- 1School of Nursing, Jilin University, Changchun, China
- 2The First Hospital of Jilin University, Changchun, China
- 3Department of Pathogenobiology, The Key Laboratory of Zoonosis, Chinese, Ministry of Education, College of Basic Medicine, Jilin University, Changchun, China
- 4The Key Laboratory for Bionics Engineering, Ministry of Education, Jilin University, Changchun, China
- 5Engineering Research Center for Medical Biomaterials of Jilin Province, Jilin University, Changchun, China
- 6Key Laboratory for Health Biomedical Materials of Jilin Province, Jilin University, Changchun, China
- 7State Key Laboratory of Pathogenesis, Prevention and Treatment of High Incidence Diseases in Central Asia, Urumqi, Xinjiang, China
Background: Heart failure (HF) brings not only physical pain but also psychological distress. This systematic review investigated the influence of spiritual care on the psychological well-being and quality of life in adults with HF.
Methods: We conducted a systematic literature review following PRISMA guidelines, searching seven electronic databases for relevant randomized controlled studies without language or temporal restrictions. The studies were assessed for quality using the Cochrane Bias Risk tool.
Results: A total of 13 studies (882 participants) were reviewed, investigating interventions such as religion, meditation, mental health, cognitive interventions, and spiritual support. Key factors influencing the effectiveness of spiritual care implementation included integration into routine care, respect for diversity, patient engagement, intervention quality, and alignment with patient beliefs. The majority of the studies indicated that spiritual care has a potentially beneficial impact on the mental health and quality of life of patients with HF.
Conclusion: The findings provide valuable insights for healthcare professionals, highlighting the importance of adopting a spiritual care approach to healthcare for this population.
Introduction
HF is a prevalent and debilitating chronic disease (1), affecting millions of individuals globally (2). It is a complex syndrome characterized by the heart’s inability to pump sufficient blood to meet the body’s metabolic demands (3, 4), resulting in symptoms such as fatigue, dyspnea, and fluid retention (5). As HF progresses, individuals may experience physical limitations, reduced exercise tolerance, and recurrent hospitalizations, significantly impacting their overall functional capacity and independence (6, 7). The psychological burden is significant, with patients experiencing anxiety, depression, fear of worsening symptoms, and uncertainty about the future (8, 9). Managing HF involves multifaceted medical treatments, lifestyle modifications, and psychosocial support from professionals and family (10). Despite medical advancements, HF still carries high morbidity, diminished quality of life, and increased mortality rates (11, 12). The physical and psychological challenges of HF require comprehensive, patient-centered care (13). As the global population ages, the prevalence of HF is expected to increase significantly (14), highlighting the importance of exploring innovative interventions to improve adults with this condition (15). In recent years, healthcare professionals and researchers have increasingly recognized the importance of addressing psychological and spiritual aspects of health in addition to traditional medical approaches (16). Spiritual care, defined as providing support in individuals’ search for meaning, purpose, and connection with something greater than themselves (17, 18), has emerged as a potential complement to conventional medical management for chronic diseases, including HF (19).
Spiritual care recognizes the importance of psychological, emotional, and spiritual factors in holistic well-being and coping (20). Beyond religious aspects, it includes practices like prayer, meditation, mindfulness, counseling, and social support (21). In healthcare settings, spiritual care aims to address existential concerns, promote resilience, instill hope and purpose, and aid in coping with chronic diseases (22). Although studies have explored spiritual care’s impact on health conditions, its influence on the psychological well-being and quality of life in adults with HF is an ongoing area of investigation (23). Recognizing the potential benefits of spiritual care is crucial as it offers a patient-centered addition to the current management of HF. However, evidence on the effectiveness of spiritual care interventions in this population is fragmented, with varying results across studies.
To address the gap in understanding the effectiveness of spiritual care in adults with HF and provide a comprehensive understanding of the topic, we conducted a systematic review. The objective of this systematic review was to determine the impact of spiritual care interventions on the psychological health and quality of life of adults with HF. Specifically, we aim to address the following research questions:
a) What are the different types of spiritual care interventions applied in the management of adults with HF?
b) What are the effects of spiritual care interventions on the quality of life and subjective well-being of adults with HF?
c) What factors influence the effectiveness of spiritual care for patients with HF?
Through this systematic review, we aimed to provide healthcare professionals, policymakers, and researchers with a comprehensive overview of the current evidence on the role of spiritual care in the management of HF. The findings may serve as a foundation for future research, leading to tailored interventions for adults with HF.
Methods
Design
Systematic review according to the recommendations of the PRISMA guidelines. Meta-analysis was not performed due to the inclusion of diverse interventions in the studies. Studies included in this review must be controlled trials (CTS) using a rigorous study design.
Identification
Electronic databases were used to search the relevant literature, such as PubMed, Web of Science, Google Scholar, Science Direct, Elsevier, Springer Link, and Wiley. The initial step involved identifying keywords and phrases relevant to the research topic: “spiritual care,” “heart failure,” “adults,” and related terms. Search strategies were created by combining the identified keywords using Boolean operators (AND, OR). Search strategies: (“spiritual care” OR “spirituality” OR “spiritual intervention” OR “prayer” OR “meditation” OR “mindfulness practices” OR “religious rituals” OR “counseling” OR “support groups) AND (“heart failure”).
Screening
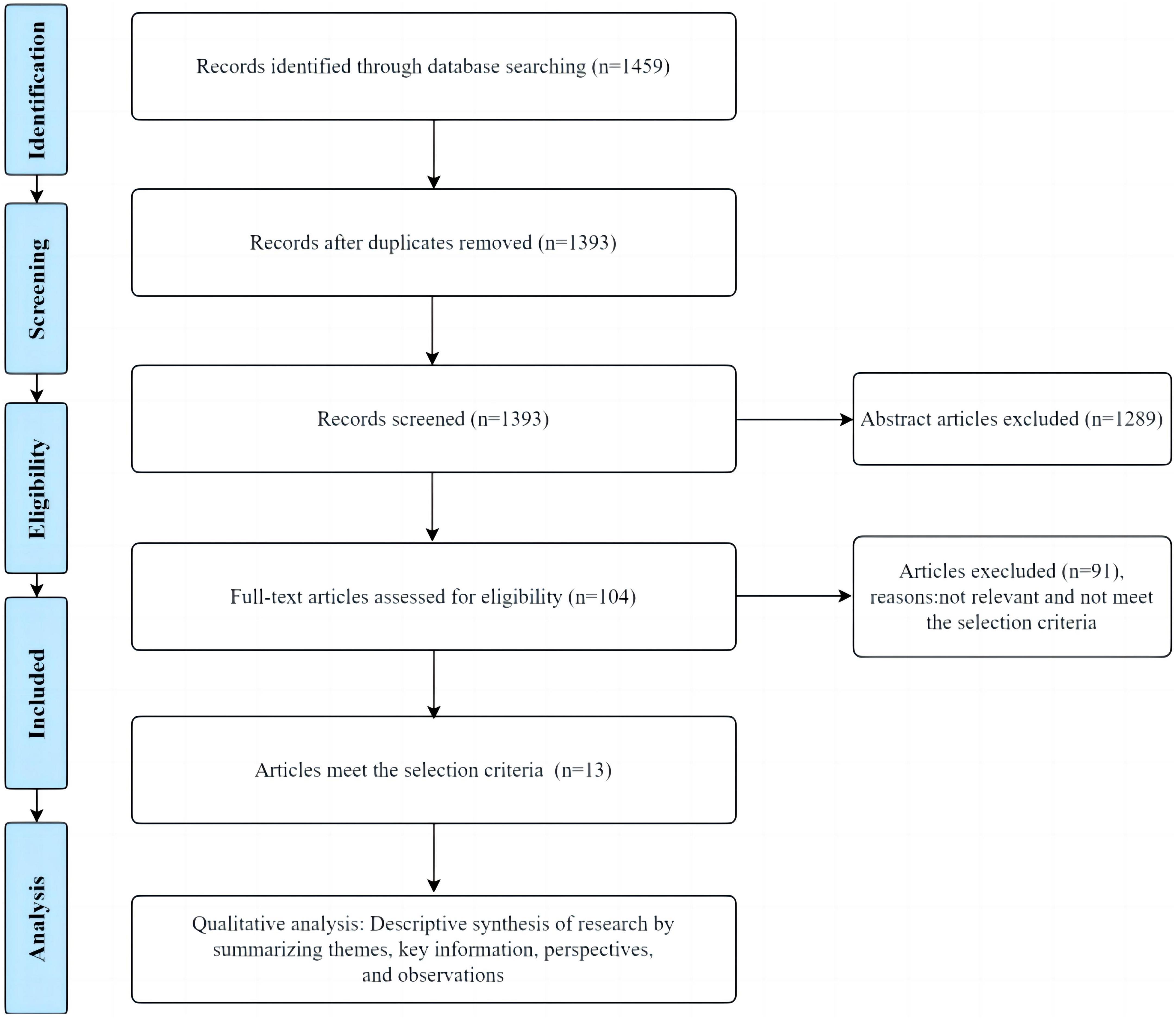
Endnote 20 software was used for literature screening (24). Initially, 1459 articles were retrieved from databases. After identifying and removing 66 duplicate articles using the software, 1393 articles remained. Subsequently, the titles and abstracts of the retrieved articles were assessed, resulting in the exclusion of 1289 articles that were irrelevant to the research topic. Next, a full-text evaluation was performed on the remaining 104 articles, excluding those that did not meet the research objectives and screening criteria.
Inclusion criteria: (1) Studies that investigated the impact of spiritual care interventions on adults with HF. (2) Spiritual care interventions could encompass a variety of approaches, such as prayer, meditation, mindfulness practices, religious rituals, counseling, support groups, and any interventions that explicitly address the spiritual well-being of the participants. (3) Controlled trial study. Eligible comparators could include standard medical care, usual care without a spiritual care component, placebo, or alternative psychosocial interventions. (4) The primary outcomes of interest were related to the psychological health and quality of life of adults with HF. Psychological health outcomes could include but were not limited to measures of depression, anxiety, stress, coping strategies, and existential well-being. Quality of life outcomes could include both disease-specific measures related to HF and generic measures assessing overall well-being, physical functioning, social functioning, and emotional well-being. (5) Studies published in the English language. (6) There were no restrictions on the date.
Exclusion criteria: (1) Review articles, editorials, conference abstracts, case reports, letters to the editor, commentaries, and opinion pieces. (2) Studies that primarily involved pediatric populations or individuals with other chronic diseases unrelated to HF. (3) Studies that did not evaluate spiritual care interventions or did not explicitly address the spiritual well-being of participants. (4) Studies that did not report relevant psychological health or quality of life outcomes. (5) Studies published in languages other than English.
The two authors (nurses) screened the titles of the retrieved articles and separated potentially relevant articles. The eligibility of the relevant abstracts was reviewed independently by the two authors, who examined the abstract of each article. The two authors used standard pretest selection forms independently to assess eligibility. When necessary, other researchers would be involved to reach a consensus.
Eligibility
The 104 articles that met the initial screening requirements were analyzed in detail according to predefined inclusion criteria, of which 13 articles cared for adults with HF by either a spiritual or spiritual care intervention or by conventional care. At least one aspect of mental health or quality of life was measured using a questionnaire and other measurement tools (Figure 1).
Included articles
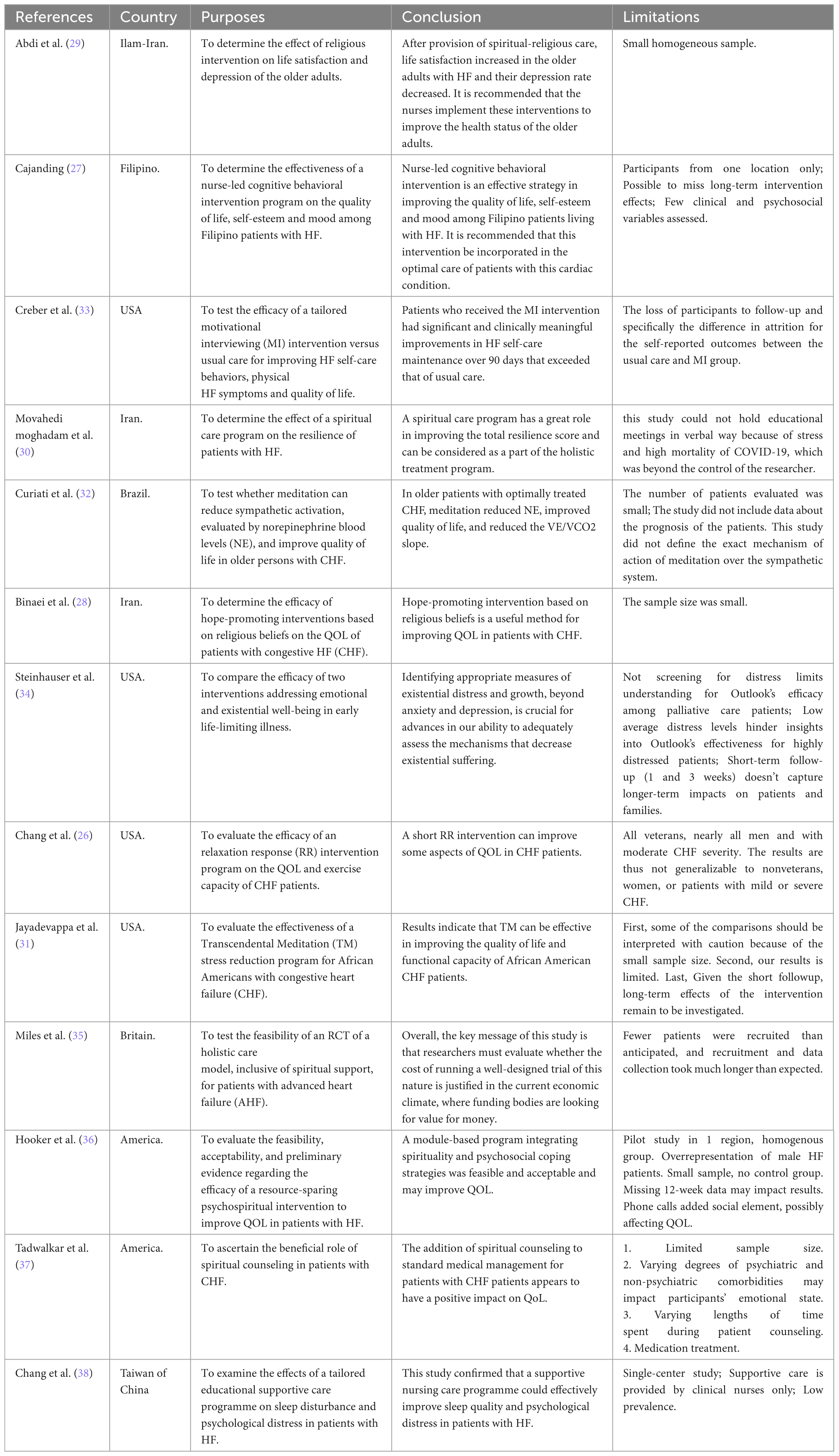
Following a full-text evaluation of the research objectives and selection criteria, we identified relevant literature for further analysis. These selected articles closely aligned with the research objectives in theme, sample, methods, and results. The eligible literature was utilized for data extraction, analysis, and synthesis to support research conclusions and findings. Table 1 lists the relevant literature meeting the research objectives and selection criteria.
Data items
Data extracted from included studies were (1) author, (2) year of publication, (3) country, (4) purposes, (5) study design, (6) sample size, (7) participants, (8) intervention measures, (9) measurement methods, (10) findings, (11) conclusion, and (12) limitations. Where information was missing or unclear, we tried to contact the trial authors for further information.
Cochrane bias risk assessment
The Cochrane bias risk assessment tool was evaluated on seven criteria, including random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other biases. For each item, low bias, uncertainty of bias risk, and high bias were used to judge and classify the study quality (25). The two nurses worked independently, and any discrepancies were resolved through consultation with two senior researchers.
Analysis
Due to the heterogeneity of the studies, statistical analysis was not conducted. Instead, thematic analysis and narrative synthesis were employed to depict the study’s content. A descriptive summary of the included studies was used to organize intervention measures, participants, and outcome indicators. The characteristics of the study interventions were compared with each integrated program group. The impact of spiritual care on the quality of life and mental health in adults with HF was reviewed narratively.
Results
Overview of included studies
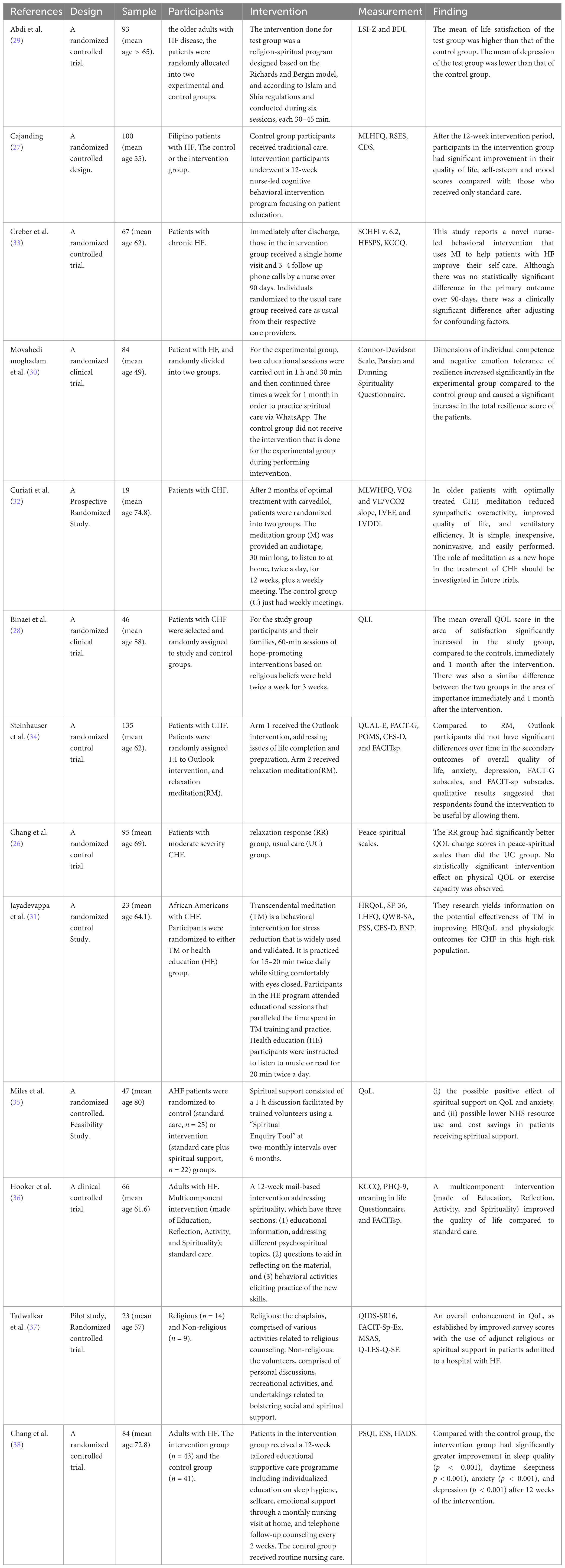
The 13 studies included were published between 2005 and 2022. The general characteristics of the selected studies are shown in Table 1. Table 2 provides a comprehensive overview of the key characteristics of the included studies in this systematic review, in study design, patient populations, interventions, and assessment outcomes. The characteristics of the included studies are summarized as follows: (1) Participants: A total of 882 patients were included in 13 studies. Diagnoses included HF (38.46%) and congestive HF (61.54%). (2) Study Group interventions: In addition to routine care, the study group included four spiritual interventions: Religion (n = 3), meditation (n = 4), mental health and cognitive interventions (n = 3), and spiritual support (n = 3). (3) Control group interventions: Most control groups received traditional usual care from their respective care providers, characterized by medical/drug-optimized therapy and HF-specific preventable risk factor modification strategies prescribed by cardiologists following Heart Association clinical practice guidelines. (4) Outcome measures: In selected studies, assessments were made on a variety of scales: Life Satisfaction and Well-being: Life Satisfaction Questionnaire (LSI-Z), Beck Depression Inventory (BDI) and QoL Enjoyment and Satisfaction (Q-LES-Q-SF); Heart Failure-Specific Quality of Life: Minnesota Living with Heart Failure Questionnaire (MLHFQ), Kansas City Cardiomyopathy Questionnaire (KCCQ) and Minnesota Living with Heart Failure Questionnaire (MLWHFQ); Self-Care and Heart Failure Management: Self-Care of Heart Failure Index (SCHFI v.6.2) and Heart Failure Somatic Perception Scale (HFSPS); Spirituality and Well-being: Connor-Davidson Resilience Scale, Parsian and Dunning Spirituality Questionnaire and Peace-Spiritual Scales; Psychological Health and Emotional Well-being: Rosenberg Self-Esteem Scale (RSES), Quick Inventory of Depressive Symptomatology (QIDS-SR16), Hospital Anxiety and Depression Scale (HADS), Cardiac Depression Scale (CDS), Profile of Mood States (POMS), Center for Epidemiologic Studies Depression Scale (CES-D), Functional Assessment of Chronic Illness Therapy Spiritual Well-Being Scale (FACITsp) and Memorial Symptom Assessment Scale (MSAS); Heart Failure Physiology and Function: VO2 and VE/VCO2 Slope, Left Ventricular Ejection Fraction (LVEF), Left Ventricular Diastolic Dimension index (LVDDi) and Brain Natriuretic Peptide (BNP); Health-Related Quality of Life (HRQoL): Health-Related Quality of Life (HRQoL), Short Form 36 (SF-36), Chinese versions of the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS) and Quality of Life Well being Scale-Self Administered (QWB-SA); Overall Quality of Life and General Well-being: Quality of Life Index (QLI), Quality of Life at the End of Life (QUAL-E) Overall Quality of Life and General Well-being: Quality of Life Index (QLI), Quality of Life at the end of Life (Qual-e) and Functional Assessment of Cancer Therapy - General (FACT-G).
Quality of included studies
The Cochrane Risk of Bias tool revealed moderate potential bias across all studies, focusing on critical domains such as random sequence generation and allocation concealment. The 13 studies (26–38) meticulously detailed the processes involved in generating the random sequence, utilizing methods such as random number tables and computer-generated randomization. However, 10 studies (26, 28–34, 36, 37) were unclear about adequate measures for concealing allocation. Given the nature of spiritual care interventions, blinding of participants was unfeasible in the majority of studies. Nevertheless, 5 studies (27, 31, 32, 34, 38) blinded outcome assessors in the intervention group. Regarding attrition bias, only one study mentioned attrition without specifying reasons (33). In contrast, other studies provided detailed explanations for participant dropouts. In summary, the moderate risk classification of included studies highlights the need for cautious interpretation and emphasizes the importance of considering potential biases while assessing the evidence. Figures 2, 3 provide detailed insights into each study’s risk of bias.
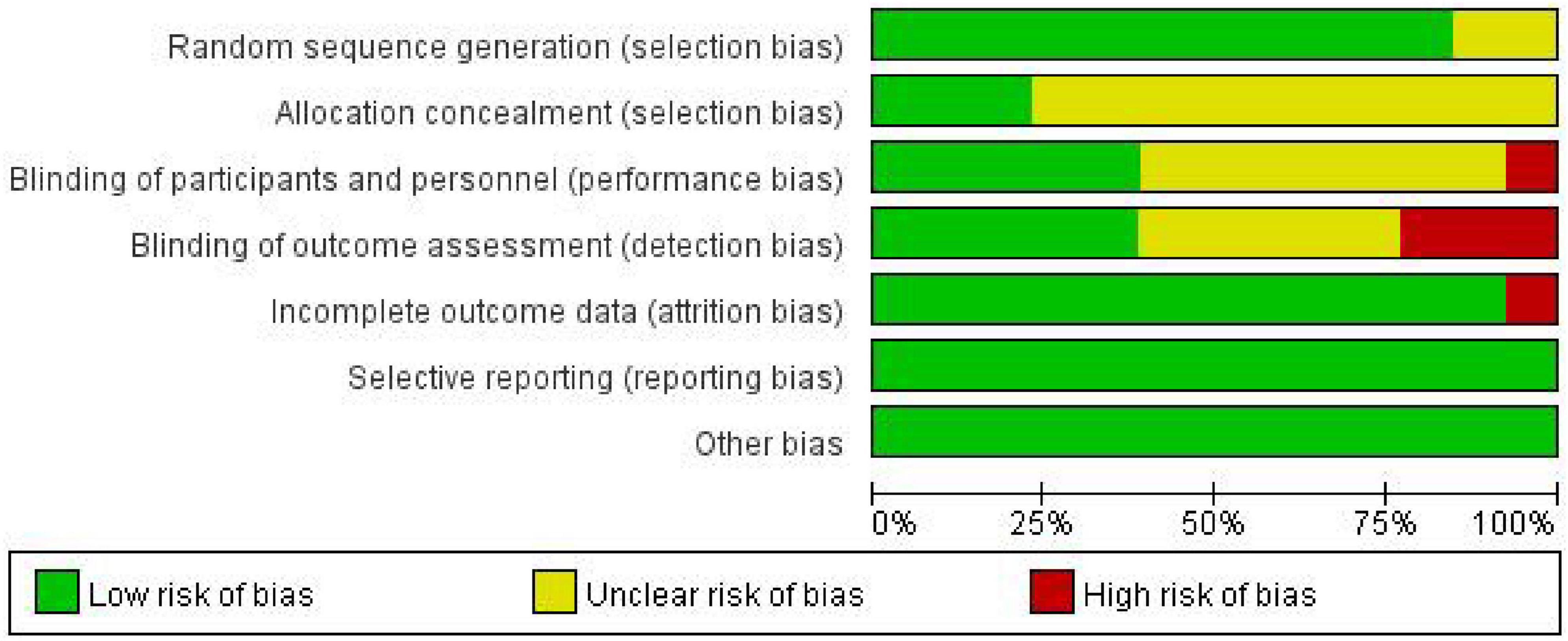
Figure 2. Risk of bias graph: review authors’ judgments about each risk of bias item presented as percentages across all included studies.
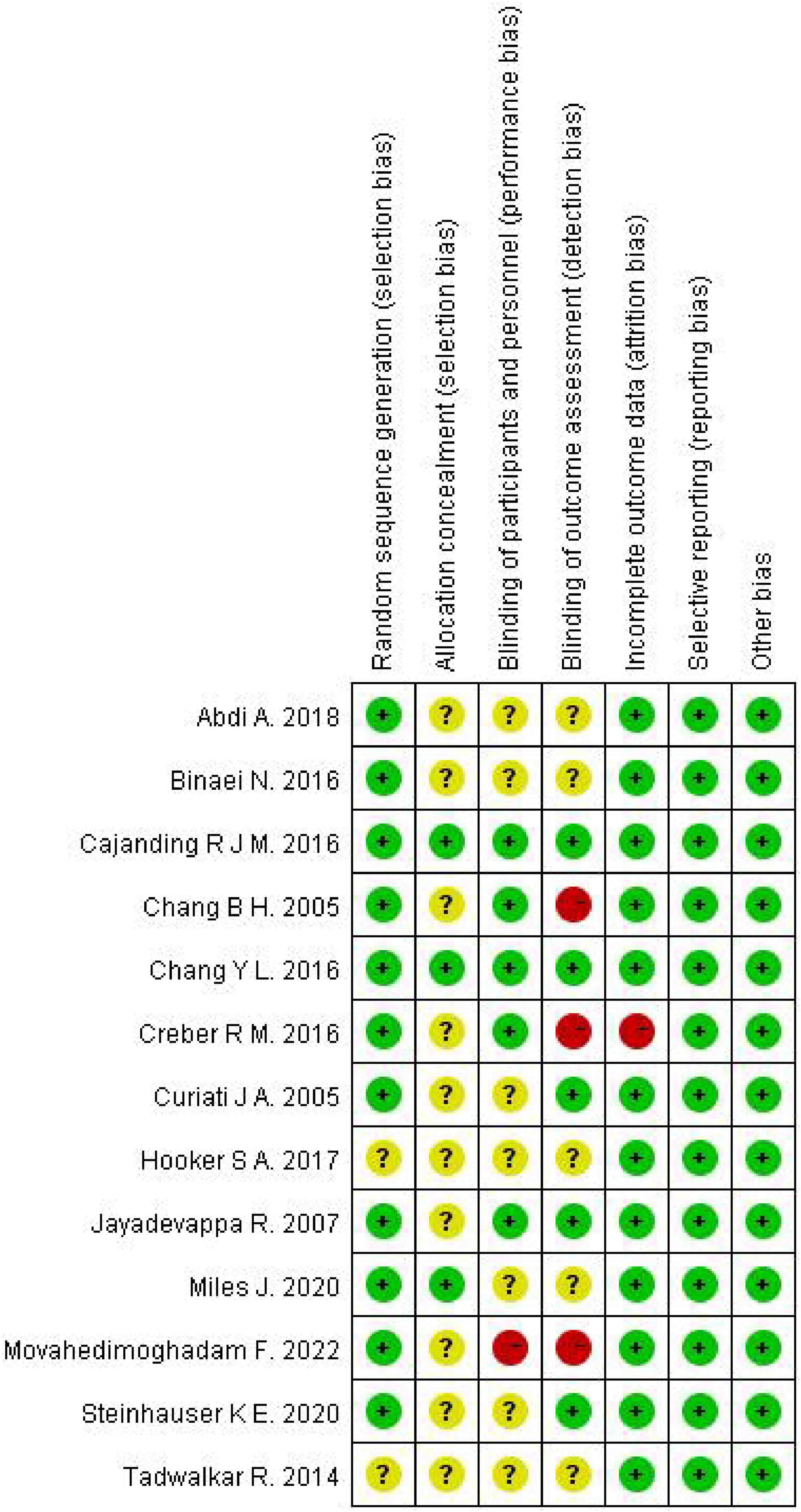
Figure 3. Risk of bias summary: review authors’ judgments about each risk of bias item for each included study.
The impact of spiritual care
A total of 13 studies (26–38) investigated the impact of spiritual care on mental health and quality of life in patients with HF. 9 of these studies (26–32, 37, 38) reported that spiritual care was associated with statistically and clinically significant improvements in mental health and quality of life. The effects of spiritual care are as follows:
(1) Quality of life and satisfaction
11 studies (26–29, 32–38) evaluated the impact of spiritual care on the quality of life of patients with HF. Among them, 8 studies involving interventions such as meditation (26, 32, 34), religious beliefs (28, 29, 37), spiritual support (38) and cognitive interventions (27) demonstrated significant improvement in the life quality of the intervention group, with mean life satisfaction higher than that of the control group. 3 studies (33, 35, 36) showed no significant difference in the quality of life between the intervention and control groups.
(2) Emotional health
8 studies (26, 27, 29, 31, 32, 34, 37, 38) assessed the impact of spiritual care on emotional health (anxiety, depression). In these 8 studies, the intervention group exhibited improvements in overall scores on scales related to emotional well-being, such as the POMS and CESD scale, compared to the control group, leading to an enhancement in patients’ emotional health.
(3) Physical function
Three studies (31–33) evaluated the impact of spiritual care on physical function. Two studies (31, 32) indicated that meditation led to improvements in physical functions, such as blood pressure levels and exercise tolerance, among the intervention group. However, one study (33) suggested that tailored Motivational Interviewing (MI) intervention showed no difference in improving physical symptoms of HF compared to standard care.
(4) Mental Health
Two studies (28, 30) reported the impact of spiritual care on mental health. The results showed a statistically significant increase in spiritual scores and improved mental well-being for the experimental group after the intervention (t72 = 0.66, p = 0.511).
Discussion
The findings of this systematic review have significant implications for the field of spiritual care, especially for patients with HF. After reviewing the studies, it is evident that existing theories and models of spiritual care strongly support the role of spirituality in enhancing patients’ well-being. The positive outcomes observed in mental health and quality of life support the theoretical frameworks proposing a holistic approach to patient care, considering physical, psychological, and spiritual dimensions. Furthermore, the variety of interventions utilized throughout the studies presents a new perspective on how spiritual care can be customized to fulfill the unique needs of patients with different cultural backgrounds, religious beliefs, and personal values. This indicates that spiritual care is an adaptive practice that can be adapted to different theoretical foundations while respecting individual variations. In addition, the findings highlight the importance of incorporating spiritual care interventions into the clinical management of patients with HF. Integrating spiritual care into the comprehensive treatment plan can provide emotional support, improve coping mechanisms, and increase overall quality of life. Healthcare professionals should receive training and resources to communicate effectively about spiritual care. Developing educational materials and guidelines that respect patients’ cultural and religious beliefs can improve spiritual care interventions. It is also crucial to recognize that spiritual care is not limited to religious practices and encompasses personal beliefs and practices that contribute to patients’ emotional and psychological well-being.
In managing patients with HF, medical treatment, lifestyle adjustments, and emotional well-being are crucial aspects. Spiritual care is a nursing approach that prioritizes the spiritual and inner needs of patients. It emphasizes the cultivation of inner calm and hope, aiming to improve their psychological well-being and quality of life (39). The study indicated that spiritual care can improve the psychological well-being and quality of life of cancer patients and their family caregivers (40, 41). Vespa et al. (42) found that mindfulness training can enhance emotional and cognitive balance, as well as happiness, for early-stage Alzheimer’s disease patients and their caregivers, thereby improving their quality of life. Spiritual care encompasses various religious and non-religious practices, aimed at helping patients find inner strength and meaning and establishing connections with others, nature, and a higher power (43). In this study, we have identified several key factors that influence the effectiveness of spiritual care: (1) Alignment with patient beliefs and values. Tailoring spiritual care to align with a patient’s beliefs and values is essential. Studies have shown that spiritual care is more effective when it resonates with an individual’s personal belief system, ensuring the intervention is meaningful and relevant to their spiritual journey (44). (2) Quality and relevance of the intervention. The impact of spiritual care on patients is influenced by its quality, relevance, and appropriateness (31, 32, 37, 38). Interventions like meditation, when well-designed and relevant to the patient’s needs, have demonstrated improvements in various aspects of well-being, highlighting the importance of a well-crafted intervention. (3) Patient participation. Actively involving patients in spiritual care and encouraging their participation can significantly impact its effectiveness (34). Patients who actively engage in spiritual practices and discussions often experience deeper benefits, indicating the importance of patient involvement in the process. (4) Respect for diversity and cultural competence. The effectiveness of spiritual nursing interventions is significantly influenced by cultural, religious, and individual contexts. Recognizing and respecting the diversity of spiritual and religious beliefs among patients is crucial. Cultural competence and sensitivity ensure that spiritual care is tailored to individual cultural contexts, making it more effective and meaningful for the patient (45). (5) Integration into routine care. To achieve the best treatment outcomes, it is crucial for healthcare providers, to integrate spiritual care into routine healthcare practices (27, 30, 38). When healthcare providers integrate spiritual care with medical treatments, patients experience better outcomes.
With the healthcare landscape evolving, virtual mental nursing platforms offer exciting opportunities to enhance spiritual care for patients with HF (46). This adaptability to modern healthcare contexts while retaining core spiritual care principles is a testament to the dynamic nature of the field. From a clinical perspective, incorporating technology into spiritual care interventions offers promising prospects. For example, virtual spiritual care platforms can help overcome the challenges of social distancing and limited physical interactions (47). Particularly relevant in the context of pandemics and widespread digital connectivity, these platforms provide patients with a means to access spiritual care remotely, transcending barriers like transportation, physical limitations, or geographical distances (48). This technological evolution not only improves patient access to care but also highlights the adaptability of spiritual care practices to meet the demands of modern healthcare (49). Methodologically, the introduction of virtual spiritual care platforms brings new considerations. These technologies broaden the feasibility and scalability of spiritual care interventions, potentially reaching a wider patient population (50). However, it is crucial to substantiate the effectiveness and safety of these interventions through rigorous research. Comparative studies that evaluate outcomes between traditional in-person spiritual care and technology-driven interventions can establish the reliability and validity of these innovative methods. Despite these advancements, it is important to acknowledge potential limitations. Patient technological literacy, device accessibility, and comfort with virtual interactions may impact the feasibility and acceptance of technology-driven interventions (51). Ensuring inclusivity is crucial, requiring investigations into these aspects to prevent any unintended exclusion of certain patient groups (52). Additionally, the ethical considerations of utilizing virtual mental nursing platforms in spiritual care must be addressed, encompassing concerns related to data privacy, algorithm transparency, and patient autonomy (53, 54).
The methodological considerations arising from the reviewed studies offer insights into the rationality and feasibility of spiritual care interventions. The range of spiritual care interventions used in studies highlights their adaptability to meet the unique needs of patients. Additionally, the use of validated assessment tools for spiritual care, such as those focusing on depression, quality of life, and coping mechanisms, enhances the credibility and reliability of the findings. However, the limitations identified in the reviewed studies prompt considerations for future research in this field. While the positive outcomes of spiritual care interventions are promising, biases stemming from small sample sizes and single-site studies underscore the need for larger, multicenter trials. Furthermore, the cultural and religious diversity among patients necessitates more research on specific populations to determine how different belief systems and practices interact with spiritual care interventions. Exploring the impact of interventions across various cultural backgrounds and religious affiliations can offer a nuanced understanding of how spirituality influences patient outcomes. Additionally, the potential mediating role of spirituality in influencing patients’ adherence to medical treatments and lifestyle modifications warrants further investigation.
There are some limitations in this study. First, there is methodological heterogeneity in the studies included. There are some differences in study sample size, intervention methods, and assessment tools, which may affect the accuracy of the analysis. Second, most studies have focused on patients in specific regions or cultures, which limits the generalisability and generalization of the findings. Finally, The number of included studies is limited and more studies are needed to strengthen the robustness of our findings. Therefore, the current review cannot rule out possible publication bias. Nevertheless, these results have important implications for practice, policy, and future research. For example, these findings may prompt medical professionals to re-examine and improve the care they give to patients with HF. In addition, these results may guide future research and encourage further exploration of interventions related to mental health and quality of life in patients with HF.
Conclusion
In conclusion, this systematic review highlights the positive influence of spiritual care interventions on the psychological health and quality of life of patients with HF. It emphasizes the need for tailored interventions, healthcare professional involvement, and continued research to better understand and optimize the impact of spiritual care in this patient population. The review bridges the gap between theoretical foundations and practical applications, emphasizing the adaptive nature of spiritual care that accommodates the diverse cultural and religious backgrounds of patients.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
GZ: Writing – original draft, Resources, Methodology, Formal analysis, Data curation, Conceptualization. QZ: Writing – original draft, Validation, Software, Resources, Formal analysis, Data curation. FL: Writing – review and editing, Methodology, Funding acquisition, Formal analysis.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study received funding from the Health Science and Technology Ability Improvement Project Foundation of Jilin Province (Grant No. 2021GL001).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Brunner-La Rocca HP, Fleischhacker L, Golubnitschaja O, Heemskerk F, Helms T, Hoedemakers T, et al. Challenges in personalised management of chronic diseases–heart failure as prominent example to advance the care process. EPMA J. (2016) 7:2. doi: 10.1186/s13167-016-0051-9
2. Ziaeian B, Fonarow GC. Epidemiology and aetiology of heart failure. Nat Rev Cardiol. (2016) 13:368–78.
4. Chen L, Song J, Hu S. Metabolic remodeling of substrate utilization during heart failure progression. Heart Fail Rev. (2019) 24:143–54.
5. Pearse SG, Cowie MR. Heart failure: Classification and pathophysiology. Medicine. (2014) 42:556–61.
6. Upadhya B, Kitzman DW. Heart failure with preserved ejection fraction: New approaches to diagnosis and management. Clin Cardiol. (2020) 43:145–55.
7. Bloom MW, Greenberg B, Jaarsma T, Januzzi JL, Lam CSP, Maggioni AP, et al. Heart failure with reduced ejection fraction. Nat Rev Dis Prim. (2017) 3:1–19.
8. Gysels MH, Higginson IJ. The lived experience of breathlessness and its implications for care: A qualitative comparison in cancer, COPD, heart failure and MND. BMC Palliat Care. (2011) 10:15. doi: 10.1186/1472-684X-10-15
9. Niu H, Liu J. The psychological trajectory from diagnosis to approaching end of life in patients undergoing hemodialysis in China: A qualitative study. Int J Nurs Sci. (2016) 4:29–33. doi: 10.1016/j.ijnss.2016.10.006
10. Naghi JJ, Philip KJ, Phan A, Cleenewerck L, Schwarz ER. The effects of spirituality and religion on outcomes in patients with chronic heart failure. J Relig Health. (2012) 51:1124–36.
11. Savarese G, Lund LH. Global public health burden of heart failure. Card Fail Rev. (2017) 3:7–11.
12. Azad N, Lemay G. Management of chronic heart failure in the older population. J Geriatr Cardiol. (2014) 11:329–37.
13. Pratt R, Hibberd C, Cameron IM, Maxwell M. The patient centered assessment method (PCAM): Integrating the social dimensions of health into primary care. J Comorb. (2015) 5:110–9. doi: 10.15256/joc.2015.5.35
14. Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. (2006) 3:e442. doi: 10.1371/journal.pmed.0030442
15. Kubzansky LD, Huffman JC, Boehm JK, Hernandez R, Kim ES, Koga HK, et al. Positive psychological well-being and cardiovascular disease: JACC health promotion series. J Am Coll Cardiol. (2018) 72:1382–96.
16. Solomon B, Sutton D, McKenna B. The experience and meaning of recovery-oriented practice for nurses working in acute mental health services. Int J Ment Health Nurs. (2021) 30:963–74.
17. Tavares AP, Martins H, Pinto S, Caldeira S, Sousa PP, Rodgers B. Spiritual comfort, spiritual support, and spiritual care: A simultaneous concept analysis. Nurs Forum. (2022) 57:1559–66. doi: 10.1111/nuf.12845
18. Sawatzky R, Pesut B. Attributes of spiritual care in nursing practice. J Holist Nurs. (2005) 23:19–33.
19. Kushner RF, Sorensen KW. Lifestyle medicine: The future of chronic disease management. Curr Opin Endocrinol Diabetes Obes. (2013) 20:389–95.
21. Vis JA, Marie Boynton H. Spirituality and transcendent meaning making: Possibilities for enhancing posttraumatic growth. J Relig Spiritual Soc Work. (2008) 27:69–86.
22. Haufe, M, Leget C, Potma M, Teunissen S. How can existential or spiritual strengths be fostered in palliative care? An interpretative synthesis of recent literature. BMJ Support Palliat Care. (2020):2379.
23. Park CL, Sacco SJ. Heart failure patients’ desires for spiritual care, perceived constraints, and unmet spiritual needs: Relations with well-being and health-related quality of life. Psychol Health Med. (2017) 22:1011–20. doi: 10.1080/13548506.2016.1257813
24. Idris SA, Qureshi AG, Elkhair IS, Idris TA, Adam AM, Mohammed NK. Usefulness of EndNote software for writing scientific manuscripts: A comparative study. Health Res. (2019) 7:6–10.
25. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:d5928.
26. Chang BH, Hendricks A, Zhao Y, Rothendler JA, LoCastro JS, Slawsky MT. A relaxation response randomized trial on patients with chronic heart failure. J Cardiopulm Rehabil. (2005) 25:149–57.
27. Cajanding RJ. The effectiveness of a nurse-led cognitive–behavioral therapy on the quality of life, self-esteem and mood among Filipino patients living with heart failure: A randomized controlled trial. Appl Nurs Res. (2016) 31:86–93. doi: 10.1016/j.apnr.2016.01.002
28. Binaei N, Moeini M, Sadeghi M, Najafi M, Mohagheghian Z. Effects of hope promoting interventions based on religious beliefs on quality of life of patients with congestive heart failure and their families. Iran J Nurs Midwifery Res. (2016) 21:77–83. doi: 10.4103/1735-9066.174755
29. Abdi A, Soufinia A, Borji M, Tarjoman A. The effect of religion intervention on life satisfaction and depression in elderly with heart failure. J Relig Health. (2019) 58:823–32. doi: 10.1007/s10943-018-0727-7
30. Movahedimoghadam F, Naderi N, Shabani F, Fathollahi MS. Effect of spiritual care program on resilience in patients with heart failure: A randomized controlled clinical trial. Iran J Nurs Midwifery Res. (2022) 27:266–73. doi: 10.4103/ijnmr.ijnmr_61_21
31. Jayadevappa R, Johnson JC, Bloom BS, Nidich S, Desai S, Chhatre S, et al. Effectiveness of transcendental meditation on functional capacity and quality of life of African Americans with congestive heart failure: A randomized control study. Ethn Dis. (2007) 17:72–7.
32. Curiati JA, Bocchi E, Freire JO, Arantes AC, Braga M, Garcia Y, et al. Meditation reduces sympathetic activation and improves the quality of life in elderly patients with optimally treated heart failure: A prospective randomized study. J Altern Complement Med. (2005) 11:465–72. doi: 10.1089/acm.2005.11.465
33. Creber RM, Patey M, Lee CS, Kuan A, Jurgens C, Riegel B. Motivational interviewing to improve self-care for patients with chronic heart failure: MITI-HF randomized controlled trial. Patient Educ Couns. (2016) 99:256–64. doi: 10.1016/j.pec.2015.08.031
34. Steinhauser KE, Stechuchak KM, Ramos K, Winger J, Tulsky JA, Olsen MK. Current measures of distress may not account for what’s most important in existential care interventions: Results of the outlook trial. Palliat Support Care. (2020) 18:648–57.
35. Miles J, Ross L, Jarvis P, Pickett S. Spiritual support in advanced heart failure: A randomized controlled feasibility study. Health Social Care Chaplain. (2021) 9:148.
36. Hooker S, Ross K, Masters K, Park C, Hale A, Allen L, et al. Denver spirited heart: Mixed-methods pilot study of a psychospiritual intervention for heart failure patients. J Cardiovasc Nurs. (2017) 32:226–35. doi: 10.1097/JCN.0000000000000337
37. Tadwalkar R, Udeoji D, Weiner R, Avestruz F, LaChance D, Phan A, et al. The beneficial role of spiritual counseling in heart failure patients. J Relig Health. (2014) 53:1575–85. doi: 10.1007/s10943-014-9853-z
38. Chang Y, Chiou A, Cheng S, Lin K. Tailored educational supportive care programme on sleep quality and psychological distress in patients with heart failure: A randomised controlled trial. Int J Nurs Stud. (2016) 61:219–29. doi: 10.1016/j.ijnurstu.2016.07.002
39. Whoqol Srpb Group. A cross-cultural study of spirituality, religion, and personal beliefs as components of quality of life. Soc Sci Med. (2006) 62:1486–97.
40. Spatuzzi R, Giulietti M, Ricciuti M, Merico F, Fabbietti P, Raucci L, et al. Exploring the associations between spiritual well-being, burden, and quality of life in family caregivers of cancer patients. Palliat Support Care. (2019) 17:294–9.
41. Vespa A, Spatuzzi R, Merico F, Ottaviani M, Fabbietti P, Meloni C, et al. Spiritual well-being associated with personality traits and quality of life in family caregivers of cancer patients. Support Care Cancer. (2018) 26:2633–40. doi: 10.1007/s00520-018-4107-3
42. Vespa A, Fabbietti P, Giulietti M. Study of the effects of mindfulness training on quality of life of patients with Alzheimer’s disease and their caregivers (dyad mindfulness project). Aging Clin Exp Res. (2022) 34:65–71. doi: 10.1007/s40520-021-01907-x
43. Chiang YC, Lee HC, Chu TL, Han CY, Hsiao YC. The impact of nurses’ spiritual health on their attitudes toward spiritual care, professional commitment, and caring. Nurs Outlook. (2016) 64:215–24. doi: 10.1016/j.outlook.2015.11.012
44. Selman LE, Brighton LJ, Sinclair S, Karvinen I, Egan R, Speck P, et al. Patients’ and caregivers’ needs, experiences, preferences and research priorities in spiritual care: A focus group study across nine countries. Palliat Med. (2018) 32:216–30. doi: 10.1177/0269216317734954
45. Fang ML, Sixsmith J, Sinclair S, Horst G. A knowledge synthesis of culturally-and spiritually-sensitive end-of-life care: Findings from a scoping review. BMC Geriatr. (2016) 16:107. doi: 10.1186/s12877-016-0282-6
47. Tavakoli M, Carriere J, Torabi A. Robotics, smart wearable technologies, and autonomous intelligent systems for healthcare during the COVID-19 pandemic: An analysis of the state of the art and future vision. Adv Intell Syst. (2020) 2:2000071.
48. Lee, P, Abernethy A, Shaywitz D, Gundlapalli AV, Weinstein J, Doraiswamy PM, et al. Digital health COVID-19 impact assessment: Lessons learned and compelling needs. NAM Perspect. (2022) 2022. doi: 10.31478/202201c
49. Archibald MM, Barnard A. Futurism in nursing: Technology, robotics and the fundamentals of care. J Clin Nurs. (2018) 27:2473–80. doi: 10.1111/jocn.14081
50. Lee EE, Torous J, De Choudhury M, Depp CA, Graham SA, Kim HO, et al. Artificial intelligence for mental health care: Clinical applications, barriers, facilitators, and artificial wisdom. Biol Psychiatry Cogn Neurosci Neuroimaging. (2021) 6:856–64. doi: 10.1016/j.bpsc.2021.02.001
51. Fujioka JK, Budhwani S, Thomas-Jacques T, De Vera K, Challa P, Fuller K, et al. Challenges and strategies for promoting health equity in virtual care: Protocol for a scoping review of reviews. JMIR Res Protoc. (2020) 9:e22847. doi: 10.2196/22847
52. Pons P, Navas-Medrano S, Soler-Dominguez JL. Extended reality for mental health: Current trends and future challenges. Front Comput Sci. (2022) 4:1034307. doi: 10.3389/fcomp.2022.1034307
53. Jacobson NC, Bentley KH, Walton A, Wang SB, Fortgang RG, Millner AJ, et al. Ethical dilemmas posed by mobile health and machine learning in psychiatry research. Bull World Health Organ. (2020) 98:270–6. doi: 10.2471/BLT.19.237107
Keywords: heart failure, spiritual care, psychological health, quality of life, randomized controlled study
Citation: Zhang G, Zhang Q and Li F (2024) The impact of spiritual care on the psychological health and quality of life of adults with heart failure: a systematic review of randomized trials. Front. Med. 11:1334920. doi: 10.3389/fmed.2024.1334920
Received: 08 November 2023; Accepted: 05 March 2024;
Published: 17 April 2024.
Edited by:
Jacqueline G. Bloomfield, The University of Sydney, AustraliaReviewed by:
Eron Grant Manusov, The University of Texas Rio Grande Valley, United StatesPaolo Fabbietti, National Institute of Health and Sciences on Aging (IRCCS), Italy
Copyright © 2024 Zhang, Zhang and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fan Li, bGlmYW5Aamx1LmVkdS5jbg==
 Guangwei Zhang1,2
Guangwei Zhang1,2 Fan Li
Fan Li