- Klinik für Innere Medizin I, Universitätsklinik Tübingen, Tübingen, Germany
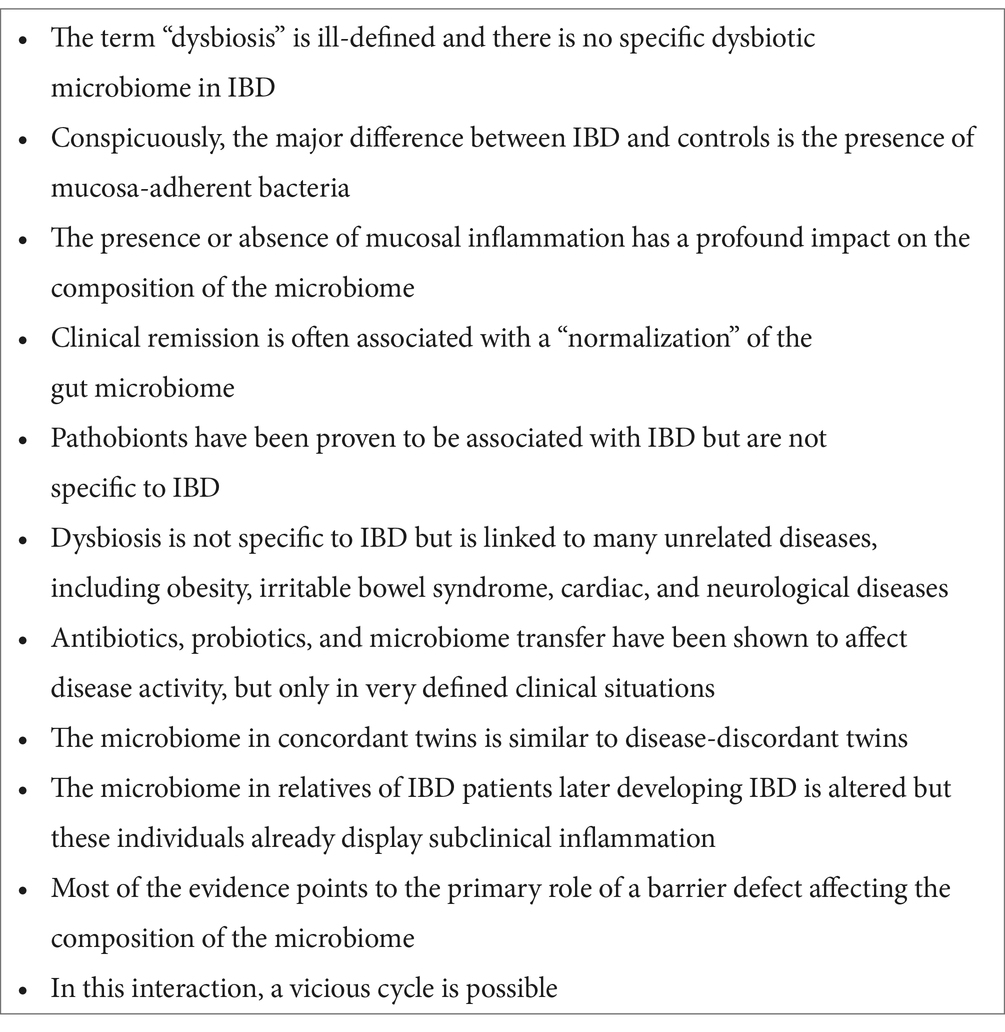
There is agreement that inflammatory bowel diseases are, both in terms of species composition and function, associated with an altered intestinal microbiome. This is usually described by the term “dysbiosis,” but this is a vague definition lacking quantitative precision. In this brief narrative review, the evidence concerning the primary or secondary role of this dysbiotic state is critically evaluated. Among others, the following facts argue against a primary etiological impact: 1) There is no specific dysbiotic microbiome in IBD, 2) the presence or absence of mucosal inflammation has a profound impact on the composition of the microbiome, 3) dysbiosis is not specific for IBD but linked to many unrelated diseases, 4) antibiotics, probiotics, and microbiome transfer have a very limited therapeutic effect, 5) the microbiome in concordant twins is similar to disease-discordant twins, and 6) the microbiome in relatives of IBD patients later developing IBD is altered, but these individuals already display subclinical inflammation.
1 Introduction
Dysbiosis is not only a prolific topic but also poorly defined; at least there is no quantitative definition. The term dysbiosis is generally described “as an alteration in the ecosystem associated to pathology” (1). Dysbiosis may manifest not only as reduced diversity but also as relative or absolute alterations in the microbial composition (increases or decreases), the proliferation of pathobionts, and shifts in the functional capacities of the microbiome. Since even one of these alterations may indicate “dysbiosis,” the concept implied by this term is quite diffuse. Efforts to define more quantitative dysbiotic enterotypes have yielded considerable overlap (2). There are many diverse pathologies associated with different forms of intestinal dysbiosis: diabetes, obesity, depression, multiple sclerosis, and cardiovascular disease, in addition to IBD (3).
The major human IBDs, Crohn’s disease and ulcerative colitis, are well-defined diseases exhibiting a chronic mucosal or transmural, sometimes even extraintestinal, inflammatory state related to the mere presence of the intestinal microbiome (4). The commensal microbes and pathobionts may adhere to and invade the mucosa, and, as a consequence, antimicrobial antibodies and T-cell reactivity against bacteria appear early in the disease course (5–7). Surgical diversion of the intestinal contents has long been known to alleviate distal inflammation, and a limited benefit of fecal microbiome transfer has also been shown, at least for ulcerative colitis. The evidence for Crohn’s disease is less convincing (8, 9). However, with a few exceptions, such as pouchitis, antibiotics generally are not effective in IBD (10).
Explaining this bacterial microinvasion and the consequent immune response, there is extensive evidence of a defective mucosal barrier in both diseases (11, 12). It is linked to both genetics (13) and the environment (14) and appears to trigger the inflammation. The standard suspicion of an “overshooting immune response” may simply reflect a perfectly adequate defense against this intrusion.
In IBD, this mutually aggressive host/microbe interaction dysbiosis has been suggested to play a primary role in leading to pathology (15, 16), answering the chicken and egg question in favor of dysbiosis acting as the chicken. The present narrative minireview, after critically screening the data, might convince the reader of the opposite, i.e., the altered microbiome may indeed be secondary (arguments listed in Table 1). The focus is on human IBD, less on experimental models that may or may not reflect these diseases. The relevant literature was screened using the keywords Crohn’s disease and ulcerative colitis in PubMed.
2 Mucosal microbes as a trigger for inflammation
In pioneering study, Swidsinski et al. (5) found high concentrations of bacteria in the intestinal mucosa of patients with IBD but not in controls. The concentrations of bacteria increased progressively with the severity of disease in the inflamed and non-inflamed colon, and some bacteria were also found intracellularly in the mucosa, i.e., had invaded. They concluded that this observation was not secondary to inflammation and that “the healthy mucosa is capable of holding back fecal bacteria” (5). This capacity was apparently defective in IBD. In later studies, they described a biofilm containing particularly bacteroides species, approximately 100-fold more than a similar biofilm in irritable bowel syndrome (IBS) (17). Such a biofilm in cases with IBS and IBD was later confirmed (18).
The relevance of the intestinal microbiome in the pathogenesis of IBD was introduced in a seminal study by Sartor et al. (4). They had originally based their argument for the key role of the microbiome on gnotobiotic experimental animals because most, if not all, animal models of IBD depended on the luminal microbiome for inducing chemically or genetically mediated mucosal inflammation. In a complementary development, it was shown that antibodies known to be associated with IBD, such as ANCA’s or anti-cBir, are not autoimmune in the strict sense but directed primarily against bacterial structures (19), although the full spectrum is much more complex (20). Actually, some truly autoimmune antibodies directed against human tissues may well be initially induced by bacterial antigens with cross-reactivity.
Accordingly, dendritic cells loaded with bacteria stimulate an IgA secretion that limits the penetration of bacteria into the mucosa in the normal state (21, 22). This antibody response is joined and supported by a T-cell activation (TH1/TH17), which is also triggered by and directed against bacterial epitopes (23, 24), mostly described as “exaggerated.” Alternatively, this “overactivation,” which obviously leads to a breakdown of mucosal tolerance to enteric bacteria, may well be secondary to an abnormally massive bacterial invasion due to a primary barrier defect.
3 Dysbiosis in IBD, with and without inflammation
In 2004, Ott et al. (25) described a reduction in diversity of the colonic mucosa-associated bacterial microflora in patients with active inflammatory bowel disease. This drop by 50% compared with controls was mostly due to a loss of normal anaerobic bacteria such as Bacteroides, Eubacterium, and Lactobacillus species. Since all patients exhibited active inflammation, there was no non-inflamed IBD control. Using a metagenomic approach, this reduced diversity was essentially confirmed in the fecal microbiota of Crohn’s disease patients with respect to firmicutes such as Clostridium leptum and the Bacteroides fragilis subgroup (26). However, using a quantitative rather than a relative approach, some differences between Crohn’s disease and controls were lost (2). Another interesting species in this context is Akkermansia, which appears to be protective despite its role in mucin degradation (27).
Since further studies were inconsistent, Gevers et al. (28) focused on the treatment-naïve microbiome in new-onset Crohn’s disease, and although the diversity tended to be lower in IBD, there was considerable overlap with controls. They found an axis defined by an increased abundance in bacteria which included Enterobacteriaceae, Pasteurellaceae, Veillonellaceae, and Fusobacteriaceae, and decreased abundance in Erysipelotrichales, Bacteroidales, and Clostridiales, correlating strongly with disease severity (28). They also noted that certain metabolic functions, including carbohydrate, energy, lipid, and amino acid metabolism, as well as glycan biosynthesis capacities, were diminished in the Crohn’s disease microbiome. This functional aspect was then extended in a study on the functional disturbances in relapsing refractory Crohn’s disease (29). The study clearly demonstrated that there were fundamental differences between patients with active vs. quiescent disease. This aspect had already been emphasized already in a study comparing inflamed and non-inflamed regions, which concluded that the overall dysbiosis observed in inflammatory bowel disease patients relative to non-IBD controls might to some extent be a result of the disturbed gut environment rather than the direct cause of disease (30). Furthermore, a recent study concluded that colonic microbiota is associated with inflammation in IBD, although a residual difference vs. controls remained even in its apparent absence (31).
It has become evident that there is a complex interplay between the gut microbiota and host genetics (32), nutrition (33), and even something as “banal” as stool consistency (34). While these details are beyond the scope of this discussion, it is interesting to note that IBD risk genes alter the microbiome, even in healthy individuals without IBD (32). Finally, upon achieving remission, for example, by anti-TNF treatment, the distance to the healthy centroid of the microbiome is minimized, whereas it remains abnormal in non-remitters (35). Similarly, in ulcerative colitis, the principal components of the microbiome normalize after achieving long-term, but not short-term remission (36). In a very recent study, it appeared that microbial normalization upon achieving remission was much more pronounced following anti-TNF treatment compared to vedolizumab and ustekinumab treatment (16). Some studies, including the latter, found an association between the pre-therapy microbiome and therapy response but a solid prediction using the bacterial composition data alone is still not available (16). When taken together, a large part of the alterations observed in the IBD microbiome appear to be reversible and secondary to inflammation. At any rate, the details of this multi-omics interaction in this ecosystem are still not fully understood (37).
4 Pathobionts in IBD
A microbiota of low diversity may favor the outgrowth of a “symbiont that is able to promote pathology only when specific genetic and environmental conditions are altered in the host.” This is the definition of a pathobiont (38), and the most common is E. coli LF83, which has adherent/invasive properties (39). It may indeed survive in macrophages and have strong proinflammatory effects. However, this pathobiont is not specific to Crohn’s disease: in ileal specimens, AIEC strains were found in 21.7% of CD chronic lesions vs. in 6.2% of controls. In neoterminal ileal specimens, AIEC strains were found in 36.4% of CD early lesions (p = 0.034 vs. controls) and 22.2% of the healthy mucosa of CD patients. In colonic specimens, AIEC strains were found in 3.7% of CD patients, 0% of UC patients, and 1.9% of controls (39).
A potential counterpart is Faecalibacterium prausnitzii (40), which has been shown to be an anti-inflammatory commensal diminished in Crohn’s disease and ulcerative colitis. The overrepresentation of AIECs and the low counts of faecalibacterium may contribute to the inflammatory state, but, lacking specificity, both are unlikely to be causal in the strict sense. With these two exceptions, it is also worth noting that there is a lot of incongruency in various studies in the field at the species level (1). Recently identified new pathobiont candidates comprise Clostridium innocuum, Atopobium parvulum, Ruminococcus gnavus, Bacteroides vulgatus, and some others, but their truly pathogenic role is unconfirmed (41).
5 Dysbiosis is not specific for IBD
Another aspect of questioning the role of dysbiosis in IBD is the simple fact that this microbial disturbance has been described in a multitude of unrelated diseases (3). A prominent instance is obesity, where the gut microbiome may alter the intestinal barrier, gut-associated lymphoid tissues, induce insulin resistance, and increase food intake through interference with gastrointestinal peptides related to satiety (42). Both major types of diabetes, type I as well as type II, are associated with dysbiosis (43), and even its microvascular complications appear to be associated with the intestinal microbiome (44). There are also data linking celiac disease and cardiovascular diseases to the intestinal microbiome (45). Another review lists necrotizing enterocolitis, colorectal cancer, and C. difficile-associated enterocolitis as potential consequences of dysbiosis (3). Even various diseases with neuropathology are characterized by a dysbiotic intestinal microbiome (46). It may be argued that all of these represent different types of dysbiosis associated with a “leaky gut,” but none is accompanied by the massive inflammation typical for IBD.
6 Antibiotics, probiotics, and microbiome transfer in IBD
Antibiotics have been described as “deep modulators of gut microbiota between good and evil” (47). This implies that these compounds may, depending on their specificities, be harmful but sometimes even beneficial to a healthy microbiome. Considering the negative role as a risk factor of early antibiotic administration for IBD, the evidence of epidemiology warns against their unlimited use (48). Actually, specific antibiotics may increase the risk of flares in IBD (49). Although some specific IBD situations may benefit from antibiotics, including the postoperative state following ileal resection or pouchitis, no antibiotic has unequivocally been demonstrated to treat standard IBD. Some probiotics, such as E. coli Nissle, have clinical effects (50), but only in specific situations, such as the maintenance of remission in ulcerative colitis. It may be argued, however, that no antibiotic and no probiotic have been demonstrated to reverse the dysbiosis.
Indeed, the somewhat “messy” alternative of microbiome transfer to enhance diversity in IBD may be an option. In accordance with this idea, the donor microbiota richness and the number of transferred phylotypes were associated with treatment success (51). Accordingly, multi-donor studies were superior to single-donor designs (8). As a limitation of this approach, in most randomized controlled trials, remission was observed in only approximately 30% of patients (but superior to controls) (52), and the benefit of fecal microbiome transfer in Crohn’s disease has not been consistently observed (9, 53). At any rate, this therapy has shown that in some patients, a change in the microbiome (often not permanent) may impact disease activity, but this is not proof of dysbiosis causing the disease.
7 Microbiome in twins and other relatives
Early studies in twins already suggested that there were subtle differences between discordant twins, for example, the healthy twins exhibited more Lachnospiraceae and Ruminococcaceae than twins who were both healthy (54). A more recent and more detailed study revealed that the gut microbiome composition of healthy cotwins from IBD-discordant twin pairs displayed IBD-like signatures both on a species and pathway level (55). No differences were detected in the gut microbiome composition (beta-diversity) between healthy cotwins and IBD-twins, but both gut microbiomes differed from healthy controls. Thus, healthy discordant IBD twins live permanently with an IBD-like microbiome and most of them will stay healthy.
Another interesting series of studies stems from a large Canadian cohort of 3,483 IBD-patient relatives, 73 of whom developed IBD during the course of these investigations (56). Using a machine learning approach, they developed a microbiome risk score, yielding a modest hazard ratio of 2.2. This score “predicted” the (later) development up to 5 years before Crohn’s disease onset. The five most important taxa contributing to the MRS included Ruminococcus torques, Blautia, Colidextribacter, an uncultured genus-level group from Oscillospiraceae, and Roseburia. They found fecal calprotectin levels to reduce the hazard ratio to 1.42 but it was still statistically significant (p = 0.041). Since they found evidence of a non-linear effect of fecal calprotectin on CD risk, it is conceded by the authors that a proportion of healthy FDRs may already have had subclinical gut inflammation at the time of recruitment. Indeed, in prior studies in this cohort with later IBD, an antimicrobial antibody response, increased intestinal permeability, proteomic markers of subclinical inflammation and an association of the microbiome changes with the gut barrier had been described (57–59). Thus, it seems possible that even years before disease onset, the local milieu was abnormal, causing microbiome changes and bacterial translocations that stimulated an antibody response. As the authors concluded, experimental studies will be needed to assess whether the associations presented in this study represent a cause or effect of CD pathogenesis. However, fecal microbiome transfer from IBD-patients to healthy controls is, of course, unethical and, when it happened once by accident with a donor later developing Crohn’s disease, there was no IBD induced in the recipients (60).
8 Barrier vs. dysbiosis in a vicious cycle?
As discussed above, there is considerable evidence that dysbiosis is a secondary “epiphenomenon” related to disease activity but not causally related to IBD etiology. Most likely, the primary defect in IBD governing both the potential of microbial intrusion and microbiome composition is mucosal antimicrobial peptide (AMP) secretion (61) and local mucus production (14). All gastrointestinal surfaces synthesize several AMPs, such as defensins, cathelicidin, Reg3γ, lysozyme, and many others. This occurs in specialized Paneth cells of the small intestine, absorptive epithelial cells of the colon, and metaplastic Paneth cells. Many commensals exhibit relative resistance, which may explain their survival in the gut lumen and outer mucus layer, but only a few bacteria survive in the inner mucus layer (62, 63). In the healthy situation the outer mucus layer hosts a distinct intestinal microbial niche, different and separate from the lumen (62, 64). As mentioned above, even the protective inner layer is highly contaminated in IBD (5) because the basic defect in these diseases is most likely a decreased secretion of these peptides in the ileum (12) or inadequate induction in the colon of Crohn’s disease (61). In ulcerative colitis, these AMPs are adequately induced, but the mucus layer is defective in retaining these peptides (14).
These peptides, among other factors, control not only the ability of microbes to invade but also the microbial composition in the gut lumen. This apparently applies to defensins such as HD5 (65), whereas others, such as Reg3g, rather suppress local invasion with little effect in the lumen (66). It is Reg3γ that promotes the spatial separation between the epithelium and the microbes. Paneth cell-derived lysozyme defines the composition of the mucolytic microbiota and the inflammatory tone of the intestine (67). Furthermore, in humans, intestinal antibacterial gene expression is linked to bacterial composition (68), and both mucosal antibacterial response profile and fecal microbiota composition are linked to the disease progression in ulcerative colitis (69).
Recently, it has become evident that many of these peptides are enzymatically modified (70) or proteolytically degraded into a multitude of peptide fragments, some of which maintain antibiotic activity (71). These peptide fragments display defined specificities against various species and contribute to overall defense. The secretion of multiple AMPs determines the local milieu for the luminal and mucosal microbiomes, as well as regulating the intestinal microbiome, allowing for mutually beneficial cohabitation under normal conditions. There is now ample evidence that this homeostasis is disturbed in IBD (11–14). It seems at least plausible that inflammation-associated microbiome changes provide feedback on mucosal protective factors while also negatively impacting microbial composition.
Microbiota, on the other hand, control the secretion of antibacterial peptides (72) and mucins (73). Mucus not only forms a semisolid layer physically inhibiting bacterial invasion but also, through electrophilic charge interaction, retains AMP’s to form a chemical defense line (14). Furthermore, the expression of defensins and mucins is coordinated (74). Therefore, the real scenario is a close interplay and also the interdependency of the host defense and the microbiome in the gut (14, 75).
This is most apparent if the impact of both genetics and diet on the microbiome is focused. This impact may be mediated by internal factors, including AMPs, which are regulated by both genetics, including bacterial regulators such as NOD2 and ATG16L1, an autophagy gene, and diet (12). Thus, a fat-rich “Western” diet affects both Paneth cell function and the microbiome (76), suggesting that a part of these diet effects is not simply mediated by the “nutrient.” The multiple other mediators regulating defensins, such as smoking, known to be deleterious in Crohn’s disease have been reviewed previously (12). The other major effectors directing the production of both defensins and mucins are microbe-derived short-chain fatty acids and propionate (14), again in concordance with the concept of a tight interplay between microbes and mucosal defense. However, this control of the microbiome in the intestinal contents is not restricted to these players of innate immunity but also others, including T-cells (77). These, however, are also responsible for mucosal damage in IBD.
9 Conclusion
In conclusion, “dysbiosis” may represent a response of the gut microbiome to primary (partly genetic) alterations in mucosal antibacterial and mucus defense, rather than initially triggering the disease. However, with regard to the data implying a role in modulating disease activity (including fecal transfer), it is highly possible that a vicious cycle between dysbiosis and barrier occurs during the inflammatory process: some selected species may directly degrade mucus (78). It seems plausible that the barrier is the chicken and dysbiosis the egg, but after hatching all chicken will interact. Accordingly, we remain skeptical that the direct microbial approach using certain species, probiotics, or fecal microbiome transplants will effectively and permanently treat, or even heal, these chronic debilitating diseases (79, 80). Finally, it should be emphasized that fungi (81) and intestinal virome (82) add further complexity to the field but remain to be investigated more extensively in the future.
Author contributions
EFS: Conceptualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Buttó, LF, Schaubeck, M, and Haller, D. Mechanisms of microbe-host interaction in Crohn's disease: Dysbiosis vs. Pathobiont selection. Front Immunol. (2015) 6:555. doi: 10.3389/fimmu.2015.00555
2. Vandeputte, D, Kathagen, G, D’hoe, K, Vieira-Silva, S, Valles-Colomer, M, Sabino, J, et al. Quantitative microbiome profiling links gut community variation to microbial load. Nature. (2017) 551:507–11. doi: 10.1038/nature24460
3. Weiss, GA, and Hennet, T. Mechanisms and consequences of intestinal dysbiosis. Cell Mol Life Sci. (2017) 74:2959–77. doi: 10.1007/s00018-017-2509-x
4. Sartor, RB, and Wu, GD. Roles for intestinal Bacteria, viruses, and Fungi in pathogenesis of inflammatory bowel diseases and therapeutic approaches. Gastroenterology. (2017) 152:327–339.e4. doi: 10.1053/j.gastro.2016.10.012
5. Swidsinski, A, Ladhoff, A, Pernthaler, A, and Swidsinski, S, Loening–Baucke V, Ortner, M, Weber, J, Hoffmann, U, Schreiber, S, Dietel, M, et al. Mucosal flora in inflammatory bowel disease. Gastroenterology (2002) 122:44–54. doi: 10.1053/gast.2002.30294
6. Alexander, KL, Targan, SR, and Elson, CO. Microbiota activation and regulation of innate and adaptive immunity. Immunol Rev. (2014) 260:206–20. doi: 10.1111/imr.12180
7. Chang, JT. Pathophysiology of inflammatory bowel diseases. N Engl J Med. (2020) 383:2652–64. doi: 10.1056/NEJMra2002697
8. Levast, B, Fontaine, M, Nancey, S, Dechelotte, P, Doré, J, and Lehert, P. Single-donor and pooling strategies for fecal microbiota transfer product preparation in ulcerative colitis: a systematic review and Meta-analysis. Clin Transl Gastroenterol. (2023) 14:e00568. doi: 10.14309/ctg.0000000000000568
9. Fehily, SR, Basnayake, C, Wright, EK, and Kamm, MA. Fecal microbiota transplantation therapy in Crohn’s disease: systematic review. J Gastro Hepatol. (2021) 36:2672–86. doi: 10.1111/jgh.15598
10. Jha, DK, Mishra, S, Dutta, U, and Sharma, V. Antibiotics for inflammatory bowel disease: current status. Indian J Gastroenterol. (2024) 43:145–59. doi: 10.1007/s12664-024-01537-x
11. Antoni, L. Intestinal barrier in inflammatory bowel disease. WJG. (2014) 20:1165–79. doi: 10.3748/wjg.v20.i5.1165
12. Wehkamp, J, and Stange, EF. An update review on the Paneth cell as key to Ileal Crohn’s disease. Front Immunol. (2020) 11:646. doi: 10.3389/fimmu.2020.00646
13. Schreiber, S, Rosenstiel, P, Albrecht, M, Hampe, J, and Krawczak, M. Genetics of Crohn disease, an archetypal inflammatory barrier disease. Nat Rev Genet. (2005) 6:376–88. doi: 10.1038/nrg1607
14. Stange, EF, and Schroeder, BO. Microbiota and mucosal defense in IBD: an update. Expert Rev Gastroenterol Hepatol. (2019) 13:963–76. doi: 10.1080/17474124.2019.1671822
15. Grellier, N, Sokol, H, and Seksik, P. Gut dysbiosis in Crohn’s disease: never so close to solving the chicken-and-egg enigma: commentary to “gut microbiome composition is associated with future onset of Crohn’s disease in healthy first-degree relatives, by Raygoza Garay JA et al., gastroenterology 2023.”. Clin Res Hepatol Gastroenterol. (2024) 48:102272. doi: 10.1016/j.clinre.2023.102272
16. Caenepeel, C, Falony, G, Machiels, K, Verstockt, B, Goncalves, PJ, Ferrante, M, et al. Dysbiosis and associated stool features improve prediction of response to biological therapy in inflammatory bowel disease. Gastroenterology. (2024) 166:483–95. doi: 10.1053/j.gastro.2023.11.304
17. Swidsinski, A, Weber, J, Loening-Baucke, V, Hale, LP, and Lochs, H. Spatial organization and composition of the mucosal Flora in patients with inflammatory bowel disease. J Clin Microbiol. (2005) 43:3380–9. doi: 10.1128/JCM.43.7.3380-3389.2005
18. Baumgartner, M, Lang, M, Holley, H, Crepaz, D, Hausmann, B, Pjevac, P, et al. Mucosal biofilms are an endoscopic feature of irritable bowel syndrome and ulcerative colitis. Gastroenterology. (2021) 161:1245–1256.e20. doi: 10.1053/j.gastro.2021.06.024
19. Landers, CJ, Cohavy, O, Misra, R, Yang, H, Lin, Y, Braun, J, et al. Selected loss of tolerance evidenced by Crohn’s disease–associated immune responses to auto-and microbial antigens. Gastroenterology. (2002) 123:689–99. doi: 10.1053/gast.2002.35379
20. Bourgonje, AR, Andreu-Sánchez, S, Vogl, T, Hu, S, Vich Vila, A, Gacesa, R, et al. Phage-display immunoprecipitation sequencing of the antibody epitope repertoire in inflammatory bowel disease reveals distinct antibody signatures. Immunity. (2023) 56:1393–1409.e6. doi: 10.1016/j.immuni.2023.04.017
21. Fagarasan, S, and Honjo, T. Intestinal IgA synthesis: regulation of front-line body defences. Nat Rev Immunol. (2003) 3:63–72. doi: 10.1038/nri982
22. Macpherson, AJ, and Harris, NL. Interactions between commensal intestinal bacteria and the immune system. Nat Rev Immunol. (2004) 4:478–85. doi: 10.1038/nri1373
23. Brand, S. Crohn’s disease: Th1, Th17 or both? The change of a paradigm: new immunological and genetic insights implicate Th17 cells in the pathogenesis of Crohn’s disease. Gut. (2009) 58:1152–67. doi: 10.1136/gut.2008.163667
24. Fonseca-Camarillo, G, and Yamamoto-Furusho, JK. Immunoregulatory pathways involved in inflammatory bowel disease. Inflamm Bowel Dis. (2015) 21:2188–93. doi: 10.1097/MIB.0000000000000477
25. Ott, SJ. Reduction in diversity of the colonic mucosa associated bacterial microflora in patients with active inflammatory bowel disease. Gut. (2004) 53:685–93. doi: 10.1136/gut.2003.025403
26. Manichanh, C. Reduced diversity of faecal microbiota in Crohn’s disease revealed by a metagenomic approach. Gut. (2006) 55:205–11. doi: 10.1136/gut.2005.073817
27. Zheng, M, Han, R, Yuan, Y, Xing, Y, Zhang, W, Sun, Z, et al. The role of Akkermansia muciniphila in inflammatory bowel disease: current knowledge and perspectives. Front Immunol. (2023) 13:1089600. doi: 10.3389/fimmu.2022.1089600
28. Gevers, D, Kugathasan, S, Denson, LA, Vázquez-Baeza, Y, Van Treuren, W, Ren, B, et al. The treatment-naive microbiome in new-onset Crohn’s disease. Cell Host Microbe. (2014) 15:382–92. doi: 10.1016/j.chom.2014.02.005
29. Cohort, SIBD, Investigators, YB, Juillerat, P, Øyås, O, Ramon, C, Bravo, FD, et al. Microbial network disturbances in relapsing refractory Crohn’s disease. Nat Med. (2019) 25:323–36. doi: 10.1038/s41591-018-0308-z
30. Walker, AW, Sanderson, JD, Churcher, C, Parkes, GC, Hudspith, BN, Rayment, N, et al. High-throughput clone library analysis of the mucosa-associated microbiota reveals dysbiosis and differences between inflamed and non-inflamed regions of the intestine in inflammatory bowel disease. BMC Microbiol. (2011) 11:7. doi: 10.1186/1471-2180-11-7
31. Ryan, FJ, Ahern, AM, Fitzgerald, RS, Laserna-Mendieta, EJ, Power, EM, Clooney, AG, et al. Colonic microbiota is associated with inflammation and host epigenomic alterations in inflammatory bowel disease. Nat Commun. (2020) 11:1512. doi: 10.1038/s41467-020-15342-5
32. Imhann, F, Vich Vila, A, Bonder, MJ, Fu, J, Gevers, D, Visschedijk, MC, et al. Interplay of host genetics and gut microbiota underlying the onset and clinical presentation of inflammatory bowel disease. Gut. (2018) 67:108–19. doi: 10.1136/gutjnl-2016-312135
33. Metwaly, A, Jovic, J, Waldschmitt, N, Khaloian, S, Heimes, H, Häcker, D, et al. Diet prevents the expansion of segmented filamentous bacteria and ileo-colonic inflammation in a model of Crohn’s disease. Microbiome. (2023) 11:66. doi: 10.1186/s40168-023-01508-y
34. Vandeputte, D, Falony, G, Vieira-Silva, S, Tito, RY, Joossens, M, and Raes, J. Stool consistency is strongly associated with gut microbiota richness and composition, enterotypes and bacterial growth rates. Gut. (2016) 65:57–62. doi: 10.1136/gutjnl-2015-309618
35. Lewis, JD, Chen, EZ, Baldassano, RN, Otley, AR, Griffiths, AM, Lee, D, et al. Inflammation, antibiotics, and diet as environmental stressors of the gut microbiome in pediatric Crohn’s disease. Cell Host Microbe. (2017) 22:247. doi: 10.1016/j.chom.2017.07.011
36. Herrera-deGuise, C, Varela, E, Sarrabayrouse, G, Pozuelo Del Río, M, Alonso, VR, Sainz, NB, et al. Gut microbiota composition in long-remission ulcerative colitis is close to a healthy gut microbiota. Inflamm Bowel Dis. (2023) 29:1362–9. doi: 10.1093/ibd/izad058
37. Investigators, IBDMDB, Lloyd-Price, J, Arze, C, Ananthakrishnan, AN, Schirmer, M, Avila-Pacheco, J, et al. Multi-omics of the gut microbial ecosystem in inflammatory bowel diseases. Nature. (2019) 569:655–62. doi: 10.1038/s41586-019-1237-9
38. Chow, J, and Mazmanian, SK. A Pathobiont of the microbiota balances host colonization and intestinal inflammation. Cell Host Microbe. (2010) 7:265–76. doi: 10.1016/j.chom.2010.03.004
39. Darfeuille-Michaud, A, Boudeau, J, Bulois, P, Neut, C, Glasser, A-L, Barnich, N, et al. High prevalence of adherent-invasive Escherichia coli associated with ileal mucosa in Crohn’s disease. Gastroenterology. (2004) 127:412–21. doi: 10.1053/j.gastro.2004.04.061
40. Sokol, H, Pigneur, B, Watterlot, L, Lakhdari, O, Bermudez-Humaran, LG, Gratadoux, J-J, et al. Faecalibacterium prausnitzii is an anti-inflammatory commensal bacterium identified by gut microbiota analysis of Crohn disease patients. Proc Natl Acad Sci. (2008) 105:16731–6. doi: 10.1073/pnas.0804812105
41. Gilliland, A, Chan, JJ, De Wolfe, TJ, Yang, H, and Vallance, BA. Pathobionts in inflammatory bowel disease: origins, underlying mechanisms, and implications for clinical care. Gastroenterology. (2024) 166:44–58. doi: 10.1053/j.gastro.2023.09.019
42. Gomes, AC, Hoffmann, C, and Mota, JF. The human gut microbiota: metabolism and perspective in obesity. Gut Microbes. (2018) 9:1–18. doi: 10.1080/19490976.2018.1465157
43. Lau, WL, Tran, T, Rhee, CM, Kalantar-Zadeh, K, and Vaziri, ND. Diabetes and the gut microbiome. Semin Nephrol. (2021) 41:104–13. doi: 10.1016/j.semnephrol.2021.03.005
44. Hasani, M, Asadi Pilerud, Z, Kami, A, Abbas Vaezi, A, Sobhani, S, Ejtahed, H-S, et al. Association between gut microbiota compositions with MicrovascularComplications in individuals with diabetes: a systematic review. CDR. (2024) 20. doi: 10.2174/0115733998280396231212114345
45. Losurdo, G, Principi, M, Iannone, A, Ierardi, E, and Di Leo, A. The interaction between celiac disease and intestinal microbiota. J Clin Gastroenterol. (2016) 50:S145–7. doi: 10.1097/MCG.0000000000000682
46. Gubert, C, Gasparotto, J, and Morais, L. Convergent pathways of the gut microbiota–brain axis and neurodegenerative disorders. Gastroenterol Rep. (2022) 10:goac017. doi: 10.1093/gastro/goac017
47. Ianiro, G, Tilg, H, and Gasbarrini, A. Antibiotics as deep modulators of gut microbiota: between good and evil. Gut. (2016) 65:1906–15. doi: 10.1136/gutjnl-2016-312297
48. Narula, N, Wong, ECL, Pray, C, Marshall, JK, Rangarajan, S, Islam, S, et al. Associations of antibiotics, hormonal therapies, Oral contraceptives, and long-term NSAIDS with inflammatory bowel disease: results from the prospective urban rural epidemiology (PURE) study. Clin Gastroenterol Hepatol. (2023) 21:2649–2659.e16. doi: 10.1016/j.cgh.2022.11.037
49. Lo, B, Biederman, L, Rogler, G, Dora, B, Kreienbühl, A, Vind, I, et al. Specific antibiotics increases the risk of flare-ups in patients with inflammatory bowel disease – results from a Danish nationwide population-based nested case-control study. J Crohn's Colitis. (2024) 17:jjae027. doi: 10.1093/ecco-jcc/jjae027
50. Losurdo, G, Iannone, A, Contaldo, A, Ierardi, E, Di Leo, A, and Principi, M. Escherichia coli Nissle 1917 in ulcerative colitis treatment: systematic review and Meta-analysis. JGLD. (2015) 24:499–505. doi: 10.15403/jgld.2014.1121.244.ecn
51. Vermeire, S, Joossens, M, Verbeke, K, Wang, J, Machiels, K, Sabino, J, et al. Donor species richness determines Faecal microbiota transplantation success in inflammatory bowel disease. ECCOJC. (2016) 10:387–94. doi: 10.1093/ecco-jcc/jjv203
52. El Hage, CN, Ghoneim, S, Shah, S, Chahine, A, Mourad, FH, Francis, FF, et al. Efficacy of fecal microbiota transplantation in the treatment of active ulcerative colitis: a systematic review and Meta-analysis of double-blind randomized controlled trials. Inflamm Bowel Dis. (2023) 29:808–17. doi: 10.1093/ibd/izac135
53. Network, S-AIBD, Sokol, H, Landman, C, Seksik, P, Berard, L, Montil, M, et al. Fecal microbiota transplantation to maintain remission in Crohn’s disease: a pilot randomized controlled study. Microbiome. (2020) 8:12. doi: 10.1186/s40168-020-0792-5
54. Lepage, P, Häsler, R, Spehlmann, ME, Rehman, A, Zvirbliene, A, Begun, A, et al. Twin study indicates loss of interaction between microbiota and mucosa of patients with ulcerative colitis. Gastroenterology. (2011) 141:227–36. doi: 10.1053/j.gastro.2011.04.011
55. Brand, EC, Klaassen, MAY, Gacesa, R, Vich Vila, A, Ghosh, H, De Zoete, MR, et al. Healthy Cotwins share gut microbiome signatures with their inflammatory bowel disease twins and unrelated patients. Gastroenterology. (2021) 160:1970–85. doi: 10.1053/j.gastro.2021.01.030
56. Raygoza Garay, JA, Turpin, W, Lee, S-H, Smith, MI, Goethel, A, Griffiths, AM, et al. Gut microbiome composition is associated with future onset of Crohn’s disease in healthy first-degree relatives. Gastroenterology. (2023) 165:670–81. doi: 10.1053/j.gastro.2023.05.032
57. Lee, S-H, Turpin, W, Espin-Garcia, O, Raygoza Garay, JA, Smith, MI, Leibovitzh, H, et al. Anti-microbial antibody response is associated with future onset of Crohn’s disease independent of biomarkers of altered gut barrier function, subclinical inflammation, and genetic risk. Gastroenterology. (2021) 161:1540–51. doi: 10.1053/j.gastro.2021.07.009
58. Turpin, W, Lee, S-H, Raygoza Garay, JA, Madsen, KL, Meddings, JB, Bedrani, L, et al. Increased intestinal permeability is associated with later development of Crohn’s disease. Gastroenterology. (2020) 159:2092–2100.e5. doi: 10.1053/j.gastro.2020.08.005
59. Leibovitzh, H, Lee, S-H, Xue, M, Raygoza Garay, JA, Hernandez-Rocha, C, Madsen, KL, et al. Altered gut microbiome composition and function are associated with gut barrier dysfunction in healthy relatives of patients with Crohn’s disease. Gastroenterology. (2022) 163:1364–1376.e10. doi: 10.1053/j.gastro.2022.07.004
60. Fischer, M, Bittar, M, Papa, E, Kassam, Z, and Smith, M. Can you cause inflammatory bowel disease with fecal transplantation? A 31-patient case-series of fecal transplantation using stool from a donor who later developed Crohn’s disease. Gut Microbes. (2017) 8:205–7. doi: 10.1080/19490976.2017.1283469
61. Ostaff, MJ, Stange, EF, and Wehkamp, J. Antimicrobial peptides and gut microbiota in homeostasis and pathology: homeostasis in the gut. EMBO Mol Med. (2013) 5:1465–83. doi: 10.1002/emmm.201201773
62. Johansson, MEV, Larsson, JMH, and Hansson, GC. The two mucus layers of colon are organized by the MUC2 mucin, whereas the outer layer is a legislator of host–microbial interactions. Proc Natl Acad Sci USA. (2011) 108:4659–65. doi: 10.1073/pnas.1006451107
63. Chassaing, B, and Gewirtz, AT. Identification of inner mucus-associated Bacteria by laser capture microdissection. Cell Mol Gastroenterol Hepatol. (2019) 7:157–60. doi: 10.1016/j.jcmgh.2018.09.009
64. Li, H, Limenitakis, JP, Fuhrer, T, Geuking, MB, Lawson, MA, Wyss, M, et al. The outer mucus layer hosts a distinct intestinal microbial niche. Nat Commun. (2015) 6:8292. doi: 10.1038/ncomms9292
65. Salzman, NH, Hung, K, Haribhai, D, Chu, H, Karlsson-Sjöberg, J, Amir, E, et al. Enteric defensins are essential regulators of intestinal microbial ecology. Nat Immunol. (2010) 11:76–82. doi: 10.1038/ni.1825
66. Vaishnava, S, Yamamoto, M, Severson, KM, Ruhn, KA, Yu, X, Koren, O, et al. The antibacterial lectin RegIIIγ promotes the spatial segregation of microbiota and host in the intestine. Science. (2011) 334:255–8. doi: 10.1126/science.1209791
67. Yu, S, Balasubramanian, I, Laubitz, D, Tong, K, Bandyopadhyay, S, Lin, X, et al. Paneth cell-derived lysozyme defines the composition of mucolytic microbiota and the inflammatory tone of the intestine. Immunity. (2020) 53:398–416.e8. doi: 10.1016/j.immuni.2020.07.010
68. Bennet, SMP, Sundin, J, Magnusson, MK, Strid, H, Tap, J, Derrien, M, et al. Altered intestinal antibacterial gene expression response profile in irritable bowel syndrome is linked to bacterial composition and immune activation. Neurogastroenterol Motil. (2018) 30:e13468. doi: 10.1111/nmo.13468
69. Magnusson, MK, Strid, H, Isaksson, S, Simrén, M, and Öhman, L. The mucosal antibacterial response profile and fecal microbiota composition are linked to the disease course in patients with newly diagnosed ulcerative colitis. Inflamm Bowel Dis. (2017) 23:956–66. doi: 10.1097/MIB.0000000000001130
70. Schroeder, BO, Wu, Z, Nuding, S, Groscurth, S, Marcinowski, M, Beisner, J, et al. Reduction of disulphide bonds unmasks potent antimicrobial activity of human β-defensin 1. Nature. (2011) 469:419–23. doi: 10.1038/nature09674
71. Wendler, J, Schroeder, BO, Ehmann, D, Koeninger, L, Mailänder-Sánchez, D, Lemberg, C, et al. Proteolytic degradation of reduced human Beta Defensin 1 generates a novel antibiotic Octapeptide. Sci Rep. (2019) 9:3640. doi: 10.1038/s41598-019-40216-2
72. Campbell, Y, Fantacone, ML, and Gombart, AF. Regulation of antimicrobial peptide gene expression by nutrients and by-products of microbial metabolism. Eur J Nutr. (2012) 51:899–907. doi: 10.1007/s00394-012-0415-4
73. Breugelmans, T, Oosterlinck, B, Arras, W, Ceuleers, H, De Man, J, Hold, GL, et al. The role of mucins in gastrointestinal barrier function during health and disease. Lancet Gastroenterol Hepatol. (2022) 7:455–71. doi: 10.1016/S2468-1253(21)00431-3
74. Cobo, ER, Kissoon-Singh, V, Moreau, F, and Chadee, K. Colonic MUC2 mucin regulates the expression and antimicrobial activity of β-defensin 2. Mucosal Immunol. (2015) 8:1360–72. doi: 10.1038/mi.2015.27
75. Vaishnava, S, Behrendt, CL, Ismail, AS, Eckmann, L, and Hooper, LV. Paneth cells directly sense gut commensals and maintain homeostasis at the intestinal host-microbial interface. Proc Natl Acad Sci. (2008) 105:20858–63. doi: 10.1073/pnas.0808723105
76. Liu, T-C, Kern, JT, Jain, U, Sonnek, NM, Xiong, S, Simpson, KF, et al. Western diet induces Paneth cell defects through microbiome alterations and farnesoid X receptor and type I interferon activation. Cell Host Microbe. (2021) 29:988–1001.e6. doi: 10.1016/j.chom.2021.04.004
77. Hooper, LV, Littman, DR, and Macpherson, AJ. Interactions between the microbiota and the immune system. Science. (2012) 336:1268–73. doi: 10.1126/science.1223490
78. Desai, MS, Seekatz, AM, Koropatkin, NM, Kamada, N, Hickey, CA, Wolter, M, et al. A dietary Fiber-deprived gut microbiota degrades the colonic mucus barrier and enhances pathogen susceptibility. Cell. (2016) 167:1339–1353.e21. doi: 10.1016/j.cell.2016.10.043
79. Zhao, H, Zhang, W, Cheng, D, You, L, Huang, Y, and Lu, Y. Investigating dysbiosis and microbial treatment strategies in inflammatory bowel disease based on two modified Koch’s postulates. Front Med. (2022) 9:1023896. doi: 10.3389/fmed.2022.1023896
80. Oka, A, and Sartor, RB. Microbial-based and microbial-targeted therapies for inflammatory bowel diseases. Dig Dis Sci. (2020) 65:757–88. doi: 10.1007/s10620-020-06090-z
81. Gravina, AG, Pellegrino, R, Auletta, S, Palladino, G, Brandimarte, G, Onofrio, R, et al. Hericium erinaceus, a medicinal fungus with a centuries-old history: evidence in gastrointestinal diseases. World J Gastroenterol. (2023) 29:3048–65. doi: 10.3748/wjg.v29.i20.3048
Keywords: Crohn’s disease, ulcerative colitis, microbiome, dysbiosis, intestinal barrier
Citation: Stange EF (2024) Dysbiosis in inflammatory bowel diseases: egg, not chicken. Front. Med. 11:1395861. doi: 10.3389/fmed.2024.1395861
Edited by:
Abbas Yadegar, Shahid Beheshti University of Medical Sciences, IranReviewed by:
Raffaele Pellegrino, University of Campania Luigi Vanvitelli, ItalyMaria Manuela Rosado, Hospital Physiotherapy Institutes (IRCCS), Italy
Copyright © 2024 Stange. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eduard F. Stange, ZWR1YXJkLnN0YW5nZUBpY2xvdWQuY29t
 Eduard F. Stange
Eduard F. Stange