- 1School of Public Health, Lanzhou University, Lanzhou, China
- 2Department of Public Health, Lanzhou Second People’s Hospital, Lanzhou, China
- 3Department of Ophthalmology, Baiyin Second People's Hospital, Baiyin, China
Background: Myopia is a significant public health problem across the globe. This study aimed to examine the regional disparity in prevalence and correlated factors of myopia in children and adolescents in two typical regions, Gannan Tibetan Autonomous Prefecture (Gannan Prefecture for short, a Tibetan residential area) and Wuwei City (a Han residential area) in Gansu Province, China, and to provide a reference for the prevention and control of regional myopia.
Methods: The study was a cross-sectional study of children and adolescents in Gansu Province, China. A total of 6,187 (Wuwei City: 3,266, Gannan Tibetan Autonomous Prefecture: 2,921) students were selected by stratified cluster sampling. Eye examinations and questionnaires were administered to the participants. Myopia is defined as a condition in which the spherical equivalent refractive error of an eye is less than or equal to −0.50 D when ocular accommodation is relaxed. The χ2 test and multivariate logistic regression analysis were used to analyze the correlated factors of myopia.
Results: The myopia rate of 6,187 students was 71.4%, and students had a higher rate of myopia (77.5%) in Wuwei City compared to Gannan Prefecture (64.6%) (p < 0.001). The results of multivariate analysis in Wuwei City showed that girls (odds ratio (OR) = 1.325), junior students (OR = 2.542), senior students(OR = 4.605), distance between eyes and book less than one foot (OR = 1.291), and parents with myopia (one, OR = 2.437; two, OR = 4.453) had higher risks of myopia (all, p < 0.05). For Gannan Prefecture, girls (OR = 1.477), senior students (OR = 1.537), daily time spent doing homework ≥2 h (OR = 1.420), the distance between eyes and book less than one foot (OR = 1.205), mean time continuous eye use (0.25–<0.5 h, OR = 1.345, 0.5–<1 h, OR = 1.317, ≥1 h, OR = 1.313), average daily sleep duration <8 h (OR = 1.399), and parents with myopia (one, OR = 1.852; two, OR = 2.913) had higher risks of myopia (all, p < 0.05).
Conclusion: The prevalence of myopia is at a relatively high level in Gansu Province. The prevalence and risk factors for myopia vary by region.
1 Introduction
Myopia is currently widely recognized as a significant public health issue causing significant visual loss and a risk factor for a range of other serious ocular conditions (1). Myopia can increase the risk of eye complications such as myopic macular degeneration, retinal detachment, and open-angle glaucoma (2). Myopia also imposes a heavy economic burden. It is estimated that the global productivity loss due to uncorrected refractive errors amounts to $202 billion per year (3).
Myopia is a significant public health problem across the globe. In recent years, there has been a significant increase in the number of cases of myopia globally. It was estimated that 22.9% of the world’s population had myopia in 2020, and it is projected to double in prevalence by the year 2050 (4). Myopia has become a health problem affecting children and adolescents. The prevalence of myopia has been shown to vary widely with geographic location. For example, in Germany from 2014 to 2017, the prevalence of myopia among children and adolescents 0 to 17 years of age was 11.4% (5). Myopia was found in 3.7% of children aged 6–7 years old and 22.8% of children aged 12–13 years old in Ireland (6). However, the level of myopia in Asian countries is considerably higher in East and Southeast Asia. For example, the prevalence rates of myopia were 76.5% among elementary school students and 94.9% among junior high school students (7), 64.6% of children aged 5–18 years old in Korea (8), and 81.2% of children aged 16–18 years old in China (9). Multiple measures and much effort have been taken to curb the prevalence of myopia.
One important measure to enable the effective prevention of myopia is understanding the modifiable risk factors. The high prevalence of myopia is associated with a variety of factors. Previous studies indicated that a family history of myopia is important in myopia occurrences, with an estimated adjusted OR of 2.83 [95% confidence interval (95%CI), 2.47–3.24] in children with two myopic parents compared to no parental myopia in China (10); especially for high myopia, the additive genetic portion remained roughly constant at approximately 60% in South Korea (11). Environmental factors also play a role in the etiology of myopia (12). For example, associations between time outdoors and less myopia were stronger and more consistently observed; daily outdoor time of 120 to 150 min at 5,000 lux/min or cumulative outdoor light intensity of 600,000 to 750,000 lux significantly reduced the incidence risk ratio of myopia by 15% ~ 24% in Shanghai, China (13, 14).
A previous study showed that myopia displayed a regionalization feature, and the incidence of myopia in Gansu Province was at the middle level in China (15). Gansu Province, located in northwest China, is a multi-ethnic populated area. The population of Gansu Province is mainly Han, in addition, there are also 53 other ethnic groups, such as Tibetans. Wang et al. (16) found that prevalence and risk factors for myopia varied between Han and Yugur older adults in Gansu Province. Therefore, we speculate whether there are different factors affecting myopia among primary and secondary school students in different ethnic residential areas in Gansu Province. Based on this, Gannan Tibetan Autonomous Prefecture (Gannan Prefecture for short, a Tibetan residential area) and Wuwei City (a Han residential area) were selected. The purpose of the present study was to examine the variability of prevalence and associated risk factors of myopia in children and adolescents from the Han and Tibetan residential regions. Identification of modifiable correlative factors of myopia in different population settings may help provide a reference for the regional eye health intervention.
2 Materials and methods
2.1 Participants
This is a cross-sectional survey in Gansu Province. Gansu Province is located in the west of China. There are 55 ethnic groups in Gansu Province, with the Han being the main ethnic group. Tibetans are one of the most populous ethnic minorities. In this study, we selected two typical survey areas: (1) Gannan Prefecture and (2) Wuwei City. Gannan Prefecture is located in the southwest of Gansu Province, where the ethnic composition is mainly Tibetan, Han, Hui, and Tu, and the Tibetan population accounts for more than half of Gannan Prefecture. Wuwei City is located in the central of Gansu Province, with a majority Han population an epidemiological investigation was conducted in the two survey areas during 2020. The stratified cluster sampling method was adopted. First, schools were stratified by urban/rural status, and by elementary/junior/senior status, where we randomly selected 22 schools, including 6 senior high schools, 8 junior high schools, and 8 elementary schools from these two regions. Second, a total of 6,271 students from grades four to six in elementary school, grades seven to nine in junior high schools, and grades one to three in senior high schools were selected as a whole class from the 22 schools. These 6,271 students underwent myopia screening and questionnaire survey. We excluded students with eye diseases other than refractive defects or those who underwent eye surgery. After exclusion, 6,187 (98.7%) students were selected to participate in the study: 3,266 from Wuwei City and 2,921 from Gannan Prefecture. This study was approved by the Ethics Committee of the School of Basic Medical Sciences, Lanzhou University (No: jcyxy20200325), with the consent of students and their guardians, and all information was strictly confidential.
2.2 Eye examinations and determination of myopia
Eye examinations of all participants by qualified optometrists from Baiyin Second People’s Hospital. First, a 5-meter standard logarithmic visual acuity chart is used for the examination of distant vision. The right eye’s visual acuity was first measured, followed by the left eye. Second, refractive error was carried out to all participants. The international consensus for defining myopia in epidemiological studies suggests that myopia is defined as a condition in which the spherical equivalent refractive error (SE) of an eye is ≤ −0.50 D when ocular accommodation is relaxed (1). Low myopia is defined as a condition in which the SE of an eye is ≤ −0.50 D and > −6.00 D when ocular accommodation is relaxed (1). High myopia is defined as a condition in which the SE of an eye is ≤ −6.00 D when ocular accommodation is relaxed (1). Pre-myopia is defined as a condition in which the SE of an eye is ≤ +0.75 D and > −0.50 D in children where a combination of baseline refraction, age, and other quantifiable risk factors provide a sufficient likelihood of the future development of myopia to merit preventative interventions (1). However, there is evidence of a high correlation between non-cycloplegic and cycloplegic refraction tests in myopia screening, and The China National Health Commission recommends the use of non-cycloplegic for vision screening in schools (17, 18). Therefore, refractive error was measured using an automatic refractometer (VS100, Welch Allyn, Jiangsu, China) when ocular accommodation was non-relaxation. Before the refractive examination, the instrument was placed in a stable environment. During the refractive examination, participants were asked to focus on the vision screen until an aperture appeared on the gray screen. After the inspection, the result was automatically output by the instrument. SE is the sum of the spherical value plus half the cylindrical value.
2.3 Questionnaire
We designed a self-administered questionnaire based on “the work plan of monitoring and intervention of common diseases and health effects among students in 2020 in Gansu Province,” normative guidelines, and similar previous studies (17, 19, 20). The questionnaire included three parts: (1) Basic information: residential district, name of school, age, gender (boy, girl), ethnicity (Han, Tibetan, other ethnic), education level (elementary, junior, senior), daytime outdoor activity hours, average daily sleep duration, and parental history of myopia (neither, one, two); (2) ocular behaviors and environment: frequency of daily eye exercises (zero, one time, two, or more times), recess activity space (inside the teaching building, outdoor), daily time spent doing homework, distance between eyes and book more than one feet (never, occasionally, often, always), teachers emphasizing proper reading and writing posture (never, occasionally, often, always), reading while reclined or lying down (never, occasionally, often, always), daily time spent using computer, mean time between continuous eye use (less than 15 min, 15 min–<30 min, 30 min–< 60 min, 60 min, or more), and previous diagnosis or treatment of eye diseases other than refractive defects. The questionnaires were administered to the students and their parents or legal guardians by trained investigators from September to November 2020. Before filling in the questionnaire, the investigators met with the students, their parents, or legal guardians, and explained what the questionnaires were about and how to fill out the questionnaire. The students and their parents or legal guardians discussed the study and gave their consent.
2.4 Statistical analysis
The data were statistically analyzed by SPSS 18.0 software. The χ2 test was used to compare the difference in demographic characteristics and the prevalence of myopia stratified by region. Variables, which have a p-value of less than 0.05 in the univariate analysis of myopia, were selected and evaluated by multivariate logistic regression models. The results of multivariate logistic regression are presented with ORs and 95%CIs. Every statistical test was two-sided, and a p-value of less than 0.05 was regarded as statistically significant.
3 Results
3.1 Characteristics of study participants
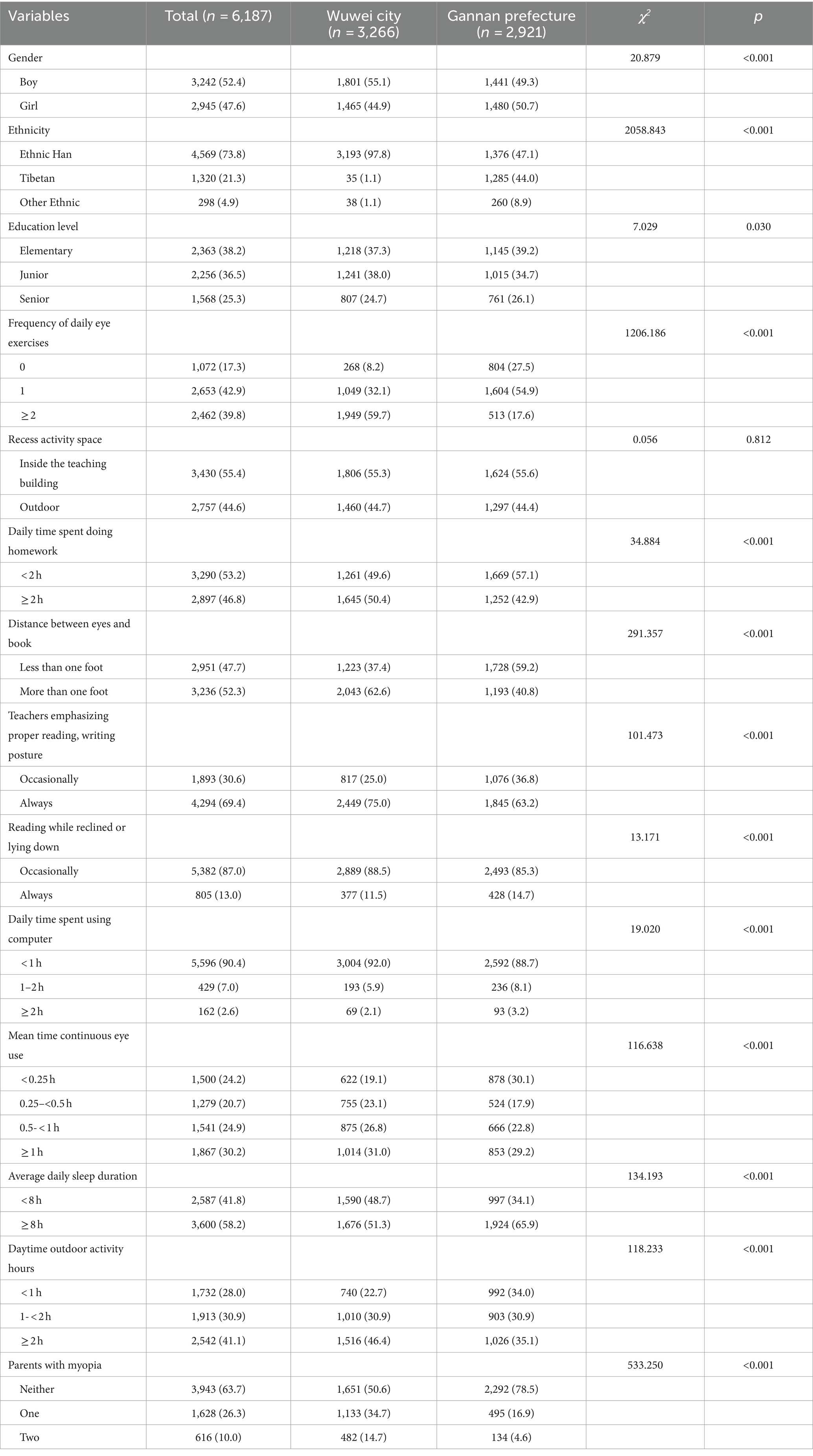
The demographic characteristics stratified by region are described in Table 1. Statistically significant differences between regional groups were observed in the gender, ethnicity, education level, frequency of daily eye exercises, daily time spent doing homework, the distance between eyes and book, teachers emphasizing proper reading, writing posture, reading while reclined or lying down, daily time spent using a computer, mean time continuous eye use, average daily sleep duration, daytime outdoor activity hours, and parental history of myopia (all, p < 0.05).
3.2 Univariate analysis of myopia
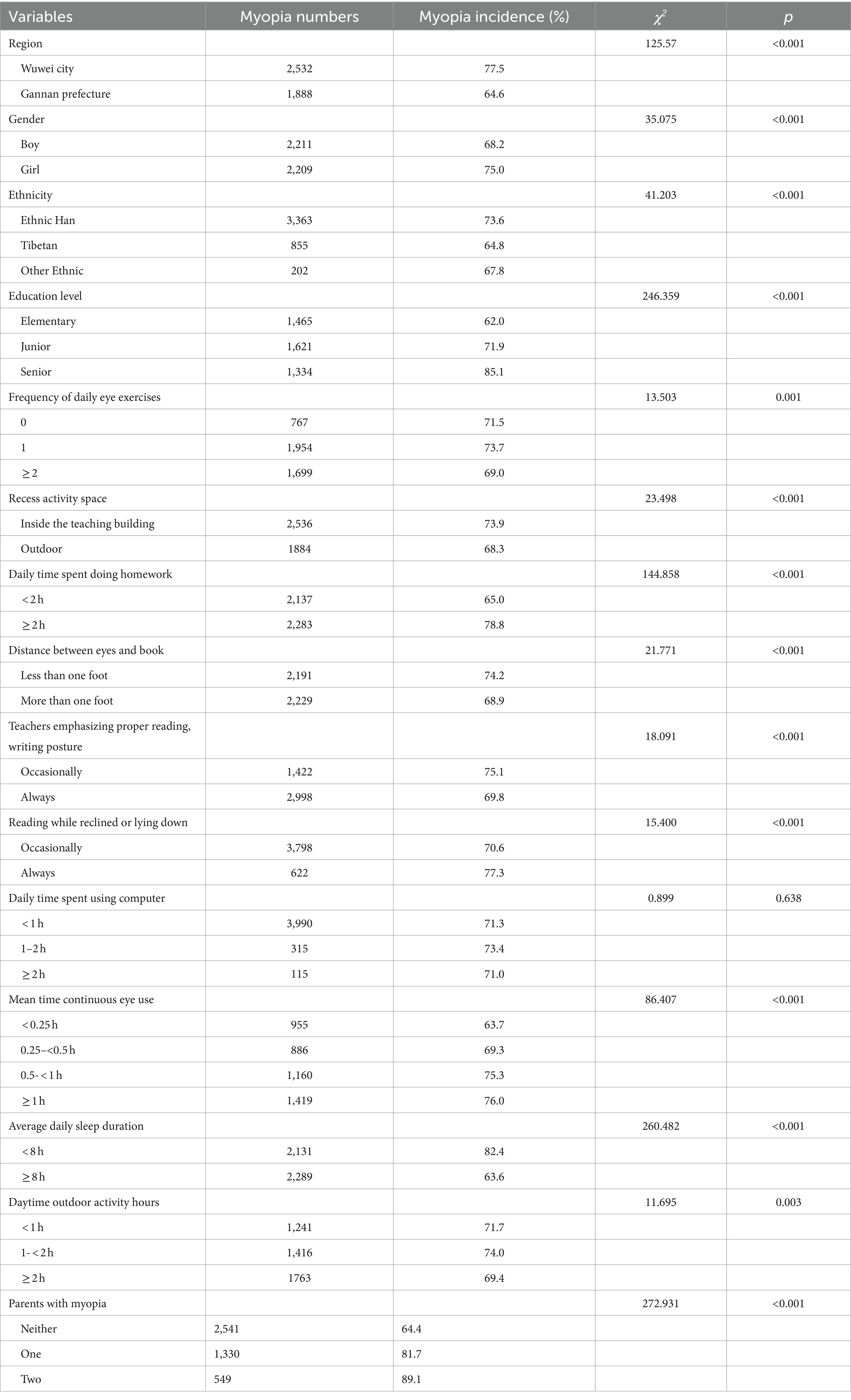
The prevalence rate of myopia was 71.4% (4,420/6187) for all participants. The univariate analysis of myopia for all participants is shown in Table 2. Statistically significant differences were observed in factors such as region, gender, ethnicity, education level, recess activity space, daily time spent doing homework, the distance between eyes and book, teachers emphasizing proper reading, writing posture, reading while reclined or lying down, mean time continuous eye use, average daily sleep duration, daytime outdoor activity hours, and parental history of myopia (all, p < 0.05).
Univariate analysis of myopia stratified by region is shown in Table 3. In the two regions, statistically significant differences were all observed in factors such as gender, education level, frequency of daily eye exercises, recess activity space, daily time spent doing homework, distance between eyes and book, mean time continuous eye use, average daily sleep duration, and parental history of myopia (all, p < 0.05). However, factors such as teachers emphasizing proper reading, writing posture, reading while reclined or lying down, daily time spent using a computer, and daytime outdoor activity hours were associated with myopia only in Wuwei City (all, p < 0.05).
Figures 1, 2 show the prevalence of myopia of different basic characters and different ocular behaviors of students in the two regions, respectively. The results showed that the myopia rates were higher in Wuwei City than those in Gannan Prefecture, and there were statistical differences in myopia rates of other groups between the two regions except primary school students and other ethnic students.
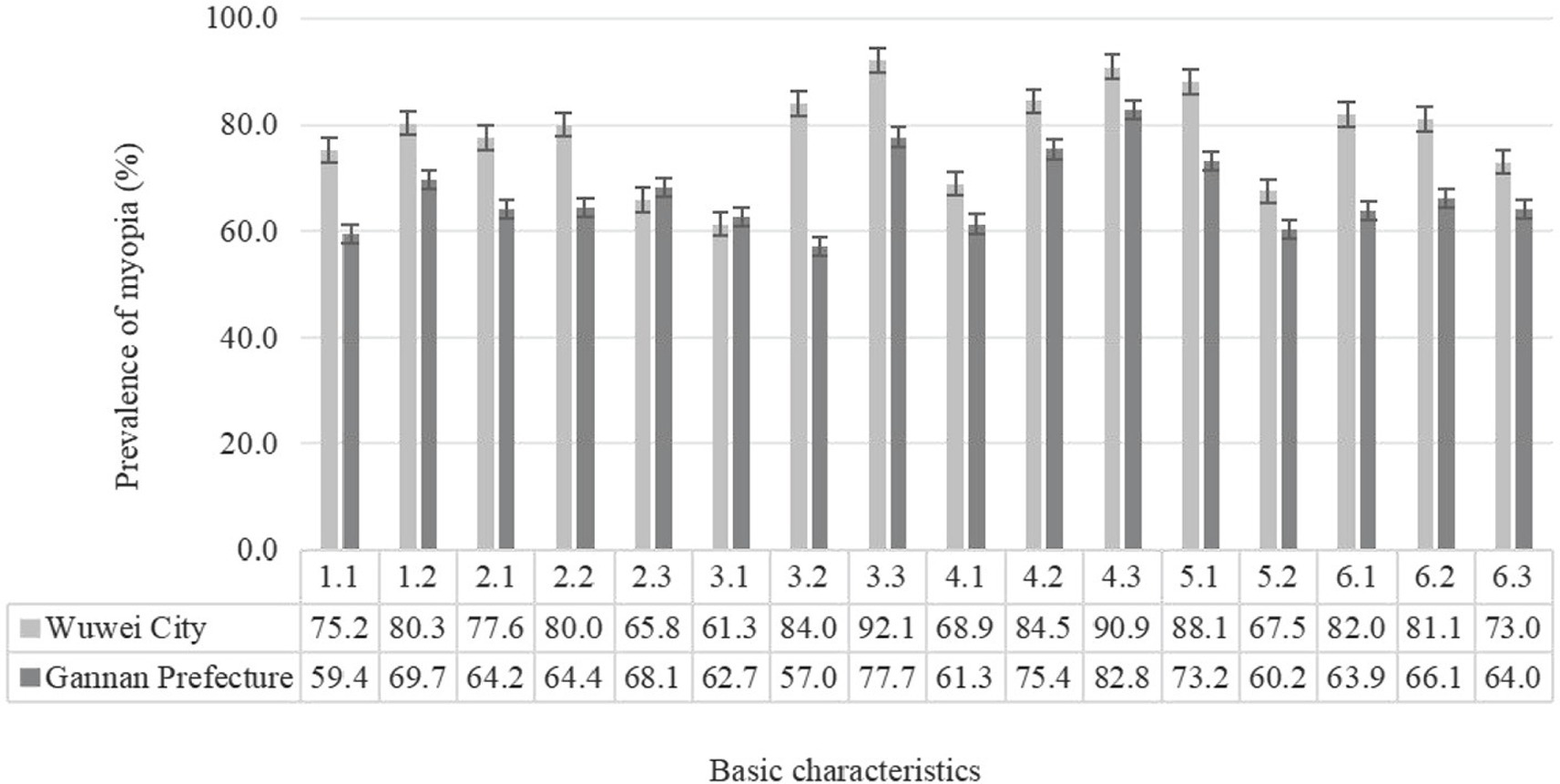
Figure 1. Prevalence of myopia of different basic characters students in the two regions (%). 1.1, Boys; 1.2, girls; 2.1, ethnic han; 2.2, Tibetan; 2.3, other ethnic; 3.1, elementary; 3.2, junior; 3.3, senior; 4.1, no parental myopia; 4.2, father or mother with myopia; 4.3, parents with myopia; 5.1, average daily sleep duration < 8 h; 5.2, average daily sleep duration ≥ 8 h; 6.1, daytime outdoor activity < 1; 6.2, daytime outdoor activity 1–2 h; 6.3, daytime outdoor activity ≥2 h.
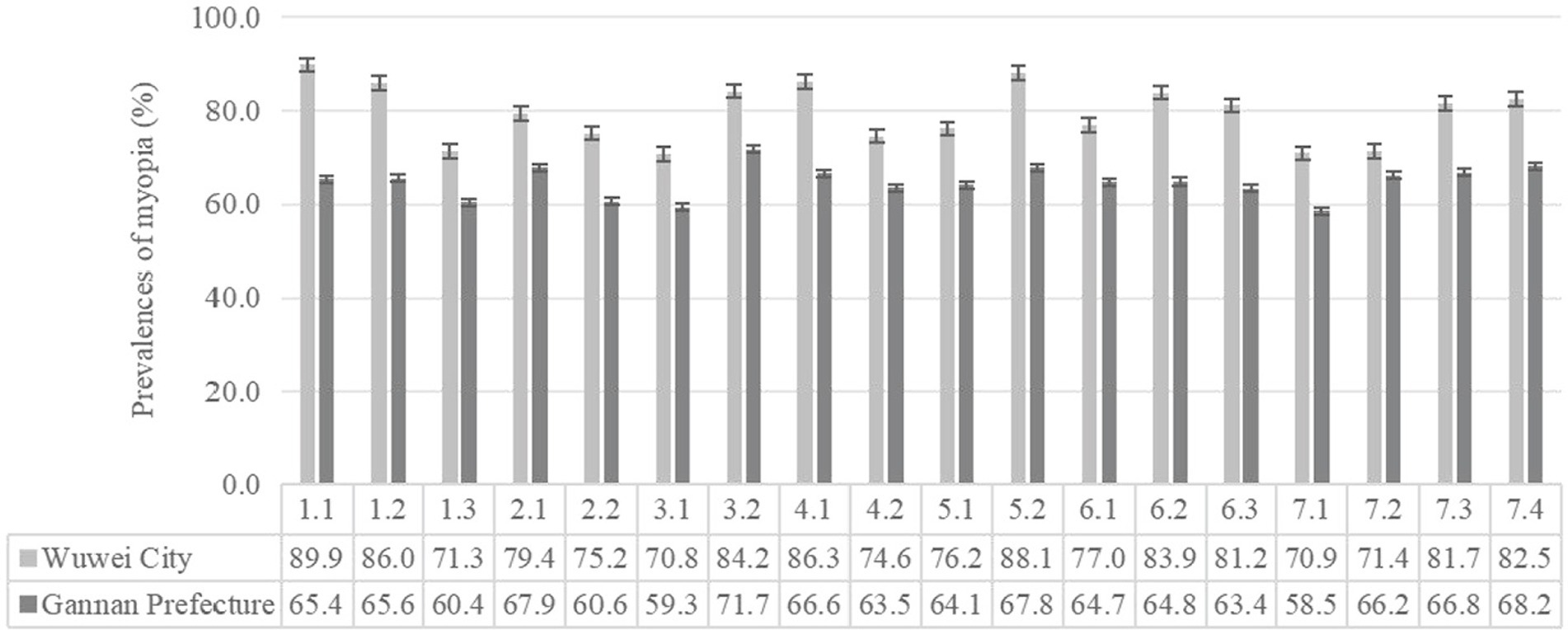
Figure 2. Prevalence of myopia of different ocular behaviors students in the two regions (%). 1.1, doing eye exercises 0 time/d; 1.2, doing eye exercises 1 time/d; 1.3, doing eye exercises ≥2 times/d; 2.1, recess in the teaching building; 2.2, recess outdoor; 3.1, daily time spend doing homework < 2 h; 3.2, daily time spend doing homework ≥2 h; 4.1, distance between eyes book less than one foot; 4.2, distance between eyes book more than one foot; 5.1, reading occasionally while reclined or lying down; 5.2, reading always while reclined or lying down; 6.1, daily time spend using computer < 1 h; 6.2, daily time spend using computer 1–2 h; 6.3, daily time spend using computer ≥2 h; 7.1, mean time continuous eye use < 0.25 h; 7.2, mean time continuous eye use 0.25–0.5 h; 7.3, mean time continuous eye use 0.5–1 h; 7.4, mean time continuous eye use ≥1 h.
3.3 Multivariate analysis of myopia
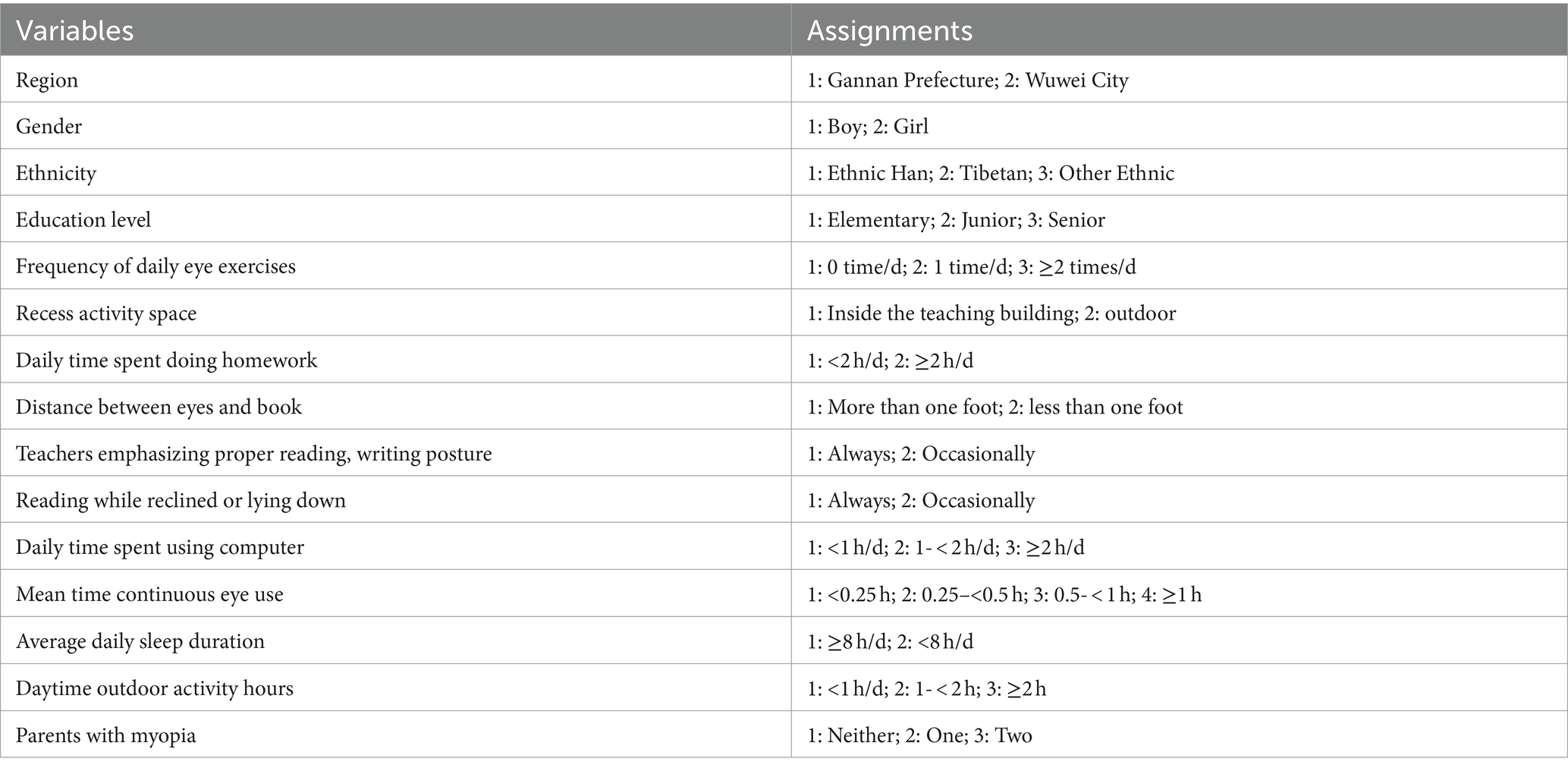
With myopia as a dependent variable (0, no, 1, yes), factors with statistical significance in the results of the univariate analysis were included as covariates in the multivariate logistic regression model for analysis. The backward deletion method is used to screen covariates, and α = 0.10 is the criterion for removing covariates. The covariables and assignments in logistic regression analysis are shown in Table 4. After adjustment of confounding variables that were significant in the corresponding univariate analysis, the results of multivariate analysis are shown in Table 5.
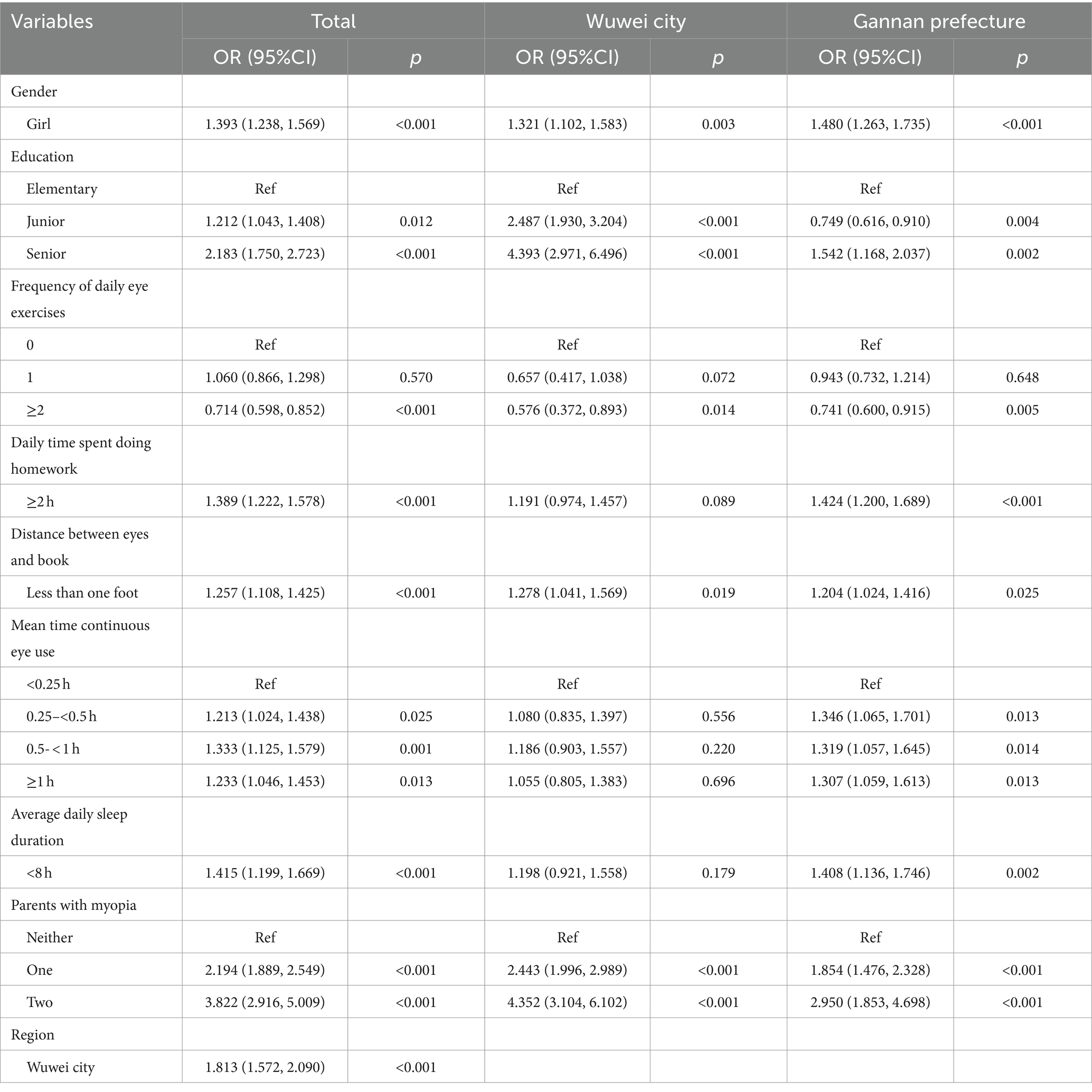
For the whole participants, compared to their respective references, Wuwei City students, girls, junior and senior students, daily time spent doing homework ≥2 h, the distance between eyes and book less than one foot, mean time continuous eye use ≥0.25 h, average daily sleep duration <8 h, and parents with myopia had higher risks of myopia. However, doing daily eye exercises two or more times had a lower risk of myopia (all, p < 0.05).
For the participants from Gannan Prefecture, the influencing factors of myopia were consistent with the whole group. For the participants in Wuwei City, the factors affecting myopia only included girls, junior students, senior students, distance between eyes and books less than one foot, and parents with myopia doing daily eye exercises two or more times (all, p < 0.05).
4 Discussion
This study investigated myopia status and its correlated factors in children and adolescents in two typical regions in Gansu Province, China. Our results suggested that there was a relatively high prevalence of myopia in Gansu. The multivariate analysis showed some factors, which included gender, education, heredity, and environmental factors, correlated with myopia. When stratified by region, the results also showed the regional disparity in prevalence and correlated factors of myopia.
According to the current study, the prevalence of myopia in Gansu (71.4%) was higher than the levels of Asia (60%) and North America (42%) (21), and the results also displayed the regional disparity in prevalence of myopia. Myopia has become an important health problem for children and adolescents in Gansu. Identifying the factors related to myopia, which vary by region, is crucial for reducing its incidence and promoting population health.
Previous studies showed that heredity might play an important role in myopia (22). Rathi et al. (23) reported that the proportion was 30.1, 19.3%, and 13.% among children with myopia in two parents, mother and father, in North India, respectively. Lim et al. (10) reported an OR (2.83) in children with two myopic parents compared to no parental myopia. The current study also showed the importance of parental myopia for the myopia of students. For the whole participants, a father or mother with myopia (OR = 2.194) and parents with myopia (OR = 3.822) had higher risks of myopia with no parental myopia, and these ORs were higher in Wuwei City than those of Gannan Prefecture. The regional differences of these ORs may correlate to the proportion of parental myopia in the two regions. The proportion of parental myopia was 49.4% among students in Wuwei City, while was only 21.5% in Gannan Prefecture. Research from Japan found that longer axial length (AL) or higher AL to the corneal radius of curvature (AL/CR) was significantly associated with parental myopia (24). While AL and AL/CR could be used as obtainable indicators for identifying subjects at high risk of developing premyopia and myopia in young preschool children (25). It has been suggested that students with a family history of myopia should be prioritized for intervention to prevent and manage myopia onset and progression from an early age.
The results of our study indicated the difference in gender and education levels of myopia. The risk of myopia was higher among girls than that of boys and increased with grade level, which was consistent with the findings of other studies (26–28). Possible reason, one aspect may involve the physiological differences in AL and corneal curvature (CR) among children of different genders and ages. As age progresses, AL tends to increase, and girls typically exhibit a deeper CR compared to boys (29). As discussed earlier (25), an increase in AL, deeper CR, and a combination of these changes in AL/CR were associated with myopia. However, this inference could be attributed to not performing revision under cycloplegia (24). Another possibility could be the influence of environmental factors.
In addition to genetics, the environment can also influence the development of myopia. Zhang et al. (30) found that genetic factors may play a role of 12.5%, while environmental factors may play a role of 87.5% in the formation of myopia, which suggests that environmental factors play an essential role in myopia. In the present study, we found that environmental factors, which included time spent on homework, incorrect reading and writing posture, mean time between continuous eye use, doing eye exercises, and average daily sleep were correlated with myopia.
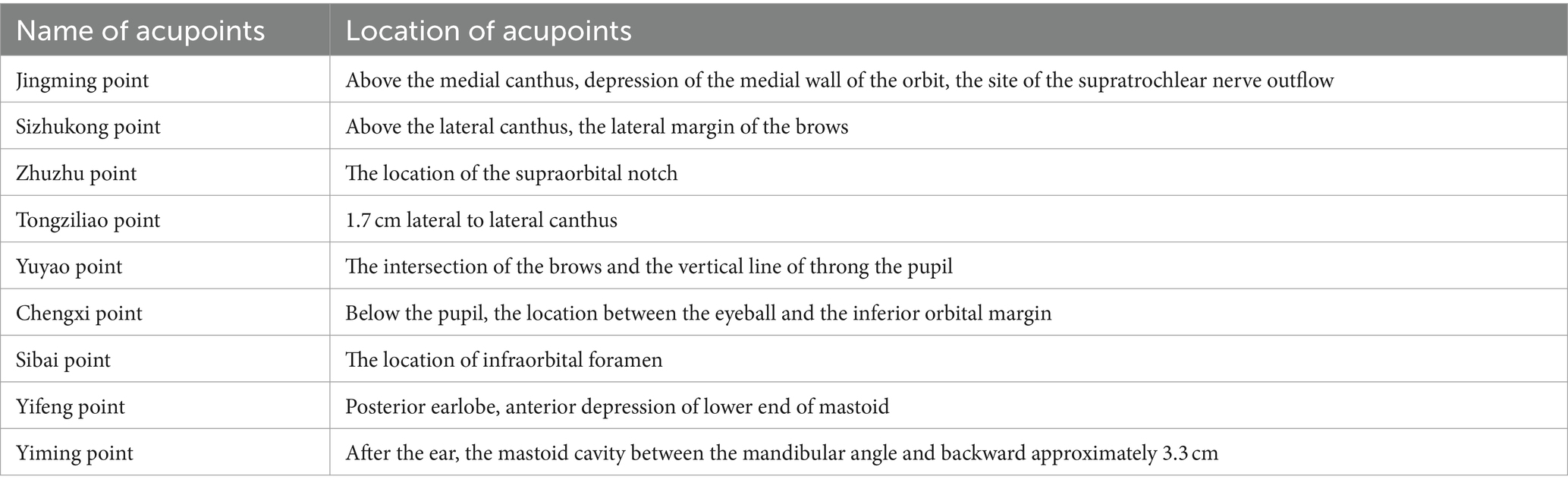
The findings in this study indicated that the risks of myopia were higher among the students who spent less than 2 h compared to those with more than 2 h of homework. There may be three possible explanations for these findings. First, the homework burden increases with grades, which may lead to a reduction in exercise time. Previous studies had confirmed that exercise was a protective factor against myopia. Increasing outdoor time reduced the risk of myopia onset and myopic shifts, especially in non-myopic children, and daily outdoor time of 120 to 150 min at 5,000 lux/min or cumulative outdoor light intensity of 600,000 to 750,000 lux significantly reduced the incidence risk ratio of myopia by 15% ~ 24% (14, 31). Tracing the causes, the increasing outdoor physical activity time against myopia was mainly attributed to increasing vitamin D and dopamine levels (32–34). Girls were found to spend less time on outdoor physical activities compared to boys (35, 36). While physiological parameters are beyond control, it remains crucial to promote increased activity time to mitigate and manage myopia. This emphasizes the significance of engaging in outdoor activities as much as possible and ensuring exposure to sunlight, particularly for girls, as a preventive measure against myopia (37). Second, increasing homework burden leads to more frequent use of eyes and eye strain for children. As a result, our study showed that the risk of myopia increased significantly when studying for more than a quarter without taking a break while doing eye exercises twice a day or more was the protective factor for total participants and children in Gannan Prefecture. However, the protection role of doing eye exercises for myopia was only found in univariate analysis in Wuwei City. Eye exercises are a kind of eye health exercise based on the knowledge of traditional Chinese medicine. When doing eye exercises, students were asked to regularly press some acupoints of two eyes with thumbs for 10–15 s. These acupoints include Jingming point, Sizhukong point, Zhuzhu point, Tongziliao point, Yuyao point, Chengxi point, Sibai point, Yifeng point, and Yiming point (Table 6). Doing eye exercises may regulate the blood circulation and muscles of the eye and improve eye fatigue, so as to achieve the purpose of preventing and controlling myopia (38–40). Wang et al. (41) also found no evidence for an effect of eye exercises on change in vision. Lin et al. (42) found that only the seriousness of attitude toward performing the eye exercises of acupoints showed a protective effect toward myopia. The value of OR(95%CI) was 0.51(0.33–0.78) (42). Therefore, it is important for students to complete eye exercises with high quality rather than as a formality (43). Third, increasing homework burden also leads to less duration sleep time for children. There is controversy about the correlation between sleep and myopia. For example, in a cross-sectional study on Chinese children aged 6–18 years, univariate regression analysis showed that compared to sleep duration <8 h per day, children with sleep duration of 8–9 and > 9 h per day had lower rates of myopia. However, after adjusting for age, gender, parental myopia, outdoor time, and continuous near work duration without breaks, sleep duration was not associated with myopia (44). Xu et al. (45) found that nighttime sleep duration of <7 h/day (OR = 1.27, 95%CI: 1.17–1.38) was likely to be associated with increased risks of self-reported myopia after adjusting age, sex, grade, parental education level, family income, parental myopia, academic record, and academic workload. After reviewing 864 published articles, members of the American Academy of Sleep Medicine recommended children aged 6–12 years old and teenagers aged 13–18 years old should sleep 9 to 12 h and 8 to 10 h per 24 h on a regular basis to promote optimal health (46). According to the current study, sleep duration of <8 h per day was the dependent risk factor of myopia for total participants and children in Gannan Prefecture, while there was an independent association in Wuwei City. Ensuring 8 h of sleep may be conducive to the prevention and control of myopia. At present, the mechanism between sleep and myopia is not clear. The fundamental regulator of sleep depends on the circadian cycle in melatonin synthesis and release (47). It seemed reasonable that deprivation caused disorder of the circadian rhythm, delayed melatonin circadian rhythm phasing, and lower melatonin output, which led to myopia (48). Therefore, ensuring adequate sleep is beneficial for the eye health of children and teenagers.
Our study showed that incorrect reading and writing posture was correlated factors of myopia; the values of OR (95%CI) were 1.257 (1.108, 1.425), 1.278 (1.041, 1.569), and 1.204 (1.024, 1.416) among all participants, Gannan Prefecture and Wuwei City. Zhang et al. found that reading and writing with eyes more than one foot from books was a correlated factor for preventing myopia. The value of OR (95%CI) was 0.75 (0.68, 0.82) (49). A cross-sectional study from Xi’an, China, displayed that doing “one punch, one foot, one inch “(when reading and writing, 10 cm from the chest to the table, 33 cm from the eye to the book, and 3.3 cm from the tip of the pen to the finger) was also correlated with myopia. The value of OR (95%CI) was 0.81 (0.73–0.91) (50). Therefore, maintaining a correct reading and writing posture and keeping the eyes more than one foot away from books would be beneficial for preventing and controlling myopia. Our research further indicated that students who frequently or always received encouragement from their teachers regarding proper reading and writing posture had a lower prevalence of myopia (69.8%) compared to those who never or only occasionally received such encouragement (75.1%). Taking into account the fact that students spend a long time at school and are compliant with teachers, teachers should remind students to pay attention to good reading and writing posture and protect their eye health (51).
Our study has some limitations. First, the data on lifestyle, ocular behaviors, and environment were collected from a self-administered questionnaire, which may lead to recall bias. Second, refraction was determined by cycloplegic autorefraction in the international consensus for defining myopia. However, refraction was determined by non-cycloplegic autorefraction in the present study, which may result in an overestimation of myopia, while myopia was assessed by combining refractive correction and visual acuity to reduce this effect. Nevertheless, it is necessary to perform the refractive examination in cycloplegia to obtain more realistic data in further studies, which may be conducive to better prevention and control of myopia.
5 Conclusion
Our study confirms the role of both hereditary and environmental factors in the prevalence of myopia among students from two regions within Gansu Province, highlighting regional disparities. Students with parental myopia and girls should be the key population to prevent and control myopia by taking multiple intervention measures, including mainly homework reduction, outdoor activities in the presence of the sun, adequate lighting in reading-writing activities, reading and writing with correct posture, adequate sleep, doing eye exercises, controlling electronic device use, relaxing eyes after studying for some time, and frequent ophthalmologic evaluations.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by the Ethics Committee of School of Basic Medical Sciences, Lanzhou University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin. Written informed consent was obtained from the minor(s)' legal guardian/next of kin for the publication of any potentially identifiable images or data included in this article.
Author contributions
JW: Investigation, Methodology, Writing – original draft, Writing – review & editing. SL: Data curation, Investigation, Resources, Writing – review & editing. SH: Investigation, Writing – review & editing. YF: Investigation, Writing – review & editing. PL: Investigation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. The study was supported by the Key Research and Development Project of Gansu Province (23YFFA0003) and Lanzhou Talent Innovation and Entrepreneurship Project(2023-RC-30).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Flitcroft, DI, He, MG, Jonas, JB, Jong, M, Naidoo, K, Ohno-Matsui, K, et al. IMI-defining and classifying myopia: a proposed set of standards for clinical and epidemiologic studies. Invest Ophthalmol Vis Sci. (2019) 60:M20–30. doi: 10.1167/iovs.18-25957
2. Haarman, AEG, Enthoven, CA, Tideman, JWL, Tedja, MS, Verhoeven, VJM, and Klaver, CCW. The complications of myopia: a review and meta-analysis. Invest Ophthalmol Vis Sci. (2020) 61:49. doi: 10.1167/iovs.61.4.49
3. Naidoo, KS, Fricke, TR, Frick, KD, Jong, M, Naduvilath, TJ, Resnikoff, S, et al. Potential lost productivity resulting from the global burden association of myopia: systematic review, Mata-analysis, and modeling. Ophthalmology. (2019) 126:338–46. doi: 10.1016/j.ophtha.2018.10.029
4. Holden, BA, Fricke, TR, Wilson, DA, Jong, M, Naidoo, KS, Sankaridurg, P, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmol. (2016) 123:1036–42. doi: 10.1016/j.ophtha.2016.01.006
5. Schuster, AK, Krause, L, Kuchenbäcker, C, Prütz, F, Elflein, HM, Pfeiffer, N, et al. Prevalence and time trends in myopia among children and adolescents. Dtsch Arztebl Int. (2020) 117:855–60. doi: 10.3238/arztebl.2020.0855
6. Harrington, SC, Stack, J, and O’Dwyer, V. Risk factors associated with myopia in schoolchildren in Ireland. Br J Ophthalmol. (2019). 1–8. doi: 10.1136/bjophthalmol-2018-313325
7. Yotsukura, E, Torii, H, Inokuchi, M, Tokumura, M, Uchino, M, Nakamura, K, et al. Current prevalence of myopia and association of myopia with environmental factors among schoolchildren in Japan. JAMA Ophthalmol. (2019) 137:1233–9. doi: 10.1001/jamaophthalmol.2019.3103
8. Lim, DH, Han, J, Chung, TY, Kang, S, and Yim, HW. On behalf of the epidemiologic survey Committee of the Korean Ophthalmologic Society. The high prevalence of myopia in Korean children with influence of parental refractive errors: the 2008-2012 Korean National Health and nutrition examination survey. PLoS One. (2018) 13:e0207690. doi: 10.1371/journal.pone.0207690
9. Zhou, J, Ma, Y, Ma, J, Zou, ZY, Meng, XK, Tao, FB, et al. Prevalence of myopia and influencing factors among primary and middle school students in 6 provinces of China. Zhonghua Liu Xing Bing Xue Za Zhi. (2016) 37:29–34. doi: 10.3760/cma.j.issn
10. Lim, LT, Gong, YH, Ah-kee, EY, Xiao, G, Zhang, XL, and Yu, SC. Impact of parental history of myopia on the development of myopia in mainland China school-aged children. Ophthalmol Eye Dis. (2014) 6:31–5. doi: 10.4137/OEd.s16031
11. Ahn, H, Lyu, IS, and Rim, TH. The influence of parental myopia on children’s myopia in different generations of parent-offspring pairs in South Korea. Semin Ophthalmol. (2018) 33:419–28. doi: 10.1080/08820538.2017.1284870
12. Ramamurthy, D, Chua, SYL, and Saw, SM. A review of environmental risk factors for myopia during early life, childhood and adolescence. Clin Exp Optom. (2015) 98:497–506. doi: 10.1111/cxo.12346
13. Morgan, IG, Wu, PC, Ostrin, LA, Tideman, WL, Yam, JC, Lan, WZ, et al. IMI risk factors for myopia. Invest Ophthalmol Vis Sci. (2021) 62:3. doi: 10.1167/iovs.62.5.3
14. He, XG, Sankaridurg, P, Wang, JJ, Che, J, Naduvilath, T, He, MG, et al. Time outdoors in reducing myopia: a school-based cluster randomized trial with objective monitoring of outdoor time and light intensity. Ophthalmology. (2022) 129:1245–54. doi: 10.1016/j.ophtha.2022.06.024
15. Shi, XJ, Gao, ZR, Leng, L, and Guo, Z. Temporal and spatial characterization of myopia in China. Front Public Health. (2022) 10:896926. doi: 10.3389/fpubh.2022.896926
16. Wang, XQ, He, HJ, Wang, XJ, Shan, GL, Tao, ZY, Pan, L, et al. Prevalence and risk factors of myopia in Han and Yugur older adults in Gansu, China: a cross-sectional study. Sci Rep. (2020) 10:8249. doi: 10.1038/s41598-020-65078-x
17. Shi, JJ, Wang, YJ, Lyu, PP, Hu, JW, Wen, XS, and Shi, XJ. Effects of school myopia management measures on myopia onset and progression among Chinese primary school students. BMC Public Health. (2023) 23:1819. doi: 10.1186/s12889-023-16719-z
18. Wang, NL, Li, SM, and Wei, SF. The key points and difficulties in prevention of myopia in Chinese children and adolescents. Zhonghua Yan Ke Za Zhi. (2021) 57:241–4. doi: 10.3760/cma.j.cn112142-20210123-00047
19. Tan, H, Yu, HQ, Wang, L, Qian, X, Lu, Y, and Liu, F. Development reliability and validity of child vision care related behavior assessment scale. Chin J School Health. (2009) 30:1007–10.
20. Tao, FB. Expert interpretation on appropriate technical guidelines for prevention and control of myopia in children and adolescents. Chin J school. Health. (2020) 41:166–72. doi: 10.16835/j.cnki.1000-9817.2020.02.002
21. Grzybowski, A, Kanclerz, P, Tsubota, K, Lanca, C, and Saw, SM. A review on the epidemiology of myopia in school children worldwide. BMC Ophthalmol. (2020) 20:27. doi: 10.1186/s12886-019-1220-0
22. Cai, XB, Shen, SR, Chen, DF, Zhang, QJ, and Jin, ZB. An overview of myopia genetics. Exp Eye Res. (2019) 188:107778. doi: 10.1016/j.exer.2019.107778
23. Rathi, M, Chhabra, S, Sachdeva, S, Rustagi, IM, Soni, D, and Dhania, S. Correlation of parental and childhood myopia in children aged 5-16 years in North India. Indian J Ophthalmol. (2022) 70:3366–8. doi: 10.4103/ijo.IJO_653_22
24. Matsumura, S, Dannoue, K, Kawakami, M, Uemura, K, Kameyama, A, Takei, A, et al. Prevalence of myopia and its associated factors among Japanese preschool children. Front Public Health. (2022) 10:901480. doi: 10.3389/fpubh.2022.901480
25. Liu, L, Li, R, Huang, D, Lin, X, Zhu, H, Wang, Y, et al. Prediction of premyopia and myopia in Chinese preschool children:a longitudinal cohort. BMC Ophthalmol. (2021) 21:283. doi: 10.1186/s12886-021-02045-8
26. Dong, L, Kang, YK, Li, Y, Wei, WB, and Jonas, JB. Prevalence and time trends of myopia in children and adolescents in China: a systemic review and meta-analysis. Retina. (2020) 40:399–411. doi: 10.1097/IAE.0000000000002590
27. Zhu, MH, Lin, TN, Lin, JH, and Wen, Q. Myopia among children and adolescents:an epidemiological study in Fuzhou City. Front Pediatr. (2023) 11:1161329. doi: 10.3389/fped.2023.1161329
28. Jiang, DJ, Zhang, DD, Zhang, Y, Shi, BJ, Gao, H, Guo, YB, et al. The trend of myopia rate in 61 350 children and adolescents:a cross sectional research in Ningbo. Zhejiang Acta Ophthalmol. (2020) 98:e525–6. doi: 10.1111/aos.14343
29. Zhao, MH, Song, Y, Liu, JL, Li, J, Wang, Y, Hua, YG, et al. Investigation of ocular biometry in 4- to 9-year-old Chinese children. BMC Ophthalmol. (2023) 23:225. doi: 10.1186/s12886-023-02975-5
30. Zhang, XY, Wang, Y, Pan, CW, Yang, WY, Xiang, Y, Yang, J, et al. Effect of genetic-environmental interaction on Chinese childhood myopia. J Ophthalmol. (2020) 2020:6308289. doi: 10.1155/2020/6308289
31. Dhakal, R, Shah, R, Huntjens, B, Verkicharla, PK, and Lawrenson, JG. Time spent outdoors as an intervention for myopia prevention and control in children: an overview of systematic reviews. Ophthalmic Physiol Opt. (2022) 42:545–58. doi: 10.1111/opo.12945
32. Zhang, J, and Deng, GH. Protective effects of increased outdoor time against myopia: a review. J Int Med Res. (2019) 48:030006051989386–9. doi: 10.1177/0300060519893866
33. Landis, EG, Park, HN, Chrenek, M, He, L, Sidhu, C, Chakraborty, R, et al. Ambient light regulates retinal dopamine signaling and myopia susceptibility. Invest Ophthalmol Vis Sci. (2021) 62:28. doi: 10.1167/iovs.62.1.28
34. Tideman, JWL, Polling, JR, Voortman, T, Jaddoe, VWV, Uitterlinden, AG, Hofman, A, et al. Low serum vitamin D is associated with axial length and risk of myopia in young children. Eur J Epidemiol. (2016) 31:491–9. doi: 10.1007/s10654-016-0128-8
35. Portela-Pino, L, Portela-Pino, A, Martínez-Patiño, MJ, Valverde-Esteve, T, and Domínguez-Alonso, J. Gender differences in motivation and barriers for the practice of physical exercise in adolescence. Int J Environ Res Public Health. (2019) 17:168. doi: 10.3390/ijerph17010168
36. Brazo-Sayavera, J, Aubert, S, Aubert, JD, Gonza’lez, SA, and Tremblay, MS. Gender differences in physical activity and sedentary behavior: results from over 200,000 Latin-American children and adolescents. PLoS One. (2021) 16:e0255353. doi: 10.1371/journal.pone.0255353
37. Torii, H, Kurihara, T, Seko, Y, Negishi, K, Ohnuma, K, Inaba, T, et al. Violet light exposure can be a preventive strategy against myopia progression. EBioMedicine. (2017) 15:210–9. doi: 10.1016/j.ebiom.2016.12.007
38. Lu, XH, and Pan, JJ. Effect of traditional Chinese medicine eye health exercises combined with family interaction management program on the improvement of eye habits and visual acuity in children and adolescents with refractive errors. Hebei J TCM. (2024) 46:815–20. doi: 10.3969/j.issn.1002-2619.2024.05.024
39. Zhang, QX, Jing, YX, Deng, CH, and Wang, JM. Effects and potential mechanisms of exercise and physical activity on eye health and ocular diseases. Front Med. (2024) 11:1353624. doi: 10.3389/fmed.2024.1353624
40. Liang, YB, Vasudevan, B, Lin, Z, Zhou, HJ, and Ciuffreda, KJ. The effect of eye exercises of acupoints on myopia progression: a 3-year cohort report from the Beijing myopia progression study. Risk Manag Healthc. (2020) 13:2793–9. doi: 10.2147/RMHP.S281289
41. Wang, H, Qian, YW, Congdon, N, Boswell, M, Rozelle, S, and Ma, XC. Effect of Chinese eye exercises on change in visual acuity and eyeglasses wear among school-aged children in rural China: a propensity-score-matched cohort study. BMC Complement Med. (2020) 20:82. doi: 10.1186/s12906-020-2878-9
42. Lin, Z, Vasudevan, B, Jhanji, V, Gao, TY, Wang, NL, Wang, Q, et al. Eye exercises of acupoints: their impact on refractive error and visual symptoms in Chinese urban children. BMC Compl Altern M. (2013) 13:306. doi: 10.1186/1472-6882-13-306
43. Tang, J, Pei, YF, Wang, JG, Yan, N, Luo, YJ, Zhou, W, et al. The association between Chinese eye exercises and myopia in children and adolescents: a systematic review and meta-analysis. Front Public Health. (2023) 11:950700. doi: 10.3389/fpubh.2023.950700
44. Huang, LM, Chen, XL, Lin, JJ, Fan, XM, Chen, T, Yu, Y, et al. Association between sleep duration and myopia among Chinese children during the COVID-19 pandemic: a cross-sectional study. Front Public Health. (2023) 10:1015138. doi: 10.3389/fpubh.2022.1015138
45. Xu, SJ, Zong, ZQ, Zhu, Y, Zhang, XD, Zhang, Y, Wang, X, et al. Association between sleep-wake schedules and myopia among Chinese school-aged children and adolescents: a cross-sectional study. BMC Ophthalmol. (2023) 23:135. doi: 10.1186/s12886-023-02874-9
46. Paruthi, S, Brooks, LJ, D’Ambrosio, C, Hall, MW, Kotagal, S, Lloyd, RM, et al. Consensus statement of the American Academy of sleep medicine on the recommended amount of sleep for healthy children: methodology and discussion. J Clin Sleep Med. (2016) 12:1549–61. doi: 10.5664/jcsm.6288
47. Stone, RA, Pardue, MT, Michael Iuvone, P, and Khurana, TS. Pharmacology of myopia and potential role for intrinsic retinal circadian rhythms. Exp Eye Res. (2013) 114:35–47. doi: 10.1016/j.exer.2013.01.001
48. Chakraborty, R, Micic, G, Thorley, L, Nissen, TR, Lovato, N, Collins, MJ, et al. Myopia,or near-sightedness, is associated with delayed melatonin circadian timing and lower melatonin output in young adult humans. Sleep. (2021) 44:zsaa208. doi: 10.1093/sleep/zsaa208
49. Zhang, D, Sun, BJ, Wu, M, Liu, HY, Zhou, L, and Guo, LY. Prevalence and associated factors of myopia among school students in Shenyang, China: a cross-sectional study. Front Public Health. (2023) 11:1239158. doi: 10.3389/fpubh.2023.1239158
50. Zhao, XX, Lu, X, Yu, L, Zhang, YP, Li, J, Liu, YY, et al. Prevalence of myopia and associated risk factors among key schools in Xi’an. China BMC Ophthalmol. (2022) 22:519. doi: 10.1186/s12886-022-02735-x
Keywords: children and adolescents, myopia, influencing factors, regional disparity, prevention and control
Citation: Wang J, Li S, He S, Feng Y and Li P (2024) Regional disparities in the prevalence and correlated factors of myopia in children and adolescents in Gansu, China. Front. Med. 11:1375080. doi: 10.3389/fmed.2024.1375080
Edited by:
Claudia Carolina Cruz-Gálvez, University of Guadalajara, MexicoReviewed by:
Vanessa Bosch, National Institute of Pediatrics (Mexico), MexicoSiti Nurliyana Abdullah, University of Brunei Darussalam, Brunei
Martha Edith Cancino Marentes, Autonomous University of Nayarit, Mexico
Copyright © 2024 Wang, Li, He, Feng and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jinyu Wang, MjQyMTU0ODY1NkBxcS5jb20=; Sheng Li, MTE3ODcwODQwN0BxcS5jb20=
 Jinyu Wang
Jinyu Wang Sheng Li2*
Sheng Li2*