- 1Department of Anesthesiology, Shapingba District Hospital of Traditional Chinese Medicine, Chongqing, China
- 2Department of Anesthesiology, The Second Affiliated Hospital of Chongqing Medical University, Chongqing, China
Objective: To investigate the effects of perioperative general anesthesia (GA) and spinal anesthesia (SA) on postoperative rehabilitation in elderly patients with lower limb surgery.
Methods: This retrospective propensity score-matched cohort study included patients aged 65 years or older who underwent lower limb surgery between January 1, 2020, and May 31, 2023. The GA and SA were selected at the request of the orthopedic surgeon, patient, and their family members. The main outcomes included the incidence of the patient’s inability to self-care at discharge, postoperative complications including pulmonary infection, thrombus of lower extremity veins, infection of incisional wound and delirium, length of hospital stay, and incidence of severe pain in the first 2 days postoperatively.
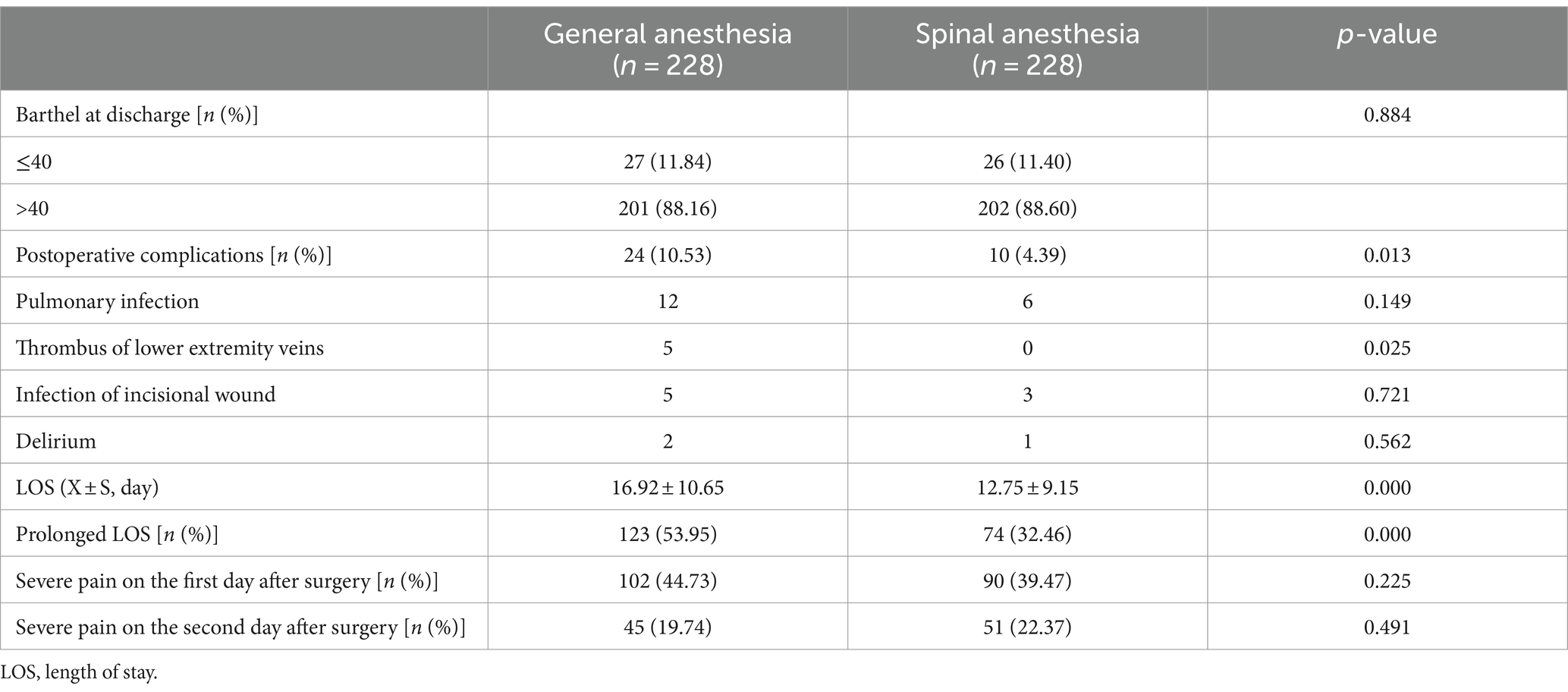
Results: In total, 697 patients met the inclusion criteria, and 456 were included in the final analysis after propensity score matching. In the GA and SA groups, 27 (11.84%) and 26 (11.40%) patients, respectively, could not care for themselves at discharge. The incidence rates did not differ between the groups (p = 0.884). In contrast, the incidence of postoperative complications (GA: 10.53% and SA: 4.39%; p = 0.013) and the length of hospital stay (GA: 16.92 ± 10.65 days and SA: 12.75 ± 9.15 days; p < 0.001) significantly differed between the groups.
Conclusion: The choice of anesthesia is independent of the loss of postoperative self-care ability in older patients (>65 years) and is not a key factor affecting postoperative rehabilitation after lower limb surgery. However, compared with GA, SA reduces the incidence of postoperative complications and a prolonged hospital stay. Thus, SA as the primary anesthetic method is a protective factor against a prolonged hospital stay.
1 Introduction
The global population is aging, and older adults are affected by bone loss and physical aging, making them vulnerable to lower limb fractures. Consequently, the proportion of hip fractures is increasing, with an estimated 2.6 million cases worldwide by 2025 (1), most of which are caused by falling. The prognosis of lower extremity fractures in older patients is usually poor for many reasons, such as advanced age, sex, and underlying diseases (cardiovascular and cerebrovascular diseases, frailty, and cognitive dysfunction). Lower limb fractures in this patient population require surgery to restore mobility and relieve pain.
Effective and successful surgeries require anesthesia, which provides pain relief during the procedure to ensure the operation is smooth and safe. However, surgery also puts the patient at risk for various complications, including infection, thrombosis in the lungs or legs, bedsores, urinary tract infections, and pneumonia. For older or frail adults, rehabilitation may take months, depending on the patient’s age, comorbidities, and postoperative pain, as well as infection. The choice of anesthesia affects patients’ intraoperative hemodynamics and cardiopulmonary function, affecting their prognosis. Therefore, anesthesia has been controversial for older patients with lower limb fractures (2–8), but how anesthesia affects postoperative rehabilitation remains unknown.
Therefore, this study investigated the effects of general anesthesia (GA) and spinal anesthesia (SA) on postoperative rehabilitation in older adults undergoing lower extremity surgery, such as their postoperative self-care ability, postoperative complications, and hospital stay, aiming to provide a reference for selecting the optimal anesthesia method for these patients.
2 Methods
2.1 Study design
This was a retrospective propensity-score-matched cohort study. The Ethics Committee of the Shapingba District Hospital of Chongqing Municipality approved this study No: (2024) (03), which was conducted following the Declaration of Helsinki. The confidentiality of patient data was guaranteed owing to the study’s retrospective nature.
2.2 Patients
Patients who underwent lower limb surgery at the Shapingba District Hospital of Traditional Chinese Medicine in Chongqing between January 1, 2020, and May 31, 2023, were selected. The inclusion criteria were: (1) patients undergoing elective lower limb surgery (including total hip replacement, lower limb fracture, internal fixation, debridement, and other lower limb surgeries) under GA and SA and (2) patients older than 65 years. The exclusion criteria were: (1) receiving local anesthesia, nerve block or intravenous anesthesia, (2) postoperative death, and (3) lack of data on self-care assessment.
2.3 Observational indicators
Patient data were obtained from the hospital’s electronic record system and the SA follow-up system. The general data collected in this study included demographic information, such as sex, age, preoperative comorbidities, the American Society of Anesthesiologists classification, the preoperative and discharge Barthel scores, preoperative routine blood markers, liver and renal function, the visual analog scale (VAS) scores for postoperative pain after 2 days and at discharge, and the length of hospital stay. Comorbidities included cardiovascular diseases (coronary heart disease, hypertension, and arrhythmia), nervous system diseases (cerebral infarction and Parkinson’s disease), respiratory diseases (chronic obstructive pulmonary disease, pulmonary infection, and bronchitis), and other diseases. Other information related to surgery included the operation duration, intraoperative use of pressure pressor (yes/no), postoperative analgesia (intravenous analgesia, controlled analgesia/ward load dose analgesia mode), and nerve block use.
The Barthel score was used to assess self-care at discharge. In this study, a total score of 40 indicated severe self-care dysfunction (i.e., the inability to care for themselves). A total score of 41–60 indicated that auxiliary care was required, and a score of >60 indicated mild dysfunction, and only partial care was required (9–11). The main study index was the incidence of a Barthel score below 40 at discharge. The VAS was used to assess postoperative pain. Scores ≥5 were defined as severe pain, and patients with a VAS score of ≥5 at any period after surgery were classified with severe postoperative pain. A hospital stay longer than 2 weeks was defined as a prolonged hospital stay and a surgical duration of more than 2 h was defined as prolonged surgery.
Finally, patients were divided into GA and SA groups, and the incidences of patients unable to take care of themselves at discharge, postoperative complications, and prolonged hospitalization were analyzed.
2.4 Sample size calculation
Statistical software PASS version 11.0 (Copyright 2011 NCSS, LLC) was used for the Sample size calculation. The main outcome of this study was the incidence of postoperative self-care. According to the results of previous literature (12), GA (48%) and SA (31%), a minimum of 258 evaluable patients (129 per arm) would be required to detect a difference between the two groups at p = 0.05 (2-tailed), with a power of 90%. Thus, the sample size is enough for the current study.
2.5 Statistical analyses
Statistical software SPSS version 26.0 (IBM Corp., Armonk, NY, United States) was used for the data analyses. Normally distributed measurement data were expressed as X ± S, and qualitative variables as the number of cases and percentages. Normally distributed continuous data were evaluated using independent sample t-tests, non-normally distributed measurement data were analyzed with the Mann–Whitney U test and expressed as M (P25, P75), and qualitative data were analyzed with X for qualitative data2 checkout. p-values of <0.05 indicated statistical significance.
To address possible confounders, propensity-score matching (PSM) was used to validate the study rationale and methods. To investigate the predictors of postoperative rehabilitation, univariate and multivariate logistic regression analyses were performed for postoperative self-care ability, postoperative complications, and prolonged hospital stay. Variables with p-values <0.05 in the univariate analysis were used in the multivariate analysis. In addition to anesthesia, the model included age, sex, comorbidities, length of hospitalization, postoperative analgesia, combined nerve block, and routine preoperative blood test indicators.
3 Results
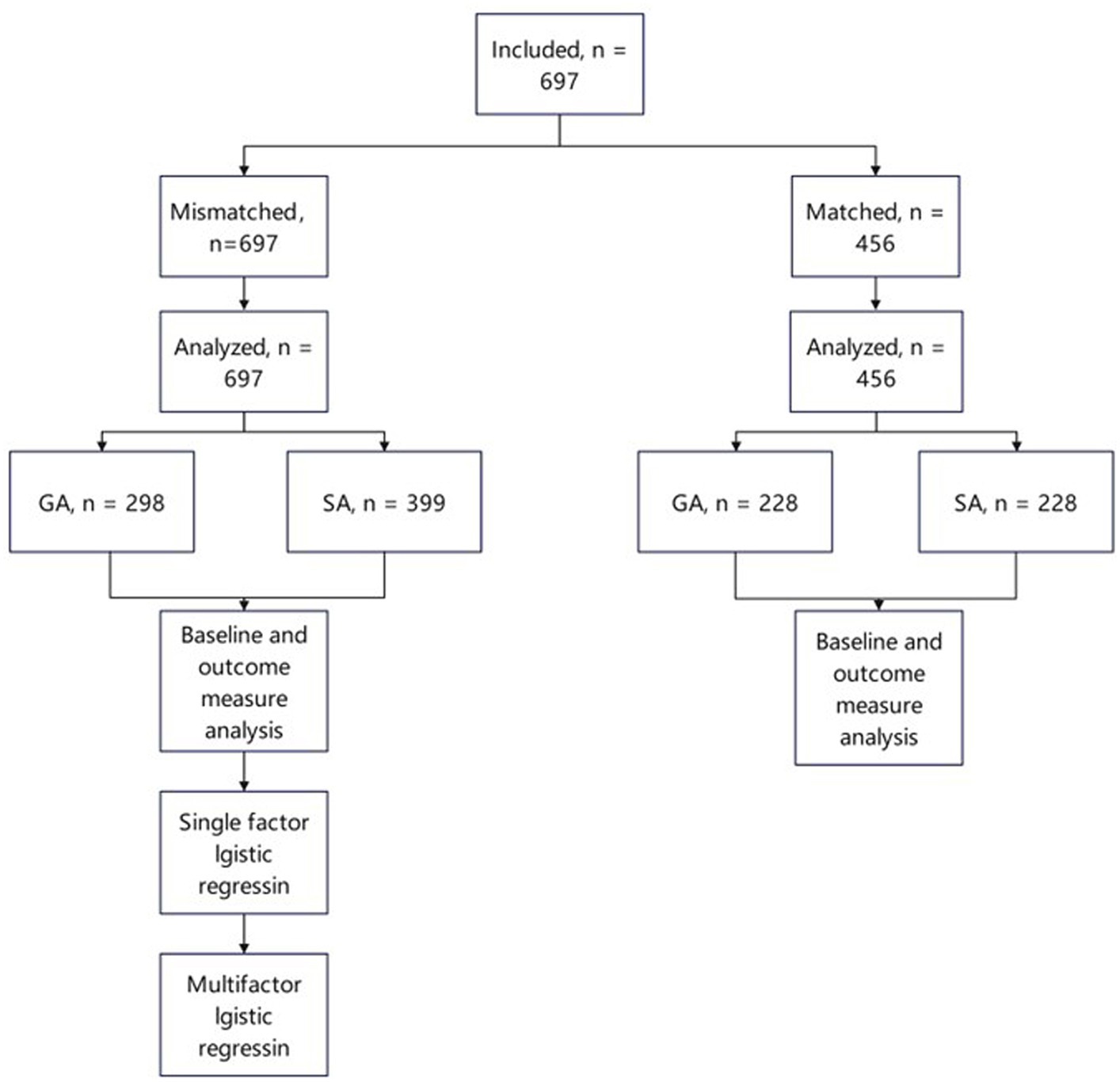
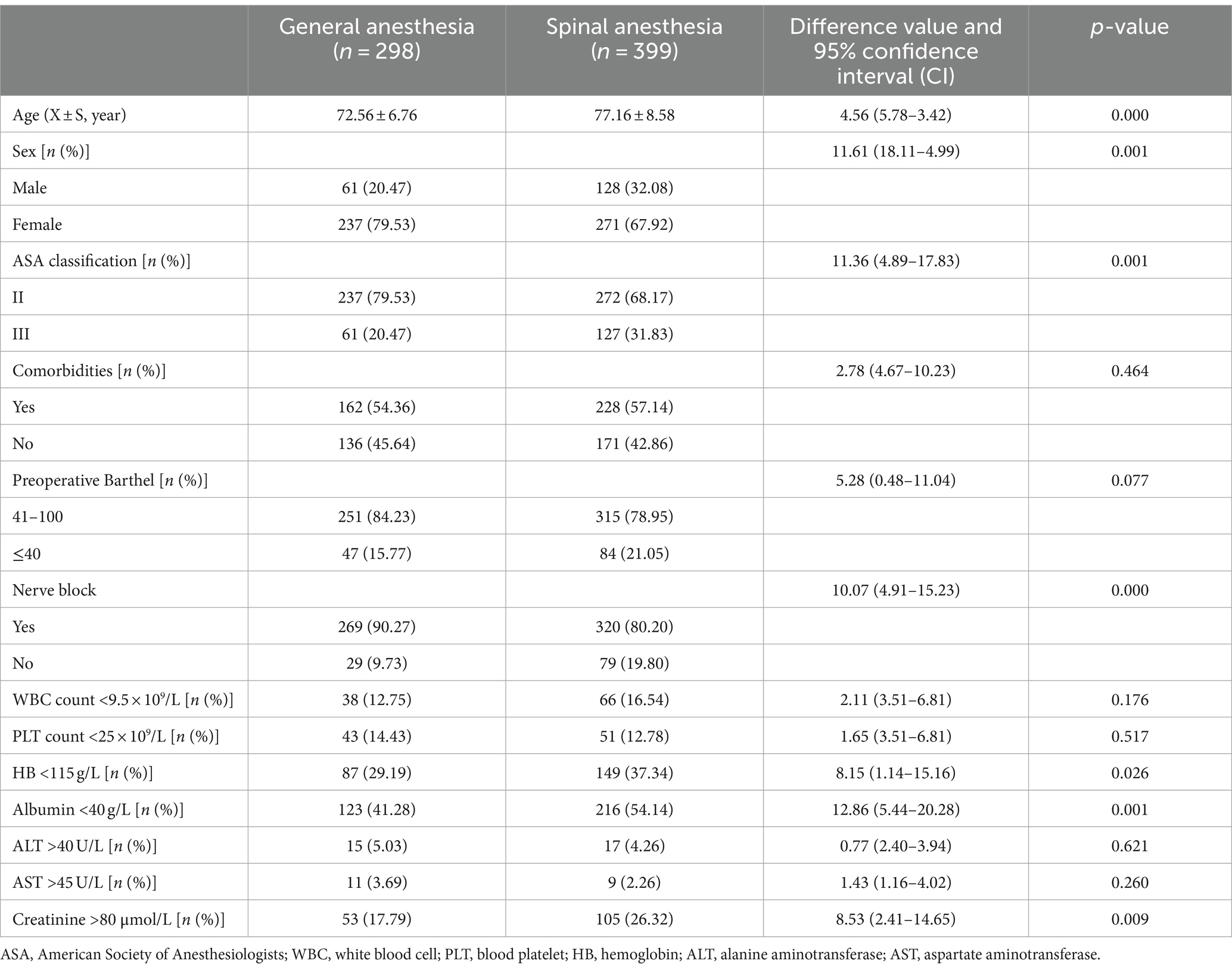
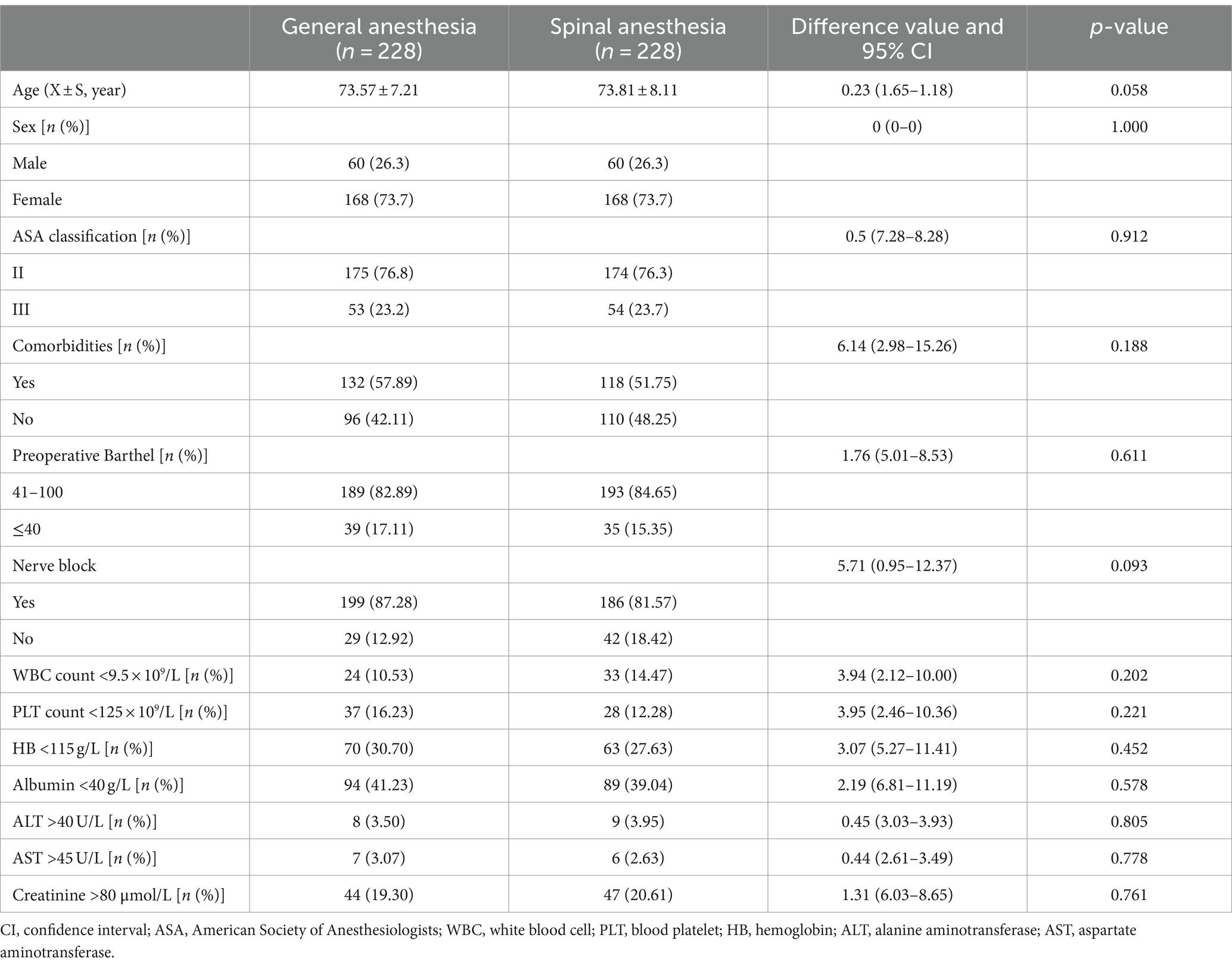
Figure 1 presents a flowchart of the participant selection process. In total, 697 patients met the inclusion criteria. Before PSM, the baseline data for age (p < 0.001), sex (p = 0.001), and combined nerve block (p < 0.001) were unbalanced between the groups. Therefore, PSM (caliper value = 0.02) was used to reduce selection bias and potential baseline differences between the GA and SA groups. After PSM, the distributions of the background variables were well-balanced, and 456 patients were included in the analysis. Tables 1, 2 detail the baseline comparisons before and after matching, respectively.
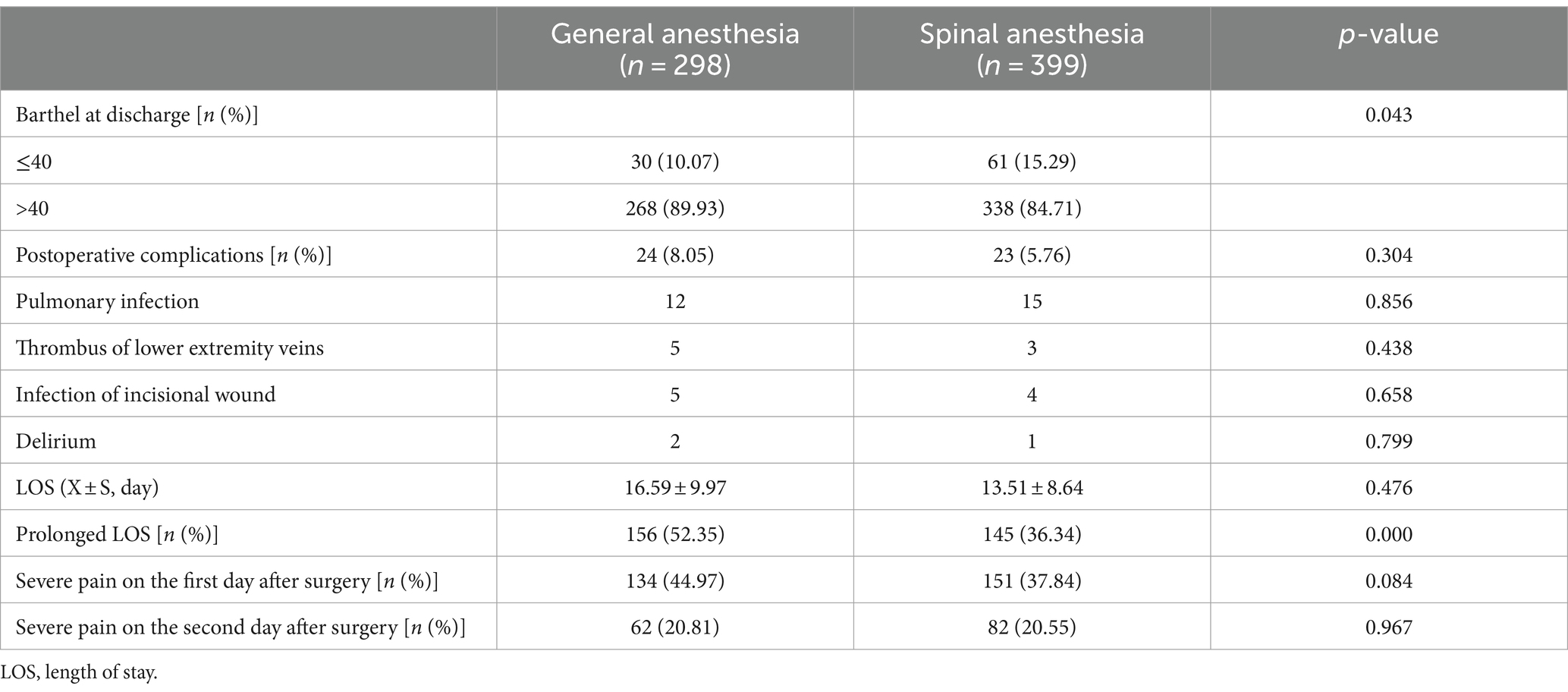
After PSM, 27 (11.84%) and 26 (11.40%) patients in the GA and SA groups, respectively, were unable to care for themselves at discharge; the incidence rate did not differ between the groups (p = 0.884). In contrast, the incidence of postoperative complications (e.g., pulmonary infection, lower limb venous thrombosis, incision infection, and postoperative delusion) (GA: 10.53% and SA: 4.39%; p = 0.013) and length of hospital stay (GA: 16.92 ± 10.65 days and SA: 12.75 ± 9.15 days; p < 0.001) significantly differed between the groups. The VAS scores 2 days postoperatively and on the day of discharge did not differ between the groups (p > 0.05). Thus, the anesthesia method was independent of the incidence of self-care dysfunction at discharge, prolonged hospital stay, and the rate of postoperative complications. The use of intravenously controlled analgesia varied greatly after surgery; however, there was an incidence of severe pain on the first day and the day of discharge (Tables 3, 4).
The univariate analysis demonstrated that postoperative self-care ability was associated with increased age [0.122 years, 95% confidence interval (CI): 0.069 to 0.214, p < 0.05], comorbidities (2.389, 95% CI: 1.440 to 3.962, p < 0.05), anesthesia method (0.620, 95% CI: 0.389 to 0.998, p < 0.05), preoperative Barthel score (12.833, 95% CI: 7.843 to 20.998, p < 0.001), patient-controlled intravenous analgesia (PCIA; 1.980, 95% CI: 1.163 to 3.373, p < 0.05), nerve block (3.552, 95% CI: 1.395 to 8.893, p < 0.05), decreased platelet (PLT) count (2.186 × 109/L, 95% CI: 1.267 to 3.773, p < 0.05), decreased hemoglobin (HB) levels (4.718 g/L, 95% CI: 2.955 to 7.531, p < 0.001), and decreased albumin levels (0.153 g/L, 95% CI: 0.086 to 0.273, p < 0.001). Increased age (0.395 years, 95% CI: 0.200 to 0.778, p < 0.05), preoperative Barthel score (6.692, 95% CI: 3.910 to 11.542, p < 0.001), decreased PLT count (1.999 × 109/L, 95% CI: 1.022 to 3.907, p < 0.05), decreased HB levels (1.938 g/L, 95% CI: 1.117 to 3.360, p < 0.05), and decreased albumin levels (0.323 g/L, 95% CI: 0.169 to 0.617, p < 0.05) were associated with postoperative self-care ability in the multivariate analysis. Therefore, age and normal albumin levels were protective factors, and the inability to self-care preoperatively, a low PLT count, and anemia were risk factors for the inability to self-care postoperatively (Figure 2).
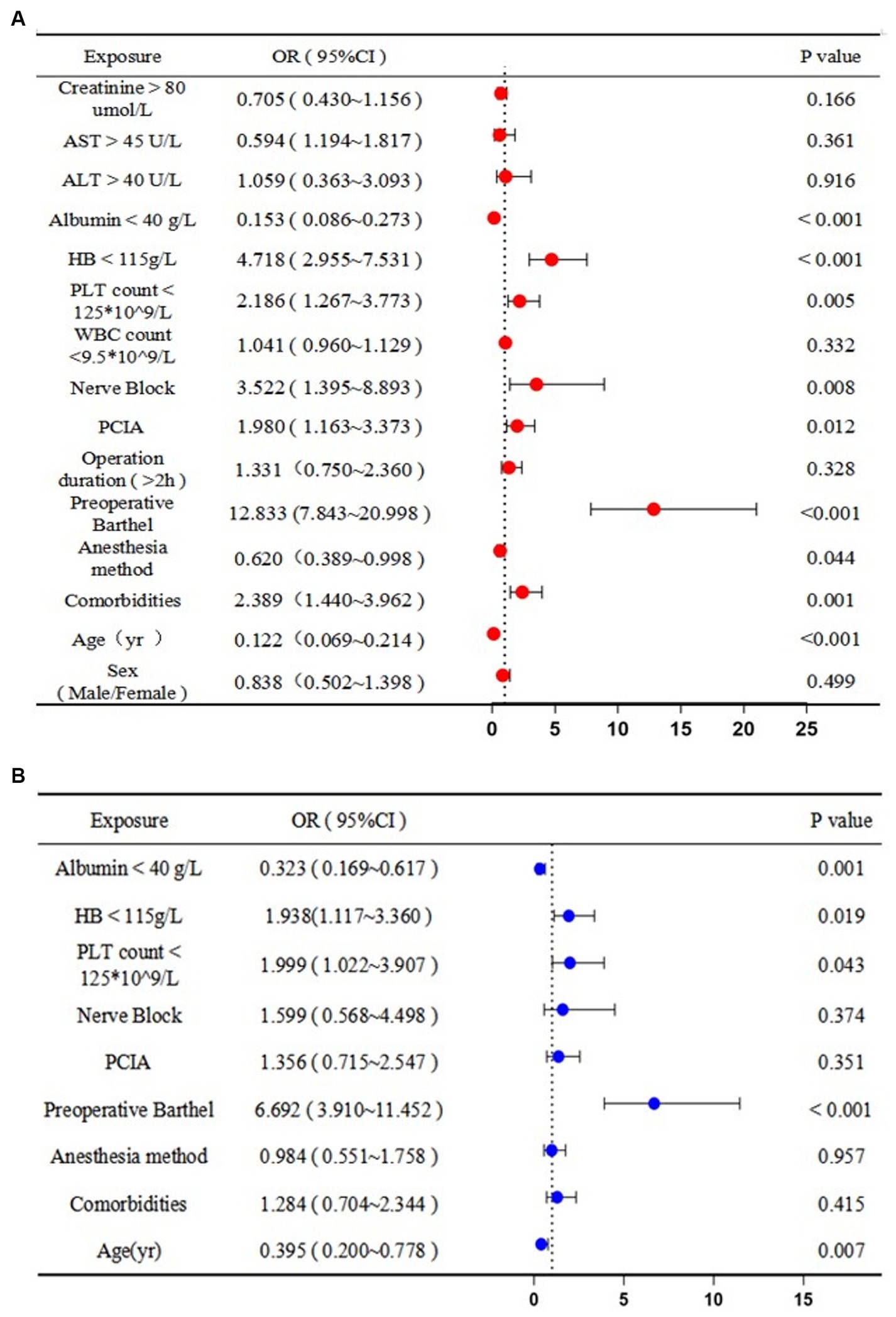
Figure 2. Predictors of postoperative disability (i.e., inability to self-care): (A) univariate and (B) multivariate logistic regression analyses. OR, odds ratio; CI, confidence interval; AST, aspartate aminotransferase; ALT, alanine aminotransferase; HB, hemoglobin; PLT, platelet; WBC, white blood cell; PCIA, patient-controlled intravenous analgesia.
The univariate analysis demonstrated that postoperative complications were associated with increased age (0.286 years, 95% CI: 0.150 to 0.546, p < 0.001), preoperative Barthel score (3.597, 95% CI: 1.948 to 6.641, p < 0.001), operation duration >2 h (0.454 h, 95% CI: 0.243 to 0.848, p < 0.05), increased white blood cell (WBC) count (0.427 × 109/L, 95% CI: 0.217 to 0.840, p < 0.05), decreased albumin levels (0.342 g/L, 95% CI: 0.177 to 0.660, p < 0.05), and increased creatinine levels (0.448 μmol/L, 95% CI: 0.241 to 0.830, p < 0.05). Increased age (0.474 years, 95% CI: 0.228–0.983, p < 0.05), preoperative Barthel score (2.126, 95% CI: 1.068–4.230, p < 0.05), operation duration >2 h (0.354 h, 95% CI: 0.183–0.688, p < 0.05), and WBC count (0.481 × 109/L, 95% CI: 0.235–0.985, p < 0.05) were associated with postoperative complications in the multivariate analysis. Therefore, younger age, an operative time of less than 2 h, and a normal WBC count were protective factors, and the inability to self-care preoperatively was a risk factor for postoperative complications (Figure 3).
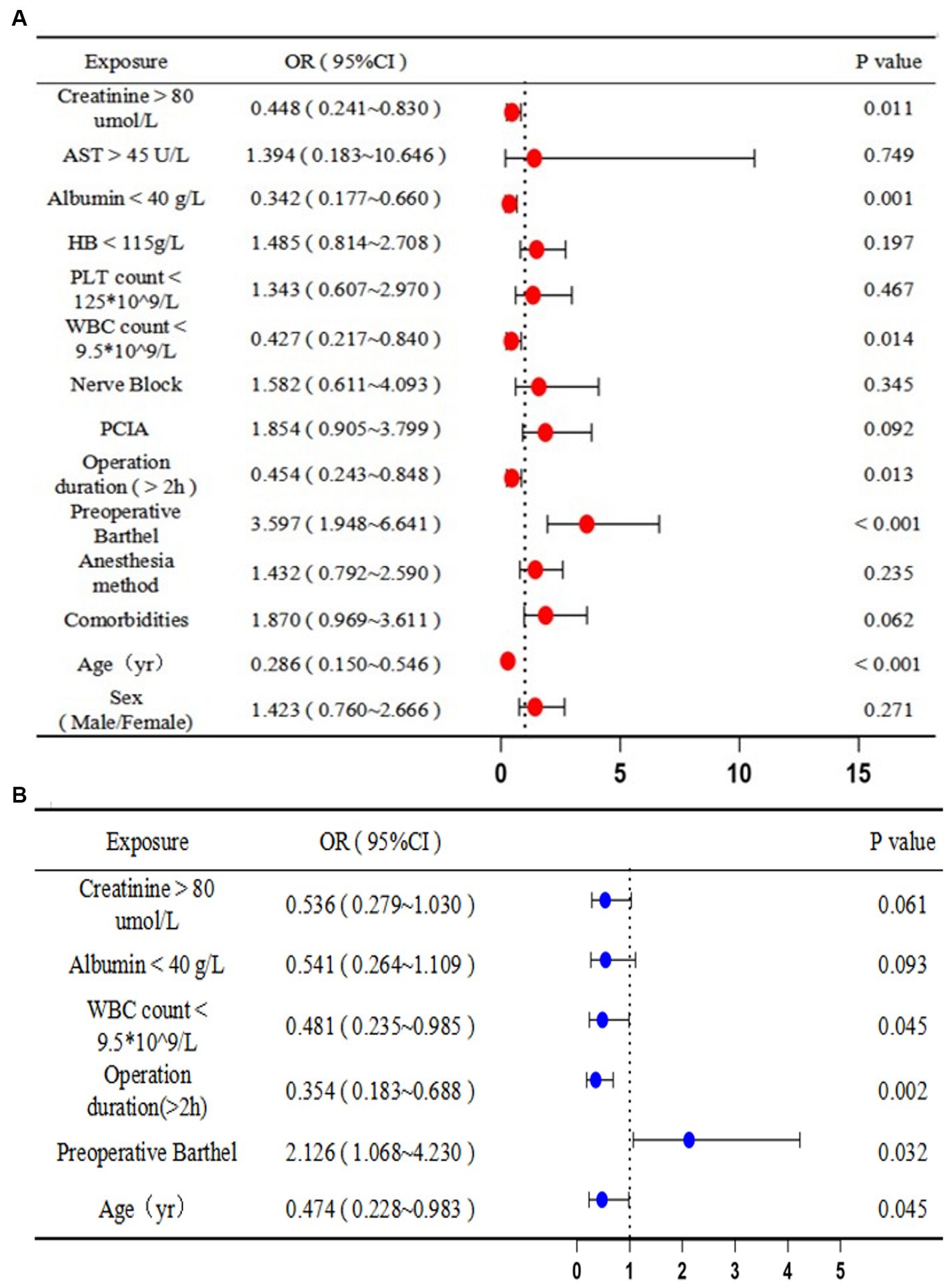
Figure 3. Predictors of postoperative complications: (A) univariate and (B) multivariate logistic regression analyses. OR, odds ratio; CI, confidence interval; AST, aspartate aminotransferase; ALT, alanine aminotransferase; HB, hemoglobin; PLT, platelet; WBC, white blood cell; PCIA, patient-controlled intravenous analgesia.
The univariate analysis demonstrated that prolonged hospital stay was associated with increased age (1.561 years, 95% CI: 1.152 to 2.116, p < 0.05), comorbidities (0.559, 95% CI: 0.410 to 0.763, p < 0.001), anesthesia method (0.520, 95% CI: 0.383 to 0.705, p < 0.001), preoperative Barthel score (0.557, 95% CI: 0.380 to 0.817, p < 0.05), operation duration >2 h (4.179 h, 95% CI: 2.828 to 6.175, p < 0.001), PCIA (0.341, 95% CI: 0.242 to 0.483, p < 0.001), nerve block (0.383, 95% CI: 0.241 to 0.610, p < 0.001), decreased HB level (0.696 g/L, 95% CI: 0.507 to 0.955, p < 0.05), and decreased albumin level (1.818 g/L, 95% CI: 1.342 to 2.464, p < 0.001). Comorbidities (0.672, 95% CI: 0.475 to 0.950, p < 0.05), anesthesia method (0.680, 95% CI: 0.467 to 0.991, p < 0.05), operation duration >2 h (3.225 h, 95% CI: 2.092 to 4.971, p < 0.001), PCIA (0.475, 95% CI: 0.325 to 0.693, p < 0.001), and decreased albumin levels (1.676 g/L, 95% CI: 1.170 to 2.401, p < 0.05) were associated with prolonged hospital stay in the multivariate analysis. Therefore, the absence of comorbidities, anesthetic method, and postoperative use of PCIA were protective factors, and a surgery duration longer than 2 h and low preoperative albumin levels were risk factors for a prolonged hospital stay (Figure 4).
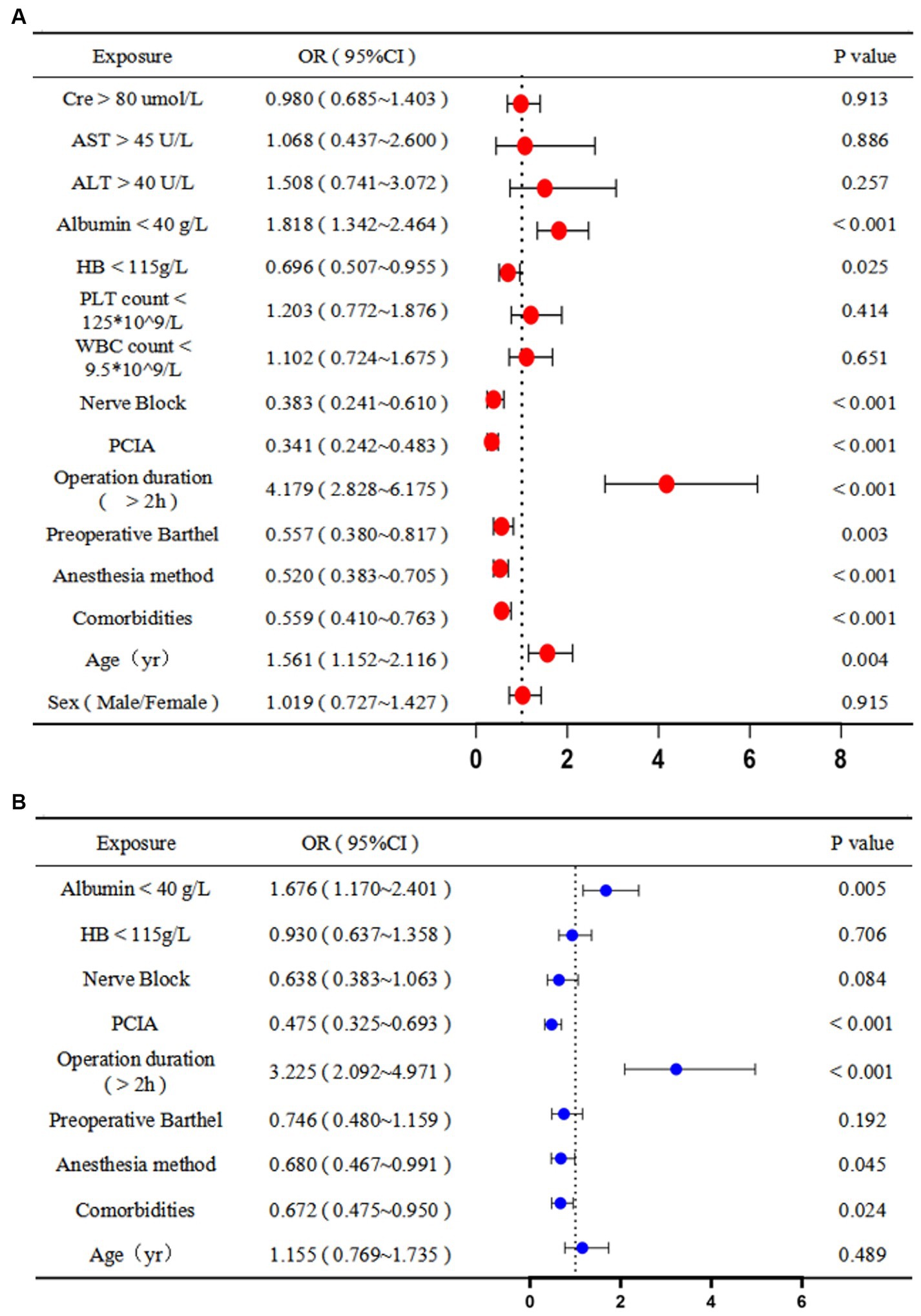
Figure 4. Predictors of prolonged hospital stay: (A) univariate and (B) multivariate logistic regression analyses. OR, odds ratio; CI, confidence interval; AST, aspartate aminotransferase; ALT, alanine aminotransferase; HB, hemoglobin; PLT, platelet; WBC, white blood cell; PCIA, patient-controlled intravenous analgesia.
4 Discussion
As society advances, the proportion of adults over the age of 65 years in China is increasing. According to a survey, there are currently approximately 280 million older adults in China, accounting for approximately 17.5% of the total population (13). However, physical and organ function gradually declines with age, and older individuals often develop various diseases, negatively affecting postoperative recovery. The choice of anesthesia can also affect recovery in older patients; therefore, selecting the appropriate method for this patient population is crucial for promoting recovery and reducing pain.
GA and SA are commonly used for lower limb fractures, and their effects on patients after hip fracture and total knee replacement surgeries have been investigated (14–17). However, the sample sizes of those studies were small, and no studies have explored how GA and SA affect self-care ability and length of stay in older patients. We found that the anesthesia method did not contribute to the loss of postoperative self-care ability in patients over age 65 years. However, we found that SA reduced the incidence of postoperative complications compared to GA and that SA was a protective factor against a prolonged hospital stay. And reducing postoperative complications and hospitalization time are important indicators for accelerating postoperative rehabilitation. There are studies have reported that SA may be associated with a reduced incidence of postoperative complications, including death, deep vein thrombosis, pulmonary complications, and myocardial infarction (2, 3, 12, 15, 18), which aligns with our results.
Selection bias is an obvious limitation of observational studies, resulting in unreliable results if improperly addressed. Logistic regression and PSM are two common statistical methods for reducing selection bias. PSM is a data processing method used to control for confounding factors in observational and retrospective studies and is often used in orthopedic studies (19). This study included 697 patients based on the inclusion and exclusion criteria. However, certain characteristics (e.g., age, sex, and nerve block use) significantly differed between the two groups prior to PSM. However, after PSM, 456 patients were included, and significant differences in the general or preoperative data were not observed between the two groups. Subsequently, logistic regression was used to analyze and predict the factors affecting postoperative rehabilitation.
This study has some limitations. First, only patients who underwent lower limb surgery were included, and the anesthesia method was mainly GA with a spinal nerve block; the type of nerve block medication and nerve block needle nor the type or dose of systemic anesthesia or SA were assessed. Therefore, the applicability of these results for patients receiving other types of anesthesia remains to be clarified. Second, we did not collect data on several variables that may affect the results, such as body mass index, although a high body mass index has been associated with surgical site infection after total hip replacement (20). We also did not collect postoperative routine blood test data despite an independent association between a neutrophil-to-lymphocyte ratio of >10.5 and severe pain within 48 h postoperatively (21).
Although this study cannot definitively support one mode of anesthesia over another, the results highlight each method’s relative risks and benefits, especially SA, which was a protective factor against a prolonged length of stay. Overall, these results provide objective evidence for selecting an anesthesia method for lower limb surgery to encourage rapid postoperative recovery.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics Committee of the Shapingba District Hospital of Chongqing Municipality. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because this was a retrospective propensity-score-matched cohort study. The manuscript presents research on animals that do not require ethical approval for their study.
Author contributions
GL: Data curation, Investigation, Validation, Writing – original draft. QM: Data curation, Formal analysis, Writing – original draft. YL: Data curation, Writing – original draft. FT: Data curation, Writing – original draft. XL: Data curation, Investigation, Writing – original draft. JC: Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors wish to acknowledge JC for his help with technical and practical considerations for administration.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Gullberg, B, Johnell, O, and Kanis, JA. World-wide projections for hip fracture. Osteoporos Int. (1997) 7:407–13. doi: 10.1007/PL00004148
2. Zhou, S-L, Zhang, S-Y, Si, H-B, and Shen, B. Regional versus general anesthesia in older patients for hip fracture surgery: a systematic review and meta-analysis of randomized controlled trials. J Orthop Surg Res. (2023) 18:428. doi: 10.1186/s13018-023-03903-5
3. Luger, TJ, Kammerlander, C, Gosch, M, Luger, MF, Kammerlander-Knauer, U, Roth, T, et al. Neuroaxial versus general anaesthesia in geriatric patients for hip fracture surgery: does it matter? Osteoporos Int. (2010) 21:S555–72. doi: 10.1007/s00198-010-1399-7
4. Neuman, MD, Feng, R, Ellenberg, SS, Sieber, F, Sessler, DI, Magaziner, J, et al. Pain, analgesic use, and patient satisfaction with spinal versus general anesthesia for hip fracture surgery: a randomized clinical trial. Ann Intern Med. (2022) 175:952–60. doi: 10.7326/M22-0320
5. McIsaac, DI, Wijeysundera, DN, Huang, A, Bryson, GL, and van Walraven, C. Association of hospital-level neuraxial anesthesia use for hip fracture surgery with outcomes: a population-based cohort study. Anesthesiology. (2018) 128:480–91. doi: 10.1097/ALN.0000000000001899
6. Guay, J, Parker, MJ, Gajendragadkar, PR, and Kopp, S. Anaesthesia for hip fracture surgery in adults. Cochrane Database Syst Rev. (2016) 2:CD000521. doi: 10.1002/14651858.CD000521.pub3
7. Neuman, MD, Silber, JH, Elkassabany, NM, Ludwig, JM, and Fleisher, LA. Comparative effectiveness of regional versus general anesthesia for hip fracture surgery in adults. Anesthesiology. (2012) 117:72–92. doi: 10.1097/ALN.0b013e3182545e7c
8. Nordström, P, Gustafson, Y, Michaëlsson, K, and Nordström, A. Length of hospital stay after hip fracture and short term risk of death after discharge: a total cohort study in Sweden. BMJ. (2015) 350:h696. doi: 10.1136/bmj.h696
9. Ryg, J, Engberg, H, Mariadas, P, Pedersen, SGH, Jorgensen, MG, Vinding, KL, et al. Barthel index at hospital admission is associated with mortality in geriatric patients: a Danish nationwide population-based cohort study. Clin Epidemiol. (2018) 10:1789–800. doi: 10.2147/CLEP.S176035
10. Mahoney, FI, and Barthel, DW. Functional evaluation: the BARTHEL index. Md State Med J. (1965) 14:61–5.
11. Mahoney, FI, Wood, OH, and Barthel, DW. Rehabilitation of chronically ill patients: the influence of complications on the final goal. South Med J. (1958) 51:605–9. doi: 10.1097/00007611-195805000-00011
12. Fukuda, T, Imai, S, Shimoda, S, Maruo, K, Nakadera, M, and Horiguchi, H. Aspiration pneumonia and anesthesia techniques in hip fracture surgery in elderly patients: a retrospective cohort study using administrative data. J Orthop Surg. (2022) 30:10225536221078622. doi: 10.1177/10225536221078622
13. Liqing, X. The domestic elderly population has reached 280 million aging and accelerated. China Bus News. (2023):D03. doi: 10.38300/n.cnki.nzgjy.2023.002580
14. Leibold, C, Falbo, R, Gupta, A, Miller, R, Pederson, JM, and Malpe, M. A systematic review and meta-analysis of anesthesia type on hip fracture post-surgery outcomes. OTA Int. (2022) 5:e204. doi: 10.1097/OI9.0000000000000204
15. Fields, AC, Dieterich, JD, Buterbaugh, K, and Moucha, CS. Short-term complications in hip fracture surgery using spinal versus general anaesthesia. Injury. (2015) 46:719–23. doi: 10.1016/j.injury.2015.02.002
16. Berninger, MT, Friederichs, J, Leidinger, W, Augat, P, Bühren, V, Fulghum, C, et al. Effect of local infiltration analgesia, peripheral nerve blocks, general and spinal anesthesia on early functional recovery and pain control in total knee arthroplasty. BMC Musculoskelet Disord. (2018) 19:232. doi: 10.1186/s12891-018-2154-z
17. Büttner, B, Mansur, A, Hinz, J, Erlenwein, J, Bauer, M, and Bergmann, I. Combination of general anesthesia and peripheral nerve block with low-dose ropivacaine reduces postoperative pain for several days after outpatient arthroscopy: a randomized controlled clinical trial. Medicine. (2017) 96:e6046. doi: 10.1097/MD.0000000000006046
18. Guo, L-S, Wang, L-N, Xiao, J-B, Zhong, M, and Zhao, GF. Association between anesthesia technique and complications after hip surgery in the elderly population. World J Clin Cases. (2022) 10:2721–32. doi: 10.12998/wjcc.v10.i9.2721
19. Kane, LT, Fang, T, Galetta, MS, Goyal, DKC, Nicholson, KJ, Kepler, CK, et al. Propensity score matching: a statistical method. Clin Spine Surg. (2020) 33:120–2. doi: 10.1097/BSD.0000000000000932
20. Liu, X, Dong, Z, Li, J, Feng, Y, Cao, G, Song, X, et al. Factors affecting the incidence of surgical site infection after geriatric hip fracture surgery: a retrospective multicenter study. J Orthop Surg Res. (2019) 14:382. doi: 10.1186/s13018-019-1449-6
Keywords: general anesthesia, spinal anesthesia, Barthel score, older adults, lower limb surgery
Citation: Li G, Ma Q, Li Y, Tan F, Li X and Chen J (2024) Effects of general and spinal anesthesia on postoperative rehabilitation in older adults after lower limb surgery: a retrospective cohort study. Front. Med. 11:1386797. doi: 10.3389/fmed.2024.1386797
Reviewed by:
Qi Chen, Chongqing University, ChinaJiaoli Sun, Huazhong University of Science and Technology, China
Sheng Jing, Second Affiliated Hospital of Army Medical University, China
Edited by:
Zongbin Song, Central South University, ChinaCopyright © 2024 Li, Ma, Li, Tan, Li and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jie Chen, MzA1MDQ1QGhvc3BpdGFsLmNxbXUuZWR1LmNu
†These authors have contributed equally to this work and share first authorship
 Guifei Li1†
Guifei Li1† Jie Chen
Jie Chen