
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Med., 06 June 2024
Sec. Intensive Care Medicine and Anesthesiology
Volume 11 - 2024 | https://doi.org/10.3389/fmed.2024.1393781
This article is part of the Research TopicInfections in the Intensive Care Unit, volume IIView all 17 articles
The benefit of temperature control in sepsis or septic shock is still under debate in the literature. We developed a national survey to assess the current state of knowledge and the practical management of spontaneous septic hypothermia in French intensive care units. Out of more 764 intensivists who were contacted, 436 responded to the survey. The majority of doctors (52.4%) considered spontaneous septic hypothermia to be a frequently encountered situation in intensive care, and 62.1% were interested in this problem. Definition of spontaneous septic hypothermia among French intensivists was not consensual. More than half of the doctors questioned (57.1%) stated that they did not actively rewarm patients suffering from spontaneous septic hypothermia.
The benefit of temperature control in sepsis or septic shock is still under debate in the literature (1, 2). The concept of a protective and adaptive effect of fever is controversial (3, 4) and the current randomised trial, SEPSISCOOL 2 (NCT04494074), compares two thermal control strategies for febrile patients in septic shock undergoing mechanical ventilation: namely, maintaining fever and maintaining normothermia via external cooling. However, a recent pilot study of afebrile septic patients found all-cause mortality at 28 days to be lower when hyperthermia (increase in body temperature of +1.5°C) was induced by external rewarming (5). In contrast, spontaneous hypothermia is thought to be associated with increased mortality among patients with sepsis (6). The benefits of induced hypothermia have also been reported in animal studies (7, 8), but clinical benefits have not been demonstrated in mechanically ventilated human patients with septic shock (9).
Unlike accidental hypothermia (10), hypothermia associated with haemorrhagic shock (11), or perioperative-associated hypothermia (12), there is no consensus on the management of spontaneous septic hypothermia. Two surveys—one involving patients in the United Kingdom (13) and the other on a European scale (14)—looked at the practices of different intensivists with regards to hypothermia in septic patients. Both studies revealed great variability in the definition and clinical management of the condition.
The aim of this survey is to assess the current state of knowledge and the practical management of spontaneous septic hypothermia in French intensive care units.
We developed a national survey containing simple or multiple-choice questions and open questions. In the first phase, the survey was distributed to intensivists in the surgical intensive care unit at Rennes University Hospital. In the second phase, the survey was submitted to doctors working in intensive care units in other departments (medical and cardio-thoracic intensive care) for testing and validation. The questions were revised and adapted according to the comments received. It was then circulated to members of the SFAR (French Society of Anesthesia and Intensive Care Medicine) and SRLF (French Intensive Care Society) societies between 1 March and 4 July 2023. Respondents were asked to answer the survey anonymously, referring to the usual practices within their respective intensive care units. The survey was distributed by e-mail to SRLF members, and also distributed to SFAR members including through social networks.
All analyses and graphs were produced using Excel® software. Categorical variables were presented as counts and percentages.
The survey was distributed by e-mail (764 e-mails) and through social networks. However, we do not know exactly how many intensivists actually received the survey and so cannot calculate an accurate response rate. The 2021 French demographic survey reported 2,350 intensivists practicing in France (15), of whom we hope to have contacted close to 50%.
Out of more 764 intensivists who were contacted, 436 responded to the survey. Of these, 405 worked in public hospitals, almost half in general intensive care units. The most represented specialisation was anaesthesiology. Over one-third of respondents declared 0–5 years’ experience in intensive care. All French regions were represented, as were the majority of departments (96%). Table 1 presents the characteristics of survey respondents.
The majority of doctors (52.4%) considered spontaneous septic hypothermia to be a frequently encountered situation in intensive care, and 62.1% were interested in this problem. Table 2 illustrates the heterogeneity in the definition of spontaneous septic hypothermia among French intensivists.
More than half of the doctors questioned (57.1%) stated that they did not actively rewarm patients suffering from spontaneous septic hypothermia, but 42.3% of these reported using survival blankets to limit heat loss. The primary reason for not using active rewarming (reported by 76.1% of respondents) was the lack of evidence in the literature and 30% of intensivists who did not use it actually associated the practice with deleterious effects, particularly in terms of haemodynamics. Furthermore, 30% of doctors who did not use active rewarming considered hypothermia to be an adaptive response that should be tolerated, and 5.2% thought it may have beneficial effects.
Of the doctors prescribing active rewarming, 80% used it in cases of sepsis or septic shock and 17% used it for septic shock only. The vast majority (97.3%) administered rewarming using pulsed hot-air blankets, while rewarming through infusion fluids and targeted temperature control equipment were rarely used (by 6.5 and 14%, respectively). Most of the doctors who used active rewarming reported starting it at 35°C (Table 3) with a target temperature of 36°C (Table 4). The speed at which hypothermia was corrected was uncontrolled by 52.4% of doctors, with 36.8 and 9.2% reportedly aiming for 0.5 and 1°C/h, respectively.
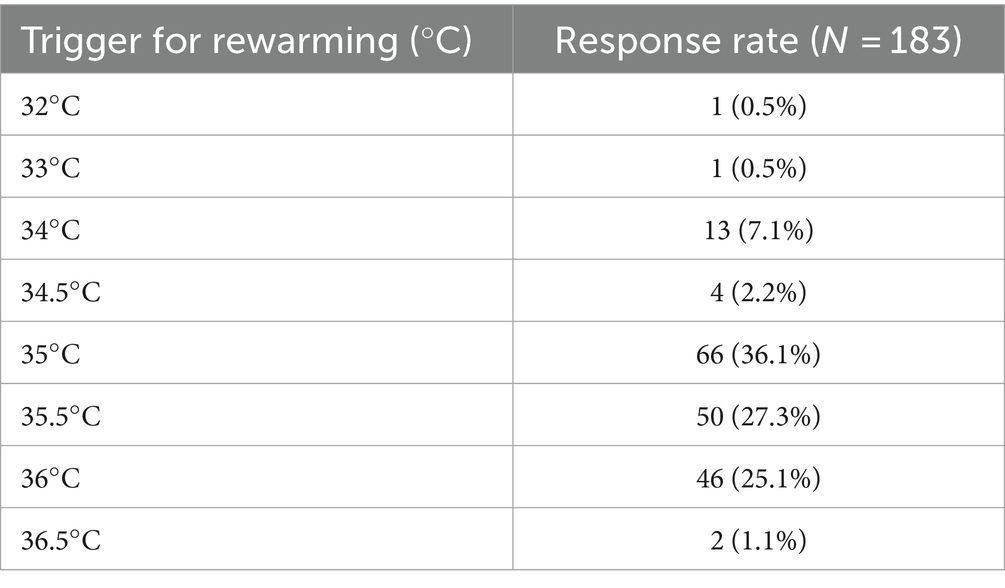
Table 3. The trigger temperature at which respondents consider rewarming patients with hypothermic sepsis.
Regarding the reasons for practising active rewarming, the majority of respondents (69.8%) wanted to combat coagulation disorders induced by hypothermia. Half of the intensivists surveyed used this practice because of the excess mortality associated with septic hypothermia, and 41.2% implemented rewarming for the immunomodulatory effects. Among the other responses, clinical tolerance of hypothermia and shivering were cited by 3% as justification for rewarming, while the prevention of hypothermia-induced cardiovascular events was reported by 4%.
There is currently no consensual definition of spontaneous septic hypothermia, and huge heterogeneity exists in the management of this condition with a poor prognosis. The results of the present survey provide an overview of the clinical practices in French intensive care units, which are mainly based on medical experience or extrapolation from the management of hypothermic non-septic patients (haemorrhagic shock, accidental hypothermia, peri-operative hypothermia). The data presented here highlight the gaps in the current literature on this subject. The publications are mainly descriptive or pathophysiological and do not make it possible to identify a clear and consensual definition or a strategy for the therapeutic management of spontaneous septic hypothermia. No therapeutic trial has assessed the impact of active rewarming in terms of morbidity and mortality. This could explain the results of our survey, in which less than half of the doctors questioned practised active rewarming, with the methods and objectives varying widely from centre to centre. Our findings highlight the necessity of further therapeutic trials involving intensive care teams for improving the management of patients with spontaneous septic hypothermia.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
GE: Conceptualization, Data curation, Formal analysis, Funding acquisition, Writing – original draft, Writing – review & editing. PB: Writing – review & editing. YL: Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Cariou, A, Payen, J-F, Asehnoune, K, Audibert, G, Botte, A, Brissaud, O, et al. Guidelines from a French expert panel. Anaesth Crit Care Pain Med. (2018) 37:481–91. doi: 10.1016/j.accpm.2017.06.003
2. Doman, M, Thy, M, Dessajan, J, Dlela, M, Do Rego, H, Cariou, E, et al. Temperature control in sepsis. Front Med. (2023) 10:1292468. doi: 10.3389/fmed.2023.1292468
3. Seguin, P, Launey, Y, Nesseler, N, and Malledant, Y. Is control fever mandatory in severe infections? Reanimation. (2016) 25:266–73. doi: 10.1007/s13546-015-1168-x
4. Schortgen, F, Clabault, K, Katsahian, S, Devaquet, J, Mercat, A, Deye, N, et al. Fever control using external cooling in septic shock: a randomized controlled trial. Am J Respir Crit Care Med. (2012) 185:1088–95. doi: 10.1164/rccm.201110-1820OC
5. Drewry, AM, Mohr, NM, Ablordeppey, EA, Dalton, CM, Doctor, RJ, Fuller, BM, et al. Therapeutic hyperthermia is associated with improved survival in afebrile critically ill patients with sepsis: a pilot randomized trial. Crit Care Med. (2022) 50:924–34. doi: 10.1097/CCM.0000000000005470
6. Rumbus, Z, Matics, R, Hegyi, P, Zsiboras, C, Szabo, I, Illes, A, et al. Fever is associated with reduced, hypothermia with increased mortality in septic patients: a meta-analysis of clinical trials. PLoS One. (2017) 12:e0170152. doi: 10.1371/journal.pone.0170152
7. Huet, O, Kinirons, B, Dupic, L, Lajeunie, E, Mazoit, JX, Benhamou, D, et al. Induced mild hypothermia reduces mortality during acute inflammation in rats. Acta Anaesthesiol Scand. (2007) 51:1211–6. doi: 10.1111/j.1399-6576.2007.01419.x
8. L’Her, E, Amerand, A, Vettier, A, and Sebert, P. Effects of mild induced hypothermia during experimental sepsis. Crit Care Med. (2006) 34:2621–3. doi: 10.1097/01.CCM.0000240231.76837.DC
9. Itenov, TS, Johansen, ME, Bestle, M, Thormar, K, Hein, L, Gyldensted, L, et al. Induced hypothermia in patients with septic shock and respiratory failure (CASS): a randomised, controlled, open-label trial. Lancet Respir Med. (2018) 6:183–92. doi: 10.1016/S2213-2600(18)30004-3
10. Musi, ME, Sheets, A, Zafren, K, Brugger, H, Paal, P, Hölzl, N, et al. Clinical staging of accidental hypothermia: the revised Swiss system: recommendation of the International Commission for Mountain Emergency Medicine (ICAR MedCom). Resuscitation. (2021) 162:182–7. doi: 10.1016/j.resuscitation.2021.02.038
11. Rossaint, R, Afshari, A, Bouillon, B, Cerny, V, Cimpoesu, D, Curry, N, et al. The European guideline on management of major bleeding and coagulopathy following trauma: sixth edition. Crit Care. (2023) 27:80. doi: 10.1186/s13054-023-04327-7
12. Riley, C, and Andrzejowski, J. Inadvertent perioperative hypothermia. BJA Educ. (2018) 18:227–33. doi: 10.1016/j.bjae.2018.05.003
13. Beverly, A, Walter, E, and Carraretto, M. Management of hyperthermia and hypothermia in sepsis: a recent survey of current practice across UK intensive care units. J Intensive Care Soc. (2016) 17:88–9. doi: 10.1177/1751143715601124
14. Harmon, MBA, Pelleboer, I, Steiner, AA, Wiewel, M, Schultz, MJ, Horn, J, et al. Opinions and Management of Hypothermic Sepsis: results from an online survey. Ther Hypothermia Temp Manag. (2020) 10:102–5. doi: 10.1089/ther.2019.0002
15. Ehrmann, S, Guitton, C, Aissaoui, N, Terzi, N, Capellier, G, and Vinsonneau, C. Démographie des réanimations françaises, enquête 2021 - État des lieux hors pandémie. Collège des Enseignants de Médecine Intensive Réanimation. (2021). Available at: https://www.ce-mir.fr/UserFiles/File/national/documents/divers/rapport-enquete-demographique-cemir.pdf
Keywords: spontaneous septic hypothermia, sepsis, septic shock, temperature control, hypothermia
Citation: Eustache G, Le Balc’h P and Launey Y (2024) Management of spontaneous septic hypothermia in intensive care. A national survey of French intensive care units. Front. Med. 11:1393781. doi: 10.3389/fmed.2024.1393781
Received: 29 February 2024; Accepted: 14 May 2024;
Published: 06 June 2024.
Edited by:
Zhongheng Zhang, Sir Run Run Shaw Hospital, ChinaReviewed by:
Wasineenart Mongkolpun, Mahidol University, ThailandCopyright © 2024 Eustache, Le Balc’h and Launey. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gabriel Eustache, Z2FicmllbC5ldXN0YWNoZUBjaHUtcmVubmVzLmZy
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.