
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Med. , 06 January 2025
Sec. Healthcare Professions Education
Volume 11 - 2024 | https://doi.org/10.3389/fmed.2024.1401124
Background: The integration of interdisciplinary clinical reasoning and decision-making into the medical curriculum is imperative. Novel, high-quality e-learning environments, encompassing virtual clinical and hands-on training, are essential. Consequently, we evaluated the efficacy of a case-based e-learning approach.
Method: The impact of a case-based interdisciplinary e-learning environment with an integrated question/feedback system on medical students' academic performance was examined in a cross-sectional sample of different study years, longitudinally matched per academic year. Differences between the groups were analyzed through an unpaired t-test.
Results: The exam results of students who participated in the e-learning course (n = 296) were compared with those of all students at the university (n = 5,800). A statistically significant (p-value < 0.01) improvement in students' final examination grades was observed through intensive training on the offered platform.
Conclusions: Our analyses demonstrated the positive influence of a case-based e-learning approach within the Viennese medical curriculum.
Clinical reasoning is an essential tool for all kinds of thinking processes. It consists of developing internalized terms [e.g., via scenarios or integrated thematic instructions (1)] and their integration into new situations. Clinical reasoning can be divided into intuitive and analytical components (2). Research on mental processes shows that key characteristics for training the analytic components are disease patterns stored in 'frames', clinical scenarios, semantic networks or qualifiers, or illness scripts. Repeated presentation and exercise of clinical cases are crucial for efficient learning (2–4).
Associative learning must be stimulated to provide a training tool that helps students transfer their declarative knowledge to procedural knowledge. In case of associative learning, two stimuli have a temporal relationship: a person responds to the first stimulus in anticipation of the second (neural link/association = foundation) (5–8). As a result of the reclassification of stimuli, response drivers arise: conditional appetence, conditional action, conditional aversion, and conditioned inhibition. For clinical reasoning trained through associative learning, procedural knowledge must be built through polythematic or crosslinking thinking. The ability to link information (thoughts, symbols, images, and scenes) in a meaningful way and master it requires creative processes that combine seemingly unrelated areas (domains) (9–14). Case-based learning environments are optimal for teaching and training clinical reasoning (7).
To foster motivational aspects of lifelong learning in students, e-learning is an ideal approach for teaching students (15). Moreover, controlled e-learning programs with detailed feedback are a tool to prevent emotional exhaustion and are highly accepted among students (16). As one form of e-learning, distance learning is defined by UNESCO as the separation of teachers and learners of various shapes in space or time in exchange for electronic or printed materials (15, 17).
Martin et al. (18) evaluated the term' online learning' to specify the latest form of distance education. Significant developments have occurred since the first flare-up on the horizon of didactics, which have also been scientifically supported. Over time, meta-analyses and second-order meta-analyses show the significant superiority of distance learning over face-to-face learning (18). One aspect that fosters learning efficacy is affective involvement (13, 19). Affective involvement, mentalized affectivity, the intuitive and analytical components (c.f. slow and fast thinking processes) are the basis and target factors to be addressed in training (20). Especially for clinical reasoning the importance of associative learning is evident; the stimulus-response principle needed in clinical reasoning is best trained via high affective involvement, time-space autonomy, which is predominantly provided in e-learning formats.
In terms of e-learning, newer concepts based on artificial intelligence and modern visualization software have become, of course, effective teaching methods (21), especially when they are constructed playfully; previous analysis showed good to high acceptance and satisfaction with the course and learning method (13, 22, 23) and had shown to be a bridge to research, especially fostering translational research (10).
AI-supported systems were recently applied and evaluated in a pilot online simulation training based on the dual process theory of clinical reasoning, that is a practicum script, which showed alignment with neurocognitive science principles and a high acceptance among students (24). However, this method lacks interaction with simulated patient training, and outcomes like improved student grades have not yet been evaluated (24).
Hornos et al. stated that errors in complex and uncertain situations are not triggered by inadequate knowledge but by cognitive failures (24). At a certain level, medical students should be trained by patient cases to simulate clinical scenarios over theoretical knowledge (24, 25). Simulation platforms become increasingly popular and show outstanding results (18, 24). It is our conviction that scientific support and the inclusion of scientific professional societies and specialist associations for each medical specialty are essential.
This study aimed to demonstrate how a case-based e-learning approach influences medical students' grades. We hypothesized that the average exam results would improve with additional training with our case-based elective course compared to the students without any extra training. However, the superiority of case-based teaching can only be proven by a hard endpoint, such as the final grade.
The study findings should facilitate a discussion on the role of a case-based e-learning approach as an essential part of undergraduate and postgraduate education. Certainly, case-based teaching can be implemented without e-learning; however, this aspect was not examined in the current study and will be addressed in subsequent research.
Furthermore, the results of this study should contribute to the enhancement of e-learning methodologies, as the teaching methods incorporate a feedback system and authentic clinical scenarios (22).
In 2016, the course “Fallorientierte Lehre (Case-based teaching)—Übungen (Practice): Clinical Reasoning and Clinical Decision Making” was introduced at the Medical University of Vienna provided on a Moodle e-Learning platform (26) (Figure 1).
The course is the result of extensive research in the field of case-based learning. Patient histories from individuals treated at the General Hospital of Vienna were anonymized and processed to learning material, starting in 2014 (27). Guidelines and quizzes have been incorporated into this learning material to create patient cases (25). The test sections were analyzed to ensure good quality and efficacy (28).
The course structure (Figure 2) (12, 13), case designs (Figure 3) (13), blueprints of patient cases (13), scientific background (22), preliminary evaluation results (14), consumer demand and satisfaction, course efficacy, and didactic background had already been described (12, 26, 28). The content was carried out in German. The main idea behind the course structure was to create a stimulating environment where students can apply their knowledge and learn from mistakes without fear of failure (29).
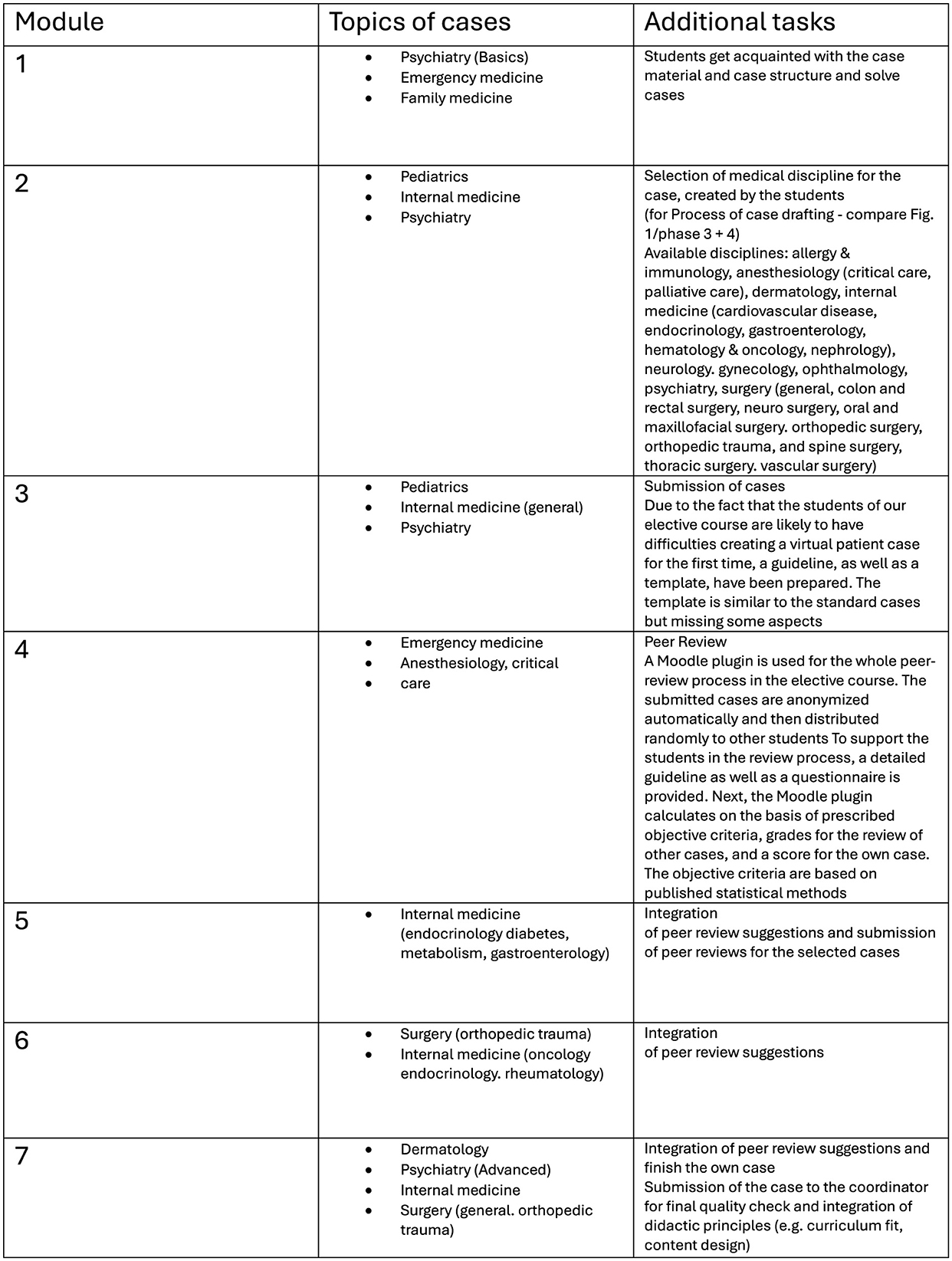
Figure 2. Course structure adapted from Ertl et al. (13).

Figure 3. Course design adapted from Ertl et al. (13).
The concept for this course was based on Bloom's taxonomy criteria (30) and followed the CanMEDS framework (31) and aimed to foster interdisciplinary and crosslinked thinking (22). Case structure is interdisciplinary as they are real world cases. Observing and supporting students are vital strategies for fostering self-assessed learning, and interdisciplinary question-based blended cases promote individual learning plans for optimal knowledge acquisition. However, evaluating these newly implemented teaching concepts should enable further improvements in the medical curriculum. In total, 25,000 exam results were tracked; participants of the elective course were matched to students of the academic year for an individual matching (11, 26).
Beginning in 2013 with small groups, large student cohorts (N = 740 per academic year) have been involved since 2016, as the course can be utilized for preparation and training for the annual final examinations.
Various studies have already analyzed aspects such as student satisfaction, skills transfer, and the transition from declarative to procedural knowledge (7). Different forms of e-learning have been implemented in the medical curriculum, such as clinical rounds (elective non-structured discussion groups) in the fifth academic year (32). As clinical reasoning is the main task and important skill to be acquired before going to real-world care working with real patients in hospital in the sixth and last academic year, the “clinical practical year”, it is necessary to test, if at the end of the fifth academic year students perform well-enough all in all in the summative integrative exam (SIP 5). In this last exam, many questions refer to clinical reasoning. The structured e-learning approach of this course was used to reach students affectively and with more sustainability.
The “Summative Integrative Prüfung” (SIP), a summative integral exam, takes place every year/semester. The last exam (SIP 5) is particularly noteworthy, as it is conducted before the clinical internships. Additionally, the “Objective Structured Clinical Examination” (OSCE) takes place in the fourth academic year (33, 34). The OSCE is used after 4 years of intensive training to evaluate cardiopulmonary resuscitation, basic ultrasound, physical examination, diagnosis and history taking, communication with severe cases and difficult situations, and hospital emergency skills (35).
Medical students from all academic years (n = 5,800) were allowed to participate in the course from the winter term of 2016/17 to the winter term of 2020/21. There were no advertisements for the course, it has been added into the teaching catalog of elective offerings at the administrative platform of the university.
Students provided informed consent to participate and completed the elective course successfully. Subsequently, they then voluntarily submitted detailed questionnaires and exam results through a native built-in Moodle plugin that anonymized all data automatically.
A total of 296 medical students participated in the case-based teaching course and completed all the tasks (26); 32 co-registered students from different universities attended the course but were not analyzed. The study population comprised of 53% female and 47% male students with an average age of 24.1 ± 2.921 (median: 24.00). The nationality of the students was not recorded. From the entrance test a proportion of at least 75% Austrian, 20% foreign mainly German-speaking EU-countries, 5% non-EU countries is known, the language is German.
The questionnaire assessed the educational environment and served as a secondary outcome measure. The instrument employed closed-ended questions, Likert scales, and multiple-choice items to evaluate various soft skills, as depicted in Table 2 (questions in the first column). To capture the attitude toward the course the semantic differential, a standardized and validated assessment was used (results also in 13). To grasp affective involvement and attitudes toward a topic, a semantic differential technique is optimal as it also shows unconscious connotations. The questions presented in Table 2 were self-selected with pending validation (26).
Apart from the main question (primary research question; exam grades), all information was descriptively analyzed and published in various studies (11–14, 22, 26).
The data were collected from the Moodle website and transferred to an SPSS database. Students' answers were used to calculate general questions and explorative analyses. The exam results of the participants were analyzed and compared with those of all medical students. T-tests (for independent samples) for each cohort and exam were performed, and descriptive statistics were used for the questionnaire.
Due to multiple testing, a Bonferroni correction was performed (36). Numeric data are presented as mean ± standard deviation. Statistical analysis, graphics, and diagram generation were performed using SPSS® 26.0 statistics software [SPSS Inc., Chicago, IL, USA (37)]. Bonferroni correction was applied for multiple comparisons, and statistical significance was assumed at a p-value < 0.01.
In Table 1 an overview of all exam results and group comparison between students with or without participation in the e-learning course are given. Participants in the e-learning course performed significantly better on the fourth (SIP4a), fifth (SIP5) (p-value < 0.01), and third years' exams (SIP 3) (p < 0.05) (Table 1).
No statistically significant effect on examination outcomes was observed for OSCE and the annual examinations in the first and second years (SIP1a, SIP1b, and SIP2).
Students in the e-learning course obtained significantly better grades, depending on their experience level (11).
Secondary outcome parameters are presented in Table 2, including students' self-assessment (self-awareness) of soft skills and their attitude toward the offered course, which were evaluated using the open-response sections of the questionnaire employed in the study and have already been published (13, 22), but some notable parameters should be mentioned:
90.5% of the students [1.51 ± 0.774 (M ± SD)] recommended the elective course, and 74.7% suggested using a case-based teaching approach even for postgraduate board certification exams. Among the students, 65.2% preferred a bilingual teaching approach. The elective course was available only in Germany. Skill and exam tracking systems are implemented at many universities, and 56.1% of the students also favored such systems in our study.
A slightly positive increase in subjectively observed patient-centered thinking was reported [0.62 ± 0.928 (M ± SD)]. Furthermore, 60.6% of the students reported that they believed interdisciplinary thinking was cultivated [0.94 ± 0.888 (M ± SD)].
We expected the students to use the courses by themselves. Surprisingly, the students worked in groups to solve the cases, and the average group size was 1.65 students [1.65 ±2.099 (M ± SD)].
Our research demonstrates the substantial impact on clinical reasoning of a structured case-based e-learning approach on students' exam performance, as evidenced by the statistically significant improvement in mean scores.
To our knowledge, no previous evaluation utilizing objective outcome measures such as examination grades has been conducted on a cohort of this magnitude.
From a legal perspective, it is not feasible to implement randomization in a mandatory examination at a public university.
The course was evaluated positively, affectively involving, as the detailed analysis of the semantic differential displaying attitudes, in general, had shown (13, 22).
Being affectively involved fosters intuitive 'fast thinking' (Kahneman) processes, which are necessary for a clinician to build a sound working alliance with the patient. The latter competency is hard to incorporate into training via algorithms or artificial intelligence (AI)-driven programs.
Additionally, slow thinking processes, that is conscious analytical processing, are trained via answering questions and getting feedback. Both ways of learning result in mentalized affectivity, which could be demonstrated as the training course stimulated inquiries and curiosity. Interdisciplinary collaboration was also stimulated. We implemented a forum to make discussions possible directly on the platform (13).
The Viennese e-learning platform, combined with simulated patient contact and an integrated feedback system, is designed to train crosslinking thinking in recognizing clinical patterns and arguing hypotheses and treatment decisions (10, 25). Moreover, controlled feedback is associated with student satisfaction and can be regarded as a major part of burnout prevention in medical students (7, 16, 23, 28).
As individual concepts for learning are required, teaching environments should also be augmented by traditional methods, such as continuous knowledge tests and skills training (e.g., following and practicing with the same cases as provided in the e-learning course via simulated patients) to achieve sufficient medical skills (38, 39).
Moreover, case-based teaching scenarios enriched with modern visualization software, artificial intelligence, and simulation programs should be fostered to train resident physicians or students alongside their bedside teaching. Precise feedback from experienced clinical mentors is a key feature for further curricular planning and, of course, for evaluation and research.
A limitation of the study design was the non-compulsory nature of the elective course. Another potential limitation of this study is the possibility of selection bias among highly motivated and skilled students who enrolled in the offered elective course for additional examination preparation. However, previous studies have similar limitations (2, 39–43). For the SIP1a, SIP1b and the OSCE (first academic year, first semester, and second semester), data available to perform the analysis and compare with the control group was insufficient. Nevertheless, based on our previous studies, we already gained significant results, particularly for the OSCE (7, 27).
A strength of this study is the comparison of the students at different levels. Case-based learning is essential for medical students at a certain training level. A consistent difficulty level of exams was ensured (35, 37, 44) because the exam and test levels were accurately aligned to a specific learning objective and competence level (CanMEDS) (31). Therefore, different annual examinations could be compared, variations in the examination performance of individual cohorts, therefore, need not be considered.
For further teaching considerations, carefully structured learning formats are essential, as medical knowledge expands at an unprecedented rate, and the clinician must be trained as an efficient, judicious, responsible decision-maker and compassionate professional (45).
To the best of our knowledge, this study analyzed the largest cohort of medical students.
In conclusion, the Viennese concept of interdisciplinary case-based e-learning combined with simulated patient contact and a feedback system on implemented questions significantly improves students' academic performance. Further development of the e-learning software, specifically artificial intelligence support for generating feedback questions, is warranted.
Nevertheless, the development of patient cases by clinical physicians remains a crucial component in imparting practical experience.
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: Moodle platform.
SE: Formal analysis, Software, Writing – original draft. PW: Writing – review & editing. HL-S: Writing – review & editing, Conceptualization, Data curation, Methodology, Project administration, Resources, Supervision, Validation.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was carried out within the framework of a diploma thesis at the Medical University of Vienna.
Parts of this manuscript was reviewed by Editage for spelling and grammar errors.
The authors declare that the research was conducted without any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Thistlethwaite JE, Davies D, Ekeocha S, Kidd JM, MacDougall C, Matthews P, et al. The effectiveness of case-based learning in health professional education. A BEME systematic review: BEME Guide No 23. Med Teach. (2012) 34:e421–44. doi: 10.3109/0142159X.2012.680939
2. Kassirer JP. Teaching clinical reasoning: case-based and coached. Acad Med. (2010) 85:1118–24. doi: 10.1097/ACM.0b013e3181d5dd0d
3. Caspar F. What goes on in a psychotherapist's mind? Psychother Res. (1997) 7:105–25. doi: 10.1080/10503309712331331913
4. Norman G. Research in clinical reasoning: past history and current trends. Med Educ. (2005) 39:418–27. doi: 10.1111/j.1365-2929.2005.02127.x
5. Schmidmaier R, Eiber S, Ebersbach R, Schiller M, Hege I, Holzer M, et al. Learning the facts in medical school is not enough: which factors predict successful application of procedural knowledge in a laboratory setting? BMC Med Educ. (2013) 13:28. doi: 10.1186/1472-6920-13-28
6. Förtsch C, Sommerhoff D, Fischer F, Fischer MR, Girwidz R, Obersteiner A, et al. Systematizing professional knowledge of medical doctors and teachers: development of an interdisciplinary framework in the context of diagnostic competences. Educ Sci. (2018) 8:207. doi: 10.3390/educsci8040207
7. Turk B, Ertl S, Wong G, Wadowski PP, Löffler-Stastka H. Does case-based blended-learning expedite the transfer of declarative knowledge to procedural knowledge in practice? BMC Med Educ. (2019) 19:447. doi: 10.1186/s12909-019-1884-4
8. Bormann T, Weiller C. Neuropsychological disorders of memory. Nervenarzt. (2020) 91:543–52. doi: 10.1007/s00115-020-00934-9
9. Löffler-Stastka H, Wong G. Learning and competence development via clinical cases – what elements should be investigated to best train good medical doctors? World J Meta-Anal. (2020) 8:178–89. doi: 10.13105/wjma.v8.i3.178
10. Wadowski PP, Litschauer B, Seitz T, Ertl S, Löffler-Stastka H. Case-based blended eLearning scenarios—adequate for competence development or more? Neuropsychiatrie. (2019) 33:207–11. doi: 10.1007/s40211-019-00322-z
11. Ertl S, Löffler-Stastka H. Vienna tracking students in 25.000 exam results. In: AMEE Congress. Abstract book (2018).
12. Ertl S, Stastka L, Löffler-Stastka H. Strukturiertes fallorientiertes LernenStructured Case-Oriented Learning. Psychopraxis Neuropraxis. (2020) 23:240–5. doi: 10.1007/s00739-020-00655-3
13. Ertl S, Steinmair D, Löffler-Stastka H. Encouraging communication and cooperation in e-learning: solving and creating new interdisciplinary case histories. GMS J Med Educ. (2021) 38:Doc62. doi: 10.3205/zma001458
14. Ertl S, Löffler-Stastka H. Case Based Blended Learning (CBBL) – a strategy to foster the transfer of declarative to procedural knowledge or more? In: AMEE Congress. Abstract book (2019).
15. Tirziu AM, Vrabie C. Education 20: E-learning methods. Proc Soc Behav Sci. (2015) 186:376–80. doi: 10.1016/j.sbspro.2015.04.213
16. Pathipati AS, Cassel CK. Addressing student burnout: what medical schools can learn from business schools. Acad Med. (2018) 93:2215. doi: 10.1097/ACM.0000000000002215
17. Ellaway R, Masters K, AMEE. Guide 32: E-learning in medical education Part 1: learning, teaching and assessment. Med Teach. (2008) 30:455–73. doi: 10.1080/01421590802108331
18. Martin F, Sun T, Westine CD, Ritzhaupt AD. Examining research on the impact of distance and online learning: a second-order meta-analysis study. Educ Res Rev. (2022) 36:100438. doi: 10.1016/j.edurev.2022.100438
19. Leake DB. Case-Based Reasoning: Experiences, Lessons and Future Directions. Cambridge, MA: MIT Press (1996).
21. Mergen M, Junga A, Risse B, Valkov D, Graf N, Marschall B. Immersive training of clinical decision making with AI driven virtual patients–a new VR platform called medical training. GMS J Med Educ. (2023) 40.
22. Ertl S, Steinmair D, Wadowski PP, Löffler-Stastka H. What we need for encoding of memory and emotional reconsolidation. Psychiatr Danub. (2022) 34:209–18. doi: 10.24869/psyd.2022.209
23. Chéron M, Ademi M, Kraft F, Löffler-Stastka H. Case-based learning and multiple choice questioning methods favored by students. BMC Med Educ. (2016) 16:1–7. doi: 10.1186/s12909-016-0564-x
24. Hornos E, Pleguezuelos EM, Bala L, van der Vleuten C, Sam AH. Online clinical reasoning simulator for medical students grounded on dual-process theory. Med Educ. (2024) 58:580–1. doi: 10.1111/medu.15322
25. Wadowski PP, Steinlechner B, Schiferer A, Löffler-Stastka H. From clinical reasoning to effective clinical decision making—new training methods. Front Psychol. (2015) 6:473. doi: 10.3389/fpsyg.2015.00473
26. Ertl S. Impact of e-Learning on Learning Efficiency and Interdisciplinary Collaboration (Diploma Thesis). Vienna: Medical University of Vienna (2020).
27. Turk BR, Krexner R, Otto F, Wrba T, Löffler-Stastka H. Not the ghost in the machine: transforming patient data into E-learning cases within a case-based blended learning framework for medical education. Proc Soc Behav Sci. (2015) 186:713–25. doi: 10.1016/j.sbspro.2015.04.106
28. Seitz T, Löffler-Stastka H. Do our medical students even want e-learning? A user rated evaluation of case based e-learning in undergraduate medical education at the medical university of Vienna. Adv Soc Sci Res J. (2015) 2:156–61. doi: 10.14738/assrj.24.1003
29. Ronningstam E, Baskin-Sommers AR. Fear and decision-making in narcissistic personality disorder—a link between psychoanalysis and neuroscience. Dialog Clin Neurosci. (2013) 15:191–201. doi: 10.31887/DCNS.2013.15.2/eronningstam
30. Bloom B, Englehart M, Furst E, Hill W, Krathwohl D. (1956). Taxonomy of Educational Objectives: The Classification of Educational Goals. Handbook I Cognitive Domain. New York and Toronto Longmans, Green. - References - Scientific Research Publishing. Available at: https://www.scirp.org/(S(lz5mqp453edsnp55rrgjct55))/reference/ReferencesPapers.aspx?ReferenceID=463242 (accessed May, 2024).
31. Frank JR, Snell L, Sherbino J, Boucher A. CanMEDS 2015. Physician Competency Framework Series I. Collège royal des médecins et chirurgiens du Canada (2015).
32. MedUni Wien. Curriculum Humanmedizin (2024). Available at: https://www.meduniwien.ac.at/web/studierende/mein-studium/diplomstudium-humanmedizin/studienplan-studienplanfuehrer/ (accessed September 28, 2024).
33. Himmelbauer M, Koller D, Bäwert A, Horn W. Der Prüfungsmix an der Medizinischen Universität Wien. Wiener Medizinische Wochenschrift. (2019) 169:101–9. doi: 10.1007/s10354-018-0662-y
34. MedUni Wien. Prüfungskalender (2024). Available at: https://www.meduniwien.ac.at/web/studierende/mein-studium/diplomstudium-humanmedizin/pruefungen-pruefungsergebnisse/pruefungskalender/ (accessed May 23, 2024).
35. MedUni Vienna. OSCE - Integriertes Klinisch-Praktisches Propädeutikum (2024). Available at: https://teachingcenter.meduniwien.ac.at/en/unsere-abteilungen/assessment-skills/osce-integriertes-klinisch-praktisches-propaedeutikum/ (accessed May 23, 2024).
36. Kowalski A, Enck P. Statistische methoden bei mehrfachtestung die bonferroni-korrektur. Psychother Psychosom Med Psychol. (2010) 60:286–7. doi: 10.1055/s-0030-1248493
37. Österreich IBM. SPSS Statistics. (2024). Available at: https://www.ibm.com/at-de/products/spss-statistics (accessed May, 2024).
38. Himmelbauer M, Seitz T, Seidman C, Löffler-Stastka H. Standardized patients in psychiatry–the best way to learn clinical skills? BMC Med Educ. (2018) 18:1–6. doi: 10.1186/s12909-018-1184-4
39. Dickinson BL, Lackey W, Sheakley M, Miller L, Jevert S, Shattuck B. Involving a real patient in the design and implementation of case-based learning to engage learners. Adv Physiol Educ. (2018) 42:118–22. doi: 10.1152/advan.00174.2017
40. Maleck M, Fischer MR, Kammer B, Zeiler C, Mangel E, Schenk F, et al. Do computers teach better? A media comparison study for case-based teaching in radiology. Radiographics. (2001) 21:1025–32. doi: 10.1148/radiographics.21.4.g01jl091025
41. Srinivasan M, Wilkes M, Stevenson F, Nguyen T, Slavin S. Comparing problem-based learning with case-based learning: effects of a major curricular shift at two institutions. Acad Med. (2007) 82:74–82. doi: 10.1097/01.ACM.0000249963.93776.aa
42. Gartmeier M, Bauer J, Fischer MR, Hoppe-Seyler T, Karsten G, Kiessling C, et al. Fostering professional communication skills of future physicians and teachers: effects of e-learning with video cases and role-play. Instr Sci. (2015) 43:443–62. doi: 10.1007/s11251-014-9341-6
43. Kopp V, Stark R, Fischer MR. Fostering diagnostic knowledge through computer-supported, case-based worked examples: effects of erroneous examples and feedback. Med Educ. (2008) 42:823–9. doi: 10.1111/j.1365-2923.2008.03122.x
44. MedUni Wien. Prüfungen & Prüfungsergebnisse Humanmedizin Studium an der MedUni Wien. (2024). Available at: https://www.meduniwien.ac.at/web/en/studierende/mein-studium/diplomstudium-humanmedizin/pruefungen-pruefungsergebnisse/ (accessed May, 2024).
Keywords: case-based blended learning, computer-assisted instruction, e-learning, distance learning competence, transfer learning
Citation: Ertl S, Wadowski PP and Löffler-Stastka H (2025) Improving students' performance via case-based e-learning. Front. Med. 11:1401124. doi: 10.3389/fmed.2024.1401124
Received: 22 March 2024; Accepted: 10 December 2024;
Published: 06 January 2025.
Edited by:
Ashraf Alam, Indian Institute of Technology Kharagpur, IndiaReviewed by:
Luh Putu Putrini Mahadewi, Ganesha University of Education, IndonesiaCopyright © 2025 Ertl, Wadowski and Löffler-Stastka. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Henriette Löffler-Stastka, aGVucmlldHRlLmxvZWZmbGVyLXN0YXN0a2FAbWVkdW5pd2llbi5hYy5hdA==
†ORCID: Sebastian Ertl orcid.org/0000-0001-9234-2232
Patricia P. Wadowski orcid.org/0000-0003-2462-4515
Henriette Löffler-Stastka orcid.org/0000-0001-8785-0435
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.