
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med., 31 July 2024
Sec. Obstetrics and Gynecology
Volume 11 - 2024 | https://doi.org/10.3389/fmed.2024.1397258
Objective: This study aimed to investigate the efficacy of postpartum nursing guidance in the treatment of early pelvic floor dysfunction (PFD) in women of advanced maternal age.
Methods: A total of 146 patients of advanced maternal age admitted to our hospital between January and December 2021 were enrolled in this study and randomly divided into two groups: the control group and the experimental group, with 73 patients in each group. Parturients in the control group received routine pelvic floor rehabilitation treatment, whereas those in the experimental group were given individualized postpartum nursing guidance alongside routine pelvic floor rehabilitation treatment. The recovery of pelvic floor muscle (PFM) strength, the incidence of PFD diseases and nursing satisfaction were compared between the two groups after 3 months of treatment.
Results: The enhancement of PFM strength in the experimental group significantly surpassed that in the control group. Furthermore, the experimental group exhibited a notably lower overall occurrence of PFD and significantly greater maternal satisfaction compared with the control group, and the difference was statistically significant (p < 0.05).
Conclusion: Combining postpartum nursing guidance with pelvic floor rehabilitation for women of advanced maternal age represents a treatment regimen deserving of clinical endorsement, as it offers numerous advantages, including substantial improvement in PFM strength, decreased incidence of PFD and enhanced patient satisfaction.
Female pelvic floor dysfunction (PFD) is a group of gynecological diseases with high incidence due to defects, degeneration, injury and dysfunction of the pelvic support structure (1). Data from epidemiological studies reveal high-risk factors for PFD, including age, obesity, constipation, reproductive system inflammation, heredity, pregnancy and delivery, diabetes, connective tissue diseases and neuropathy (2, 3). In the process of vaginal delivery, excessive stretching of maternal pelvic floor muscles (PFMs) and fascia caused by vaginal dilation and injury leads to decreased elasticity of the maternal PFMs and is accompanied by the disruption of muscle fibers and other symptoms (4, 5). Consequently, PFD can severely affect women’s quality of life and mental health (6) and can easily induce other gynaecological diseases (7).
The recent enforcement of China’s universal two-child policy has resulted in a rise in the prevalence of clinically advanced maternal-age cases. With older age and diminished reproductive organ function, women of advanced maternal age exhibit notably higher rates of pregnancy and delivery complications, as well as pelvic floor injuries, compared with non-advanced maternal-age cases (8). Research indicates that advancing age is a contributing factor to the onset and progression of PFD (9). Therefore, it is important to conduct studies on rehabilitation treatment for postpartum PFD in women of advanced maternal age. Currently, no surgical treatment for PFD has been proposed in clinical practice. Most patients are advised to undergo rehabilitation training to improve their PFM strength, thus reducing the clinical manifestations of PFD. Furthermore, electrical stimulation combined with biofeedback therapy can restore the pelvic floor function of postpartum women (10, 11).
The female pelvic floor system, including fascia, multi-layer muscles, ligaments and nerves, is crucial for maintaining the normal position of pelvic organs (12, 13). During pregnancy, the enlarged and descended uterus increases the burden on the pelvic floor support system, and failure to restore it promptly after delivery can lead to corresponding dysfunction (14).
Zhou et al. (15) found that age, delivery times, menopause and urinary tract infections are risk factors for PFD, especially during pregnancy and childbirth. Women of advanced maternal age have three superimposed high-risk factors (age, pregnancy, and delivery), making them prone to postpartum PFD, which seriously affects their quality of life. Studies have shown that active pelvic floor rehabilitation, including PFM exercises, biofeedback and electrical stimulation, can effectively improve excessive PFM strength. Training the pelvic floor support structure using the levator ani muscle can restore and strengthen pelvic floor function and promote PFM strength recovery. Furthermore, it is low risk and usually involves no complications (16). It plays a vital role in preventing and treating pelvic floor disorders (17, 18).
However, some studies have highlighted poor compliance with various clinically developed rehabilitation measures among some women due to insufficient knowledge of PFD or significant postpartum mood fluctuations. These studies also suggest that integrating postpartum nursing guidance into routine pelvic floor rehabilitation training, including health education, psychological counseling, Kegel exercises and regular follow-ups, can significantly enhance the coordination of maternal rehabilitation efforts. This approach holds positive significance in ensuring effective rehabilitation outcomes for patients. The efficacy of PFM exercises is closely related to their duration, requiring continuous exercise for more than 3 months. Better results can only be achieved through intensive training and follow-ups (19). Long-term postpartum PFM exercise can significantly improve PFM strength, which is of great importance for improving PFD symptoms and preventing urinary incontinence (20). One study (21) highlighted pessimistic postpartum PFM training (PFMT) adherence and certain limitations in addressing personalized nursing needs during the puerperium. Several studies have emphasized the crucial role of providing comprehensive and systematic rehabilitation intervention guidance for postpartum women in mitigating disease onset. These efforts have profound significance for national medical resource allocation and long-term reduction of the country’s medical burden (22–26).
A recent comprehensive review by DeLancey et al. (27) highlight vaginal birth as the largest modifiable risk factor for prolapse and stress incontinence, and discusses the multifactorial nature of risk factors for levator injury. The authors suggest potential steps to reduce injuries and emphasize the importance of prenatal education, informed decision-making during labor, and postpartum care and rehabilitation.
We hypothesize that postpartum nursing guidance is an independent predictor of parturient recovery beyond physical therapy alone. This study aims to investigate the effect of postpartum nursing guidance on early pelvic floor function rehabilitation in advanced maternal age to promote the improvement of postpartum pelvic floor function and reduce the occurrence of PFD.
This prospective study enrolled pregnant women of advanced maternal age who provided signed written consent. The inclusion criteria were based on the diagnosis of PFD after delivery, which was confirmed by the International Continence Society (ICS) criteria (28). The exclusion criteria were as follows: (1) parturients with a history of pelvic disease surgery; (2) parturients who experienced multiple pregnancies or underwent cesarean section surgeries; (3) parturients with a history of other chronic diseases known to impact pelvic floor function, such as diabetes, hypertension or neurological disorders; and (4) parturients who expressed unwillingness or inability to adhere to the intervention protocol.
A total of 146 parturients of advanced maternal age (aged ≥35 years at delivery) admitted to our hospital between January and December 2021 were included in this study. We included the participants within 1 week after vaginal delivery, as we wanted to assess the early PFD and intervene as soon as possible. The advanced maternal age cohort was randomly divided into two groups using the random number table method: the control group and the experimental group, each comprising 73 parturients.
In the control group, the parturients’ age ranged from 35 to 42 years, with an average of 37.55 ± 1.73 years and a median of 37 years. Gestational age varied from 242 to 286 days, with an average of 268.38 ± 9.43 days. The PFM strength scale indicated grade 0 in 5 cases, grade I in 32 cases, grade II in 26 cases and grade III in 10 cases. Disease types included urinary incontinence in 26 cases and pelvic organ prolapse in 54 cases. For the experimental group, the parturients’ age ranged from 35 to 47 years, with an average of 38.12 ± 2.02 years and a median of 38 years. Gestational age ranged from 239 to 287 days, with an average of 266.79 ± 10.86 days. The PFM strength scale showed grade 0 in 6 cases, grade I in 30 cases, grade II in 26 cases and grade III in 9 cases. Disease types included urinary incontinence in 26 cases and pelvic organ prolapse in 58 cases. There were no statistically significant differences observed between the two groups of parturients regarding general data (p > 0.05), which were comparable.
The median values for age and gestational data for both the control and experimental groups are presented in Table 1. No significant differences were found between the two groups in terms of parity, fetal weight, delivery mode, episiotomy, perineal tear or pelvic floor injury (p > 0.05), indicating comparability and balance across these aspects, as depicted in Table 1. The normality of the data in Table 1 was confirmed using the Kolmogorov–Smirnov test, with the results indicating a normal distribution (p > 0.05). The study was approved by the ethics committee of our hospital (Approval number: Fast Review-Research-2018-093). The CONSORT flow diagram illustrating the enrollment, allocation, follow-up, and analysis of the study participants is depicted in Figure 1.
The parturients in the control group received routine pelvic floor rehabilitation therapy, including low-frequency electrical stimulation and biofeedback therapy, as well as routine postpartum rehabilitation guidance. The specific methods used were as follows: (1) The American neuromuscular electrical stimulation device, Automuse 930 (a therapeutic instrument for electrical muscle stimulation manufactured by Automuse Systems Inc., Salt Lake City, Utah, United States), was selected to deliver different intensities of low-frequency electrical impulses and an individualized biofeedback program. This stimulated the weakened pelvic floor muscles to contract and train rhythmically, strengthened the pelvic floor muscles and provided real-time feedback to effectively promote rehabilitation. Each treatment lasted 30 min and was provided twice a week for a total of 15 treatments. (2) During routine postpartum rehabilitation instruction, parturients were educated on the significance of postpartum pelvic floor rehabilitation to enhance their self-care awareness and self-management skills. A full-time nurse provided health education to each parturient, and a personalized rehabilitation plan was devised based on individual differences to facilitate systematic exercise.
The parturients in the experimental group received the same pelvic floor rehabilitation therapy as the control group, including low-frequency electrical stimulation and biofeedback therapy. In addition to this routine therapy, the experimental group received a postpartum nursing guidance intervention encompassing the following measures: (1) Health education: pelvic floor rehabilitation-related knowledge and cooperation techniques were presented to parturients through visual aids, such as images, videos and health brochures. Additionally, one-on-one consultation services were extended through telephone, WeChat or other means. Prompt responses to parturients’ inquiries and targeted guidance were provided to enhance awareness and compliance with rehabilitation training. (2) Psychological counseling: due to their age and concerns about treatment outcomes, disease recurrence and the demands of childcare, parturients of advanced maternal age are susceptible to anxiety and other negative emotions. To address this, individualized psychological counseling was provided to the parturients based on their educational background and personality traits. This aimed to assist them in accurately recognizing their current pelvic floor issues and understanding the potential outcomes. Additionally, successful cases of pelvic floor rehabilitation were shared with them, enhancing the trust of postpartum women undergoing rehabilitation training and motivating active participation in the exercises. (3) Pelvic floor muscle training, commonly known as Kegel training, involves engaging the anal muscles. Parturients were instructed to contract their PFMs upon exhaling and to relax them while inhaling. Advanced stages of the training included holding the PFM contraction while maintaining normal breathing. They were encouraged to perform focused PFMT without distraction for at least 15 min daily, integrating PFM contractions into their daily activities as a complementary strategy. Additionally, parturients were advised to empty their bladders before starting the exercise by lying flat with the knees naturally bent and open at the width of the iliac crest, followed by a gentle upward tightening of the vagina and anus. The above movements were repeated for 5 min each time at the start of the exercise and gradually increased to 15–25 min, 2–3 times/day. (4) Regular follow-ups: during the treatment, the parturients were supervised and instructed daily to adhere to the PFMT through WeChat. The parturients were scheduled for weekly follow-up sessions to foster positive communication with them and their families, who were urged to provide full support, helping the parturients maintain a positive attitude toward their rehabilitation training.
Three months after completing treatment, the parturients returned to the hospital for follow-up appointments. On average, the experimental group spent 30 min per week with the nurse or engaging in interactive chats.
The differences in treatments received by the control and experimental groups are summarized in Table 2.
Electrophysiological testing of PFM endurance was performed before and 3 months after treatment, and muscle endurance was measured by the percentage of parturients who were able to hold the contraction for 10 s or more, following the recommendations of the ICS report on the terminology of PFM assessment (29). The PFMs were classified into two types according to their function and innervation: Type I muscle fibers, responsible for the maintenance of pelvic organ support and innervated by the pudendal nerve, and Type II muscle fibers, responsible for the rapid contraction and relaxation of the PFM and innervated by the sacral nerve. The muscle endurance of each type was calculated according to the percentage of parturients who met the criterion.
The presence of a levator ani tear, defined as a detachment of the pubovisceral portion of the levator ani muscle from the pubic bone, was assessed by palpating bilaterally during the PFM strength assessment using the pubovisceral muscle palpation technique described by Dietz and Shek (30). The PFM strength was graded using the modified Oxford scale, which ranges from 0 (no contraction) to 5 (strong contraction) (30, 31).
Improvement in urinary incontinence was assessed and compared between the two groups before treatment and 3 months after treatment. Occasional leakage of urine during laughing, coughing or sneezing was considered mild; frequent leakage of urine during walking, climbing stairs or sexual intercourse was considered moderate; involuntary leakage of urine at rest or while standing was considered severe. Urinary incontinence was evaluated using a questionnaire that was developed based on the International Consultation on Incontinence Questionnaire-Short Form (ICIQ-SF) questionnaire. The questionnaire asked the parturients to rate the frequency and severity of their urinary leakage during different activities, such as laughing, coughing, sneezing, walking, climbing stairs or sexual intercourse. The questionnaire also asked the parturients to rate the impact of their urinary incontinence on their quality of life. It had a total score of 21, with higher scores indicating worse urinary incontinence, which was classified as mild, moderate or severe according to score ranges of 1–5, 6–12, and 13–21, respectively.
Pelvic organ prolapse was evaluated before treatment and 3 months after treatment. The pelvic organ prolapse quantitative quantification (POP-Q) scale was used to evaluate pelvic organ prolapse in a quiet environment after the participants were instructed to voluntarily empty their bladder, maintain the lithotomy position and sterilize the vulva. Pelvic organ prolapse was graded according to the POP-Q scale as follows: scale 0 indicated no prolapse; scale I indicated that the farthest end of prolapse was located at <−1 cm; scale II indicated that the farthest end of prolapse was located at −1 to +1 cm; scale III indicated that the farthest end of prolapse was located at +1 cm – (total vaginal length – 2) cm; scale IV indicated that the farthest end of prolapse was located at >(total length of vagina – 2) cm.
The nursing satisfaction was measured using a questionnaire that included four rating indices: health education, psychological care, service attitude and rehabilitation effect. Each index was evaluated in three grades: satisfied, basically satisfied and unsatisfied. The questionnaire had a total score of 12, with higher scores indicating higher nursing satisfaction. Satisfaction = (number of satisfied cases + number of basically satisfied cases)/total number of cases × 100%.
The sample size was determined by a power analysis using G*Power software (v.3.1.9.7). This study assumed a medium effect size of 0.5 for the main outcome of PFM strength. The power was set at 0.8, and the significance level was set at 0.05, which resulted in 64 participants per group. The sample size was increased to 73 participants per group to account for possible dropouts and missing data. All data in this study were statistically analyzed using SPSS 22.0 statistical software. The measurement data were expressed as mean ± standard deviation, and a t-test was conducted between the groups. Count data were expressed as rates, and a chi-squared (χ2) test was performed between the groups; p < 0.05 was considered statistically significant.
No statistically significant differences were observed in PFM strength between the two groups before intervention (p > 0.05). Three months after the intervention, the improvement of PFM strength in the experimental group was significantly better than that in the control group, with a statistically significant difference (p < 0.05) (Table 3). The normality of the data in Table 3 was verified using the Kolmogorov–Smirnov test, and the results showed that the data were normally distributed (p > 0.05).
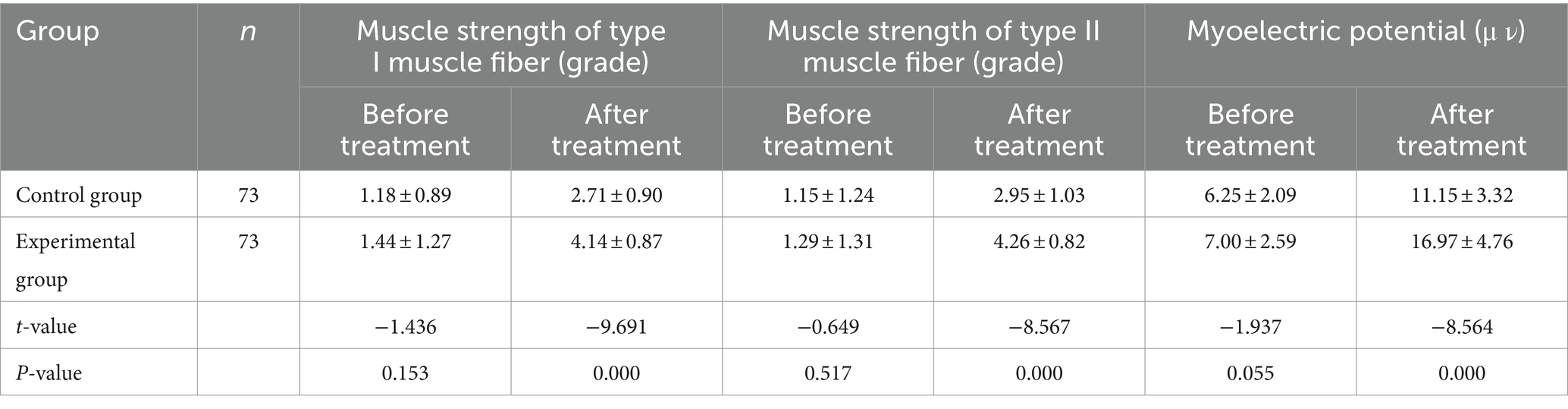
Table 3. Comparison of pelvic floor muscle strength between the two groups before and after treatment (x ± s).
Three months after the intervention, the total incidence of urinary incontinence in the experimental group was significantly lower than that in the control group, with a statistically significant difference (p < 0.05) (Table 4). This study assessed the types of incontinence using the ICIQ-SF questionnaire, which classified the incontinence into stress, urge or mixed types. Most participants had stress incontinence (56.8%), followed by mixed incontinence (32.9%) and urge incontinence (10.3%). The intervention improved all types of incontinence, but the improvement was more significant for stress incontinence (p < 0.01) than for mixed or urge incontinence (p < 0.05).
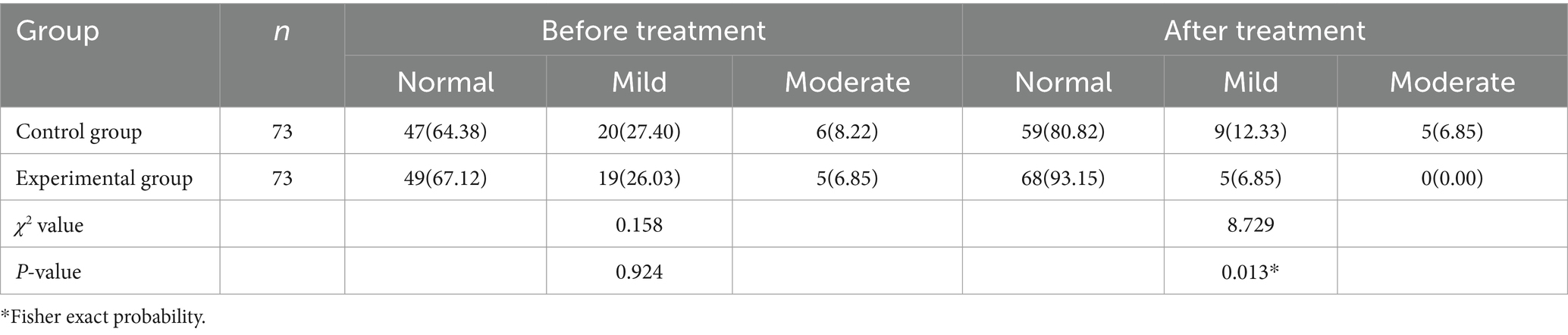
Table 4. Comparison of the improvement of urinary incontinence between the two groups before and after treatment [cases (%)].
After treatment, the POP-Q of both groups improved, and the improvement degree of the experimental group was better than that of the control group (p < 0.05), with a statistically significant difference (p < 0.05) (Table 5). The POP-Q system utilized six specified points on the vagina (Aa, Ba, C, D, Ap, and Bp) to measure the distance from the hymen, which served as the reference point (defined as zero). These points could be positive (below the hymen) or negative (above the hymen), with the severity of the prolapse increasing as the point moved higher. This study calculated the mean and standard deviation of the POP-Q points for each group and used the t-test to compare the differences between the groups. The results are shown in Table 6. After treatment, the POP-Q of both groups improved, and the improvement degree of the experimental group was higher than that of the control group (p < 0.05), which was statistically significant (p < 0.05).
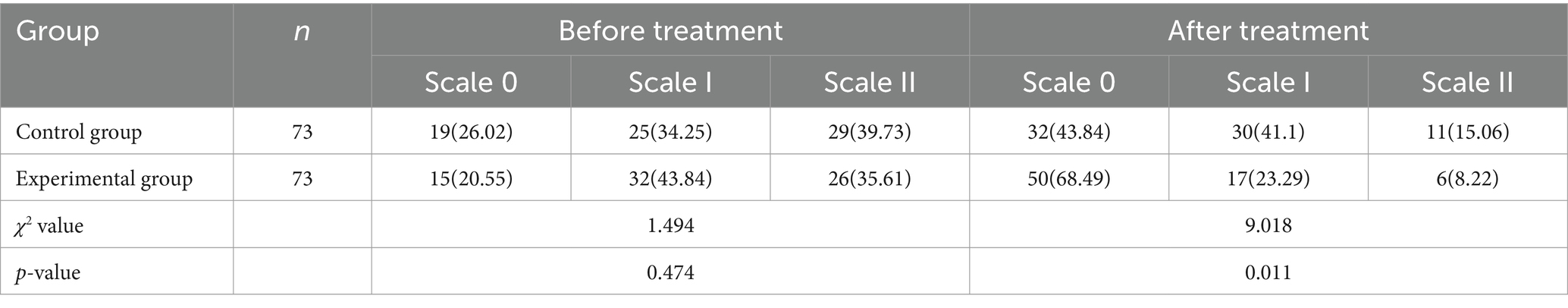
Table 5. Comparison of quantitative stages of pelvic organ prolapse before and after treatment between the two groups [cases (%)].
The nursing satisfaction of the experimental group was significantly higher than that of the control group, which was statistically significant (p < 0.05). A separate statistical analysis was performed for each of the four rating indices of the questionnaire, and the results showed that the experimental group had significantly higher scores than the control group in terms of all indices (p < 0.05) (Table 7).
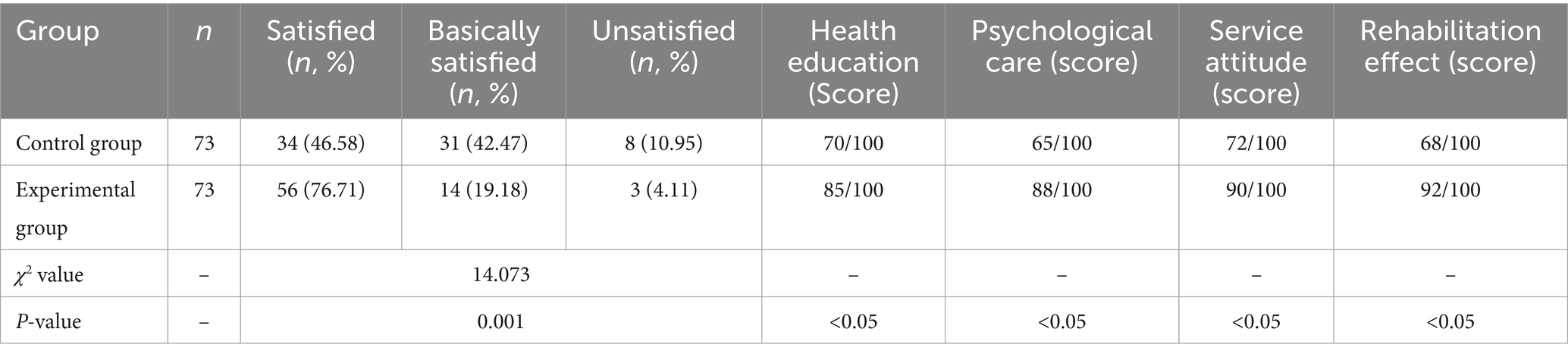
Table 7. Comparison of nursing satisfaction between the two groups (including health education, psychological care, service attitude, and rehabilitation effect).
The remarkable success of postpartum nursing guidance in improving PFD recovery can be attributed to several factors. First, the comprehensive nature of the nursing intervention, which included health education, psychological counseling, PFMT and regular follow-ups, provided a holistic approach to addressing the complex needs of postpartum women (32, 33). Health education empowered patients with the knowledge and skills necessary to actively participate in their recovery, while psychological counseling helped alleviate anxiety and promote adherence to the rehabilitation programme (34).
Moreover, the individualized approach to postpartum nursing guidance, tailored to each patient’s educational background and personality traits, likely enhanced the effectiveness of the intervention (35). By establishing a trusting relationship and providing ongoing support, nurses were able to motivate patients and encourage consistent engagement in PFMT (36). The regular follow-up sessions also allowed for the early identification and resolution of any challenges or concerns, further promoting patient adherence and satisfaction (37).
Another potential factor contributing to the success of postpartum nursing guidance is the increased awareness and self-efficacy that it fosters among postpartum women (38). Through education and support, patients develop a better understanding of their pelvic floor health and the importance of active participation in their recovery process. This heightened awareness and sense of control may lead to improved outcomes and long-term maintenance of pelvic floor function.
However, we acknowledge certain limitations, such as the relatively small sample size and the short follow-up period. Future studies with larger cohorts and longer-term follow-ups are warranted to confirm the sustainability of the observed benefits.
In recent years, there has been growing interest in exploring innovative strategies for the prevention and management of pelvic floor disorders. One promising area of research is the use of regenerative medicine approaches, such as stem cell therapy, to promote the regeneration and repair of damaged pelvic floor tissues (39). While still in the early stages of development, these novel therapies may offer new possibilities for the treatment of PFD in the future.
Another emerging trend is the integration of digital health technologies into pelvic floor rehabilitation programs. Mobile health apps, wearable devices, and virtual reality systems have shown potential for improving patient engagement, adherence, and outcomes in PFMT (40). These technologies can provide real-time feedback, personalized guidance, and remote monitoring capabilities, enabling more efficient and accessible care delivery (41).
Furthermore, there is a growing recognition of the importance of a multidisciplinary approach to the management of PFD. Collaboration among healthcare professionals from various specialties, including urogynecology, physiotherapy, nursing, and mental health, can provide comprehensive and coordinated care that addresses the complex needs of women with pelvic floor disorders (42). Implementing multidisciplinary care pathways and fostering interprofessional education and communication are essential for optimizing patient outcomes and experiences (43).
In light of these evolving trends and the findings of our study, future research should focus on investigating the effectiveness of integrating postpartum nursing guidance with other innovative approaches, such as regenerative medicine, digital health technologies, and multidisciplinary care models. By leveraging the strengths of each approach and tailoring interventions to individual needs and preferences, we may be able to develop more effective, efficient, and patient-centered strategies for the prevention and management of PFD in women of advanced maternal age and beyond.
Moreover, there is a need for further research on the optimal timing, duration, and intensity of postpartum nursing guidance interventions. While our study demonstrated significant benefits with a 3-month intervention starting within 1 week after delivery, it would be valuable to explore the effects of earlier initiation, longer duration, or varying intensities of nursing support on PFD outcomes and patient satisfaction. Such research could inform the development of evidence-based guidelines and care pathways for the postpartum management of pelvic floor health.
In addition to clinical outcomes, future studies should also consider the cost-effectiveness and feasibility of implementing postpartum nursing guidance programs in various healthcare settings. Economic evaluations, process evaluations, and qualitative studies exploring the perspectives of healthcare providers, patients, and other stakeholders could provide valuable insights into the barriers, facilitators, and potential impact of scaling up this approach in real-world practice (33).
Ultimately, the goal of advancing research and practice in postpartum pelvic floor health is to improve the quality of life and well-being of women throughout their lifespan. By prioritizing patient-centered care, interprofessional collaboration, and evidence-based practice, we can work toward a future where all women have access to the support and resources they need to prevent, manage, and recover from pelvic floor disorders, enabling them to lead fulfilling and active lives.
The strengths of our study include the randomized controlled design, the comprehensive assessment of pelvic floor function using validated tools and the inclusion of a diverse sample of women of advanced maternal age.
Based on the findings, pelvic floor rehabilitation combined with postpartum nursing guidance is an effective treatment regimen for women of advanced maternal age with early PFD. It offers numerous benefits, such as significantly improving pelvic prolapse and urinary incontinence, facilitating the recovery of PFM strength and enhancing patient satisfaction with nursing care, thus warranting widespread adoption.
In conclusion, our study provides strong evidence for the effectiveness of integrating postpartum nursing guidance with pelvic floor rehabilitation for the management of early PFD in women of advanced maternal age. These findings contribute to the growing body of literature supporting the value of comprehensive, individualized, and multidisciplinary approaches to postpartum pelvic floor health. As we continue to advance research and practice in this field, it is essential to keep the diverse needs and experiences of postpartum women at the forefront, working collaboratively to develop innovative, evidence-based, and patient-centered solutions that promote optimal pelvic floor health across the lifespan.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving humans were approved by Liuzhou maternity and child healthcare hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
QH: Conceptualization, Investigation, Methodology, Resources, Validation, Writing – original draft, Writing – review & editing. JT: Funding acquisition, Investigation, Methodology, Project administration, Writing – original draft, Writing – review & editing. DZ: Investigation, Methodology, Project administration, Software, Supervision, Visualization, Writing – original draft, Writing – review & editing. YZ: Conceptualization, Formal analysis, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. TY: Conceptualization, Investigation, Methodology, Project administration, Visualization, Writing – original draft, Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by Guangxi Key R&D Program (Guike AB18126056), Liuzhou Science and Technology Key R&D Program (2018BJ10301), and Liuzhou Science and Technology Plan Project (2018DB20501).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Pang, H, Zhang, L, Han, S, Li, Z, Gong, J, Liu, Q, et al. A nationwide population-based survey on the prevalence and risk factors of symptomatic pelvic organ prolapse in adult women in China – a pelvic organ prolapse quantification system-based study. BJOG. (2021) 128:1313–23. doi: 10.1111/1471-0528.16675
2. Eickmeyer, SM . Anatomy and physiology of the pelvic floor. Phys Med Rehabil Clin N Am. (2017) 28:455–60. doi: 10.1016/j.pmr.2017.03.003
3. Quaghebeur, J, Petros, P, Wyndaele, JJ, and De Wachter, S. Pelvic-floor function, dysfunction, and treatment. Eur J Obstet Gynecol Reprod Biol. (2021) 265:143–9. doi: 10.1016/j.ejogrb.2021.08.026
4. Liu, Z . Clinical efficacy analysis of pelvic floor rehabilitation treatment at different times on postpartum pelvic floor dysfunction in primiparas with natural delivery[D]. J Chongqing Med Univ. (2022)
5. Delancey, JO, Kane Low, L, Miller, JM, Patel, DA, and Tumbarello, JA. Graphic integration of causal factors of pelvic floor disorders: an integrated life span model. Am J Obstet Gynecol. (2008) 199:610.e1–5. doi: 10.1016/j.ajog.2008.04.001
6. Romeikienė, KE, and Bartkevičienė, D. Pelvic-floor dysfunction prevention in Prepartum and postpartum periods. Medicina. (2021) 57:387. doi: 10.3390/medicina57040387
7. Zhou, J . Study on the effect of pelvic floor rehabilitation training for female patients with pelvic floor dysfunction. Contemp Med Symp. (2021) 19:182–3. doi: 10.3969/j.issn.2095-7629.2021.03.131
8. Li, X, Zhang, Y, Wu, Y, Lin, S, Zheng, W, and Lin, J. Study on the effect of second pregnancy on pelvic floor function in elderly women and the mechanism of biofeedback electrical stimulation to promote pelvic floor function rehabilitation. Chin Manipulat Rehabilit Med. (2019) 10:5–7.
9. Zhao, L . Clinical nursing effect of intermediate frequency pulse electrotherapy on 80 cases of postpartum pelvic floor rehabilitation. Shanxi Med J. (2019) 48:392–3. doi: 10.3969/j.issn.0253-9926.2019.03.052
10. Soave, I, Scarani, S, Mallozzi, M, Nobili, F, Marci, R, and Caserta, D. Pelvic floor muscle training for prevention and treatment of urinary incontinence during pregnancy and after childbirth and its effect on urinary system and supportive structures assessed by objective measurement techniques. Arch Gynecol Obstet. (2019) 299:609–23. doi: 10.1007/s00404-018-5036-6
11. Patel, DN, and Anger, JT. Surgery for pelvic organ prolapse. Curr Opin Urol. (2016) 26:302–8. doi: 10.1097/MOU.0000000000000288
12. Li, L, and Yan, L. Analysis of the influence of postpartum pelvic floor rehabilitation time on urinary incontinence and pelvic floor muscles. China Health Care Nutr. (2019) 29:350. doi: 10.3969/j.issn.1004-7484.2019.11.471
13. Mi, W, and Duan, X. Exploring the screening and nursing strategies for postpartum pelvic floor dysfunction in women. World Lat Med Infor. (2020) 20:361–2. doi: 10.3969/j.issn.1671-3141.2020.88.200
14. Ma, X . The effect of targeted nursing on postpartum patients with pelvic floor dysfunction treated by biofeedback electrical stimulation. Contemp Med Symp. (2019) 17:236–7.
15. Zhou, L, Feng, G, Hu, Y, and Liu, S. Effect of postpartum pelvic floor rehabilitation time on urinary incontinence and pelvic floor muscles. China Modern Doctor. (2020) 58:89–95.
16. Wang, Y, Li, H, Wang, J, Hao, Q, Tu, Y, Chen, Y, et al. A network meta-analysis protocol of conservative interventions for urinary incontinence in postpartum women. Medicine. (2020) 99:e21772. doi: 10.1097/MD.0000000000021772
17. Li, W, Hu, Q, Zhang, Z, Shen, F, and Xie, Z. Effect of different electrical stimulation protocols for pelvic floor rehabilitation of postpartum women with extremely weak muscle strength: randomized control trial. Medicine. (2020) 99:e19863. doi: 10.1097/MD.0000000000019863
18. Woodley, SJ, Lawrenson, P, Boyle, R, Cody, JD, Mørkved, S, Kernohan, A, et al. Pelvic floor muscle training for preventing and treating urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Syst Rev. (2020) 2021:CD007471. doi: 10.1002/14651858.CD007471.pub4
19. Yuan, P . Development of a questionnaire on the nursing needs of women's pelvic floor muscle exercise in puerperium and its current investigation[D] Yangtze University. Chinese Journal of Nursing (2022).
20. Wang, L, Shi, L, Ping, L, Li, L, and Li, H. Analysis of influencing factors of pelvic floor muscle functional exercise for puerperal women. Shanxi Med J. (2021) 50:1000–2. doi: 10.3969/j.issn.0253-9926.2021.06.046
21. Tian, C, Jiang, Y, Yang, F, Xu, Y, Lee, S, Zhao, H, et al. Analysis of the puerperae’s expectations and perceived status of puerperal health management services. Chin J Nurs. (2020) 55:1796–801. doi: 10.3761/j.issn.0254-1769.2020.12.007
22. van Bavel, J, Hukkelhoven, CWPM, de Vries, C, Papatsonis, DNM, de Vogel, J, Roovers, JWR, et al. The effectiveness of mediolateral episiotomy in preventing obstetric anal sphincter injuries during operative vaginal delivery: a ten-year analysis of a national registry. Int Urogynecol J. (2018) 29:407–13. doi: 10.1007/s00192-017-3422-4
23. Ali-Masri, H, Hassan, S, Fosse, E, Zimmo, KM, Zimmo, M, Ismail, KMK, et al. Impact of electronic and blended learning programs for manual perineal support on incidence of obstetric anal sphincter injuries: a prospective interventional study. BMC Med Educ. (2018) 18:258. doi: 10.1186/s12909-018-1363-3
24. Liu, D . Clinical efficacy evaluation of postpartum female pelvic floor function rehabilitation interventions. J China Med Univ. (2019). doi: 10.27652/d.cnki.gzyku.2019.000701
25. Shamliyan, TA, Kane, RL, Wyman, J, and Wilt, TJ. Systematic review: randomized, controlled trials of non-surgical treatments for urinary incontinence in women. Ann Intern Med. (2008) 148:459–73. doi: 10.7326/0003-4819-148-6-200803180-00211
26. Lee, HN, Lee, SY, Lee, YS, Han, JY, Choo, MS, and Lee, KS. Pelvic floor muscle training using an extracorporeal biofeedback device for female stress urinary incontinence. Int Urogynecol J. (2013) 24:831–8. doi: 10.1007/s00192-012-1943-4
27. DeLancey, JOL, Masteling, M, Pipitone, F, LaCross, J, Mastrovito, S, and Ashton-Miller, JA. Pelvic floor injury during vaginal birth is life-altering and preventable: what can we do about it? Am J Obstet Gynecol. (2024) 230:279–294.e2. doi: 10.1016/j.ajog.2023.11.1253
28. Liu, S, Ding, M, Yin, M, He, J, and Li, H. Effect of biofeedback+electrical stimulation on postpartum pelvic floor muscle function. Shenzhen J Integ Tradit Chin West Med. (2020) 30:102–3. doi: 10.16458/j.cnki.1007-0893.2020.13.051
29. Frawley, H, Shelly, B, Morin, M, Bernard, S, Bø, K, Digesu, GA, et al. An international continence society (ICS) report on the terminology for pelvic floor muscle assessment. Neurourol Urodyn. (2021) 40:1217–60. doi: 10.1002/nau.24658
30. Dietz, HP, and Shek, C. Levator avulsion and grading of pelvic floor muscle strength. Int Urogynecol J Pelvic Floor Dysfunct. (2008) 19:633–6. doi: 10.1007/s00192-007-0491-9
31. de Oliveira, CF, Rodrigues, AM, Arruda, RM, Ferreira Sartori, MG, Girão, MJ, and Castro, RA. Pelvic floor muscle training in female stress urinary incontinence: comparison between group training and individual treatment using PERFECT assessment scheme. Int Urogynecol J Pelvic Floor Dysfunct. (2009) 20:1455–62. doi: 10.1007/s00192-009-0971-1
32. Schiavi, MC, D'Oria, O, Faiano, P, Prata, G, di Pinto, A, Sciuga, V, et al. Vaginal native tissue repair for posterior compartment prolapse: long-term analysis of sexual function and quality of life in 151 patients. Female Pelvic Med Reconstr Surg. (2018) 24:419–23. doi: 10.1097/SPV.0000000000000463
33. Bernard, S, Evans, H, Hoy, NY, Suderman, K, Cameron, B, Sexsmith, J, et al. Control4Life: a randomized controlled trial protocol examining the feasibility and efficacy of a combined pelvic health rehabilitation and exercise fitness program for individuals undergoing prostatectomy. Contemp Clin Trials. (2024) 139:107482. doi: 10.1016/j.cct.2024.107482
34. Hay-Smith, J, Mørkved, S, Fairbrother, KA, and Herbison, GP. Pelvic floor muscle training for prevention and treatment of urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Syst Rev. (2008) 4:CD007471. doi: 10.1002/14651858.CD007471
35. Yin, P, and Wang, H. Evaluation of nursing effect of pelvic floor rehabilitation training on pelvic organ prolapse in postpartum pregnant women under ultrasound imaging with artificial intelligence algorithm. Comput Math Methods Med. (2022) 2022:1786994–13. doi: 10.1155/2022/1786994
36. Chiarelli, P, Murphy, B, and Cockburn, J. Acceptability of a urinary continence promotion programme to women in postpartum. BJOG. (2003) 110:188–96. doi: 10.1046/j.1471-0528.2003.02205.x
37. Johannessen, HH, Frøshaug, BE, Lysåker, PJG, Salvesen, KÅ, Lukasse, M, Mørkved, S, et al. Regular antenatal exercise including pelvic floor muscle training reduces urinary incontinence 3 months postpartum-follow up of a randomized controlled trial. Acta Obstet Gynecol Scand. (2021) 100:294–301. doi: 10.1111/aogs.14010
38. Li, X, Liu, L, He, J, Yan, J, and Wang, Y. Analysis of the effectiveness of the application of pelvic floor rehabilitation exercise and the factors influencing its self-efficacy in postoperative patients with cervical cancer. Front Oncol. (2023) 13:1118794. doi: 10.3389/fonc.2023.1118794
39. Gargett, CE, Gurung, S, Darzi, S, Werkmeister, JA, and Mukherjee, S. Tissue engineering approaches for treating pelvic organ prolapse using a novel source of stem/progenitor cells and new materials. Curr Opin Urol. (2019) 29:450–7. doi: 10.1097/MOU.0000000000000634
40. Agrawal, K, and Agrawal, N. Role of digital health in pelvic floor disorders. Curr Opin Obstet Gynecol. (2021) 33:416–8. doi: 10.1097/GCO.0000000000000741
41. Lamin, E, Parrillo, LM, Newman, DK, and Smith, AL. Pelvic floor muscle training: underutilization in the USA. Curr Urol Rep. (2016) 17:10. doi: 10.1007/s11934-015-0572-0
42. Arnouk, A, De, E, Rehfuss, A, Cappadocia, C, Dickson, S, and Lian, F. Physical, complementary, and alternative medicine in the treatment of pelvic floor disorders. Curr Urol Rep. (2017) 18:47. doi: 10.1007/s11934-017-0694-7
Keywords: advanced maternal age, postpartum nursing guidance, pelvic floor function, rehabilitation, pelvic floor rehabilitation
Citation: Huang Q, Tang J, Zeng D, Zhang Y and Ying T (2024) The effect of postpartum nursing guidance on early pelvic floor dysfunction recovery in women of advanced maternal age: a randomized controlled trial. Front. Med. 11:1397258. doi: 10.3389/fmed.2024.1397258
Received: 07 March 2024; Accepted: 18 June 2024;
Published: 31 July 2024.
Edited by:
Andrea Giannini, Umberto 1 Hospital, ItalyReviewed by:
Janis Miller, University of Michigan, United StatesCopyright © 2024 Huang, Tang, Zeng, Zhang and Ying. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dingyuan Zeng, ZGluZ3l1YW56ZW5nMzExNXpAMTYzLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.