- 1Department of Medical Education, School of Medical Education and Learning Technology, Shahid Beheshti University of Medical Sciences, Tehran, Iran
- 2HIV/STI Surveillance Research Center, and WHO Collaborating Center for HIV Surveillance, Institute for Futures Studies in Health, Kerman University of Medical Sciences, Kerman, Iran
- 3Student Research Committee, Tabriz University of Medical Sciences, Tabriz, Iran
- 4Research Center for Integrative Medicine in Aging, Aging Research Institute, Tabriz University of Medical Sciences, Tabriz, Iran
- 5Department of Microbiology, School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Background: The coronavirus disease 2019 (COVID-19) pandemic affected many aspects of lifestyle and medical education during the recent years. We aimed to determine the impacts of COVID-19 pandemic on medical education to provide an overview of systematic reviews on it.
Methods: We searched PubMed, Scopus, Web of Science, Cochrane library, Google Scholar, and medRxiv, with the following keywords: “SARS-CoV-2,” “COVID-19,” “Medical Education,” “E-learning,” “Distance Education,” “Online Learning,” “Virtual Education,” “systematic review,” and “meta-analysis,” up to 15 April 2023. Studies were included if they were systematic reviews assessing the impacts of the COVID-19 pandemic on medical sciences students. We used A MeaSurement Tool to Assess systematic Reviews 2 (AMSTAR-2) checklist for quality assessment.
Results: A total of 28 systematic reviews were included. The eligible reviews included between five and 64 primary studies, ranging from 897 to 139,381 participants. Technology-enhanced learning and simulation-based learning were the most frequently used strategies. Virtual teaching has several drawbacks like technical difficulties, confidentiality problems, lower student involvement, connection problems, and digital fatigue. The overall satisfaction rate for online learning was above 50%. Also, favorable opinions about perception, acceptability, motivation, and engagement were reported. The quality of 27 studies were critically low and one was low.
Conclusion: There were reduced clinical exposure and satisfaction for medical students during the pandemic. Further high-quality systematic reviews are required.
1 Introduction
Following the World Health Organization declaration on the coronavirus disease 2019 (COVID-19) as a pandemic, different countries have implemented measures like quarantine and lockdown on cities to control the spread of the virus (1). As a results, it has several mental health consequences like anxiety, depression and post-traumatic stress disorder (2). Moreover, fatigue, headache, and attention disorders were three most common long-term adverse events of COVID-19 (3). Following the initiation of COVID-19 vaccination, other complications like thrombotic events and myocarditis were occurred (4).
Following the closure of educational institutes, over 91% of students have been affected (5). It led to a significant learning deficit in students, especially in regions with low socioeconomic status (6). The pandemic also resulted in economic challenges for universities to find money for their staff, facilities, and research projects (7). Transition from face-to-face to online learning leads to challenges and opportunities for teacher education (8). Regarding the medical education, shifting to online distance education, reduced interpersonal interaction and limited opportunities to practice interviewing (9). Furthermore, the written or clinical examinations have been postponed and a debate between open and close book examinations has been arisen (9). There are several concerns for medical students for career choice, including the impossibility of pursuing desired specialties, the removal of elective courses and core rotations during the pandemic (10). On the other hand, roles of medical students in the frontline of the pandemic can lead to gaining clinical experiences about infected patients, despite an increase in exposure and risk of affecting by COVID-19 (11).
While we acknowledge that the COVID-19 pandemic has receded, its long-term effects on medical education, both positive and negative, are still emerging. The lessons learned from this pandemic are crucial for preparing for future health crises that might necessitate quarantines and isolations. Therefore, the topic remains highly relevant. Several previous systematic reviews have evaluated the effects of COVID-19 pandemic on education, satisfaction and assessments of students of medical sciences. However, their findings are dispersed. To our knowledge, no previous umbrella review has comprehensively examined the impact of the COVID-19 pandemic across various fields of medical education. Although several systematic and scoping reviews have explored specific aspects, there has been no study that synthesizes these findings to provide consolidated recommendations and insights. Furthermore, an umbrella review is essential to evaluate the quality of these systematic reviews. This study aims to fill that gap by offering a comprehensive analysis and assessment of existing literature on the subject. Therefore, we aimed to conduct an umbrella review to evaluate the current evidence regarding the medical education during the COVID-19 pandemic.
2 Method
2.1 Search strategy
We searched PubMed, Scopus, Web of Science, and Cochrane library up to April 15, 2023. Also, the first 300 results of the medRxiv preprint server and the Google Scholar search engine were searched up to April 28, 2033. No limitations on the search fields, such as language, date or study type was implemented. Backward and forward citation searching of the included studies were conducted. The relevant search terms were a combination of the following keywords: (“SARS-CoV-2” OR “COVID-19″) AND (“Medical Education” OR “E-learning” OR “Distance Education” OR “Online Learning” OR “Virtual Education”) AND (“Systematic Review” OR “Meta-analysis”) (Supplementary Table S1).
2.2 Study selection
All of the identified articles were exported to the EndNote software version 8.1. Following duplicate removal, two authors independently screened the title and abstracts of the articles. Then, the same ones reviewed the full-texts of the remaining papers. Any discrepancies between the two groups were resolved by discussion or consultation with a third author. The inclusion criteria were those systematic reviews (with or without meta-analysis) evaluating the impact of COVID-19 pandemic on medical education. The exclusion criteria were as follow: (1) study types other than systematic reviews, such as cross-sectional, case-control, cohort or clinical trials; (2) studies using a systematic approach such as living or rapid systematic reviews; (3) systematic reviews on preclinical or animal studies; (4) studies that investigated medical education before the COVID-19 pandemic; and (5) studies not included medical sciences students.
2.3 Data extraction
We used a predesigned table in Microsoft Office Word for data extraction. Two researchers extracted the following information from each included study and performed the quality assessment and disagreements were resolved with discussion: basic information (e.g., first author’s name, year of publication and journals), search date and relevant databases, number of included articles, sample size, study designs of the included articles, quality assessment tools, participants’ age and sex, summary of key findings of each study.
2.4 Quality assessment
We used “A Measurement Tool to Assess Systematic Reviews 2 (AMSTAR 2)” checklist for quality assessment of included studies (12). Seven of the 16 items on this checklist—protocol registration, adequate literature search, justification for excluding individual studies, risk of bias from the inclusion of individual studies, appropriateness of the meta-analytical methods, consideration the risk of bias when interpreting the review’s findings, and assessment of the presence and likely impact of publication bias—are regarded as critical domains. The checklist does not produce an overall grade; instead, it offers a total assessment based on flaws found in the crucial areas. There are four qualitative levels of confidence in the review’s findings: “high” for no or one non-critical weakness, “moderate” for more than one non-critical weakness, “low” for one critical weakness with or without non-critical weaknesses, and “critically low” more than one critical weakness with or without non-critical weaknesses for the overall level of confidence.
2.5 Data synthesis
Due to the high heterogeneity between studies and since most of the included systematic reviews were only reported qualitative data, meta-analysis was not be performed in this study and the data were reported qualitatively and in the form of tables.
3 Results
3.1 Literature search
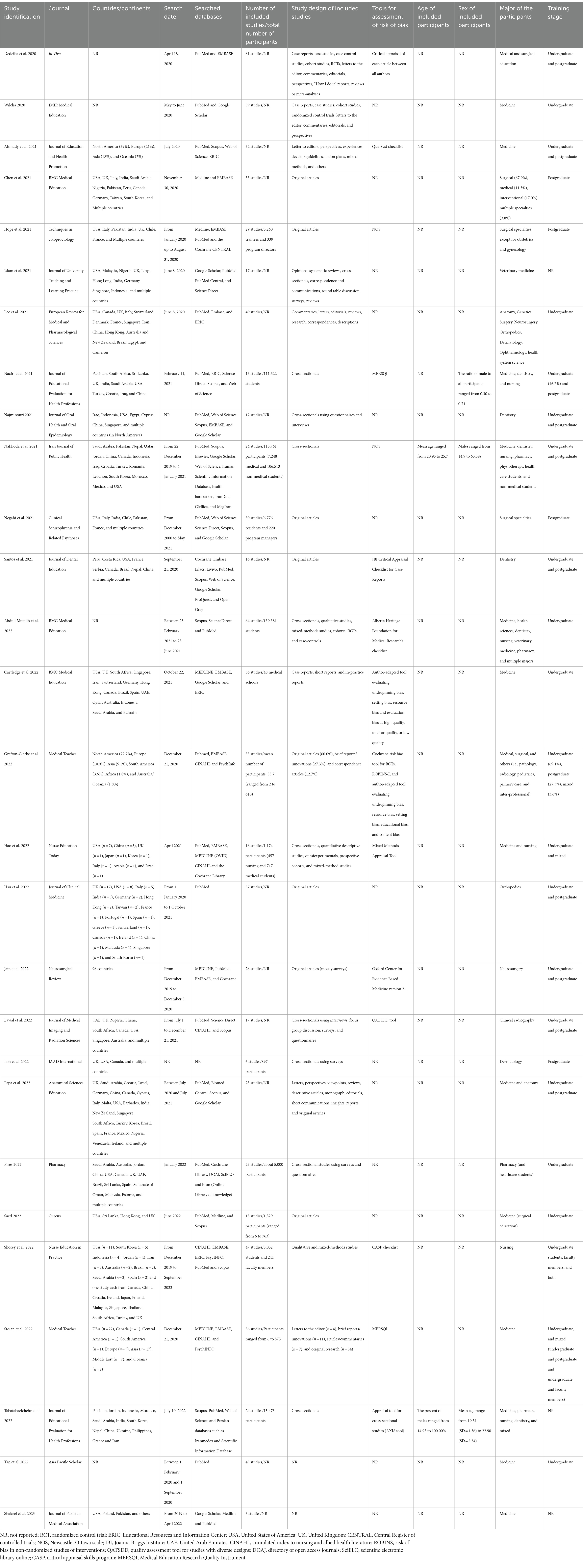
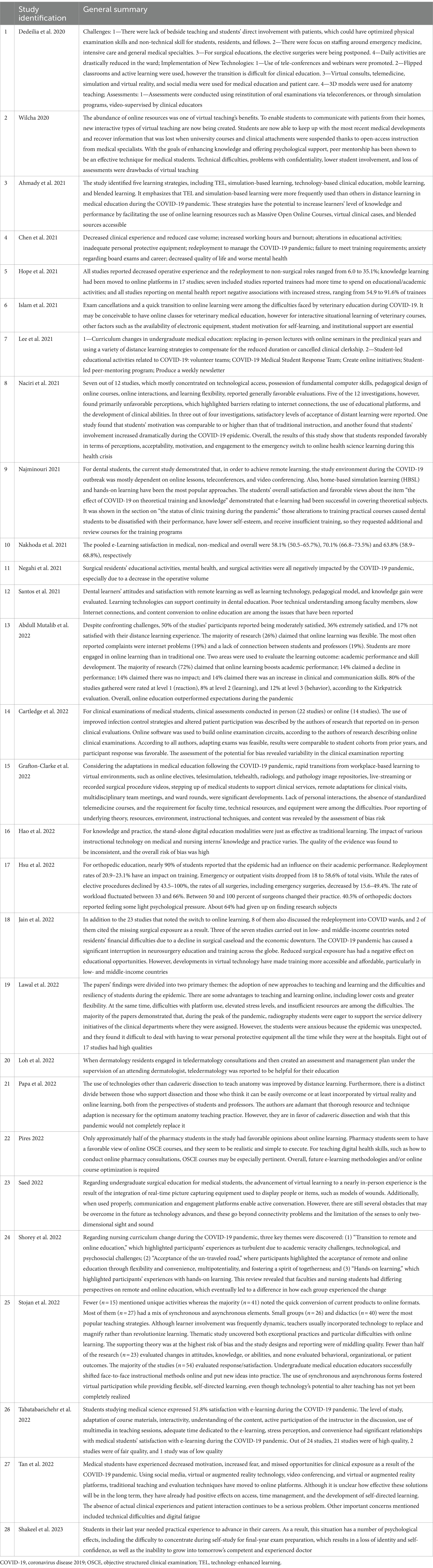
The systematic search identified a total of 815 studies, which came from PubMed (n = 136), Scopus (n = 397), the Web of Science (n = 279), the Cochrane library (n = 3). Following the removal of duplicate studies, the remaining 521 studies were screened and 47 publications were selected for full text review. After evaluating the other 47 articles for eligibility, 19 studies were excluded for the following reasons: 12 studies were not conducted during the COVID-19 pandemic (13–24), four did not evaluate medical education (25–28), two did not have eligible study designs (29, 30), and one was not conducted on students of medical sciences (31). No additional relevant studies were found in medRxiv, Google Scholar, or backward and forward citation searching. Finally, 28 articles met the eligibility criteria and were included (32–59) (Figure 1).
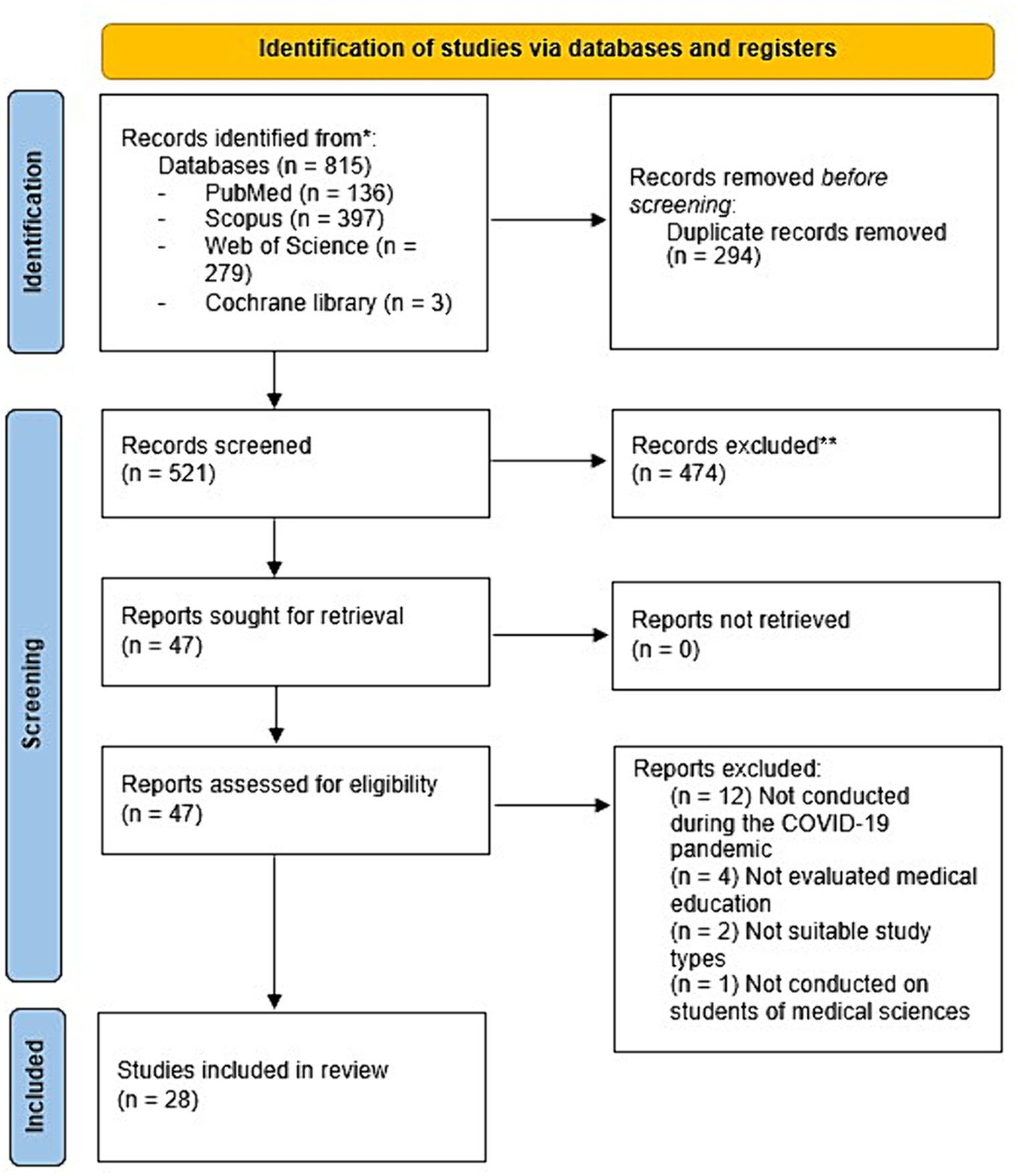
Figure 1. Flowchart of the study selection process. A systematic search yielded 815 studies from PubMed (n = 136), Scopus (n = 397), Web of Science (n = 279), and the Cochrane Library (n = 3). After removing duplicates, 521 studies were screened, and 47 were selected for full-text review. Of these, 19 were excluded due to various reasons: 12 were not related to the COVID-19 pandemic, four did not focus on medical education, two had ineligible study designs, and one was not on medical sciences students. Additional hand searching in medRxiv, Google Scholar, and through citation tracking did not yield further studies. In the end, 28 articles met the inclusion criteria.
3.2 Characteristics of the included studies
The included articles were all published in English and published from 2020 to 2023. They were published in 25 different journals in which BMC Medical Education (n = 3) and Medical Teacher (n = 2) were the most common ones. The primary studies conducted in almost all continents, most commonly in the United States, the United Kingdom, Canada, and multiple countries. The eligible reviews included between five and 64 primary studies, ranging from 897 to 139,381 participants. Studies used different quality appraisal tools which Newcastle–Ottawa scale (n = 2) and Medical Education Research Quality Instrument (n = 2) were the most commonly used. Studies evaluated undergraduate, postgraduate or both of them in clinical medicine or its specialties, as well as other health sciences like nursing, pharmacy, veterinary medicine, dentistry, clinical radiography, or mixed of them. Only one study conducted the meta-analysis (41) (Table 1).
3.3 Outcomes
3.3.1 Medicine
Ten studies evaluated the education of undergraduate and postgraduate medical students during this pandemic (32–34, 45, 46, 52, 54, 56, 58, 59). The pandemic had some challenges like decreased motivation and clinical exposure, increased fear, reduction in bed-side teaching and daily ward activities, as well as postponing elective surgeries (32, 58). However, it led to opportunities like use of teleconference, flipped classrooms, virtual consults, live-streaming or recorded surgical procedure videos, development of online resources and peer mentorship, remote clinical visits, multidisciplinary team meetings, and developments of three-dimensional models (32, 33, 46). Technology-enhanced learning and simulation-based learning, as well as small groups and didactics were the most frequently used teaching strategies during the period (34, 56). Several methods for online assessment and clinical examination like simulation programs and video-supervision by clinical educators and comparing the responses with prior studies showed acceptable participants’ responses (32, 45) (Table 2).
Virtual teaching has several drawbacks like technical difficulties, confidentiality problems, lower student involvement, restriction of involved senses to sight and sound, connection problems, and digital fatigue (33, 54, 58). However, it can provide flexible, easy access and self-directed learning and improved time management (56, 58) (Table 2).
For anatomy teaching, there is a discrepancy between those support virtual reality and those in favor of cadaver dissection and they recommend that resource and technical developments are necessary for optimal anatomy teaching (52). Another study evaluated the psychological effects of the pandemic on last-year medical students and mentioned loss of identity and self-confidence as the consequences of virtual learning (59) (Table 2).
3.3.1.1 Surgery
Two studies evaluated the effects of COVID-19 on education of residents of surgical specialties (36, 42). The studies reported decreased operative experiences which led to negative effects on mental health, as well as educational and surgical activities (36, 42). Also, the frequency of stress and redeployment to non-surgical roles increased from 54.9 to 91.6% and 6.0 to 35.1%, respectively (36) (Table 2).
3.3.1.2 Orthopedics
The study by Hsu and colleagues evaluated orthopedics education during the pandemic and showed redeployment of 20.9–23.1% participants, 18.0–58.6% decrease in emergency or outpatient visits, and 15.6–49.4% decrease in all surgeries (48). Also, 40.5% of orthopedic doctors reported psychological pressure and 50–100% changed their practice (48) (Table 2).
3.3.1.3 Neurosurgery
Jain et al. reported financial difficulties and educational opportunities for neurosurgery education due to decreased surgical exposure (49). However, virtual technology developments provided accessible and affordable training (49) (Table 2).
3.3.1.4 Dermatology
The article by Loh and colleagues included six studies consisting of 897 dermatology residents revealed that teledermatology can be helpful for their education under the supervision of an attending dermatologist (51) (Table 2).
3.3.2 Dentistry
Two systematic reviews including 12 and 16 studies evaluated the effects of COVID-19 pandemic on undergraduate and postgraduate dentistry students (40, 43) (Table 1). During the pandemic, home-based simulation learning and hands-on learning were the most frequent approaches which reported appropriate coverage of theoretical concepts, while there were dissatisfactions with their practical trainings (40). Overall, online learning technologies can be used to continue dental education despite some problems like low technical understanding among faculty members and slow Internet connections (43) (Table 2).
3.3.3 Pharmacy
The systematic review by Pires on 23 primary studies showed about half of undergraduate pharmacy students did not have satisfying opinions about online learning, whereas objective structured clinical examination was a suitable option for health skills like how to conduct online pharmacy consultations (53) (Table 2).
3.3.4 Nursing
The systematic review by Shorey et al. revealed three changes in nursing curriculum which were transition to online education, acceptance of remote education, and experiences with hands-on learning (55). Undergraduate nursing students and faculty members had various perspectives about this type of education which led to act in different ways (55). Improving remote learning platforms and augmented virtual stimulation are recommended ways for nursing education in pandemics (55) (Table 2).
3.3.5 Veterinary medicine
The systematic review by Islam and colleagues on 17 eligible studies reported that exam cancellation and rapid transition to online learning as the most prominent problems for veterinary students (37). Although it is feasible for veterinary students to have online classes, there are issues such as low availability of electronic equipment and institutional supports (37) (Table 2).
3.3.6 Clinical radiography
The article by Lawal et al. showed some pros (e.g., lower costs and higher flexibility) and cons (e.g., problems with use of platforms and insufficient resources) for clinical radiography students during the pandemic (50) (Table 2).
3.3.7 Mixed disciplines
Seven articles included participants of mixed majors of health sciences (35, 38, 39, 41, 44, 47, 57). One of the studies conducted a meta-analysis to compare the satisfaction rate of medical and non-medical students regarding e-learning which were 58.1 and 70.1%, respectively (41). Moreover, 36 and 50% of undergraduate health science students were extremely and moderately satisfied with online education, respectively (44). In addition, 72% reported improvements in academic performance and 14% in clinical skills (44). In this regard, online education was as effective as traditional methods in terms of knowledge and practice (47) with a satisfaction rate of 51.8% for medical sciences students (57). Favorable opinions about perception, acceptability, motivation, and engagement have been reported (39), while it had some issues like burnout and decreased quality of life and anxiety for the exams (35, 39). To deal with the transition, some student-led educational activities like COVID-19 medical student response team and student-led peer-mentoring program have been developed (38) (Table 2).
3.4 Quality assessment
The quality assessment results showed 27 (96.4%) were critically low and one (3.6%) was low. Among the critical domains, the most common problem was not considering to report the source of funding in the included studies and justifying and discussing the observed heterogeneity in the included studies (Supplementary Table S2).
4 Discussion
The results of our umbrella review on 28 systematic reviews showed a reduction in clinical and surgical exposure, as well as bed-side teaching which were the most common problems of online education. There were some problems like technical problems and insufficient resources with virtual learning. The satisfaction of medical students with online learning was low to moderate and clinical skills need the most attention.
In accordance with our findings, the results of an international survey on 1,604 participants from 45 countries showed that 81.4% of participants reported negative impacts of COVID-19 on medical education (60). We also found that reduced educational activities and surgeries, especially for surgery-related specialties led to dissatisfaction, psychological pressure, and redeployment. The abovementioned study also found that reduced in-person and ward teaching had a significant negative impact on medical education (60). Several alternative methods like problem-based learning techniques, virtual meetings, remote clinical visits, or live-streaming procedures were also developed in response to COVID-19 (61, 62). Moreover, results of one of the studies on clinical examination of medical students showed comparable results with before the COVID-19 pandemic (45). Also, postponing or cancellation of exams were other problems caused by the pandemic for students of medical sciences. In this regard, there are debates whether use open or closed book examinations and methods used for grading (9). It seems that both types of open and closed book examinations can be used for blended assessment during or post-pandemics (9).
COVID-19 had several consequences on mental health of students of health sciences like increase of fear and depression. In the same way with our findings, a meta-analysis of 41 studies on 36,608 medical students showed pooled prevalence of 37.9 and 33.7% for depression and anxiety among medical students, respectively (63). Furthermore, it led to higher levels of stress, in addition to emotional and behavioral changes among medical students (64). In an effort to encourage prospering during COVID-19, innovative wellness initiatives and mental health counseling programs for medical students are suggested (65).
Dental students were not satisfied with practical and hands-on practices during the pandemic, as our results suggested. Arponen et al. who evaluated the dentistry students’ performance on examinations showed no significant improvement in examinations of undergraduate dentistry students during the COVID-19 pandemic (66). The differences could be due to study design and number of participants in the studies. To improve the quality of teaching strategies like development of virtual reality, inter-institutional training programs, virtual computerized patients, and facilitating access to online learning resources are recommended (67). Adaptation in the curriculum of dental education with embracing new technologies and simulation-based training should be also considered after the pandemic (68).
Our findings showed dissatisfaction about online learning in approximately half of pharmacy students. Results of a questionnaire on 482 pharmacy students showed limited hospital training, problems with concentration for a long time, and technical problems like the Internet access problems and poor gadgets functioning as barriers of virtual learning during the COVID-19 pandemic (69). Implementation and development of interactive pedagogical methods like computer-based simulation in pharmacy education can help improvements of pharmacy education in the post-pandemic era (70).
Hands-on learning experiences and online learning transitions were among the changes that were occurred in medical and nursing curriculum during the pandemic. Gaur et al. also revealed transition to emergency remote teaching and assessments environments like virtual simulation and artificial intelligence that can be used in the post-COVID era (71). Previous research suggested five challenges for online education transition, including integration of learning tools, technology access, online proficiency of staff and students, academic dishonesty, and confidentiality and security, that should be considered for improving medical education curriculums (72).
The quality of all of the included systematic reviews in the present study were critically low except for one study with low quality. Previous umbrella reviews which were conducted on different aspects of COVID-19 showed that most of the studies had critically low, low, or moderate quality (73–75). Therefore, it sounds that the primary and secondary studies that were conducted during the COVID-19 pandemic had high risk of bias, so further high-quality research are required. Also, it should be considered that the findings should be interpreted with caution.
Despite conduction of several systematic reviews on the effects of COVID-19 pandemic on medical education, to our best of knowledge, no previous umbrella review was conducted to evaluate the quality of them and summarize the findings. So, it is one of the pioneer studies that was conducted on systematic reviews on medical education and COVID-19. However, it has several limitations that should be considered. Firstly, most of our studies were focused on students of medicine, while there are limited ones on dentistry, nursing, pharmacy, and veterinary medicine students. Therefore, further studies on other specialties are suggested. Secondly, despite searching different databases and conduction of grey literature search, we cannot rule out the possibility of missing some suitable studies. Also, we searched for preprints that are not peer-reviewed in order to reduce the possibility of missing relevant systematic review, but no eligible study was found in medRxiv. Thirdly, only one study conducted meta-analysis, so we could not perform meta-analysis and only conducted qualitative synthesis. Fourthly, the protocol of the umbrella review was not registered in the International Prospective Register of Systematic Reviews (PROSPERO) due to the necessity to conduct and report the findings soon. Nevertheless, it was submitted to and approved by the relevant committee in the university. Fifthly, the age and sex of participants included in the systematic reviews were not reported, as a result we could not prepare the COVID-19 impacts on medical education by age and sex. Sixthly, the included studies did not report data on second-tier courses (e.g., legal medicine). So, the specific data on these courses were not provided in the current umbrella review. It is suggested that future original articles and systematic reviews consider evaluation of the effects of the COVID-19 pandemic on these types of courses.
5 Conclusion
There were reduced clinical exposure during the pandemic, so teleconference and flipped classrooms were most used for virtual teaching. There was reduced satisfaction for medical students, especially for clinical skills, while online education was effective for knowledge. Further high-quality systematic reviews on the effects of COVID-19 pandemic on medical education are recommended.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
SN: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. ZK: Conceptualization, Methodology, Project administration, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing. AF: Data curation, Writing – original draft, Writing – review & editing. MN: Conceptualization, Investigation, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to acknowledge the support of the Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2024.1358084/full#supplementary-material
References
1. Nejadghaderi, SA, Saghazadeh, A, and Rezaei, N. Health care policies and COVID-19 prevalence: is there any association? Int J Health Serv. (2022) 52:9–22. doi: 10.1177/0020731421993940
2. Xiong, J, Lipsitz, O, Nasri, F, Lui, LMW, Gill, H, Phan, L, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. (2020) 277:55–64. doi: 10.1016/j.jad.2020.08.001
3. Lopez-Leon, S, Wegman-Ostrosky, T, Perelman, C, Sepulveda, R, Rebolledo, PA, Cuapio, A, et al. More than 50 long-term effects of COVID-19: a systematic review and meta-analysis. Sci Rep. (2021) 11:16144. doi: 10.1038/s41598-021-95565-8
4. Sadeghalvad, M, Mansourabadi, AH, Noori, M, Nejadghaderi, SA, Masoomikarimi, M, Alimohammadi, M, et al. Recent developments in SARS-CoV-2 vaccines: a systematic review of the current studies. Rev Med Virol. (2023) 33:e2359. doi: 10.1002/rmv.2359
5. Zhu, X, and Liu, J. Education in and after Covid-19: immediate responses and long-term visions. Postdigital Sci Educ. (2020) 2:695–9. doi: 10.1007/s42438-020-00126-3
6. Betthäuser, B, Bach-Mortensen, A, and Engzell, P. A systematic review and meta-analysis of the impact of the COVID-19 pandemic on learning. LIEPP Working Paper. (2022) 134. doi: 10.31235/osf.io/g2wuy
7. Burki, TK . COVID-19: consequences for higher education. Lancet Oncol. (2020) 21:758. doi: 10.1016/S1470-2045(20)30287-4
8. Flores, MA, and Swennen, A. The COVID-19 pandemic and its effects on teacher education. Eur J Teach Educ. (2020) 43:453–6. doi: 10.1080/02619768.2020.1824253
9. Papapanou, M, Routsi, E, Tsamakis, K, Fotis, L, Marinos, G, Lidoriki, I, et al. Medical education challenges and innovations during COVID-19 pandemic. Postgrad Med J. (2022) 98:321–7. doi: 10.1136/postgradmedj-2021-140032
10. Fodje, T, and Choo, E. Applying for residency in the time of COVID-19. Lancet. (2020) 396:1718. doi: 10.1016/S0140-6736(20)32476-4
11. Bank IWijnen-Meijer, M . Why should medical students (not) be recruited to care for patients with COVID-19? BMC Med Educ. (2020) 20:342. doi: 10.1186/s12909-020-02261-8
12. Shea, BJ, Reeves, BC, Wells, G, Thuku, M, Hamel, C, Moran, J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. (2017) 358:j4008. doi: 10.1136/bmj.j4008
13. Abualadas, HM, and Xu, L. Achievement of learning outcomes in non-traditional (online) versus traditional (face-to-face) anatomy teaching in medical schools: a mixed method systematic review. Clin Anat. (2023) 36:50–76. doi: 10.1002/ca.23942
14. Co, M, Cheung, KYC, Cheung, WS, Fok, HM, Fong, KH, Kwok, OY, et al. Distance education for anatomy and surgical training—a systematic review. Surgeon. (2022) 20:e195–205. doi: 10.1016/j.surge.2021.08.001
15. de Lima, ACB, dos Santos, DCM, de Almeida, SL, da Silva, EL, and Pereira, E. Hybrid education in healthcare education: a systematic review. Rev Cuid. (2022) 13:17. doi: 10.15649/cuidarte.2051
16. Kim, JY, and Kim, ME. Can online learning be a reliable alternative to nursing students? Learning during a pandemic?—A systematic review and meta-analysis. Nurse Educ Today. (2023) 122:8.
17. Mulyadi, M, Lea, BO, Malara, RT, Bidjuni, HJ, and Knowledge, E, (Eds.), The effectiveness of blended learning in basic life support training among nursing students: a systematic review. 4th International Virtual Conference on Nursing (IVCN); (2020), 30; STIKep PPNI Jawa, Bandung, INDIA DUBAI: Knowledge E; 402–414.
18. Nowell, L, Dhingra, S, Carless-Kane, S, McGuinness, C, Paolucci, A, Jacobsen, M, et al. A systematic review of online education initiatives to develop students remote caring skills and practices. Med Educ Online. (2022) 27:11. doi: 10.1080/10872981.2022.2088049
19. Patano, A, Cirulli, N, Beretta, M, Plantamura, P, Inchingolo, AD, Inchingolo, AM, et al. Education Technology in Orthodontics and Paediatric Dentistry during the COVID-19 pandemic: A systematic review. Int J Environ Res Public Health. (2021) 18:116056. doi: 10.3390/ijerph18116056
20. Rahayuwati, L, Pramukti, I, and Susanti, RD. The effectiveness of tele-education for health field university students as a learning method during a covid-19 pandemic: a systematic review. Open Access Maced J Med Sci. (2021) 9:159–63. doi: 10.3889/oamjms.2021.7350
21. Romli, MH, Yunus, FW, Cheema, MS, Hamid, HA, Mehat, MZ, Hashim, NFM, et al. A Meta-synthesis on technology-based learning among healthcare students in Southeast Asia. Med Sci Educ. (2022) 32:657–77. doi: 10.1007/s40670-022-01564-3
22. Santos, VA, Barreira, MP, and Saad, KR. Technological resources for teaching and learning about human anatomy in the medical course: systematic review of literature. Anat Sci Educ. (2022) 15:403–19. doi: 10.1002/ase.2142
23. Savage, AJ, McNamara, PW, Moncrieff, TW, and O’Reilly, GM. Review article: E-learning in emergency medicine: a systematic review. Emerg Med Australas. (2022) 34:322–32. doi: 10.1111/1742-6723.13936
24. Wu, YJ, Fan, YF, Sun, S, Chien, CY, and Wu, YE. Perceptions of medical students towards and effectiveness of online surgical curriculum: a systematic review. BMC Med Educ. (2021) 21:8. doi: 10.1186/s12909-021-03014-x
25. Akudjedu, TN, Mishio, NA, Elshami, W, Culp, MP, Lawal, O, Botwe, BO, et al. The global impact of the COVID-19 pandemic on clinical radiography practice: a systematic literature review and recommendations for future services planning. Radiography. (2021) 27:1219–26. doi: 10.1016/j.radi.2021.07.004
26. Lo, CK, and Hew, KF. Design principles for fully online flipped learning in health professions education: a systematic review of research during the COVID-19 pandemic. BMC Med Educ. (2022) 22:720. doi: 10.1186/s12909-022-03782-0
27. Pallavicini, F, Pepe, A, Clerici, M, and Mantovani, F. Virtual reality applications in medicine during the COVID-19 pandemic: systematic review. JMIR Serious Games. (2022) 10:e35000. doi: 10.2196/35000
28. Sadhasivam, S, Arora, RK, Rekapalli, R, Chaturvedi, J, Goyal, N, Bhargava, P, et al. A systematic review on the impact of the COVID-19 pandemic on neurosurgical practice and Indian perspective. Asian J Neurosurg. (2021) 16:24–32. doi: 10.4103/ajns.AJNS_379_20
29. Garcia, LS . E-learning and impact on the teaching and evaluation of human anatomy during COVID-19: a review of the quality of the literature. Int J Morphol. (2022) 40:902–8. doi: 10.4067/S0717-95022022000400902
30. Vathenen, R, Khan, J, Edwards, A, Gelding, SV, Khanji, MY, and Gunganah, K. Challenges and opportunities to diabetes and endocrinology training during and beyond the COVID-19 pandemic. Pract Diabetes. (2022) 39:31–4. doi: 10.1002/pdi.2397
31. Ali, DM, Hisam, B, Shaukat, N, Baig, N, Ong, MEH, Epstein, JL, et al. Cardiopulmonary resuscitation (CPR) training strategies in the times of COVID-19: a systematic literature review comparing different training methodologies. Scand J Trauma Resusc Emerg Med. (2021) 29:53. doi: 10.1186/s13049-021-00869-3
32. Dedeilia, A, Sotiropoulos, MG, Hanrahan, JG, Janga, D, Dedeilias, P, and Sideris, M. Medical and surgical education challenges and innovations in the COVID-19 era: a systematic review. In Vivo. (2020) 34:1603–11. doi: 10.21873/invivo.11950
33. Wilcha, RJ . Effectiveness of virtual medical teaching during the COVID-19 crisis: systematic review. JMIR Med Educ. (2020) 6:20963. doi: 10.2196/20963
34. Ahmady, S, Kallestrup, P, Sadoughi, M, Katibeh, M, Kalantarion, M, Amini, M, et al. Distance learning strategies in medical education during COVID-19: a systematic review. J Edu Health Promotion. (2021) 10:421. doi: 10.4103/jehp.jehp_318_21
35. Chen, SY, Lo, HY, and Hung, SK. What is the impact of the COVID-19 pandemic on residency training: a systematic review and analysis. BMC Med Educ. (2021) 21:618. doi: 10.1186/s12909-021-03041-8
36. Hope, C, Reilly, JJ, Griffiths, G, Lund, J, and Humes, D. The impact of COVID-19 on surgical training: a systematic review. Tech Coloproctol. (2021) 25:505–20. doi: 10.1007/s10151-020-02404-5
37. Islam, MA, and Alam, MS. Impact of sars-cov-2 infection on veterinary medical education. J Univ Teach Learn Pract. (2021) 18:257–80. doi: 10.53761/1.18.5.14
38. Lee, IR, Kim, HW, Lee, Y, Koyanagi, A, Jacob, L, An, S, et al. Changes in undergraduate medical education due to COVID-19: a systematic review. Eur Rev Med Pharmacol Sci. (2021) 25:4426–34. doi: 10.26355/eurrev_202106_26155
39. Naciri, A, Radid, M, Kharbach, A, and Chemsi, G. E-learning in health professions education during the COVID-19 pandemic: a systematic review. J Edu Eval Health Prof. (2021) 18:18. doi: 10.3352/jeehp.2021.18.27
40. Najminouri, F . The effect of the coronavirus disease-2019 challenge on oral and dental health education: a systematic review. J Oral Health Oral Epidemiol. (2021) 10:4–10. doi: 10.22122/johoe.2021.196017.1317
41. Nakhoda, K, Ahmady, S, Fesharaki, MG, and Azar, NG. COVID-19 pandemic and E-learning satisfaction in medical and non-medical student: a systematic review and meta-analysis. Iran J Public Health. (2021) 50:2509–16. doi: 10.18502/ijph.v50i12.7933
42. Negahi, A, Nafissi, N, Eghbali, F, Nouri, B, Nassiri, S, and Nasiri, M. A literature review about impact of COVID-19 on operative activity, educational process and mental health of surgical residents. Clin Schizophr Relat Psychoses. (2021) 15
43. Santos, GNM, da Silva, HEC, Leite, AF, Mesquita, CRM, Figueiredo, PTS, Stefani, CM, et al. The scope of dental education during COVID-19 pandemic: a systematic review. J Dent Educ. (2021) 85:1287–300. doi: 10.1002/jdd.12587
44. Abdull Mutalib, AA, Akim, A, and Jaafar, MH. A systematic review of health sciences students’ online learning during the COVID-19 pandemic. BMC Med Educ. (2022) 22:524. doi: 10.1186/s12909-022-03579-1
45. Cartledge, S, Ward, D, Stack, R, and Terry, E. Adaptations in clinical examinations of medical students in response to the COVID-19 pandemic: a systematic review. BMC Med Educ. (2022) 22:607. doi: 10.1186/s12909-022-03662-7
46. Grafton-Clarke, C, Uraiby, H, Gordon, M, Clarke, N, Rees, E, Park, S, et al. Pivot to online learning for adapting or continuing workplace-based clinical learning in medical education following the COVID-19 pandemic: A BEME systematic review: BEME guide no. 70. Med Tech. (2022) 44:227–43. doi: 10.1080/0142159X.2021.1992372
47. Hao, X, Peng, X, Ding, X, Qin, Y, Lv, M, Li, J, et al. Application of digital education in undergraduate nursing and medical interns during the COVID-19 pandemic: a systematic review. Nurse Educ Today. (2022) 108:105183. doi: 10.1016/j.nedt.2021.105183
48. Hsu, CH, Huang, HT, Chen, CH, Fu, YC, Chou, PH, and Hsu, NC. Review global impact of the COVID-19 pandemic on orthopedics and the implications of telemedicine: a systematic review of the literature. J Clin Med. (2022) 11:12983. doi: 10.3390/jcm11112983
49. Jain, R, Carneiro, RAVD, Vasilica, AM, Chia, WL, de Souza, ALB, Wellington, J, et al. The impact of the COVID-19 pandemic on global neurosurgical education: a systematic review. Neurosurg Rev. (2022) 45:1101–10. doi: 10.1007/s10143-021-01664-5
50. Lawal, O, Omiyi, D, York, H, and Akudjedu, TN. Towards describing the global impact of the COVID-19 pandemic on clinical radiography education: a systematic review. J Med Imaging Radiat Sci. (2022) 53:487–97. doi: 10.1016/j.jmir.2022.05.009
51. Loh, CH, Ong, FLL, and Oh, CC. Teledermatology for medical education in the COVID-19 pandemic context: a systematic review. JAAD Int. (2022) 6:114–8. doi: 10.1016/j.jdin.2021.12.012
52. Papa, V, Varotto, E, Galli, M, Vaccarezza, M, and Galassi, FM. One year of anatomy teaching and learning in the outbreak: has the Covid-19 pandemic marked the end of a century-old practice? A systematic review. Anat Sci Educ. (2022) 15:261–80. doi: 10.1002/ase.2162
53. Pires, C . Perceptions of pharmacy students on the E-learning strategies adopted during the COVID-19 pandemic: a systematic review. Pharmacy. (2022) 10:20. doi: 10.3390/pharmacy10010031
54. Saed, A . A systematic review of the medical student feedback on undergraduate surgical education during the pandemic. Cureus. (2022) 14:e30440. doi: 10.7759/cureus.30440
55. Shorey, S, Pereira, TLB, Teo, WZ, Ang, E, Lau, TC, and Samarasekera, DD. Navigating nursing curriculum change during COVID-19 pandemic: a systematic review and meta-synthesis. Nurse Educ Pract. (2022) 65:103483. doi: 10.1016/j.nepr.2022.103483
56. Stojan, J, Haas, M, Thammasitboon, S, Lander, L, Evans, S, Pawlik, C, et al. Online learning developments in undergraduate medical education in response to the COVID-19 pandemic: A BEME systematic review: BEME guide no. 69. Med Tech. (2022) 44:109–29. doi: 10.1080/0142159X.2021.1992373
57. Tabatabaeichehr, M, Babaei, S, Dartomi, M, Alesheikh, P, Tabatabaee, A, Mortazavi, H, et al. Medical students’ satisfaction level with e-learning during the COVID-19 pandemic and its related factors: a systematic review. J Educ Eval Health Prof. (2022) 19:37. doi: 10.3352/jeehp.2022.19.37
58. Tan, CJW, Cai, C, Ithnin, F, and Lew, E. Challenges and innovations in undergraduate medical education during the COVID-19 pandemic—a systematic review. Asia Pacific Scholar. (2022) 7:1–9. doi: 10.29060/TAPS.2022-7-3/OA2722
59. Shakeel, F, Saghir, I, Toufique, G, Khalid, N, and Kalas, ZA. Effect of COVID 19 lockdown on medical education: a systematic review. J Pak Med Assoc. (2023) 73:853–7. doi: 10.47391/JPMA.6635
60. Wanigasooriya, K, Beedham, W, Laloo, R, Karri, RS, Darr, A, Layton, GR, et al. The perceived impact of the Covid-19 pandemic on medical student education and training—an international survey. BMC Med Educ. (2021) 21:566. doi: 10.1186/s12909-021-02983-3
61. Ahmed, H, Allaf, M, and Elghazaly, H. COVID-19 and medical education. Lancet Infect Dis. (2020) 20:777–8. doi: 10.1016/S1473-3099(20)30226-7
62. Sahi, PK, Mishra, D, and Singh, T. Medical education amid the COVID-19 pandemic. Indian Pediatr. (2020) 57:652–7. doi: 10.1007/s13312-020-1894-7
63. Jia, Q, Qu, Y, Sun, H, Huo, H, Yin, H, and You, D. Mental health among medical students during COVID-19: a systematic review and meta-analysis. Front Psychol. (2022) 13. doi: 10.3389/fpsyg.2022.846789
64. Paz, DC, Bains, MS, Zueger, ML, Bandi, VR, Kuo, VY, Cook, K, et al. COVID-19 and mental health: A systematic review of international medical student surveys. Front Psychol. (2022) 13:1028559. doi: 10.3389/fpsyg.2022.1028559
65. Chandratre, S, Knight, C, and Dodson, L. Supporting medical student mental health during COVID-19: strategies implemented for an accelerated curriculum medical campus. J Med Educat Curri Develop. (2021) 8:238212052110063. doi: 10.1177/23821205211006392
66. Arponen, H, Zou-Kopsa, Q, and Karaharju-Suvanto, T. Examination performance of dentistry students during the COVID-19 pandemic. Acta Odontol Scand. (2023) 81:124–30. doi: 10.1080/00016357.2022.2096922
67. Farrokhi, F, Mohebbi, SZ, Farrokhi, F, and Khami, MR. Impact of COVID-19 on dental education- a scoping review. BMC Med Educ. (2021) 21:587. doi: 10.1186/s12909-021-03017-8
68. Clemente, MP, Moreira, A, Pinto, JC, Amarante, JM, and Mendes, J. The challenge of dental education after COVID-19 pandemic—present and future innovation study design. INQUIRY J Health Care Organiz Prov Finan. (2021) 58:469580211018293. doi: 10.1177/00469580211018293
69. Karattuthodi, MS, Thorakkattil, SA, Chandrasekhar, D, Punnoth Poonkuzhi, N, Mohammed Ahmed Ageeli, M, et al. Pharmacy Student’s challenges in virtual learning system during the second COVID 19 wave in southern India. Soc. Sci. Humanities Open. (2022) 5:100241. doi: 10.1016/j.ssaho.2021.100241
70. Gharib, AM, Peterson, GM, Bindoff, IK, and Salahudeen, MS. Potential barriers to the implementation of computer-based simulation in pharmacy education: a systematic review. Pharmacy. (2023) 11:30086. doi: 10.3390/pharmacy11030086
71. Gaur, U, Majumder, MAA, Sa, B, Sarkar, S, Williams, A, and Singh, K. Challenges and opportunities of preclinical medical education: COVID-19 crisis and beyond. SN Compr Clin Med. (2020) 2:1992–7. doi: 10.1007/s42399-020-00528-1
72. Turnbull, D, Chugh, R, and Luck, J. Transitioning to E-learning during the COVID-19 pandemic: how have higher education institutions responded to the challenge? Educ Inf Technol. (2021) 26:6401–19. doi: 10.1007/s10639-021-10633-w
73. Rezaei Tolzali, MM, Noori, M, Shokri, P, Rahmani, S, Khanzadeh, S, Nejadghaderi, SA, et al. Efficacy of tocilizumab in the treatment of COVID-19: an umbrella review. Rev Med Virol. (2022) 32:e2388. doi: 10.1002/rmv.2388
74. Muka, T, Li, JJX, Farahani, SJ, and Ioannidis, JPA. An umbrella review of systematic reviews on the impact of the COVID-19 pandemic on cancer prevention and management, and patient needs. eLife. (2023) 12:e85679. doi: 10.7554/eLife.85679
Keywords: medical education, virtual education, COVID-19, dentistry, nursing, pharmacy, veterinary medicine, umbrella review
Citation: Nejadghaderi SA, Khoshgoftar Z, Fazlollahi A and Nasiri MJ (2024) Medical education during the coronavirus disease 2019 pandemic: an umbrella review. Front. Med. 11:1358084. doi: 10.3389/fmed.2024.1358084
Edited by:
Vincent Salvatore Gallicchio, Clemson University, United StatesReviewed by:
Ivan Šoša, University of Rijeka, CroatiaTelmo Raul Aveiro Róbalo, Pacific University, Paraguay
Copyright © 2024 Nejadghaderi, Khoshgoftar, Fazlollahi and Nasiri. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zohreh Khoshgoftar, Qmtob3NoZ29mdGFyN0BnbWFpbC5jb20=; Ymtob3NoZ29mdGFyN0BzYm11LmFjLmly; Mohammad Javad Nasiri, bWoubmFzaXJpQGhvdG1haWwuY29t
 Seyed Aria Nejadghaderi
Seyed Aria Nejadghaderi Zohreh Khoshgoftar
Zohreh Khoshgoftar Asra Fazlollahi
Asra Fazlollahi Mohammad Javad Nasiri
Mohammad Javad Nasiri