribed to the rarity of this type of uterine malformation, it is susceptible to misdiagnosis as other types of uterine malformations, such as unicornuate uterus. Selecting an inadequate surgical approach may exert unfavorable effects on the patient’s future fertility (8). At present, there is no standardized surgical plan recommended for the management of Robert’s uterus combined with a transverse uterine septum. This case report outlines the diagnosis and treatment of Robert’s uterus combined with transverse uterine septum and intrauterine adhesion.
Case presentation
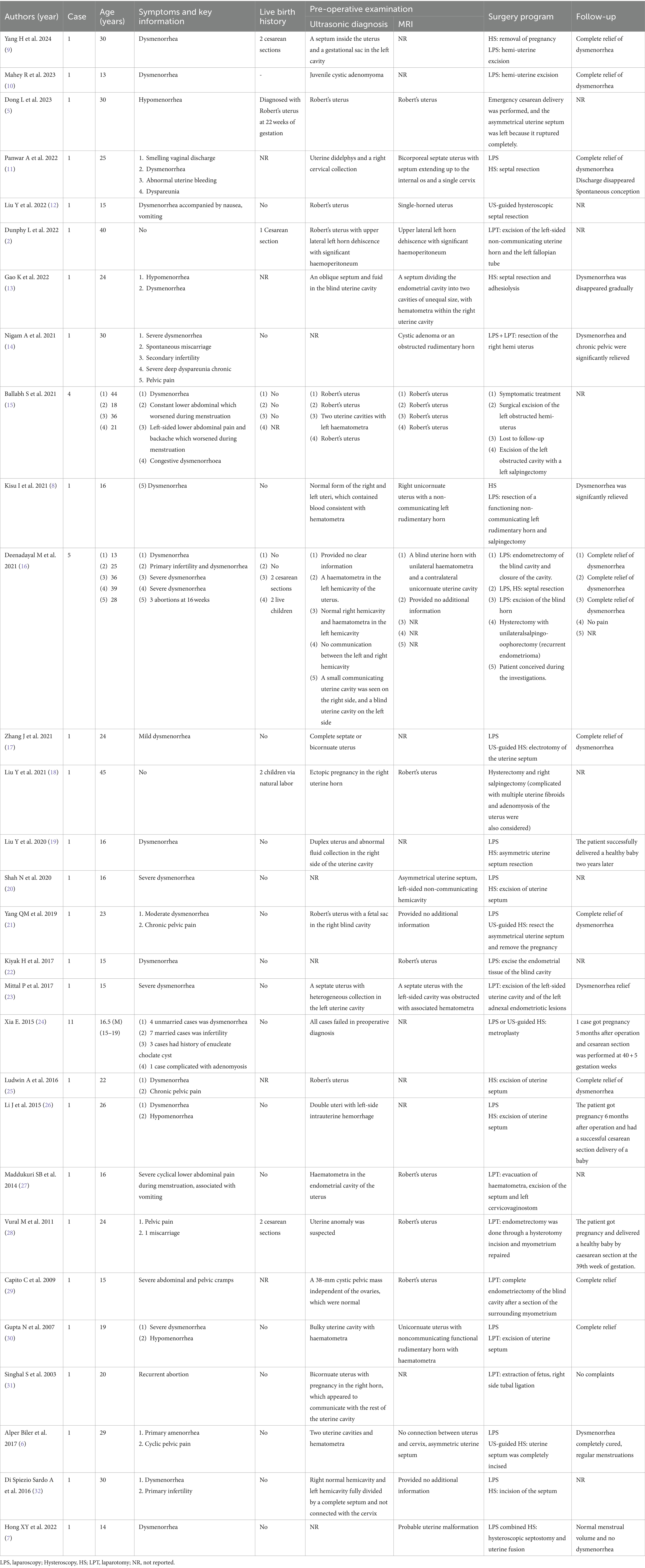
The patient, a 19-year-old female with no sexual history, has been experiencing periodic lower abdominal pain since the age of 16 years. After many visits to local hospitals, no obvious abnormality was found in female hormone. Multiple ultrasound only showed adnexal mass, small uterus, no uterine malformation. The patient underwent progesterone testing and artificial cycle treatment, both displaying the absence of menstrual flow and no significant improvement in abdominal pain. While the periodic abdominal pain was relieved in January 2023, she did not menstruate. Afterward, the patient attended our hospital for further treatment. The gynecological vulvar examination was unremarkable, with visible hymen holes visible. Anal examination exposed that the right index finger could be extended into the rectum, allowing the visualization of part of the posterior vaginal wall at the margin of the hymen. At 7 cm into the rectum, the cervical canal was palpable, and no abnormal mass was detected. Review transrectal three-dimensional ultrasound (3D US) (GE Voluson E8, America) (Figure 1A) depicted that the horizontal transverse section of the uterine fundus revealed a hypoechoic separation between the two endometria, with a distance of roughly 3.3 cm between the bilateral uterine horns. In addition, the midpoint was approximately 0.7 cm away from the serosal layer of the uterine fundus, with a downward depression of about 0.9 cm and about 0.7 cm away from the internal cervix opening. Moreover, the angle between the bilateral uterine horns and the lowest point of the depression was 103.84°. An echoless area was detected in both uterine cavities. Diagnostic considerations: 1. Uterine malformation (consistent with sonographic changes of incomplete septate uterine); 2. Biadnexal cystic mass; 3. Bilateral horn strip echo zone: The possibility of fluid accumulation in the interstitial area of the fallopian tube was considered. MRI (Figure 1B) images delineated that the size of the uterus was about 4.7 × 3.7 × 7.0 cm, with a uterine body-to-cervical diameter ratio of about 3/4. The myometrium at the fundus of the uterus was locally convex toward the uterine cavity. In addition, the volume of the right kidney was significantly reduced to about 3.0 × 2.0 × 3.6 cm. Diagnostic considerations: 1. uterine malformation: possible uterine dysplasia with incomplete septum; 2. Right kidney dysplasia with multiple cysts; 3. Cystic space occupying bilateral adnexal areas, benign lesions, multiple cysts, and cystadenoma were considered; 4. Blood or fluid accumulation in the uterine cavity and bilateral fallopian tubes. Lastly, the results of the thyroid function, liver and kidney function, and coagulation function tests were normal. Following a multidisciplinary discussion, a preliminary diagnosis of Robert’s uterus combined with transverse uterine septum was made.
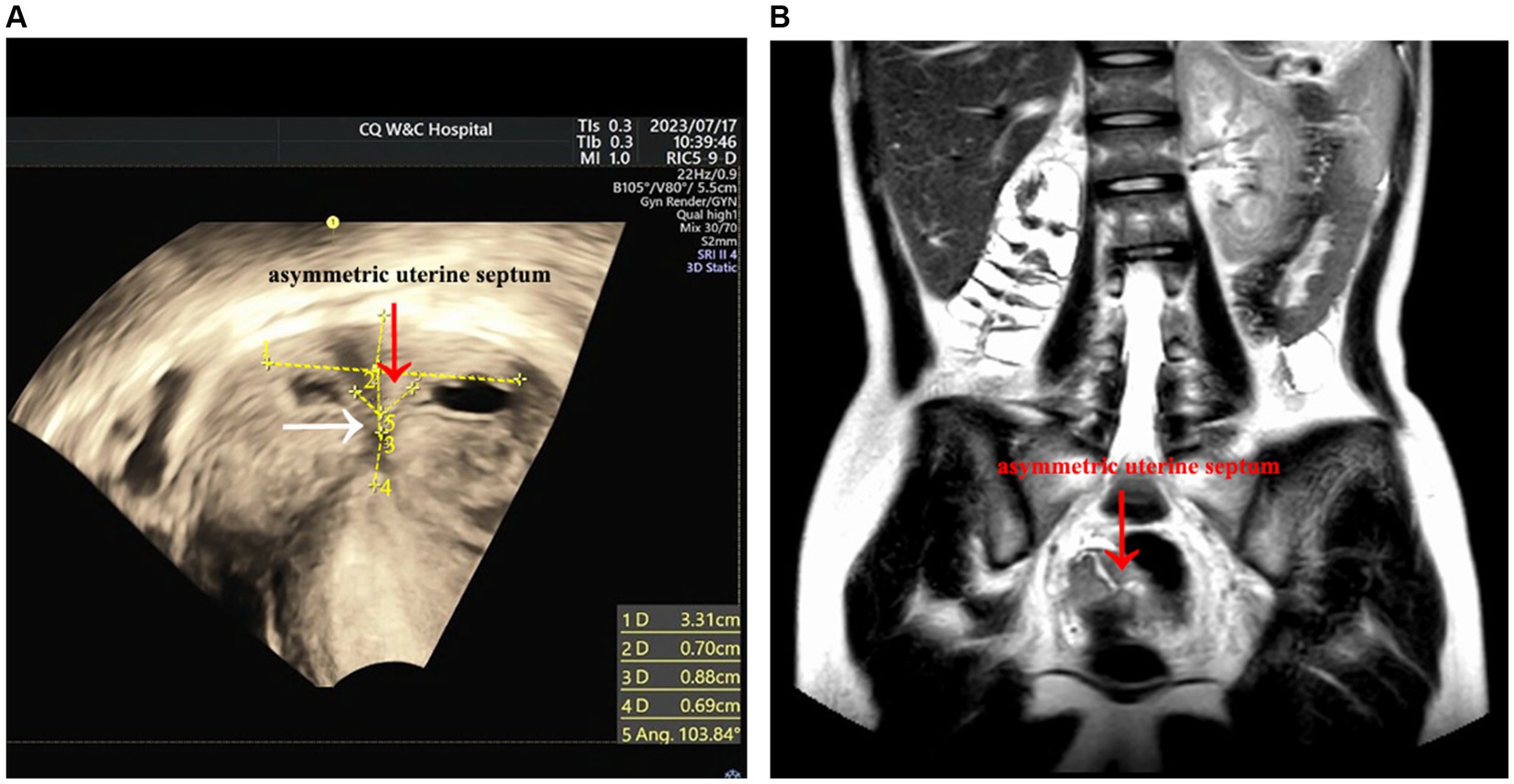
Figure 1. Preoperative imaging examination. (A) The red arrow points to the asymmetrical uterine septum, while the white arrow points to the obstruction site, i.e., the transverse uterine septum. However, the ultrasound was not completely clear, and the transverse uterine septum was not visualized. (B) The uterine fundus, indicated by the arrow, is depressed downward toward the uterine septum. Given that the thickness of the transverse uterine septum was below the MRI slice gap, the MRI image did not capture the transverse uterine septum.
During the surgical intervention, hysteroscopy (ShenDa J0100A, China) revealed a single cervix with normal cervical canal morphology. The length of the cervical canal was 4 cm, and a transverse septum was identified 7 mm above the internal opening of the cervix, preventing access to the uterine cavity Figure 2A. The septum was punctured using an transabdominal US-guided (Mindray M11T, China) probing needle, unveiling the presence of brown menstrual blood, as illustrated in Figure 2B. An oblique adhesive band was observed extending from the right side wall of the uterine cavity to the septum, and the opening of the right fallopian tube was visible, as displayed in Figures 3A,B. While the adhesive band was separated to expose the right uterine cavity, the opening of the left fallopian tube was not visible. Ultrasound showed that the left and right uterine cavities remained unconnected, and an oblique septum was found from the bottom of the left uterine wall to the left lateral wall. Miniature scissor was employed to excise the weaker portion of the septum, gradually exposing the left uterine cavity. No menstrual blood retention was found inside, and the opening of the left fallopian tube was visible (Figure 3C). Most of the endometrium was defective, with only a small amount of endometrial tissue noted at the bilateral uterine horns (Figure 3D). The two-dimensional model of the uterine cavity is portrayed in Figure 4. During laparoscopic examination, the left interstitial of the fallopian tube was thick and twisted, and a tubular structure over 3 cm long was observed at its proximal end, whereas no lumen or umbrellum structure was observed at the distal end. Besides, the left fallopian tube and left ovary were wrapped and adherent to form a mass of about 4*3 cm (Figure 5A). At the same time, the right ovary was cystically enlarged by approximately 5*5*4 cm, exhibiting a multilocular morphology and filled with clear fluid (Figure 5A). A blind end of approximately 3.5 cm long was noted in the right fallopian tube, and no umbrella structure was observed (Figure 5B). The uterus was flat in the posterior position and measured about 4*3*3 cm (Figure 5C). Following the separation of pelvic adhesion, hysteroscopic intubation was performed on the fallopian tube. The left interstitial area was blue-stained, with no methylene blue outflow observed at the distal end of the left fallopian tube. Consider that bilateral fallopian tubes may be non-functional, bilateral fallopian tubes were excised after communicating with the patient’s family. While the cystic area of the right ovary was physiological. The external outline of the uterus after hysteroscopic metroplasty reveals a fullness at the base of the uterus, indicating that uterine morphology was restored (Figure 5D). Prior to terminating the procedure, an intrauterine balloon was placed, and 4 mL of normal saline was injected. The intrauterine balloon was retained for 5 days post-operatively, and one cycle of Femoston (2 mg:10 mg) was administered to the patient.
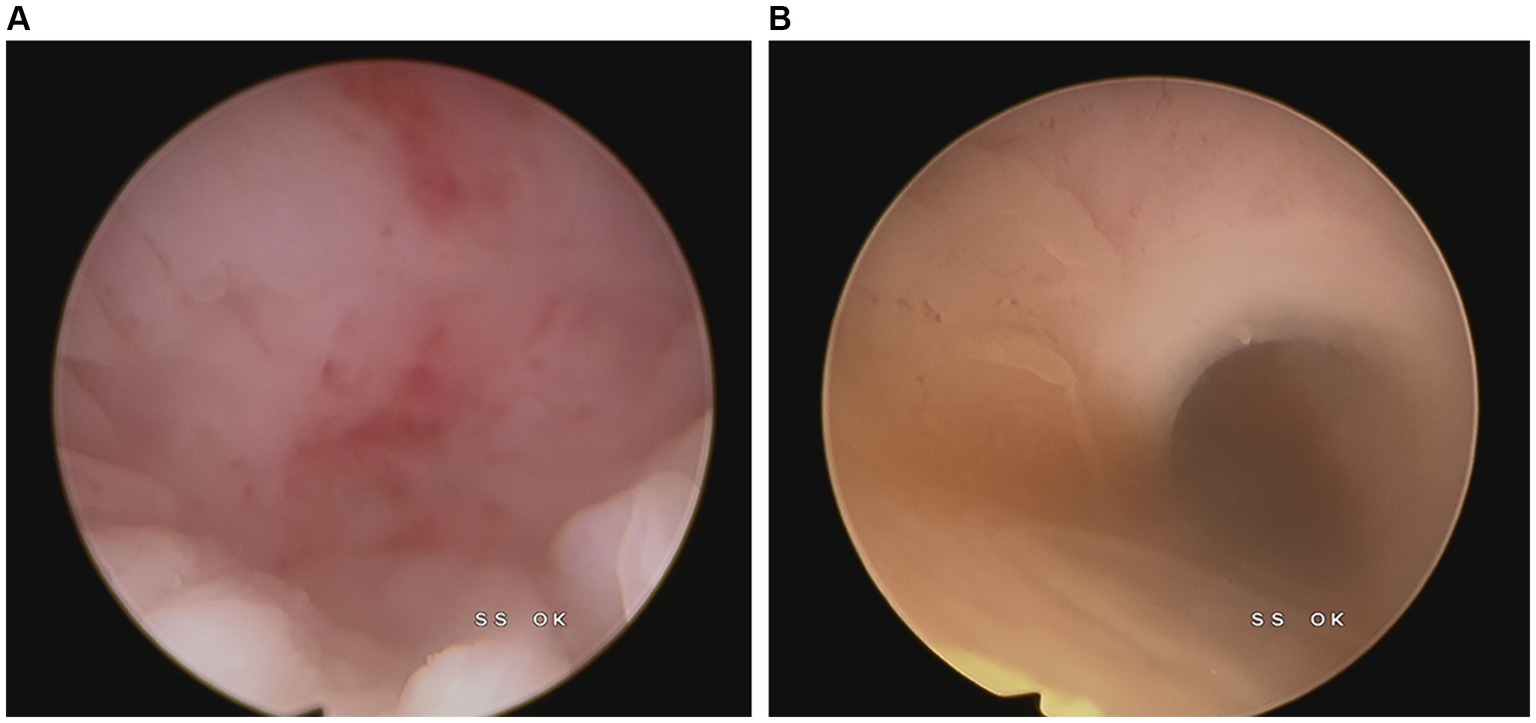
Figure 2. Cervical image during hysteroscopy. (A) The internal opening of the cervix is closed. (B) Brown menstrual blood outflow after puncturing the transverse uterine septum.
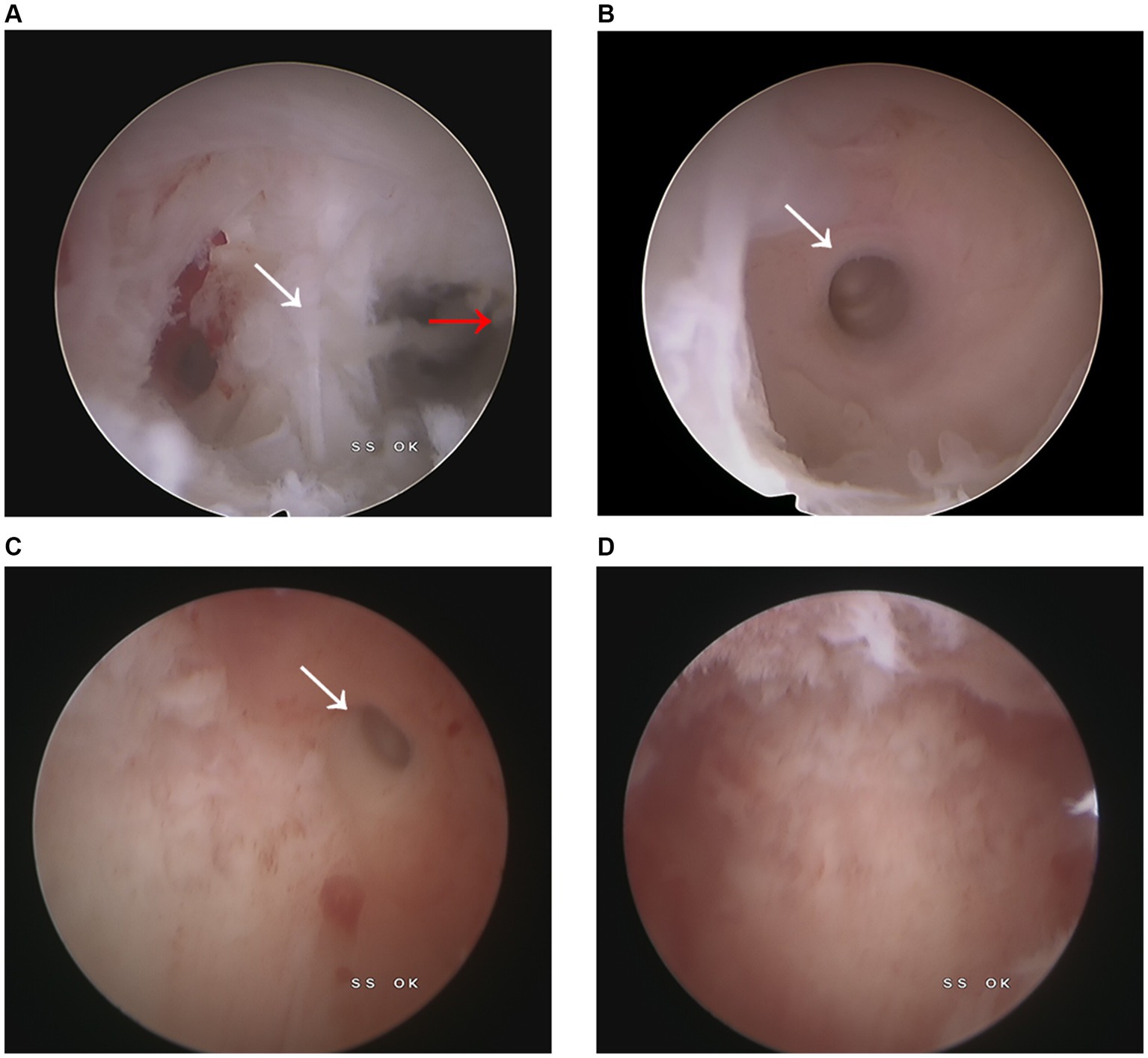
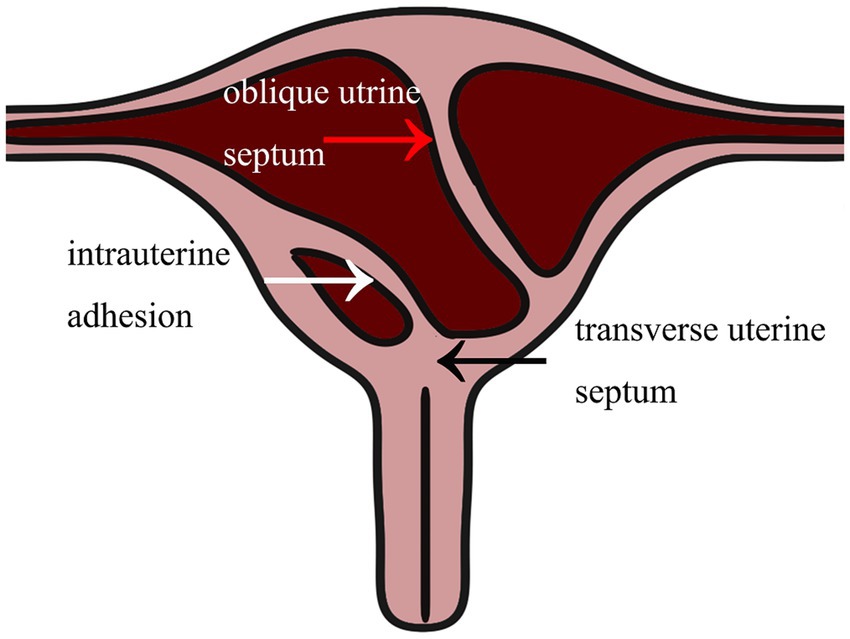
Figure 3. Intrauterine image. (A) The white arrow points to the right intrauterine adhesion, whereas the red arrow points to the oblique uterine septum. (B) The right fallopian tube opening could be visualized after the separation of the right uterine adhesion. (C) The left fallopian tube opening was exposed following the excision of the oblique uterine. (D) After complete resection of the oblique septum, the uterine cavity morphology was restored to normal.
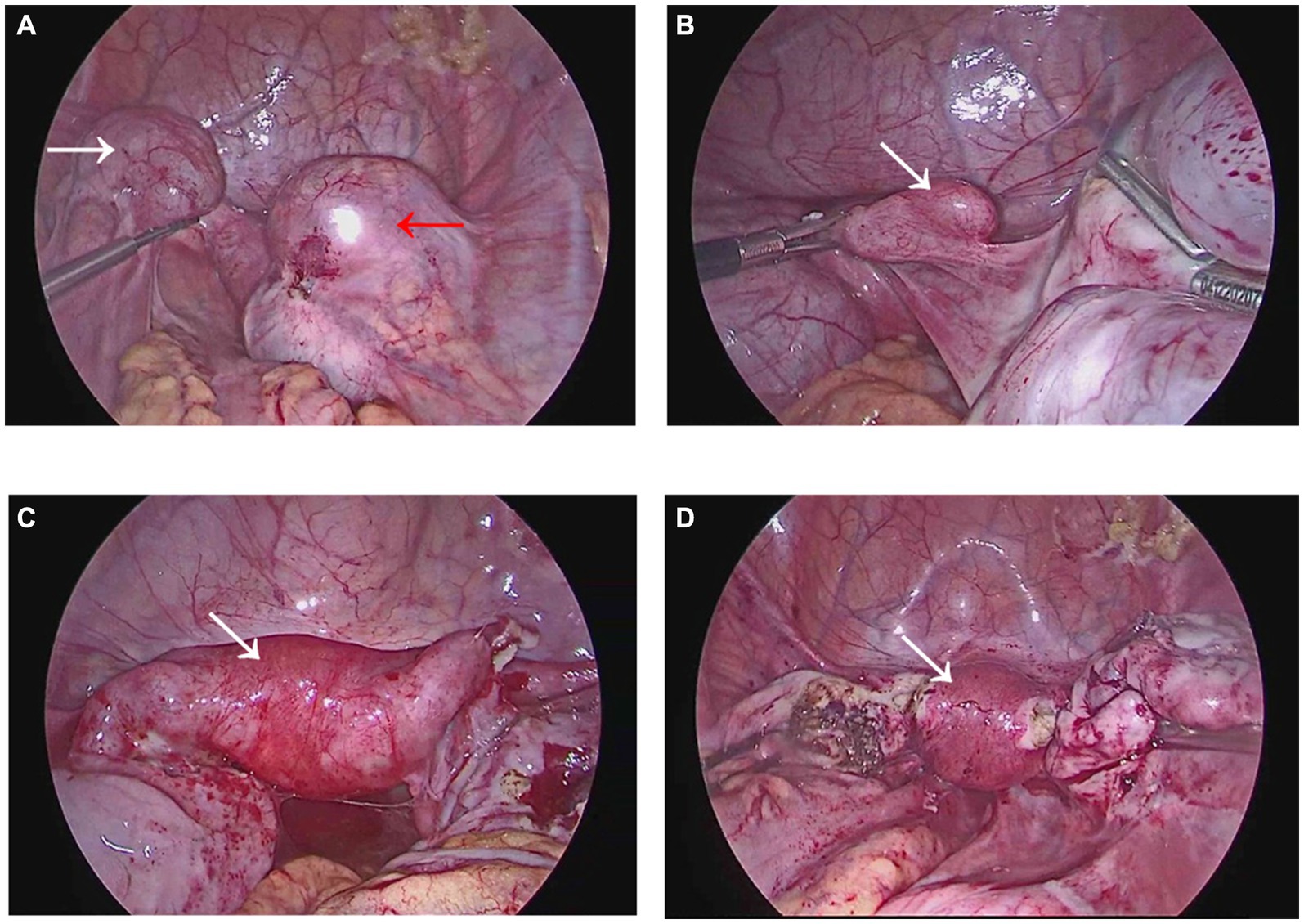
Figure 5. Images during laparoscopy. (A) The white arrow points toward the adhesion in the left attachment area, while the red arrow points toward the adhesion in the right attachment area. (B) Displays the blind end of the right fallopian tube. (C) Exhibits the external uterine silhouette prior to hysteroscopic metroplasty, with a slight downward depression near the base of the left uterus. (D) The external outline of the uterus after hysteroscopic metroplasty reveals a fullness at the base of the uterus, indicating that uterine morphology was restored.
On the 5th day after surgery, the intrauterine balloon was removed, and a 3D US showed no obvious abnormalities in the shape of the uterine cavity (Figure 6A). The patient menstruated 5 days after the discontinuation of Fenmorton, lasting for 3 days. On the first day, the menstrual blood soaked the area of the sanitary pad about the size of 2 coins, whereas on the 2nd and 3rd days, it was about the size of 1 coin per day. Importantly, ultrasonography exposed an endometrial thickness of about 0.3 cm, with a Y-shaped uterine cavity. Hysteroscopy conducted on the 10th day of menstruation depicted normal uterine morphology, with a thin endometrial layer in the uterine cavity, partial endometrium defects, and visible openings of the bilateral fallopian tubes (Figure 6B). At present, the patient experiences periodic menstruation with a small amount of menstrual blood. The amount and duration of menstruation were comparable to the first menstrual cycle post-operatively. Indeed, the patient did not present with dysmenorrhea.
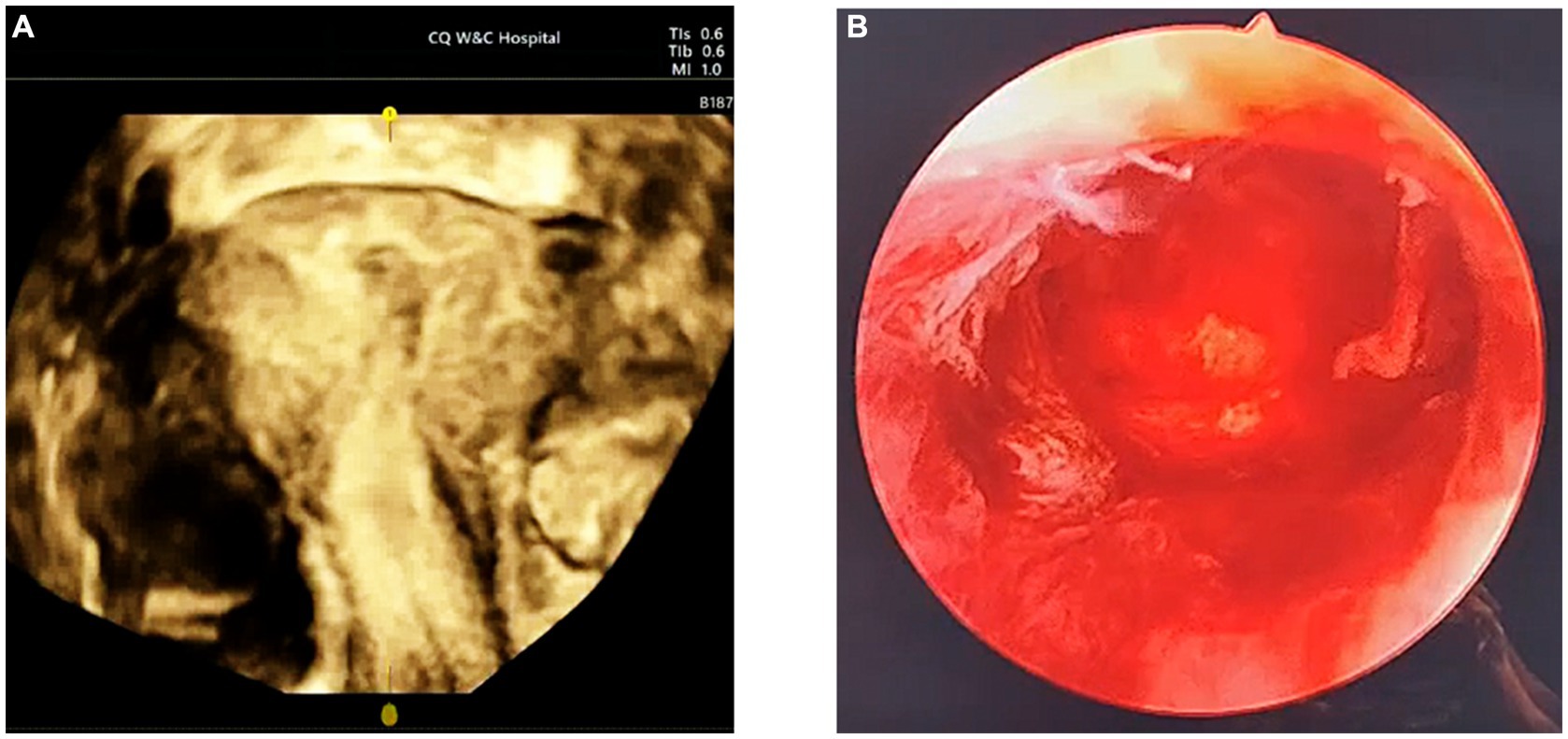
Figure 6. Postoperative follow-up ultrasound and hysteroscopy. (A) There was no significant echo in the uterine cavity by postoperative 3D ultrasound. (B) Follow-up hysteroscopy after menstruation showed normal uterine cavity morphology, with a thin endometrial layer visible.
Discussion
The current study aimed to analyze the clinical protocol for the preoperative diagnosis and surgical management of Robert’s uterus combined with transverse uterine septum. Our clinical case provides valuable insights into the diagnosis and treatment of this unique uterine malformation.
Robert’s uterus combined with transverse uterine septum is a rare congenital malformation of the reproductive tract. Only one case of Robert’s uterus combined with a transverse uterine septum was documented in 2017 (6). The case in 2017 was roughly the same as ours, with symptoms of primary amenorrhea and cyclic pelvic pain, both of which were misdiagnosed and the surgical methods was basically the same. However, the case reported in 2017 was very simple without graphic explanation, but our case described the diagnosis and treatment process in detail and analyzed the main points. Ascribed to the rarity of this disease, it is easily misdiagnosed. Actually, we identified 46 Robert’s uterus cases in our systematic literature review, only 21 cases had a preoperative diagnosis of Robert’s uterus or an asymmetric uterine septum by US or MRI (Table 1). The majority of existing studies on Robert’s uterus comprise case reports, predominantly involving intraoperative diagnosis, while studies focused on Robert’s uterus complicated with transverse uterine septum are limited, and preoperative diagnosis proves more challenging. This patient’s uterine malformation was not diagnosed via multiple ultrasound examinations conducted in other hospitals, thereby delaying the treatment. Prolonged menstrual blood accumulation in the uterine cavity may promotes the development of endometritis and uterine adhesions. The endometrial defects impair the production of menstrual blood, which may have accounted for the alleviation of subsequent abdominal pain in patients. Even after the surgical relief of the obstruction, the endometrium defect can not be completely repaired, limiting menstrual flow and fertility. Therefore, timely detection and treatment are critical for the long-term fertility of patients.
An earlier study reported that Robert’s uterus was misdiagnosed as a unicornuate uterus with a non-communicating rudimentary horn and hematometra. The patient was then subjected to laparoscopic hemi-hysterectomy, which further lowered the probability of conception and increased the risk of uterine rupture (8). Herein, Robert’s uterus combined with the transverse uterine septum, was misdiagnosed as an incomplete septate uterus. Thus, preoperative multidisciplinary consultation and discussion are key to avoiding permanent damage to patients caused by misdiagnosis and inappropriate surgical modalities. Owing to the limitation of the MRI slice gap, MRI failed to detect the transverse uterine septum. The possibility of transverse uterine septum was proposed by ultrasound physicians during the multidisciplinary discussion. Due to the limitations of ultrasound instrument resolution and the rarity of Robert’s uterus combined with transverse uterine septum, preoperative ultrasound reports refrain from making a hasty diagnosis of transverse uterine septum. After a multidisciplinary discussion, a preliminary diagnosis of Robert’s uterus combined with transverse uterine septum was established. As anticipated, the diagnosis made through the preoperative multidisciplinary discussion was consistent with the intraoperative findings.
The surgical management of Robert’s uterus combined with transverse uterine septum is guided by some considerations. The primary objective of the treatment is to restore the physiological anatomy of the uterine cavity and enhance reproductive outcomes. Hysteroscopic metroplasty, a minimally invasive procedure, is the preferred approach for resecting the septum (33). US-guided hysteroscopic electrotomy of the uterine septum can be used for three different types of Robert’s uterus (34). However, certain factors, including the location and thickness of the septum, may necessitate alternative surgical techniques such as laparoscopic metroplasty. For this particular uterine malformation, hysteroscopic metroplasty may induce myometrial damage and uterine perforation due to mislocation, while laparoscopic surveillance may only observe the external silhouette of the uterus but cannot detect intrauterine morphology. During the operation, the adhesion was misidentified as the uterine septum. It was only under the guidance of an experienced sonographer that the real uterine septum was discovered and excised to restore the shape of the uterine cavity and avoid intraoperative missed diagnosis. Based on our experience, ultrasound-guided hysteroscopic metroplasty with the assistance of an experienced sonographer is critical to the success of the procedure. Given the limited number of cases, the effect of surgical treatment on the reproductive prognosis of patients with Robert’s uterus combined with transverse uterine septum could not be evaluated. However, the surgical alleviation of obstruction can contribute to the outflow of menstrual blood, attenuate abdominal pain, improve the quality of life of patients, and minimize the adverse effects of menstrual blood reflux on the pelvic cavity.
Conclusion
In summary, Robert’s uterus combined with transverse uterine septum is a rare uterine malformation, with hysteroscopic metroplasty being the preferred surgical option. Due to challenges in its diagnosis, primary hospitals should actively refer patients presenting with unexplained primary amenorrhea accompanied by periodic lower abdominal pain and normal ovarian function to higher-level medical centers. Following diagnosis, surgery should be promptly performed. Preoperative multidisciplinary consultations are recommended to preliminarily assess the type of uterine malformation and the location of obstruction. Surgery should ideally be conducted under the guidance of experienced ultrasound physicians.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by Ethics Committee of Women and Children’s Hospital of Chongqing Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
MC: Data curation, Formal analysis, Writing – original draft, Writing – review & editing, Investigation, Visualization. XY: Investigation, Methodology, Validation, Writing – review & editing. BZ: Data curation, Software, Visualization, Writing – review & editing. JF: Data curation, Software, Visualization, Writing – review & editing. YL: Conceptualization, Investigation, Methodology, Project administration, Supervision, Writing – review & editing. YC: Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Resources, Validation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Chongqing Health Appropriate Technology Promotion Project (2022jstg014); Chongqing Young and Middle-aged Medical High-end Talent Project; and Chongqing Education Commission Key Project (KJZD-K202300407).
Acknowledgments
We are grateful to everyone who helped us carry out this study and Home for Researchers editorial team (www.home-for-researchers.com) for language editing service.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Robert, H. Asymmetrical bifidities with unilateral menstrual retention (apropos of l2 cases). Chirurgie. (1970) 96:796–9.
2. Dunphy, L, Taylor, S, Whitby, EH, Agarwal, U, and Alfirević, Ž. Robert's uterus (asymmetric septate uterus): a rare congenital Müllerian duct anomaly. BMJ Case Rep. (2022) 15:e244237. doi: 10.1136/bcr-2021-244237
3. Pfeifer, SM, Attaran, M, Goldstein, J, Lindheim, SR, Petrozza, JC, Rackow, BW, et al. ASRM müllerian anomalies classification 2021. Fertil Steril. (2021) 116:1238–52. doi: 10.1016/j.fertnstert.2021.09.025
4. Chinese experts' consensus on the nomenclature and definition revision of female genital malformations. Zhonghua Fu Chan Ke Za Zhi. (2022) 57:575–80. doi: 10.3760/cma.j.cn112141-20220321-00177
5. Dong, L, Qin, S, Che, R, Pei, J, and Hua, X. Successful pregnancy in the blind hemicavity of Robert's uterus: a rare case report and brief literature review. BMC Pregnancy Childbirth. (2023) 23:211. doi: 10.1186/s12884-023-05541-5
6. Biler, A, Akdemir, A, Peker, N, and Sendag, F. A rare uterine malformation: asymmetric septate uterus. J Minim Invasive Gynecol. (2018) 25:28–9. doi: 10.1016/j.jmig.2017.06.015
7. Hong, XY, Ding, B, and Shen, Y. Laparo-endoscopic single site combined with hysteroscopy to diagnose and treat Robert's uterine malformation: a case report. Front Surg. (2022) 9:926935. doi: 10.3389/fsurg.2022.926935
8. Kisu, I, Nakamura, K, Shiraishi, T, Iijima, T, Iijima, M, Matsuda, K, et al. Inappropriate surgery in a patient with misdiagnosed Robert's uterus. BMC Womens Health. (2021) 21:264. doi: 10.1186/s12905-021-01404-3
9. Yang, H, Shi, Y, and Ji, G. Minimally invasive surgical treatment of Robert's uterus with missed miscarriage: case report. J Obstet Gynaecol. (2024) 44:2305204. doi: 10.1080/01443615.2024.2305204
10. Mahey, R, Cheluvaraju, R, Kumari, S, Kachhawa, G, Kumari, A, Rajput, M, et al. Robert's uterus versus juvenile cystic Adenomyoma-diagnostic and therapeutic challenges-case report and review of literature. J Hum Reprod Sci. (2023) 16:79–86. doi: 10.4103/jhrs.jhrs_10_23
11. Panwar, A, Lata, K, Kriplani, I, Sharma, S, and Kriplani, A. Role of laparoscopic Transillumination guidance during Hysteroscopic Metroplasty in simplifying surgical Management of Type II Robert's uterus. J Obstet Gynaecol India. (2022) 72:421–4. doi: 10.1007/s13224-021-01609-4
12. Liu, Y, Hou, C, and Zhou, Y. Ultrasound combined with hysteroscopy for optimum treatment of Robert's uterus: a case report and a review. BMC Womens Health. (2022) 22:334.
13. Gao, K, Zhang, H, Zhu, J, and Yu, M. Intrauterine adhesions combined with Robert's uterus: a case report and literature review. Arch Gynecol Obstet. (2022) 306:1069–75. doi: 10.1007/s00404-022-06574-5
14. Nigam, A, Basanti, N, Sharma, S, Gupta, N, and Jain, A. Robert's uterus-rare cause of intractable dysmenorrhea and chronic pelvic pain. J Hum Reprod Sci. (2021) 14:317–20. doi: 10.4103/jhrs.jhrs_32_21
15. Ballabh, S, Simon, B, Ebenezer, ED, John, RA, and Chandramohan, A. Imaging features of Robert's uterus: case series of a rare Mullerian duct anomaly. Trop Dr. (2021) 51:553–60. doi: 10.1177/00494755211034061
16. Deenadayal, M, Günther, V, Alkatout, I, Freytag, D, Deenadayal-Mettler, A, Deenadayal Tolani, A, et al. Critical role of 3D ultrasound in the diagnosis and management of Robert's uterus: a single-Centre case series and a review. Facts Views Vis Obgyn. (2021) 13:41–9. doi: 10.52054/FVVO.13.1.008
17. Zhang, J, Zhou, W, Tang, Y, Tan, S, and Qiao, L. Robert's uterus with delayed diagnosis and potential consequences: a case report. J Int Med Res. (2021) 49:300060521999531. doi: 10.1177/0300060521999531
18. Liu, Y, Wang, S, Hong, Y, Wang, J, Niu, J, Li, X, et al. Pregnancy in the blind hemi-cavity of Robert's uterus: a case report. Radiol Case Rep. (2021) 16:1085–8. doi: 10.1016/j.radcr.2021.02.013
19. Liu, Y, Yang, Y, Duan, J, Liu, L, Zhang, W, and Wang, Y. Favorable pregnancy outcome for a patient with Robert's uterus, bicornuate uterus, and ipsilateral renal agenesis. Int J Gynaecol Obstet. (2020) 151:302–3. doi: 10.1002/ijgo.13274
20. Shah, N, and Changede, P. Hysteroscopic Management of Robert's uterus. J Obstet Gynaecol India. (2020) 70:86–8. doi: 10.1007/s13224-019-01208-4
21. Yang, QM, Li, H, He, SH, Chen, D, and Chen, L. Pregnancy in a blind hemi-cavity of Robert's uterus with ipsilateral renal agenesis: a case report and literature review. J Int Med Res. (2019) 47:3427–34. doi: 10.1177/0300060519850422
22. Kiyak, H, Karacan, T, Wetherilt, LS, Seckin, KD, and Ozyurek, ES. Laparoscopic blinded endometrial cavity resection for Robert's uterus. J Minim Invasive Gynecol. (2018) 25:340. doi: 10.1016/j.jmig.2017.09.003
23. Mittal, P, Gupta, R, Mittal, A, Taneja, A, Sekhon, PS, and Gupta, S. Magnetic resonance imaging (MRI) depiction of Robert's uterus: a rare Müllerian duct anomaly presenting with cyclical pain in young menstruating woman. Pol J Radiol. (2017) 82:134–6. doi: 10.12659/PJR.900436
24. Xia, E. Eleven cases Robert's uterus treated by hysteroscopy and laparoscopy successfully delivered in 1 case. J Minim Invasive Gynecol. (2015) 22:S192–192S193. doi: 10.1016/j.jmig.2015.08.702
25. Ludwin, A, Ludwin, I, and Martins, WP. Robert's uterus: modern imaging techniques and ultrasound-guided hysteroscopic treatment without laparoscopy or laparotomy. Ultrasound Obstet Gynecol. (2016) 48:526–9. doi: 10.1002/uog.15976
26. Li, J, Yu, W, Wang, M, and Feng, LM. Hysteroscopic treatment of Robert's uterus with laparoscopy. J Obstet Gynaecol Res. (2015) 41:1491–4. doi: 10.1111/jog.12735
27. Maddukuri, SB, Karegowda, LH, Prakashini, K, and Kantipudi, S. Robert's uterus: a rare congenital müllerian duct anomaly causing haematometra. BMJ Case Rep. (2014):bcr2014204489. doi: 10.1136/bcr-2014-204489
28. Vural, M, Yildiz, S, Cece, H, and Camuzcuoglu, H. Favourable pregnancy outcome after endometrectomy for a Robert's uterus. J Obstet Gynaecol. (2011) 31:668–9. doi: 10.3109/01443615.2011.593653
29. Capito, C, and Sarnacki, S. Menstrual retention in a Robert's uterus. J Pediatr Adolesc Gynecol. (2009) 22:e104–6. doi: 10.1016/j.jpag.2008.03.004
30. Gupta, N, Mittal, S, Dadhwal, V, and Misra, R. A unique congenital mullerian anomaly: Robert's uterus. Arch Gynecol Obstet. (2007) 276:641–3. doi: 10.1007/s00404-007-0389-2
31. Singhal, S, Agarwal, U, Sharma, D, and Sirohiwal, D. Pregnancy in asymmetric blind hemicavity of Robert's uterus--a previously unreported phenomenon. Eur J Obstet Gynecol Reprod Biol. (2003) 107:93–5. doi: 10.1016/S0301-2115(02)00238-5
32. Di Spiezio, SA, Giampaolino, P, Scognamiglio, M, Varelli, C, Nazzaro, G, Mansueto, G, et al. An exceptional case of complete septate uterus with unilateral cervical aplasia (class U2bC3V0/ESHRE/ESGE classification) and isolated Mullerian remnants: combined Hysteroscopic and laparoscopic treatment. J Minim Invasive Gynecol. (2016) 23:16–7. doi: 10.1016/j.jmig.2015.09.006
33. Yu, Y, Zou, L, Zhao, X, and Xu, D. Hysteroscopic incision of a complete uterine septum with double cervices using a slim hysteroscope. Asian J Surg. (2023) 46:886–7. doi: 10.1016/j.asjsur.2022.07.039
Keywords: Robert’s uterus, transverse uterine septum, asymmetric septate uterus, uterine malformation, hysteroscopic metroplasty
Citation: Chen M, Yang X, Zhang B, Fu J, Lan Y and Chi Y (2024) Diagnosis and treatment of Robert’s uterus combined with transverse uterine septum: a case report and review of the literature. Front. Med. 11:1434957. doi: 10.3389/fmed.2024.1434957
Edited by:
Stefano Restaino, Ospedale Santa Maria della Misericordia di Udine, ItalyReviewed by:
Chiara Paglietti, University of Udine, ItalyGiulia Pellecchia, University of Udine, Italy
Copyright © 2024 Chen, Yang, Zhang, Fu, Lan and Chi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yi Lan, MTA5ODE1MjM2QHFxLmNvbQ==; Yugang Chi, Y2hpeXVnYW5nQDE2My5jb20=
†ORCID: Mingqian Chen, orcid.org/0009-0002-4156-9589
Yi Lan, orcid.org/0009-0007-5249-2624
Yugang Chi, orcid.org/0000-0001-8278-984X
 Mingqian Chen
Mingqian Chen Xiaoyu Yang1
Xiaoyu Yang1 Jialiang Fu
Jialiang Fu Yugang Chi
Yugang Chi