
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Med. , 11 June 2024
Sec. Family Medicine and Primary Care
Volume 11 - 2024 | https://doi.org/10.3389/fmed.2024.1401577
 Mojca Hriberšek1,2
Mojca Hriberšek1,2 Fabian Eibensteiner1,3
Fabian Eibensteiner1,3 Nils Bukowski1,4
Nils Bukowski1,4 Andy Wai Kan Yeung1,5
Andy Wai Kan Yeung1,5 Atanas G. Atanasov1,6
Atanas G. Atanasov1,6 Eva Schaden1,4*
Eva Schaden1,4*Introduction: Family-centered care (FCC) is a model of care provision that sees a patient’s loved ones as essential partners to the health care team and positively influences the psychological safety of patients and loved ones.
Objectives: This review aims to present an overview of impactful publications, authors, institutions, journals, countries, fields of application and trends of FCC in the 21st century as well as suggestions on further research.
Methods: The Web of Science Database was searched for publications on FCC between January 2000 and Dezember 2023. After screening for duplicates, VOS Viewer and CiteSpace were used to analyze and visualize the data.
Results: Scientific interest in FCC has grown and resulted in the scientific output of 4,836 publications originating from 103 different countries. Based on the frequent author keywords, FCC was of greatest interest in neonatology and pediatrics, nursing, critical and intensive care, end-of-life and palliative care, and patient-related outcomes. The recent research hotspots are “patient engagement,” “qualitative study,” and “health literacy.”
Conclusion: FCC has gained recognition and spread from the pediatric to the adult palliative, intensive, end-of-life and geriatric care settings. This is a very reassuring development since adults, especially when older, want and need the assistance of their social support systems. Recent research directions include the involvement of patients in the development of FCC strategies, health literacy interventions and the uptake of telemedicine solutions.
Two major systems support patients on their healthcare journey: the healthcare system and their social circle (family, friends, caregivers, or other loved ones). Family-centered care (FCC) defines a patient’s loved ones as a source of strength and support, and sees them as inseparable unit and/or equal partners to patients and healthcare professionals (HCPs) in the treatment and management of disease (1, 2). They aim at building a partnership between HCPs and the patients and their social circle and together with shared decision making (SDM), FCC interventions are increasingly being recognized and implemented to improve the quality of healthcare (3, 4). While there is no official definition of FCC, a scoping review from 2019 identified the following key components: (1) collaboration between family members and healthcare providers, (2) consideration of family contexts, (3) education for patients, families, and HCPs, and (4) dedicated policies and procedures (5). Furthermore, the COVID-19 pandemic and associated hospital visitation restrictions have served as a reminder of the importance of the presence of loved ones in the patient’s healthcare journey (6, 7).
Overall, FCC promotes a respectful partnership between the provider and receiver of care (patient and their closest social support circle), supports a culture of patient safety as well as psychological safety (1, 8) and furthermore helps build health-care and management competences that result in community empowerment. The ability to speak up regarding your thoughts and concerns without interpersonal risk is essential in an environment such as healthcare. Independent of care setting, family members actively engaged in the care of their loved ones can serve as additional eyes and ears, helping to identify potential safety concerns or issues and ensuring timely interventions (9). Moreover, healthcare providers can gain valuable insights and perspectives that can contribute to safer and more effective care (3). Thereby, healthcare systems that embrace family- and patient-centeredness and mutual acknowledgement support patient participation in safety practices and increase psychological as well as patient safety (10).
Hence, to analyze the whole literature of FCC regarding their origin, content and impact, the bibliometric review was chosen as the appropriate method. To date, only systematic and scoping reviews summarizing the growing body of evidence on FCC have been published and while these review methods focus on a specific research question and implementations and their results, they do not provide a comprehensive overview of the existing literature.
The purpose of this paper is, firstly, to highlight impactful publications, authors, journals, institutions, and countries on FCC, secondly, to provide an overview of the medical fields in which FCC is applied, thirdly, to provide insight into past and current trends within FCC and, finally, to offer suggestions for further research.
Bibliometric review is a method used to depict and analyze cumulative scientific knowledge in an area of interest. It can be used to (1) gain an overview and uncover new research trends, co-working patterns among single authors, organizations or countries, and define impactful research works, (2) identify knowledge gaps, (3) derive novel ideas for investigation, and (4) position new research to contribute to the field (11). Bibliometric analyses have already been used to give a literature overview of 21st century developments in topics such as SDM (12) and palliative care research (13). The review was conducted according to the Prisma-ScR extension framework, which is the closest to the methodology of a bibliometric review, as no framework for bibliometric reviews exists.
Data for this bibliometric review was extracted from Web of Science on October 10, 2023, at the Medical University of Vienna, Vienna, Austria. To identify FCC developments in the 21st century, the time span was set from January 1, 2000, to December 31, 2022. Due to the different spellings in British and American English (family-centered/family-centered), the following search query was used “TS = (“family-centered*” or “family-centered*”) and TS = (“care”).” Titles, abstracts, and keywords (both author keywords and KeyWords Plus (14) were scanned, ensuring that not only publications explicitly mentioning FCC but also those on topic of FCC were taken into account.
As this was a comprehensive analysis of the literature in question, all resulting papers were included without exception (Multimedia Appendix 1).
The identified papers were scanned for duplicates and since none were found, all identified papers were submitted to analysis.
Since the bibliometric review aims to analyze the whole body of literature on FCC in the 21st century, the focus of this analysis is on the topics, types and contributors of the research and not on the quality of the work.
The identified papers were exported in full record with cited references from Web of Science. The following data were used for analysis: author, institution, country, year of publication, publishing journal, citation count and author keywords.
Data analysis and visualizations were conducted using R software (15) and VOS Viewer (Version 1.6.18) (16). Continuous data was summarized using mean and standard deviation; categorical data was summarized using absolute and relative frequencies. VOS viewer was also used to visualize network maps of the co-authorship connections of organizations and authors, and co-occurrence of author keywords. The maps were generated by constructing a similarity matrix based on association strength, followed by optimization using the majorization algorithm, and finally transformations to ensure consistent solutions (16). The distance-based networks generated visualize items with circles; frequency of occurrence is indicated by node size; strength of relation between items by the length of the edge. When analyzing data, full counting was applied, i.e., all co-authorships and co-occurrences were weighted equally. For authors keywords, a thesaurus file was created to merge the spelling of FCC to “Family-centered care.” Furthermore, thresholds (T) were applied and adapted to select for top contributors. Finally, the VOS Viewer unique variant of modularity-based clustering with a resolution parameter (17) was used to cluster these contributors. Citation bursts – frequency surges of author keywords used in the cited publications – can be used as indicators for research hotspots. They were analyzed using CiteSpace (Version 6.1.R4) (18, 19) under the following parameters: time span (2000–2022), years per slice (1), links (strength: cosine, scope: within slices), term source (Author Keywords), selection criteria (TopN% = 5; max. Items per slice 100). Since.
A total of 4,986 FCC-related publications were published and included in the Web of Science core collection between 2000 and 2022. In 2000, only 29 articles were published, while in 2022, this figure had risen to 580 (Figure 1A). Overall, there is a steady increase in the number of published articles over the progress of the 21st century.
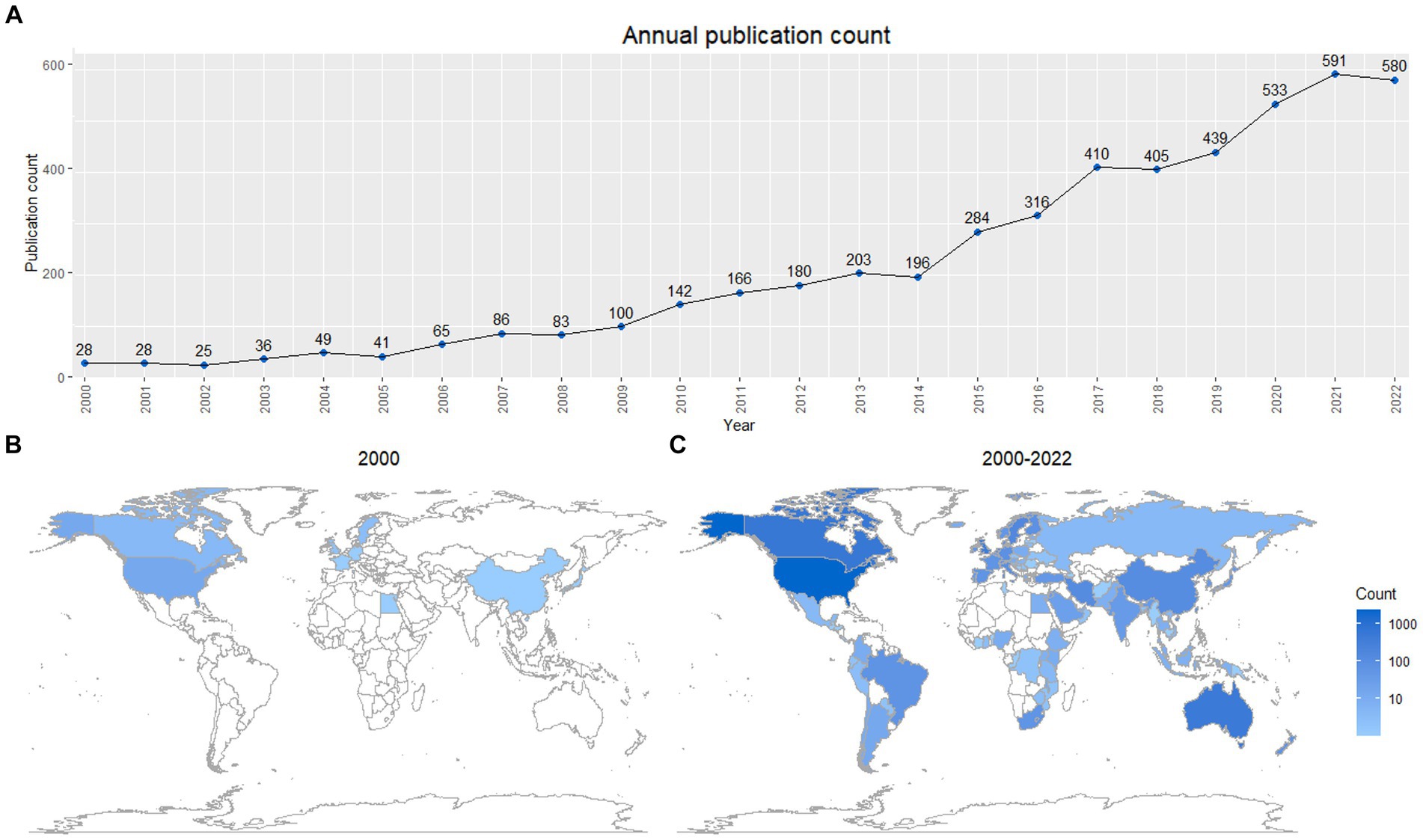
Figure 1. FCC publication rates during the 21st century. (A) Annual output of FCC publications in the 21st century. (B) Countries publishing on FCC in the year 2000 (9 countries). (C) Countries publishing on FCC in the years 2000 to 2022 (103 countries). Scale is logarithmic.
Alongside the increase in publication volume, the number of publishing countries also increased. In 2000, 9 countries published FCC-related articles (Figure 1B), while between 2000 to 2022, this figure grew to 103 countries (Figure 1C). The majority of articles were published in the United States (2,438/4663; 52.3%), followed by three other major English-speaking countries: Canada (626/4663; 13.4%), Australia (504/4663; 10.8%) and the United Kingdom (338/4663; 7.2%), amounting to 83.8% (Table 1). Among the top 10 contributing countries, each country contributed a mean of 466.3 ± 680.47 publications. Articles from these countries were cited with an average citations per publication ratio (CPP) of 17.46 ± 5.172.
The top 10 publishing organizations contributed a mean of 97.0 ± 24.36 articles related to FCC (Table 1). At 159, the University of Toronto published the most articles, while the highest citation per publication ratio was achieved by University of California – San Francisco with 65.65. The network of top 2% (101/4945) of organizations by publishing volume (at least 21 articles) shows 4 clusters that very largely coincide with the organizations’ host countries (Supplementary Figure S1): The largest cluster contains organizations from the United States; the second largest from Canada; the third largest from Australia, New Zealand and Europe; and the smallest from Iran and United States. Based on this cluster analysis of co-authorship, stronger associations are observable between organizations in the United States and Canada, while Australian and New Zealand organizations are more associated with European organizations.
Most papers were published in the journal Pediatrics, with a total count of 138 papers (Table 2). The top 10 journals together published 818 articles, accounting for 16.4% of the total 4,986 articles. Among the top publishing journals, Pediatrics leads with an IF of 8.0 and CPP of 89.71, while Advances in Neonatal Care has the lowest IF of 1.7 and CPP of 11.45. The average IF of the journals is 4.1 ± 2.42. According to the Science Citation Index Expanded (SCIE) of WoS, the journals fall into the categories nursing, pediatrics, critical care medicine, and obstetrics and gynecology.
The 10 most frequently published authors are listed in Table 1. The highest publication count of 33 publications was recorded by Latour Jos M., while the highest CPP ratio of 57.55 was achieved by Curtis J. Randall. There were very few co-authorships among the top 10 publishing authors (Supplementary Figure S2). However, when considering the authors publishing at least 5 papers on FCC, all the top 10 authors except one are connected through co-authorships with other authors within a single network (Supplementary Figure S2).
Of the 4,986 FCC-related publications in the 21st century, the most common publication types are articles (3,878; 77.8%), reviews (513; 10.3%), meeting abstracts (232; 4.7%) and editorial material (207; 4.2%) (Supplementary Table S3). The 10 most cited articles on FCC were cited on average 673.9 ± 184.54 times (Table 3). Most of them (6/10) are or comprise of guidelines or recommendations (2, 20–24) on how to best implement FCC. The others are focused on the perspectives, experience, and well-being of patients and loved ones (family, caregivers), also from the perspective of racially or ethnically diverse groups (25–28). The most cited article, with 1,082 citations, is entitled Family Perspectives on End-of-Life Care at the Last Place of Care by Teno et al. (25), published in 2004. The 10 articles with the highest yearly citation rate were cited with an average of 62.7 ± 19.99 citations/year. Among them were 4 of the 10 most cited papers: guidelines for the application of FCC on the Neonatal, Pediatric, and Adult ICU, the role of the pediatrician in FCC and family perspectives at end of life care (2, 22, 24, 25). The article with the highest yearly citation ratio of 119.2 is titled Guidelines for Family-Centered Care in the Neonatal, Pediatric, and Adult ICU by Davidson JE et al. (22). Among the articles with the highest yearly citation were also 3 related to COVID-19: managing the ICU surge (29), FCC applications in normal care (30) and telehealth opportunities (31).
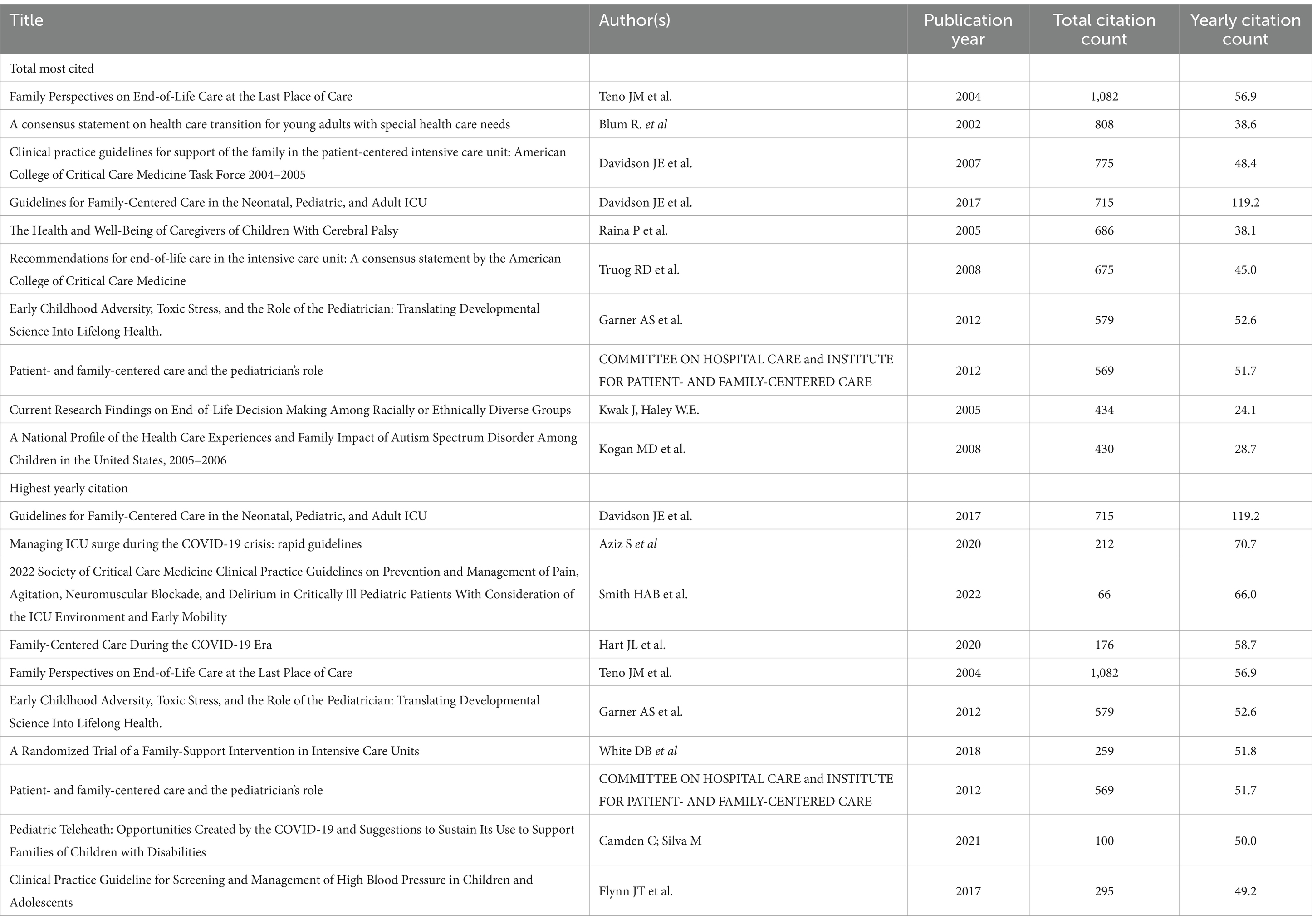
Table 3. Top 10 most cited articles on total and yearly citation counts in the field of family-centered care.
Publications published in 2000 yielded 87 different author keywords, related to neonatology and intensive care, pediatrics and children with special care needs, parents and families (Supplementary Figure S4). The 4,986 FCC-related publications appearing between 2000 and 2022 yielded 7,272 unique author keywords, of which the top 140 (2%) are clustered and depicted in Figure 2. They form 5 different clusters: “pediatric and adolescent care,” “neonatology and pediatric intensive care,” “end-of-life care,” “adult intensive care and nursing,” “inclusion in care,” and “patient-related outcomes,” the main themes of FCC. In terms of publication year, among the earliest are “children with special care needs,” “medical home,” “chronic illness,” “neonatal nursing,” and “developmental care,” while the most recent are “Covid-19,” “telemedicine,” “telehealth” “patient,” and “patient engagement” (Supplementary Figure S5).
For author keywords, the top 25 experiencing citation bursts are shown in Figure 3. The earliest and longest lasting bursts were at the beginning of the 21st century and are “neonatal nursing,” “medical home,” “decision making,” and “family-centered service,” with an average duration of 12.5 ± 2.18 years. The newest bursts lasting into 2022 are “patient engagement,” “qualitative study” and “health literacy,” lasting on average 3.3 ± 0.47 years.
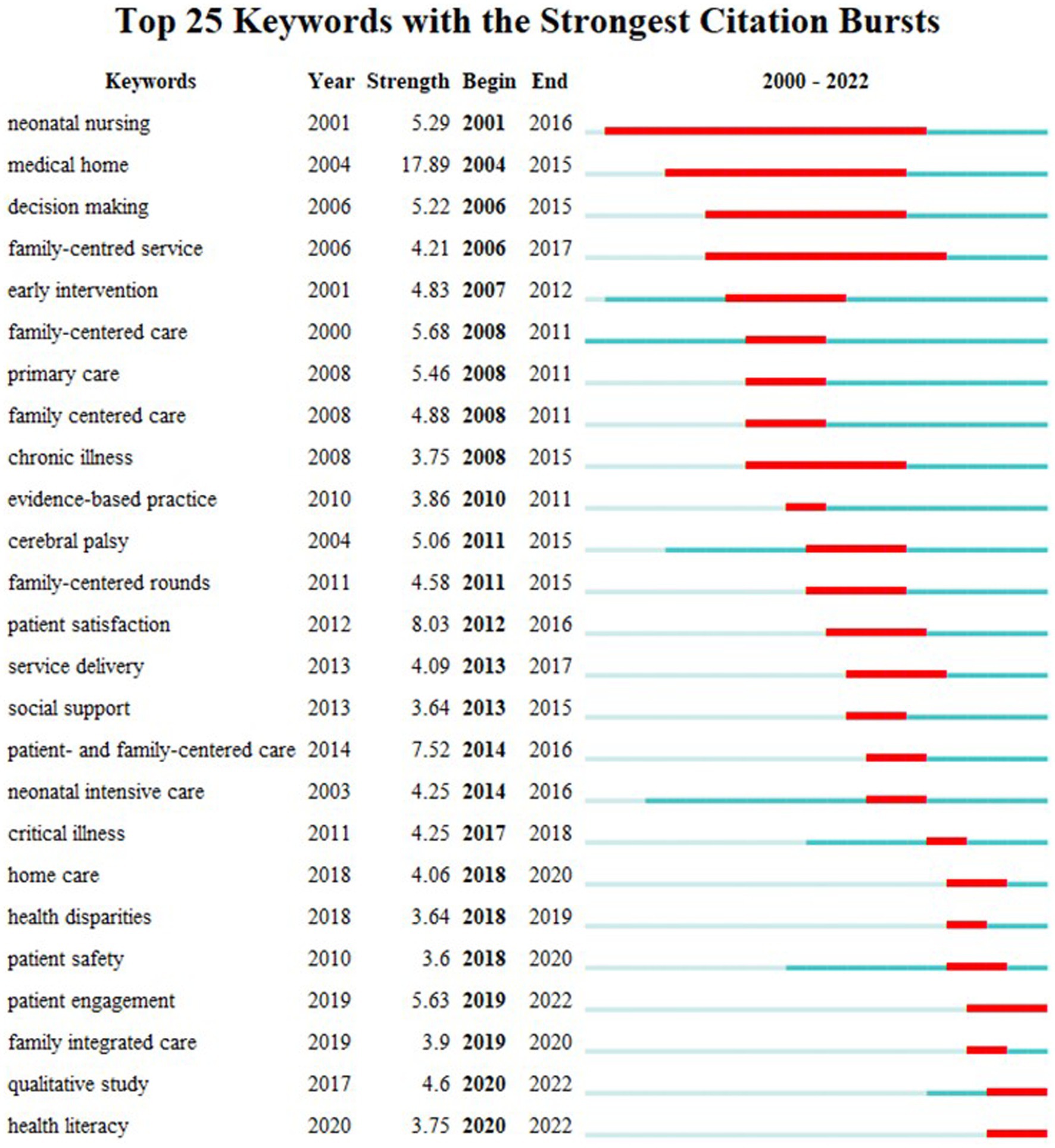
Figure 3. Top 25 author keywords experiencing citation bursts within the 21st century in FCC publications. Blue represents the occurrence of the keyword while red represents the burst.
This bibliometric review shows a significant increase in publications on FCC in the 21st century, spreading from the pediatric to the adult care setting, from a few to more than 100 countries worldwide, and with an increasing focus on patient experience and patient-reported outcomes. The largest areas of interest and application are nursing, neonatology and pediatrics, critical and intensive care, end-of-life (palliative) care and patient-related outcomes. The newest research areas are “health literacy,” “family involvement,” “family-integrated care” and “older adults.”
In the first decade of the 21st century, FCC was still primarily associated with pediatric care (32). FCC experienced the strongest growth in publications since 2015, when “patient and family-centered care” (PFCC) experienced a burst in citations (Figure 2). This term was coined in the 1990s to give focus to engaging and viewing the patient and family/caregivers as an inseparable unit and essential members of the healthcare team and supporting them to increasing the patient’s health and quality of healthcare (3, 33). Although originating in pediatrics, this bibliometric review relates PFCC to many different applications across all healthcare settings.
There has been a recent paradigm shift in clinical research, especially with respect to clinical trials, with more active patient involvement and increased utilization of qualitative research methods focusing on patient-reported outcome measures (PROMs) and patient-reported experience measures (PREMs) (34–36). This can also be observed in our bibliometric review, as indicated by prominent clustering (Figure 2) for terms such as “patient satisfaction,” “patient-centered care,” “qualitative research,” “qualitative study,” and “patient experience.”
FCC has developed from its activist origins in the pediatric sector in the United States and United Kingdom during the post-WWII era, when the experience of mass separations of children from their parents and children’s subsequent trauma were still very recent (32, 37). Furthermore, in some ways the term FCC reflects a response to western medical practice with its historically paternalistic system, in contrast to other cultures (often Asian and Hispanic) in which family involvement has always been the norm (28, 37). Overall, in terms of the number of published articles, top publishing authors and institutions, the leading proponents of FCC are the western English-speaking countries (United States, Canada, United Kingdom, and Australia). While there are international collaborations among researchers and organizations, most work on FCC is being conducted within tightly-knit working groups and national organizations (Figure 3) – a finding also described in a bibliometric review on palliative care research (13). While this allows for tailored approaches to the hospital and country settings, it may potentially result in institutional bias and a limited diversity of perspectives and potential exclusion of diverse viewpoints and experiences of different communities. Collaborations between institutions and countries are crucial for broad and inclusive application.
Currently, FCC seems to be most relevant at the beginning of life, centering around neonatology and pediatrics, and at the end of life, centering around intensive, palliative and end-of-life care. In both stages, patients are more dependent on others, both physically and mentally. This is coupled with tightly embedded social and emotional family structures, forming an indivisible unit of patients and their family/caregivers that must be respected and utilized, but not disrupted, by medical care. However, as a consequence of medical progress in treating many chronic illnesses (e.g., diabetes mellitus, chronic kidney disease), as well as increasing life expectancy and prolongation of palliative care, statistically people spend more years in poor health and dependent on others (38–40). The recent increasing use of FCC in geriatric care is further indicated by the author keywords “dementia,” “family caregivers” and “quality-of-life” for very recent publication dates (Supplementary Figure S5). Willingness to care is negatively impacted by caregiver burden (41) however positively affected by reciprocal altruism and offering FCC approaches could further incentivize and support family caregiving.
While sharing the principles of family or loved one integration, FCC has different characteristics when applied in different clinical settings.
The concept of family-centered care originates from pediatric primary care (Figure 2; Supplementary Figure S5), where FCC regards the patient, their parents and the family system as a single inseparable unit (2). However, the care differs according to the level of understanding and maturity of the patient, changing with the progression from infancy to adolescence and young adulthood, and with an increasing focus on the autonomy of the patient while still under parental guidance. One specific pediatric focus lies in children with severe chronic diseases, disabilities, and psychomotor retardation, as included in Figure 2 (disability, cerebral palsy, chronic illness). Here, the single inseparable unit of patient and family system and high level of received support does not significantly decrease as the child ages, reflecting the specific illness and degree of mental and physical maturity (42).
During the 21st century, FCC has also become closely associated with neonatal (intensive) care (Figure 2; Supplementary Figure S5). There, FCC not only ensure that infants are not separated from their parents, but also supports education of parents on relevant topics such as appropriate hygiene maintenance (43). COVID-19 related visitation restrictions showed the importance of FCC and the absence of mothers at the bedside lead to a cascade of disruptions to newborn care and breastfeeding practices (44). In recent years, the term family-integrated care has been gaining traction (Figure 3; Supplementary Figure S5). Family-integrated care focuses on the involvement family members in patient care to the extent that it allows families to perform care tasks that are normally performed by HCPs, to provide daily parent education programs (45), to enable parents to become primary caregivers in the neonatal intensive care unit (46) and to support lactation and breastfeeding (47).
In contrast, in the adult care setting the goal of FCC is to include a patient’s loved ones as equal partners in the provision of care, especially in the palliative and end-of-life setting (5).However usually adult healthcare is predominantly striving to be patient-centered with the aim to strengthen the patient-clinician relationship, promote communication about things that matter, help patients know more about their health, and facilitate their involvement in their own care (48). For patients who feel confident in managing their care independently, who have privacy concerns or strong personal values and beliefs profit from and may prioritize this approach. For example, a review of end-of-life decision making among racially or ethnically diverse groups shows not all ethnic groups are equally open to FCC (28). However health has a strong psychosocial aspect where social support, mental health, and emotional well-being have a high influence on a person’s well-being (49). Family-centered care recognizes the interconnectedness of family relationships and their impact on individual health outcomes and strives for the inclusion of the patients support system into the care plan. However patient privacy and autonomy are at the forefront of the needs to be guaranteed by the healthcare system. Therefore, FCC should be offered to the patient but introduced up to the level of the patients wishes. Then, effective communication between healthcare providers, patients, and their families is crucial to understanding and respecting the specific wishes and needs of each patient but also their family members.
It could be argued that FCC is less relevant during adulthood compared to the beginning and end of life, because, unless suffering from chronic illness involving countless diagnostic and therapeutic interventions with frequent follow-up visits and in-patient stays, for most adults medical visits or temporary medical conditions are infrequent occurrences. However, humans are social creatures and there is an extraordinary amount of interdependence in adults, not just dependency of children on adults. It is often independent of how serious the medical problems or preventive or clinical care that happens is that patients seek support and try to contextualize the problem within their socioecological system. In a recent study conducted by our group, we found a wish for adult health care to be generally more like pediatrics (6), in the sense of considering the patient as a whole including its social support circle.
As seen in Figure 2, FCC associates with SDM, which is relevant in pediatric and adult care settings (50), as well as in advance care planning, a process in which individuals make decisions about the health care they wish to receive when they are no longer able to make their own medical decisions (51) and which often includes family members in the process (40). Involving family members in adult medical care in general should be considered not only in cases where the patient has a legally appointed representative or surrogate decision maker, but also for routine medical care. Furthermore, by involving families in the care process, healthcare providers can gain valuable insights and perspectives that can contribute to safer and more effective care (3). However, in many cases, a collaborative approach that combines elements of both person-centered and family-centered care may be the most effective in meeting the diverse needs of patients.
FCC is closely related to patient safety, as shown in Figures 2, 3. Improved communication, coordination, and engagement of patients and their loved ones allows healthcare plans to be better communicated and risks better identified and mitigated (3) and patient participation is advocated as a means to improve patient safety (52). Furthermore, it increases psychological safety especially of patients and loved ones, which in turn supports patient satisfaction and improves the patient experience. In the United States, FCC has been officially recognized as an intervention that promotes safety and quality of care, and hospitals in the United States are actively encouraged to incorporate patient- and family-centered practices (2). Such initiatives should also be adopted in other countries.
As well as the constant need for social support and having loved ones present throughout the healthcare journey, interest in FCC might also be influenced by digitalization and our culture of information sharing, as well as generational changes in the behavior and value systems of patients and health care providers (53–55). Our modern information age is probably also a contributing factor in the growing interest in FCC. Furthermore, the Internet gives patients and their loved ones greater access to information, leading to increased health literacy, but also greater misinformation and misconceptions about diagnoses, diagnostics, and treatment options (56). Therefore, it is even more critical that medical information is communicated in a trustworthy and reliable manner, irrespective of whether by an institution or a single healthcare provider. Increasing health literacy is one of the main strategies for promoting PFCC (33), and the “health literacy” citation burst reflects this development (Figure 3).
With respect to the modern information age, two of the author keywords associated with FCC are “telemedicine” and “telehealth” (Figure 2). Although telemedicine solutions were already in existence prior to the pandemic (57–59), their expansion was facilitated by COVID-19 (60, 61). However, while telemedicine and telehealth have positive outcomes and enjoy acceptance among HCPs, patients, and their loved ones, the solutions have not yet been widely adopted.
To remain as current as possible, our literature search strategy included all complete years in the 21st century. However, as Web of Science is continuously and retrospectively updated, and as there can be delays in indexing by some journals, the bibliometric data for the last couple of years may be subject to minor changes. While more literature databases are available, the data for this study was only extracted from the Web of Science Core Collection, which is standard practice for most bibliometric analyses (62). This however has the drawback that it does not index all literature on a topic, but only selected articles and journals as described by Clarivate (63). In order to capture all published articles on FCC, we did not limit the article type. A limitation of the VOS Viewer is that all authors of a publication are included in the analysis. Therefore, according to the affiliations of its authors, a publication can be attributed to several countries and organizations. Lastly, while there are many different indices for measuring the impact of publications, we only used the total count and citations of author/organization/country/article impact, which are generally the most known and frequently used metrics.
Scientific interest in FCC is growing and during the first 22 years of the 21st century has spread from the pediatric to the adult intensive, palliative and end-of-life settings. It is closely connected with patient safety, experience and satisfaction. The recent research directions include involving patients in the development of FCC strategies, health literacy interventions, and the uptake of telemedicine solutions.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
MH: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Visualization, Writing – original draft, Writing – review & editing. FE: Conceptualization, Formal analysis, Validation, Visualization, Writing – review & editing. NB: Formal analysis, Writing – review & editing. AY: Methodology, Software, Writing – review & editing. AA: Writing – review & editing, Data curation. ES: Conceptualization, Supervision, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2024.1401577/full#supplementary-material
1. Kuo, DZ, Houtrow, AJ, Arango, P, Kuhlthau, KA, Simmons, JM, and Neff, JM. Family-centered care: current applications and future directions in pediatric health care. Matern Child Health J. (2012) 16:297–305. doi: 10.1007/s10995-011-0751-7
2. Committee on Hospital Care and Institute for Patient- and Family-Centered Care. Patient- and family-centered care and the pediatrician’s role. Pediatrics. (2012) 129:394–404. doi: 10.1542/peds.2011-3084
3. Park, M, Giap, TTT, Lee, M, Jeong, H, Jeong, M, and Go, Y. Patient- and family-centered care interventions for improving the quality of health care: a review of systematic reviews. Int J Nurs Stud. (2018) 87:69–83. doi: 10.1016/j.ijnurstu.2018.07.006
4. Pieterse, AH, Stiggelbout, AM, and Montori, VM. Shared decision making and the importance of time. JAMA. (2019) 322:25–6. doi: 10.1001/jama.2019.3785
5. Kokorelias, KM, Gignac, MAM, Naglie, G, and Cameron, JI. Towards a universal model of family centered care: a scoping review. BMC Health Serv Res. (2019) 19:564. doi: 10.1186/s12913-019-4394-5
6. Hriberšek, M, Eibensteiner, F, Kapral, L, Teufel, A, Nawaz, F, Cenanovic, M, et al. “Loved ones are not ‘visitors’ in a patient’s life”—the importance of including loved ones in the patient’s hospital stay: an international twitter study of #HospitalsTalkToLovedOnes in times of COVID-19. Front Public Health. (2023) 11:1100280. doi: 10.3389/fpubh.2023.1100280
7. Hugelius, K, Harada, N, and Marutani, M. Consequences of visiting restrictions during the COVID-19 pandemic: an integrative review. Int J Nurs Stud. (2021) 121:104000. doi: 10.1016/j.ijnurstu.2021.104000
8. Correia, TSP, Martins, MMFPS, Barroso, FF, Valentim, O, Fonseca, C, Lopes, M, et al. Safety and family-centered care during restriction of hospital visits due to COVID-19: the experience of family members. J Pers Med. (2022) 12:1546. doi: 10.3390/jpm12101546
9. Schyve, PM. Language differences as a barrier to quality and safety in health care: the joint commission perspective. J Gen Intern Med. (2007) 22:360–1. doi: 10.1007/s11606-007-0365-3
10. Vaismoradi, M, Jordan, S, and Kangasniemi, M. Patient participation in patient safety and nursing input – a systematic review. J Clin Nurs. (2015) 24:627–39. doi: 10.1111/jocn.12664
11. Donthu, N, Kumar, S, Mukherjee, D, Pandey, N, and Lim, WM. How to conduct a bibliometric analysis: an overview and guidelines. J Bus Res. (2021) 133:285–96. doi: 10.1016/j.jbusres.2021.04.070
12. Lu, C, Li, X, and Yang, K. Trends in shared decision-making studies from 2009 to 2018: a bibliometric analysis. Front Public Health. (2019) 7:384. doi: 10.3389/fpubh.2019.00384
13. Abu-Odah, H, Molassiotis, A, and Liu, JYW. Global palliative care research (2002-2020): bibliometric review and mapping analysis. BMJ Support Palliat Care. (2022) 12:376–87. doi: 10.1136/bmjspcare-2021-002982
14. Garfield, E, and Sher, IH. KeyWords PlusTM algorithmic derivative indexing. J Am Soc Inf Sci. (1993) 44:298–9. doi: 10.1002/(SICI)1097-4571(199306)44:5<298::AID-ASI5>3.0.CO;2-A
15. R: The R Project for Statistical Computing. (2022). Available at: https://www.r-project.org/.
16. Van Eck, NJ, and Waltman, L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics. (2010) 84:523–38. doi: 10.1007/s11192-009-0146-3
17. Waltman, L, van Eck, NJ, and Noyons, ECM. A unified approach to mapping and clustering of bibliometric networks. J Informetr. (2010) 4:629–35. doi: 10.1016/j.joi.2010.07.002
18. Chen, C. Searching for intellectual turning points: progressive knowledge domain visualization. Proc Natl Acad Sci USA. (2004) 101:5303–10. doi: 10.1073/pnas.0307513100
19. Chen, C. CiteSpace II: detecting and visualizing emerging trends and transient patterns in scientific literature. J Am Soc Inf Sci Technol. (2006) 57:359–77. doi: 10.1002/asi.20317
20. Davidson, JE, Powers, K, Hedayat, KM, Tieszen, M, Kon, AA, Shepard, E, et al. Clinical practice guidelines for support of the family in the patient-centered intensive care unit: American College of Critical Care Medicine Task Force 2004–2005. Crit Care Med. (2007) 35:605–22. doi: 10.1097/01.CCM.0000254067.14607.EB
21. Truog, RD, Campbell, ML, Curtis, JR, Haas, CE, Luce, JM, Rubenfeld, GD, et al. Recommendations for end-of-life care in the intensive care unit: a consensus statement by the American College of Critical Care Medicine. Crit Care Med. (2008) 36:953–63. doi: 10.1097/CCM.0B013E3181659096
22. Davidson, JE, Aslakson, RA, Long, AC, Puntillo, KA, Kross, EK, Hart, J, et al. Guidelines for family-centered Care in the Neonatal, pediatric, and adult ICU. Crit Care Med. (2017) 45:103–28. doi: 10.1097/CCM.0000000000002169
23. Blum, R, Hirsch, D, Kastner, TA, Quint, RD, Sandler, AD, Anderson, SM, et al. A consensus statement on health care transition for young adults with special health care needs. Pediatrics. (2002) 110:1304–6.
24. Garner, AS, Shonkoff, JP, Siegel, BS, Dobbins, MI, Earls, MF, et al. Early childhood adversity, toxic stress, and the role of the pediatrician: translating developmental science into lifelong health. Pediatrics. (2012) 129:e224–31. doi: 10.1542/peds.2011-2662
25. Teno, JM, Clarridge, BR, Casey, V, Welch, LC, Wetle, T, Shield, R, et al. Family perspectives on end-of-life Care at the Last Place of care. JAMA. (2004) 291:88–93. doi: 10.1001/jama.291.1.88
26. Raina, P, O’Donnell, M, Rosenbaum, P, Brehaut, J, Walter, SD, Russell, D, et al. The health and well-being of caregivers of children with cerebral palsy. Pediatrics. (2005) 115:e626–36. doi: 10.1542/peds.2004-1689
27. Kogan, MD, Strickland, BB, Blumberg, SJ, Singh, GK, Perrin, JM, and van Dyck, PC. A National Profile of the health care experiences and family impact of autism Spectrum disorder among children in the United States, 2005–2006. Pediatrics. (2008) 122:e1149–58. doi: 10.1542/peds.2008-1057
28. Kwak, J, and Haley, WE. Current research findings on end-of-life decision making among racially or ethnically diverse groups. The Gerontologist. (2005) 45:634–41. doi: 10.1093/geront/45.5.634
29. Aziz, S, Arabi, YM, Alhazzani, W, Evans, L, Citerio, G, Fischkoff, K, et al. Managing ICU surge during the COVID-19 crisis: rapid guidelines. Intensive Care Med. (2020) 46:1303–25. doi: 10.1007/s00134-020-06092-5
30. Hart, JL, Turnbull, AE, Oppenheim, IM, and Courtright, KR. Family-centered care during the COVID-19 era. J Pain Symptom Manag. (2020) 60:e93–7. doi: 10.1016/j.jpainsymman.2020.04.017
31. Camden, C, and Silva, M. Pediatric Teleheath: opportunities created by the COVID-19 and suggestions to sustain its use to support families of children with disabilities. Phys Occup Ther Pediatr. (2021) 41:1–17. doi: 10.1080/01942638.2020.1825032
32. Jolley, J, and Shields, L. The evolution of family-centered care. J Pediatr Nurs. (2009) 24:164–70. doi: 10.1016/j.pedn.2008.03.010
33. Clay, AM, and Parsh, B. Patient- and family-centered care: It’s not just for pediatrics anymore. AMA J Ethics. (2016) 18:40–4. doi: 10.1001/journalofethics.2016.18.1.medu3-1601
34. Hawkins, M, Elsworth, GR, and Osborne, RH. Application of validity theory and methodology to patient-reported outcome measures (PROMs): building an argument for validity. Qual Life Res. (2018) 27:1695–710. doi: 10.1007/s11136-018-1815-6
35. Lai, CH, Shapiro, LM, Amanatullah, DF, Chou, LB, Gardner, MJ, Hu, SS, et al. A framework to make PROMs relevant to patients: qualitative study of communication preferences of PROMs. Qual Life Res. (2022) 31:1093–103. doi: 10.1007/s11136-021-02972-5
36. Carfora, L, Foley, CM, Hagi-Diakou, P, Lesty, PJ, Sandstrom, ML, Ramsey, I, et al. Patients’ experiences and perspectives of patient-reported outcome measures in clinical care: a systematic review and qualitative meta-synthesis. PLoS One. (2022) 17:e0267030. doi: 10.1371/journal.pone.0267030
37. Igel, LH, and Lerner, BH. Moving past individual and “pure” autonomy: the rise of family-centered patient care. AMA J Ethics. (2016) 18:56–62. doi: 10.1001/journalofethics.2016.18.1.msoc1-1601
38. GBD 2019 Ageing Collaborators. A Global, regional, and national burden of diseases and injuries for adults 70 years and older: systematic analysis for the global burden of disease 2019 study. BMJ. (2022) 376:e068208. doi: 10.1136/bmj-2021-068208
39. Vos, T, Lim, SS, Abbafati, C, Abbas, KM, Abbasi, M, Abbasifard, M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. (2020) 396:1204–22. doi: 10.1016/S0140-6736(20)30925-9
40. Lum, HD, Sudore, RL, and Bekelman, DB. Advance care planning in the elderly. Med Clin North Am. (2015) 99:391–403. doi: 10.1016/j.mcna.2014.11.010
41. Li, J, Xie, CH, and Han, SY. Family caregiver’s willingness to care from the perspective of altruism. Front Public Health. (2023) 2023:1237241. doi: 10.3389/fpubh.2023.1237241
42. State of Queensland (Queensland Health). Child and Family Centred Care: Evidence-based principles for the statewide delivery of health services to critically unwell children. (2021). Available at: https://www.childrens.health.qld.gov.au/wp-content/uploads/PDF/qcycn/child-and-family-centred-care-principles-paper.pdf (Accessed Sep 12, 2023).
43. Maria, A, Litch, JA, Stepanchak, M, Sarin, E, Wadhwa, R, and Kumar, H. Assessment of feasibility and acceptability of family-centered care implemented at a neonatal intensive care unit in India. BMC Pediatr. (2021) 21:171.
44. Maria, A, Mukherjee, R, Upadhyay, S, Pratima, K, Bandyopadhyay, T, Gupta, R, et al. Barriers and enablers of breastfeeding in mother–newborn dyads in institutional settings during the COVID-19 pandemic: a qualitative study across seven government hospitals of Delhi, India. Front Nutr. (2022) 9:1052340. doi: 10.3389/fnut.2022.1052340
45. Bracht, M, O’Leary, L, Lee, SK, and O’Brien, K. Implementing family-integrated care in the NICU: a parent education and support program. Adv Neonatal Care. (2013) 13:115–26. doi: 10.1097/ANC.0b013e318285fb5b
46. O’Brien, K, Robson, K, Bracht, M, Cruz, M, Lui, K, Alvaro, R, et al. Effectiveness of family integrated care in neonatal intensive care units on infant and parent outcomes: a multicentre, multinational, cluster-randomised controlled trial. Lancet Child Adolesc Health. (2018) 2:245–54. doi: 10.1016/S2352-4642(18)30039-7
47. Parker, MG, Stellwagen, LM, Noble, L, Kim, JH, Poindexter, BB, Puopolo, KM, et al. Promoting human Milk and breastfeeding for the very low birth weight infant. Pediatrics. (2021) 148:e2021054272. doi: 10.1542/peds.2021-054272
48. Epstein, RM, and Street, RL. The values and value of patient-centered care. Ann Fam Med. (2011) 9:100–3. doi: 10.1370/afm.1239
49. Thoits, PA. Mechanisms linking social ties and support to physical and mental health. J Health Soc Behav. (2011) 52:145–61. doi: 10.1177/0022146510395592
50. Elwyn, G, Frosch, D, Thomson, R, Joseph-Williams, N, Lloyd, A, Kinnersley, P, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. (2012) 27:1361–7. doi: 10.1007/s11606-012-2077-6
51. Michael, N, O’Callaghan, C, Baird, A, Hiscock, N, and Clayton, J. Cancer caregivers advocate a patient- and family-centered approach to advance care planning. J Pain Symptom Manag. (2014) 47:1064–77. doi: 10.1016/j.jpainsymman.2013.07.009
52. Longtin, Y, Sax, H, Leape, LL, Sheridan, SE, Donaldson, L, and Pittet, D. Patient participation: current knowledge and applicability to patient safety. Mayo Clin Proc. (2010) 85:53–62. doi: 10.4065/mcp.2009.0248
53. Twenge, JM, Campbell, WK, and Freeman, EC. Generational differences in young adults’ life goals, concern for others, and civic orientation, 1966–2009. J Pers Soc Psychol. (2012) 102:1045–62. doi: 10.1037/a0027408
54. Lyons, ST, Duxbury, L, and Higgins, C. An empirical assessment of generational differences in basic human values. Psychol Rep. (2007) 101:339–52. doi: 10.2466/pr0.101.2.339-352
55. Leijen, I, Van Herk, H, and Bardi, A. Individual and generational value change in an adult population, a 12-year longitudinal panel study. Sci Rep. (2022) 12:17844. doi: 10.1038/s41598-022-22862-1
56. Swire-Thompson, B, and Lazer, D. Public health and online misinformation: challenges and recommendations. Annu Rev Public Health. (2020) 41:433–51. doi: 10.1146/annurev-publhealth-040119-094127
57. Hooshmand, M, and Yao, K. Challenges facing children with special healthcare needs and their families: telemedicine as a bridge to care. Telemed E Health. (2017) 23:18–24. doi: 10.1089/tmj.2016.0055
58. Yager, PH, Clark, M, Cummings, BM, and Noviski, N. Parent participation in pediatric intensive care unit rounds via telemedicine: feasibility and impact. J Pediatr. (2017) 185:181–186.e3. doi: 10.1016/j.jpeds.2017.02.054
59. Stelson, EA, Carr, BG, Golden, KE, Martin, N, Richmond, TS, Delgado, MK, et al. Perceptions of family participation in intensive care unit rounds and telemedicine: a qualitative assessment. Am J Crit Care. (2016) 25:440–7. doi: 10.4037/ajcc2016465
60. Banks, J, Corrigan, D, Grogan, R, El-Naggar, H, White, M, Doran, E, et al. LoVE in a time of CoVID: clinician and patient experience using telemedicine for chronic epilepsy management. Epilepsy Behav. (2021) 115:107675. doi: 10.1016/j.yebeh.2020.107675
61. Abbatemarco, JR, Hartman, J, McGinley, M, Bermel, RA, Boissy, A, Chizmadia, DT, et al. Providing person-centered care via telemedicine in the era of COVID-19 in multiple sclerosis. J Patient Exp. (2021) 8:81474. doi: 10.1177/2374373520981474
62. Wang, Y, Shan, C, Tian, Y, Pu, C, and Zhu, Z. Bibliometric analysis of global research on perinatal palliative care. Front Pediatr. (2022) 9:827507. doi: 10.3389/fped.2021.827507
63. Web of Science Journal Evaluation Process and Selection Criteria. Clarivate. (2024). Available at: https://clarivate.com/products/scientific-and-academic-research/research-discovery-and-workflow-solutions/webofscience-platform/web-of-science-core-collection/editorial-selection-process/editorial-selection-process (Accessed May 17, 2024).
Keywords: neonatal care, pediatrics, adult medicine, intensive care, palliative care, end-of-life care, family involvement, digitalisation
Citation: Hriberšek M, Eibensteiner F, Bukowski N, Yeung AWK, Atanasov AG and Schaden E (2024) Research areas and trends in family-centered care in the 21st century: a bibliometric review. Front. Med. 11:1401577. doi: 10.3389/fmed.2024.1401577
Received: 20 March 2024; Accepted: 27 May 2024;
Published: 11 June 2024.
Edited by:
Waseem Jerjes, Imperial College London, United KingdomReviewed by:
Andréia Cruz, Federal University of São Paulo, BrazilCopyright © 2024 Hriberšek, Eibensteiner, Bukowski, Yeung, Atanasov and Schaden. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eva Schaden, ZXZhLnNjaGFkZW5AbWVkdW5pd2llbi5hYy5hdA==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.