- 1Clalit Health Services, Tel Aviv, Israel
- 2Shmuel Harofe Geriatric Medical Center, Beer Ya’akov, Israel
- 3Tel Aviv University School of Medicine, Ramat Aviv, Israel
- 4Rabin Medical Center, Beilinson Hospital, Petah-Tikva, Israel
- 5Technion University School of Public Health, Haifa, Israel
Background: Nursing care residents have high hospitalization rates. To address this, we established a unique virtual geriatric unit that has developed a program aimed at providing support to nursing homes.
Aims: We aimed to evaluate effectiveness of in-house intravenous antibiotic treatment in nursing hospitals after the implementation of the specially designed training program.
Methods: A cohort study of nursing home residents to evaluate a training program for providers, designed to increase awareness and give practical tools for in-house treatment of acute infections. Data obtained included types of infections, antibiotics used, hospital transfer, and length of treatment. Primary outcomes were in-house recovery, hospitalization and mortality. Univariate analysis and multivariable logistic regression analysis to assess association between different factors and recovery.
Results: A total of 890 cases of acute infections were treated with intravenous antibiotics across 10 nursing homes over a total of 4,436 days. Of these cases, 34.8% were aged 90 years or older. Acute pneumonia was the most prevalent infection accounted for 354 cases (40.6%), followed by urinary tract infections (35.7%), and fever of presumed bacterial infection (17.1%). The mean duration of intravenous antibiotic treatment was 5.09 ± 3.86 days. Of the total cases, 800 (91.8%) recovered, 62 (7.1%) required hospitalization and nine (1.0%) resulted in mortality. There was no significant difference observed in recovery rates across different types of infections.
Discussion: Appling a simple yet unique intervention program has led to more “in-house” residents receiving treatment, with positive clinical results.
Conclusion: Treating in-house nursing home residents with acute infections resulted in high recovery rates. Special education programs and collaboration between healthcare organizations can improve treatment outcomes and decrease the burden on the healthcare system.
Introduction
Hospitalization rates and recurrent hospitalization rates are significantly higher in older patients compared to the general adult population (1). Nursing care residents, experience higher hospitalization rates, often due to acute infections (2, 3). The relatively crowded living conditions in the nursing homes (NH) and treatment by the same healthcare providers increase the risk of contagion spread (4, 5). The residents usually suffer from multiple co-morbidities and are prescribed numerous medications (6, 7). The most common infections are urinary tract and respiratory tract, including aspiration pneumonia (2, 8). Proper management of acute infections is a crucial aspect of providing high-quality care to nursing facility residents (9, 10). Literature reports that approximately 40% of patients over 65 with acute infections require hospitalization for treatment (11, 12). Hospitalization of older adults increases negative outcomes such as acute delirium during the hospital stay, cognitive decline, decubitus ulcers, falls, nosocomial infections, and difficulty in returning to previous levels of functioning (13–15). Reducing these negative outcomes can probably be achieved by improving NH in-house treatment. Enabling intravenous treatment may be an important step in that direction. To address this a designated program was designed and executed at the central district of Clalit medical service, the largest mandated health service organization in Israel. Clalit Health Services is the major insurance organization in Israel, with 4,394,000 members. Among the insured, 13.52% are aged 65 or older (16). In the Central Region 15.71% of insured are aged 65 or older with approximately 2,800 residing in skilled nursing care facilities. High quality management of older patients living in long-term care facilities is one of the important aims of older adults’ care. To address this need, we established a unique virtual nursing home center (VNHC) with qualified geriatric professionals. One of the primarily goals of the unit was to improve treatment of acute infections.
Providers in nursing care facilities frequently face the challenging decision whether to treat residents with acute infections in-house or to hospitalize them (17, 18). The decision is complex and depends on various factors. In Israel, skilled nursing facilities are managed and regulated by the Health Ministry, while each resident continues to be insured by their health maintenance organization (HMO). The provisions of medications and of medical services outside of the facility are therefore the responsibility of the HMO. One crucial factor in Israel is the ability of the facility to provide intravenous (IV) antibiotics according to the health ministry criteria and whether the facility has been licensed by the health department to administer that treatment. However, despite being licensed, many facilities still prefer to hospitalize patients with acute infections. We observed other factors influencing this decision. Firstly, there is the additional workload imposed on the medical and nursing staff. Secondly, bureaucratic and logistic difficulties arise in obtaining the appropriate antibiotics. Furthermore, the inertia presents in many facilities with long-standing routines and protocols makes changes difficult to accomplish (19). Lastly, there is a lack of awareness about the complications of hospitalization for older adult patients. The program implemented was designed to address these factors in order to improve in-house quality of infection care. The aims of this study were to evaluate the positive and negative clinical outcomes of the program on in-house intravenous antibiotic treatment in the participating NH.
Materials and methods
In an effort to improve quality of care for residents with acute infections and to prevent hospitalizations, our VNHC staff developed a program to train and provide support to nursing care staff in facilities specially focusing on treatment of acute infections with IV antibiotics. The program included improving the logistics and coordination between the NH and the HMO to facilitate efficient in-house treatment.
Skilled nursing care facilities within the Clalit Health Services in the Central District of Israel were contacted to assess their compliance with the Health Ministry’s criteria for administering IV treatment and whether they had obtained the necessary approval. Out of 26 facilities, only 10 met the criteria. Surprisingly, a review of our HMO database showed high hospitalizations rates (34%) and low IV antibiotics order rates (5%) at these facilities. A 3-pronged intervention was developed by the VNHC staff to aid facilities in providing IV antibiotic treatment. Usually, NH personal receives lower quality of education compared to the hospital staff. Therefore, firstly experienced specialist in geriatric medicine provided lectures to the providers, aiming to increase their awareness and knowledge of hospital complications on older adults’ patients. The providers staff were encouraged to enroll in a designated course on infection diseases treatment in older adult patients. These educational steps helped enhance the knowledge of NH staff and created stronger connections between the healthcare organization’s staff and NH staff. Secondly, enhanced support system was given to the providers. Telephone consultations by the VNHC staff, including senior physician, geriatric expert practitioner nurse and pharmacological staff were made available to the nursing home providers. Thirdly, the logistics of ordering and transporting the required IV antibiotics were streamlined to allow for rapid delivery of the necessary treatments. Ultimately, the decision on how to treat each patient was entrusted to the nursing home staff. While all decisions were made by an in-house physician, a geriatric specialist was always a geriatric specialist on call as needed.
Over a four-year period (2012–2016) following the initiation of the intervention in 2012, the VNHC chief physician kept a register of data on each resident who was treated for an acute infection requiring IV antibiotics in the 10 facilities. All residents met the criteria of the Health Ministry for nursing care or mental frailty, including dependence on others for activities of daily living such as mobility, eating, bathing, getting dressed, toileting, transferring, and continence or requiring continues supervision because of advanced dementia
The data was obtained from the electronic medical records (EMR) of each patient. Data collected included age, gender, name of nursing home facility (NHF); for each acute infection, we recorded the diagnosis, date of diagnosis, date of initiation and completion of treatment, and type of antibiotic given. Recovery or a positive outcome were defined as completing antibiotic course and recovery from symptoms within the NHF while hospital transfer or death were defined as negative outcomes.
Statistical analysis
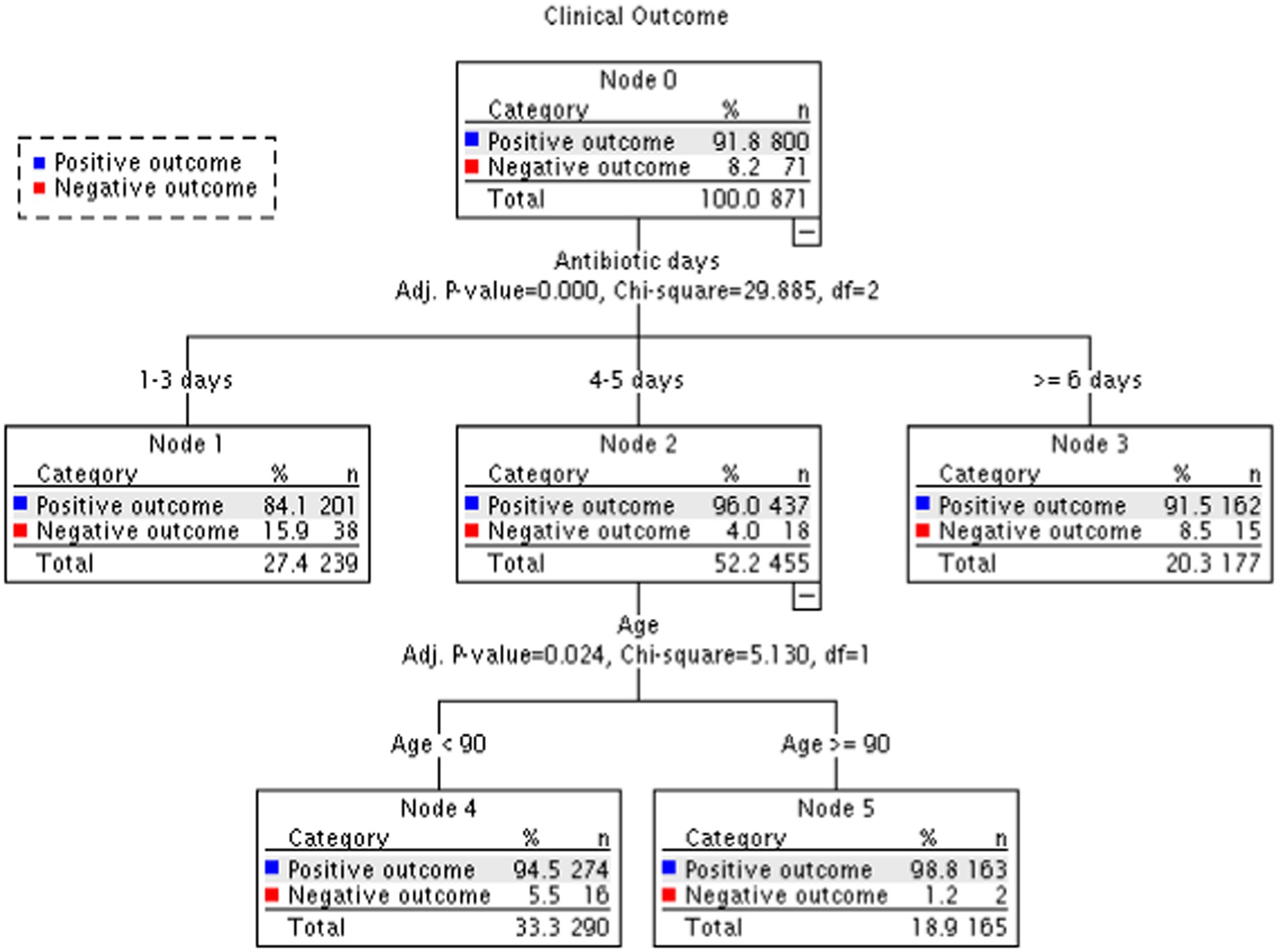
Distribution of categorical variables among type of infections as well as the association between these variables with outcome (recovery or negative outcome) were assessed using Chi square test or Fishers exact test in case of 2*2 tables (Tables 1, 2). T-test was used to compare mean age between men and women. We used univariate and multivariable Logistic regression to assess association between factors (diagnosis, patient sex and age, antibiotic type, days of antibiotic treatment, NH type and year of treatment) and recovery (Figure 1; Supplementary Table 1). Collinearity diagnosis shows VIF (variance inflation factor) values <1.4 except for Pneumonia 2.07 and UTI 2.16. We also classified patients according to recovery using a decision tree with CHAID (Chi-squared Automatic Interaction Detection) as a growing method (Figure 2). We performed all the statistical analysis using the IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY: IBM Corp. Two-sided p-value ≤0.05 was considered statistically significant.
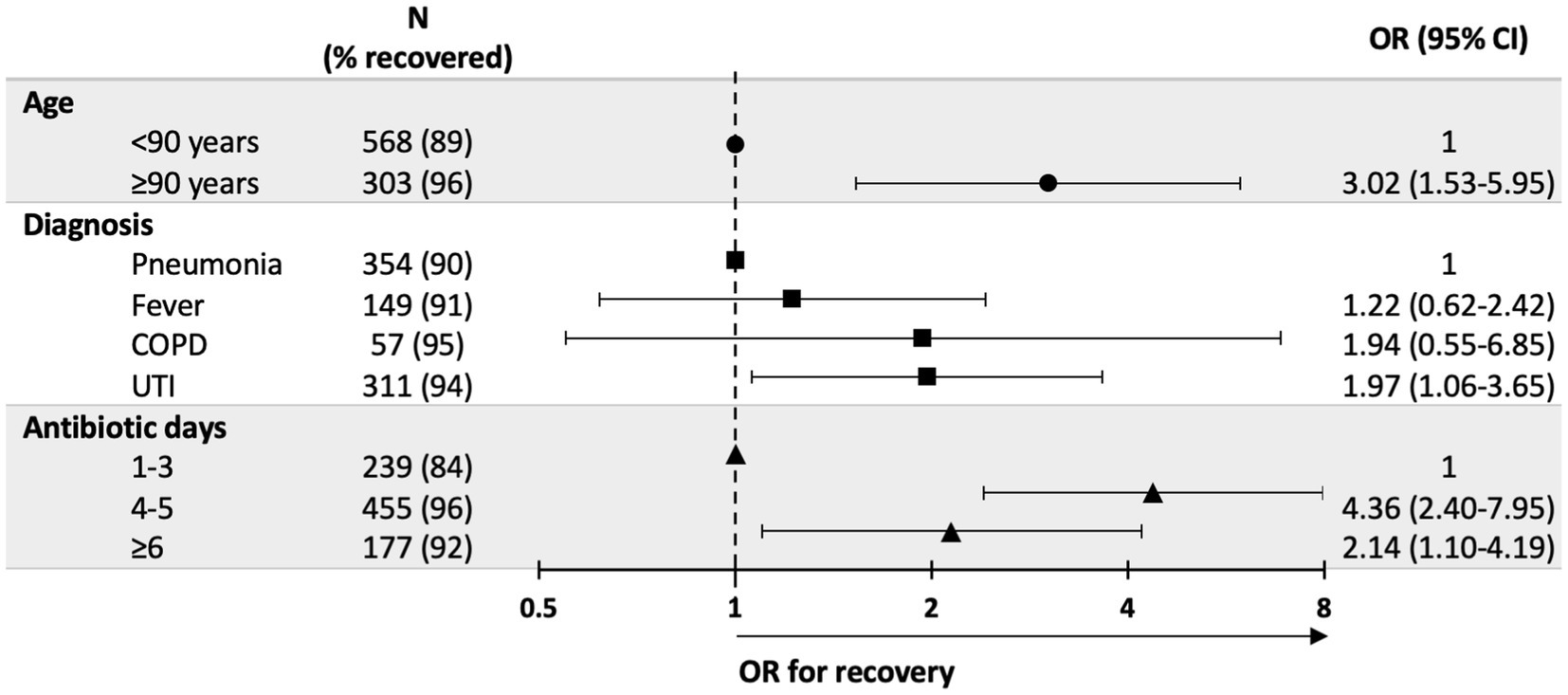
Figure 1. Factors associated with recovery–results from multivariable logistic regression*. *Variables included in the model: diagnosis, patient sex and age, antibiotic type, days of antibiotic treatment, nursing homes type and year of treatment. Variables not statistically significant were not included in figure. UTI, urinary tract infection, COPD, chronic obstructive pulmonary disease, OR, Odds Ratio.
Results
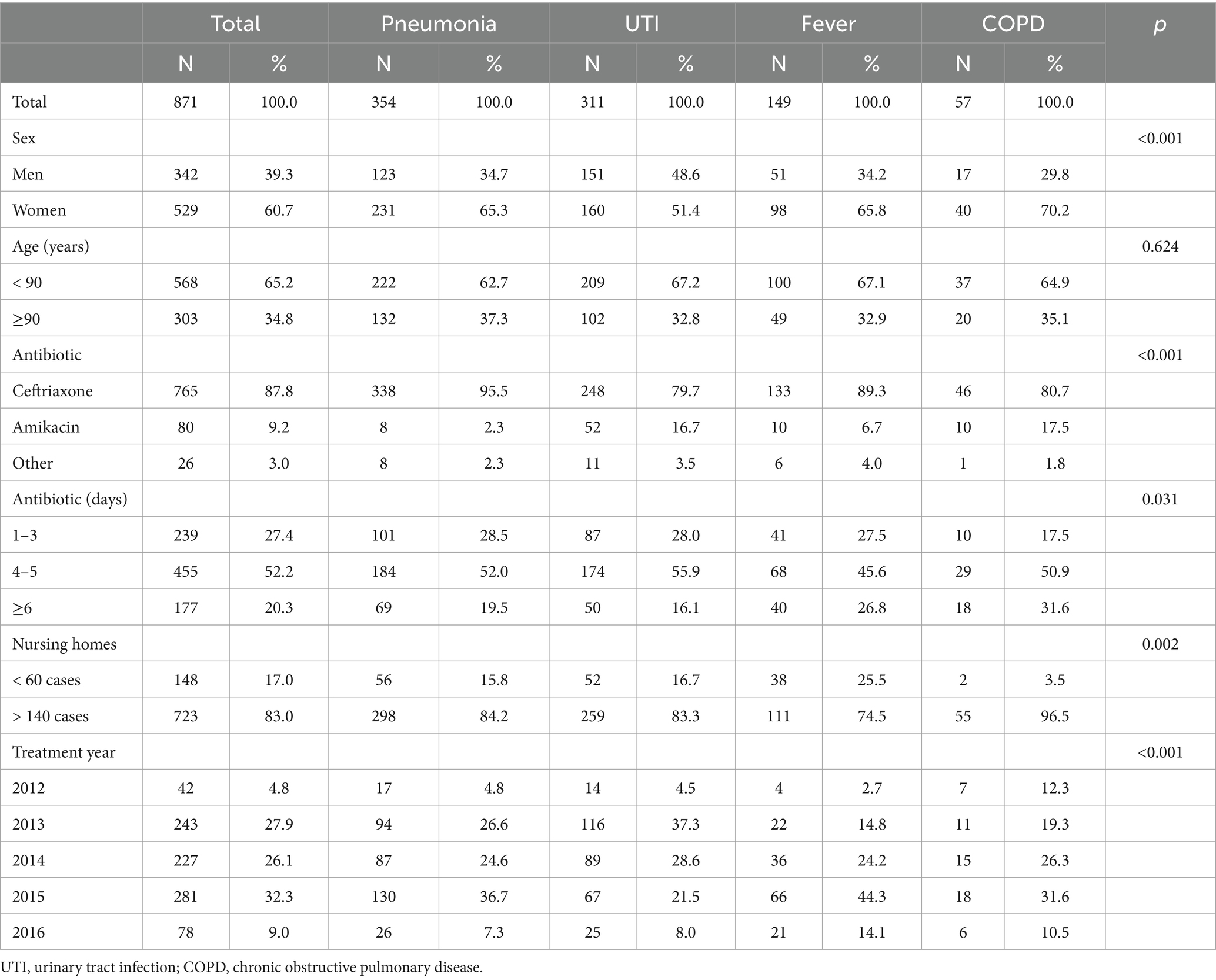
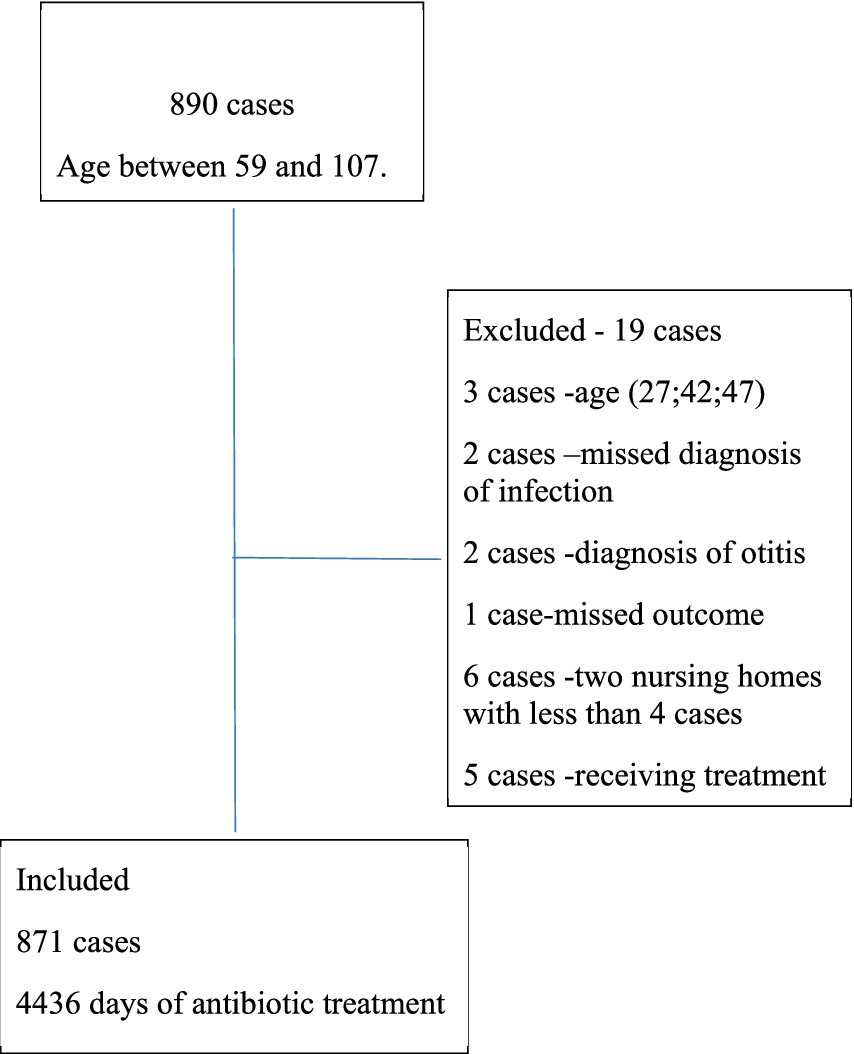
Between the 2012–2016, a total of 890 cases with acute infections received IV antibiotics treatment in 10 NH. A total of 871 cases were included in the analysis representing a total of 4,436 treatment days as specified in Figure 3. Demographic and clinical characteristics of the cases are presented in Table 1. The average age was 85.1 ± 7.0 years among men and 86.4 ± 7.8 years among women (p = 0.008), the majority (60.7%) of cases were female. Respiratory tract infections were the most common type of infection in our study, with 354 cases (40.6%) diagnosed as acute pneumonia, and 57 cases (6.5%) with Chronic Obstructive Pulmonary Disease (COPD) exacerbation. Additionally, 35.7% of the cases were diagnosed with urinary tract infections (UTI) and 17.1% were listed as fever due to suspected bacterial infection. There were significant differences between men and women in the types of infections, with a higher proportion of women suffering from respiratory tract infections (65.3% of pneumonia cases and 70.2% of COPD cases were women vs. 34.7 and 29.8%, respectively, in men, p = 4.4E-04). Significantly more cases with COPD received treatment with antibiotics for more than 6 days (p = 0.031). The majority of patients, 765 (87.8%) were treated with IV Ceftriaxone, 80 (9.2%) received aminoglycosides, and 26 cases (3%) were treated with another antibiotic’s regiments or combinations of antibiotics. There was a significant correlation between the type of infection and the antibiotic treatment. Use of aminoglycosides was more prevalent in UTI (16.7%) and COPD (17.5%) vs. pneumonia (2.3%) and fever (6.7%; p < 0.001).
Over the course of 4 years, antibiotic treatment was administered to more than 100 cases in most nursing home. Among this cases, 148 cases (17%) were from NH with fewer than 60 treated cases, while 723 cases (83%) were attributed to NH with more than 140 cases treated. The mean number of treatment days was 5.09 ± 3.86, median 5 days (IQR 3–5 days). Approximately 239 cases (27.4%) received treatment for up to 3 days, and 455 cases (52.2%) received treatment for 4 to 5 days and 177 cases (20.3%) received treatment for 6 days or more.
Over one third of the cases, totaling 303 cases (34.8%) were aged 90 years or older, while 568 cases (65.2%) were younger than 90. There was no significant difference between cases younger and older than 90 years in terms of infection type, antibiotic treatment and duration of treatment.
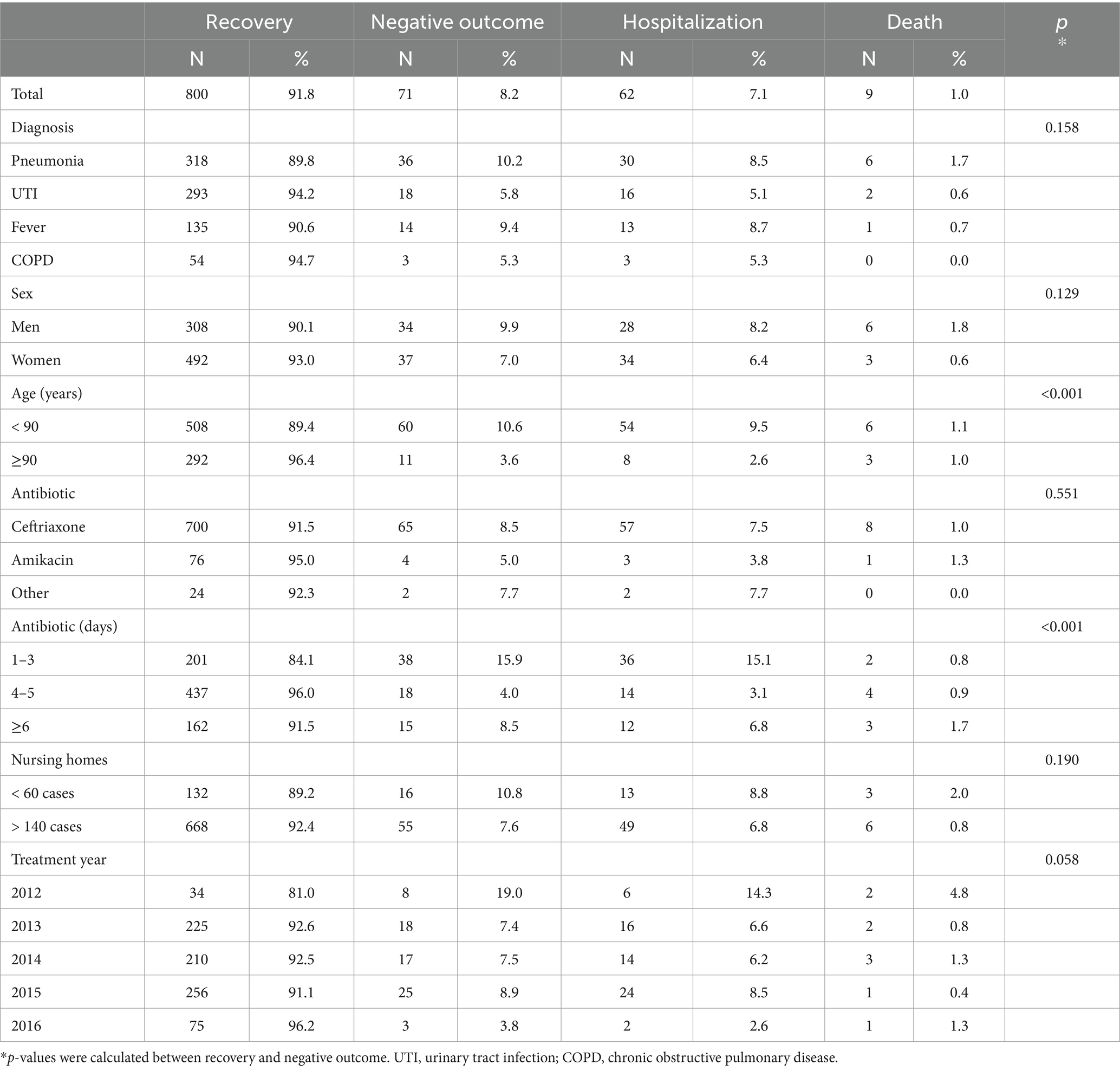
Table 2 presents the outcomes of the intervention program. Of the cases, 800 (91.8%) recovered after receiving in-house IV treatment, while 62 cases (7.1%) required hospitalization in a general care hospital and 9 cases (1.0%) resulted in mortality. There was no significant difference in recovery rates between men and women, different NH, different types of antibiotics. Recovery was seen in 94.2% of UTI cases, 94.7% of COPD cases, 89.8% of pneumonia and 90.6% in cases with fever. However, the differences in recovery rates were not statistically significant.
Cases aged 90 years and older exhibited better recovery rates compared to younger patients (OR = 3.02; 95%CI 1.53–5.95; p = 0.001). These differences were mostly driven from a lower hospitalization rate (2.6% vs. 9.5%). Days of treatment were strongly associated with recovery rate. The OR = 4.36 (95%CI 2.40–7.95) and OR = 2.14 (95%CI 1.10–4.19) respectively for 4–5 days and ≥ 6 days compared to treatment duration of 1–3 days (Figure 1; Supplementary Table 1).
Similar results were obtained from the decision tree analysis (Figure 2), which revealed a significant difference between days of treatment and clinical outcomes. In the group treated for 1–3 days, 84.1% of cases recovered, while for 4–5 days of treatment, 96.0% recovered, and in the group treated for 6 days or more, 91.5% recovered (p < 0.001). Patients who received antibiotic treatment for 4–5 days exhibited better recovery rates and lower hospitalization rates (nodes 1, 2 and 3). The rates of recovery decline mildly after 5 days of treatment, with the lowest rate observed in the group treated for up to 3 days (positive outcome for 96.0, 91.5 and 84.1% accordingly). Patients aged over 90 years old demonstrated better outcomes with a higher success rate (nodes 4 and 5).
There was no significant difference in outcomes observed among different types of infections.
Discussion
Over the course of our four-year study, focused on increasing in-house antibiotic treatment in nursing home patients. We presented a unique intervention program that effectively shifted perception of possibility for giving appropriate treatment for acute infections within NH. As a result, 10 NH adopted the practice of treating eligible patients “in-house.” Most of the patients who received in-house antibiotic treatment recovered. Only 8.2% required hospital transfer after starting IV antibiotics. The majority of the patients were successfully treated with single antibiotics and did not require combination regimens or extremely broad antibiotics, which further reinforces the view that quality treatment can be given “in-house.” We observed a learning effect, particularly in the first year where the percentage of negative outcomes was higher. Interestingly, among nursing home residents aged over 90 years old, who are considered to be predisposed to complications compared to younger old patients, the highest recovery rates were observed. This finding may be partly attributed to a reduced inclination to resort to hospitalizations for the oldest old individuals.
Our outcomes support the importance of teaching and administrative interventions to decrease hospital transfers of nursing care patients with acute infections. As opposed to most guidelines which focused on evaluating patients and determining when to refer to acute care (20, 21), our approach focused on increasing awareness and knowledge among nursing home staff and offering support for their clinical decisions.
While hospital care is crucial in certain situations, there are well-known potential risks and complications, particularly for the frail older patients with multiple comorbidities (21, 22). Longer hospital stays, cognitive decline, decubitus ulcers, falls, infections and functional decline have been described in many studies, mostly, among nursing care residents who are particularly vulnerable (23). Ahearn et al. reported a mortality rate of 33.9% among nursing home residents during hospitalization in a general hospital, with a 51.6% mortality rate among at 6 weeks following hospitalization (15).
Studies looking at the appropriateness of referrals of residents from nursing facilities to general hospitals have shown high percentages of unnecessary referrals (10, 24, 25). Saliba et al. reported that 36% of emergency room referrals and 40% of hospital referrals were inappropriate (10). Both quantitative and qualitative studies have analyzed the characteristics and associated factors of inappropriate referrals, suggesting interventions aimed at reducing potentially preventable hospitalizations (25–27). In 2001, practice guidelines were published in the US for treating fever and infections in nursing home residents. These guidelines recommend minimizing hospital referrals and specify in what situations referral to hospital can be avoided (28). One such situation is an acute infection with stable hemodynamic and respiratory measurements (29). Our study focused on increasing in-house antibiotic treatment in appropriate patients. We referenced two previous studies conducted over 15 years ago, both comparing antibiotic treatment in nursing home residents with and without hospital transfer. Dosa et al. compared nursing home residents with acute pneumonia had significantly higher mortality and functional decline compared to those treated in-house (30). Boockvar et al. in the 2005 study found significantly higher mortality and decubitus ulcers in the hospitalized patients with pneumonia compared to those treated in the nursing facility (13). The spectrum of infections in our study, primarily involving lower respiratory tract and urinary tract infections, was similar to that reported in other countries (31). Despite our patients belonging to the highest risk category as residents of NH, our outcomes were better than those of older patients admitted to hospitals with pneumonia (32) and mortality rate was lower (1%) than those reported in the literature for NH residents (33).
In our study, there was a significant cohort of nursing home residents aged over 90. Previous studies have often indicated higher mortality rates among of patients older than 85, with studies like Lee et al. (34) demonstrating that octogenarians had the highest mortality rates, and Garibaldi et all (35) suggesting that older adult patients are predisposed to serious infections due to underlying chronic or acute illness. As opposite to these findings, our study revealed that the group of patients older than 90 exhibited the highest recovery rates. This finding carries potential clinical implications and may impact decisions regarding hospitalization indications for octogenarians.
Our study has several limitations. We focused on outcomes post- intervention in 10 NH lacking pre-intervention data for comparison. Advanced health care directives and patient preferences were not assessed and may theoretically influence hospitalization rate. Giving the high recovery rate, there is a low probability for significant selection bias. We also did not include a comparison with NH that did not receive an intervention, limiting our ability to gage the intervention’s effectiveness comprehensively. We did not obtain bacterial culture as part of the protocol, potentially impacting the quality of care, mainly for UTIs. However, we believed making cultures mandatory may have lowered compliance from the stuff. Primary diagnosis and treatment are based on clinical evaluation, given the common occurrence of asymptomatic bacteriuria in NH (36). We looked at the three parts of the intervention as a whole, and therefore, cannot say which part was the most effective—the educational aspect, the clinical support, or the logistic intervention. Moreover, while we did not assess costs or cost-effectiveness, our interventions used resources within the HMO, and therefore were low cost. Nonetheless, they effectively prevented costly outcomes such as hospitalizations and deaths (37, 38), highlighting their value both economically and in terms of human life.
Conclusion
Our study provides an example of an effective intervention for improving outcomes of acute infections in nursing home residents. By focusing on increasing awareness and knowledge among nursing home staff, and facilitating the logistics of in-house IV antibiotic treatment, it is possible to improve compliance, achieved high recovery rates and minimized hospitalizations, thus improving quality of care in NH residents.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: data set is from classified EMR not open to the public. Requests to access these datasets should be directed to YmF0aWFfbmFkeWEua2FnYW5za3lAbW9oLmdvdi5pbA==.
Ethics statement
The studies involving humans were approved by the Kupat Cholim Clalit Central ethics committee and conforms to the principles outlined in the Declaration of Helsinki (IRB 0234-16-COM2). Due to the study’s retrospective nature, informed consent was wavered by the ethics committee. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
NK: Conceptualization, Supervision, Data curation, Investigation, Methodology, Writing – original draft. RR: Data curation, Investigation, Resources, Writing – review & editing. ED: Writing – review & editing, Formal analysis, Methodology, Visualization. EM: Writing – review & editing, Investigation, Validation. YL: Writing – review & editing, Conceptualization, Project administration, Supervision, Visualization. MB: Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2024.1333523/full#supplementary-material
References
1. Fry, AM, Shay, DK, Holman, RC, Curns, AT, and Anderson, LJ. Trends in hospitalizations for pneumonia among persons aged 65 years or older in the United States, 1988-2002. JAMA. (2005) 7:2712–9. doi: 10.1001/jama.294.21.2712
2. Kruger, K, Jansen, K, Grimsmo, A, Eide, GE, and Geitung, GT. Hospital admissions from nursing homes: rates and reasons. Nurs Res Pract. (2011) 2011:1–6. doi: 10.1155/2011/247623
3. Cheng, VC, Tai, JW, Wong, ZS, Chen, JHK, Pan, KBQ, Hai, Y, et al. Transmission of methicillin-resistant staphylococcus aureus in the long term care facilities in Hong Kong. BMC Infect Dis. (2013) 13:205–15. doi: 10.1186/1471-2334-13-205
4. Strausbaugh, LJ, Sukumar, SR, and Joseph, CL. Infectious disease outbreaks in nursing homes: an unappreciated Hazard for frail elderly persons. CID. (2003) 36:870–6. doi: 10.1086/368197
5. Hullick, C, Conway, J, Higgins, I, Hewitt, J, Dilworth, S, Holliday, E, et al. Emergency department transfers and hospital admissions from residential aged care facilities: a controlled pre-post design study. BMC Geriatr. (2016) 16:102–12. doi: 10.1186/s12877-016-0279-1
6. Marengoni, A, Rizzuto, D, Wang, HX, Winblad, B, and Fratiglioni, L. Patterns of chronic multimorbidity in the elderly population. JAGS. (2009) 57:225–30. doi: 10.1111/j.1532-5415.2008.02109.x
7. American Geriatrics Society Expert Panel on the Care of Older Adultswith Multimorbidity. Guiding principles for the Care of Older Adults with multimorbidity: an approach for clinicians. J Am Geriatr Soc. (2012) 60:E1–E25. doi: 10.1111/j.1532-5415.2012.04188.x
8. Thigpen, MC, Richards, CL, Lynfield, R, Barrett, NL, Harrison, LH, Arnold, KE, et al. Invasive group a streptococcal infection in older adults in long term care facilities and the community, United States, 1998-2003. Emerg Infect Dis. (2007) 13:1852–9. doi: 10.3201/eid1312.070303
9. Mody, L, Bradley, SF, Galecki, A, Olmsted, RN, Fitzgerald, JT, Kauffman, CA, et al. Conceptual model for reducing infections and antimicrobial resistance in skilled nursing facilities: focusing on residents with indwelling devices. Clin Infect Dis. (2011) 52:654–61. doi: 10.1093/cid/ciq205
10. Saliba, D, Kington, R, Buchanan, J, Bell, R, Wang, M, Lee, M, et al. Appropriateness of the decision to transfer nursing facility residents to the hospital. JAGS. (2000) 48:154–63. doi: 10.1111/j.1532-5415.2000.tb03906.x
11. Intrator, O, Grabowski, DC, Zinn, J, Schleinitz, M, Feng, Z, Miller, S, et al. Hospitalization of nursing home residents: the effects of states’ Medicaid payment and bed-hold policies. HSR. (2007) 42:1651–71. doi: 10.1111/j.1475-6773.2006.00670.x
12. Fried, TR, Gillick, MR, and Lipsitz, LA. Short –term functional outcomes of long-term care residents with pneumonia treated with and without hospital transfer. J Amer Geriat Soc. (1997) 45:302–6. doi: 10.1111/j.1532-5415.1997.tb00944.x
13. Boockvar, KS, Gruber-Baldini, AL, Burton, L, Zimmerman, S, May, C, and Magaziner, J. Outcomes of infection in nursing home residents with and without early hospital transfer. J Amer Geriat Soc. (2005) 53:590–6. doi: 10.1111/j.1532-5415.2005.53205.x
14. Mudge, AM, McRae, P, Hubbard, RE, Peel, NM, Lim, WK, Barnett, AG, et al. Hospital-associated complications of older people: a proposed multicomponent outcome for acute care. J Amer Geriat Soc. (2019) 67:352–6. doi: 10.1111/jgs.15662
15. Ahearn, D, Jackson, T, Mcllmoyle, J, and Weatherburn, A. Improving and of life care for nursing home residents an analysis of hospital mortality and readmission rates. Postgrad Med J. (2010) 86:131–5. doi: 10.1136/pgmj.2008.076430
17. Villas Bôas, PJ, and Ferreira, AL. Infection in elderly interned in long-term care facilities. Rev Assoc Med Bras. (2007) 53:126–9. doi: 10.1590/S0104-42302007000200016
18. Hammond, CL, Pinnington, LL, and Phillips, MF. A qualitative examination of inappropriate hospital admissions and lengths of stay. BMC Health Serv Res. (2009) 9:44–53. doi: 10.1186/1472-6963-9-44
19. Daras, LC, Wang, JM, Ingber, MJ, Ormond, C, Breg, NW, Khatutsky, G, et al. What are nursing facilities doing to reduce potentially avoidable hospitalizations? JAMDA. (2017) 18:442–4. doi: 10.1016/j.jamda.2017.02.007
20. Bentley, DW, Bradley, S, High, K, Schoenbaum, S, Taler, G, and Yoshikawa, TT. Practice guideline for evaluation of fever and infection in long –term care facilities. JAGS. (2001) 49:210–22. doi: 10.1046/j.1532-5415.2001.49999.x
21. Naughton, BJ, and Mylotte, JM. Treatment guideline for nursing home‐acquired pneumonia based on community practice. J Amer Geriat Soc. (2000) 48:82–8. doi: 10.1111/j.1532-5415.2000.tb03034.x
22. Creditor, MC. Hazards of hospitalization of the elderly. Ann Intern Med. (1993) 118:219–23. doi: 10.7326/0003-4819-118-3-199302010-00011
23. Polverino, E, Dambrava, P, Cilloniz, C, Balasso, V, Marcos, MA, Esquinas, C, et al. Nursing home acquired pneumonia: a10 year single-Centre experience. Thorax. (2010) 65:354–9. doi: 10.1136/thx.2009.124776
24. Godden, S, and Pollock, AM. The use of acute hospital services by elderly residents of nursing and residential care homes. Health Soc Care in the Community. (2001) 9:367–74. doi: 10.1046/j.1365-2524.2001.00314.x
25. Bowmana, CE, Elforda, J, Doveya, J, Campbella, S, and Barrowcloughb, H. Acute hospital admissions from nursing homes: some may be avoidable. Postgrad Med. (2001) 77:40–2. doi: 10.1136/pmj.77.903.40
26. McDermott, C, Coppin, R, Little, P, and Leydon, G. Hospital admissions from nursing homes: a qualitative study of GP decision making. Br J Gen Pract. (2012) 62:e538–45. doi: 10.3399/bjgp12X653589
27. Pulia, M, Kern, M, Schwei, RJ, Shah, MN, Sampene, E, and Crnich, CJ. Comparing appropriateness of antibiotics for nursing home residents by setting of prescription initiation: a cross-sectional analysis. Antimicrob Resist Infect Control. (2018) 7:74–82. doi: 10.1186/s13756-018-0364-7
28. Ingold, BB, Yersin, B, Wietlisbach, V, Burckhardt, P, Burnand, B, and Bula, CJ. Characteristics associated with inappropriate hospital use in elderly patients admitted to a general internal medicine service. Aging Clin Exp Res. (2000) 12:430–8. doi: 10.1007/BF03339873
29. Sloane, PD, Huslage, K, Kistler, C, and Zimmerman, C. Optimizing antibiotic use in nursing homes through antibiotic stewardship. N C Med J. (2016) 77:324–9. doi: 10.18043/ncm.77.5.324
30. Dosa, D. Should I hospitalize my resident with nursing home-acquired pneumonia? JAMDA. (2006) 7:s74–80. doi: 10.1016/j.jamda.2005.12.019
31. Kane, RL, Huckfeldt, P, and Tappen, R. Effects of an intervention to reduce hospitalizations from nursing homes a randomized implementation trial of the INTERACT program. JAMA. (2017) 177:1257–64. doi: 10.1001/jamainternmed.2017.2657
32. Healthcare Cost and Utilization Project (HCUP). HCUP facts and figures: Statistics on hospital –based care in the United States. Rockville (MD): Agency for Healthcare Research and Quality (US); 2010 (2008).
33. Greenberg, SA, Halpern, P, Ziv-Baran, T, and Gamzu, R. Reduced hospitalization rates are not associated with increased mortality or readmission rates in an emergency department in Israel. Isr J Health Policy Res. (2018) 7:69–76. doi: 10.1186/s13584-018-0265-5
34. Lee, CC, Liu, Y, Lu, KT, Wei, C, Su, K, Hsu, WT, et al. Comparison of influenza hospitalization outcomes among adults, older adults, and octogenarians: a US national population-based study. Clin Microbiol Infect. (2021) 27:435–42. doi: 10.1016/j.cmi.2020.04.013
35. Garibaldi, RA, and Nurse, BA. Infections in the elderly. Am J Med. (1986) 81:53–8. doi: 10.1016/0002-9343(86)90514-0
36. Leihof, RF, Nielsen, KL, and Frimodt-Møller, N. Asymptomatic bacteriuria (ABU) in elderly: prevalence, virulence, phylogeny, antibiotic resistance and complement C3 in urine. Microorganisms. (2021) 9:390. doi: 10.3390/microorganisms9020390
37. Schrøder, CK, Kristiansen, EB, Flarup, L, Christiansen, CF, Thomsen, RW, and Kristensen, PK. Preadmission morbidity and healthcare utilization among older adults with potentially avoidable hospitalizations: a Danish case-control study. Eur Geriatr Med. (2024) 15:127–38. doi: 10.1007/s41999-023-00887-7
Keywords: acute infections, hospitalization, nursing homes, intravenous, training program
Citation: Kagansky N, Rosenberg R, Derazne E, Mazurez E, Levy Y and Barchana M (2024) Implementation of a program for treatment of acute infections in nursing homes without hospital transfer. Front. Med. 11:1333523. doi: 10.3389/fmed.2024.1333523
Edited by:
Tzvi Dwolatzky, Technion Israel Institute of Technology, IsraelCopyright © 2024 Kagansky, Rosenberg, Derazne, Mazurez, Levy and Barchana. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yochai Levy, eW9jaGF5bGV2aUBtYWlsLnRhdS5hYy5pbA==
†These authors have contributed equally to this work
‡ORCID: Yochai Levy, http://orcid.org/0000-0003-0066-2736
 Nadya Kagansky1,2
Nadya Kagansky1,2 Yochai Levy
Yochai Levy Micha Barchana
Micha Barchana