- 1Department of Pain Medicine, Helios University Hospital Wuppertal, Wiuppertal, Germany
- 2Chair of Anasthaesia, School of Medicine, Faculty of Health, University of Witten/Herdecke, Witten, Germany
- 3Leipzig Heart Center, Leipzig, Germany
- 4Real World Evidence and Health Technology Assessment at Helios Health Institute, Berlin, Germany
- 5Center for Clinical Trials, Faculty of Health, Witten/Herdecke University, Witten, Germany
- 6Department of Clinical Pharmacology, School of Medicine, Faculty of Health, Witten/Herdecke University, Witten, Germany
- 7Philipp Klee-Institute for Clinical Pharmacology, Helios University Hospital Wuppertal, Wuppertal, Germany
Objectives: The COVID-19 pandemic affected patients’ access to health services, including patients with severe chronic pain. Since limited data on pandemic-caused changes in pain therapy is available, we analyzed its effect on hospital-based pain treatment.
Methods: For this retrospective claims data analysis conducted in n = 37 hospitals, we included patients treated for a chronic pain-related diagnosis. Discharge rates stratified by region and pain unit size were analyzed for different time periods between January 2019 and June 2022.
Results: There was a significant decrease in day-care, inpatient interdisciplinary multimodal pain management, from a total of 5,533 hospital pre-pandemic treatments in 2019, to 3,942 in 2020 and 4,262 in 2021, with a slight increase in the first half of 2022. The extent of COVID-19-related changes differed depending on region and pain unit size.
Conclusion: The decreased number of hospital pain treatments during the pandemic implies a relevant analgesic undertreatment. During future pandemics, the ethical dimension of potentially non-sufficient pain treatment should be weighted against social, medical and hygienic restrictions influencing the hospitalization rate.
Introduction
The COVID-19 pandemic led to worldwide restrictions on citizens’ freedom and changed access to health services, affecting not only acute medicine but also the care of chronically ill individuals, including those suffering from chronic pain, which affects patients worldwide (1). Chronic non-tumor related pain has a high prevalence in several countries, including Germany (2–9). The influence of the COVID-19 pandemic on the health care of patients with documented chronic pain during the pandemic has been described in several countries patients around the world (1). An impact on the different determinants of health could affect pain patients more (6, 10). The COVID-19 pandemic had an impact on mental health of people with pre-existing psychiatric disorders, but also led to mental distress in others (11–14). The social distance had an impact on mental stability, well-being, and health, and thus had medical consequences (15). COVID-19 associated challenges arose in several medical care settings, were sometimes unexpected but had also an impact on pain treatment. For example, the availability of several drug classes like antidepressants or opiates was limited by supply shortages (16). In addition, different regional and federal state policies during different pandemic phases had also an impact on the care for pain patients (17, 18).
Since its introduction into medicine, the bio-psycho-social model of a disease (19, 20) has become important and established in clinical practice (21). For patients with chronic pain the bio-psycho-social model of illness is used as the basis for care, and it has an impact on the design of inpatient interdisciplinary multimodal pain therapy (IMMST). A multimodal pain therapy that includes psychological and social factors is more effective than a purely medical treatment approach, but requires accompanying critical consideration with regard to individuality (22, 23). Interdisciplinary interprofessional pain conferences are an important indispensable component of multimodal pain management in hospitals (24, 25). For several patient groups, e.g., patients with back pain, benefits were clearly shown (24). Patients eligible for IMMST are those with chronic pain whose quality of life and/or ability to work is limited despite outpatient pain therapies, and who have additional illnesses that need to be taken into account for treatment or who have misused analgesic drugs. IMMST plays an important role in the care. Of interest are the potential changes in inpatient pain management care during the pandemic progresses. Pandemic-related treatment interruptions in pain management with effects on pain control, quality of life, and course have been reported (26). All parts of the bio-psycho-social model of chronic pain have been affected.
Chronic pain is a chronic condition and requires both outpatient care and the possibility of inpatient treatment. Because the pandemic changed key factors in outpatient care, and because pain patients, often with co-occurring mental health conditions, were more severely affected by the overall situation, it is likely that more inpatient care was needed during this period. However, this presumed need coincides with an overall situation of reduced in-patient treatment capacity. Although there was a greater need for in-patient treatment, the treatment options were severely limited in terms of treating patients with severe pain sufficiently. In addition, there was a general feeling of insecurity among the population at various stages, which was also associated with a reluctance to visit health care facilities. To summarize the overall impact of these conflicting trends and taking into account scare data for COVID-19 associated changes in treatment of patients with severe chronic pain, we aim to analyze the effect of COVID-19 pandemic on hospital-based pain treatment in our study.
Methods
Data source
Claims data from n = 37 hospitals of the largest private German hospital group (i.e., Helios) fulfilling the inclusion criteria defined below were used for this retrospective analysis.
Definition of patients
Inclusion criteria
Patients were included, if they were discharged from hospital between 2019-01-01 and 2022-06-30 following an in-patient or day care patient (admission due to one of the following diagnosis-related group (DRG) codes):
– B47A: Multimodal pain therapy for diseases and disorders of the nervous system at least 14 treatment days
– B47B: Multimodal pain therapy for diseases and disorders of the nervous system less than 14 treatment days
– I42A: Multimodal pain therapy for diseases and disorders of musculoskeletal system and connective tissues at least 14 treatment days
– I42B: Multimodal pain therapy for musculoskeletal and connective tissue diseases and disorders less than 14 treatment days
– U42A: Multimodal pain therapy for mental diseases and disorders, age under 19 years
– U42B: Multimodal pain therapy for mental diseases and disorders at least 14 treatment days, age over 18 years
– U42C: Multimodal pain therapy for mental diseases and disorders less than 14 treatment days, age over 18 years.
Since these codes take into account not only the chronic pain but also the main cause, there are three codes, one each for the musculoskeletal system, the nervous system, and psychological and somatoform disorders. Minimum lengths of hospital stay of at least 14 treatment days or under 14 treatment days are coded separately, and the codes are doubled to 6, allowing the number of IMMST treatments over time to be shown using the DRG coding. By comparing the number of different IMMST DRGs before and during the pandemic, changes in care can be determined. To obtain a more precise representation, the Helios data set was analyzed, revealing changes in care in different federal states but also showing that care was provided at all times in the Helios hospitals, albeit at a reduced level, especially during lockdowns, at the beginning of the pandemic, and under the incentive of freehold flat rates.
Exclusion criteria
Cases with several DRG codes (4 cases in total) due to case merging by hospital controlling were removed to avoid double counting patients/cases. For this study, no further exclusion criteria (e.g., patients’ age) were applied.
Comparisons
Patient characteristics considered in our analysis were age, age group, gender, Elixhauser weighted score (AHRQ algorithm was applied (27, 28)) and corresponding comorbidities. Uncomplicated and complicated diabetes were lumped into one single category, as were uncomplicated and complicated hypertension.
Comparisons of discharged patients, discharged cases (hospital stays), and discharge rates were made for different time periods according to the following definitions:
Annual comparison: Discharge rates were analyzed for the years 2019, 2020, 2021, and 2022. For 2022, only the first six months (January to June) were included due to limited data availability.
Quarterly comparisons: Quarterly discharge rates in 2020, 2021 and 2022 were compared to the respective quarter in 2019 to minimize annual effects. As the first quarter of 2020 overlap both periods (prepandemic and pandemic), results for this comparison (Q1 2020 vs. Q1 2019) should be treated with caution.
Prepandemic vs. pandemic: Prepandemic period is the time interval between 2019-01-01 and the week including 2020-02-28 whereas the pandemic period is the time interval between the week starting after 2020-02-28 and 2022-06-30. We have defined the beginning of the pandemic period according to the date when the first patients with COVID-19 were detected in two large German federal states (i.e., Baden-Wuerttemberg, North Rhine-Westphalia) on the 26th of February 2020.1 The end date of the pandemic period was defined taking into account the distinct decrease of COVID-19 cases and associated healthcare utilization in the second quarter of 2022 (29).
Stratification
Analyses were startified for regions (federal states of Germany) and pain units size. Pain unit size were defined as follows, (i) ‘high volume’: units with at least 300 cases in 2019 and (ii) ‘low volume’ with less than 300 cases according to the aforementioned DRG definitions.
Assessment of comorbidities
For assessing the comorbidities of patients, the AHRQ Elixhauser Comorbidity Index was used (28). For this index, comorbidites were defined via patients’ ICD codes and entered the index with different weights. The index was evaluated with respect to in-hospital mortality and readmissions.
Statistical analysis
For the analysis of patient characteristics, categorical variables were analyzed using χ2 test, and two-sample t-test was used for analyzing continuous variables.
For the comparison of the discharge rate between different cohorts, a Poisson GLMMs with log-link function and the hospitals and a random intercept (30) was used. Hospitals entered the analyses as random factor. We analyzed weekly numbers for linear trends over time with Poisson regression. Discharge rates are reported as mean weekly discharge (SD), incidence rate ratios (IRR) together with 95% confidence intervals and p values. For weekly data, IRRs indicate average weekly changes. Stratified analyses were conducted for DRG and hospital regions. For all tests we applied a two-tailed 5% error criterion for significance. All the analyses are patient-based analyses (and not case-based). In case of multiple admissions for a patient (which appears to be rather rare), only the first case was included in our analysis.
Inferential statistics were performed in the R environment for statistical computing (version 4.0.2), 64-bit build (31) Effects of mixed models were estimated with the lme4 package (version 1.1–26) (30, 32).
Results
Patient characteristics
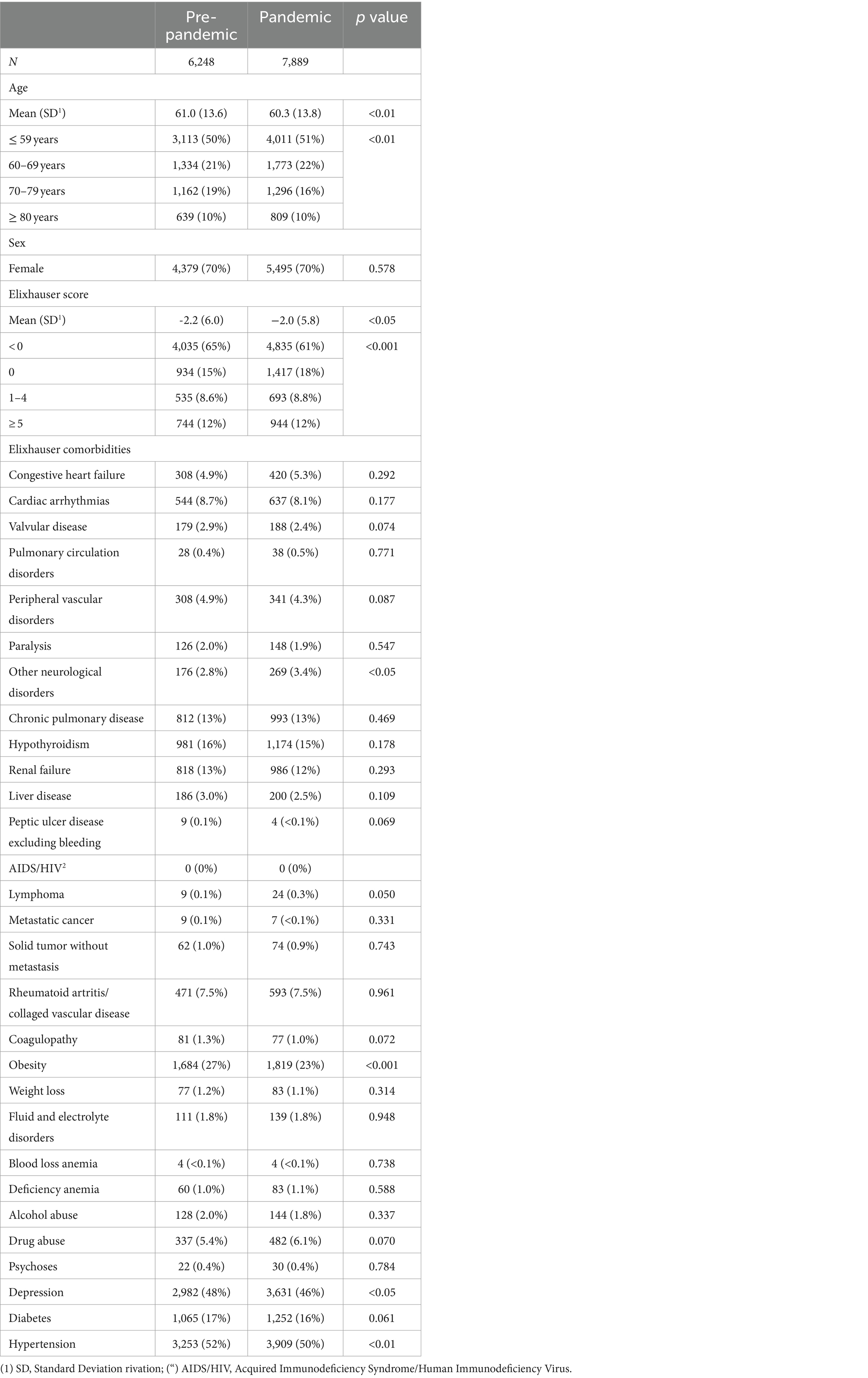
Comparing the characteristics of patients discharged during the observed pandemic versus pre-pandemic period, only minor differences were found (Table 1). During the pandemic period, patients were slightly younger (mean age: 60.3 ± 13.8 yrs. vs. 61.0 ± 13.6 yrs., p < 0.01) and had a slightly higher mean Elixhauser score (−2.0 ± 5.8 vs. −2.2 ± 6.0, p < 0.05). With regard to comorbidities used for defining the Elixhauser score, a slightly increased proportion was found during the pandemic period for patients suffering from ‘other neurological disorders’ (3.4% vs. 2.8%, p < 0.05) whereas a decreased proportion of patients had a documented diagnosis of obesity (23% vs. 27%, p < 0.001), depression (46% vs. 48%, p < 0.05), and hypertension (50% vs. 52%, p < 0.01).
Starting from a total of 5,533 cases in 2019, the COVID-19 pandemic reduced the number of cases to 3,942 in 2020 and to 4,262 in 2021. Hence, in 2020 the most significant decrease was recorded in day-care, inpatient interdisciplinary multimodal pain therapy. In 2021, there was a slight increase which, however, did not reach the level of care in 2019. The same is true for the first half of 2022 (Table 2).

Table 2. Number of cases and patients, stratified by DRG type and discharge year (2019, 2020, 2021, 01–06/2022).
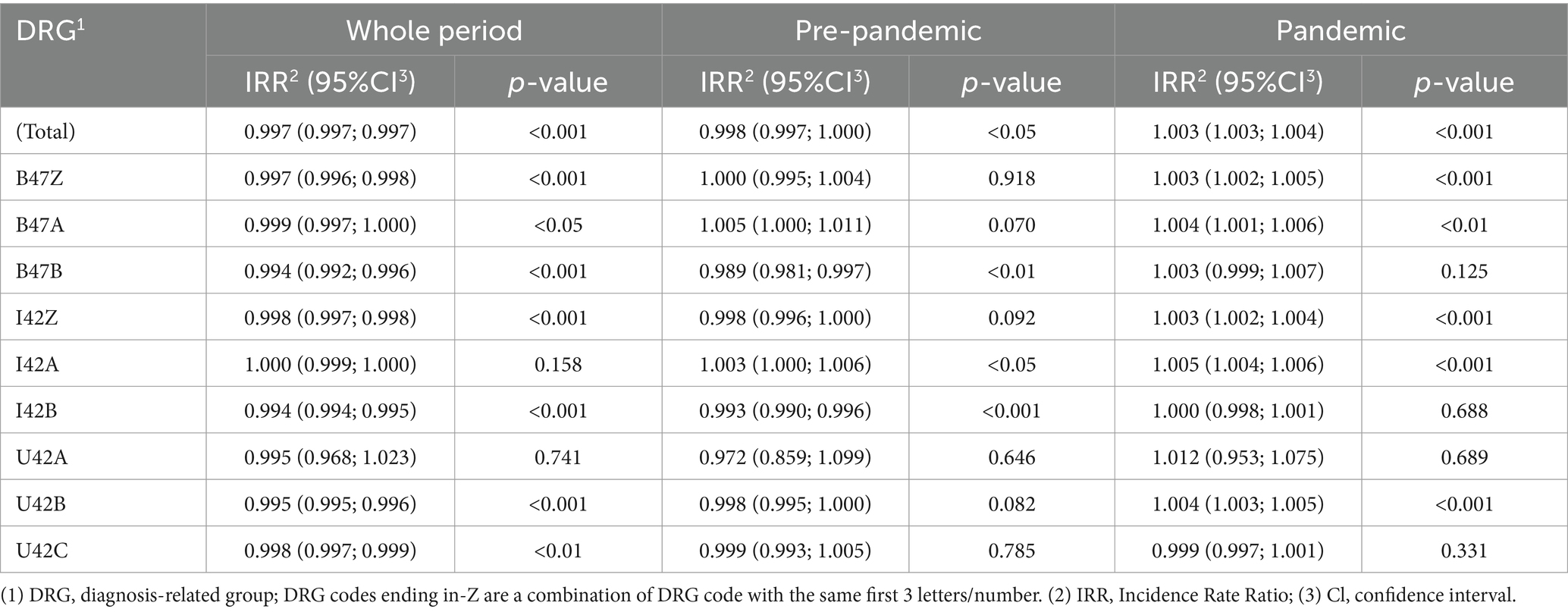
Regarding the whole study period, we found a trend for a decreased number of discharged patients for almost all DRGs (Table 3). By separating the two main period (pre-pandemic vs. pandemic) we found for the majority of DRGs a significant increase of patients during the pandemic period underlining the sharp decrease at the beginning of the pandemic followed by a slight increase of treated patients.
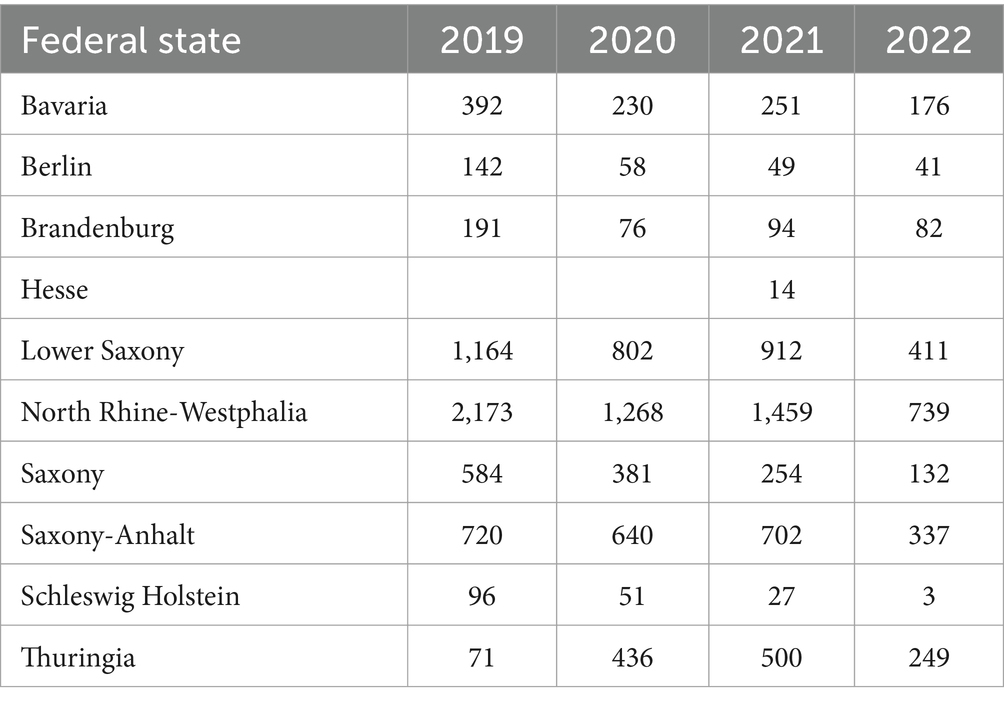
Regional differences (federal states)
In our analysis, we found some regional differences at level of the federal states of Germany. Saxony-Anhalt has shown the smallest changes of discharged pain patients over the course of the pandemic (Table 4).
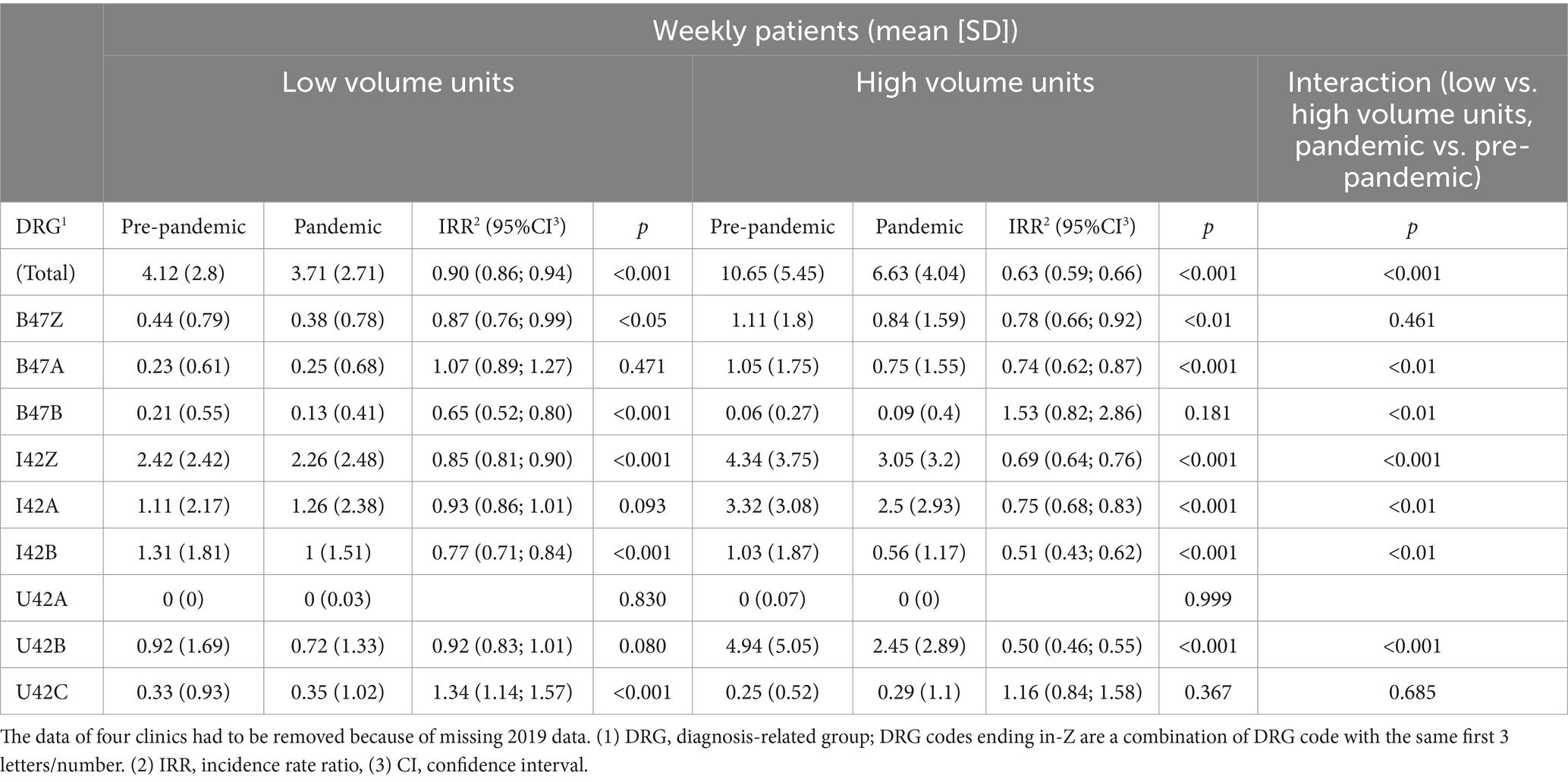
Pain unit size
With regard to the total discharge rates, we found statistically significant differences between the pre-pandemic and pandemic period for both, low and high volume pain units (Table 5). In a combined analysis of all selected DRGs, a more pronounced decrease was revealed for high volume pain units [incidence rate ratio [IRR]: 0.63 (95% CI: 0.59 to 0.66)] compared to low volume units [IRR: 0.90 (95% CI: 0.86 to 0.94)] between the two periods for the DRGs (Table 5).
With regard to single DRGs, a more complex picture was found. There are three codes, one each for the musculoskeletal system, the nervous system, and psychological and somatoform disorders. Minimum lengths of hospital stay of at least 14 treatment days or under 14 treatment days are coded separately. These 6 codes allowing the number of IMMST treatments over time to be shown using the DRG coding. Whereas for most DRGs a decreased discharge rate was found for both, high and low volume units comparing the pre-pandemic and the pandemic period, discrepant results were found for B47A and B47B. For both unit types, an increased IRR (i.e., increased discharge rate comparing pre-pandemic and pandemic period) was found for U42 C.
Discussion
In our study, we found that there was a substantial decrease in the number of patients hospitalized for severe pain during the COVID-19 pandemic.
Changes in hospital treatment
Changes in hospital care for patients with chronic pain occurred as a result of the COVID-19 pandemic. There was a significant decrease in inpatient multidisciplinary multimodal pain care, from a total of 5,533 hospitalizations in 2019 before the pandemic to 3,942 in 2020 and to 4,262 in 2021. There was a slight increase in the first half of 2022. Overall, however, these figures are also lower than the pre-pandemic figures from 2019.
Patient populations and regional variation
In our study, we found some small but statistically significant differences between the two cohorts. For example, patients of pandemic cohort were slightly younger and had a slightly higher Elixhauser Score than pre-pandemic patients. These results suggest a shift of treating severe pain under in-hospital conditions from elderly patients to younger, sicker patients (i.e., suffering from a higher number of comorbidities). However, these difference are small and of questionable clinical relevance.
Regarding regional variation, it’s worth mentioning that there are 16 federal states in Germany responsible for the regional hospital care. The measures to contain the pandemic were not the same in all of them. However, Table 4 provides an overview of the absolute care figures by federal state. Discussing all different regional COVID-19 related measures and their impact on our study results would be far beyond of our study topic.
The bio-psycho-social disease model under tightened hygiene measures
The multimodal inpatient and day-care treatment of chronic pain patients is based on the bio-psycho-social disease model and is an important component of pain medicine care. However, because of patient-centered therapies and participation in treatment groups, IMMST was very limited during the different phases of the pandemic due to stricter hygiene measures. This was compounded by uncertainty and anxiety among patients and their families, which led to a decline in demand for this healthcare service.
General conditions
Emergency treatments and treatments that could not be postponed in the hospital were prioritized (33). In addition to these medically sound care decisions, there were also economic incentives in Germany to keep bed capacities free for patients infected with COVID-19 or to use the remaining capacities as economically as possible (18). Staff reassignments were also necessary to care for wards with a focus on COVID-19 patients, intermediate care, and intensive care units.
The impact of the COVID-19 pandemic on the pain patient
The experience of psychosocial and spiritual aspects of palliative care can be used to evaluate pain care under COVID-19 conditions (34, 35). The pandemic had an impact on the components of the bio-psycho-social disease model of chronic pain patients. However, mood changes, social isolation, physical inactivity, and changes in dietary habits affected all populations to varying degrees. When pain patients have less contact with medical providers, it affects quality of life and pain severity. The risk of pain becoming chronic may be greater under the impact of a pandemic (35, 36). The pandemic has been and continues to be a psychosocial challenge for society and individuals. Coping strategies were different and should be the basis for reorienting medical action. The basis of pain management is the holistic approach, which is also required in psychosomatic treatment (1, 4, 24, 37). The pandemic has had a significant impact on patients with chronic pain. With increasing instability and chronification of pain and insufficient outpatient treatment options, an increase in multimodal inpatient treatment would have been logical. However, this did not happen because of the restrictive hygiene regulations and the focus of clinical treatment on COVID-19 patients.
Pain unit size and interdisciplinary multimodal pain management (IMMST) under tightened hygiene measures
Despite all the aforementioned legal restrictions and other challenges related to COVID-19, pain medicine care has taken place in hospitals. Even under these aggravated conditions, multimodal pain management has been implemented (38).
In our anlysis, a more pronounced decrease of patients receiving multimodal pain treatment was revealed for high volume pain units compared to low volume units. This might be related to the fact, that larger pain clinics or wards were more difficult to organize IMMST because these hospitals required more staff to care for critically ill COVID-19 infected patients and had to deal with staff absences due to sick leaves.
Whereas for most multimodal pain therapy DRGs, a decrease of discharge rates were found comparing pre-pandemic and pandemic period, an increase was found for selected DRGs (B74A: low volume units, B74B: high volume units). In other words, at least for ‘Multimodal pain therapy for diseases and disorders of the nervous system’ we found an increase of ‘short term treatments’ (less than 14 days) in low volume units whereas in high volume units, an increase of ‘long term treatment’ (at least 14 days) was found. Hence, we hypothesize a “centralisation” of severe (and long term cases) in high volume units.
Interestingly, discharge rates for multimodal pain therapy for mental diseases and disorders were increased for both unit types underlining the treatment need of pain and psychiatric comorbidities during the COVID-19 pandemia.
In addition to the problems of inpatient care, options in outpatient care for pain patients were also limited (39). Patients visited primary care physicians and specialists less frequently. This resulted in a lack of the usual hospital admissions. Desired treatments were postponed, and there was a general reluctance on the part of patients to undergo inpatient therapies. Skepticism and fear of infection when in contact with medical facilities were major issues here. An expected larger number of patients suffering from chronic pain due to inadequate care, as well as pandemic-related health restrictions in the biological, psychological, and social spheres due to lock-related movement restrictions, generally depressed mood, and reduced social contacts, should actually have led to a significant increase in inpatient IMMST after the end of the pandemic care restrictions, according to our expectations. However, this was not the case in the clinics studied. Overall, IMMST occurred despite the pandemic. The continued decline could be a temporary phenomenon. Another interpretation is that the perception of this form of treatment by referring physician colleagues has decreased. The clinics studied care for patients in different ways, some caring for more patients than before the pandemic, but others caring for fewer. The high demands placed on the structure of an IMMST can be better met by larger units of care (7, 40, 41).
Has the COVID-19 pandemic led to more chronic pain patients?
Data from orthopedic practices show an increase in new neck and back pain diagnosed during the pandemic (42). There are some data showing that delay or even failure to diagnose pain-related conditions may lead to an increased risk of developing chronic pain (42). Periods of crisis that affect the psychological stability of people with chronic pain lead to a higher risk of exacerbation of the disease (32). Our study does not provide evidence that a greater number of patients are hospitalized for multimodal pain management after the pandemic. However, because patients with complex pain syndromes often receive frustrating therapy for an extended period of time, a general pandemic-related increase in complex pain treatments, which may occur somewhat later, cannot be ruled out at this time. It is possible, however, that a shift of complex pain treatments to the outpatient setting could also lead to a situation in which any increased post-pandemic need for care is not reflected in the inpatient setting.
Pain management under difficult conditions
We were able to show that pain medicine care in hospitals took place and was possible during the COVID-19 pandemic. This is important because a combination of methods is also necessary for the individual components of multimodal pain therapy, as the example of psychotherapy shows (43). The DRG-based reimbursement system is also viewed critically in terms of utilization and efficiency, even in international comparison (44, 45). This and the differences in care limit international comparability. In addition to inpatient treatment of severe pain, outpatient interdisciplinary pain treatment is also possible under certain conditions (2). Promising results have been shown, for example, for patients with chronic nonspecific back pain (10). We did not investigate medical care in this area.
COVID-19 and pain: future research needs
Even after recovery from an acute COVID-19 infection, several pain-related long-term complaints were reported in post-COVID and long-COVID patients. For example, testicular pain, headache, chronic pain, and chest pain were reported as long-term pain syndromes (46). Hence, preventive measures are necessary to prevent chronic concomitant diseases, such as the chronic pain of COVID-19 infection (47). Vaccinations leading to an activation of antiviral immunity are preventive measures, as are presumably also the improvement of vitamin D deficiency and the intake of other micronutrients (48). However, further research is needed to fully understand and optimize treatment new onset and long lasting pain in COVID-19 patients as well as deterioration of chronic pain syndromes in patients with a COVID-19 infection. Furthermore, there is also a huge need for research in view of the emergence of new COVID variants or future pandemics which may build on the knowledge gained during the first pandemic waves.
Strengths
A particular strength of our study is the large number of included hospitals, which includes a variety of different departments in different regions of Germany and reflects the diversity of the German hospital landscape. Especially the avoidance of a one-sided focus on specialized pain centers and the large number of included patients underlines the high external validity of our results.
Limitations
As with any observational study using electronic hospital data, undercoding and miscoding of diagnoses must be expected. In addition, changes in the population during the observation period (hospitals newly admitted to the Helios Group or department closures) may also influence the absolute number of patients and cases considered. However, the case numbers of Helios hospitals under consideration can also be influenced by decisions of other hospital operators, such as possible new openings/closures or changes in the department structure. Since not all hospitals in Germany are included in the data, this limitation exists.
Against this background, the use of incidence rates in our study is explained in order to minimize such fluctuations in the population as far as possible.
Due to the data structure and because of data protection regulations, linking patient data between different hospitals was not possible. This limitation implies the possibility of double-counting specific patients who received treatment at multiple hospitals.
Conclusion
What can we learn for the future care of pain patients? There is an ethical dimension to the treatment of pain and how society deals with it (11, 39, 49). To date, this has not been considered in the care of patients. This is also reflected in the possible inadequate consideration and undertreatment of pain during the COVID-19 pandemic and a possible next one. Implications for future research include continued monitoring of inpatient multimodal treatment for pain and outpatient therapy after the official end of the pandemic. Whether the number of pain patients will increase as a result of the COVID-19 pandemic is also worth investigating.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: Raw data can not be provided due to data protection laws. Requests to access the aggregated datasets should be directed to Sven Hohenstein, c3Zlbi5ob2hlbnN0ZWluQGhlbGlvcy1oZWFsdGgtaW5zdGl0dXRlLmNvbQ==.
Ethics statement
The studies involving humans were approved by Ethics Committee at the Medical Faculty, Leipzig University (490/20-ek; Date: 7th February 2022.). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of in accordance with the national legislation and institutional requirements.
Author contributions
TC: Conceptualization, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing. SH: Data curation, Formal analysis, Methodology, Validation, Visualization, Writing – original draft, Writing – review & editing. AB: Conceptualization, Writing – original draft, Writing – review & editing. VP: Formal analysis, Validation, Writing – original draft, Writing – review & editing. VB: Writing – original draft, Writing – review & editing. SS: Conceptualization, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by Helios Kliniken GmbH, Grant-ID:2022-0198.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
1. Scheidlich, C. Psychosoziale Herausforderungen in der COVID-19-Pandemie In: R Bering and C Eichenberg, editors. Die Psyche in Zeiten der Corona-Krise: Herausforderungen und Lösungsansätze für Psychotherapeuten und soziale Helfer. 3rd ed. Stuttgart: Klett-Cotta (2021). 74–89.
2. Röhr, S, Müller, F, Jung, F, Apfelbacher, C, Seidler, A, and Riedel-Heller, SG. Psychosocial impact of quarantine measures during serious coronavirus outbreaks: a rapid review. [Psychosoziale Folgen von Quarantänemaßnahmen bei schwerwiegenden coronavirus-Ausbrüchen: ein rapid review]. Psychiatr Prax. (2020) 47:179–89. doi: 10.1055/a-1159-5562
3. Wolff, R, Clar, C, Lerch, C, and Kleijnen, J. Epidemiology of chronic non-malignant pain in Germany. [Epidemiologie von nicht tumorbedingten chronischen Schmerzen in Deutschland]. Schmerz. (2011) 25:26–44. doi: 10.1007/s00482-010-1011-2
4. Vogel, RT. Psychotherapie in Zeiten kollektiver Verunsicherung: Therapieschulen übergreifende Gedanken am Beispiel der Corona-Krise: Therapieschulübergreifende Gedanken am Beispiel der Corona-Krise. 1st ed. Wiesbaden: (2020).
5. van Hecke, O, Torrance, N, and Smith, BH. Chronic pain epidemiology and its clinical relevance. Br J Anaesth. 111:13–8. doi: 10.1093/bja/aet123
6. Tanaka, S. What changes occurred in patients with chronic pain in the early phase of the COVID-19 pandemic? J Anesth. (2022) 36:332–4. doi: 10.1007/s00540-022-03042-x
7. BVSD. (2020). Berufsverband der Ärzte und Psychologischen Psychotherapeuten in der Schmerz-und Palliativmedizin in Deutschland e.V. (BVSD). BVSD: 75 Prozent der stationären Schmerzeinrichtungen in Deutschland wegen COVID-19 geschlossen. Available online at: https://www.bvsd.de/bvsd-75-prozent-der-stationaeren-schmerzeinrichtungen-in-deutschland-wegen-covid-19-geschlossen/ (Accessed February 19, 2024)
8. World Health Organization. The Global Health Observatory. Available online at: http://www.who.int/topics/epidemiology/en/ (Accessed February 12, 2021)
9. Rikard, SM, Strahan, AE, Schmit, KM, and Guy, GP. Chronic pain among adults — United States, 2019–2021. MMWR Morb Mortal Wkly Rep. (2023) 72:379–85. doi: 10.15585/mmwr.mm7215a1
10. Müßgens, D, Burgard, LC, Kleine-Borgmann, J, Frettlöh, J, Sorgatz, H, and Bingel, U. Impact of the COVID-19 pandemic on patients with chronic pain in Germany: associations with expectations and control beliefs. Eur J Pain. (2022) 26:1343–54. doi: 10.1002/ejp.1955
11. Bering, R, and Eichenberg, C. Die Psyche in Zeiten der Corona-Krise: Herausforderungen und Lösungsansätze für Psychotherapeuten und soziale Helfer. 3rd ed. Stuttgart: Klett-Cotta (2020).
12. Jaeschke, T, Löbig, U, Berthold-Trümper, K, Welper, H, Korebrits, A, and Stengler, K. “Psyche in Not”– eine Telefonhotline in Corona-Zeiten. Psychiatr Prax. (2020) 47:392–4. doi: 10.1055/a-1249-0808
13. Strauß, B, Berger, U, and Rosendahl, J. Indirect and direct psychosocial consequences of the corona pandemic-part 1 of a (preliminary) review. Psychotherapeut. (2021) 66:175–85. doi: 10.1007/s00278-021-00504-7
14. Musazzi, UM, Di Giorgio, D, and Minghetti, P. New regulatory strategies to manage medicines shortages in Europe. Int J Pharm. (2020) 579:119171. doi: 10.1016/j.ijpharm.2020.119171
15. Beck, V. "You can say to me "- Subjektivität von sozialkörperlicher Distanz in Zeiten der Corona-Pandemie In: R Bering and C Eichenberg, editors. Die Psyche in Zeiten der Corona-Krise: Herausforderungen und Lösungsansätze für Psychotherapeuten und soziale Helfer. 3rd ed. Stuttgart: Klett-Cotta (2021). 151–63.
16. Deutsche Apothekerzeitung. (2020). CORONA-KRISE Bundestag stellt “epidemische Lage von nationaler Tragweite” fest. Available online at: https://www.deutsche-apotheker-zeitung.de/news/artikel/2020/03/25/bundestag-stellt-epidemische-lage-von-nationaler-tragweite-fest (Accessed November 4, 2020)
17. Bundesministerium der Justiz. Gesetz zum Schutz der Bevölkerung bei einer epidemischen Lage von nationale Tragweite. In: Bundesgesetzblatt 27.03.2020. Teil I Nr. 14. (2020). 587–592.
18. Ministeriums für Gesundheit, Arbeit und Soziales des Landes Nordrhein-Westfalen. (2020). Notwendige Maßnahmen zur Eindämmung des Corona-Virus und zur Behandlung von Covid-19-Patientinnen und Patienten. Runderlass des Ministeriums für Gesundheit, Arbeit und Soziales des Landes Nordrhein-Westfalen vom. Available online at: https://www.mags.nrw/coronavirus-rechtlicheregelungen-nrw (Accessed November 4, 2020)
19. Engel, GL. The need for a new medical model: a challenge for biomedicine. Science. (1977) 196:129–36. doi: 10.1126/science.847460
20. Engel, GL. The clinical application of the biopsychosocial model. Am J Psychiatry. (1980) 137:535–44. doi: 10.1176/ajp.137.5.535
21. Egger, JW. Der biopsychosoziale Krankheitsbegriff in der Praxis. Psychotherapeut. (2001) 46:309–16. doi: 10.1007/s002780100165
22. Kaiser, U, Treede, R-D, and Sabatowski, R. Multimodal pain therapy in chronic noncancer pain—gold standard or need for further clarification? Pain. (2017) 158:1853–9. doi: 10.1097/j.pain.0000000000000902
23. Bach, M, and Simhandl, C. Chronischer Schmerz – eine psychosomatische Sichtweise. Man Med. (2020) 58:27–33. doi: 10.1007/s00337-019-00634-9
24. Giesche, F, Streicher, H, Maiwald, M, and Wagner, P. Inpatient multimodal pain therapy: additive value of neuromuscular core stability exercises for chronic back pain. [die stationäre multimodale Schmerztherapie: Additiver wert eines sensomotorischen Stabilisationstrainings bei chronischem Rückenschmerz]. Schmerz. (2017) 31:115–22. doi: 10.1007/s00482-016-0178-6
25. Cegla, T. Schmerzkonferenzen In: M Schäfer and J Hubert, editors. Thomas Standl, Jochen Schulte am Esch, Rolf-Detlef Treede. Schmerztherapie: Akutschmerz-Chronischer Schmerz-Palliativmedizin. 2nd ed. Stuttgart: Georg Thieme Verlag KG (2010). 563.
26. Valladales-Restrepo, LF, Gaviria-Mendoza, A, Machado-Duque, ME, Prado-Echeverry, JA, Cortés-Navarro, JL, and Machado-Alba, JE. Chronic pain and continuity of analgesic treatment during the COVID-19 pandemic. Pain Pract. (2023) 23:359–67. doi: 10.1111/papr.13197
27. Gasparini, A. Comorbidity: an R package for computing comorbidity scores. JOSS. (2018) 3:648. doi: 10.21105/joss.00648
28. Moore, BJ, White, S, Washington, R, Coenen, N, and Elixhauser, A. Identifying increased risk of readmission and in-hospital mortality using hospital administrative data: the AHRQ Elixhauser comorbidity index. Med Care. (2017) 55:698–705. doi: 10.1097/MLR.0000000000000735
29. König, S, Hohenstein, S, Pellissier, V, Leiner, J, Hindricks, G, Nachtigall, I, et al. Changing trends of patient characteristics and treatment pathways during the COVID-19 pandemic: a cross-sectional analysis of 72, 459 inpatient cases from the German Helios database. Front Public Health. (2022) 10:1028062. doi: 10.3389/fpubh.2022.1028062
30. Baayen, RH, Davidson, DJ, and Bates, DM. Mixed-effects modeling with crossed random effects for subjects and items. J Mem Lang. (2008) 59:390–412. doi: 10.1016/j.jml.2007.12.005
31. Bates, D, Mächler, M, Bolker, B, and Walker, S. Fitting linear mixed-effects models using lme4. J Stat Soft. (2015) 67:1–48. doi: 10.18637/jss.v067.i01
32. R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. (2020). Available at: https://www.R-project.org/
33. Leiner, J, Hohenstein, S, Pellissier, V, König, S, Winklmair, C, Nachtigall, I, et al. COVID-19 and severe acute respiratory infections: monitoring trends in 421 German hospitals during the first four pandemic waves. Infect Drug Resist. (2023) 16:2775–81. doi: 10.2147/IDR.S402313
34. Kiepke-Ziemes, S, and Münch, U. Sechs Monate Corona-Pandemie in Deutschland: Psychosoziale und spirituelle Aspekte aus Sicht der Palliativversorgung. Zeitschrift für Palliativmedizin. (2020) 21:279–84. doi: 10.1055/a-1266-7203
35. Münch, U, Müller, H, Deffner, T, von Schmude, A, Kern, M, Kiepke-Ziemes, S, et al. Empfehlungen zur Unterstützung von belasteten, schwerstkranken, sterbenden und trauernden menschen in der Corona-Pandemie aus palliativmedizinischer Perspektive: Empfehlungen der Deutschen Gesellschaft für Palliativmedizin (DGP), der Deutschen Interdisziplinären Vereinigung für Intensiv-und Notfallmedizin (DIVI), des Bundesverbands Trauerbegleitung (BVT), der Arbeitsgemeinschaft für Psychoonkologie in der Deutschen Krebsgesellschaft, der Deutschen Vereinigung für Soziale Arbeit im Gesundheitswesen (DVSG) und der Deutschen Gesellschaft für Systemische Therapie, Beratung und Familientherapie (DGSF). [recommendations for the support of suffering, severely ill, dying or grieving persons in the corona pandemic from a palliative care perspective: Recommendations of the German Society for Palliative Medicine (DGP), the German interdisciplinary Association for Intensive and Emergency Medicine (DIVI), the Federal Association for Grief Counseling (BVT), the working Group for Psycho-oncology in the German Cancer society, the German Association for Social Work in the healthcare system (DVSG) and the German Association for Systemic Therapy, counseling and family therapy (DGSF)]. Schmerz. (2020) 34:303–13. doi: 10.1007/s00482-020-00483-9
36. Reck, T, Dumat, W, Krebs, J, and Ljutow, A. Outpatient multimodal pain therapy: results of a 1-week intensive outpatient multimodal group program for patients with chronic unspecific back pain - retrospective evaluation after 3 and 12 months [Ambulante multimodale Schmerztherapie: Ergebnisse eines 1-wöchigen ambulanten intensiven multimodalen Gruppenprogramms für Patienten mit chronischen unspezifischen Rückenschmerzen – retrospektive evaluation nach 3 und 12 Monaten]. Schmerz. (2017) 31:508–15. doi: 10.1007/s00482-017-0211-4
37. von Uexküll, T. Psychosomatische Medizin: Modelle ärztlichen Denkens und Handelns. 6th ed. München: Urban & Fischer (2003).
38. Luchting, B. Interdisziplinäre multimodale Schmerztherapie unter den Schutzmaßnahmen der COVID-19-Pandemie. Schmerz. (2020) 34:431–4. doi: 10.1007/s00482-020-00491-9
39. Breivik, H, Collett, B, Ventafridda, V, Cohen, R, and Gallacher, D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. (2006) 10:287–333. doi: 10.1016/j.ejpain.2005.06.009
40. Arnold, B, Böger, A, Brinkschmidt, T, Casser, H-R, Irnich, D, Kaiser, U, et al. Umsetzung der interdisziplinären multimodalen Schmerztherapie nach OPS 8-918. Schmerz. (2018) 32:5–14. doi: 10.1007/s00482-018-0266-x
41. Pfingsten, M, Arnold, B, Böger, A, Brinkschmidt, T, Casser, H-R, Irnich, D, et al. Cross-sectoral interdisciplinary multimodal pain therapy: recommendations on structural and process parameters of the ad hoc commission "interdisciplinary multimodal pain therapy" of the German pain society (deutsche Schmerzgesellschaft e. V.). [Sektorenübergreifende interdisziplinäre multimodale Schmerztherapie: Empfehlungen zu Struktur-und Prozessparametern der ad-hoc-Kommission "Interdisziplinäre Multimodale Schmerztherapie"der Deutschen Schmerzgesellschaft e. V]. Schmerz. (2019) 33:191–203. doi: 10.1007/s00482-019-0374-2
42. Jacob, L, Oh, H, Smith, L, Koyanagi, A, Konrad, M, and Kostev, K. Impact of the coronavirus disease 2019 (COVID-19) pandemic on the diagnosis of neck and low back pain in outpatient practices in Germany. Prev Med Rep. (2023) 31:102096. doi: 10.1016/j.pmedr.2022.102096
43. Koesling, D, Kieselbach, K, and Bozzaro, C. Chronic pain and society: sociological analysis of a complex interconnection. [Chronischer Schmerz und Gesellschaft: Soziologische analyse einer komplexen Verschränkung]. Schmerz. (2019) 33:220–5. doi: 10.1007/s00482-019-0361-7
44. Barouni, M, Ahmadian, L, Anari, HS, and Mohsenbeigi, E. Investigation of the impact of DRG based reimbursement mechanisms on quality of care, capacity utilization, and efficiency-a systematic review. Int J Healthc Manag. (2021) 14:1463–74. doi: 10.1080/20479700.2020.1782663
45. Lüngen, M, and Lauterbach, KW. Applicability of diagnostic related groups (DRG) in an international comparison. [Nutzung von diagnosis-related groups (DRG) im internationalen Vergleich]. Chirurg. (2000) 71:1288–95. doi: 10.1007/s001040051218
46. Fiala, K, Martens, J, and Abd-Elsayed, A. Post-COVID pain syndromes. Curr Pain Headache Rep. (2022) 26:379–83. doi: 10.1007/s11916-022-01038-6
47. Dmytriiev, D, and Dobrovanov, O. Post-COVID pain syndrome. Archives. (2021):505–12. doi: 10.35975/apic.v25i4.1582
48. Dobrovanov, O, Dmytriiev, D, Prochotsky, A, Vidiscak, M, and Furkova, K. Pain in COVID-19: Quis Est culpa? Electron J Gen Med. (2023) 20:em435. doi: 10.29333/ejgm/12672
Keywords: COVID-19 pandemic, pain, inpatient treatment, chronic pain, undertreated pain, undertreatment of pain, undertreatment, COVID-19
Citation: Cegla T, Hohenstein S, Bollmann A, Pellissier V, Bencheva V and Schmiedl S (2024) Impact of the pandemic on hospital care for chronic pain patients in Germany. Front. Med. 11:1393855. doi: 10.3389/fmed.2024.1393855
Edited by:
Pranav Prasoon, University of Pittsburgh, United StatesReviewed by:
Shivkumar Biradar, University of Pittsburgh, United StatesOleksandr Dobrovanov, A. Getlik Clinic for Children and Adolescents of SMU and UHB, Slovakia
Vipendra Kumar Singh, Indian Institute of Technology Mandi, India
Copyright © 2024 Cegla, Hohenstein, Bollmann, Pellissier, Bencheva and Schmiedl. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Thomas Cegla, dGhvbWFzLmNlZ2xhQGhlbGlvcy1nZXN1bmRoZWl0LmRl
 Thomas Cegla
Thomas Cegla Sven Hohenstein3,4
Sven Hohenstein3,4 Andreas Bollmann
Andreas Bollmann Vincent Pellissier
Vincent Pellissier Veronika Bencheva
Veronika Bencheva