- 1Disease Prevention and Control Department, Jima Arjo District Health Office, Oromia, Ethiopia
- 2Department of Nursing, Institute of Health Sciences, Wollega University, Nekemte, Ethiopia
- 3Department of Public Health, Institute of Health Sciences, Wollega University, Nekemte, Ethiopia
Introduction: In resource-constrained countries, the incidence of mortality among patients admitted to adult intensive care units is higher than that in developed countries, which has a physical, economic, and emotional impact on the lives of patients and their families. However, there is limited evidence on factors related to nursing care that can potentially contribute to predicting and reducing mortality rates in intensive care units. Therefore, this study aimed to assess the incidence of mortality and its predictors in patients admitted to an adult intensive care unit.
Methods: A retrospective cohort study was conducted among 403 patients admitted to the adult intensive care unit from 1 January 2021 to 31 December 2021. The collected data were entered into Epi Data Manager v4.6.0.6 and exported to SPSS version 24 for analysis. Binary logistic regression was used to identify the predictors of mortality. Variables with a p-value less than 0.25 in bivariable logistic regression were selected for multivariable logistic regression. A p-value <0.05 was used to indicate a significant association in multivariable analysis. Finally, the adjusted relative risk (RR) with 95% CI was calculated.
Results: A total of 403 patients were included in the analysis. The cumulative incidence of death was 40.9% (95% CI 36, 45.9%). Mortality was significantly associated with the need for mechanical ventilation (adjusted RR = 1.45; 95% CI: 1.04, 1.85), the Glasgow Coma Scale score < 8 (adjusted RR, 3.52; 95% CI: 2.90, 4.05), presence of comorbidity (adjusted RR, 1.47; 95% CI: 1.09, 1.83), length of stay in ICU < 24 h (adjusted RR, 1.84; 95% CI: 1.37, 2.04), oxygen saturation level, and Feeding, Analgesia, Sedation, Thrombosis prophylaxis, Head elevation, Ulcer prophylaxis, and Glucose control (FASTHUG) treatment received were significantly associated with mortality.
Conclusion: The study found a high incidence proportion of death. The need for mechanical ventilation, length of stay, comorbidity, and the Glasgow Coma Scale score were significantly associated with mortality. Therefore, close monitoring and evaluation of patients are essential to improve treatment outcomes.
Introduction
An intensive care unit (ICU) is a special hospital or healthcare facility department that provides intensive care treatment to patients with severe or life-threatening illnesses and injuries, which require constant care and close supervision under life support equipment and medication. Intensive care is the specialized treatment given to acutely unwell patients requiring critical medical care (1, 2). By 1953, Bjorn Ibsen, the anesthetist who proposed that positive pressure ventilation be the treatment of choice during the polio epidemic, had constructed Europe’s first intensive care unit; many consider him to be the “father” of intensive care (3).
Based on equipment availability and skilled medical and nursing personnel, the World Federation of Societies of Intensive Care Medicine (WFSICCM) classified ICUs into three categories. A level 1 ICU can provide oxygen and non-invasive monitoring, while a level 2 ICU can provide invasive monitoring and basic life support for a limited amount of time. A level 3 ICU offers a comprehensive range of monitoring and life support systems and may contribute to the advancement of intensive care medicine through research and education (4).
ICUs began to develop in many resource-limited countries after decades compared with the industrialized countries. However, the burden of critical illness is especially high in low-income countries as infections such as pneumonia, diarrhea, and malaria are endemic, and traffic accidents, obstetric complications, and surgical emergencies are common (5, 6).
In Ethiopia, the Ministry of Health established an Emergency Medicine and Critical Care Directorate and Implementation Guidelines in 2015 to standardize ICU organization, design, and common practices including rounds, admission, and discharge, reflecting increased attention to emergency medicine and critical care capacity (7). Currently, 53 public hospitals in Ethiopia, provide adult intensive care services (8).
Mortality is a major endpoint in epidemiological and interventional studies conducted in the ICU. Despite medical advances in patient management, ICU mortality remains high as approximately one-third of patients dying in the hospital died in ICU, though the mortality has large variations according to patient case mix and organization of care in ICU (9, 10).
Critically ill patients are admitted to the ICU to reduce morbidity and mortality associated with acute illness, trauma, or surgical procedures (11). Globally, the incidence of death in ICU roughly ranges from 20 to 47% though this magnitude varies between regions and countries (12, 13). It varies across the world depending on the ICU infrastructure, staff availability, training, pattern, and cause of ICU admission.
The incidence of mortality is high in African countries. A retrospective study conducted in Ugandan Mulago Hospital and Kenyan Hospital showed an incidence proportion of mortality of 43.7% (14) and 53.6% (15), respectively. In Ethiopia, studies have indicated poor outcomes for patients admitted to intensive care units with the mortality ranging from 39 to 47% (16–18). ICUs in Addis Ababa faced a high incidence of mortality, 32% of admitted patients to emergency care died (19), and it was 27% in Ayder Hospital (20) and 38.7% in Gondar Hospital (21).
The major causes of ICU admission include trauma, cardiac disease, acute abdominal presentations, septic shock, tetanus, and hysterectomy secondary to uterine rupture. Medical diagnoses accounted for 50.1% of ICU admissions followed by surgery (43.2%) and obstetrics (5.8%) and the corresponding survival rates of the cases were 53.6% for medical admissions, 48.0% for surgery, and 42.9% for obstetrics (22). A shortage of ICU beds, lack of sufficiently trained healthcare professionals, constraints in critical technologies, shortage of medications, scarce data on patient outcomes, immaturity of the program, lack of partnership, and stakeholders are the major challenges of critical care service in developing nations (11, 23).
Morbidity and mortality in the ICU due to critical illness or accident can have a huge physical, social, economic, and emotional impact on the life and family of the admitted patients (24). A study conducted in Malaysia showed that patients who spent a lot of money on treatment had a 2-fold increased risk of dying (25, 26). The influence of death on overall ICU expenses was studied in the United States, and the median observed cost of a unit stay was $9,619 (mean = $16,353). A national study conducted in Scotland demonstrated that ICU survivorship is associated with higher ($25,608 versus $16,913/patient) hospital resource utilization than hospital controls (27). Financial and psychological burdens, shattered family expectations and family integrity, lack of confidence in hospitals’ service delivery system, families being immersed in an unfriendly environment, and a sense of fulfillment in helping the patient were among the problems faced in ICUs by patient caregivers, according to a study conducted in Addis Ababa, Ethiopia (28).
The Ethiopian Federal Ministry of Health has shown a renewed commitment to emergency care systems through the development of the Emergency and Critical Care Directorate (ECCD) in its administrative structure. This directorate aimed to reduce unfavorable outcomes in ICUs to less than 25% by 2020 by training emergency physicians and developing out-of-hospital emergency care (7), but the incidence of mortality rate of patients admitted to ICU is still high and far beyond the target.
Despite the incidence of mortality, which is high among patients admitted to the ICU and results in loss of human and economic resources, prior studies only assessed factors associated with sociodemographic and clinical characteristics and did not assess factors associated with care in the ICU. Thus, this study aimed to fill these gaps by assessing the factors associated with mortality among patients admitted to the ICU in Nekemte City public hospitals using a retrospective cohort study method by incorporating factors related to care components.
Methods
Study area
The study was conducted in Western Ethiopian public hospitals on patients admitted to the adult ICU from 1 January 2021 to 31 December 2021. Nekemte Specialized Hospital and Wollega University Referral Hospitals are the two hospitals with adult ICUs in the western part of Ethiopia. The data were collected from 11 April 2022 to 11 May 2022. Wollega University Referral Hospital was established in 2017. It serves a catchment population of 3.5 million people. The ICU service provision started in 2018 and was equipped with six beds, four mechanical ventilators, one defibrillator, and one ultrasound machine. One consultant anesthesiologist, two emergency and critical care nurses, six rotating general practitioners, and ten rotating BSc nurses. Nekemte Specialized Hospital serves as a referral center for western Ethiopia, with approximately 11 million people, and ICU service provision was started recently in March 2020 GC. The ICU of the Nekemte Specialized Hospital is equipped with six beds, four mechanical ventilators, two defibrillators, and one ultrasound machine. It was also staffed by one general practitioner, one emergency and critical care nurse, one consultant physiotherapist, and nine rotating BSc nurses.
Study design
An institutional-based retrospective cohort study design was conducted.
Study period
A study was conducted on data of patients admitted to adult ICU at Nekemte Specialized Hospital and Wollega University Referral Hospital from 1 January 2021 to 31 December 2021.
Source population
All patients who were admitted to adult intensive care units at Nekemte City public hospitals.
Study population
Patients who were admitted and registered into the adult ICU at Nekemte Specialized Hospital and Wollega University Referral Hospital from 1 January 2021 to 31 December 2021.
Inclusion criteria
All patients admitted and registered to the adult ICU of Nekemte Specialized Hospital and Wollega University Referral Hospital from 1 January 2021 to 31 December 2021 were included in the study.
Exclusion criteria
Patients whose charts were incomplete, patients whose charts were not found or lost, and patients referred to other higher facilities for better diagnosis and management were excluded from the study.
Sample size determination
The sample size was calculated by using a two or double population proportion formula, and it was calculated through Epi Info version 7 statistical software package with the assumption of confidence level 95% (Z𝛼/2 = 1.96), power 80% (Z1-𝛽= 0.84), the ratio of unexposed to exposed is 2, and the proportion of outcome in exposed and RR. Independent predictors, such as the presence of sepsis, need for mechanical ventilation, hypoxia, shorter duration of ICU stay, and age greater than 80 years, were considered for sample size calculation. Among these predictors, the primary exposure variable, which was the need for mechanical ventilation, yielded the largest sample size of 414. Therefore, the final sample size of the study was 414.
Sampling procedure
The source population during the specified study period was 473, which is relatively small when compared to the minimum required sample size of 414. Therefore, a census of all patients who were registered and admitted to both ICUs was taken and analyzed. Consequently, 403 patient charts with complete data were included in the analysis (Figure 1).
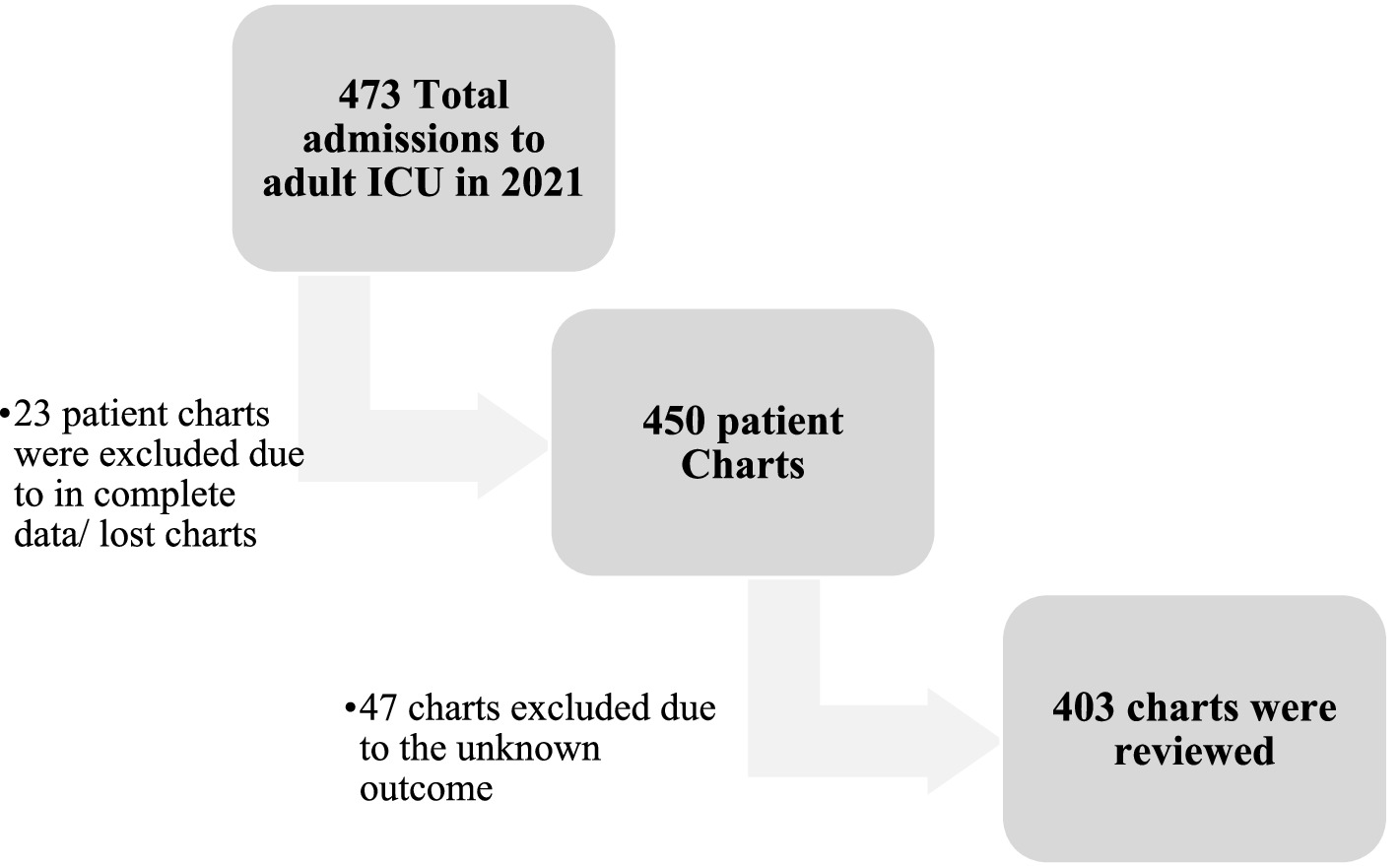
Figure 1. Sampling procedure of patient charts, incidence and predictors of mortality among patients admitted to adult ICU, Western Ethiopia, 2021.
Data collection tool and procedure
A data extraction checklist was prepared after an extensive literature review and patient charts. It is comprised of three parts: sociodemographic characteristics, related clinical characteristics, and laboratory parameters. Four nurses (two for each hospital) gathered the data under the supervision of two additional BSc Nurses (one for each hospital). The medical registration number of admitted patients from the ICU registry was used to extract patient charts from the chart room. The data collectors completed the checklist by reviewing patient records and charts. Then, the supervisor checked sample data for error and completeness of the data and submitted it to the principal investigator.
Study variables
Dependent variable: status at discharge from ICU (alive or deceased).
Independent variables: the explanatory variables were sociodemographic factors and laboratory-related and clinical factors.
Operational definition
Deceased: those who passed away while in the ICU and given code number 3 on the ICU registry.
Alive: those who survived during ICU stay, including patients who improved and were discharged, and those who left against medical advice (code 1) and were transferred to (code 2).
FASTHUG score: FASTHUG is a shorthand representation for Feeding, Analgesia, Sedation, Thrombosis prophylaxis, Head elevation, Ulcer prophylaxis, and Glucose control. From the patient chart, whether the patient received this routine care was checked and coded ‘Yes’ if the patient had received that specific treatment, and care, and ‘No’ if that patient had not received that treatment and care. Finally, all the answers ‘yes’ were added, and the mean was calculated and yielded 3. Patients were categorized based on their scores as above or below the mean.
Comorbidity: the condition of having two or more diseases at the same time in addition to the main disease with which the patient was admitted to the ICU.
Incomplete data: patient charts with dependent variables were not found, and those with <80% of the variables were found.
Data quality control
A one-day training was given to data collectors and supervisors on the objective of the study, the contents of the checklist, ethical issues, and the data collection approach. To identify the reliability of the data collection instruments, a pre-test was conducted before actual data collection, followed by a discussion with data collectors and supervisors, which was modified to enhance the completeness of the data. The supervisors checked the completeness of the checklist at the end of each data collection day.
Data processing and analysis
Data were coded and entered into Epi Data Manager version 4.6.06 and exported to SPSS version 24 for cleaning and analysis. Descriptive statistics, such as frequencies, proportions, and mean with SD and median with IQR, were used to describe the data. Data were organized using tables, graphs, and charts. A binary logistic regression model was used to determine the association between each independent variable and the patient outcome at ICU discharge (29, 30). Variables with a p-value less than 0.25 in bivariable logistic regression were selected for multivariable logistic regression. In the multivariable model, a statistical significance was set at p < 0.05. The goodness of fit of the model was checked by the Hosmer–Lemeshow test with a p-value of 0.35, indicating that the model was well fitted, and multicollinearity was checked by VIF; values were below 10. The adjusted odds ratio (AOR) was converted to adjusted relative risk using the Zhang and Yu formula (31), based on the STROBE recommendation (32). Finally, the adjusted relative risk with 95% CI was reported.
Ethics statement
Ethical approval was obtained from the Ethical Clearance Committee of Wollega University in its review held on 15 March 2022 (reference number WU/RD/555/2014). A letter of cooperation was written to the Nekemte Specialized Hospital and Wollega University Referral Hospital. A formal permission letter was written to the Emergency and Critical Care Department and Chart Room Office by the CED of both hospitals, and data were extracted from the patient charts. The need for informed consent was waived by the ethical review committee of Wollega University by the Declaration of Helsinki. In addition, the data collection tool was fully anonymized as it did not contain individual patient identifiers, such as name and Medical Record Numbers, and the authors had no access to the patient identifier.
Result
Socio-demographic characteristics of patients
A total of 403 patients were included in the analysis. The remaining 70 patient charts were excluded because of unknown patient outcomes, lost charts, or incomplete data. The mean (±SD) age of the patients admitted to adult ICU was 41 (17) years. The age category greater than 55 years constituted more admissions (28.3%), and the mortality rate was relatively high (45.2%) among the age category of 35–44 years. Of the total study participants, 221 (54.8%) were men, and 240 (59.6%) were from rural residents (Table 1).
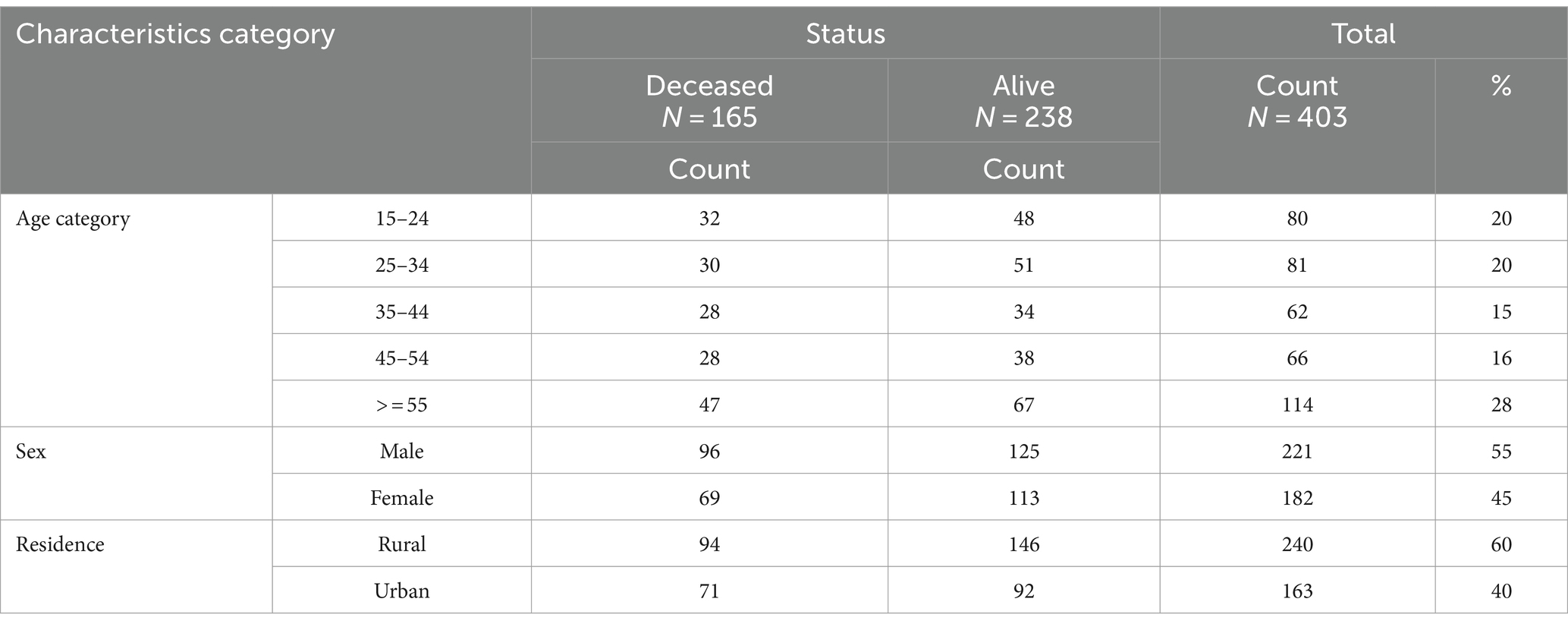
Table 1. Socio-demographic characteristics of patients admitted to adult ICU, Western Ethiopia, 2021.
Clinical characteristics of the patients
Admission diagnosis and disease category
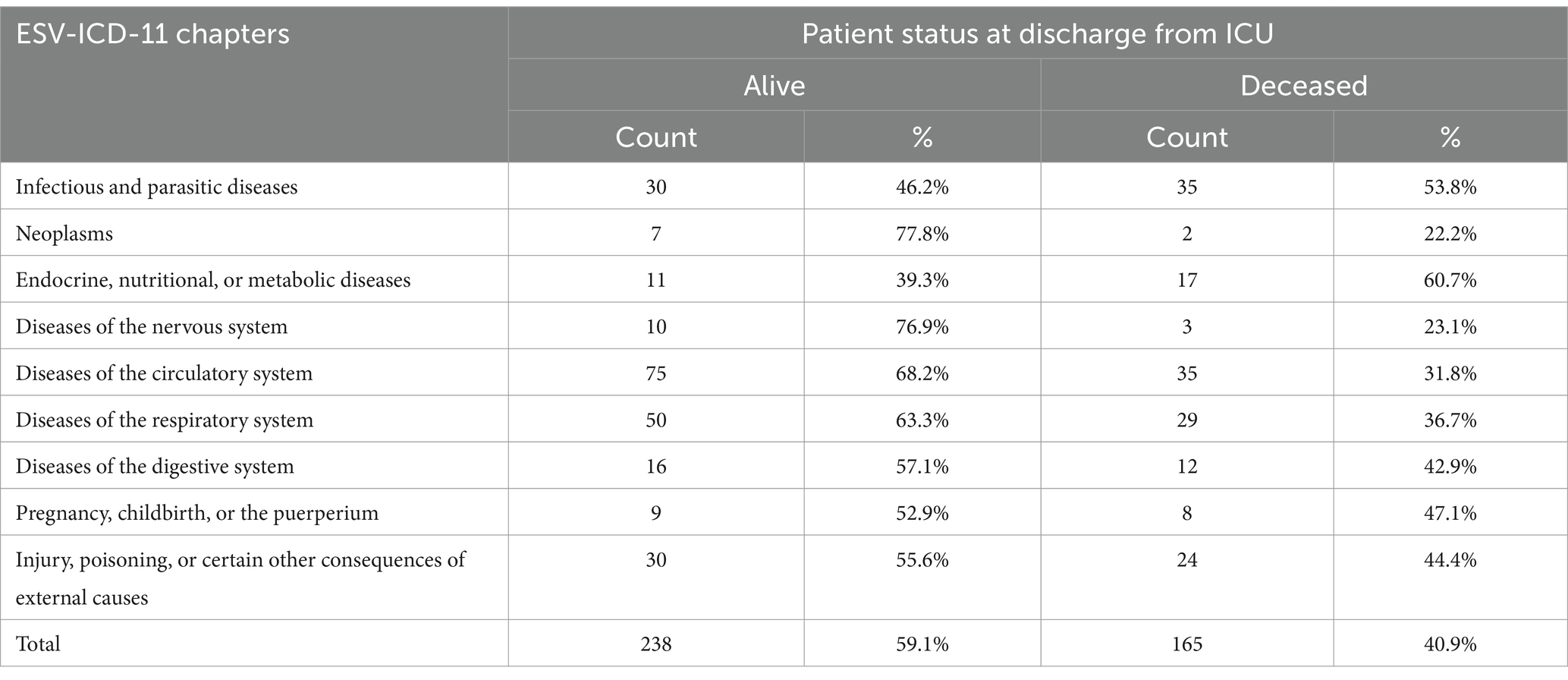
Cardiovascular diseases were the most common underlying cause of ICU admission accounting for 110 (27.3%) followed by diseases of the respiratory system which contributed 79 (19.6%). The death rate was high among patients admitted with endocrine, nutritional, and metabolic diseases, of which 17 (61%) died, followed by infectious and parasitic diseases, in which 35 (54%) died (Table 2).
Comorbidity status, source of admission, and other clinical characteristics
The study also showed that 149 (37%) patients had at least one comorbid disease, with hypertension being the most common (59, 15%), followed by diabetes mellitus (all types 19; 4%), acute and chronic kidney disease (18, 4.5%), and pneumonia (17, 4.2%). Among all admissions, 327 (81.1%) were for medical reasons, and the mortality rate was 41% in this group.
This study revealed that the median length of stay in the ICU was 72 h (IQR = 96 h). Of the patients, 285 (70.7%) stayed longer than 24 h, and 118 (29.3%) stayed for less than 24 h in ICU. Of patients who stayed less than 24 h in the ICU, 74 (62.7%) and 91 (31.9%) of patients who stayed for longer than 24 h died in ICU.
One hundred fifty-seven (39%) patients were referred from other health facilities (had referral forms), while others were self-referrals. Regarding the time of admission to the ICU, 297 (74%) patients were admitted during regular working days and the remaining 106 (26%) were admitted during weekends and holidays.
Vital signs and care-related characteristics
At admission, 195 (48.4%) patients had a normal respiratory rate of 12–20 breaths per minute, whereas 208 (51.6%) patients had unstable respiration of less than 12 or greater than 20 breaths per minute. The incidence proportion of mortality rates was 83 (42.6%) and 82 (39.4%) in patients with normal and deteriorated respiratory rates, respectively. Blood pressure measurement was another vital sign measured at admission to ICU; 110 (27.3%) patients were normotensive (90–140 mmHg), while 293 (72.7%) patients were either hypotensive or hypertensive. One hundred and one patients (25%) required mechanical ventilation on admission to the ICU, of whom 59 (58.4%) died, and 106 (35.1%) died among those who were not on mechanical ventilation (Table 3).
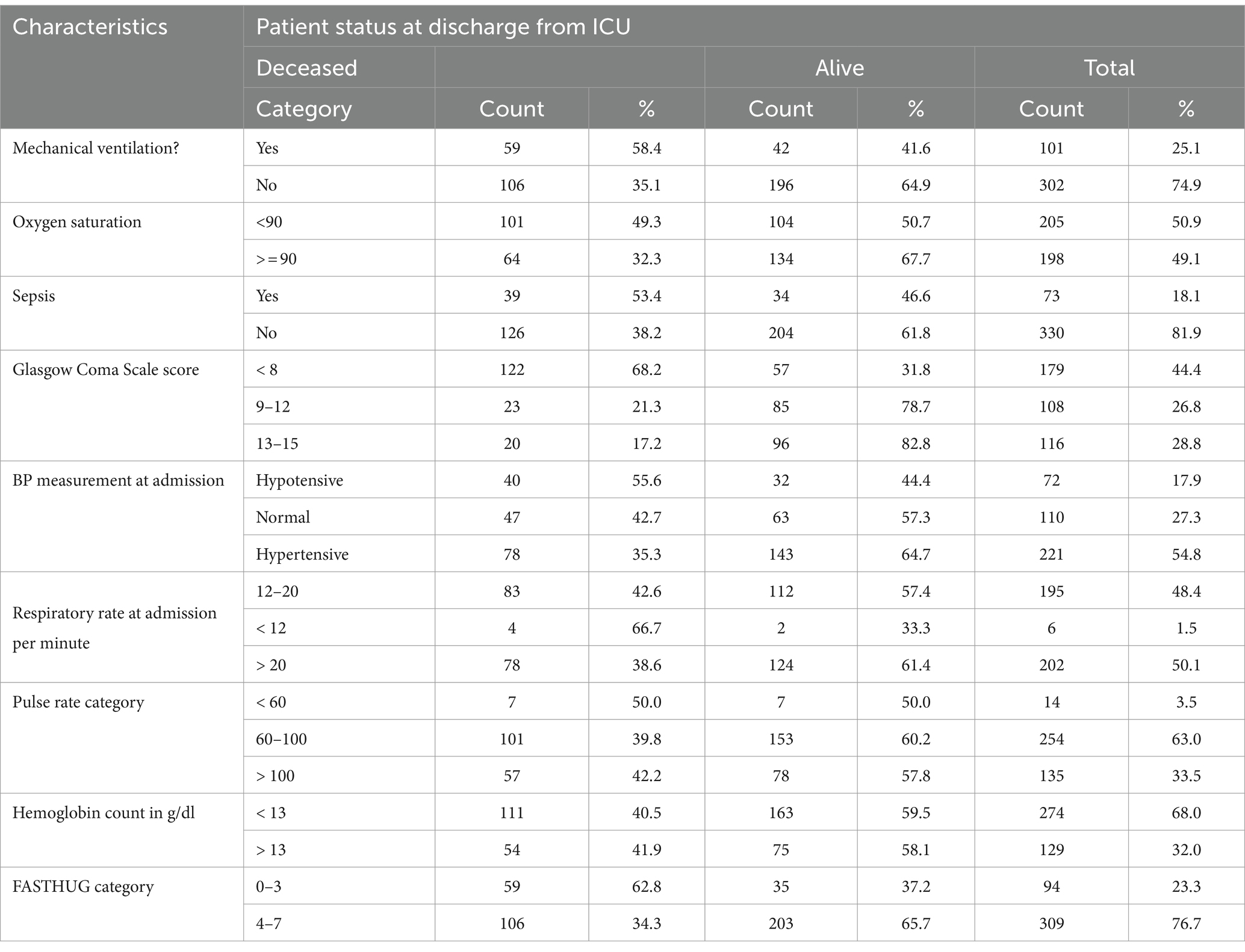
Table 3. Vital signs and related parameters among patients admitted to adult ICU, Western Ethiopia, 2021.
This study showed that 396 (98.3%) patients had received at least one component of FASTHUG treatment, and 52 (12.9%) patients received all seven components. Glucose control was the most treatment provided 367 (91.1%) followed by anti-pain provision 356 (88.3%) and ulcer prophylaxis 315 (78.2%) (Figures 1, 2).
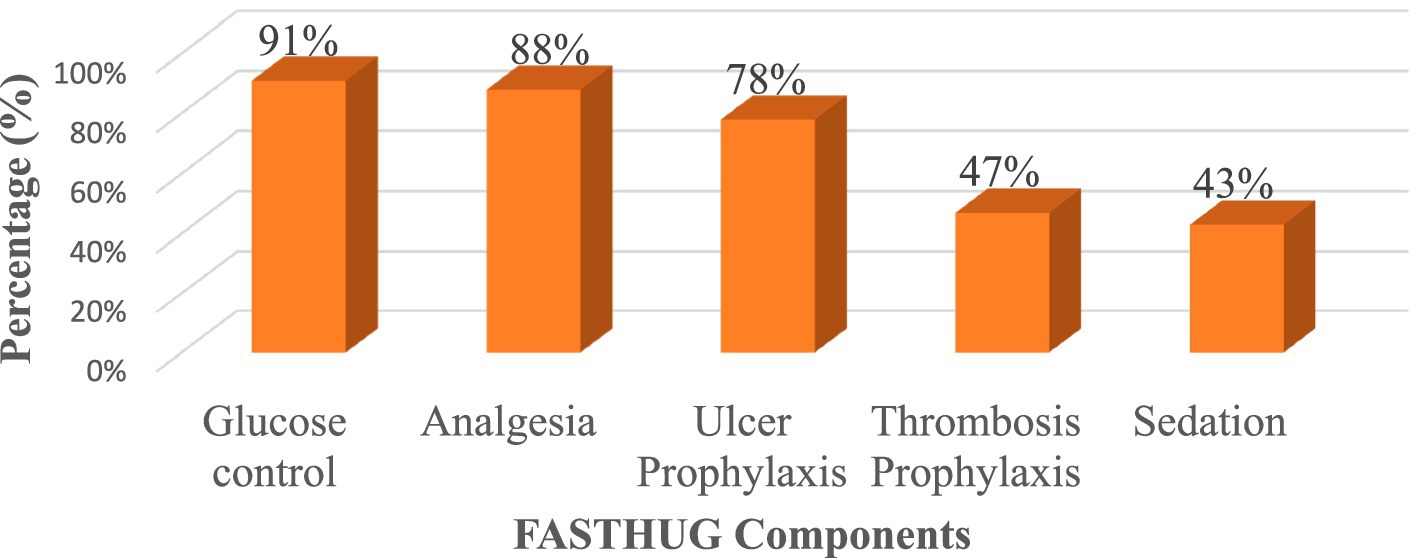
Figure 2. Frequency of FASTHUG treatment components among patients admitted to adult ICU; Western Ethiopia, 2021.
Incidence and predictors of mortality in ICU
A total of 403 patients were retrospectively followed up until discharge from ICU. The incidence proportion of mortality in ICU was 40.9% (95% CI: 36.1–45.9%) in 1 year.
Eighteen variables were tested for their association with mortality at ICU discharge. In the bivariable analysis, variables such as the need for mechanical ventilation, comorbidity, length of stay in ICU, GCS, sepsis, deteriorated BP, oxygen saturation level, and FASTHUG score were significant at a p-value <0.25 and were selected for multivariable logistic regression at p value <0.25 (Table 5).
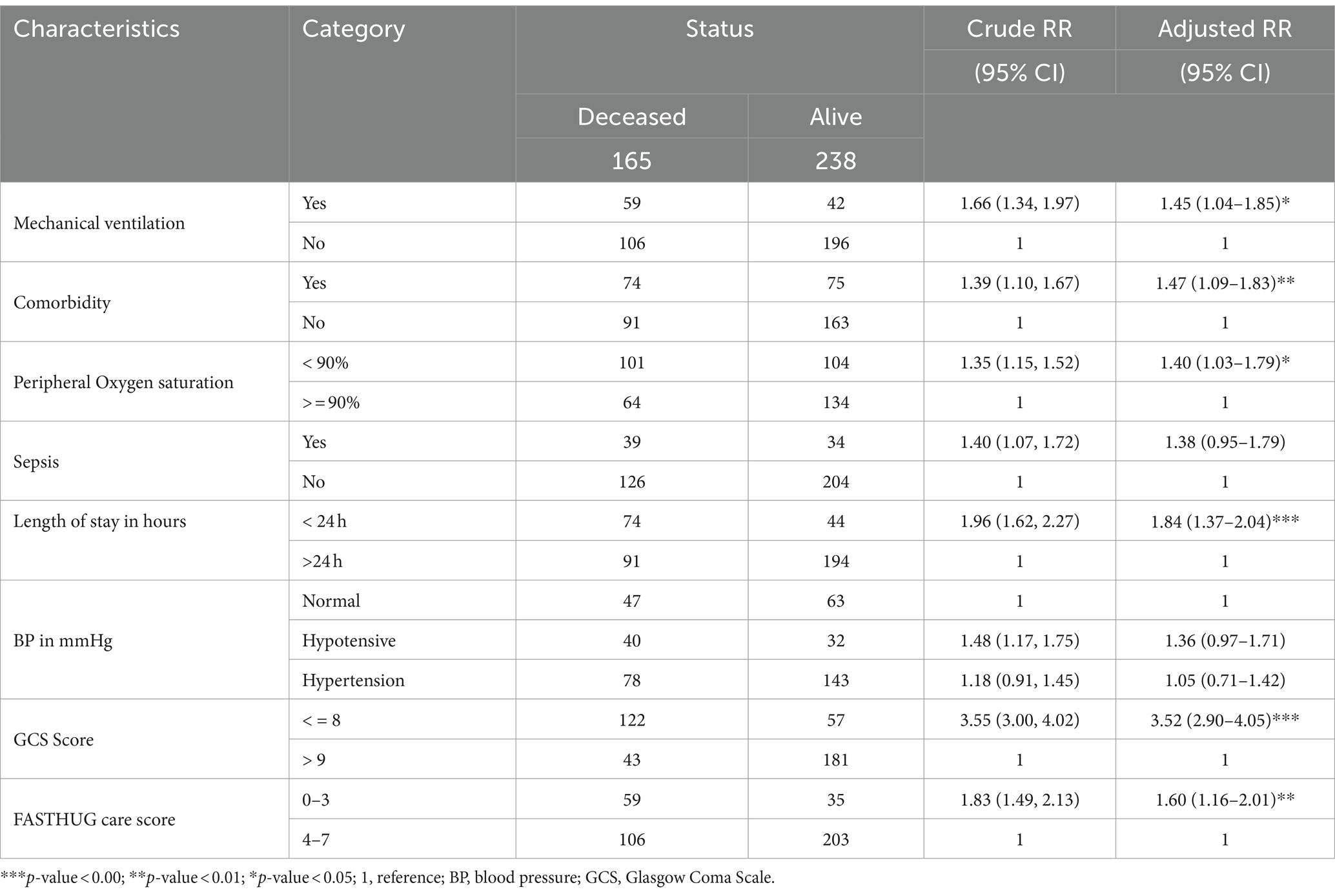
Table 5. Bivariable logistic regression analysis of predictors of mortality among patients admitted to adult ICU, Western Ethiopia, 2021.
However, in the multivariable analysis, only the need for mechanical ventilation, presence of comorbidity, length of stay in the ICU, GCS, oxygen saturation level, and FASTHUG score remained statistically significant. The prediction ability of the model was checked using the area under the receiver operating characteristic curve. The area under receiver operating characteristics value was 8.853 (95% CI: 0.853, 0.889).
Patients who were on mechanical ventilation were 1.45 times more likely to die than those who were not on mechanical support (adjusted RR = 1.45, 95% CI: 1.04, 1.85). The length of stay in the ICU was another strong predictor of ICU mortality. This study showed that patients who stayed for less than 24 h were 1.84 times more likely to die than patients who stayed for longer than 24 h (adjusted RR = 1.84, 95% CI: 1.37, 2.04). This study showed that there is an inverse association between the GCS score and the risk of death in patients admitted to the ICU. Patients with a GCS of <8 were 3.52 times at risk of death in the ICU compared to those with a score greater than or equal to 9 GCS score (adjusted RR = 3.52, 95% CI: 2.90, 4.05).
Patients whose oxygen saturation of less than 90% by pulse oximetry were 1.4 times more likely to die than those with oxygen saturation greater than 90% (adjusted RR = 1.40, 95% CI: 1.03, 1.79).
Patients receiving less or equal to three components of the FASTHUG care are found to be 1.6 times at higher risk of death than those receiving four or more care components (adjusted RR, 1.60; 95% CI: 1.16, 2.01). Patients with one or more comorbidities had 1.47 times more chance of dying (Table 4).
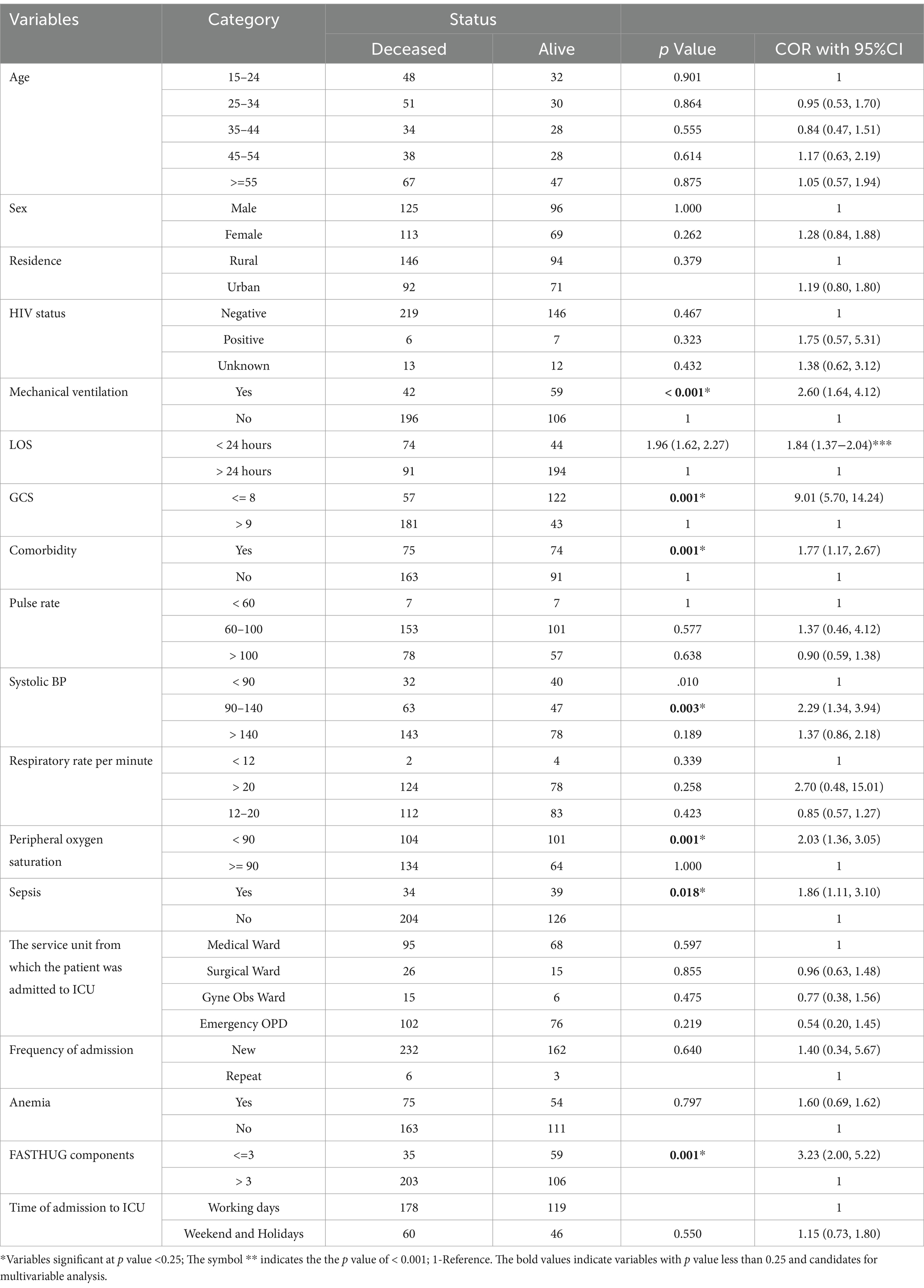
Table 4. Multivariable logistic regression analysis of predictors of mortality among patients admitted to adult ICU, Western Ethiopia, 2021.
Discussion
The incidence proportion of mortality in this study was found to be comparable with the results of a study conducted in Hosanna, Gondar University, St. Paul’s Hospital, and Mulago Hospital of Uganda, which reported a mortality incidence proportion of 46.2% (16), 38.7% (21), 39% (18), and 43.7% (14), respectively. However, it was found to be lower than the result of a study conducted in Southern Ethiopia hospitals and Kenya, which reported a mortality rate of 46.8% (17) and 53.6% (15), respectively. This discrepancy might be due to the difference in admission diagnosis in which 54–80% of patients admitted in Southern Ethiopia and Western Kenyan hospitals presented with acute respiratory distress syndrome requiring respiratory support compared to the 25% in this study. This is not surprising that acute respiratory failure and acute respiratory distress syndrome are drivers of high mortality (33). The difference in the level of ICU care provided, which can be explained by differences in ICU equipment, healthcare professionals, and availability of medications could also contribute to the observed discrepancy in mortality rates between hospitals.
It is not a surprise that the incidence proportion of mortality in the current study is much higher than the finding of the study conducted in resource-affluent countries. The study conducted in Brazil reported 21% (34), and a multicenter European cohort study reported 19.1% (35). This huge discrepancy might be due to the difference in the level of ICU care, availability of medical supplies, availability of trained staff, and the use of high-cost technologies.
In this study, patients who required mechanical ventilation were more likely to die than those who were not. This finding is in line with the findings of a study conducted in Gondar (21), Kenya (15), and Brazil (34). Patients with respiratory distress are more unstable and susceptible to ventilator-associated pneumonia and other nosocomial infections, posing a risk to their clinical prognosis (36).
The Glasgow Coma Scale score was another predictor of mortality for patients in the ICU. Patients with a GCS score of <8 were more likely to die than patients with a GCS score of > = 9. This finding is similar to the finding of a study conducted in Southern Ethiopia (17), Gondar (21), and Mulago Hospital of Uganda (14). This can be explained by the fact that GCS is a significant indicator of disease severity and individuals who have suffered a head injury or other traumas are likely to have lower GCS scores (37).
Oxygen saturation level below 90% is also a predictor of death among ICU patients. This finding is similar to the finding of a study conducted in Peru and France (38, 39). Hypoxemia leads to respiratory distress syndrome due to low hemoglobin concentration in the blood. Patients may have to wait longer for ICU admission due to resource limitations and delayed hospital arrival (40).
This study also revealed that the likelihood of death decreases as the length of hospital stay increases. This finding is in agreement with a study conducted in different parts of the world (41–43). The probable cause of these early fatalities is most likely due to a late presentation to care after potential complications are developed and delayed referral from another health facility. In contrast to this study, a prospective investigation done in Turkey failed to discover a link between the length of time spent in the intensive care unit and the risk of death (42). This is due to the Turkish study’s exclusion of patients who spent less than 48 h in an intensive care unit, a period associated with a higher risk of mortality in this study.
This study found that patients who have at least one comorbidity were more likely to die than those who did not have comorbidity. This finding is consistent with the study done in West Scotland the UK (44). This can be explained by the fact that patients with comorbidities show higher Charlson Comorbidity Index and are older age patients, which are, in turn, statistically associated with mortality in the ICU (45).
FASTHUG-based care enables critically ill patients to receive holistic care that encompasses all critical issues and is proven effective in preventing adverse outcomes. This study showed that patients who had received less than three of the seven FASTHUG care components were more likely to die than those who had received at least four components of care. A comparative study conducted in Mexico and the United States revealed that the application of the FASTHUG bundle of care decreased mortality rate (46) and ventilator-associated pneumonia (47), respectively. This suggests that the nursing care model developed is effective in increasing the quality of nursing care given to critically ill patients.
Limitations of the study
Due to the retrospective nature of the study, a limited number of variables were found; as a result, some variables like severity scores (such as APACHE II and SOFA scores) of the patients could not be found, which might have a significant association with mortality of patients admitted to ICU. This mortality incidence is not disease-specific and includes a variety of disease entities that may each have a variable mortality rate. In addition to this, factors associated with ICU resources, staffing, and training status of the staff were not assessed by this study as these factors might have an impact on the outcome of the patients.
The study followed the patients only until their discharge from the ICU and considered patients who were transferred to wards and those left against medical advice as if they were survived or alive. These patients may die after discharge, which may underestimate the incidence of mortality.
Conclusion and recommendations
This study found a high incidence of mortality among patients admitted to the adult ICU. The severity of the condition, which is determined by the GCS score, need for mechanical ventilation, oxygen saturation level, and comorbidity significantly predict mortality among patients admitted to ICU. Patients who require mechanical ventilation were at higher risk of death because these patients were at risk of developing ventilator-associated pneumonia and the limited availability of mechanical ventilators. In addition, it can be due to poor quality of care, which is observed in the number of FASTHUG care. Hospitals should use severity scores (such as APACHE, SAPS II, and SOFA) as a crucial component at the ICU for improving clinical decisions and identifying patients with higher unexpected outcomes. Healthcare providers should also prioritize and give due attention to acutely ill patients like those with respiratory failure, lower GCS scores, and comorbidities. The application of standardized treatment protocols such as the FASTHUG bundle of care should also encouraged and applied regularly as it improves the quality of care and the favorable clinical outcomes. Future investigators should conduct a prospective follow-up study by including important variables such as severity scores and variables related to human resources, equipment, and quality of care.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Ethical clearance obtained from the Ethical Clearance Committee of Wollega University. The studies were conducted by the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin because the study was retrospective, and it was a card review.
Author contributions
FK: Conceptualization, Software, Supervision, Visualization, Writing – original draft, Writing – review & editing, Data curation, Formal analysis, Investigation, Methodology. GM: Conceptualization, Software, Supervision, Visualization, Writing – original draft, Writing – review & editing, Validation. MY: Conceptualization, Formal analysis, Methodology, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to thank Wollega University, the Institute of Health Science, and the Department of Public Health staff for their efforts in facilitating the student research project time frame. We would also like to express our gratitude to the ICU staff at Wollega University Referral Hospital and Nekemte Specialized Hospital. We are also grateful to the data collectors and supervisors for their commitment and dedication during the process of data collection.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
COPD, Chronic Obstructive Pulmonary Disease; ESV-ICD, Ethiopian Simplified Version of the International Classification of Diseases; FASTHUG, Feeding, Analgesia, Sedation, Thrombosis prophylaxis, Head elevation, Ulcer prophylaxis, Glucose control; GCS, Glasgow Coma Scale; LOS, length of stay.
References
1. Smith, SE. What is an ICU? wiseGEEK (2013); Available at: http://www.wisegeek.com/what-is-an-icu.htm
2. Marshall, JC, Bosco, L, Adhikari, NK, Connolly, B, Diaz, JV, Dorman, T, et al. What is an intensive care unit? A report of the task force of the world Federation of Societies of intensive and critical care Medicine. J Crit Care. (2017) 37:270–6. doi: 10.1016/j.jcrc.2016.07.015
3. Kelly, FE, Fong, K, Hirsch, N, and Nolan, JP. Intensive care medicine is 60 years old: the history and future of the intensive care unit. Clin Med. (2017) 14:376–9. doi: 10.7861/clinmedicine.14-4-376
4. Units, IC, Island, N, Icus, W, Medicine, CC, and Icu, A. What is an ICU? WFSICCM Reports. (2014), 2–3.
5. Dünser, MW, Baelani, I, and Ganbold, L. A review and analysis of intensive care medicine in the least developed countries. Crit Care Med. (2006) 34:1234–42. doi: 10.1097/01.CCM.0000208360.70835.87
6. Baker, T. Critical care in low-income countries. Trop Med Int Heal. (2009) 14:143–8. doi: 10.1111/j.1365-3156.2008.02202.x
7. Firew, T, Gebreyesus, A, Woldeyohannes, L, Ebrahim, F, and Patel, S. Human resources for emergency care systems in Ethiopia: challenges and triumphs. African J Emerg Med. (2020) 10:S50–5. doi: 10.1016/j.afjem.2020.09.006
8. Kifle, F, Boru, Y, Tamiru, HD, Sultan, M, Walelign, Y, Demelash, A, et al. Intensive Care in sub-Saharan Africa: a National Review of the service status in Ethiopia. Anesth Analg. (2021):1–8. doi: 10.1213/ANE.0000000000005799
9. Ay, E, Weigand, MA, Röhrig, R, and Gruss, M. Dying in the intensive care unit (ICU): a retrospective descriptive analysis of deaths in the ICU in a communal tertiary Hospital in Germany. Anesthesiol Res Pract. (2020) 2020:1–10. doi: 10.1155/2020/2356019
10. Orban, JC, Walrave, Y, Mongardon, N, Allaouchiche, B, Argaud, L, Aubrun, F, et al. Causes and characteristics of death in intensive care Units. Anesthesiology. (2017) 126:882–9. doi: 10.1097/ALN.0000000000001612
11. Rn, ME, Carter, Rn LW, Rn, KP, and Vincent, S. Factors associated with in-hospital mortality following ICU discharge: a comprehensive review. (2012);120–125.
12. Colpan, A, Akinci, E, Erbay, A, Balaban, N, and Bodur, H. Evaluation of risk factors for mortality in intensive care units: a prospective study from a referral hospital in Turkey. Am J Infect Control. (2017) 33:42–7. doi: 10.1016/j.ajic.2004.09.005
13. Du, B, An, Y, Kang, Y, Yu, X, Zhao, M, Ma, X, et al. Characteristics of critically ill patients in ICUs in mainland China. Crit Care Med. (2013) 41:84–92. doi: 10.1097/CCM.0b013e31826a4082
14. C44. Critical Illness Predictors and Outcomes. Mortality rate and associated factors among intensive care unit patients at Mulago hospital, Uganda: a prospective cohort study (2022). Available at: https://www.atsjournals.org/doi/abs/10.1164/ajrccm-conference.2014.189.1_MeetingAbstracts.A4521
15. Lalani, HS, Waweru-Siika, W, Mwogi, T, Kituyi, P, Egger, JR, Park, LP, et al. Intensive care outcomes and mortality prediction at a National Referral Hospital in Western Kenya. Ann Am Thorac Soc. (2018) 15:1336–43. doi: 10.1513/AnnalsATS.201801-051OC
16. Mohammed, SO, Abdi, OA, and Getish, BG. Clinical outcomes of patients admitted in intensive care units of Nigist Eleni Mohammed memorial Hospital of Hosanna, southern Ethiopia. Int J Med Med Sci. (2017) 9:79–85. doi: 10.5897/IJMMS2017.1297
17. Abate, SM, Assen, S, Yinges, M, and Basu, B. Survival and predictors of mortality among patients admitted to the intensive care units in southern Ethiopia: a multi-center cohort study. Ann Med Surg. (2021) 65:102318. doi: 10.1016/j.amsu.2021.102318
18. Kedir, S, Berhane, A, Bayisa, T, and Wuletaw, T. Admission patterns and outcomes in the medical intensive care unit of St. Paul’s hospital millennium medical college, Addis Ababa, Ethiopia. Ethiop Med J. (2017) 55:19–26.
19. Sultan, M, Mengistu, G, Debebe, F, Azazh, A, and Trehan, I. The burden on emergency centers to provide care for critically ill patients in Addis Ababa, Ethiopia. African J Emerg Med. (2018) 8:150–4. doi: 10.1016/j.afjem.2018.07.006
20. Gidey, K, and Abraha, HA. Pattern and outcome of medical intensive care unit admission to Ayder Càmprehensive specialised hospitalised Hospital in Tigray, Etiopia. Ethiop Med J. (2018) 56:31–6.
21. Tessema, HG, Lema, GF, Mesfin, N, Fentie, DY, and Arefaynie, NR. Admission pattern, clinical outcomes, and associated factors among patients admitted in medical intensive care unit at University of Gondar Comprehensive and Specialized Hospital, Northwest Ethiopia, 2019. A retrospective cross-sectional study (2019):1–23. doi: 10.21203/rs.2.13346/v1,
22. Smith, ZA, Ayele, Y, and McDonald, P. Outcomes in critical care delivery at Jimma University specialised hospital. Ethiopia Anaesth Intensive Care. (2013) 41:363–8. doi: 10.1177/0310057X1304100314
23. Schultz, MJ, Dunser, MW, Dondorp, AM, Adhikari, NKJ, Iyer, S, Kwizera, A, et al. Current challenges in the management of sepsis in ICUs in resource-poor settings and suggestions for the future. Intensive Care Med. (2017) 43:612–24. doi: 10.1007/s00134-017-4750-z
24. Intensive care units (ICUs). (2021). Available at: https://www.healthywa.wa.gov.au/Articles/F_I/Intensive-care-units-ICUs
25. Aung, YN, Nur, AM, Ismail, A, and Aljunid, SM. Characteristics and outcome of high-cost ICU patients. Clin Outcomes Res. (2019) 11:505–13. doi: 10.2147/CEOR.S209108
26. McLaughlin, AM, Hardt, J, Canavan, JB, and Donnelly, MB. Determining the economic cost of ICU treatment: a prospective “micro-costing” study. Intensive Care Med. (2017) 35:2135–40. doi: 10.1007/s00134-009-1622-1
27. Lone, NI, Gillies, MA, Haddow, C, Dobbie, R, Rowan, KM, Wild, SH, et al. Five-year mortality and hospital costs associated with surviving intensive care. Am J Respir Crit Care Med. (2016) 194:198–208. doi: 10.1164/rccm.201511-2234OC
28. Kehali, H, Berhane, Y, and Gize, A. A phenomenological study on the lived experiences of families of ICU patients, Addis Ababa, Ethiopia. PLoS One. (2020) 15:e0244073. doi: 10.1371/journal.pone.0244073
29. Sprent, P. An Introduction to categorical data analysis. J R Stat Soc A Stat Soc. (2007) 170:1178–8. doi: 10.1111/j.1467-985X.2007.00506_2.x
31. Zhang, J, and Yu, KF. What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA J Am Med Assoc. (1998) 280:1690–1. doi: 10.1001/jama.280.19.1690
32. von Elm, E, Altman, DG, Egger, M, Pocock, SJ, Gotzsche, PC, and Vandenbroucke, JP. STROBE eigen doc (from the Equator) (2008) 1:12–3. Available at: http://www.epidem.com/
33. Summers, C, Singh, NR, Worpole, L, Simmonds, R, Babar, J, Condliffe, AM, et al. Incidence and recognition of acute respiratory distress syndrome in a UK intensive care unit. Thorax. (2016) 71:1050–1. doi: 10.1136/thoraxjnl-2016-208402
34. Pinheiro, FGDMS, Santos, ES, Barreto, DDC, Weiss, C, Vaez, AC, Oliveira, JC, et al. Mortality predictors and associated factors in patients in the intensive care unit: a cross-sectional study. Crit Care Res Prac. (2020) 2020:1–6. doi: 10.1155/2020/1483827
35. Capuzzo, M, Volta, CA, Tassinati, T, Moreno, RP, Valentin, A, Guidet, B, et al. Hospital mortality of adults admitted to intensive care units in hospitals with and without intermediate care units: a multicentre European cohort study. Crit Care. (2014) 18:1–15. doi: 10.1186/s13054-014-0551-8
36. Papazian, L, Klompas, M, and Luyt, CE. Ventilator-associated pneumonia in adults: a narrative review. Intensive Care Med. (2020) 46:888–906. doi: 10.1007/s00134-020-05980-0
37. Weingarten, S, Bolus, R, Riedinger, MS, Maldonado, L, Stein, S, and Ellrodt, AG. The principle of parsimony: the Glasgow coma scale score predicts mortality as well as the Apache II score for stroke patients. Stroke. (1990) 21:1280–2. doi: 10.1161/01.STR.21.9.1280
38. Grimaldi, D, Hraiech, S, Boutin, E, Lacherade, JC, Boissier, F, Pham, T, et al. Hypoxemia in the ICU: prevalence, treatment, and outcome. Ann Intensive Care. (2018) 8: 8–9. doi: 10.1186/s13613-018-0424-4
39. Mejía, F, Medina, C, Cornejo, E, Morello, E, Vásquez, S, Alave, J, et al. Oxygen saturation as a predictor of mortality in hospitalized adult patients with COVID-19 in a public hospital in Lima, Peru. PLoS One. (2020) 15:1–12. doi: 10.1371/journal.pone.0244171
41. Kwizera, A, Dünser, M, and Nakibuuka, J. National intensive care unit bed capacity and ICU patient characteristics in a low-income country. BMC Res Notes. (2012) 5:4–6. doi: 10.1186/1756-0500-5-475
42. Unal, AU. Prognosis of patients in a medical intensive care unit. North Clin Istanbul. (2016) 2:189–95. doi: 10.14744/nci.2015.79188
43. MedskEDSK, E, Khani, Y, Hashemi-Nazari, SS, Izadi, N, Eshrati, B, and Mehrabi, Y. Survival rate in patients with ICU-acquired infections and its related factors in Iran’s hospitals. BMC Public Health. (2021) 21:1–9.
44. Simpson, A, Puxty, K, McLoone, P, Quasim, T, Sloan, B, and Morrison, DS. Comorbidity and survival after admission to the intensive care unit: a population-based study of 41,230 patients. J Intensive Care Soc. (2021) 22:143–51. doi: 10.1177/1751143720914229
45. El-Adawy, A, Khafagy, M, El Adawi, N, Bahgat, M, and El-Gilany, AH. Intensive care morbidity and mortality and their associated factors: a National Study in Egypt. Benha Med J. (2021) 39:52. doi: 10.21608/bmfj.2021.62776.1383
46. Barrera, JB, Correa, JC, and Ruiz, MLAMR. Application of the FAST-HUG protocol and its association with the mortality of the critical patient in the ICU. Medicina Crítica. (2018):130–8.
Keywords: ICU, mortality, incidence, predictors, Western Ethiopia
Citation: Kebede F, Mosisa G and Yilma M (2024) Incidence and predictors of mortality among patients admitted to adult intensive care unit at public hospitals in Western Ethiopia: a retrospective cohort study. Front. Med. 11:1370729. doi: 10.3389/fmed.2024.1370729
Edited by:
Ifeoma Ekwere, Johns Hopkins University, United StatesReviewed by:
Jesus Rico-Feijoo, Hospital Universitario Río Hortega, SpainImaobong Chinedozi, Johns Hopkins University, United States
Copyright © 2024 Kebede, Mosisa and Yilma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fetene Kebede, ZmV0eWtlYkBnbWFpbC5jb20=
 Fetene Kebede
Fetene Kebede Getu Mosisa
Getu Mosisa Mekdes Yilma
Mekdes Yilma