- 1Faculty of Medicine and Health Technology, Tampere University, Tampere, Finland
- 2Tays Eye Centre, Tampere University Hospital, Tampere, Finland
Ocular sarcoidosis most commonly presents with symptoms and is first diagnosed before systemic sarcoidosis in at least half of the patients with sarcoidosis. Prevalence of ocular involvement in sarcoidosis varies between 2–80% depending on the study setting, included ocular diseases, and studied population. In many studies, ocular involvement in sarcoidosis has been overestimated mainly because study populations have been collected from eye clinics and because the study criteria have included ocular findings or symptoms that do not require treatment or monitoring. In a screening setting, asymptomatic ocular sarcoidosis has been detected in only 2–5%. 0–1% of the screened sarcoidosis patients have required treatment. For these reasons, ocular screening in sarcoidosis seems generally of little value. Patients with sarcoidosis who present with ocular symptoms should be screened for ocular sarcoidosis in a timely manner because they are at high risk of ocular disease.
Although asymptomatic ocular sarcoidosis is rare, screening has been recommended for patients with sarcoidosis to rule out ocular inflammation. In 2020, the American Thoracic Society (ATS) recommended baseline eye exams in sarcoidosis because ocular inflammation may be common in sarcoidosis, screening is not harmful nor burdensome, and treatment can be beneficial in maintaining vision (1). The ATS screening recommendation increased screening referrals to Tays Eye Centre, Tampere University Hospital, Tampere, Finland in 2020–2021, even though the pandemic was ongoing, and the clinical experience was that asymptomatic ocular sarcoidosis is rarely seen (1, 2). Therefore, a registry study and a literature review were conducted to better understand the value of ocular screening in sarcoidosis (2).
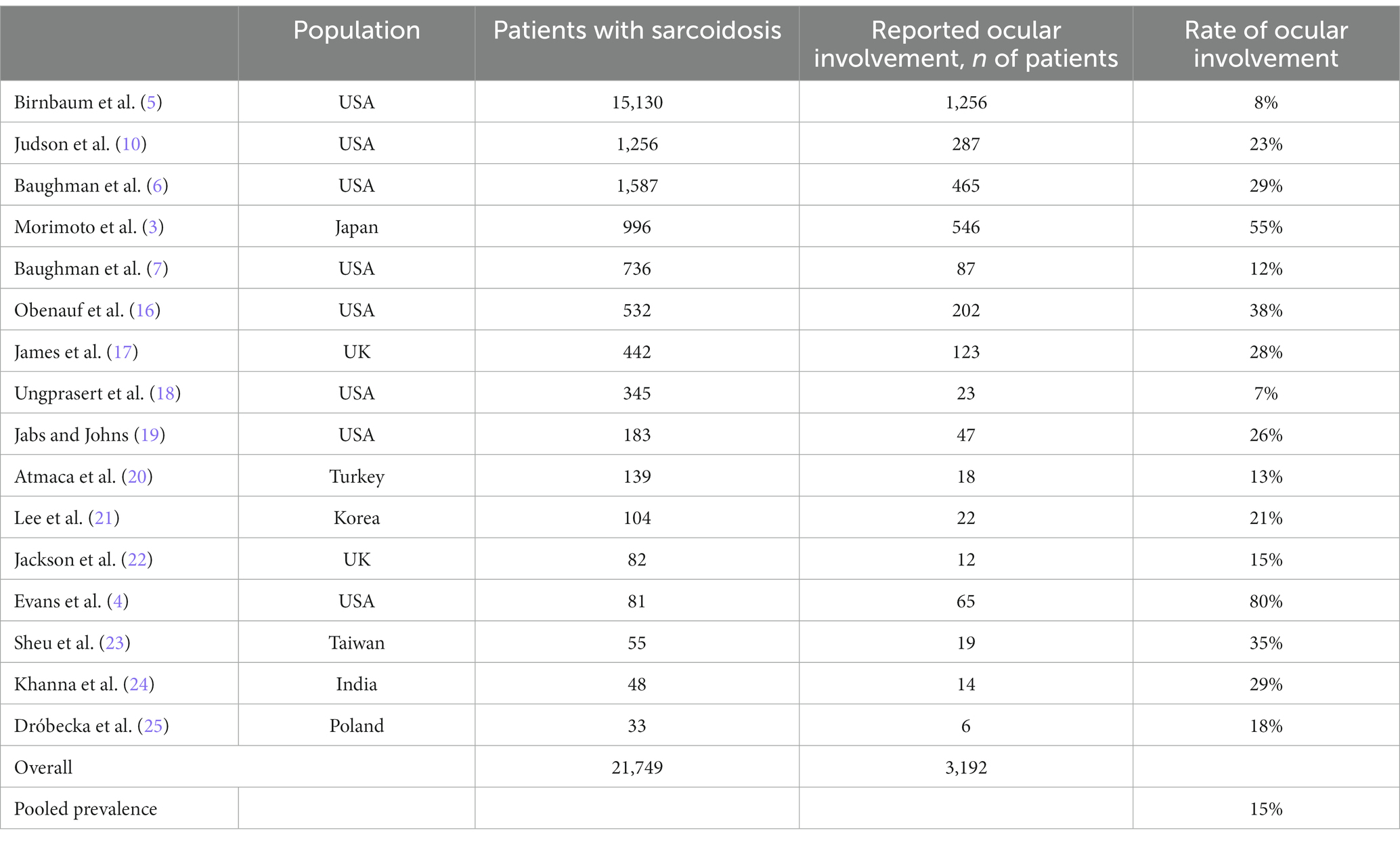
The rate of ocular involvement in sarcoidosis varies widely, between 2–80% in different studies (2–7). Length of follow-up affects the cumulative rate of ocular inflammation in sarcoidosis and provides one explanation for differences in study results. One study has evaluated the incidence of ocular inflammation in sarcoidosis in an American veteran population, where the incidence of ocular inflammation over a 3-year period was 8% (5). Most commonly, ocular inflammation is diagnosed during the first year after the diagnosis of systemic sarcoidosis (8, 9). The rate of ocular sarcoidosis also depends on the population. The risk of ocular sarcoidosis is especially high in Japan, where for example uveitis occurs in up to 41% of patients with sarcoidosis (3). African-Americans may also have a high risk of developing ocular sarcoidosis but not all results are consistent regarding their risk (4, 7, 10).
Ocular sarcoidosis has been screened in three studies, in which asymptomatic intraocular inflammation was found in 2–5% of patients (2, 11, 12). In the study by Sunshine et al., asymptomatic intraocular inflammation was detected in 2 of 42 patients with histopathologically confirmed sarcoidosis, and neither required treatment (11). In the screening study from Tays Eye Centre, 262 patient records were reviewed: 172 asymptomatic patients were specifically screened for ocular sarcoidosis and 90 patients without any inflammatory symptoms underwent an untargeted comprehensive ocular exam. Two patients (0.8%) had asymptomatic intraocular inflammation that was high enough to require treatment (2). In a screening study by Lee et al., none of the 27 asymptomatic patients required treatment. In their study, 45% of screened patients had ocular symptoms. Two of the 22 patients with symptoms had active intraocular inflammation necessitating treatment (13). Pooling these numbers together, 2 of 331 asymptomatic patients were treated for ocular sarcoidosis. To find one asymptomatic inflammation that required treatment, as many as 165 patients were screened.
Registry studies may underestimate a prevalence because occult diseases are not revealed without screening asymptomatic patients (5). Screening studies estimate disease prevalence better than registry studies, but they also catch clinically insignificant conditions (14). For example, in the screening study by Lee et al., 12% had signs of intraocular inflammation, and more than half of the patients presented with some finding related to ocular sarcoidosis but only 2 were treated (13).
Studies that investigate data from eye centers may overestimate the rate of ocular involvement in sarcoidosis because only some of the patients with sarcoidosis, particularly patients with symptoms, will visit the eye clinic. An example of an overestimate can be created from our registry data. In the population served by Tampere University Hospital, there should have been approximately 480 new sarcoidosis cases during 2014–2021 (15). During 2014–2021, altogether 568 people who had a recorded ICD-10 code for sarcoidosis were treated at Tays Eye Centre. We found confirmation of the diagnosis of sarcoidosis in the electronic charts for 400 patients. During 2014–2021, 97 patients were treated for ocular sarcoidosis (2). Thus, the rate of ocular sarcoidosis was 24% for patients with chart-confirmed sarcoidosis and visiting the Tays Eye Centre, and lower, when unconfirmed cases or the cumulative incidence of sarcoidosis are considered.
Ocular conditions included in the study criteria significantly impact the rate of reported ocular sarcoidosis (Table 1). Study results may be misleading if they report both harmful and harmless conditions in their overall rates. Inclusion of common but less harmful conditions, such as conjunctival nodules detected in up to 59% of patients with sarcoidosis, or cataract in up to 38%, increase the rate of ocular involvement in sarcoidosis (13, 26). For example, in the study by Morimoto et al., one of the recorded ocular findings was visual disturbance which occurred in 20% of patients with sarcoidosis, which potentially affected the overall rate of ocular involvement (55%) in their data (3). Similarly, if we included visual disturbances in our results at Tays Eye Centre, the rate of eye involvement would be 28% instead of 2% although none of the patients experiencing vision problems were diagnosed with ocular sarcoidosis. If we included dry eyes in our study criteria, the rate of ocular sarcoidosis would be 13% in our screening study although none of the patients with dry eye symptoms required follow-up (2).
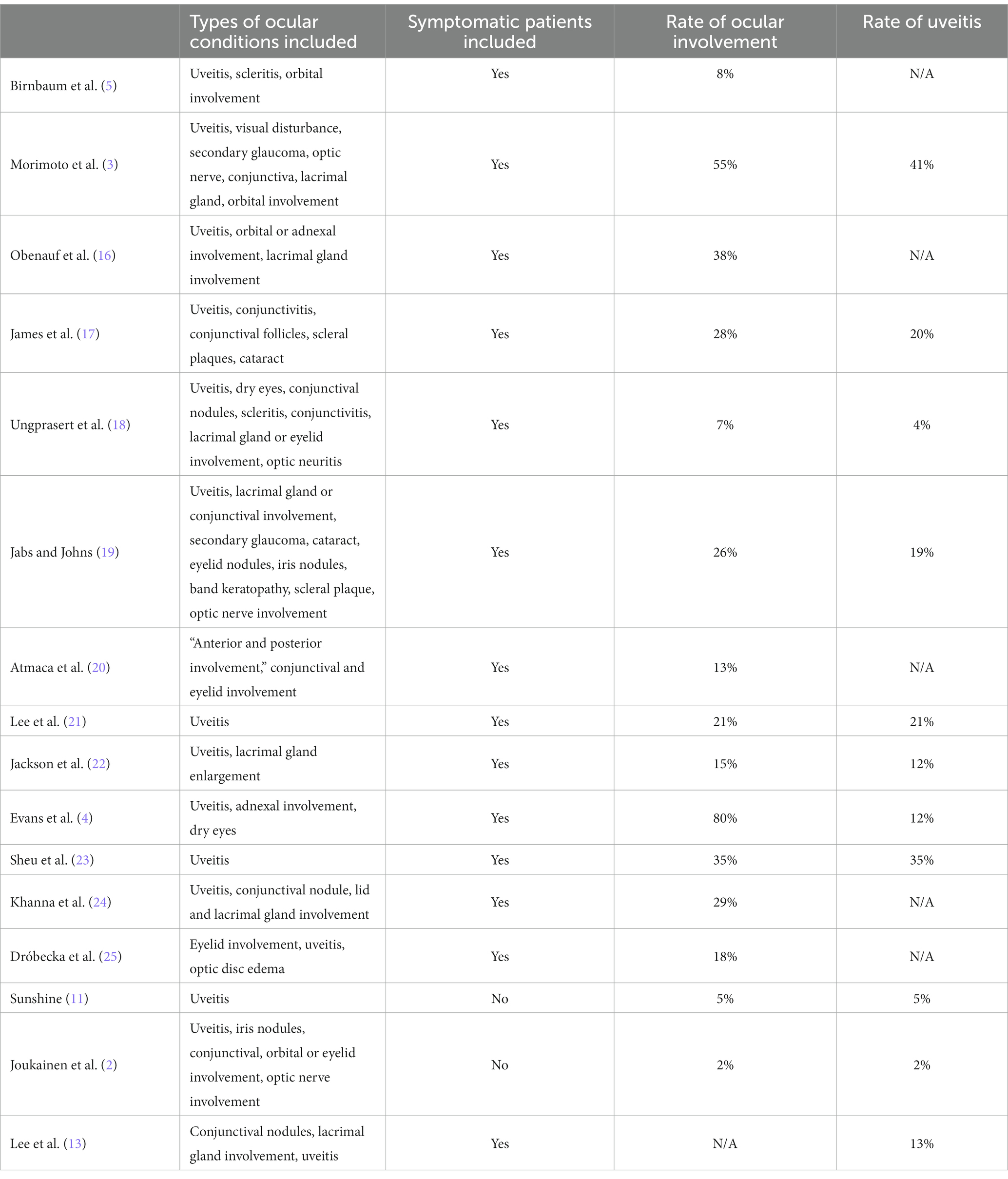
Table 1. Included ocular conditions, rate of ocular involvement, and rate of uveitis in different studies.
Also, the rate of complications in ocular sarcoidosis varies mainly depending on the included ocular conditions. Only one patient (0.3%) in our screening study had developed a uveitis-related complication by the time of screening visit, without any impact in their vision (2). In long-term follow-up, with long-term high-dose steroid treatment, and including both symptomatic and asymptomatic eyes, ocular complications are observed often, especially in uveitis. Cataracts are seen in 62%, secondary glaucoma in 28%, and macular edema in up to 23% in intraocular inflammation related to sarcoidosis (27–29). Chronic or severe sarcoidosis-related ocular inflammation may cause vision loss (28, 29), but not all sarcoidosis-related ocular findings lead to impaired vision, such as conjunctival nodules (13). During the past decades, visual prognosis has improved in ocular sarcoidosis likely due to improved surgical techniques especially in the field of cataract surgery, better inflammatory management, and with advances in antirheumatic treatment (19, 27–29). In 2022, Suzuki et al. reported that only 6% of eyes with ocular sarcoidosis (22 of 323) had irreversible vision loss, mostly due to secondary glaucoma (27). In 1999, the rate of vision loss was much higher, 46%, and 5% of patients lost vision below 20/120 in both eyes (28). Earlier, in 1986, as many as 26% of patients with ocular sarcoidosis lost vision below 20/120 (19). No study has compared treatment outcomes in patients with and without ocular symptoms at diagnosis.
To sum up, rate of ocular involvement in sarcoidosis varies between 2–80% depending mainly on the included ocular conditions, study setting, and population. Low rates occur in a screening setting and high rates occur when including symptomatic patients, primary ocular sarcoidosis, non-inflammatory ocular conditions, and in high-risk populations (2–7, 17, 18). A good way to make a general estimate of the overall prevalence is to calculate a pooled prevalence if the reported results vary. The pooled prevalence estimated from the studies included in the ATS review is 15%, which is much lower than the average prevalence (26%) calculated by the ATS (1) (Table 2). Thus, there was a methodological error in the ATS review (1). In the current analysis, the pooled prevalence of ocular sarcoidosis is 14% among the larger studies (n > 500) included in the ATS review (3, 5–7, 10, 30). Among the small studies (n < 200), the pooled prevalence is as high as 40% (4, 16, 19, 20, 22, 24, 25), explaining the difference between the reported average rate in the ATS review (26%) and the calculated pooled prevalence (15%) in this review (1). One study published in 1974 was excluded from the current analysis because the original paper was not available (23). It is good to note that some of the included studies in the ATS review overestimated the rate of ocular sarcoidosis, as explained in this article and previously by Lee et al. (13).
Studies including patients with primary ocular sarcoidosis should not guide recommendations for ocular screening in sarcoidosis. Ocular sarcoidosis is diagnosed before systemic sarcoidosis in up to 80% of patients (8, 18, 28). Systemic sarcoidosis is routinely screened in bilateral granulomatous, anterior uveitis, which may present with iris nodules and anterior synechiae; in intermediate or panuveitis with snowballs or strings of pearls; and in uveitis with periphlebitis, multifocal chorioretinitis, or posterior granuloma(s) (31). Systemic sarcoidosis is considered also in inflammatory orbital conditions, or when granulomas are detected on the conjunctiva or eyelids (9). If sarcoidosis is suspected, the patient is asked about their extraocular symptoms (32). Screening panel for asymptomatic systemic sarcoidosis includes at least chest imaging, serum ACE and/or LZM measurement, serum lymphocyte count, and tuberculin test or interferon-gamma releasing assay to rule out tuberculosis (31).
Majority of patients with ocular sarcoidosis present with symptoms (1, 5, 26), further reducing the value of ocular screening in sarcoidosis. Ocular sarcoidosis may present with a wide variety of symptoms including pain, photophobia, lacrimation, redness, blurriness of vision, floaters, eyelid swelling, or even diplopia (9, 13). Studies including patients with ocular symptoms should not guide the future recommendations for screening. The US screening studies did not find any evidence to support screening of asymptomatic sarcoidosis patients (11, 13). After completing our screening study, we stopped screening asymptomatic sarcoidosis patients at Tampere University Hospital, Finland (2). We should conduct similar screening studies in different patient populations and report in detail which findings were related to inflammation, which findings required follow-up and treatment, and which findings caused ocular symptoms. Further screening studies should be performed in potentially high-risk populations such as Japan (3), Korea (21), and among African-Americans (4, 7).
The benefits of screening asymptomatic ocular sarcoidosis seem very uncertain because majority of the patients present with ocular symptoms (1, 5, 26), patients are commonly first diagnosed with ocular sarcoidosis (8, 18, 28), and because asymptomatic ocular sarcoidosis requiring treatment is rare (2, 11, 13). All patients with sarcoidosis who present with ocular symptoms should be screened for ocular sarcoidosis in a timely manner because they are at high risk of ocular disease.
Author contributions
SL: Conceptualization, Methodology, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Crouser, ED , Maier, LA , Wilson, KC , Bonham, CA , Morgenthau, AS , Patterson, KC, et al. Diagnosis and detection of sarcoidosis. An official American Thoracic Society clinical practice guideline. Am J Respir Crit Care Med. (2020) 201:e26–51. doi: 10.1164/rccm.202002-0251ST
2. Joukainen, E , Antonen, J , and Leinonen, S . Low utility of ocular screening in sarcoidosis in Finland. Acta Ophthalmol. (2023):15749. doi: 10.1111/aos.15749
3. Morimoto, T , Azuma, A , Abe, S , Usuki, J , Kudoh, S , Sugisaki, K, et al. Epidemiology of sarcoidosis in Japan. Eur Respir J. (2008) 31:372–9. doi: 10.1183/09031936.00075307
4. Evans, M , Sharma, O , LaBree, L , Smith, RE , and Rao, NA . Differences in clinical findings between caucasians and African Americans with biopsy-proven sarcoidosis. Ophthalmology. (2007) 114:325–333.e1. doi: 10.1016/j.ophtha.2006.05.074
5. Birnbaum, AD , French, DD , Mirsaeidi, M , and Wehrli, S . Sarcoidosis in the National Veteran Population. Ophthalmology. (2015) 122:934–8. doi: 10.1016/j.ophtha.2015.01.003
6. Baughman, RP , Lower, EE , Ingledue, R , and Kaufman, AH . Management of ocular sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis. (2012) 29:26–33.
7. Baughman, RP , Teirstein, AS , Judson, MA , Rossman, MD , Yeager, H Jr, Bresnitz, EA, et al. Clinical characteristics of patients in a case control study of sarcoidosis. Am J Respir Crit Care Med. (2001) 164:1885–9. doi: 10.1164/ajrccm.164.10.2104046
8. Ma, SP , Rogers, SL , Hall, AJ , Hodgson, L , Brennan, J , Stawell, RJ, et al. Sarcoidosis-related uveitis: clinical presentation, disease course, and rates of systemic disease progression after uveitis diagnosis. Am J Ophthalmol. (2019) 198:30–6. doi: 10.1016/j.ajo.2018.09.013
9. Rothova, A . Ocular involvement in sarcoidosis. Br J Ophthalmol. (2000) 84:110–6. doi: 10.1136/bjo.84.1.110
10. Judson, MA , Boan, AD , and Lackland, DT . The clinical course of sarcoidosis: presentation, diagnosis, and treatment in a large white and black cohort in the United States. Sarcoidosis Vasc Diffuse Lung Dis. (2012) 29:119–27.
11. Sunshine, S , Pyatetsky, D , Birnbaum, AD , and Goldstein, DA . Should patients with sarcoidosis be screened for asymptomatic ocular inflammation? Invest Ophthalmol Vis Sci. (2017) 58:2172.
12. Lee, J, et al. The role of screening for asymptomatic ocular inflammation in sarcoidosis. Ocul. Immunol. Inflamm. (2022).
13. Lee, J , Zaguia, F , Minkus, C , Koreishi, AF , Birnbaum, AD , and Goldstein, DA . The role of screening for asymptomatic ocular inflammation in sarcoidosis. Ocul Immunol Inflamm. (2022) 30:1936–9. doi: 10.1080/09273948.2021.1976216
14. Raffle, AE , Mackie, A , and Gray, JAM . Screening: Evidence and practice. 2nd ed. Oxford: Oxford University Press (2019).
15. Pietinalho, A , Hiraga, Y , Hosoda, Y , Löfroos, AB , Yamaguchi, M , and Selroos, O . The frequency of sarcoidosis in Finland and Hokkaido, Japan. A comparative epidemiological study. Sarcoidosis. (1995) 12:61–7.
16. Dróbecka, E , Swituła, M , Godowska, J , Skórska, I , Płodziszewska, M , and Szopiński, J . Ocular manifestations in sarcoidosis. Klin Ocz. (1999) 101:201–4.
17. James, DG , Anderson, R , Langley, D , and Ainslie, D . OCULAR SARCOIDOSIS. Br J Ophthalmol. (1964) 48:461–70. doi: 10.1136/bjo.48.9.461
18. Ungprasert, P , Tooley, AA , Crowson, CS , Matteson, EL , and Smith, WM . Clinical characteristics of ocular sarcoidosis: a population-based study 1976–2013. Ocul Immunol Inflamm. (2019) 27:389–95. doi: 10.1080/09273948.2017.1386791
19. Jabs, DA , and Johns, CJ . Ocular involvement in chronic sarcoidosis. Am J Ophthalmol. (1986) 102:297–301. doi: 10.1016/0002-9394(86)90001-2
21. Lee, SY , Lee, HG , Kim, DS , Kim, JG , Chung, H , and Yoon, YH . Ocular sarcoidosis in a Korean population. J Korean Med Sci. (2009) 24:413–9. doi: 10.3346/jkms.2009.24.3.413
22. Khanna, A , Sidhu, U , Bajwa, G , and Malhotra, V . Pattern of ocular manifestations in patients with sarcoidosis in developing countries. Acta Ophthalmol Scand. (2007) 85:609–12. doi: 10.1111/j.1600-0420.2006.00791.x
23. Siltzbach, LE , James, DG , Neville, E , Turiaf, J , Battesti, JP , Sharma, OP, et al. Course and prognosis of sarcoidosis around the world. Am J Med. (1974) 57:847–52. doi: 10.1016/0002-9343(74)90160-0
24. Sheu, SJ , Chang, FP , Wu, TT , and Chuang, CT . Ocular sarcoidosis in southern Taiwan. Ocul Immunol Inflamm. (2010) 18:152–7. doi: 10.3109/09273941003637502
25. Atmaca, LS , Atmaca-Sönmez, P , İdil, A , Kumbasar, ÖÖ , and Çelik, G . Ocular involvement in sarcoidosis. Ocul Immunol Inflamm. (2009) 17:91–4. doi: 10.1080/09273940802596526
26. Pefkianaki, M , Androudi, S , Praidou, A , Sourlas, V , Zakynthinos, E , Brazitikos, P, et al. Ocular disease awareness and pattern of ocular manifestation in patients with biopsy-proven lung sarcoidosis. J Ophthalmic Inflamm Infect. (2011) 1:141–5. doi: 10.1007/s12348-011-0029-7
27. Suzuki, K , Ishihara, M , Namba, K , Ohno, S , Goto, H , Takase, H, et al. Clinical features of ocular sarcoidosis: severe, refractory, and prolonged inflammation. Jpn J Ophthalmol. (2022) 66:447–54. doi: 10.1007/s10384-022-00927-y
28. Edelsten, C , Pearson, A , Joynes, E , Stanford, MR , and Graham, EM . The ocular and systemic prognosis of patients presenting with sarcoid uveitis. Eye. (1999) 13:748–53. doi: 10.1038/eye.1999.221
29. Bodaghi, B , Touitou, V , Fardeau, C , Chapelon, C , and LeHoang, P . Ocular sarcoidosis. Presse Med. (2012) 41:e349–54. doi: 10.1016/j.lpm.2012.04.004
30. Obenauf, CD , Shaw, HE , Sydnor, CF , and Klintworth, GK . Sarcoidosis and its ophthalmic manifestations. Am J Ophthalmol. (1978) 86:648–55. doi: 10.1016/0002-9394(78)90184-8
31. Mochizuki, M , Smith, JR , Takase, H , Kaburaki, T , Acharya, NR , and Rao, NA . Revised criteria of international workshop on ocular sarcoidosis (IWOS) for the diagnosis of ocular sarcoidosis. Br J Ophthalmol. (2019) 103:1418–22. doi: 10.1136/bjophthalmol-2018-313356
Keywords: sarcoidosis, ocular sarcoidosis, uveitis, sarcoidosis-related uveitis, screening
Citation: Leinonen S (2024) Ocular sarcoidosis, to screen or not to screen? Front. Med. 11:1348435. doi: 10.3389/fmed.2024.1348435
Edited by:
Georgios D. Panos, Nottingham University Hospitals NHS Trust, United KingdomReviewed by:
Ogugua Ndili Obi, East Carolina University, United StatesIlias C. Papanikolaou, General Hospital of Corfu, Greece
Copyright © 2024 Leinonen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sanna Leinonen, c2FubmEubGVpbm9uZW5AdHVuaS5maQ==
 Sanna Leinonen
Sanna Leinonen