- 1Department of Dermatology, Hebei Medical University Third Hospital, Shijiazhuang, China
- 2Department of Clinical Laboratory, Hebei Medical University Third Hospital, Shijiazhuang, China
- 3Hebei Key Laboratory of Intractable Pathogens, Shijiazhuang Center for Disease Control and Prevention, Shijiazhuang, China
- 4Department of Clinical Laboratory, Hebei Yiling Hospital, Shijiazhuang, Hebei, China
Mycobacterium marinum, a photochromogenic, slow-growing mycobacterium, thrives in both marine and freshwater environments. Optimal growth occurs between 25°C and 35°C, with survival becoming challenging above 37°C. Typically, M. marinum enters the body via skin abrasions, often leading to infections of the upper extremities. Diagnosis of M. marinum infection is frequently challenging and delayed due to the difficult pathogen identification. At present, a standardized treatment protocol has yet to be established. Presented herein is a case study detailing an infection of the right hand's middle finger caused by M. marinum. Notably, his occupation as a chef, handling fish and seafood post-injury, was a significant factor. Histological examination of the skin biopsy and positive acid-fast staining were consistent with a diagnosis of mycobacterial infection. Pathological examination confirmed a skin infection with infectious granuloma, and tissue section acid-fast staining revealed acid-fast bacill. Cultures on Columbia blood agar yielded rough, flattened, yellow-fleshy colonies after 10 days, which was identified as M. marinum through 16S rRNA sequencing. The patient responded well to a 3-month regimen of oral moxifloxacin (0.4 qd) and linezolid (0.6 qd), resulting in rash resolution and pain relief, with no recurrence observed for 1-year follow-up. This report presents the first documented acid-fast staining images of M. marinum tissue sections and colony morphology photographs, offering an in-depth view of M. marinum's morphological characteristics. It aims to enhance awareness of M. marinum infections, underscore the necessity for clinicians to delve into patient histories, and provide a review of the clinical manifestations, diagnostic techniques, therapeutic approaches, and pathogenic mechanisms associated with M. marinum.
1 Introduction
Non-tuberculous mycobacteria (NTM) are a group of mycobacteria widely distributed in the natural environment and have been isolated from air, soil, dust, plants, natural and drinking water sources, including biofilms, wild animals, milk, and food products (1–4). In recent years, the incidence and prevalence of NTM infections have been on the rise due to many factors including an aging population, increased numbers of individuals with compromised immune systems, abuse of antibiotic, and advancements in molecular biology identification techniques (4). Skin infections caused by NTM are increasingly recognized and pose a significant public health challenge. M.marinum first isolated from fish in 1926 by J.D. Aronson, was later identified as a human pathogen by Linell and Norden in 1951 (5, 6). According to Runyon's classification, it belongs to photochromogenic Group I NTM, with an optimal growth temperature around 30°C (7). M.marinum, also known as atypical mycobacterium or environmental isolate, is commonly found in disinfected saline and seawater reservoirs worldwide, leading to swimming pool or aquarium granuloma (8). Infections most commonly occur through skin wounds or abrasions. The skin lesions associated with M. marinum infection are typically solitary or multiple red papules, nodules, or ulcers, commonly found on the elbows, knees, hands, and feet. The diagnosis of M. marinum infection requires clinical foresight, as it is a slow-growing mycobacterium that requires extended culture times for positive results. Diagnosis is based on a combination of patient history, clinical presentation, and laboratory tests, including bacterial culture, molecular biology, and histopathology. There is no standardized treatment protocol for M. marinum infection; therapeutic strategies must be individualized based on infection location, severity, and patient immune status. This case report presents a chef with no notable medical or immunosuppressive history, who developed a skin infection by M. marinum following an outdoor injury. The patient achieved successful treatment outcomes with oral moxifloxacin and linezolid, showing no signs of recurrence during follow-up. This article outlines a practical clinical treatment approach and delves into the patient's clinical symptoms, diagnostic tests, outcomes, and pertinent literature, contributing to the broader understanding and management of M. marinum infections.
2 Case presentation
2.1 Patient characteristics
A 22-year-old male patient presented with a history of a finger injury sustained in October 2022 during an outdoor excursion in a wooded area. In the aftermath, he engaged in processing fish and seafood. Subsequently, the patient developed localized papules and nodules with associated pain. The condition progressed to a more severe rash with local purulent discharge. Despite treatment with an unspecified topical medication, there was no improvement. He sought medical attention at Hebei Medical University Third Hospital on January 3, 2023. Dermatological examination revealed an irregular plaque with scales on the extensor side of the right middle finger joint (see Figure 1A). Local tissue was collected for pathological examination and microbial culture, with the clinical suspicion of Sporothrix schenckii infection prompting extended culture duration.
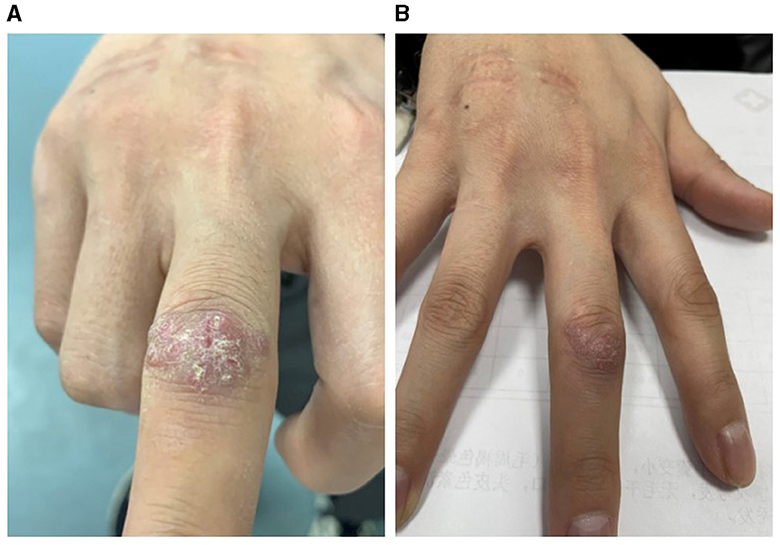
Figure 1. Photos of the patient's right hand. (A) Pre-treatment, the patient's right middle finger joint showed an irregular plaque with scales. (B) Post-treatment, the patient's right middle finger joint rash had mostly flattened.
2.2 Laboratory examination
The histopathological findings from January 5, 2023, are as follows: The histopathology of the right middle finger joint's extensor side revealed hyperplastic squamous epithelium with hyperkeratosis. The superficial dermis showed acute inflammation with localized abscess formation and extensive lymphocytic infiltration (see Figures 2A, B). Microbial examination: At the time of medical consultation, pus was collected from the patient's right middle finger for general bacterial smear and culture. Acid-fast staining of pathological tissue sections revealed acid-fast bacilli (see Figures 2C, D). After 10 days of incubation, colonies emerged. Following a week of sub-culturing on Columbia blood aga rough, flattened, yellow-fleshy colonies were observed (see Figure 3A). Colonies were sub-cultured on Lowenstein-Jensen solid medium and incubated at 28°C for 7 days, resulting in the development of yellow colonies under light exposure (see Figure 3B). The culture smear showed Gram-positive rods, acid-fast staining positive. Based on the culture characteristics and staining, it is highly suspected to be an NTM. The laboratory also identified the isolated bacteria as M. marinum through 16S gene sequence analysis. These photos are of significant importance in the diagnostic process. The histopathological acid-fast staining images and colony morphology photos provide a detailed depiction of the characteristics of M. marinum infection for the first time, aiding clinicians in better identifying and diagnosing such infections. Additionally, these photos offer valuable reference material for the academic community in clinical microbiology, showcasing specific details of laboratory diagnosis and differential diagnosis. The nucleotide homology reached 99.86% with M. marinum from the NCBI database (MK411581.1). We submit the sequences of M. marinum to the GenBank database in NCBI with the accession number of OR876336 (https://www.ncbi.nlm.nih.gov/nuccore/OR876336).
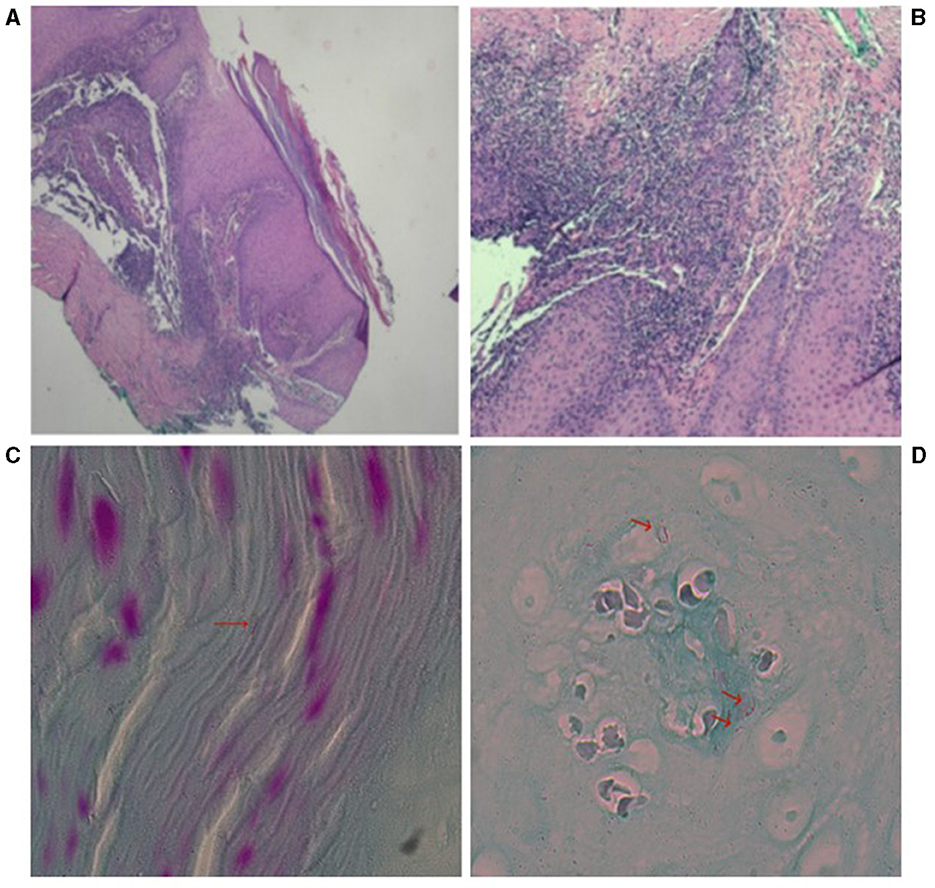
Figure 2. The pathology photograph of the dorsal aspect of the right middle finger joint. (A) Hyperplasia of the squamous epithelium of the epidermis with hyperkeratosis. H&E, magnification, 40X (B) superficial dermal acute inflammation with localized abscess formation and extensive lymphocytic infiltration. H&E, magnification, 100X (C, D) high magnification of acid-fast stained pathological tissue sections from the right middle finger joint showing curved red bacilli.
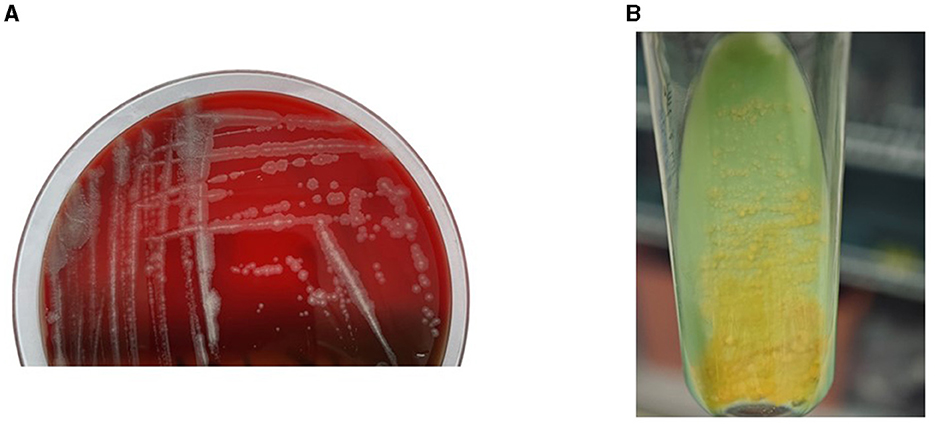
Figure 3. (A) Rough colonies grown on Columbia blood agar. (B) Colonies were subcultured on Lowenstein-Jensen solid medium and incubated at 28°C for 7 days, resulting in the development of yellow colonies under light exposure.
2.3 Treatment
While awaiting laboratory results, the patient received standard postoperative care without any special treatment. Two weeks post-suture removal, spontaneous improvement in the local lesion was noted. Considering the patient's young age, good health, and absence of immunodeficiency, coupled with the infection's location on the extensor side between the second and third interphalangeal joints of the right middle finger, surgical excision was deemed to have a significant aesthetic and functional impact on finger flexion. As the rash showed signs of subsiding, the patient was administered an oral regimen of linezolid (0.6 g daily) and moxifloxacin (0.4 g daily). After 3 months, the rash flattened, and the pain resolved. With an additional 2 weeks of treatment, the rash substantially receded (see Figure 1B), with no recurrence observed for 1-year follow-up.
3 Conclusion
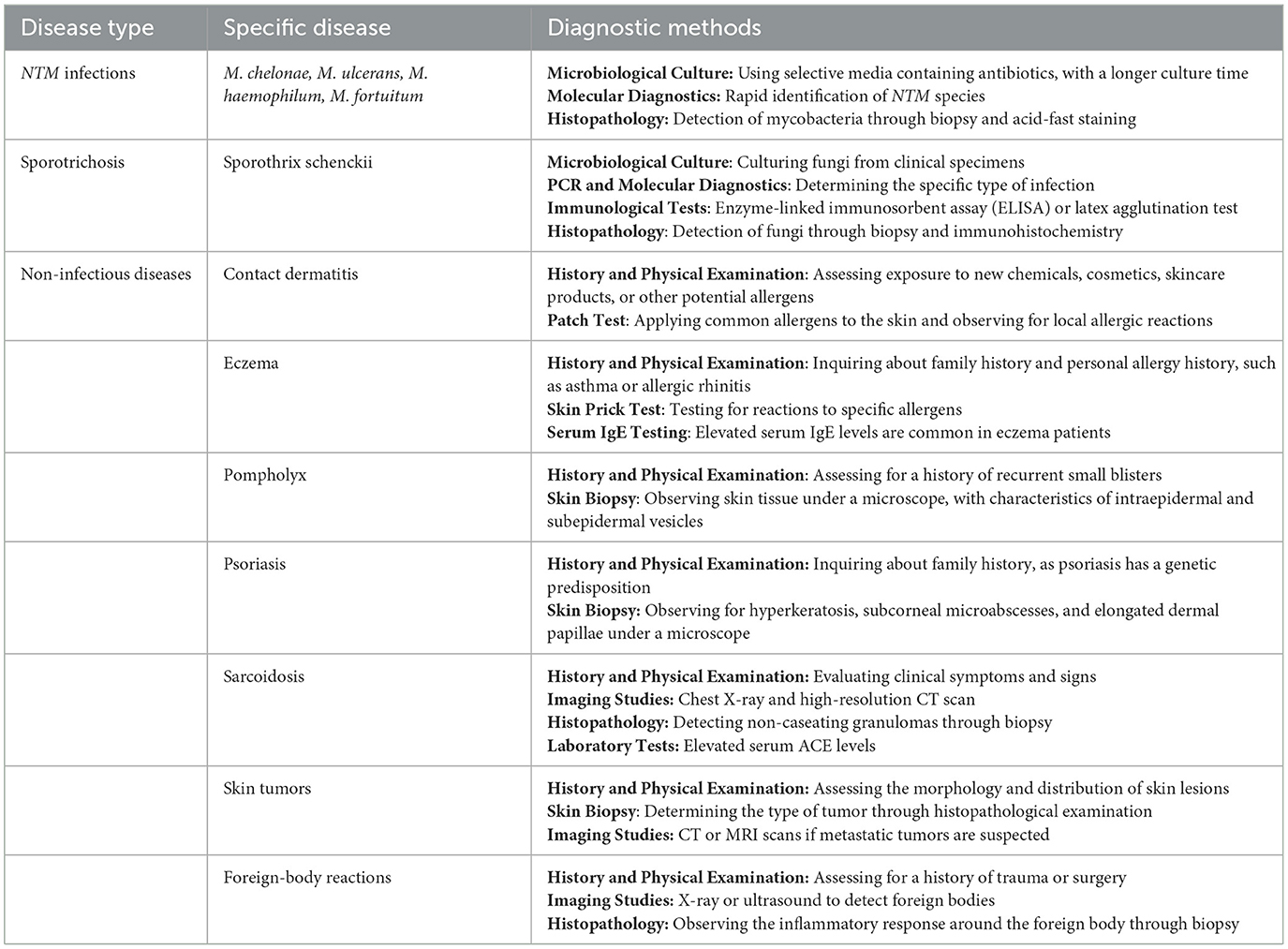
M. marinum infections, while not exceedingly common, are also not rare. Since the initial human skin infection case linked to M. marinum in a contaminated swimming pool reported by Linell and Norden in Sweden in 1951, many case reports and series have been published (9–17). The most common route of infection is through injuries caused by contaminated water or marinum products, especially prevalent in aquarium environments. Here are some possible occupations at risk: (1) Aquarium staff or enthusiasts (16, 18–22). (2) Fishermen and those handling fish and other seafood (including chefs, fishmongers, etc.) (7, 18, 23, 24). (3) Individuals engaged in water activities (10, 20, 25, 26). Reports indicate that fish pedicures can also lead to infection (27). Due to its growth characteristics, M. marinum is most active in water temperatures of 28–32°C and struggles to survive above 37°C. Therefore, it primarily infects the skin and fascia of the hands or lower limbs, especially when abrasions or wounds are present, with lesions appearing after a prolonged incubation period. The infection typically presents with red papules, nodules, ulcers, lymphangitis, cellulitis, or lymphadenopathy, particularly in the upper limbs. Extracutaneous infections may include tenosynovitis, bursitis, arthritis, and osteomyelitis. Individuals with compromised immune systems, such as HIV patients or organ transplant recipients, may experience more severe systemic infections (28). Treatment for M. marinum infection includes antibiotics and surgery, tailored to the patient's specific situation and the severity of the infection. Skin and soft tissue infections are generally treated with oral or intravenous antibiotics, with common antibiotics including macrolides (such as clarithromycin or azithromycin), tetracyclines (such as doxycycline or minocycline), compound sulfonamides, quinolones (such as ciprofloxacin or levofloxacin), aminoglycosides (such as amikacin or gentamicin), rifampicin, and ethambutol. Linezolid, an oxazolidinone antibiotic, has been reported to exhibit in vitro antibacterial activity against M.marinum at clinically achievable concentrations, but prolonged use may result in side effects such as numbness (29–32). Typically, a combination of two or more antibiotics is required, with treatment lasting at least 3 months until complete healing of the skin lesion. In certain cases, such as hand infections, surgical procedures may be necessary to remove infected tissue. For patients with compromised immune systems, treatment may need to be prolonged, and sometimes continuous prophylactic treatment is necessary to prevent recurrence of the infection (33). Therefore, early diagnosis and treatment of M. marinum infection are crucial to avoid serious complications and sequelae. M. marinum infection can be confused with other conditions due to similar clinical presentations. Differential diagnoses include the following aspects: (1) other NTM such as M. chelonae, M. ulcerans, M. haemophilum, and M. fortuitum. (2) Sporotrichosis caused by Sporothrix schenckii. (3) Non-infectious diseases such as contact dermatitis, eczema, pompholyx, psoriasis, sarcoidosis, skin tumors, and foreign-body reactions. Diagnostic methods are shown in Table 1. Accurate diagnosis of M. marinum requires multiple methods: (1) Histopathology: Granulomatous inflammation is usually observed. (2) Microbiological Culture: Cultures are typically positive for M. marinum. (3) 16S rRNA Gene Sequencing and MALDI-TOF Mass Spectrometry: These molecular techniques are crucial for identifying specific mycobacteria. (4) Acid-Fast Staining: Used to detect mycobacteria in tissue samples. Challenges in treating M.marinum infections include: (1) Diagnostic Delays: The average time to diagnosis can be long. (2) Diagnostic Complexity: The clinical manifestations of M.marinum infection are diverse. Eczematous changes may occur, and there may be only scaling and crusting without obvious inflammatory components and infiltration. (3) Treatment Resistance: Some strains may exhibit resistance to common antibiotics, necessitating tailored treatment regimens. Post-treatment sequelae may include: (1) Persistent Skin Lesions: Some patients may experience residual skin changes even after successful treatment. (2) Functional Impairment: Particularly in severe cases with delayed diagnosis and treatment (34). Therefore, Diagnosis requires clinical foresight and a complete patient history, combined with biopsy and subsequent microbiological confirmation. Jernigan et al. reported that the incubation period for M. marinum infection averages 21 days, aiding clinicians in patient history inquiry (35). In recent years, the pathogenic mechanism of M. marinum has been a hot topic, mainly because it is the closest genetic relative to the Mycobacterium tuberculosis complex. Both have a considerable degree of common genetic procedure and host immune response, but M. marinum is easier to manipulate on the experimental bench (36, 37). Mycobacteria utilize five independent Type VII secretion systems, named ESX-1 to ESX-5, which are essential for specific functions (38). Two of these systems, ESX-3 and ESX-5, are indispensable for the bacterium's extracellular growth, making them interesting targets for new antibiotic development (39). Researchers studying M. marinum infection in zebrafish models have better proposed insights into the pathogenic mechanisms of the Mycobacterium tuberculosis complex. Studies have shown that the ESX-1 system plays a significant role in the pathogenicity of M. marinum. This system is a specialized secretion system that is crucial for the virulence of M. marinum, and Ho et al. discovered the dysregulation of the ESX-5 secretion by novel 1,2,4-triazoles against M. marinum (40). By studying this system, we can gain a deeper understanding of the pathogenic mechanisms of M. marinum and the Mycobacterium tuberculosis complex, providing important guidance and insights for the development of new treatment methods and prevention strategies.
This case suggests:
1. Individuals with normal immune function can contract opportunistic NTM infections following trauma. Increased awareness and preventive measures should be emphasized for those frequently in contact with seawater, freshwater environments and seafood, such as fishermen, aquarium workers, water sports enthusiasts and chef. Moreover, with the rise in marinum activities and the consumption of seafood, public awareness and prevention of M. marinum infections should also be strengthened.
2. The clinical foresight of physicians regarding special bacterial infections (as in this case where the initial suspicion was a filamentous fungal infection, prompting the laboratory to extend culture times) and a complete medical history inquiry are instrumental in the early diagnosis of M. marinum infections.
Future research should focus on the epidemiology, pathogenic mechanisms, and treatment strategies for M. marinum infections. This includes studies on antibiotic resistance and improving diagnostic methods for earlier identification and treatment of infections. Additionally, research should explore better ways to educate the public and medical professionals to enhance awareness and prevention of M. marinum infections.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/supplementary material.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
CL: Conceptualization, Writing – review & editing, Resources. JH: Conceptualization, Writing – original draft. MS: Investigation, Writing – review & editing. JY: Investigation, Writing – review & editing. CZ: Writing – review & editing, Resources. YH: Writing – review & editing. ZF: Writing – review & editing. RJ: Writing – review & editing. YS: Writing – review & editing. WG: Writing – review & editing. HZ: Writing – review & editing. ZZ: Writing – review & editing. LZ: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors appreciate the Hebei Medical University Third Hospital for its technical assistance.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Gopalaswamy R, Shanmugam S, Mondal R, Subbian S. Of tuberculosis and NTM infections - a comparative analysis of epidemiology, diagnosis and treatment. J Biomed Sci. (2020) 27:74. doi: 10.1186/s12929-020-00667-6
2. Loret JF, Dumoutier N. Non-tuberculous mycobacteria in drinking water systems: a review of prevalence data and control means. Int J Hyg Environ Health. (2019) 222:628–34. doi: 10.1016/j.ijheh.2019.01.002
3. Monteiro NF, Peres S, Mansinho K. Non-tuberculous mycobacteria: seven-year experience of a tertiary hospital. Acta Med Port. (2019) 32:208–13. doi: 10.20344/amp.10932
4. Sharma SK, Upadhyay V. Epidemiology, diagnosis & treatment of NTM diseases. Indian J Med Res. (2020) 152:185–226. doi: 10.4103/ijmr.IJMR_902_20
5. Aronson JD. Spontaneous tuberculosis in salt water fish. J Infect Dis. (1926) 39:315–20. doi: 10.1093/infdis/39.4.315
6. Norden A, Linell F. A new type of pathogenic Mycobacterium. Nature. (1951) 168:826. doi: 10.1038/168826a0
7. Hashish E, Merwad A, Elgaml S, Amer A, Kamal H, Elsadek A, et al. Mycobacterium marinum infection in fish and man: epidemiology, pathophysiology and management; a review. Vet Q. (2018) 38:35–46. doi: 10.1080/01652176.2018.1447171
8. Zeeli T, Samra Z, Pitlik S. Ill from EEL? Lancet Infect Dis. (2003) 3:168. doi: 10.1016/S1473-3099(03)00548-6
9. Bezerra GH, Honório MLP, Costa VLdC, Vechi HT, Alves MdM, Britto MHMFd, et al. Mycobacterium marinum infection simulating chromomycosis: a case report. Rev Inst Med Trop São Paulo. (2020) 62:e95. doi: 10.1590/s1678-9946202062095
10. Dentel A, Boulanger E, Vignal-Clermont C, Caputo G, Martin GC. Incidence of eye trauma in children associated with foam bullets or foam darts from nonpowder guns. JAMA Ophthalmol. (2023) 141:604–5. doi: 10.1001/jamaophthalmol.2023.1464
11. Gu A, Han F, Ma F, Zhang L. Granuloma features of Mycobacterium marinum infections: a series of 70 retrospective cases. J Cutan Pathol. (2023) 50:1030–3. doi: 10.1111/cup.14527
12. Seidel A, Nunes DH, Fernandes C, Funchal GDG. Skin infection by Mycobacterium marinum – diagnostic and therapeutic challenge. An Bras Dermatol. (2022) 97:366–8. doi: 10.1016/j.abd.2021.03.013
13. Trčko K, Plaznik J, Miljković J. Mycobacterium marinum hand infection masquerading as tinea manuum: a case report and literature review. Acta Dermatovenerol Alpina Pann Adriat. (2021) 30:18. doi: 10.15570/actaapa.2021.23
14. Bouceiro-Mendes R, Ortins-Pina A, Fraga A, Marques T, Viveiros M, Machado D, et al. Mycobacterium marinum lymphocutaneous infection. Dermatol Online J. (2019) 25:42893. doi: 10.5070/D3252042893
15. Chumsaengsri C, Khommee J, Urairerkkul P. Mycobacterium marinum infection of the wrist. Dermatol Online J. (2023) 29:214–8. doi: 10.5070/D329260774
16. Pandian TK, Deziel PJ, Otley CC, Eid AJ, Razonable RR. Mycobacterium marinum infections in transplant recipients: case report and review of the literature. Transpl Infect Dis. (2008) 10:358–63. doi: 10.1111/j.1399-3062.2008.00317.x
17. Patel PM, Camps N, Rivera CI, Tuda C, VanOstran G. Mycobacterium marinum infection and interferon-gamma release assays cross-reactivity: a case report. Cureus. (2022). doi: 10.7759/cureus.21420
18. Bachiyska E, Atanasova Y, Baykova A, Yordanova S, Todorova Y. First etiologically confirmed cases of Mycobacterium marinum infection in Bulgaria. Folia Med. (2020) 62:398–402. doi: 10.3897/folmed.62.e47220
19. Benton J, Karkanevatos A. Preseptal cellulitis due to Mycobacterium marinum. J Laryngol Otol. (2006) 121:606–8. doi: 10.1017/S0022215106005408
20. Drakou A, Psifis M, Mitrou A, Zygoggianis K, Argyropoulou O. Unresolved swelling of the hand: think of Mycobacterium marinum infection. Trauma Case Rep. (2020) 26:100283. doi: 10.1016/j.tcr.2020.100283
21. Macek P, Bodnarova M, Zavada J, Jezek P, Pavlik I, Slany M, et al. Mycobacterium marinum epididymoorchitis: case report and literature review. Urol Int. (2011) 87:120–4. doi: 10.1159/000328220
22. Tuan J, Spichler-Moffarah A, Ogbuagu O. Mycobacterium marinum: nodular hand lesions after a fishing expedition. BMJ Case Rep. (2020) 13:e238835. doi: 10.1136/bcr-2020-238835
23. Agmon-Levin N, Theodor E, Segal RM, Shoenfeld Y. Vitamin D in systemic and organ-specific autoimmune diseases. Clin Rev Allergy Immunol. (2012) 45:256–66. doi: 10.1007/s12016-012-8342-y
24. Liu J, Yao Q, Cheng W, Ren H, Hu W. Mycobacterium marinum infection on both hands masquerading as ‘Eczema'. Am J Med. (2023) 136:e5–6. doi: 10.1016/j.amjmed.2022.09.002
25. Campos M, Sais G, Admella C. Infección cutánea por Mycobacterium marinum. Med Clín. (2017) 148:176–7. doi: 10.1016/j.medcli.2016.07.026
26. Tebruegge M, Connell T, Ritz N, Orchard D, Curtis N. Mycobacterium marinum infection following kayaking injury. Int J Infect Dis. (2010) 14:e305–e6. doi: 10.1016/j.ijid.2010.02.2246
27. Vanhooteghem O, Theate I, De Schaetzen V. Periungual Mycobacterium marinum infection following a fish manicure. Skin Appendage Disord. (2021) 7:393–6. doi: 10.1159/000514853
28. Canetti D, Riccardi N, Antonello RM, Nozza S, Sotgiu G. Mycobacterium marinum: a brief update for clinical purposes. Eur J Intern Med. (2022) 105:15–9. doi: 10.1016/j.ejim.2022.07.013
29. Ojcius DM, Wu T-S, Chiu C-H, Yang C-H, Leu H-S, Huang C-T, et al. Fish tank granuloma caused by Mycobacterium marinum. PLoS ONE. (2012) 7:e41296. doi: 10.1371/journal.pone.0041296
30. Bråbäck M, Riesbeck K, Forsgren A. Susceptibilities of Mycobacterium marinum to gatifloxacin, gemifloxacin, levofloxacin, linezolid, moxifloxacin, telithromycin, and quinupristin-dalfopristin (synercid) compared to its susceptibilities to reference macrolides and quinolones. Antimicr Agents Chemother. (2002) 46:1114–6. doi: 10.1128/AAC.46.4.1114-1116.2002
31. Brown-Elliott BA, Crist CJ, Mann LB, Wilson RW, Wallace RJ. In Vitro Activity of Linezolid against Slowly Growing Nontuberculous Mycobacteria. Antimicr Agents Chemother. (2003) 47:1736–8. doi: 10.1128/AAC.47.5.1736-1738.2003
32. Gilbert DN, Chambers HF, Eliopoulos GM, Saag MS, Pavia AT. The Sanford Guide to Antimicrobial Therapy. 54th ed Sperryville, VA: Antimicrobial Therapy, Inc. (2024).
33. Medel-Plaza M, Esteban J. Current treatment options for Mycobacterium marinum cutaneous infections. Expert Opin Pharmacother. (2023) 24:1113–23. doi: 10.1080/14656566.2023.2211258
34. Veraldi S, Molle M, Nazzaro G. Eczema-like fish tank granuloma: a new clinical presentation of Mycobacterium marinum infection. J Eur Acad Dermatol Venereol. (2018) 32:e200–e1. doi: 10.1111/jdv.14725
35. Jernigan JA, Farr BM. Incubation period and sources of exposure for cutaneous Mycobacterium marinum infection: case report and review of the literature. Clin Infect Dis. (2000) 31:439–43. doi: 10.1086/313972
36. Chirakos AE, Balaram A, Conrad W, Champion PA. Modeling tubercular ESX-1 secretion using Mycobacterium marinum. Microbiol Mol Biol Rev. (2020) 84:10–1128. doi: 10.1128/MMBR.00082-19
37. Tobin DM, Ramakrishnan L. Comparative pathogenesis of Mycobacterium marinum and Mycobacterium tuberculosis. Cell Microbiol. (2008) 10:1027–39. doi: 10.1111/j.1462-5822.2008.01133.x
38. Ates LS, Houben ENG, Bitter W. Type VII secretion: a highly versatile secretion system. Microbiol Spectr. (2016) 4:357–84. doi: 10.1128/9781555819286.ch13
39. Di Luca M, Bottai D, Batoni G, Orgeur M, Aulicino A, Counoupas C, et al. The ESX-5 associated eccB-EccC locus is essential for Mycobacterium tuberculosis viability. PLoS ONE. (2012) 7:e52059. doi: 10.1371/journal.pone.0052059
Keywords: Mycobacterium marinum, skin infection, acid-fast stain, nontuberculous mycobacteria, opportunistic pathogen
Citation: Liu C, Hao J, Song M, Ye J, Zheng C, Huang Y, Feng Z, Jiang R, Shi Y, Gao W, Zuo H, Zhao Z and Zhang L (2024) Mycobacterium marinum hand infection: a case report and literature review. Front. Med. 11:1433153. doi: 10.3389/fmed.2024.1433153
Received: 15 May 2024; Accepted: 19 July 2024;
Published: 09 August 2024.
Edited by:
Gianluca Nazzaro, IRCCS Ca 'Granda Foundation Maggiore Policlinico Hospital, ItalyReviewed by:
Andrea Carugno, University of Insubria, ItalyAnastasia Spiliopoulou, General University Hospital of Patras, Greece
Copyright © 2024 Liu, Hao, Song, Ye, Zheng, Huang, Feng, Jiang, Shi, Gao, Zuo, Zhao and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhenjun Zhao, enpqaG9zcGl0YWxAc2luYS5jb20=; Lijie Zhang, emhhbmdsaWppZUBoZWJtdS5lZHUuY24=
†These authors have contributed equally to this work and share first authorship
 Chunping Liu1†
Chunping Liu1† Lijie Zhang
Lijie Zhang