- 1Department of Urology, Uro-Oncology, Robot Assisted and Reconstructive Urologic Surgery, University of Cologne Faculty of Medicine and University Hospital Cologne, Cologne, Germany
- 2German Center for Neurodegenerative Diseases (DZNE) Site Rostock/Greifswald, Ellernholzstrasse 1-2, Greifswald, Germany
- 3Epidemiology, IQVIA, 60549, Frankfurt, Germany
- 4Clinic for Gastroenterology, Hepatology and Infectious Diseases, University Hospital Düsseldorf, Medical Faculty of Heinrich Heine University Düsseldorf, Düsseldorf, Germany
- 5Occupational Medicine, and Public Health (ISAP) of the Medical Faculty at the University of LeipzigInstitute for Social Medicine, Leipzig, Germany
Purpose: Urologists’ practices reported decreasing medical care provision and increasing stress experience in the first wave of the COVID-19 pandemic. However, long-term effects of the pandemic are unknown.
Methods: Medical record data of n = 127 urologists were used to assess changes in healthcare provision, comparing the pandemic with the pre-pandemic period. An online survey among n = 101 urologists was conducted to assess the physicians’ perceptions of the identified healthcare provision and organizational changes and experiences of anxiety, stress, and support needs during the pandemic waves. Urologists consultations, specialists’ referrals, hospital admissions, documented cancer diagnoses, urologists’ perceptions of causes for these changes and experienced stress, anxiety and support needs. Results were demonstrated using descriptive statistics.
Results: Over the first two years of the pandemic, there was a slight decline in consultations (−0,94%), but more intensive reduction in hospital admissions (−13,6%) and identified cancer diagnoses (−6,2%). Although patients’ behavior was seen as the main reason for the changes, 71 and 61% of consultations of high-risk patients or urgent surgeries were canceled. Telemedical approaches were implemented by 58% of urologists, and 88% stated that the reduced cancer detection rate would negatively affect patients’ outcomes. Urologists reported higher anxiety, stress, and need for support during all waves of the pandemic than other disciplines, especially females.
Conclusion: The pandemic tremendously affects urologists’ health care provision and stress experience, possibly causing long-term consequences for patients and physicians.
1 Introduction
As the COVID-19 pandemic led to a global crisis, contact restrictions were imposed, and medical measures were reduced to the minimum to contain the virus’ rapid dissemination (1, 2). These restrictions did not only concern hospital staff, increasing intensive care capacities and postponing elective surgical procedures, but the outpatient sector was also intensively affected (3–5).
A cross-sectional study based on nearly four million consultations evaluated the number of healthcare services during the first pandemic wave, demonstrating a 65% decline in face-to-face consultations (6). The healthcare services provided in the ambulatory sector also significantly decreased during the first wave, especially when the protective measures were imposed in March 2020, affecting mainly elective consultations (7).
At the beginning of the pandemic, urologists from the outpatient sector were not adequately prepared to deal with the new situation in their practices, causing considerable concern and fear among physicians (8–10). During the first COVID-19 wave, 24% of all urologists felt high, and 48% felt a moderate threat level (8). A German observational study revealed that hospital admissions, recognized incident diseases, and consultations significantly decreased throughout the pandemic in primary care (11). However, it is unknown whether and, if so, to what extent the reduced provision of urologist services was compensated at the end of the pandemic.
The negative impact of the pandemic on the mental health of healthcare professionals strongly influences work-life (12). A prior survey- and interview-based study revealed significant physical and psychological burden associated with the pandemic, with a high prevalence of burnout (57.7%) among physicians (13). Especially studies from Asia demonstrated high stress, depression, and anxiety symptoms with severe degrees in 2.2 to 14.5% at the pandemic’s beginning (14). However, data are lacking regarding the stress experienced by urologists during the pandemic.
This analysis’s objectives were to evaluate the impact of the COVID-19 pandemic on the daily work routine and medical service provision of urologists and their perceived stress during the first four pandemic waves in Germany.
2 Materials and methods
2.1 Study design
This study comprised a secondary data analysis based on medical record data from the Disease Analyzer database (IQVIA) to examine changes in healthcare service provision and a survey to assess perceived reasons for these changes. The secondary data captured consultations, drug prescriptions, specialist referrals, diagnoses made, and basic medical and demographic data directly and anonymously from the practices via an interface to their respective practice management software between September 2019 and February 2020 (pre-pandemic period) as well as March 2020 and September 2021 (pandemic period). The survey questionnaire was distributed using the cloud-based open-source tool LimeSurvey. The Professional Association of German Urologists e.V shared the survey link between 04 December 2021 and 28 February 2022 with their members via different communication channels. All participants agreed on the conditions of the survey before taking part. The survey was approved by the Ethical Committee of the Chamber of Physicians of Mecklenburg-Western Pomerania registry number (BB 127/21). Detailed information is given in the supplementary material.
2.2 Statistical analyses
Descriptive statistics were used to demonstrate changes in healthcare provision, recognition of cancer cases and perception and views on causes of these changes. Fisher’s exact Tests were used to check significance of these differences. Multivariate regression models were used to assess associated factors of stress, anxiety and support needed of urologists. Analyses were performed using SAS version 9.4 (Cary, NC: SAS Institute Inc) and STATA/IC 16.
3 Results
3.1 The course of consultations, drug prescriptions, hospital admissions, and incident cancer diagnoses
During the 1st COVID-19 wave (March to June 2020), 11% fewer consultations per month were seen compared to the same period in 2018 and 2019. During the subsequent waves, consultations did not reach the frequency of the corresponding period the year before the pandemic (−1%) and decreased even to a greater extent with the implementation of contact restrictions in February 2021 (−3,4%). From May to September 2021 (3rd wave and summer plateau), the consultation frequency increased again but did not reach the values of the pre-pandemic years 2018 and 2019 (−0,8%, Figure 1A).

Figure 1. (A,B) Trends in consultation frequency, drug prescriptions, hospital admissions and cancer diagnosis over the pandemic periods. Number of the examined parameter per practice is displayed on the y-axis on the left. The dark blue column indicates the reference value (average of the respective month of the years 2018/19), the light blue column shows the value in the respective month of the pandemic (2020/21). The phases of the federal contact restriction measures are indicated by two large turquoise rectangles, an average value was calculated for all phases. The red line and the y-axis on the right display the cumulative difference (%) of the target value during the pandemic compared to the pre-pandemic month. (A) Trends in consultation frequency over the pandemic periods. (B) Trends in drug prescriptions over the pandemic periods. (C) Trends in hospital admissions over the pandemic periods. (D) Trends in incident cancer diagnoses over the pandemic periods.
The number of drug prescriptions during the pandemic was less variable than the frequency of consultations. Prescriptions decreased massively during the 1st wave in May 2020 (−5,4%). They increased slowly to an even higher number of prescriptions compared to the pre-pandemic times (+1,1%), with only slight decreases in prescriptions during each wave (Figure 1B).
The number of hospital admissions was below pre-pandemic levels throughout the observer period with the largest decrease during the 1st wave (−30,3%) and the summer plateau of 2021 (−3,5%; Figure 1C).
The cancer diagnoses (ICD C00-C99) decreased rapidly during the pandemic and did not reach pre-pandemic levels throughout the study period (Figure 1D).
3.2 Changes in practice management and reasons for the decline in incidence
Approximately one-third of all urologists reduced domiciliary visits (32%), visits to nursing homes (25%), number of consultations (35%) as well as consultations hours (20%) during the pandemic. Urologists reported less reduced domiciliary visits than general physicians and other specialists (25% vs. 39%, p = 0.025; Table 1). Consultations of high-risk patients were also reduced by 71%. 61 and 90% of all urologists reported that urgent and elective surgeries were difficult to organize, even more often than non-urologists (61% vs. 42%, p = 0.003; 90% vs. 66%, p < 0.001). Compared to pre-pandemic levels in 2019, preventive medical examinations and elective consultations were canceled in 40 and 36%, respectively. Telemedical approaches (telephone consultation, videotelephony) were used in 58%. Almost 60% of all urologists reported COVID-19-related absences of employees, and one in four practices had to close temporarily during the pandemic.
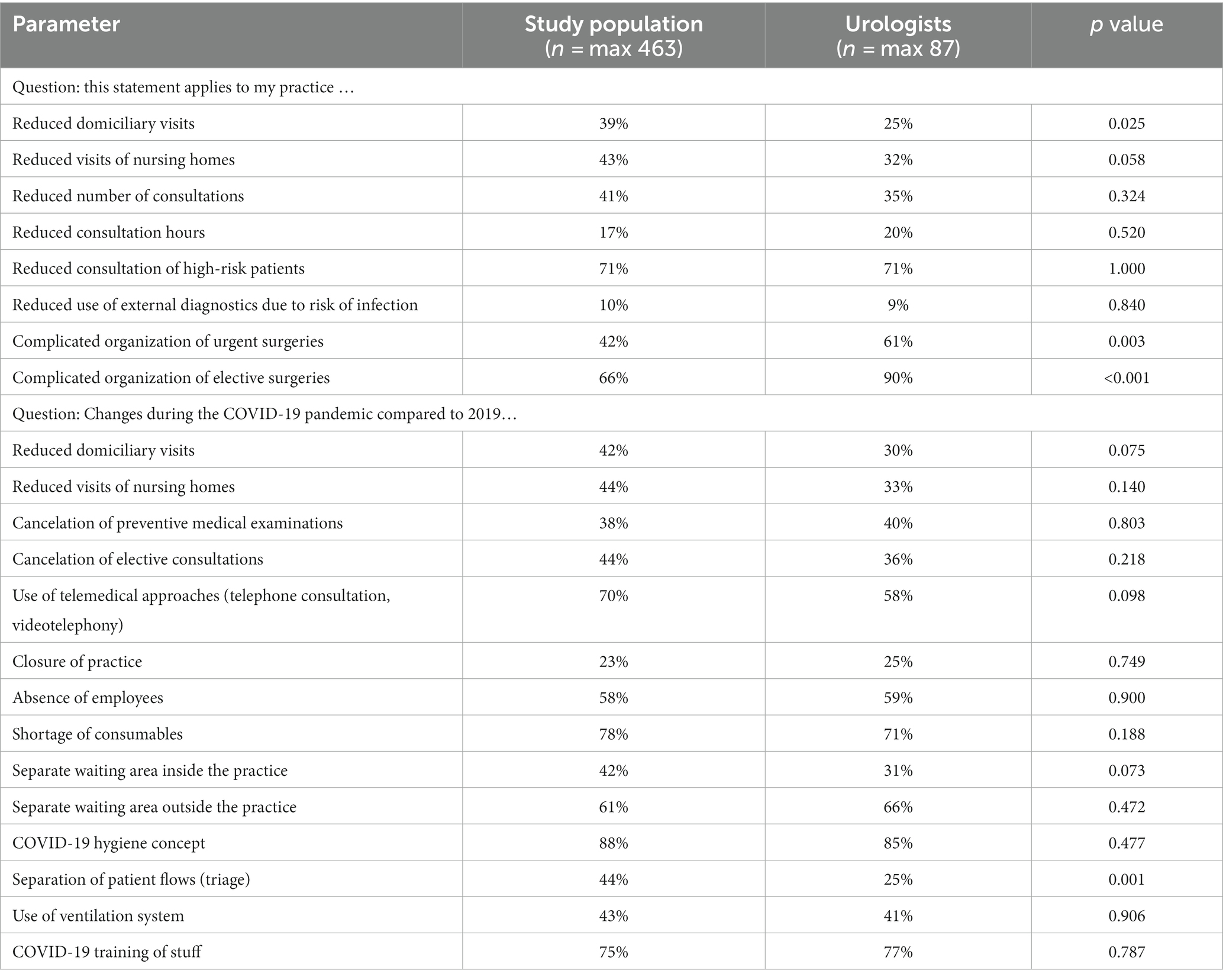
Table 1. Changes in practice management, displayed as a comparison of urologists and the whole study population (general physicians and other specialists except urologists).
3.3 Urologists perception of the reasons for the reduced consultations and recognition of incident diagnoses
87% of all urologists noticed a decreased consultation rate during the first wave of the pandemic. 95% of all urologists stated that patients’ behavior is the most important reason for reduced consultations (Table 2). Most urologists (88%) fear that the reduced detection rate of incident disease will harm patients’ outcomes. 53% of all urologists noticed the missing rise of consultations during the subsequent waves of the pandemic. The main reasons were still seen in patients’ behavior (85%) and persistent stress of the pandemic (59%).
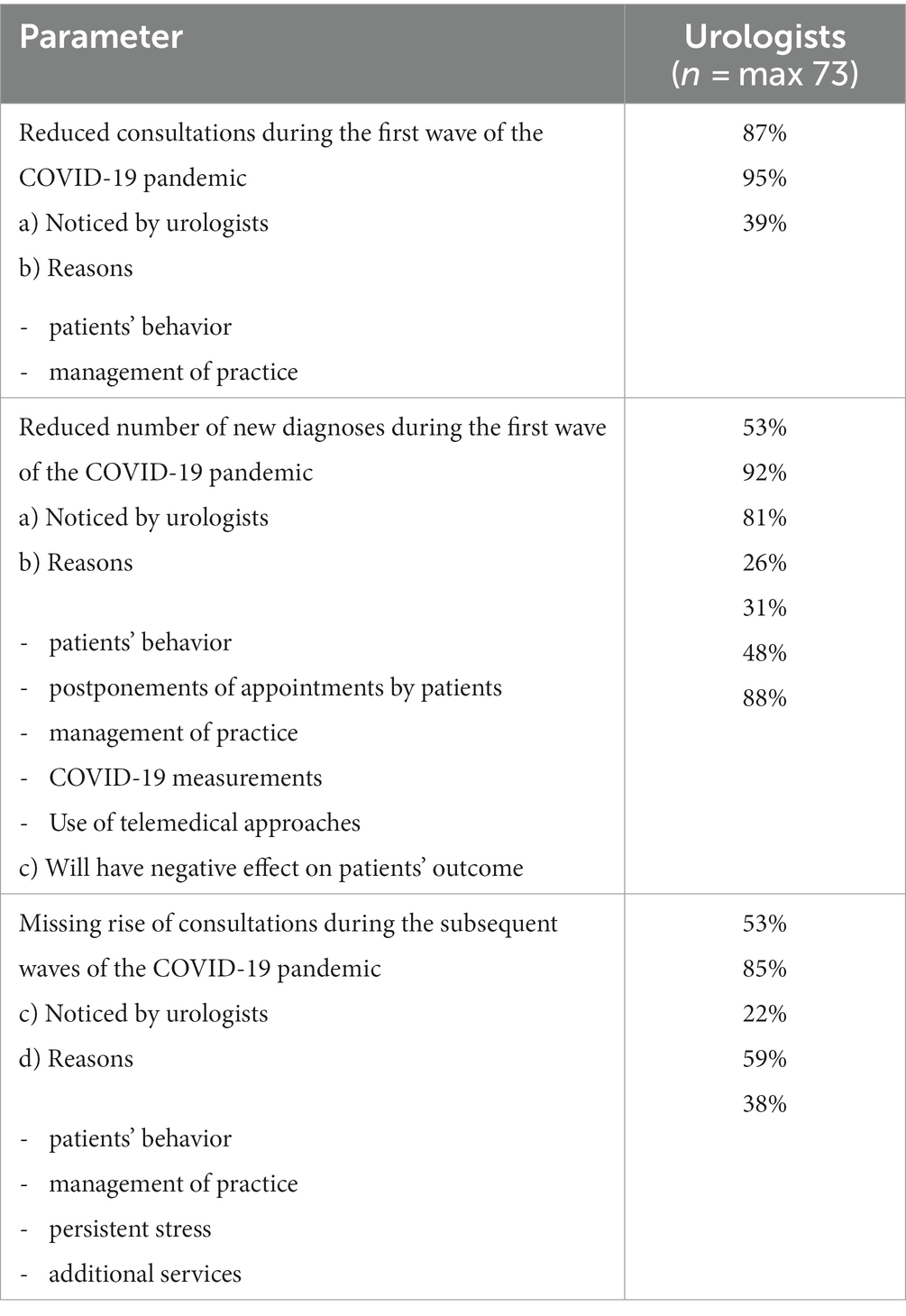
Table 2. Perception of the reasons for the reduced consultations and incidences of diagnosis, as described by German urologists.
3.4 Level of anxiety, stress, and the need for support during the pandemic
Urologists reported the highest level of anxiety during the first lockdown (Mean 6.1 (SD 2.5), Table 3). The level of anxiety slowly decreased until it increased moderately again in the fourth wave (Mean 4.4 (3.1)). Except for the fourth wave, urologists reported a significantly higher anxiety level than general physicians and other specialists (1st wave: p = 0.010; 2nd wave: p = 0.036; 3rd wave: p = 0.009; 4th wave: p = 0.121) and a higher stress level and need for support during the pandemic than in the pre-pandemic period.
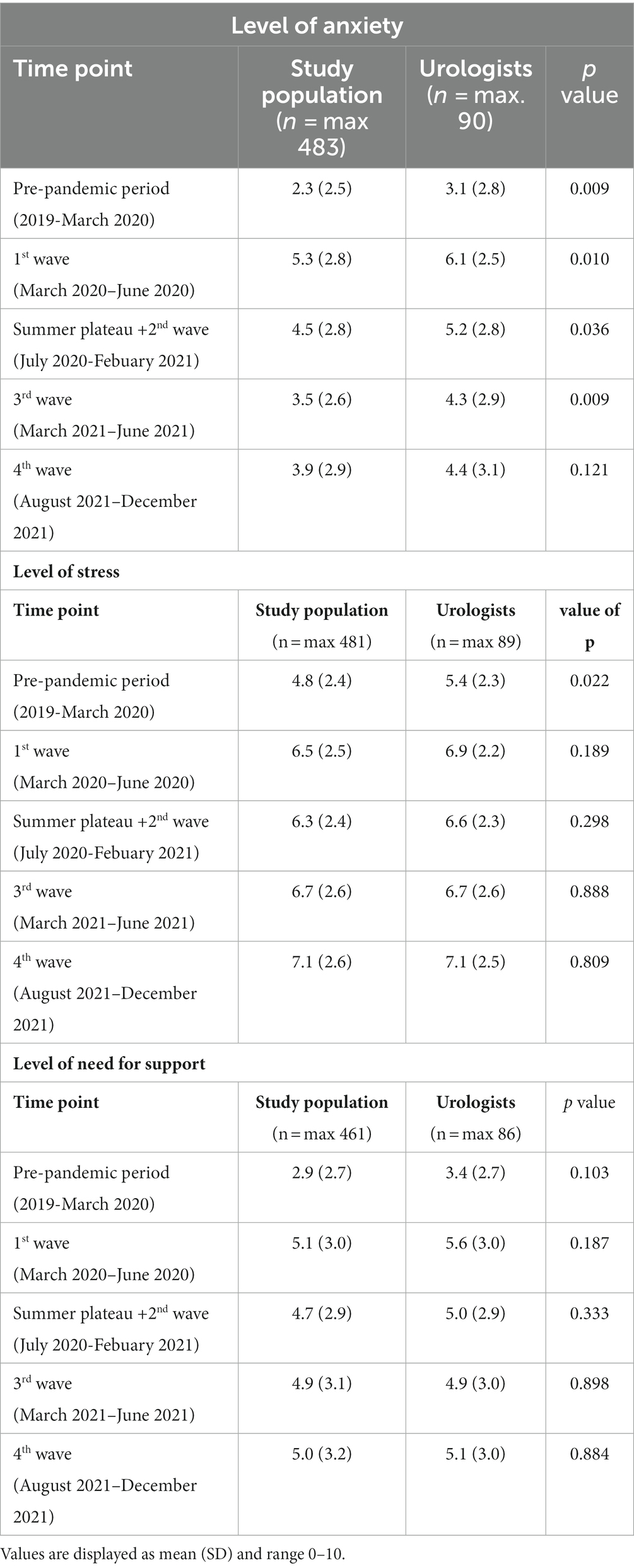
Table 3. Anxiety, stress and need for support during the pandemic, displayed as a comparison of urologists and the whole study population (general physicians and other specialists except urologists).
Multivariate analysis revealed a significantly higher level of anxiety in female urologists during the fourth wave (p = 0.016; Supplementary Table S2). Regarding the level of stress, urologists treating a higher number of patients (>1,500 patients/quarter) reported a higher level of stress in the third wave (p = 0.038) and in the fourth wave (p = 0.043). In addition, urologists in individual practices described a higher stress level in the fourth wave than urologists in community health centers (p = 0.018).
Reasons for anxiety and stress were mostly patient behavior (48.4%) and organization of practice (18.7%) in the first wave (Supplementary Table S3). In the second wave, private burdens had growing importance (20.0%). In the further course, increasing bureaucracy (third wave: 21.4%; fourth wave: 26.4%) as well as additional services (third wave: 29.2%, fourth wave: 17.1%), such as vaccination or COVID-19 testing, were the most important reasons. However, patient behavior still represented an important factor.
4 Discussion
Our study was the first to evaluate the long-term effect of the COVID-19 pandemic on work-related and personal aspects among urologists in the German ambulatory sector. The decline in consultations, drug prescriptions, hospital admissions, and cancer diagnosis detection during the pandemic was in line with previous studies, showing a significantly decreased number of cancer screenings and diagnoses during the early phase of the COVID-19 pandemic (15).
However, data evaluating its longitudinal change was lacking. A German survey assessed the provision of medical care services during the first and second waves of the COVID-19 pandemic (16). Congruent to our data, the urologic outpatient sector described a 50% reduction in consultation during the first wave. This is also in line with studies reporting a strong impact of the pandemic on German urologists’ daily work (8). An international cohort study with more than 20,000 cancer patients confirmed that cancer surgery systems were worldwide fragile to lockdowns, as 14% of all patients awaiting surgery did not undergo planned surgery and experienced longer preoperative delays during lockdowns (17). This is in line with the high number of cancelations of preventive medical examinations (40%) in our study. Our study revealed that consultations, hospital admissions, and cancer diagnoses decreased massively, not reaching pre-pandemic levels throughout the study period. A previously published analysis supports our findings regarding prostate cancer, as fewer prostate cancer patients were surgically treated during the first two waves of the pandemic, which did not reach pre-pandemic levels (18).
Nine out of ten urologists in our study fear that the reduced detection rate of incident disease will harm patients’ outcomes. French studies aroused suspicion that a reduced consultation and detection rate of cancer diagnoses during the pandemic might lead to a higher tumor burden, number of advanced tumors (pT3b: 11.2 vs. 25.6%; nodal positive: 14.8 vs. 46.1%) and metastatic disease (5.9 vs. 9.3%) of prostate cancer patients (19, 20). However, long-term data is missing so far but is urgently needed. Thus, the fine line between a shutdown and a potential negative impact on the healthcare system should be intensively evaluated in future pandemic waves.
During the pandemic’s beginning, German urologists awarded telehealth for having a high relevance. Still, only 25,5% of all urologists from the ambulatory sector already included telemedical approaches in their daily routine (8). In the survey two years later, telemedical approaches were used by 58% of all urologists from the outpatient sector, showing that telemedicine has steply risen during the pandemic (5). Although telemedicine incorporates advantages in a pandemic, our study participants stated that it might have complicated the identification of incident diagnoses, indicating a loss of vital clinical information and that physical examination and face-to-face consultations might not be replaceable. Consequently, healthcare professionals and patients must be trained in telemedical approaches before widespread uptake, and accurate electronic patient notes must be available. Especially follow-up consultations seem to be ideal for telemedical procedures (21).
Almost 60% of all urologists reported COVID-19-related absences from employees. One in four practices had to close temporarily during the pandemic, underlining the COVID-19 pandemic impact on health systems and social and economic structures (22). The observations of the pandemic’s influence can be used as a call for dynamic systemic transformation and improved resilience of healthcare workers. The World Health Organization also expounds on the potential negative impact of the COVID-19 pandemic on mental health of healthcare professionals, strongly impacting the work-life balance (12). In our study, urologists reported higher anxiety, stress, and need for support during the pandemic than in the pre-pandemic period. Anxiety and the need for support were highest during the first wave of the pandemic, which is in line with prior studies from China and Europe performed at the beginning of the pandemic revealed a high psychological burden among healthcare workers, especially in the outpatient sector (8, 23–26).
Our analysis revealed that urologists in individual practices and those treating more patients experienced the highest stress level in the third and/or fourth waves. The higher anxiety level in female urologists during the fourth wave is in line with the results of a German and French survey that evaluated mental health issues in healthcare workers during the beginning of the pandemic (8, 27). However, a previous analysis examining the pandemic-related stress experience of psychiatrists revealed that anxiety was dependent on feeling restricted (OR = 5.52) and risk of infection (OR = 5.74) but not on gender (28). The physical and psychological burden healthcare workers experienced during the COVID-19 pandemic is high, as the prevalence of burnout among physicians was nearly 60% (13). Further analysis of potential risk factors for developing mental health problems is paramount. Mental health and resilience could be supported by specific interventions and psychological support (29), which can be classified into four main categories: social/structural support, work environment, communication/information, and mental health support. However, systematic reviews revealed lacking evidence regarding selecting interventions beneficial to frontline workers’ resilience and mental health (29, 30). Future research is needed to promote mental well-being and resilience strategies in healthcare professionals during and after pandemics. Limitations of our study include the descriptive design of the analyses of consultations, drug prescriptions, hospital admission or incident cancer diagnoses over the pandemic periods, which did not account for the analyses of statistical significances. Furthermore, we used a non-validated survey, potentially leading to non-sampling errors which might negatively impact the accuracy and reliability of the results. Additionally, the low response rate of 5% of our survey could have negatively impacted the reliability and validity of the results.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The survey was approved by the Ethical Committee of the Chamber of Physicians of Mecklenburg-Western Pomerania (registry number (BB 127/21) and was conducted in accordance with Good Clinical Practice Guidelines: all participants agreed on the conditions of the survey before taking part.
Author contributions
PP: Data curation, Formal analysis, Writing – original draft, Writing – review & editing. MP: Formal analysis, Methodology, Writing – review & editing. KK: Formal analysis, Writing – review & editing. SL: Writing – review & editing. JB: Methodology, Writing – review & editing. BM: Formal analysis, Methodology, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors would like to express their gratitude to all individual participants of the survey. Furthermore, we would like to thank the Federation of German Urologists (BDU) for distributing the online survey.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2024.1320489/full#supplementary-material
References
1. Johns Hopkins Coronavirus Resource Center (2020). COVID-19 Map 2020. Available at: https://coronavirus.jhu.edu/map.html (accessed April 22, 2020).
2. DGU (Deutsche Gesellschaft für Urologie e.V.). Priorisierungsliste Urologie in Zeiten den Corona-Pandemie mit reduzierten Kapazitäten (Version 2.0., April 2020) (n.d). Available at: https://www.urologenportal.de/fileadmin/MDB/PDF/Presse/ab_Oktober_2019/DGU_Priorisierungsliste_2.0.pdf (accessed May 24, 2020).
3. Dotzauer, R, Böhm, K, Brandt, MP, Sparwasser, P, Haack, M, Frees, SK, et al. Global change of surgical and oncological clinical practice in urology during early COVID-19 pandemic. World J Urol. (2021) 39:3139–45. doi: 10.1007/S00345-020-03333-6
4. Jin, P, Park, H, Jung, S, and Kim, J. Challenges in urology during the COVID-19 pandemic. Urol Int. (2021) 105:3–16. doi: 10.1159/000512880
5. Somani, BK, Pietropaolo, A, Coulter, P, and Smith, J. Delivery of urological services (telemedicine and urgent surgery) during COVID-19 lockdown: experience and lessons learnt from a university hospital in United Kingdom. Scott Med J. (2020) 65:109–11. doi: 10.1177/0036933020951932
6. Joy, M, McGagh, D, Jones, N, Liyanage, H, Sherlock, J, Parimalanathan, V, et al. Reorganisation of primary care for older adults during COVID-19: a cross-sectional database study in the UK. Br J Gen Pract. (2020) 70:E540–7. doi: 10.3399/BJGP20X710933
7. Mangiapane, S.Z L.; Czihal, T., and Von Stillfried, D. Veränderung der vertragsärztlichen Leistungsinanspruchnahme während der COVID-Krise - Tabellarischer Trendreport für das 1. Quartal 2020. Zentralinstitut Für Die Kassenärztliche Versorgung Deutschl (2020). Available at: https://www.zi.de/publikationen/trendreport-covid-krise
8. Paffenholz, P, Peine, A, Fischer, N, Hellmich, M, Pfister, D, Heidenreich, A, et al. Impact of the COVID-19 pandemic on urologists in Germany. Eur Urol Focus. (2020) 6:1111–9. doi: 10.1016/J.EUF.2020.06.001
9. Bohlken, J, Kostev, K, Riedel-Heller, S, Hoffmann, W, and Michalowsky, B. Effect of the COVID-19 pandemic on stress, anxiety, and depressive disorders in German primary care: a cross-sectional study. J Psychiatr Res. (2021) 143:43–9. doi: 10.1016/J.JPSYCHIRES.2021.08.016
10. Bohlken, J, Schömig, F, Seehagen, T, Köhler, S, Gehring, K, Roth-Sackenheim, C, et al. Experience of practice-based psychiatrists and neurologists during the COVID-19 pandemic. Psychiatr Prax. (2020) 47:214–7. doi: 10.1055/A-1159-5575
11. Platen, M, Bohlken, J, Hoffmann, W, Kostev, K, and Michalowsky, B. The long-term impact of the COVID-19 pandemic on primary and specialized care provision and disease recognition in Germany. Front Public Heal. (2022) 10:10. doi: 10.3389/FPUBH.2022.1006578
12. Pfefferbaum, B, and North, CS. Mental health and the Covid-19 pandemic. N Engl J Med. (2020) 383:510–2. doi: 10.1056/NEJMP2008017
13. Alrawashdeh, HM, Al-Tammemi, AB, Alzawahreh, MK, Al-Tamimi, A, Elkholy, M, Al Sarireh, F, et al. Occupational burnout and job satisfaction among physicians in times of COVID-19 crisis: a convergent parallel mixed-method study. BMC Public Health. (2021) 21:811. doi: 10.1186/S12889-021-10897-4
14. Bohlken, J, Schömig, F, Lemke, MR, Pumberger, M, and Riedel-Heller, SG. COVID-19 pandemic: stress experience of healthcare workers - a short current review. Psychiatr Prax. (2020) 47:190–7. doi: 10.1055/A-1159-5551
15. Jacob, L, Loosen, SH, Kalder, M, Luedde, T, Roderburg, C, and Kostev, K. Impact of the COVID-19 pandemic on cancer diagnoses in general and specialized practices in Germany. Cancers (Basel). (2021) 13:1–11. doi: 10.3390/cancers13030408
16. Kriegmair, MC, Speck, T, Schneider, AW, Volkmer, B, and Michel, MS. Urological care in practices and clinics during the corona virus pandemic in Germany. Urologe A. (2021) 60:318–30. doi: 10.1007/S00120-021-01458-Z
17. Glasbey, J, Ademuyiwa, A, Adisa, A, AlAmeer, E, Arnaud, AP, Ayasra, F, et al. Effect of COVID-19 pandemic lockdowns on planned cancer surgery for 15 tumour types in 61 countries: an international, prospective, cohort study. Lancet Oncol. (2021) 22:1507–17. doi: 10.1016/S1470-2045(21)00493-9
18. Harke, NN, Wagner, C, Hermann, RM, Hadaschik, BA, Radtke, JP, Altay-Langguth, A, et al. Lessons learned after one year of COVID-19 from a urologist and radiotherapist view: a German survey on prostate cancer diagnosis and treatment. PLoS One. (2022) 17:e0269827. doi: 10.1371/JOURNAL.PONE.0269827
19. Thierry, AR, Pastor, B, Pisareva, E, Ghiringhelli, F, Bouché, O, De La Fouchardière, C, et al. Association of COVID-19 lockdown with the tumor burden in patients with newly diagnosed metastatic colorectal Cancer. JAMA Netw Open. (2021) 4:e2124483. doi: 10.1001/JAMANETWORKOPEN.2021.24483
20. Pepe, P, Pepe, L, Pennisi, M, and Fraggetta, F. Prostate Cancer diagnosis and management during one year of the COVID-19 pandemic. Anticancer Res. (2021) 41:3127–30. doi: 10.21873/ANTICANRES.15097
21. Pfister, D, Schmautz, M, and Paffenholz, P. COVID-19 in urology: influence of the pandemic on telemedicine, education and surgery. Urologe. (2021) 60:301–5. doi: 10.1007/s00120-021-01451-6
22. Haldane, V, De Foo, C, Abdalla, SM, Jung, AS, Tan, M, Wu, S, et al. Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries. Nat Med. (2021) 27:964–80. doi: 10.1038/S41591-021-01381-Y
23. Lai, J, Ma, S, Wang, Y, Cai, Z, Hu, J, Wei, N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
24. Qiu, J, Shen, B, Zhao, M, Wang, Z, Xie, B, and Xu, Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatry. (2020) 33:e100213. doi: 10.1136/gpsych-2020-100213
25. Frenkel, MO, Pollak, KM, Schilling, O, Voigt, L, Fritzsching, B, Wrzus, C, et al. Stressors faced by healthcare professionals and coping strategies during the early stage of the COVID-19 pandemic in Germany. PLoS One. (2022) 17:e0261502. doi: 10.1371/JOURNAL.PONE.0261502
26. El-Hage, W, Hingray, C, Lemogne, C, Yrondi, A, Brunault, P, Bienvenu, T, et al. Health professionals facing the coronavirus disease 2019 (COVID-19) pandemic: what are the mental health risks? Encéphale. (2020) 46:S73–80. doi: 10.1016/J.ENCEP.2020.04.008
27. Vallée, M, Kutchukian, S, Pradère, B, Verdier, E, Durbant, È, Ramlugun, D, et al. Prospective and observational study of COVID-19’s impact on mental health and training of young surgeons in France. Br J Surg. (2020) 107:e486–8. doi: 10.1002/BJS.11947
28. Bohlken, J, Kostev, K, Bartels, C, Wiltfang, J, Broschmann, D, Lemke, M, et al. Covid-19 pandemic: anxiety experience of resident and hospital psychiatrists. Fortschr Neurol Psychiatr. (2022) 90:30–6. doi: 10.1055/A-1562-1893
29. Pollock, A, Campbell, P, Cheyne, J, Cowie, J, Davis, B, McCallum, J, et al. Interventions to support the resilience and mental health of frontline health and social care professionals during and after a disease outbreak, epidemic or pandemic: a mixed methods systematic review. Cochrane Database Syst Rev. (2020) 2020:11. doi: 10.1002/14651858.CD013779
Keywords: ambulatory health care system, cancer, COVID-19 pandemic, mental health, SARS-CoV2, tele medicine
Citation: Paffenholz P, Platen M, Kostev K, Loosen SH, Bohlken J and Michalowsky B (2024) Medical care services provision and stress experience in urologists during all waves of the COVID-19 pandemic in Germany. Front. Med. 11:1320489. doi: 10.3389/fmed.2024.1320489
Edited by:
Redhwan Ahmed Al-Naggar, National University of Malaysia, MalaysiaReviewed by:
Vladyslav Sikora, University of Foggia, ItalyKomal Marwaha, Texas Tech University Health Sciences Center, United States
Copyright © 2024 Paffenholz, Platen, Kostev, Loosen, Bohlken and Michalowsky. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sven H. Loosen, U3Zlbi5Mb29zZW5AbWVkLnVuaS1kdWVzc2VsZG9yZi5kZQ==
 Pia Paffenholz
Pia Paffenholz Moritz Platen
Moritz Platen Karel Kostev
Karel Kostev Sven H. Loosen
Sven H. Loosen Jens Bohlken5
Jens Bohlken5 Bernhard Michalowsky
Bernhard Michalowsky