
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med. , 19 February 2024
Sec. Geriatric Medicine
Volume 11 - 2024 | https://doi.org/10.3389/fmed.2024.1331246
 Atakan Topcu1*
Atakan Topcu1* Ayse Irem Yasin1
Ayse Irem Yasin1 Mehmet Besiroglu2
Mehmet Besiroglu2 Zehra Sucuoglu Isleyen1
Zehra Sucuoglu Isleyen1 Zeynep Alaca Topcu2
Zeynep Alaca Topcu2 Melih Simsek1
Melih Simsek1 Haci Mehmet Turk1
Haci Mehmet Turk1 Mesut Seker1
Mesut Seker1 Pinar Soysal1
Pinar Soysal1Background: Geriatric syndromes may be more common in older cancer patients than in those without cancer. Geriatric syndromes can cause poor clinical outcomes. The Eastern Cooperative Oncology Group Performance Status (ECOG-PS) is often used as a clinically reported functional status score in oncology practice.
Methods: Our study was designed as a cross-sectional study and included 218 older cancer patients. This study aimed to determine the prevalence and relationship of geriatric syndromes according to the ECOG-PS in older cancer patients.
Results: The mean age of 218 participants was 73.0 ± 5.6 years, with 47.7% being women and 52.3% men in our study. ECOG-PS 0, 1, and 2 groups contained 51, 39, and 10% of the patients, respectively. The mean number of geriatric syndromes in the ECOG 0, 1, and 2 groups was 2.3 ± 2.2, 4.3 ± 2.4, and 5.7 ± 2.1, respectively (p < 0.001). After adjusting for age and sex, it was determined that dynapenia was 2.9 times, probable sarcopenia was 3.5 times, frailty was 4.2 times, depression was 2.6 times, malnutrition was 3.3 times, insomnia 2 was.2 times, falls was 2.5 times, and the risk of falling (TUG) was 2.4 times more likely in those with ECOG-PS 1 compared to those with ECOG-PS 0. In addition, it was found that dynapenia was 6 times, probable sarcopenia was 6.8 times, frailty was 10.8 times, depression was 3.3 times, malnutrition was 6.3 times, the risk of falling (Tinnetti Balance) was 28 times, and the risk of falling (TUG) was 13.6 times more likely in those with ECOG-PS 2 compared to those with ECOG-PS 0.
Conclusion: Our study found that the prevalence of geriatric syndromes increased as the ECOG-PS increased. Geriatric syndromes and their co-incidence were common in older cancer patients, even in normal performance status. Oncologists should incorporate geriatric syndromes into the decision-making process of cancer treatment to maximize the impact on clinical outcomes in older patients with cancer.
Cancer is detected more often with aging, as age represents the most potent non-modifiable risk factor for developing cancer (1). Aging is a biological process associated with a decrease in the capacity of all organ functions, and this causes individuals to be more vulnerable (2). While older cancer patients struggle with the problems caused by cancer and its treatments, they also have to fight the natural burden of aging. In clinical practice, oncologists frequently use the Eastern Cooperative Oncology Group Performance Status (ECOG-PS), which describes the patient’s baseline functional and frailty status. However, ECOG-PS may have a poor correlation with comprehensive geriatric assessment (CGA), and its usefulness in older adults with cancer is often questioned (3, 4). Although ECOG-PS is widely used by oncologists for frailty assessment, it is known that frailty is not the only issue, and geriatric syndromes can impair the quality of life and decrease the overall survival of cancer patients (5).
Assessment of older cancer patients can be more difficult for clinicians because age and tumor characteristics alone may not capture this patient group’s functional and frailty status (6, 7). Functional status can vary significantly among older cancer patients of similar chronological age. Therefore, it has been shown that CGA can add fundamental aid for the evaluation of functional assessment and treatment planning of older cancer patients, including those with a good PS (4, 8, 9).
Geriatric syndromes can be more common in older cancer patients than in those without cancer. For example, malnutrition may be common in older cancer patients because of nausea and vomiting that may develop due to chemotherapy (10). In addition, drugs that can be used to control symptoms and side effects such as nausea, fatigue, and pain may increase the frequency of polypharmacy (11). While geriatric syndromes are multifactorial, the presence of cancer also contributes to the development of these syndromes (2, 12). These syndromes can cause poor clinical outcomes, including increased morbidity and mortality. Therefore, identifying patients with geriatric syndromes is crucial in providing personalized care for older cancer patients (2, 5, 13, 14).
Geriatric syndromes such as malnutrition, frailty, fear of falling, falls, depression, insomnia, excessive daytime sleepiness, dynapenia, and sarcopenia are common in older patients. Although each geriatric syndrome has been evaluated separately in older cancer patients, there are a few studies examining all geriatric syndromes together and categorizing them based on their performance status (15, 16). Additionally, our real-life research also involves various geriatric syndromes, such as urinary incontinence, excessive daytime sleepiness, insomnia, dynapenia, and probable sarcopenia. This study aimed to determine the prevalence and relationship of geriatric syndromes according to the ECOG performance status in older cancer patients and to increase awareness of this issue.
Cancer patients of age ≥ 65 years were recruited from an ongoing longitudinal cohort treated at the University of Bezmialem Vakif University Oncology outpatient clinic from October 2020 to October 2022. Our study included 218 older cancer patients. The patients with Eastern Cooperative Oncology Group Performance Status ≥3, those under the age of 65 years, those with dementia or delirium, those with vision and hearing impairments that control understanding commands during the evaluation, and those with uncontrolled comorbid disorders were excluded. The study was designed as a cross-sectional study and was approved by the local ethics committee. Each participant provided informed consent before participating in the study.
The cancer types of the participants were categorized into five subgroups: lung, breast, gastrointestinal system, urogenital system, and others. The current stages of the patients were divided into four subgroups, as stage 1, 2, 3, and 4, and they were also evaluated as metastatic and non-metastatic diseases. In addition, we noted whether the patients received active chemotherapy for their disease.
The ECOG-PS is the most generally used clinically reported functional status score in oncology practice (17). Clinicians prefer one statement suitably defining the patient’s level of physical activity (ranging from 0 to 4). The scores were defined as 0 being fully active, 1 being restricted in strenuous activity, and 2 indicating being capable of all self-care but an inability to carry out any work activities, up and about more than 50% of waking hours. Scores of 3 and above indicate severe disability. Patients with ECOG-PS ≥3 have a poor prognosis and were excluded from our study.
Sex, age, BMI, mean upper arm and calf circumference, smoking, number of drugs, cancer type and stage, chemotherapy status, cancer treatment history, history of falling, comorbidities including diabetes mellitus, hyperlipidemia, hypertension, coronary artery disease, cerebrovascular events, chronic obstructive pulmonary disease, and Parkinson’s disease were recorded. The following geriatric syndromes were assessed in interviews with the patient and the caregiver. The evaluation of each geriatric syndrome mentioned below has been detailed in our previous studies (13).
Dynapenia: Dominant hand grip strength measured by a handgrip dynamometer less than 16 kg in women and less than 27 kg in men was defined as dynapenia (18).
Probable sarcopenia: If SARC-F ≥ 4 + dynapenia was low according to the defined cutoff (19).
Frailty: A modified Fried physical frailty scale was used to evaluate frailty, which was defined according to the physical model and the presence of three or more of the following criteria: weight loss, exhaustion, low physical activity, slowness, and weakness. Those with 0 were considered normal, while those with 1–2 criteria were considered pre-frailty and those with ≥3 were considered frailty (13).
Depression: Yesavage Geriatric Depression Scale-15 (GDS-15) score ≥ 5 (20).
Malnutrition: MNA long form scores <17 points were considered as having malnutrition. It was specified as 17–23.5 for at-risk malnutrition and ≥ 24 for normal nutritional status (20).
Insomnia: Insomnia Severity Index score ≥ 8 (20).
Excessive daytime sleepiness: Epworth Sleepiness Scale score ≥ 11 (20).
Polypharmacy: The concurrent use of five or more drugs (20).
Appetite assessment: <28 was defined as losing appetite according to the Council on Nutrition Appetite Questionnaire (CNAQ) (21).
Falls: The patient’s fall was considered positive, except for slipping on the wet floor in the previous year (13).
Risk of falling: A value of <19 was accepted according to the Tinetti Balance and Gait Test and ≥ 13.5 s according to the timed up and go (TUG) test (22, 23).
Quantitative variables are defined as mean ± standard deviation, and qualitative variables are given as numbers and proportions. A chi-squared test was utilized for comparing qualitative measures between groups. Comparisons of continuous variables between the groups were achieved using the Kruskal–Wallis test. Significant differences were compared by the Bonferroni-corrected Mann–Whitney test. Factors associated with each geriatric syndrome were assessed using univariate logistic regression analysis. The model, therefore, was adjusted for age and sex. Results are described as odds ratio (OR) with a 95% confidence interval. IBM SPSS Statistics for Windows, Version 28.0. (Armonk, NY: IBM Corp.) was used for analysis. The level of significance was determined at a p-value of <0.05.
The mean age of 218 participants was 73.0 ± 5.6 years, with 104 (47.7%) women and 114 (52.3%) men in our study. The ECOG-PS 0, 1, and 2 groups contained 51, 39, and 10% of the patients, respectively. The mean age of the patients (p < 0.001) and the prevalence of the metastatic stage (p < 0.001) increased as the ECOG-PS score increased. Gastrointestinal cancers (39.9%) were the most common cancers in our study. The mean number of geriatric syndromes in the ECOG 0, 1, and 2 groups was 2.3 ± 2.2, 4.3 ± 2.4, and 5.7 ± 2.1, respectively (p < 0.001). The prevalence of geriatric syndromes increased as the ECOG-PS score increased. The prevalence of frailty, malnutrition, EDS, depression, dynapenia, and probable sarcopenia increased as the ECOG-PS score increased in our study. While the mean of the handgrip, MNA, and CNAQ of the patients decreased as the ECOG-PS score increased, the mean of the falls, risk of falling (TUG and Tinetti Balance), GDS, SARC-F, ISI, and Epworth scores increased. However, upper arm circumference, calf circumference, urinary incontinence, and loss of appetite were not different in the ECOG-PS groups. The characteristics of the patients and all geriatric syndrome comparisons based on the ECOG-PS category are shown in Table 1. The frequency of the geriatric syndromes increased in higher ECOG-PS groups (Figure 1). Among the geriatric syndromes, insomnia had the highest incidence in the ECOG-PS 0 group (39%), while frailty had the highest incidence in the ECOG-PS 1 group (71%), and the ECOG-PS 2 group (86%). The total number of geriatric syndromes based on the ECOG-PS groups is shown in Figure 2. In the ECOG-PS 0 group, 21% of the had 0 geriatric syndrome, 29% of the patients had 1 geriatric syndrome, 12% of the patients had 2 geriatric syndromes, and 38% of the patients had 3 or more geriatric syndromes. In addition, 5% of the patients had 0 geriatric syndrome, 11% of the patients had 1 geriatric syndrome, 13% of the patients had 2 geriatric syndromes, and 71% of the patients had 3 or more geriatric syndromes in the ECOG-PS 1 group. However, there was no patient without a geriatric syndrome in the ECOG-PS 2 group. Furthermore, 5% of the patients had one geriatric syndrome, another 5% of the patients had two geriatric syndromes, and 90% of the patients had three or more geriatric syndromes. Among the patients with an ECOG-PS of 0 or 1, we analyzed the OR of an ECOG-PS of 1 versus an ECOG-PS of 0 for each geriatric syndrome (Table 2). In addition, we also analyzed the OR of ECOG-PS 2 vs. ECOG-PS 0 for each geriatric syndrome (Table 3). After adjusting for age and sex, the ORs were significantly higher in the ECOC-PS 1 group compared to the ECOC-PS 0 group, as follows: dynapenia OR: 2.9, probable sarcopenia OR: 3.54, frailty OR: 4.2, depression OR: 2.68, malnutrition OR: 3.38, insomnia OR: 2.21, falls OR: 2.52, and risk of falling (TUG) OR: 2.41. There was no difference in terms of polypharmacy, urinary incontinence, excessive daytime sleepiness, and risk of falling (Tinetti Balance) in the ECOG-PS 0 and 1 groups. Moreover, the OR rates were significantly determined in the ECOC-PS 2 group compared to the ECOC-PS 0 group as follows: dynapenia OR: 6.03, probable sarcopenia OR: 6.85, frailty OR: 10.86, depression OR: 3.34, malnutrition OR: 6.32, risk of falling (Tinnetti Balance) OR: 28.01 times, and risk of falling (TUG) OR: 13.66. There was no difference in terms of insomnia, polypharmacy, urinary incontinence, excessive daytime sleepiness, and falls in the ECOG-PS 0 and 2 groups. We also conducted an analysis adjusted for age, sex, polypharmacy, and comorbidity, both for the group with ECOG-PS 1 vs. ECOG-PS 0 (Table 4) and for the group with ECOG-PS 2 vs. ECOG-PS 0 (Table 5).
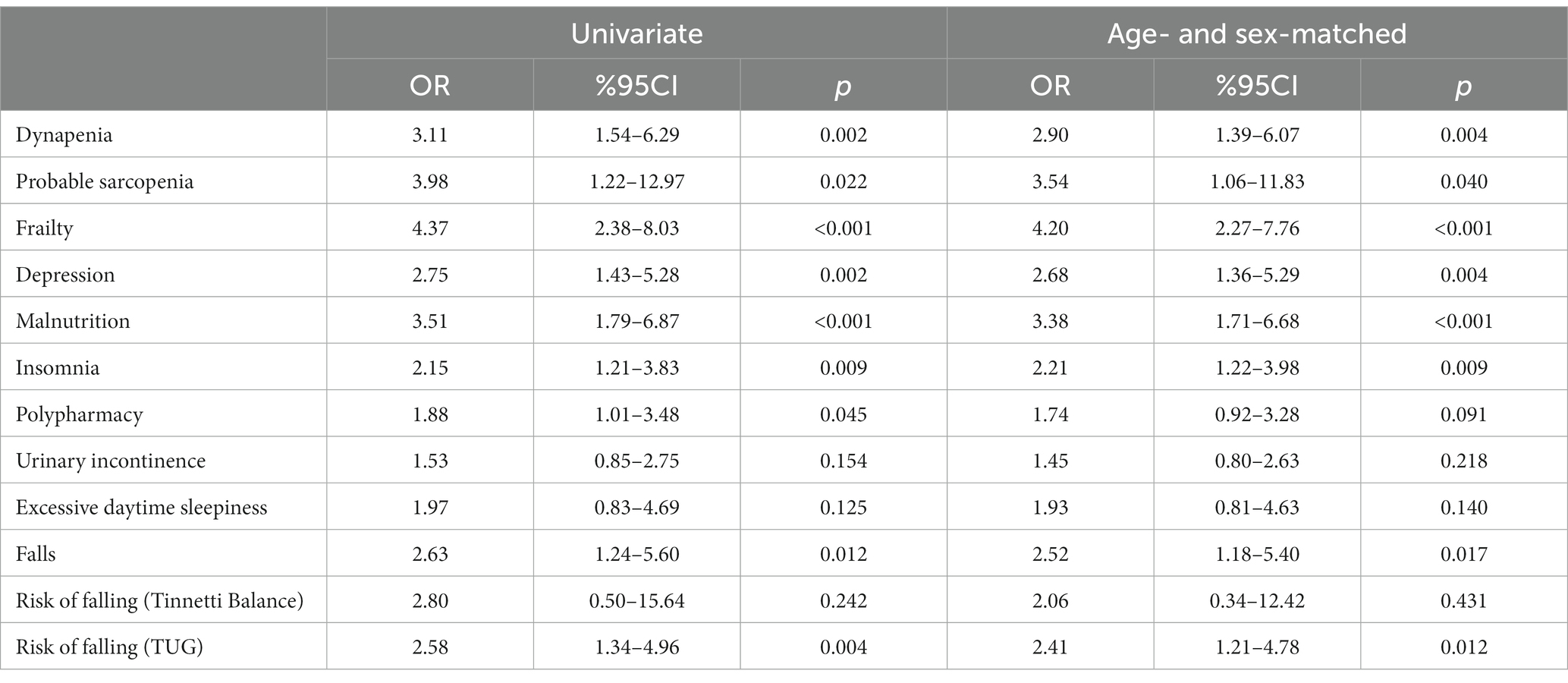
Table 2. Among patients with ECOG-PS 0 or 1, odds ratio of ECOG-PS 1 vs. ECOG-PS 0 for each geriatric syndrome.
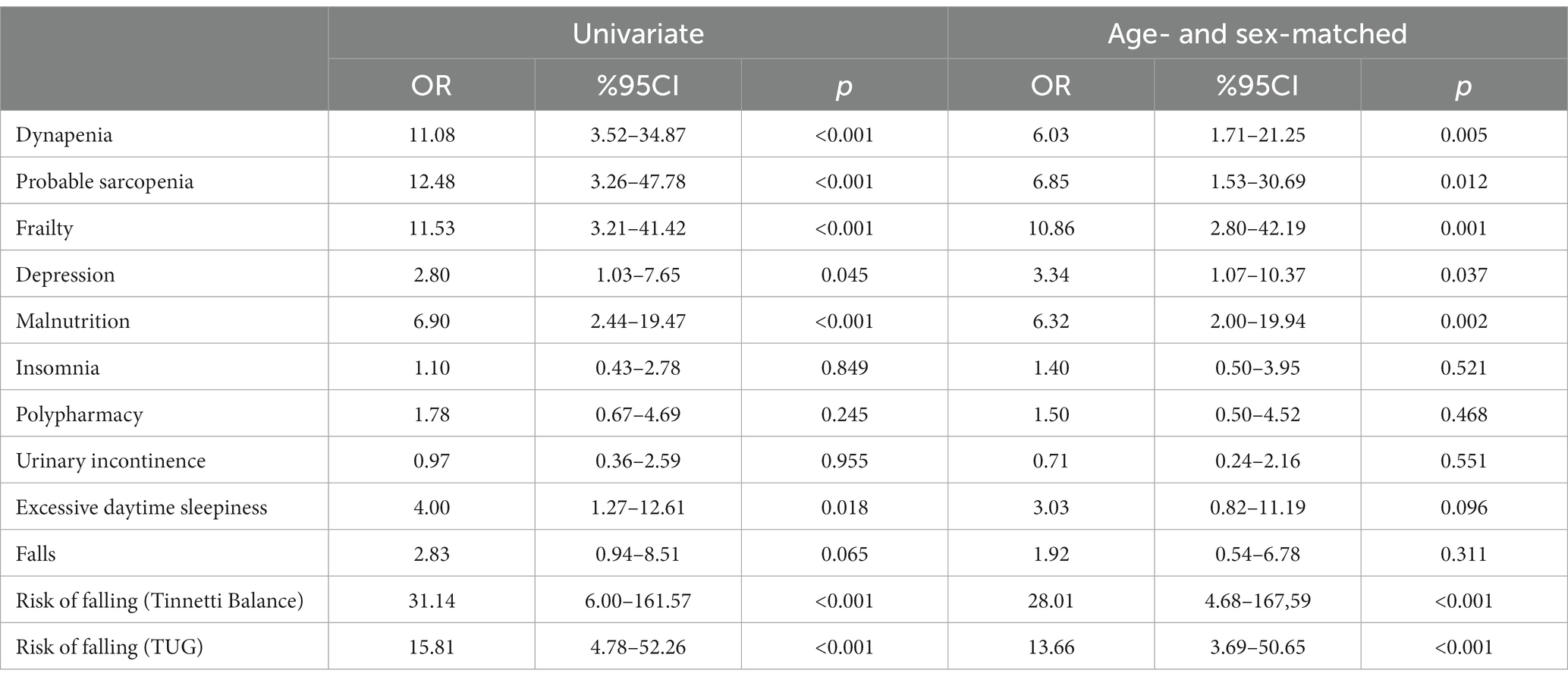
Table 3. Among patients with ECOG-PS 0 or 2, odds ratio of ECOG-PS 2 vs. ECOG-PS 0 for each geriatric syndrome.
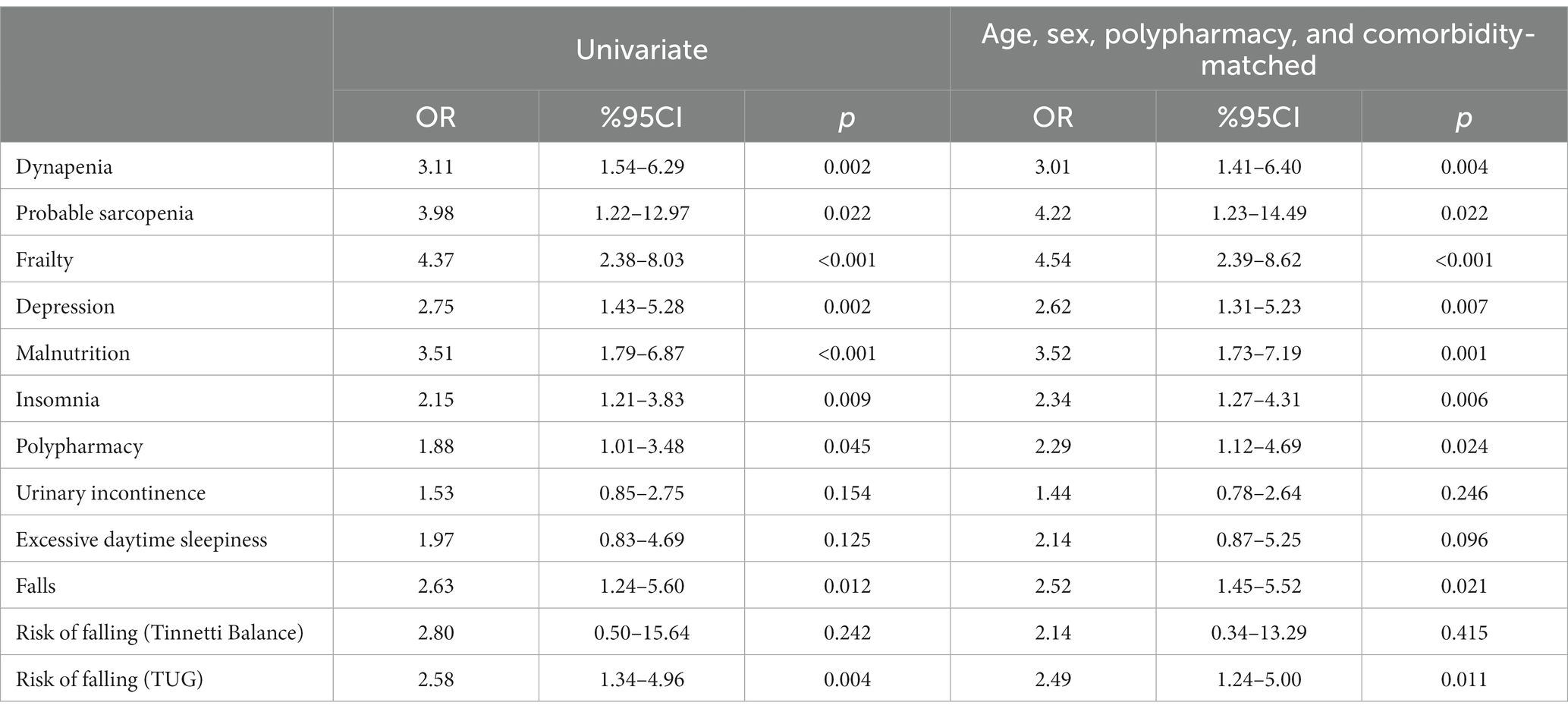
Table 4. Among patients with ECOG-PS 0 or 1, the odds ratio of ECOG-PS 1 vs. ECOG-PS 0 for each geriatric syndrome (age, sex, polypharmacy, and comorbidity-matched).
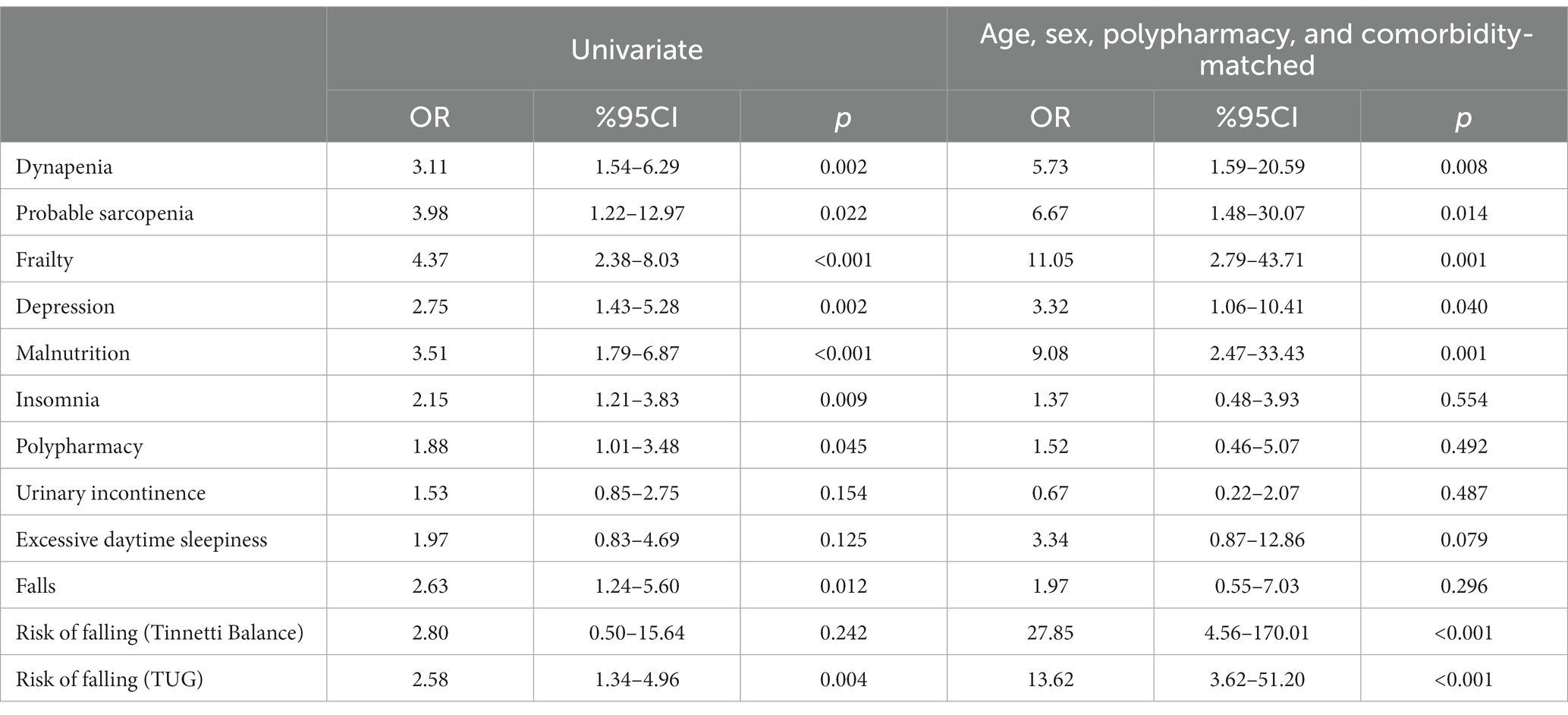
Table 5. Among patients with ECOG-PS 0 or 2, the odds ratio of ECOG-PS 2 vs. ECOG-PS 0 for each geriatric syndrome (age, sex, polypharmacy, and, comorbidity-matched).
In our study, the frequency of geriatric syndromes increased as ECOG-PS increased. Frailty was the most common geriatric syndrome in both the ECOG-PS 1 and ECOG-PS 2 groups. Moreover, in the ECOG-PS 0 group, it was the second most common geriatric syndrome after insomnia. Most patients had three or more geriatric syndromes in the ECOG-PS 1 and ECOG-PS 2 groups. In addition, in the ECOG-PS 2 group, all patients had at least one geriatric syndrome. The mean age of the patients and the prevalence of the metastatic stage increased as the ECOG-PS score increased. After adjusting for age and sex, it was determined that dynapenia was 2.9 times, probable sarcopenia was 3.5 times, frailty was 4.2 times, depression was 2.6 times, malnutrition was 3.3 times, insomnia was 2.2 times, falls was 2.5 times, and the risk of falling (TUG) was 2.4 times more likely in those with ECOG-PS 1 compared to those with ECOG-PS 0. Frailty had the highest OR. In addition, it was found that dynapenia was 6 times, probable sarcopenia was 6.8 times, frailty was 10.8 times, depression was 3.3 times, malnutrition was 6.3 times, and the risk of falling (Tinnetti Balance) was 28 times, and the risk of falling (TUG) was 13.6 times more likely in those with ECOG-PS 2 compared to those with ECOG-PS 0. The risk of falling (Tinnetti Balance) had reached the highest OR. In addition, there was no difference in the ORs between both groups (ECOG-PS 1 vs. 0 and ECOG-PS 2 vs. 0) concerning polypharmacy, urinary incontinence, and excessive daytime sleepiness in our study.
The ECOG-PS provides limited information about the patient and may be insufficient for the treatment of older cancer patients (24). An important review determined that CGA could play an effect modifier role for the results of oncological treatment and could give substantial information in addition to chronological age and performance score (25). Recent studies have underlined the importance of CGA in older cancer patients to improve treatment planning (12, 26). In a geriatric study involving multiple myeloma patients, they found that at least two geriatric assessment-identified deficits were observed in 41% of those with a normal performance score with Karnofsky Performance Status (KPS), which is another validated score for functional evaluation in cancer patients (27). In a study that included older cancer patients with normal performance status, they found at least one geriatric syndrome in 69% of the patients. They also noted that the CGA identified substantial deficits that could affect poor clinical outcomes even in normal performance status (3). Moreover, this study also pointed out that potentially modifiable deficits should be assessed with interventions in older cancer patients with normal performance scores, which is consistent with the recent studies (4, 14). In our study, 79% of the patients with normal performance status (ECOG-PS 0) had at least one geriatric syndrome. In addition, the ECOG-PS score was significantly correlated with the frequency of geriatric syndromes in the present study. Moreover, some geriatric syndromes were significantly more common in the ECOG-PS 2 group compared to the ECOG-PS 0 group or in the ECOG-PS 1 group compared to the ECOG-PS 0 group. Although ECOG-PS could play an important role in the management of cancer patients, our study found that 38% of the patients in the ECOG-PS 0 group had three or more geriatric syndromes. Moreover, even in the ECOG-PS 0 group, 39% of the patients had insomnia. In addition, in ECOG-PS 1 and 2 groups, most patients had three or more geriatric syndromes. In addition, a study in Japan found that geriatric assessment variables could predict systemic therapy toxicity in older cancer patients (28). They emphasize that ECOG-PS is frequently used in patients to predict treatment toxicity and mortality; however, it is not suitable or sufficient for predicting treatment outcomes in older cancer patients. In our study, more than two-thirds of the patients had a history of chemotherapy, and geriatric syndromes were common in patients with all ECOG-PS groups, even in the normal PS group. In our research, although the frequency of geriatric syndromes increased as ECOG-PS increased, the geriatric syndromes and co-incidence were common even in ECOG-PS 0 and 1 groups. Thus, the performance status reviews cannot possibly interrogate many parts of the CGA for older cancer patients (4). The comprehensive geriatric assessment provided crucial information on the functional assessment of older cancer patients, including patients with a good performance status. Considering the importance of these geriatric syndromes for the prognosis and clinical outcomes of older cancer patients, it is very crucial to detect and integrate these geriatric syndromes in the treatment assessment.
Depression is among the most common geriatric syndromes in patients with cancer, with prevalence estimates reaching as high as 25% (29). However, recognizing depression can be difficult and is often underdefined. In a study consisting mostly of gastrointestinal cancer patients, the prevalence of having at least one geriatric syndrome was 65.2%. Depression (30%) was the most common geriatric syndrome in this research (24). Similar to the findings of the above-mentioned study, gastrointestinal cancers were the most common cancer type in our study. In our research, at least one geriatric syndrome was present in 79% of the ECOG-PS 0 group, 95% of the ECOG-PS 1 group, and 100% of the ECOG-PS 2 group. Depression was also found at a similar rate (27.6%) in the present study. Moreover, in this study, which mostly included patients with good performance scores, urinary incontinence, one of the most important geriatric syndromes, was detected at very low rates. However, in our study, it was present in approximately one-third of the patients, and there was no difference between the ECOG-PS groups. Urinary incontinence is critical for older cancer patients because it is associated with many adverse outcomes, including depression, anxiety, poorer quality of life, higher mortality rates, falls, pressure ulcers, diabetes, arthritis, fecal incontinence, and frailty (30). A recent study showed that the risk of malnutrition is related to a poor prognosis in older cancer patients. Moreover, malnutrition can be associated with many geriatric syndromes (10). In our study, the risk of malnutrition had been considerably detected in older patients with cancer, and it was correlated with poor ECOG-PS status. Polypharmacy, an important geriatric syndrome, was shown to be predictive for chemotherapy toxicity and overall survival. It may be more common in older patients with cancer compared with the general geriatric population due to multiple factors (2). Polypharmacy was present in one-third of the patients in our study, and there was no difference between the ECOG-PS groups. In addition, sarcopenia may be a prognostic factor for treatment outcomes and the overall survival in older cancer patients. Therefore, oncologists should focus on the sarcopenia status of their patients when oncological treatment is planned (31). In our research, sarcopenia was detected more frequently in poor ECOG-PS groups. In addition, falls were prevalent among older cancer patients, and they were related to poor functional status and clinical outcomes (2, 32). In the present study, falls were more common in the ECOG 1 group than in the ECOG 0 group, and they were associated with other geriatric syndromes. In addition, sleeping disorders can also adversely affect patients’ quality of life and may even influence treatment outcomes in older patients with cancer (33). Insomnia was the most frequent geriatric syndrome in the ECOG-PS 0 group in our research. However, most of the patients had no excessive daytime sleepiness.
Frailty is defined as a result of vulnerability to the loss of reserve in response to stressors and a decline in physiological performance reserves and organ functions (34). It is a substantial predictor of poor treatment tolerance, treatment toxicities, decreased quality of life, and shorter survival in older patients with cancer (35, 36). It is often accepted as a frequent and underdiagnosed geriatric syndrome (37). In a Nordic study, it was found that the geriatric syndromes, including frailty and the ECOG-PS, showed prognostic value in older cancer patients (5). This study points out that frailty should be recognized at the initiation of the cancer treatment. Moreover, in a Norwegian study, they found that geriatric assessment was superior to oncologists’ clinical judgment in identifying frailty. In this study, 49% of the patients were frail. They found that only the geriatric assessment-frailty status could be a prognostic factor for survival (35). In our study, the prevalence and co-incidence of geriatric syndromes were common in all groups, including the ECOG-PS 0 group. In our research, frailty, the most common geriatric syndrome in the ECOG-PS 1 and 2 groups, was detected in 70 and 86% of the patients, respectively. In the ECOG-PS 0 group, frailty and insomnia were the most common geriatric syndromes, and they were detected in one-third of the patients. Moreover, frailty was 4.2 times (the highest ratio) more common in the ECOG-PS 1 group compared to the ECOG-PS 0 group. In addition, it was 10.8 times more common in the ECOG-PS 2 group compared to the ECOG-PS 0 group. It is shown that frailty can simply be identified with CGA. While oncologists usually use the ECOG-PS in clinical practice, it can have a poor correlation with the CGA, leading to questions about its usefulness in older cancer patients (3). Although using the ECOG-PS in clinical practice provides important prognostic information, the addition of CGA gives more crucial details for older frail patients with cancer (3, 35, 38).
Our study has some limitations. First, our research was a cross-sectional study. Our cancer sample was heterogeneous. Therefore, it may be difficult to generalize this conclusion to all cancer patients. In addition, we did not include all geriatric syndromes. Moreover, increasing the representation of ECOG-PS 2 patients by adding more participants could be effective in improving the study results. However, we state that our study provides substantial information for clinicians and their patients. It may be a reference for more comprehensive prospective studies planned in the future.
In conclusion, our real-life study found that the prevalence of geriatric syndromes increased as ECOG-PS increased. Some geriatric syndromes were significantly more common as ECOG-PS increased. Moreover, geriatric syndromes and their co-incidence were common in older cancer patients, even in their normal performance status. Oncologists should incorporate geriatric syndromes into the decision-making process of cancer treatment to maximize the impact on clinical outcomes in older patients with cancer.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving humans were approved by the Clinical Research Ethics Committee of Bezmialem Vakif University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
AT: Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Writing – original draft, Writing – review & editing. AY: Data curation, Investigation, Writing – review & editing. MB: Investigation, Supervision, Writing – review & editing. ZS: Resources, Writing – review & editing. ZA: Data curation, Investigation, Writing – review & editing. MSi: Formal analysis, Writing – review & editing. HT: Visualization, Writing – review & editing. MSe: Methodology, Writing – review & editing. PS: Data curation, Investigation, Methodology, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Yancik, R . Population aging and cancer: a cross-national concern. Cancer J. (2005) 11:437–41. doi: 10.1097/00130404-200511000-00002
2. Magnuson, A , Sattar, S , Nightingale, G , Saracino, R , Skonecki, E , and Trevino, KM . A practical guide to geriatric syndromes in older adults with Cancer: a focus on falls, cognition, polypharmacy, and depression. Am Soc Clin Oncol Educ Book. (2019) 39:e96–e109. doi: 10.1200/EDBK_237641
3. Jolly, TA , Deal, AM , Nyrop, KA , Williams, GR , Pergolotti, M , Wood, WA, et al. Geriatric assessment-identified deficits in older cancer patients with normal performance status. Oncologist. (2015) 20:379–85. doi: 10.1634/theoncologist.2014-0247
4. Repetto, L , Fratino, L , Audisio, RA , Venturino, A , Gianni, W , Vercelli, M, et al. Comprehensive geriatric assessment adds information to eastern cooperative oncology group performance status in elderly cancer patients: an Italian Group for Geriatric Oncology Study. J Clin Oncol. (2002) 20:494–502. doi: 10.1200/JCO.2002.20.2.494
5. Liposits, G , Ryg, J , Skuladottir, H , Winther, SB , Möller, S , Hofsli, E, et al. Prognostic value of baseline functional status measures and geriatric screening in vulnerable older patients with metastatic colorectal cancer receiving palliative chemotherapy – the randomized NORDIC9-study. J Geriatr Oncol. (2023) 14:101408. doi: 10.1016/j.jgo.2022.11.007
6. Pal, SK , Katheria, V , and Hurria, A . Evaluating the older patient with cancer: understanding frailty and the geriatric assessment. CA Cancer J Clin. (2010) 60:120–32. doi: 10.3322/caac.20059
7. Mohile, SG , and Magnuson, A . Comprehensive geriatric assessment in oncology. Interdiscip Top Gerontol. (2013) 38:85–103. doi: 10.1159/000343608
8. Extermann, M . Studies of comprehensive geriatric assessment in patients with cancer. Cancer Control. (2003) 10:463–8. doi: 10.1177/107327480301000604
9. Decoster, L , Van Puyvelde, K , Mohile, S , Wedding, U , Basso, U , Colloca, G, et al. Screening tools for multidimensional health problems warranting a geriatric assessment in older cancer patients: an update on SIOG recommendations†. Ann Oncol. (2015) 26:288–300. doi: 10.1093/annonc/mdu210
10. Sucuoglu Isleyen, Z , Besiroglu, M , Yasin, AI , Simsek, M , Topcu, A , Smith, L, et al. The risk of malnutrition and its clinical implications in older patients with cancer. Aging Clin Exp Res. (2023) 35:2675–83. doi: 10.1007/s40520-023-02538-0
11. Yasin, AI , Topcu, A , Akuc, MN , Türk, HM , and Soysal, P . A comparison of anticholinergic burden in older patients with and without cancer. Future Oncol. (2021) 17:5067–75. doi: 10.2217/fon-2021-0469
12. Mohile, SG , Fan, L , Reeve, E , Jean-Pierre, P , Mustian, K , Peppone, L, et al. Association of cancer with geriatric syndromes in older Medicare beneficiaries. J Clin Oncol. (2011) 29:1458–64. doi: 10.1200/JCO.2010.31.6695
13. Ates Bulut, E , Soysal, P , and Isik, AT . Frequency and coincidence of geriatric syndromes according to age groups: single-center experience in Turkey between 2013 and 2017. Clin Interv Aging. (2018) 13:1899–905. doi: 10.2147/CIA.S180281
14. Balducci, L , and Extermann, M . Management of cancer in the older person: a practical approach. Oncologist. (2000) 5:224–37. doi: 10.1634/theoncologist.5-3-224
15. Kim, YJ , Kim, JH , Park, MS , Lee, KW , Kim, KI , Bang, SM, et al. Comprehensive geriatric assessment in Korean elderly cancer patients receiving chemotherapy. J Cancer Res Clin Oncol. (2011) 137:839–47. doi: 10.1007/s00432-010-0945-1
16. Bruijnen, CP , van Harten-Krouwel, DG , Koldenhof, JJ , Emmelot-Vonk, MH , and Witteveen, PO . Predictive value of each geriatric assessment domain for older patients with cancer: a systematic review. J Geriatr Oncol. (2019) 10:859–73. doi: 10.1016/j.jgo.2019.02.010
17. Oken, MM , Creech, RH , Tormey, DC , Horton, J , Davis, TE , McFadden, ET, et al. Toxicity and response criteria of the eastern cooperative oncology group. Am J Clin Oncol. (1982) 5:649–56. doi: 10.1097/00000421-198212000-00014
18. Soysal, P , and Tan, SG . The prevalence and co-incidence of geriatric syndromes in older patients with early-stage Alzheimer's disease and dementia with Lewy bodies. Aging Clin Exp Res. (2021) 33:2599–603. doi: 10.1007/s40520-020-01774-y
19. Cruz-Jentoft, AJ , Bahat, G , Bauer, J , Boirie, Y , Bruyère, O , Cederholm, T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. (2019) 48:16–31. doi: 10.1093/ageing/afy169
20. Soysal, P , Heybeli, C , Koc Okudur, S , Caliskan Bozyel, E , Smith, L , and Kazancioglu, R . Prevalence and co-incidence of geriatric syndromes according to glomerular filtration rate in older patients. Int Urol Nephrol. (2023) 55:469–76. doi: 10.1007/s11255-022-03356-5
21. Mikami, Y , Watanabe, Y , Edahiro, A , Motokawa, K , Shirobe, M , Yasuda, J, et al. Relationship between mortality and Council of Nutrition Appetite Questionnaire scores in Japanese nursing home residents. Nutrition. (2019) 57:40–5. doi: 10.1016/j.nut.2018.05.030
22. Barry, E , Galvin, R , Keogh, C , Horgan, F , and Fahey, T . Is the timed up and go test a useful predictor of risk of falls in community dwelling older adults: a systematic review and meta-analysis. BMC Geriatr. (2014) 14:14. doi: 10.1186/1471-2318-14-14
23. Scura, D , and Munakomi, S . Tinetti gait and balance test. StatPearls. Treasure Island, FL: StatPearls Publishing (2024).
24. Limpawattana, P , Phimson, K , Sookprasert, A , Sirithanaphol, W , and Chindaprasirt, J . Prevalence of geriatric syndromes in elderly Cancer patients receiving chemotherapy. Curr Gerontol Geriatr Res. (2020) 2020:1–5. doi: 10.1155/2020/9347804
25. Maas, HA , Janssen-Heijnen, ML , Olde Rikkert, MG , and Machteld Wymenga, AN . Comprehensive geriatric assessment and its clinical impact in oncology. Eur J Cancer. (2007) 43:2161–9. doi: 10.1016/j.ejca.2007.08.002
26. Lund, CM , Vistisen, KK , Olsen, AP , Bardal, P , Schultz, M , Dolin, TG, et al. The effect of geriatric intervention in frail older patients receiving chemotherapy for colorectal cancer: a randomised trial (GERICO). Br J Cancer. (2021) 124:1949–58. doi: 10.1038/s41416-021-01367-0
27. Jensen, CE , Vohra, SN , Nyrop, KA , Deal, AM , Muss, HB , Lichtman, EI, et al. Geriatric-assessment-identified functional deficits among adults with multiple myeloma with normal performance status. J Geriatr Oncol. (2022) 13:182–9. doi: 10.1016/j.jgo.2021.08.004
28. Kanazu, M , Shimokawa, M , Saito, R , Mori, M , Tamura, A , Okano, Y, et al. Predicting systemic therapy toxicity in older adult patients with advanced non-small cell lung cancer: a prospective multicenter study of National Hospital Organization in Japan. J Geriatr Oncol. (2022) 13:1216–22. doi: 10.1016/j.jgo.2022.07.011
29. Nelson, CJ , Cho, C , Berk, AR , Holland, J , and Roth, AJ . Are gold standard depression measures appropriate for use in geriatric cancer patients? A systematic evaluation of self-report depression instruments used with geriatric, cancer, and geriatric cancer samples. J Clin Oncol. (2010) 28:348–56. doi: 10.1200/JCO.2009.23.0201
30. Soysal, P , Veronese, N , Ippoliti, S , Pizzol, D , Carrie, AM , Stefanescu, S, et al. The impact of urinary incontinence on multiple health outcomes: an umbrella review of meta-analysis of observational studies. Aging Clin Exp Res. (2023) 35:479–95. doi: 10.1007/s40520-022-02336-0
31. Meza-Valderrama, D , Marco, E , Dávalos-Yerovi, V , Muns, MD , Tejero-Sánchez, M , Duarte, E, et al. Sarcopenia, malnutrition, and Cachexia: adapting definitions and terminology of nutritional disorders in older people with Cancer. Nutrients. (2021) 13:761. doi: 10.3390/nu13030761
32. Fahimnia, S , Mirhedayati Roudsari, H , Doucette, J , and Shahrokni, A . Falls in older patients with Cancer undergoing surgery: prevalence and association with geriatric syndromes and levels of disability assessed in preoperative evaluation. Curr Gerontol Geriatr Res. (2018) 2018:1–7. doi: 10.1155/2018/5713285
33. Harris, B , Ross, J , and Sanchez-Reilly, S . Sleeping in the arms of cancer: a review of sleeping disorders among patients with cancer. Cancer J. (2014) 20:299–305. doi: 10.1097/PPO.0000000000000067
34. Uslu, A , and Canbolat, O . Relationship between frailty and fatigue in older Cancer patients. Semin Oncol Nurs. (2021) 37:151179. doi: 10.1016/j.soncn.2021.151179
35. Kirkhus, L , Šaltytė Benth, J , Rostoft, S , Grønberg, BH , Hjermstad, MJ , Selbæk, G, et al. Geriatric assessment is superior to oncologists' clinical judgement in identifying frailty. Br J Cancer. (2017) 117:470–7. doi: 10.1038/bjc.2017.202
36. Soto-Perez-de-Celis, E , Li, D , Yuan, Y , Lau, YM , and Hurria, A . Functional versus chronological age: geriatric assessments to guide decision making in older patients with cancer. Lancet Oncol. (2018) 19:e305–16. doi: 10.1016/S1470-2045(18)30348-6
37. Anic, K , Varchola, J , Schmidt, MW , Schwab, R , Linz, VC , Schmidt, M, et al. Influence of interdisciplinary frailty screening on perioperative complication rates in elderly ovarian cancer patients: results of a retrospective observational study. Arch Gynecol Obstet. (2023) 307:1929–40. doi: 10.1007/s00404-022-06850-4
38. Nightingale, G , Battisti, NML , Loh, KP , Puts, M , Kenis, C , Goldberg, A, et al. Perspectives on functional status in older adults with cancer: an interprofessional report from the International Society of Geriatric Oncology (SIOG) nursing and allied health interest group and young SIOG. J Geriatr Oncol. (2021) 12:658–65. doi: 10.1016/j.jgo.2020.10.018
Keywords: cancer, ECOG performance status, geriatric syndrome, prevalence, frailty
Citation: Topcu A, Yasin AI, Besiroglu M, Sucuoglu Isleyen Z, Alaca Topcu Z, Simsek M, Turk HM, Seker M and Soysal P (2024) Prevalence and co-incidence of geriatric syndromes according to the ECOG performance status in older cancer patients. Front. Med. 11:1331246. doi: 10.3389/fmed.2024.1331246
Received: 31 October 2023; Accepted: 29 January 2024;
Published: 19 February 2024.
Edited by:
Marios Kyriazis, National Gerontology Centre, CyprusReviewed by:
Tsuyoshi Harada, National Cancer Center Hospital East, JapanCopyright © 2024 Topcu, Yasin, Besiroglu, Sucuoglu Isleyen, Alaca Topcu, Simsek, Turk, Seker and Soysal. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Atakan Topcu, YXRha2FudG9wY3VAaG90bWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.