- 1Department of Cardiology, The Fourth Affiliated Hospital of Soochow University, Medical Center of Soochow University, Suzhou Dushu Lake Hospital, Suzhou, China
- 2Department of Cardiology, The First people’s Hospital of Zhangjiagang, Affiliated Hospital of Soochow University, Medical Center of Soochow University, Zhangjiagang, Jiangsu, China
- 3Institute for Hypertension, Soochow University, Suzhou, China
Irritable bowel syndrome (IBS) is a very common gastrointestinal disease that, although not as aggressive as tumors, affects patients’ quality of life in different ways. The cause of IBS is still unclear, but more and more studies have shown that the characteristics of the gut microbiota, such as diversity, abundance, and composition, are altered in patients with IBS, compared to the healthy population, which confirms that the gut microbiota plays a crucial role in the development of IBS. This paper aims to identify the commonalities by reviewing a large body of literature. Changes in the characteristics of gut microbiota in patients with different types of IBS are discussed, relevant mechanisms are described, and the treatment modalities of gut microbiota in IBS are summarized. Although there are more clinical trials that have made good progress, more standardized, more generalized, larger-scale, multi-omics clinical studies are what is missing. Overall, gut microbiota plays a crucial role in the development of IBS, and there is even more potential for treating IBS by modulating gut microbiota.
Introduction
Irritable bowel syndrome (IBS) is a common chronic gastrointestinal functional disorder characterized by persistent or intermittent abdominal pain, bloating, and changes in bowel habits, along with abnormal stool characteristics (1). According to the Rome IV, IBS can be classified into four subtypes: constipation-predominant (IBS-C), diarrhea-predominant (IBS-D), mixed (IBS-M), and unsubtyped (IBS-U) (2). Although IBS has no identifiable organic pathology in the intestines, it adversely affects the quality of life and work productivity of patients and also can lead to disability (3). Epidemiological studies show that the global prevalence of IBS is about 10–20% and continues to increase yearly (4). Currently, IBS lacks definitive diagnostic criteria and is clinically diagnosed based on the patient’s symptoms and medical history, alongside imaging and endoscopy to exclude other organic diseases (5). The exact pathophysiology of IBS remains unclear, but it may be related to changes in gastrointestinal motility, visceral hypersensitivity, low-grade mucosal inflammation, environmental factors, gut microbiota imbalance, and psychosocial disorders (6).
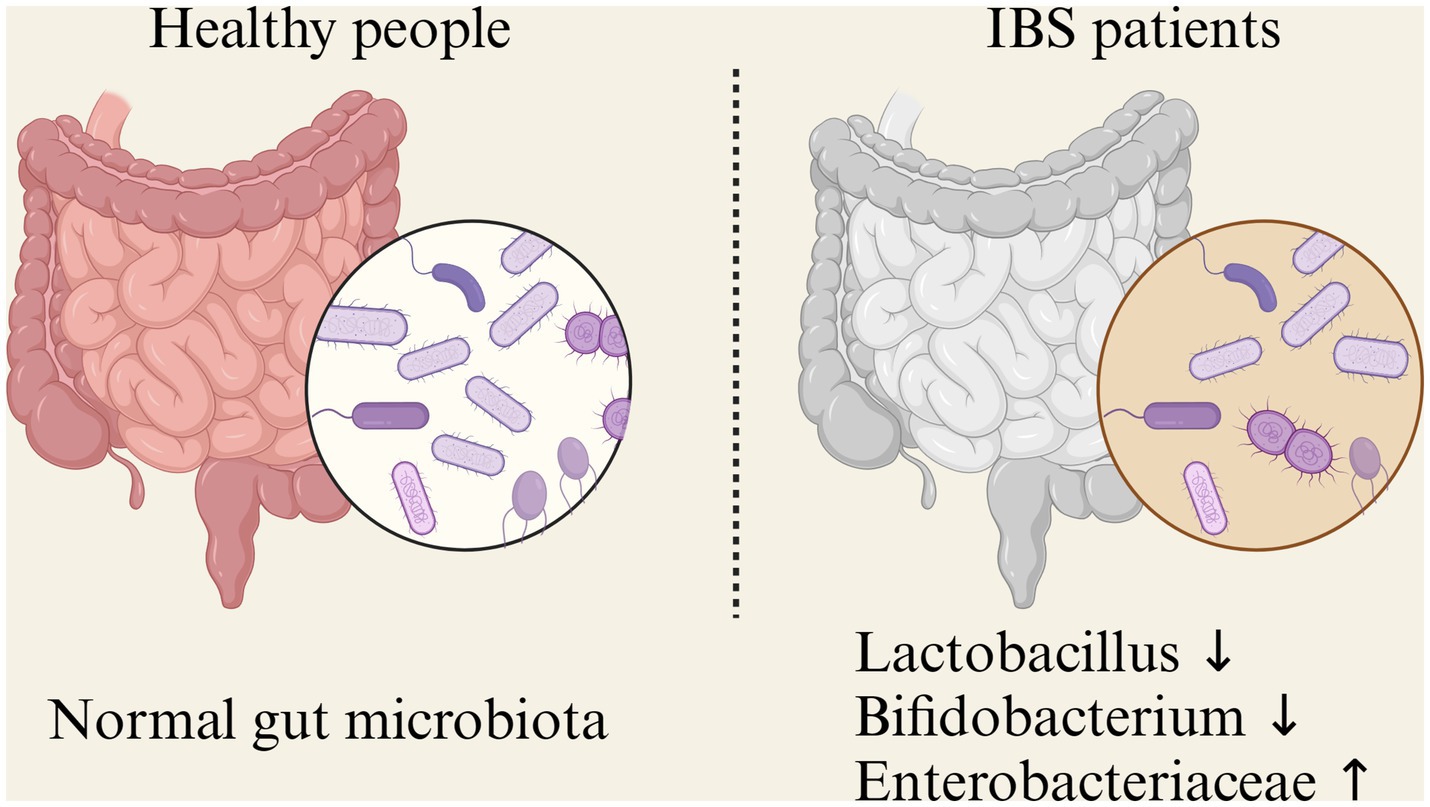
The gut microbiome is a collective term for the complex ecosystem of microorganisms in the intestines, including bacteria, viruses, fungi, and protozoa. Bacteria dominate, constituting over 99%, thus it is also known as the gut microbiota. High-throughput sequencing reveals that the human gut contains about 500–1,000 species of microbes, with a count of up to 1014, approximately 10 times the number of human cells (7). In healthy adults, over 90% of gut bacteria belong to four dominant phyla: Firmicutes, Bacteroidetes, Actinobacteria, and Proteobacteria. Other phyla have much lower abundances (8). Based on their functions, intestinal microbiota can be broadly classified into two categories:functional bacteria and pathogenic bacteria. Functional bacteria primarily including Bacteroides, Clostridium, Bifidobacterium, and Lactobacillus. They are abundant, comprising over 99% of the gut microbiota. Commensal bacteria can synthesize various vitamins, use protein residue to produce essential amino acids, and participate in carbohydrate and protein metabolism. They also facilitate the absorption of minerals like iron, magnesium, and zinc. They also contribute to food digestion, stimulate gut motility, inhibit pathogenic bacteria growth, and break down harmful and toxic substances. The second type is the pathogenic bacteria, including opportunistic pathogenic bacteria and pathogenic bacteria. Opportunistic pathogenic bacteria, primarily Enterococcus and Enterobacteriaceae. When the immune system is weakened, these bacteria can multiply excessively or migrate, leading to gut environment imbalance and intestinal disease. Although not numerous, they are highly mobile, considered foreign bacteria, and represent unstable factors in the gut. Pathogenic bacteria, primarily Salmonella and pathogenic Escherichia coli. They usually enter the gut through accidental ingestion and produce harmful substances like nitroso compounds and colicins, affecting immune function and causing various diseases (9). When the body is influenced by environmental factors, diet, medication, and other external elements, the composition and function of the gut microbiota can change, a condition known as gut dysbiosis (Figure 1).
Notably, current gut microbiota samples are usually collected via stool samples, which is easy to implement in clinical practice but has significant limitations. Some studies suggest that the mucosa-associated microbiota is more closely linked to host cells (10). One study used ingestible devices to collect samples from different regions of the small intestine and compared them to stool samples, revealing significant differences in microbiome composition. Li et al., through 16S rRNA sequencing of duodenal, rectal, and fecal samples, found that the alpha diversity and phylogenetic diversity of the duodenal microbiota were higher than those of the rectal and fecal samples. Their study also revealed that the duodenal samples had a higher abundance of Proteobacteria, with Acinetobacter and Prevotella being predominant in the duodenum, while Bacteroides and Prevotella dominated in the rectum (11). This offers new insights for future research on gut microbiota.
Microbial dysbiosis in IBS subtypes
So far, increasing evidence suggests that microbial dysbiosis leads to the development of IBS (12). This results from disruptions in host-microbiome interactions (13). By leveraging increasingly advanced next-generation sequencing technologies, such as metagenomics and 16S rRNA sequencing, our understanding of microbial ecology and host–microbe interactions has now reached the DNA level (14). High-throughput sequencing has revealed changes in microbial diversity, abundance, and composition in IBS.
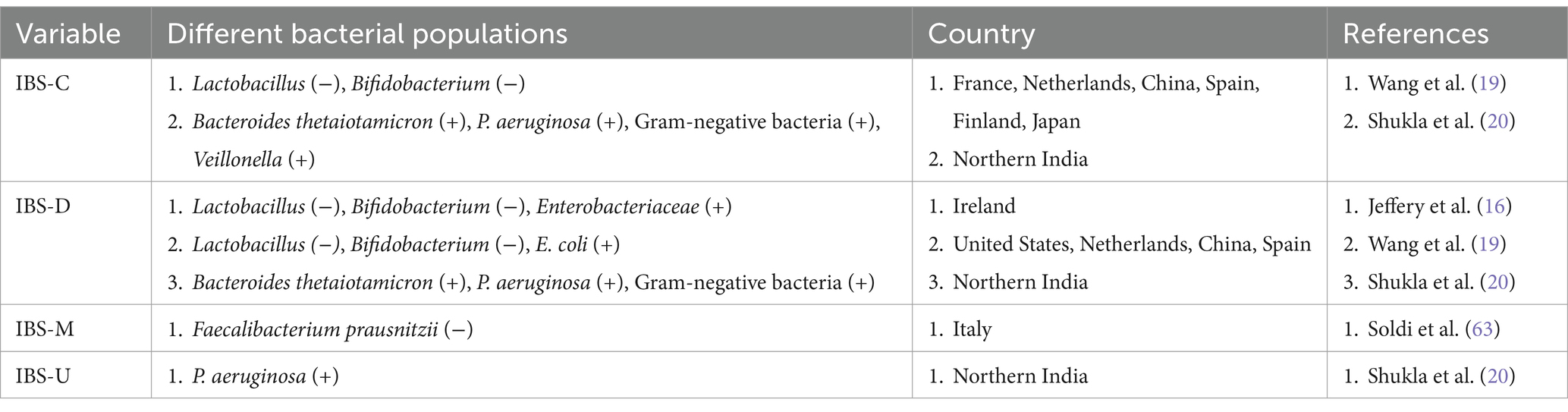
At the phylum level, most studies show that Proteobacteria increase in IBS patients (15). Several studies have also shown that IBS patients have a reduced number of Lactobacillus species, while the abundance of Ruminococcus gnavus and Lachnospiraceae is significantly higher. In contrast, Barnesiella intestinihominis and Coprococcus catus are found in notably lower abundance in IBS patients (16–18). Although some research indicates no significant differences between IBS patients and controls (12). Research on the other three phyla (Bacteroidetes, Actinobacteria, and Firmicutes) shows varying results (Figure 2).
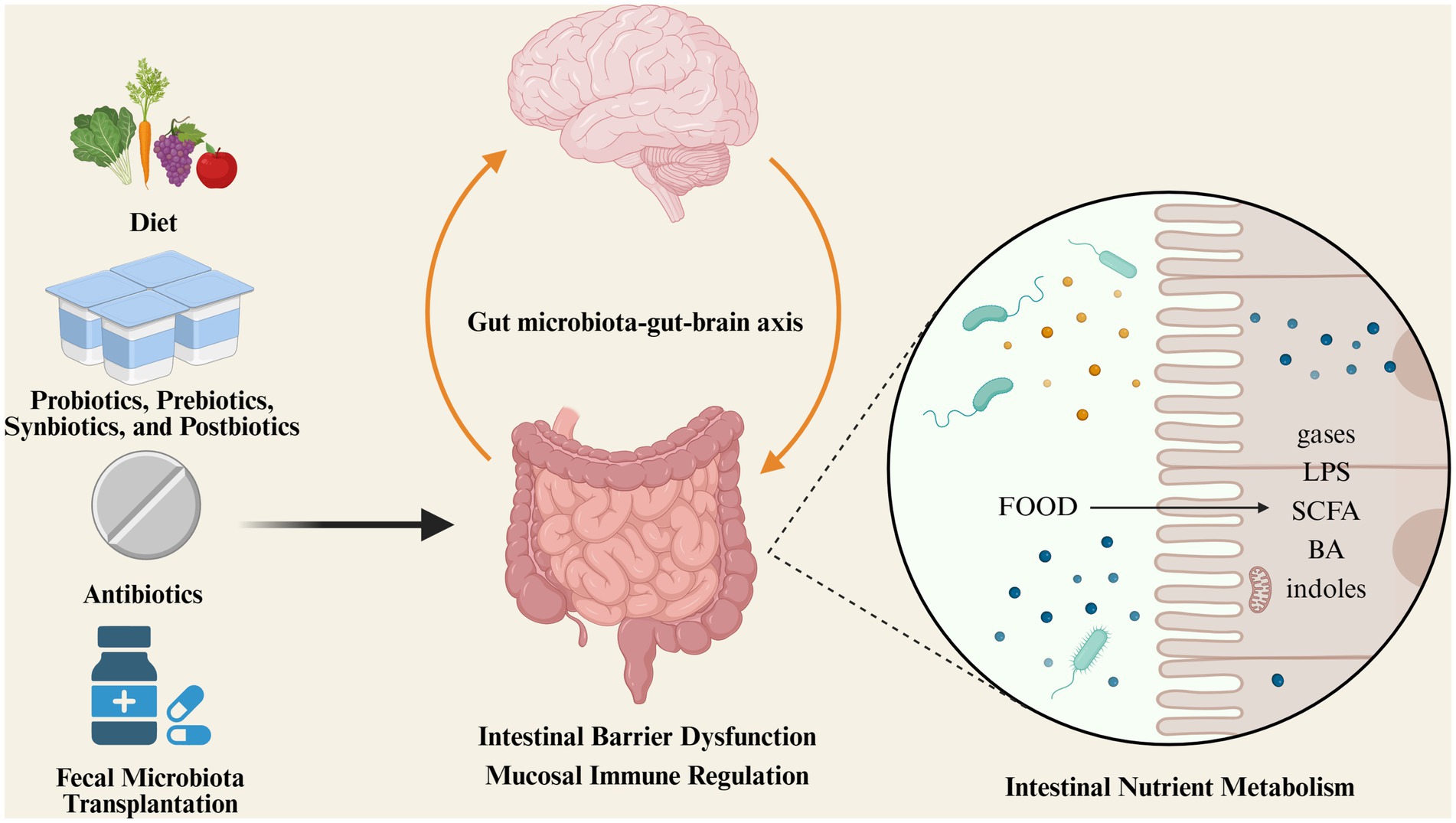
Figure 2. Gut microbiota influences the progression of IBS through different mechanisms; microbiota-targeted therapeutic approaches in IBS.
Some consistent findings exist: Jeffery’s observations show that IBS-D patients have reduced levels of Lactobacillus and Bifidobacterium, with elevated Enterobacteriaceae levels compared to healthy controls (16). Wang’s meta-analysis shows that probiotic levels decrease while pathogenic bacteria levels increase in IBS-D patients, This finding may reflect the patients’ history of prior gut infections. Another possible explanation for this observation could be changes in the gut environment, including a reduction in strict anaerobes, as well as increased inflammation and gastrointestinal motility, which favor the growth of facultative and less fastidious bacteria, such as Enterobacteriaceae. However, there may be some bias in these data (19). A meta-analysis of a randomized controlled trial studying the gut microbiota of IBS-C patients shows a significant increase in fecal Bacteroides, with no notable increase in Bifidobacterium, Lactobacillus, Enterobacteriaceae, or Enterococcus colony counts, and no differences in gut colonization resistance compared to healthy individuals (20). Research findings on IBS-M patients vary widely, A study by Soldi et al. found that the levels of Faecalibacterium prausnitzii were reduced in IBS-M patients, but increased after treatment with rifaximin, suggesting that F. prausnitzii may have some specificity in IBS-M. However, given the small sample size, the generalizability of these findings remains uncertain. But all further confirm that the development of this condition is closely tied to gut dysbiosis. Due to the small proportion of IBS-U patients, research focusing on this subtype is limited. A study on a South Indian population found an increase in Pseudomonas aeruginosa in IBS-U patients (21).
Differences in experimental methodology, target populations, psychological stress, and dietary habits lead to inconsistencies in microbial diversity and abundance among IBS patients (22). To better understand the relationship between the gut microbiota and IBS, experimental processes, such as inclusion criteria, specimen processing workflows, and data analysis, should be standardized for more reliable results. Furthermore, longitudinal and integrated multi-omics analyses are necessary for a deeper understanding of the gut microbiome’s role (14).
The role of microbial dysbiosis in IBS pathogenesis
Based on the aforementioned studies, changes in the gut microbiota are related to the development and progression of IBS. However, the causal relationship is still unclear. Physiological changes in the gut caused by IBS could be responsible for changes in the gut microbiota and its functions. Conversely, gut dysbiosis may be the key initial factor for pathophysiological changes in IBS (23). Current evidence indicates that these conditions may coexist. In any case, the gut microbiota’s effects on nutrient metabolism, gut barrier dysfunction, mucosal immunity, and the brain-gut-microbiome (BGM) axis are crucial for understanding why it plays a vital role in the onset and persistence of IBS.
Intestinal nutrient metabolism
The metabolic substrates of the gut microbiota mainly come from undigested or indigestible food and endogenous mucus secreted by intestinal epithelial cells. Through a series of metabolic processes, gut bacteria produce beneficial and harmful metabolites, such as gasses (hydrogen sulfide, methane), lipopolysaccharides, peptidoglycans, short-chain fatty acids (SCFAs), bile acids, and indoles.
Previous studies have shown that the gut microbiota of IBS-C patients exhibit greater distinctiveness and variability compared to healthy individuals and IBS-D patients (14). Among the various bacterial metabolic products, short-chain fatty acids (SCFAs) are globally acknowledged for their crucial role in maintaining colonic homeostasis (24). SCFAs are the by-products of carbohydrate fermentation by symbiotic anaerobic bacteria, playing a key role in preserving gut barrier integrity, regulating immune function, and possessing anti-inflammatory properties. Studies have shown that the levels of short-chain fatty acids are reduced in IBS-C patients compared to those with IBS-U and IBS-D (25). Therefore, short-chain fatty acids have the potential to serve as biomarkers for IBS. Additionally, evidence suggests that lipopolysaccharides, derived from commensal bacteria, regulate IBS-related visceral sensation, mucosal inflammation, and gut barrier dysfunction by activating toll-like receptor 4 (TLR4) (26). Changes in the abundance and diversity of the gut microbiota also have a profound impact on bile acid metabolism, ultimately leading to IBS (27). In summary, gut microbiota metabolites may act as messengers, regulating host gastrointestinal function and influencing the occurrence and progression of IBS.
Intestinal barrier dysfunction
In one study, pre-treatment with a Lactobacillus rhamnosus derivative prevented increased intestinal permeability in IBS patients, alleviating symptoms. This indicates a link between gut dysbiosis and intestinal barrier function in IBS (28). Changes in the gut microbiota could impair intestinal barrier function in IBS patients through various mechanisms, including metabolic and immune pathways. Previous studies have shown that increased intestinal mucosal permeability in IBS patients is likely related to the expression and distribution of tight junction protein ZO-2 in the intestinal epithelium (29). E. coli promotes ZO-2 expression, enhances the barrier function of epithelial cell tight junction complexes, and can even repair the intestinal epithelial barrier damaged by pathogenic E. coli (30). Additionally, in IBS patients, the expression levels of tight junction proteins such as Occludin and Claudin-1 were found to be reduced in the duodenum, jejunum, and colon (31, 32). Interestingly, the microbiota has been found to regulate the expression of these tight junction proteins (33), and an increased passage of bacteria through the intestinal barrier has been observed (34). This further demonstrates that gut dysbiosis contributes to the development of IBS by causing intestinal barrier dysfunction.
Mucosal immune regulation
Several studies have shown that the mucosal immune system in IBS patients is imbalanced (35), characterized by elevated inflammatory factor expression and immune cell activation. It has been reported that in IBS-D patients, the levels of 5-HT and 5-HT3 receptors in the intestinal mucosa are significantly higher than in healthy controls, indicating that the 5-HT system is impaired in IBS patients (36). An interesting finding in IBS patients is the increased expression of Toll-like receptors (TLRs) (37). These receptors are present in various cells, including intestinal epithelial cells and immune cells, and are closely related to neural and immune receptors involved in regulating intestinal mucosal homeostasis (38). TLRs recognize specific microbial components of both commensal and pathogenic bacteria, playing a role in immune tolerance to commensals and defense against pathogens (39). However, the exact pathways and targets by which the gut microbiota affects intestinal immunity are still debated and remain inconclusive.
Gut microbiota-gut-brain axis
The brain-gut axis is a bidirectional neural pathway consisting of the central nervous system, the enteric nervous system, and the autonomic nervous system, including visceral sensory conduction, neuroendocrine-immune regulation, and stress response pathways (40). Some researchers believe the brain-gut axis plays a key role in IBS pathogenesis, and the gut microbiota may also participate in this process. The interaction between the gut microbiota and the gut-brain axis is called the gut microbiota-gut-brain axis (41). Research indicates that the vagus nerve is a primary regulator of the microbiota-gut-brain (MGB) axis. It is composed of somatic and afferent fibers (80%) and general and special visceral efferent fibers (20%). Under normal conditions, the vagus nerve has sensory functions and is activated by diet-responsive gut microbes, metabolites, endocrine factors, enzymes, and neurotransmitters (42). Each of these factors can be influenced by changes in the microbiota composition and play a role in IBS pathology. In the gut, the vagal nerve endings synapse onto neurons in the enteric nervous system (ENS), which controls the function of gastrointestinal muscles, neurohormones, and secretion systems to produce functional digestive patterns. In IBS, the pathophysiology involves alterations in the gut microbiota composition, compromised mucosal integrity, and low-grade inflammation (6). Beyond the circulatory pathways, some of these factors may also trigger fluctuations in ENS activity, thereby impacting the brain. This bidirectional signaling relationship can be disrupted by chronic IBS. In the brain of chronic IBS patients, efferent signals may be perceived as unpleasant or painful, potentially leading to chronic visceral discomfort or pain (43). Gut dysbiosis activates the intestinal mucosal immune system, thereby disrupting the intestinal epithelial barrier function and causing visceral hypersensitivity and gastrointestinal motility disorders in IBS patients, which leads to abdominal pain, diarrhea, or worsening of existing symptoms. The gut microbiota and the brain are interconnected and can influence each other, jointly regulating gastrointestinal neural, endocrine, and immune functions, thus playing a role in the development and progression of IBS.
Microbiota therapeutic approaches in IBS
Increasing evidence indicates that changes in the gut microbiota are related to the development and progression of IBS. Regarding current gut microbiota treatment strategies, many promising results have been achieved, such as gut microbiota-targeted therapy being recommended for diarrhea-predominant IBS (IBS-D). Currently, finding safer and more effective gut microbiota-based treatments has become a major focus of IBS research.
Diet
In recent decades, dietary control has gradually become more prominent in IBS treatment. Initially, dietary recommendations for IBS were drawn from guidelines by the National Institute for Health and Care Excellence (NICE) (44) and the British Dietetic Association (BDA) (45). They emphasized self-management through lifestyle, diet, exercise, and symptom-based medication education. Recent studies show that a low FODMAP (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) diet has significant advantages over the BDA/NICE diet in alleviating certain clinical symptoms, especially bloating (46). The FODMAP diet increases water in the colon due to osmotic effects, leading to diarrhea. It may also be fermented by the gut microbiota, resulting in excessive gas that worsens bloating in IBS patients. However, a low FODMAP diet reduces fiber intake and may cause constipation in some patients (47). Therefore, IBS patients need to adjust according to their individual conditions.
Studies have found that a low FODMAP diet significantly reduces Bifidobacterium levels and decreases the overall bacterial count, thereby changing the gut microbiome composition (48). A comprehensive systematic review and meta-analysis of 12 trials involving 772 patients studied the effects of a low FODMAP diet on IBS symptoms in most studies. Results showed a significant improvement in IBS severity according to the IBS Severity Scoring System (IBS-SSS), with higher IBS-QoL scores compared to the control group (49). However, a low FODMAP diet does not have the same effect on different IBS subtypes, which may be related to the specific components of the diet (Table 1).
Probiotics, prebiotics, synbiotics, and postbiotics
Probiotics are orally active microorganisms that can colonize the gastrointestinal tract (50). Prebiotics are indigestible food components that selectively promote the growth or activity of beneficial bacteria to improve patient symptoms (51). Synbiotics are mixtures of probiotics and prebiotics (52), while postbiotics are active substances produced by bacteria, such as bacteriocins, vitamins, and short-chain fatty acids (SCFAs) (53). Several randomized controlled trials (RCTs) show that treatment with specific probiotics, such as Lactobacillus plantarum, Bacillus coagulans, or multi-strain probiotic formulations, significantly improves abdominal pain, bowel movement frequency, and quality of life in IBS-D patients (54). A meta-analysis of 10 studies involving 757 patients evaluated the effects of probiotics on IBS-C patients. Compared to a placebo, probiotics significantly improved diarrhea symptoms but did not show significant differences in abdominal pain or bloating (55). Studies on prebiotics found that taking non-inulin fructooligosaccharides significantly improved gastrointestinal bloating (56), but research on synbiotics and postbiotics remains multiple.
Although the American Gastroenterological Association currently does not support probiotics for IBS treatment (57), it cannot be denied that they could be a breakthrough treatment. However, this requires further large-scale RCTs to clarify the role of these compounds in treating IBS.
Antibiotics
Research indicates that using antibiotics to reset the gut microbiota could be a novel approach for treating IBS. Several randomized controlled trials show that antibiotics like rifaximin, neomycin, and norfloxacin can alleviate IBS symptoms (58). However, indiscriminate use of antibiotics can lead to side effects, adverse reactions, antibiotic resistance, and severe gut dysbiosis, limiting their application in IBS treatment (59). Currently, rifaximin is the only antibiotic approved by the U.S. Food and Drug Administration (FDA) for IBS treatment, but its approved application range is very limited (57). The standard dosage is 550 mg, taken three times daily for 2 weeks.
Fecal microbiota transplantation
With increasing awareness of the relationship between gut dysbiosis and disease onset, FMT has gained more attention in the past decade. FMT was first approved by the FDA in 2013 for the treatment of Clostridium difficile infection (60). Since then, multiple studies have explored FMT for IBS patients, but results have shown inconsistencies. Although there is significant controversy regarding the effectiveness of FMT for IBS, some studies indicate that IBS patients can benefit from it (61). A systematic review summarized results from seven randomized controlled trials (RCTs) on FMT for IBS, and four RCTs found that FMT was effective for IBS outcomes, including symptom relief and improved quality of life, while the other three showed no effect (62). However, the administration methods and adverse reactions of FMT remain significant concerns. Currently, FMT is not recommended as a primary treatment option for IBS patients, as there is still a long way to go in exploring this approach.
Reflections and perspectives
IBS is a common multifactorial functional gastrointestinal disease. Despite its benign nature, it remains challenging to manage and treat fully.
Research over the past few decades shows that gut dysbiosis is closely linked to the development and progression of IBS, though the causal relationship remains unclear. Nevertheless, the effects of gut dysbiosis on intestinal nutrient metabolism impairment, intestinal barrier dysfunction, mucosal immunity, and the brain-gut-microbiome (BGM) axis are key factors influencing the development and progression of IBS. Identifying the precise composition of the gut microbiota is crucial to unraveling this relationship and unlocking the mysteries of IBS.
Although treatment methods targeting the gut microbiota are currently contentious, they still offer promising prospects for IBS patients. This paper aims to analyze the relationship between the gut microbiota and IBS, as well as potential treatment options. Since every patient’s gut microbiota composition differs, individual responses to the same treatment can vary. Therefore, new detection methods and stable treatment approaches need in-depth exploration, such as whether the mucosa-associated microbiota aligns with the fecal microbiota, and how prebiotics, synbiotics, postbiotics, and fecal transplantation can be optimized for breakthroughs in the coming years.
Multi-omics analysis is enabling a transition toward personalized IBS characterization and treatment plans. However, this requires further longitudinal multi-omics studies and functional research into the genetic basis and mechanisms underlying gut microbiota-host interactions. Such research will enhance our understanding of the role of gut colonizers in IBS, guiding the development of more targeted dietary and therapeutic approaches, and ultimately leading to microbiome-targeted therapies.
Author contributions
XC: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. CR: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. XM: Conceptualization, Investigation, Methodology, Software, Writing – original draft, Writing – review & editing. YJ: Conceptualization, Investigation, Methodology, Software, Writing – original draft, Writing – review & editing. YZ: Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing, Investigation.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by grants from The Natural Science Foundation of the Jiangsu Higher Education Institutions of China (23KJB320020), Medical research project of Jiangsu Provincial Health Commission (Z2021011), Biomedical translational medicine innovation and applied research project (SZM2021020), Project of Suzhou Science and Technology Development Program (Applied Basic Research, SKJYD2021045), the Science and Technology Development Program of Jiangsu Province-Clinical Frontier Technology (BE2022754), Clinical Medicine Expert Team (Class A) of Jinji Lake Health Talents Program of Suzhou Industrial Park (SZYQTD202102), Suzhou Key Discipline for Medicine (SZXK202129), Demonstration of Scientifc and Technological Innovation Project (SKY2021002), Suzhou Dedicated Project on Diagnosis and Treatment Technology of Major Diseases (LCZX202132), Research on Collaborative Innovation of medical engineering combination (SZM2021014, SZM2022003, SZM2022019), Suzhou Key Laboratory of Diagnosis and Treatment of Panvascular Diseases (SZS2023021). The funders had no roles in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Acknowledgments
We would like to thank the members and staff of the Department of Cardiology, The Fourth Affiliated Hospital of Soochow University, Medical Center of Soochow University, Suzhou Dushu Lake Hospital who contributed to this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ford, AC, Sperber, AD, Corsetti, M, and Camilleri, M. Irritable bowel syndrome. Lancet. (2020) 396:1675–88. doi: 10.1016/S0140-6736(20)31548-8
2. Palsson, OS, Whitehead, WE, van Tilburg, MAL, Chang, L, Chey, W, Crowell, MD, et al. Rome IV diagnostic questionnaires and tables for investigators and clinicians. Gastroenterology. (2016) 150:1481–91. doi: 10.1053/j.gastro.2016.02.014
3. Fond, G, Loundou, A, Hamdani, N, Boukouaci, W, Dargel, A, Oliveira, J, et al. Anxiety and depression comorbidities in irritable bowel syndrome (IBS): a systematic review and meta-analysis. Eur Arch Psychiatry Clin Neurosci. (2014) 264:651–60. doi: 10.1007/s00406-014-0502-z
4. Staudacher, HM, Black, CJ, Teasdale, SB, Mikocka-Walus, A, and Keefer, L. Irritable bowel syndrome and mental health comorbidity-approach to multidisciplinary management. Nat Rev Gastroenterol Hepatol. (2023) 20:582–96. doi: 10.1038/s41575-023-00794-z
5. Pittayanon, R, Lau, JT, Yuan, Y, Leontiadis, GI, Tse, F, Surette, M, et al. Gut microbiota in patients with irritable bowel syndrome—a systematic review. Gastroenterology. (2019) 157:97–108. doi: 10.1053/j.gastro.2019.03.049
6. Enck, P, Aziz, Q, Barbara, G, Farmer, AD, Fukudo, S, Mayer, EA, et al. Irritable bowel syndrome. Nat Rev Dis Primers. (2016) 2:16014. doi: 10.1038/nrdp.2016.14
7. Thursby, E, and Juge, N. Introduction to the human gut microbiota. Biochem J. (2017) 474:1823–36. doi: 10.1042/BCJ20160510
8. Zhuang, X, Tian, Z, Li, L, Zeng, Z, Chen, M, and Xiong, L. Fecal microbiota alterations associated with diarrhea-predominant irritable bowel syndrome. Front Microbiol. (2018) 9:1600. doi: 10.3389/fmicb.2018.01600
9. Vaga, S, Lee, S, Ji, B, Andreasson, A, Talley, NJ, Agréus, L, et al. Compositional and functional differences of the mucosal microbiota along the intestine of healthy individuals. Sci Rep. (2020) 10:14977. doi: 10.1038/s41598-020-71939-2
10. Shalon, D, Culver, RN, Grembi, JA, Folz, J, Treit, PV, Shi, H, et al. Profiling the human intestinal environment under physiological conditions. Nature. (2023) 617:581–91. doi: 10.1038/s41586-023-05989-7
11. Li, G, Yang, M, Zhou, K, Zhang, L, Tian, L, Lv, S, et al. Diversity of duodenal and rectal microbiota in biopsy tissues and luminal contents in healthy volunteers. J Microbiol Biotechnol. (2015) 25:1136–45. doi: 10.4014/jmb.1412.12047
12. Mazzawi, T. Gut microbiota manipulation in irritable bowel syndrome. Microorganisms. (2022) 10:1332. doi: 10.3390/microorganisms10071332
13. Singh, P, and Lembo, A. Emerging role of the gut microbiome in irritable bowel syndrome. Gastroenterol Clin N Am. (2021) 50:523–45. doi: 10.1016/j.gtc.2021.03.003
14. Mars, RAT, Yang, Y, Ward, T, Houtti, M, Priya, S, Lekatz, HR, et al. Longitudinal multi-omics reveals subset-specific mechanisms underlying irritable bowel syndrome. Cell. (2020) 182:1460–1473.e17. doi: 10.1016/j.cell.2020.08.007
15. Rangel, I, Sundin, J, Fuentes, S, Repsilber, D, de Vos, WM, and Brummer, RJ. The relationship between faecal-associated and mucosal-associated microbiota in irritable bowel syndrome patients and healthy subjects. Aliment Pharmacol Ther. (2015) 42:1211–21. doi: 10.1111/apt.13399
16. Jeffery, IB, Das, A, O'Herlihy, E, Coughlan, S, Cisek, K, Moore, M, et al. Differences in fecal microbiomes and metabolomes of people with vs without irritable bowel syndrome and bile acid malabsorption. Gastroenterology. (2020) 158:1016–1028.e8. doi: 10.1053/j.gastro.2019.11.301
17. Rajilić-Stojanović, M, Biagi, E, Heilig, HG, Kajander, K, Kekkonen, RA, Tims, S, et al. Global and deep molecular analysis of microbiota signatures in fecal samples from patients with irritable bowel syndrome. Gastroenterology. (2011) 141:1792–801. doi: 10.1053/j.gastro.2011.07.043
18. Tap, J, Derrien, M, Törnblom, H, Brazeilles, R, Cools-Portier, S, Doré, J, et al. Identification of an intestinal microbiota signature associated with severity of irritable bowel syndrome. Gastroenterology. (2017) 152:111–123.e8. doi: 10.1053/j.gastro.2016.09.049
19. Wang, L, Alammar, N, Singh, R, Nanavati, J, Song, Y, Chaudhary, R, et al. Gut microbial Dysbiosis in the irritable bowel syndrome: a systematic review and Meta-analysis of case-control studies. J Acad Nutr Diet. (2020) 120:565–86. doi: 10.1016/j.jand.2019.05.015
20. Shukla, R, Ghoshal, U, Dhole, TN, and Ghoshal, UC. Fecal microbiota in patients with irritable bowel syndrome compared with healthy controls using real-time polymerase chain reaction: an evidence of Dysbiosis. Dig Dis Sci. (2015) 60:2953–62. doi: 10.1007/s10620-015-3607-y
21. Ghoshal, UC, Shukla, R, and Ghoshal, U. Small intestinal bacterial overgrowth and irritable bowel syndrome: a bridge between functional organic dichotomy. Gut Liver. (2017) 11:196–208. doi: 10.5009/gnl16126
22. Zhao, Y, and Zou, DW. Gut microbiota and irritable bowel syndrome. J Dig Dis. (2023) 24:312–20. doi: 10.1111/1751-2980.13204
23. Mishima, Y, and Ishihara, S. Enteric microbiota-mediated serotonergic signaling in pathogenesis of irritable bowel syndrome. Int J Mol Sci. (2021) 22:10235. doi: 10.3390/ijms221910235
24. Tan, J, McKenzie, C, Potamitis, M, Thorburn, AN, Mackay, CR, and Macia, L. The role of short-chain fatty acids in health and disease. Adv Immunol. (2014) 121:91–119. doi: 10.1016/B978-0-12-800100-4.00003-9
25. Gargari, G, Taverniti, V, Gardana, C, Cremon, C, Canducci, F, Pagano, I, et al. Fecal Clostridiales distribution and short-chain fatty acids reflect bowel habits in irritable bowel syndrome. Environ Microbiol. (2018) 20:3201–13. doi: 10.1111/1462-2920.14271
26. Jalanka-Tuovinen, J, Salojärvi, J, Salonen, A, Immonen, O, Garsed, K, Kelly, FM, et al. Faecal microbiota composition and host-microbe cross-talk following gastroenteritis and in postinfectious irritable bowel syndrome. Gut. (2014) 63:1737–45. doi: 10.1136/gutjnl-2013-305994
27. Fan, Y, and Pedersen, O. Gut microbiota in human metabolic health and disease. Nat Rev Microbiol. (2021) 19:55–71. doi: 10.1038/s41579-020-0433-9
28. Han, X, Lee, A, Huang, S, Gao, J, Spence, JR, and Owyang, C. Lactobacillus rhamnosus GG prevents epithelial barrier dysfunction induced by interferon-gamma and fecal supernatants from irritable bowel syndrome patients in human intestinal enteroids and colonoids. Gut Microbes. (2019) 10:59–76. doi: 10.1080/19490976.2018.1479625
29. Zyrek, AA, Cichon, C, Helms, S, Enders, C, Sonnenborn, U, and Schmidt, MA. Molecular mechanisms underlying the probiotic effects of Escherichia coli Nissle 1917 involve ZO-2 and PKCzeta redistribution resulting in tight junction and epithelial barrier repair. Cell Microbiol. (2007) 9:804–16. doi: 10.1111/j.1462-5822.2006.00836.x
30. Gecse, K, Roka, R, Ferrier, L, Leveque, M, Eutamene, H, Cartier, C, et al. Increased faecal serine protease activity in diarrhoeic IBS patients: a colonic lumenal factor impairing colonic permeability and sensitivity. Gut. (2008) 57:591–9. doi: 10.1136/gut.2007.140210
31. Hanning, N, Edwinson, AL, Ceuleers, H, Peters, SA, de Man, JG, Hassett, LC, et al. Intestinal barrier dysfunction in irritable bowel syndrome: a systematic review. Ther Adv Gastroenterol. (2021) 14:1756284821993586. doi: 10.1177/1756284821993586
32. Zhu, H, Xiao, X, Shi, Y, Wu, Y, Huang, Y, Li, D, et al. Inhibition of miRNA-29a regulates intestinal barrier function in diarrhea-predominant irritable bowel syndrome by upregulating ZO-1 and CLDN1. Exp Ther Med. (2020) 20:155. doi: 10.3892/etm.2020.9284
33. Singh, R, Chandrashekharappa, S, Bodduluri, SR, Baby, BV, Hegde, B, Kotla, NG, et al. Enhancement of the gut barrier integrity by a microbial metabolite through the Nrf2 pathway. Nat Commun. (2019) 10:89. doi: 10.1038/s41467-018-07859-7
34. Bednarska, O, Walter, SA, Casado-Bedmar, M, Ström, M, Salvo-Romero, E, Vicario, M, et al. Vasoactive intestinal polypeptide and mast cells regulate increased passage of colonic Bacteria in patients with irritable bowel syndrome. Gastroenterology. (2017) 153:948–960.e3. doi: 10.1053/j.gastro.2017.06.051
35. Chen, M, Ruan, G, Chen, L, Ying, S, Li, G, Xu, F, et al. Neurotransmitter and intestinal interactions: focus on the microbiota-gut-brain Axis in irritable bowel syndrome. Front Endocrinol (Lausanne). (2022) 13:817100. doi: 10.3389/fendo.2022.817100
36. Fu, R, Chen, M, Chen, Y, Mao, G, and Liu, S. Expression and clinical significance of 5-HT and 5-HT3R in the intestinal mucosa of patient with diarrhea-type irritable bowel syndrome. Exp Ther Med. (2019) 17:3077–82. doi: 10.3892/etm.2019.7297
37. Dlugosz, A, Zakikhany, K, Acevedo, N, D'Amato, M, and Lindberg, G. Increased expression of toll-like receptors 4, 5, and 9 in small bowel mucosa from patients with irritable bowel syndrome. Biomed Res Int. (2017) 2017:9624702–7. doi: 10.1155/2017/9624702
38. Assas, BM, Miyan, JA, and Pennock, JL. Cross-talk between neural and immune receptors provides a potential mechanism of homeostatic regulation in the gut mucosa. Mucosal Immunol. (2014) 7:1283–9. doi: 10.1038/mi.2014.80
39. De Kivit, S, Tobin, MC, Forsyth, CB, Keshavarzian, A, and Landay, AL. Regulation of intestinal immune responses through TLR activation: implications for pro- and prebiotics. Front Immunol. (2014) 5:60. doi: 10.3389/fimmu.2014.00060
40. Baj, A, Moro, E, Bistoletti, M, Orlandi, V, Crema, F, and Giaroni, C. Glutamatergic signaling along the microbiota-gut-brain Axis. Int J Mol Sci. (2019) 20:1482. doi: 10.3390/ijms20061482
41. Strandwitz, P. Neurotransmitter modulation by the gut microbiota. Brain Res. (2018) 1693:128–33. doi: 10.1016/j.brainres.2018.03.015
42. Leeming, ER, Johnson, AJ, Spector, TD, and Le Roy, CI. Effect of diet on the gut microbiota: rethinking intervention duration. Nutrients. (2019) 11:2862. doi: 10.3390/nu11122862
43. van Oudenhove, L, Crowell, MD, Drossman, DA, Halpert, AD, Keefer, L, Lackner, JM, et al. Biopsychosocial aspects of functional gastrointestinal disorders. Gastroenterology. (2016). S0016-5085(16)00218-3. doi: 10.1053/j.gastro.2016.02.027
44. NICE. Overview|Irritable Bowel Syndrome in Adults: Diagnosis and Management|Guidance|NICE. Available at: https://www.nice.org.uk/guidance/cg61 (Accessed September 8, 2023).
45. McKenzie, YA, Bowyer, RK, Leach, H, Gulia, P, Horobin, J, O'Sullivan, NA, et al. British dietetic association systematic review and evidence-based practice guidelines for the dietary management of irritable bowel syndrome in adults (2016 update). J Hum Nutr Diet. (2016) 29:549–75. doi: 10.1111/jhn.12385
46. Paduano, D, Cingolani, A, Tanda, E, and Usai, P. Effect of three diets (low-FODMAP, gluten-free and balanced) on irritable bowel syndrome symptoms and health-related quality of life. Nutrients. (2019) 11:1566. doi: 10.3390/nu11071566
47. Singh, P, Tuck, C, Gibson, PR, and Chey, WD. The role of food in the treatment of bowel disorders: focus on irritable bowel syndrome and functional constipation. Am J Gastroenterol. (2022) 117:947–57. doi: 10.14309/ajg.0000000000001767
48. Hustoft, TN, Hausken, T, Ystad, SO, Valeur, J, Brokstad, K, Hatlebakk, JG, et al. Effects of varying dietary content of fermentable short-chain carbohydrates on symptoms, fecal microenvironment, and cytokine profiles in patients with irritable bowel syndrome. Neurogastroenterol Motil. (2017) 29:e12969. doi: 10.1111/nmo.12969
49. van Lanen, AS, de Bree, A, and Greyling, A. Efficacy of a low-FODMAP diet in adult irritable bowel syndrome: a systematic review and meta-analysis. Eur J Nutr. (2021) 60:3505–22. doi: 10.1007/s00394-020-02473-0
50. Suez, J, Zmora, N, Segal, E, and Elinav, E. The pros, cons, and many unknowns of probiotics. Nat Med. (2019) 25:716–29. doi: 10.1038/s41591-019-0439-x
51. Sanders, ME, Merenstein, DJ, Reid, G, Gibson, GR, and Rastall, RA. Probiotics and prebiotics in intestinal health and disease: from biology to the clinic. Nat Rev Gastroenterol Hepatol. (2019) 16:605–16. doi: 10.1038/s41575-019-0173-3
52. Simon, E, Călinoiu, LF, Mitrea, L, and Vodnar, DC. Probiotics, prebiotics, and Synbiotics: implications and beneficial effects against irritable bowel syndrome. Nutrients. (2021) 13:2112. doi: 10.3390/nu13062112
53. Vinderola, G, Sanders, ME, and Salminen, S. The concept of Postbiotics. Food Secur. (2022) 11:1077. doi: 10.3390/foods11081077
54. Ishaque, SM, Khosruzzaman, SM, Ahmed, DS, and Sah, MP. A randomized placebo-controlled clinical trial of a multi-strain probiotic formulation (bio-Kult®) in the management of diarrhea-predominant irritable bowel syndrome. BMC Gastroenterol. (2018) 18:71. doi: 10.1186/s12876-018-0788-9
55. Shang, X, E, FF, Guo, KL, Li, YF, Zhao, HL, Wang, Y, et al. Effectiveness and safety of probiotics for patients with constipation-predominant irritable bowel syndrome: a systematic review and Meta-analysis of 10 randomized controlled trials. Nutrients. (2022) 14:2482. doi: 10.3390/nu14122482
56. Wilson, B, Rossi, M, Dimidi, E, and Whelan, K. Prebiotics in irritable bowel syndrome and other functional bowel disorders in adults: a systematic review and meta-analysis of randomized controlled trials. Am J Clin Nutr. (2019) 109:1098–111. doi: 10.1093/ajcn/nqy376
57. Lacy, BE, Pimentel, M, Brenner, DM, Chey, WD, Keefer, LA, Long, MD, et al. ACG clinical guideline: Management of Irritable Bowel Syndrome. Am J Gastroenterol. (2021) 116:17–44. doi: 10.14309/ajg.0000000000001036
58. Pimentel, M, Chang, C, Chua, KS, Mirocha, J, DiBaise, J, Rao, S, et al. Antibiotic treatment of constipation-predominant irritable bowel syndrome. Dig Dis Sci. (2014) 59:1278–85. doi: 10.1007/s10620-014-3157-8
59. Fodor, AA, Pimentel, M, Chey, WD, Lembo, A, Golden, PL, Israel, RJ, et al. Rifaximin is associated with modest, transient decreases in multiple taxa in the gut microbiota of patients with diarrhoea-predominant irritable bowel syndrome. Gut Microbes. (2019) 10:22–33. doi: 10.1080/19490976.2018.1460013
60. FDA. Enforcement Policy Regarding Investigational New Drug Requirements for Use of Fecal Microbiota for Transplantation to Treat Clostridioides Difficile Infection Not Responsive to Standard Therapies. Rockville, MD: FDA, Guidance for Industry (2022).
61. Wang, M, Xie, X, Zhao, S, Ma, X, Wang, Z, and Zhang, Y. Fecal microbiota transplantation for irritable bowel syndrome: a systematic review and meta-analysis of randomized controlled trials. Front Immunol. (2023) 14:1136343. doi: 10.3389/fimmu.2023.1136343
62. Xu, D, Chen, VL, Steiner, CA, Berinstein, JA, Eswaran, S, Waljee, AK, et al. Efficacy of fecal microbiota transplantation in irritable bowel syndrome: a systematic review and Meta-analysis. Am J Gastroenterol. (2019) 114:1043–50. doi: 10.14309/ajg.0000000000000198
Keywords: irritable bowel syndrome, gut microbiota, gut-brain axis, fecal microbiota transplantation, brain-gut-microbiome
Citation: Cheng X, Ren C, Mei X, Jiang Y and Zhou Y (2024) Gut microbiota and irritable bowel syndrome: status and prospect. Front. Med. 11:1429133. doi: 10.3389/fmed.2024.1429133
Edited by:
Abbas Yadegar, Shahid Beheshti University of Medical Sciences, IranReviewed by:
Valentina Caputi, University College Cork, IrelandPanida Sittipo, Burapha University, Thailand
Copyright © 2024 Cheng, Ren, Mei, Jiang and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yafeng Zhou, emhvdXlhZmVuZzczQDEyNi5jb20=
†These authors have contributed equally to this work
 Xinyu Cheng
Xinyu Cheng Cheng Ren2†
Cheng Ren2† Yufeng Jiang
Yufeng Jiang Yafeng Zhou
Yafeng Zhou