
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med. , 03 May 2024
Sec. Nephrology
Volume 11 - 2024 | https://doi.org/10.3389/fmed.2024.1393734
 Leibo Wang1,2†
Leibo Wang1,2† Xianzhe Yu3†
Xianzhe Yu3† Zuze Qiu2†
Zuze Qiu2† Puyu Liu4†
Puyu Liu4† Wu Tian1†
Wu Tian1† Wei He1†
Wei He1† Yulin Pan5†
Yulin Pan5† Feng Xu1
Feng Xu1 Zhuangding Cen1
Zhuangding Cen1 Yang Ou1
Yang Ou1 Daobing Li2*
Daobing Li2*Objective: This retrospective study aims to identify risk factors for urogenic sepsis in patients with upper urinary tract stones following ureteral flexible lithotripsy (FURL). Additionally, we analyze the clinical characteristics of bacterial infections post-surgery.
Methods: A total of 759 patients who underwent FURL at the Urology Department of Zunyi Medical University were included. Univariate and multivariate Logistic regression analyses were conducted to identify independent risk factors for urogenic sepsis post-FURL. The distribution of bacteria based on preoperative urine cultures was also analyzed. Statistical analysis was performed using R4.2.2 software.
Results: Of the 759 patients, positive preoperative urine culture, urine nitrite positivity, urine white blood cell count (WBC) ≥ 200 cells/μL, residual stones, and neutrophil-to-lymphocyte ratio (NLR) were found to be independent risk factors for urogenic sepsis after FURL. Among the 164 patients with positive preoperative urine cultures, 32 developed urogenic sepsis post-surgery, with 68.75% having positive preoperative cultures. The leading pathogens causing postoperative urogenic sepsis were Escherichia coli (E. coli), Enterococcus faecium, Proteus mirabilis, and Klebsiella pneumoniae. The probabilities of progression to urogenic sepsis were as follows: E. coli 19% (n = 12), Enterococcus faecium 43% (n = 3), Proteus mirabilis 33.3% (n = 1), and Klebsiella pneumoniae 33.3% (n = 1). The ages of affected patients were 47.17 ± 13.2, 53.7, 41, and 79 years, respectively. Rates of comorbid diabetes were 36.4, 66.7, 50, 100%, with nitrite positivity rates at 72.7, 33.3, 50, 0%. Ten female patients were infected with E. coli, while patients infected with Klebsiella pneumoniae had an NLR of 7.62.
Conclusion: Positive preoperative urine culture, urine nitrite positivity, urine WBC ≥ 200 cells/μL, residual stones, and NLR are independent risk factors for urogenic sepsis after FURL. Escherichia coli is the predominant pathogen post-FURL, with notable female prevalence and nitrite-positive urine in infections. Enterococcus faecium infections are associated with diabetes.
Urolithiasis stands as a prevalent ailment in urology, with the worldwide incidence of urinary stones ranging from 1 to 20%, and specifically within China, it falls between 1 and 5% (1, 2). The global prevalence of urolithiasis has been on the rise, attributed to shifts in dietary patterns, socioeconomic factors, and climatic variations (3). Notably, the recurrence rate within a decade following treatment is notably high, hovering around 50% (4). The escalating trends in urolithiasis pose significant health threats to patients and impose substantial financial burdens. Studies forecast a projected annual increase of $1.24 billion in costs associated with urolithiasis by the year 2030 (5). This pressing issue underscores the urgent need for effective prevention strategies and treatment modalities to mitigate the impact on patient well-being and healthcare expenditures.
In recent decades, the gradual emergence of endoluminal urological techniques has significantly expanded the use of minimally invasive procedures such as percutaneous nephrolithotomy, ureteroscopy, and ureteral flexible scopes. Notably, flexible ureteroscopic lithotripsy has emerged as a safe and effective treatment option for upper urinary tract stones due to its advantages of providing a clear surgical field, minimal invasiveness, and swift recovery (6). The European Association of Urology (EAU) has endorsed this technique as the primary treatment for kidney stones measuring ≤2cm (7). Despite the benefits of these procedures, a spectrum of surgical complications can arise, with urinary sepsis representing one of the most severe, with incidence rates ranging from 0.1 to 4.3% (8). Urinary sepsis is particularly concerning due to its rapid onset, swift progression, and alarmingly high mortality rate, which can reach up to 50% (8).
A positive mid-section urine culture is closely associated with the development of urosepsis following FURL (9–11). The release of bacteria and endotoxins from within the stones during the procedure is a significant factor leading to urinary tract infections, Systemic Inflammatory Response Syndrome (SIRS), and potentially urosepsis (9). The detailed analysis of bacterial profiles holds significant clinical importance for preventing and treating postoperative urogenic sepsis. Therefore, this study aims to investigate the risk factors for urogenic sepsis following ureteral lithotripsy in patients with upper urinary tract stones, with a specific focus on preoperative urine culture results. Additionally, the study aims to analyze the clinical characteristics of various bacteria in patients who develop postoperative urogenic sepsis. The overarching goal is to provide clinicians with valuable insights and guidance for the early prevention and effective treatment of postoperative urogenic sepsis subsequent to ureteral lithotripsy using flexible ureteroscopes.
Patients diagnosed with kidney stones or upper ureteral stones and admitted to the Affiliated Hospital of Zunyi Medical University between January 2019 and December 2022 were enrolled as study participants. Inclusion Criteria: 1. All cases were confirmed using computed tomography (CT). 2. Patients underwent treatment with ureteral flexible scope lithotripsy for upper urinary tract stones and had complete medical records. Exclusion Criteria: 1. Postoperative sepsis resulting from infections in other organ systems. 2. Patients with immunocompromised conditions such as tumors, blood disorders, or those taking oral immunosuppressive drugs. 3. Individuals with congenital anomalies such as polycystic kidneys, horseshoe kidneys, or pelvic-ureteral junction obstruction. 4. Cases with incomplete or insufficient medical records. The retrospective study was approved by the Ethics Review Board of the Affiliated Hospital of Zunyi Medical University. Informed consent requirements were waived by the Ethics Review Board due to the minimal risks associated with retrospective studies.
All surgeries were performed by attending physicians with extensive experience in the department. The principles of antibiotic use in this study were carried out according to the Chinese Guidelines for the Treatment of Urologic Stones. If preoperative urine culture is negative but there is a urinary tract infection, appropriate antibiotics such as levofloxacin, amikacin, or others should be chosen based on local bacterial spectrum and resistance profiles. The antibiotic should be selected according to the treatment course, which is typically 1 week. During the operation, first-generation, second-generation, and fluoroquinolone drugs are used for prophylaxis. If preoperative urine culture is positive or preoperative urine routine shows positive nitrites the surgeon should choose oral or intravenous antibiotics according to the drug sensitivity results. One week later, if the urine culture results are negative before surgery, the patient can undergo the surgery. If the urine culture remains positive, continue with anti-infection treatment. If preoperative urine culture is negative and there is no obvious urinary tract infection, first-generation, second-generation cephalosporins, and fluoroquinolone drugs are used for infection prophylaxis. If there are no postoperative infectious complications, the total treatment course should be ≤24 h.
Data collection for this study was a collaborative effort involving two researchers specializing in urology. Additionally, the collected data underwent scrutiny by two individuals to ensure its accuracy and validity. The study included various patient characteristics such as age, gender, presence of comorbid hypertension, comorbid diabetes mellitus status, stone location (side and site), stone size, presence of hydronephrosis, preoperative neutrophil count, absolute blood lymphocyte count, Neutrophil-to-Lymphocyte Ratio (NLR: calculated as preoperative absolute neutrophil count divided by blood lymphocyte count), absolute blood leukocyte count before surgery, preoperative urinary leukocyte count, urine nitrite test (NIT), preoperative creatinine levels, results of preoperative urine culture with drug sensitivity, duration of surgery, amount of bleeding during surgery, and presence of residual stone.
The diagnostic criteria for urogenic sepsis align with the guidelines set forth by the European Society of Urology in 2018 (12). According to these guidelines, urogenic sepsis is diagnosed when a patient presents with a urinary tract infection accompanied by systemic inflammatory response syndrome (13). The confirmation of this diagnosis requires the presence of at least two of the following SIRS criteria: (1) temperature > 38°C or < 36°C; (2) heart rate > 90 beats/min; (3) respiration >20 breaths/min or hyperventilation with PaCO2 < 32 mmHg; (4) blood leukocyte counts >12 × 10^9/L or < 4 × 10^9/L, or immature granulocytes >10%. Additionally, the patient may exhibit concurrent symptoms of urinary tract infection or have a positive blood culture.
All statistical analyses for this study were performed using R version 4.2.2 statistical software. Continuous variables were expressed as mean ± standard deviation or median with interquartile range, while categorical variables were presented as counts and corresponding percentages. Initial analysis of patient clinicopathological characteristics was conducted using Logistic univariate regression. Variables exhibiting statistically significant differences were subsequently included in a multivariate Logistic regression analysis to identify independent risk factors. The results of the multivariate Logistic regression analysis were then used to screen for these independent risk factors. With p < 0.05 for the difference is statistically significant.
A total of 759 cases of postoperative patients undergoing ureteroscopic lithotripsy in the Department of Urology, Affiliated Hospital of Zunyi Medical University, were included in this study. Among them, 32 patients developed urosepticemia after surgery. In the non-urosepticemia group, there were 142 (19.53%) patients with positive urine cultures, 307 (42.23%) patients with surgical times exceeding 90 min, and 205 (28.20%) patients with stones ≥20 mm. In the urosepticemia group, 46.88% (n = 15) of patients had positive urinary nitrite, 68.75% (n = 22) had urinary leukocytes exceeding 200 cells/μL, and 17 (53.12%) patients had positive urinary nitrite. Detailed general clinical characteristics of the patients are shown in Table 1.
The results revealed independent risk factors associated with the development of urogenital sepsis after ureteral flexible lithotripsy to be Urine Culture, Urine Nitrite, Urine White Blood Cell count, Residual Stone, and Neutrophil-to-Lymphocyte Ratio, as depicted in Table 2.
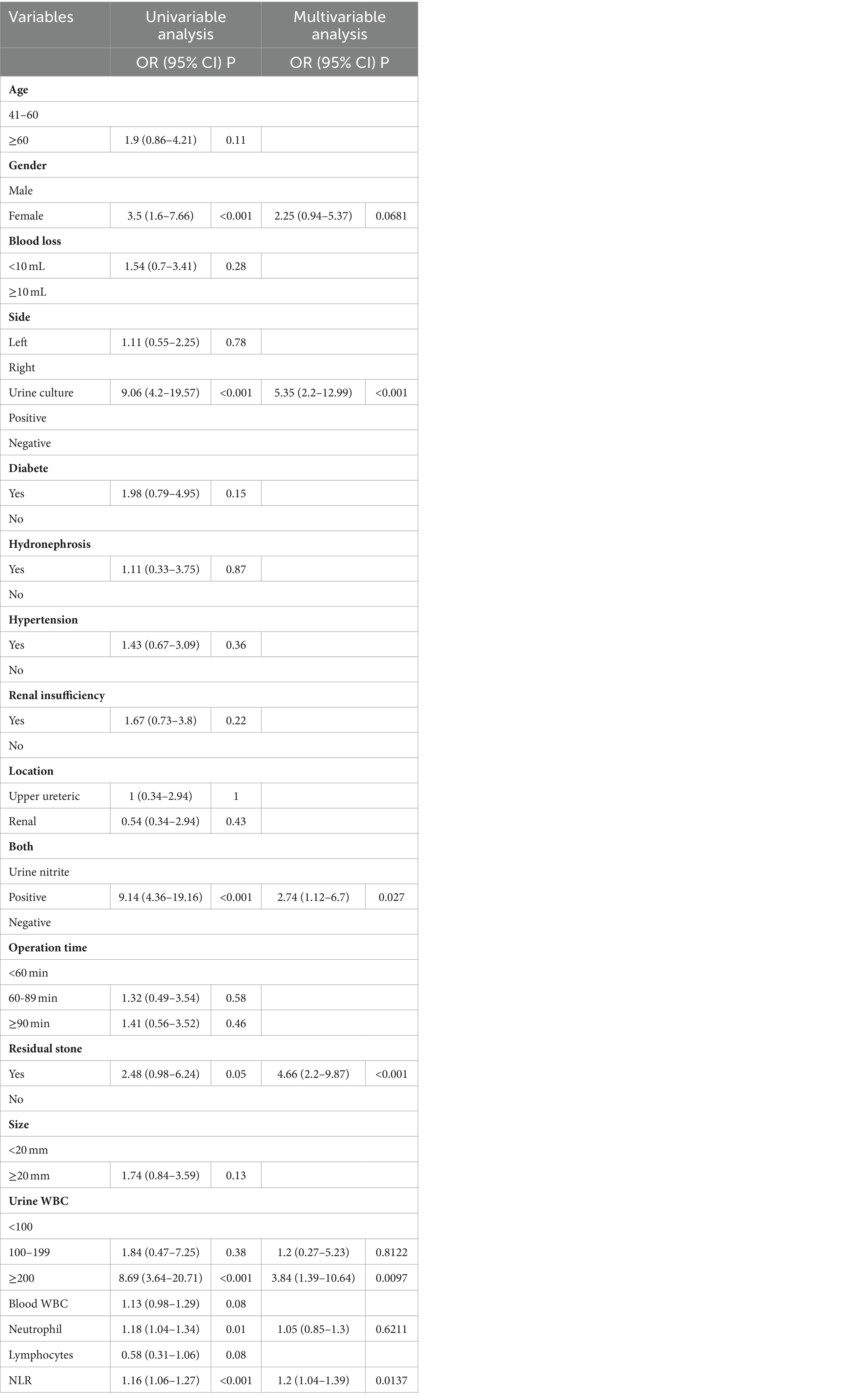
Table 2. Results of single-factor and multi-factor logistic regression analysis on urosepsis occurrence in patients after flexible ureteroscopy lithotripsy.
Out of 759 patients, 164 had positive preoperative urine cultures. Among the 32 patients with urogenic sepsis, 22 (68.75%) had positive preoperative urine cultures, three of whom had multiple bacterial infections. The bacterial species and associated statistical analysis are detailed in Table 3. The most common causative organisms were Escherichia coli, followed by Enterococcus faecalis and Gardnerella vaginalis.
The probability of progression to urogenic sepsis in patients with E. coli infection was 19% (n = 12). Among patients with Enterococcus faecium infection, three out of seven (43%) progressed to urogenic sepsis, two out of six with Proteus mirabilis (PM) infection, and one out of three with Klebsiella pneumoniae infection. Clinical features of ureterogenic septicemia following ureteral flexible lithotripsy are outlined in Table 4.
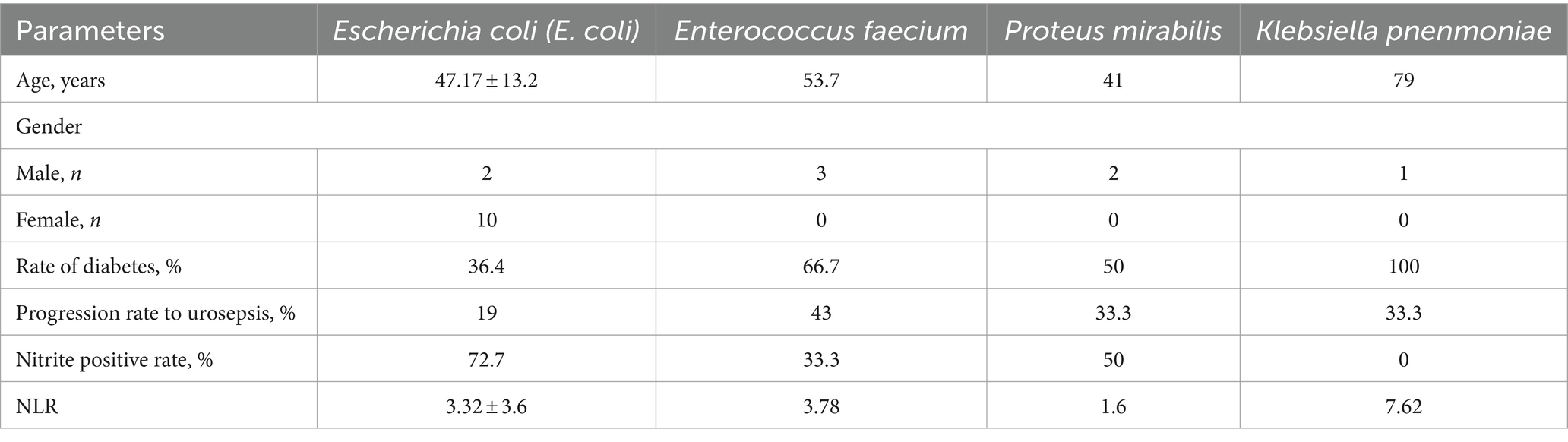
Table 4. Clinical characteristics of various bacteria causing urogenic sepsis following FURL surgery.
Despite advancements in urologic laparoscopic techniques and the evolution of lithotripsy and stone extraction equipment, FURL remains associated with postoperative infections, a prevalent complication (11, 14). Urogenic sepsis, as the most severe perioperative complication of FURL, continues to pose challenges for urologists in clinical practice. In this retrospective study, we identified Urine Culture, Urine Nitrite, Urine White Blood Cell count, Residual Stone, and Neutrophil-to-Lymphocyte Ratio as independent risk factors for urogenic sepsis after FURL, using univariate and multivariate logistic regression analyses. Furthermore, we conducted an analysis of bacterial distribution based on preoperative urine culture results, revealing Escherichia coli, Enterococcus faecalis, and Gardnerella vaginalis as the most common bacteria causing urinary tract infections. Understanding these prevalent urinary tract bacteria and their corresponding infection characteristics can aid in clinical diagnosis and treatment strategies.
The present study confirms that Urine culture stands as a significant risk factor for urogenic sepsis development following FURL, aligning with previous research findings (9, 10, 15, 16). Mi et al. (9) reported that 16 of 21 patients (76.2%) in the SIRS group exhibited positive preoperative urine cultures, with these results significantly correlating with postoperative SIRS development. Similarly, James et al. (17) in a retrospective analysis of 462 patients treated for stones via ureteroscopy, noted a significant association between positive mid-stream urine cultures and postoperative urinary sepsis findings, despite all patients receiving appropriate preoperative antibiotic therapy. Senocak et al. (16) in a retrospective analysis of 492 patients undergoing ureteral flexible lithotripsy, found an 8.5% incidence of postoperative infectious complications. Of the 59 patients (12%) with positive preoperative urine cultures, 19 patients (32.2%) were identified with multidrug-resistant (MDR) isolates from these cultures.
Urinary tract infections (UTIs) should be adequately treated with anti-infective therapy prior to various urologic surgeries, a consensus among major urologic guidelines. In this study, we adhered to the principles of antibiotic use outlined in the Chinese guidelines for urologic stone treatment, administering anti-infective therapy to all patients with positive preoperative urine cultures and evidence of UTIs. Despite this, 32 out of 164 patients with positive preoperative urine cultures developed urogenital sepsis, resulting in an incidence rate of 19.5%. Gutierrez et al. (9, 18) found in their study that even with the administration of broad-spectrum antibiotics to urine-negative patients or sensitive antibiotics to those with positive urine cultures, postoperative Systemic Inflammatory Response Syndrome following flexible ureteroscopic lithotripsy remained inevitable. Patients with gram-negative bacilli in their urine cultures were noted to be more prone to postoperative hyperthermia compared to those with gram-positive bacilli. It has been suggested that the biofilm formed in stones presents a challenge for antibiotics to effectively eliminate bacteria (9, 19). Despite patients with positive preoperative urine cultures exhibiting negative secondary urine cultures after antibiotic treatment and prior to surgery, the presence of bacterial endotoxins within stones complicates antibiotic penetration. Furthermore, significant endotoxin release during lithotripsy increases infection risks, potentially leading to systemic inflammatory responses. Some studies (10) suggest that early antibiotic treatment could be effective in reducing the incidence of SIRS. Considering that results from urine culture sensitivity tests typically take at least 48 hours (20), understanding common urinary tract bacteria and their respective infection characteristics becomes crucial. This understanding aids in the selection of appropriate empirical antibiotic treatment while awaiting urine culture results.
The primary bacteria identified in preoperative urine cultures in this study included Escherichia coli, Enterococcus faecalis, Gardnerella vaginalis, Proteus mirabilis, and Klebsiella pneumoniae. Among these, Escherichia coli ranked highest at 34.4%, consistent with findings from previous studies (21, 22). Cagri et al. (16) reported similar results in their study on risk factors for infectious complications following flexible ureteroscopic lithotripsy, with Escherichia coli and Enterococci being the predominant pathogens. In our study, Escherichia coli infection was notably associated with predominantly female patients and positive urinary nitrites. Furthermore, Escherichia coli positivity exhibited a significant association with postoperative urogenic sepsis after ureteral flexible lithotripsy. Patients positive for Enterococcus faecalis, Proteus mirabilis, and Klebsiella pneumoniae were also more likely to develop postoperative urogenic sepsis compared to Escherichia coli positivity (43, 33.3, and 33.3% vs. 19%). However, statistical analyses regarding postoperative urogenic sepsis were not obtained for Enterococcus faecalis and Gardnerella vaginalis, likely due to the small sample size. Studies suggest (21) that one-third of community-acquired urinary tract infections caused by Escherichia coli are attributed to ultrawide-spectrum β-lactamase (ESBL) strains, highly resistant to commonly used community antibiotics, thus limiting treatment effectiveness. Another study has shown (23) that the expression of the BLA CTX-M-14 gene in Escherichia coli leads to increased resistance, further restricting the empirical use of cephalosporins and fluoroquinolones in urinary tract infection treatment.
Enterococci are commonly identified as pathogens in urinary tract infections (24), with some studies suggesting that they have become the primary causative agent of such infections (22, 25). The main culprits among enterococci are Enterococcus faecalis Andenterococcus faecium, which are generally less virulent compared to other strains (22). In our study, Escherichia coli remained the predominant infection, with urogenic sepsis occurring in 3 out of 7 patients positive for Enterococcus faecium. Interestingly, no cases of urogenic sepsis were observed in the 10 patients with Enterococcus faecalis infections. Additionally, 66.7% of patients with Enterococcus faecium infections also had comorbid diabetes mellitus, highlighting this as a significant risk factor. Enterococci exhibit a natural resistance to many antibiotics, and there is a rapid increase in acquired resistance, complicating the treatment of urinary tract infections caused by these bacteria (26). Recent reports indicate a global rise in hospital-acquired vancomycin-resistant enterococcal infections, underscoring the potential for serious nosocomial infections (27). Therefore, heightened surveillance of this bacterial group is crucial for the prevention and control of nosocomial infections.
Proteus mirabilis and Klebsiella pneumoniae are two additional common bacteria found in our study. Studies have noted that (28) Klebsiella pneumoniae exhibits a strong adhesive and invasive capability, allowing it to persist in the urethra and resist urinary tract erosion. This resilience is particularly notable in diabetic patients with inadequate glycemic control, where the bacterium shows increased resistance and a tendency for recurrent infections. Furthermore, research has shown that (29, 30) Klebsiella pneumoniae has the ability to produce carbapenemases, acquiring resistance to carbapenems. Strains with this characteristic are also resistant to penicillin and cephalosporins, facilitating their transmission. In our study, patients who developed sepsis from Klebsiella pneumoniae infection tended to be of advanced age, with comorbid diabetes mellitus, and exhibited high Neutrophil-to-Lymphocyte Ratio, but the results were limited by the sample. Proteus mirabilis (31), a Gram-negative rod-shaped bacterium, is a prominent pathogen causing complicated urinary tract infections. Some studies have suggested that (31) catheter-associated urinary tract infections (CAUTI) in particular are the main pathogens. Due to its ureolytic biomineralization, Proteus mirabilis can form a crystalline biofilm on the surfaces of indwelling urethral catheters, leading to catheter scaling, blockage, and, often, urinary retention. This can result in ascending urinary tract infections, such as cystitis and pyelonephritis (32). This bacterium commonly coexists with various other members of the microbial community (32). A deeper understanding of Proteus mirabilis will aid clinicians in developing optimal strategies to control infections associated with this bacterium.
In addition to positive urine culture, this study identified positive urine nitrite, urine white blood cell count ≥200 cells/μL, residual stone, and Neutrophil-to-Lymphocyte Ratio as independent risk factors for urogenital sepsis following ureteral flexible lithotripsy. The urinary nitrite test and urine WBC count are commonly utilized for diagnosing urinary tract infections. Studies have indicated a high specificity of urinary nitrite for Gram-negative bacterial urinary tract infections (33). In our study, the risk of sepsis was found to be 2.74 times higher in preoperative urinary nitrite-positive patients compared to nitrite-negative patients. Moreover, debris remaining after ureteral flexible lithotripsy may harbor bacteria and endotoxins, which can enter the vasculature through damaged endothelium, potentially leading to infectious complications (34). The Neutrophil-to-Lymphocyte Ratio (35) serves as a straightforward and effective indicator of a patient’s immune status and infection severity. A retrospective study has demonstrated that (36) NLR values may be more effective than blood WBC and neutrophil counts in predicting or diagnosing urinary sepsis.
This study is subject to several limitations. Firstly, being a single-center retrospective study, it may have inherent selection bias and limited included data. A broader, prospective multicenter study is warranted for further analysis in the future. Secondly, the study did not delve into further analysis of bacterial resistance, which will be a focal point of our future research on this topic. Thirdly, intra-pelvic perfusion pressure during ureteral flexible lithotripsy is often linked to infection-related complications, yet this data was not collected in our study due to equipment limitations.
In conclusion, this study identified Urine culture positivity, Urine nitrite, Urine WBC count ≥200 cells/μL, Residual stone presence, and NLR as independent risk factors for postoperative urogenic sepsis following FURL. Additionally, the study analyzed the distribution of bacteria based on preoperative urine cultures, with Escherichia coli being the most prevalent pathogen associated with postoperative urogenic sepsis. This was followed by Enterococcus faecalis, Proteus mirabilis, and Klebsiella pneumoniae. Key characteristics of Escherichia coli infections included a higher prevalence among female patients and positive urine nitrite results. Patients with Enterococcus faecalis infections often presented with comorbid diabetes mellitus. Patients with Klebsiella pneumoniae infection and sepsis in this study were old, often complicated with diabetes, and had a high NLR. However, due to limited samples, more extensive data will need to be included in the future to further demonstrate this conclusion.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The Ethics Committee of Guizhou Hospital, Beijing Jishuitan Hospital approved this study (20220402). The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because retrospective studies have extremely low risk.
LW: Funding acquisition, Methodology, Writing – original draft, Writing – review & editing. XY: Writing – original draft, Methodology. ZQ: Data curation, Writing – original draft. PL: Formal analysis, Writing – original draft, Supervision. WT: Supervision, Writing – original draft. WH: Investigation, Software, Writing – original draft. YP: Methodology, Validation, Writing – review & editing. FX: Project administration, Writing – review & editing. ZC: Methodology, Validation, Writing – original draft. YO: Methodology, Resources, Writing – review & editing. DL: Methodology, Project administration, Software, Supervision, Writing – original draft.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. Science and Technology Foundation of Guizhou Provincial Health Commission (Reference number: Gzwkj2023-373). Beijing Jishuitan Hospital Guizhou Hospital Youth Innovation Fund [Reference number: YQNCX (2023)].
We thank all the reviewers for their assistance and support.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Zhang, L, Zhang, X, Pu, Y, Zhang, Y, and Fan, J. Global, regional, and National Burden of urolithiasis from 1990 to 2019: a systematic analysis for the global burden of disease study 2019. Clin Epidemiol. (2022) 14:971–83. doi: 10.2147/CLEP.S370591
2. Abedi, G, and Monga, M. Flexible Ureteroscopy for treatment of upper urinary tract Calculus. J Endourol. (2021) 35:S-56–61. doi: 10.1089/end.2020.1018
3. Wang, L, Li, D, He, W, Shi, G, Zhai, J, Cen, Z, et al. Development and validation of a predictive model for post-percutaneous nephrolithotomy urinary sepsis: a multicenter retrospective study. Minerva Urol Nephrol. (2023). doi: 10.23736/S2724-6051.23.05396-X
4. Lai, L, Zhang, W, Zheng, F, Wang, T, Bai, P, Liu, Z, et al. Comparison of the efficacy of ShuoTong Ureteroscopy and simple flexible Ureteroscopy in the treatment of unilateral upper ureteral calculi. Front Surg. (2021) 8:707022. doi: 10.3389/fsurg.2021.707022
5. Antonelli, JA, Maalouf, NM, Pearle, MS, and Lotan, Y. Use of the National Health and nutrition examination survey to calculate the impact of obesity and diabetes on cost and prevalence of urolithiasis in 2030. Eur Urol. (2014) 66:724–9. doi: 10.1016/j.eururo.2014.06.036
6. Xu, K, Ding, J, Shi, B, Wu, Y, and Huang, Y. Flexible ureteroscopic holmium laser lithotripsy with PolyScope for senile patients with renal calculi. Exp Ther Med. (2018) 16:1723–8. doi: 10.3892/etm.2018.6369
7. Liang, H, Liang, L, Lin, Y, Yu, Y, Xu, X, Liang, Z, et al. Application of tip-bendable ureteral access sheath in flexible ureteroscopic lithotripsy: an initial experience of 224 cases. BMC Urol. (2023) 23:175. doi: 10.1186/s12894-023-01347-x
8. Scotland, KB, and Lange, D. Prevention and management of urosepsis triggered by ureteroscopy. Res Rep Urol. (2018) 10:43–9. doi: 10.2147/RRU.S128071
9. Mi, Q, Meng, X, Meng, L, Chen, D, and Fang, S. Risk factors for systemic inflammatory response syndrome induced by flexible Ureteroscope combined with holmium laser lithotripsy. Biomed Res Int. (2020) 2020:1–5. doi: 10.1155/2020/6842479
10. Zhang, H, Jiang, T, Gao, R, Chen, Q, Chen, W, Liu, C, et al. Risk factors of infectious complications after retrograde intrarenal surgery: a retrospective clinical analysis. J Int Med Res. (2020) 48:030006052095683. doi: 10.1177/0300060520956833
11. Yang, B, Liu, S, Mi, Y, Wang, J, Zhang, Y, and Wang, J. The impact of watching real-time videos of flexible ureteroscopic lithotripsy on anxiety and depression in patients. Int Urol Nephrol. (2022) 54:1009–15. doi: 10.1007/s11255-022-03164-x
12. Bonkat, G, Cai, T, Veeratterapillay, R, Bruyère, F, Bartoletti, R, Pilatz, A, et al. Management of Urosepsis in 2018. Eur Urol Focus. (2019) 5:5–9. doi: 10.1016/j.euf.2018.11.003
13. Singer, M, Deutschman, CS, Seymour, CW, Shankar-Hari, M, Annane, D, Bauer, M, et al. The third international consensus definitions for Sepsis and septic shock (Sepsis-3). JAMA. (2016) 315:801–10. doi: 10.1001/jama.2016.0287
14. Liao, N, Tan, S, Yang, S, Zhai, GQ, Li, CY, Li, TY, et al. A study comparing dusting to basketing for renal stones ≤ 2 cm during flexible ureteroscopy. Int Braz J Urol. (2023) 49:194–201. doi: 10.1590/s1677-5538.ibju.2022.0382
15. Guan, Y, Ai, X, Li, Z, Teng, J, Ma, C, and Zhang, G. Early Warning Effect of CHR, NLR and U-HBP on SIRS in Patients with Upper Urinary Tract Calculus After Flexible Ureteroscopic Lithotripsy. Altern Ther Health Med. (2023) Online ahead of print.
16. Senocak, C, Ozcan, C, Sahin, T, Yilmaz, G, Ozyuvali, E, Sarikaya, S, et al. Risk factors of infectious complications after flexible Uretero-renoscopy with laser lithotripsy. Urol J. (2018) 15:158–63. doi: 10.22037/uj.v0i0.3967
17. Blackmur, JP, Maitra, NU, Marri, RR, Housami, F, Malki, M, and McIlhenny, C. Analysis of Factors' Association with risk of postoperative Urosepsis in patients undergoing Ureteroscopy for treatment of stone disease. J Endourol. (2016) 30:963–9. doi: 10.1089/end.2016.0300
18. On behalf of the CROES PCNL Study GroupGutierrez, J, Smith, A, Geavlete, P, Shah, H, Kural, AR, et al. Urinary tract infections and post-operative fever in percutaneous nephrolithotomy. World J Urol. (2013) 31:1135–40. doi: 10.1007/s00345-012-0836-y
19. Hatt, JK, and Rather, PN. Role of bacterial biofilms in urinary tract infections. Curr Top Microbiol Immunol. (2008) 322:163–92. doi: 10.1007/978-3-540-75418-3_8
20. Hansen, WL, van der Donk, CF, Bruggeman, CA, Stobberingh, EE, and Wolffs, PF. A real-time PCR-based semi-quantitative breakpoint to aid in molecular identification of urinary tract infections. PLoS One. (2013) 8:e61439. doi: 10.1371/journal.pone.0061439
21. Li, J, Jiang, F, Xie, A, and Jiang, Y. Analysis of the distribution and drug resistance of pathogens in patients with urinary tract infection in the eastern Chongming area of Shanghai from 2018 to 2020. Infect Drug Resist. (2022) 15:6413–22. doi: 10.2147/IDR.S384515
22. Yang, Z, Lin, D, Hong, Y, Hu, M, Cai, W, Pan, H, et al. The effect of preoperative urine culture and bacterial species on infection after percutaneous nephrolithotomy for patients with upper urinary tract stones. Sci Rep. (2022) 12:4833. doi: 10.1038/s41598-022-08913-7
23. Jia, P, Zhu, Y, Li, X, Kudinha, T, Yang, Y, Zhang, G, et al. High prevalence of extended-Spectrum Beta-lactamases in Escherichia coli strains collected from strictly defined community-acquired urinary tract infections in adults in China: a multicenter prospective clinical microbiological and molecular study. Front Microbiol. (2021) 12:663033. doi: 10.3389/fmicb.2021.663033
24. Ao, P, Shu, L, Zhang, Z, Zhuo, D, and Wei, Z. Levofloxacin: is it still suitable as an empirically used antibiotic during the perioperative period of flexible Ureteroscopic lithotripsy? A single-center experience with 754 patients. Urol J. (2020) 18:445–51. doi: 10.22037/uj.v16i7.6033
25. Sarti, M, Campanile, F, Sabia, C, Santagati, M, Gargiulo, R, and Stefani, S. Polyclonal diffusion of beta-lactamase-producing Enterococcus faecium. J Clin Microbiol. (2012) 50:169–72. doi: 10.1128/JCM.05640-11
26. Gajdács, M, Ábrók, M, Lázár, A, and Burián, K. Increasing relevance of gram-positive cocci in urinary tract infections: a 10-year analysis of their prevalence and resistance trends. Sci Rep. (2020) 10:17658. doi: 10.1038/s41598-020-74834-y
27. Gao, W, Howden, BP, and Stinear, TP. Evolution of virulence in Enterococcus faecium, a hospital-adapted opportunistic pathogen. Curr Opin Microbiol. (2018) 41:76–82. doi: 10.1016/j.mib.2017.11.030
28. Lin, WH, Kao, CY, Yang, DC, Tseng, CC, Wu, AB, Teng, CH, et al. Clinical and microbiological characteristics of Klebsiella pneumoniae from community-acquired recurrent urinary tract infections. Eur J Clin Microbiol Infect Dis. (2014) 33:1533–9. doi: 10.1007/s10096-014-2100-4
29. Chapelle, C, Gaborit, B, Dumont, R, Dinh, A, and Vallée, M. Treatment of UTIs due to Klebsiella pneumoniae Carbapenemase-producers: how to use new antibiotic drugs? Narrat Rev Antibiot. (2021) 10:10. doi: 10.3390/antibiotics10111332
30. Yin, D, Dong, D, Li, K, Zhang, L, Liang, J, Yang, Y, et al. Clonal dissemination of OXA-232 Carbapenemase-producing Klebsiella pneumoniae in neonates. Antimicrob Agents Chemother. (2017) 61:e00385-17. doi: 10.1128/AAC.00385-17
31. Yuan, F, Huang, Z, Yang, T, Wang, G, Li, P, Yang, B, et al. Pathogenesis of Proteus mirabilis in catheter-associated urinary tract infections. Urol Int. (2021) 105:354–61. doi: 10.1159/000514097
32. Armbruster, CE, Mobley, HLT, and Pearson, MM. Pathogenesis of Proteus mirabilis infection. EcoSal Plus. (2018) 8:8. doi: 10.1128/ecosalplus.esp-0009-2017
33. Verheij, TJM, and Platteel, TN. Looking for the optimal treatment of uncomplicated urinary tract infections. Lancet Infect Dis. (2020) 20:1001–2. doi: 10.1016/S1473-3099(20)30163-8
34. Degirmenci, T, Bozkurt, IH, Celik, S, Yarimoglu, S, Basmaci, I, and Sefik, E. Does leaving residual fragments after percutaneous nephrolithotomy in patients with positive stone culture and/or renal pelvic urine culture increase the risk of infectious complications? Urolithiasis. (2019) 47:371–5. doi: 10.1007/s00240-018-1063-9
35. Wu, Y, Wang, G, Huang, Z, Yang, B, Yang, T, Liu, J, et al. Diagnostic and therapeutic value of biomarkers in urosepsis. Ther Adv Urol. (2023) 15:175628722311518. doi: 10.1177/17562872231151852
36. Westerdijk, K, Simons, KS, Zegers, M, Wever, PC, Pickkers, P, and de Jager, CPC. The value of the neutrophil-lymphocyte count ratio in the diagnosis of sepsis in patients admitted to the intensive care unit: a retrospective cohort study. PLoS One. (2019) 14:e0212861. doi: 10.1371/journal.pone.0212861
Keywords: ureteral flexible lithotripsy, urine culture, Escherichia coli , urosepsis, urinary tract stones
Citation: Wang L, Yu X, Qiu Z, Liu P, Tian W, He W, Pan Y, Xu F, Cen Z, Ou Y and Li D (2024) Influence of preoperative urine culture and bacterial species on urogenital sepsis after ureteral flexible lithotripsy in patients with upper urinary tract stones. Front. Med. 11:1393734. doi: 10.3389/fmed.2024.1393734
Received: 29 February 2024; Accepted: 25 April 2024;
Published: 03 May 2024.
Edited by:
Sree Bhushan Raju, Nizam's Institute of Medical Sciences, IndiaReviewed by:
Panagiotis Mourmouris, National and Kapodistrian University of Athens, GreeceCopyright © 2024 Wang, Yu, Qiu, Liu, Tian, He, Pan, Xu, Cen, Ou and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Daobing Li, bGlkYW9iaW5nNjA4MEAxNjNxcS5jb20=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.