
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
GENERAL COMMENTARY article
Front. Med., 25 January 2024
Sec. Family Medicine and Primary Care
Volume 11 - 2024 | https://doi.org/10.3389/fmed.2024.1259449
This article is part of the Research TopicPatient Safety and Patient-Centred Care in Emergency Medical Services and Adjoining Care SettingsView all 9 articles
This article is a commentary on:
Commentary: Correlation of prefrontal cortical activation with changing vehicle speeds in actual driving: a vector-based functional near-infrared spectroscopy study
A Commentary on
Predicting patient deterioration by nurse intuition: The development and validation of the nurse intuition patient deterioration scale
by Haegdorens, F., Wils, C., and Franck, E. (2023). Int. J. Nurs. Stud. 142:104467. doi: 10.1016/j.ijnurstu.2023.104467
Serious adverse outcomes in patients can be avoided by early detection and response to clinical and physiological deterioration (1), and nurses play an important role in recognizing patient deterioration (2). Nurses typically make decisions based on patient's vital signs, such as heart rate, pulse, and blood pressure, rather than their intuition (3). Recently, Haegdorens et al. developed and validated the Nurse Intuition Patient Deterioration Scale (NIPDS), which was published in the International Journal of Nursing Studies (4). This scale includes nine aspects of patients' conditions (oral expression ability, self-feeling, facial expressions, consciousness, abnormal behavior, skin color, responsiveness, and gaze), which nurses rated using one of the three response categories ranging from zero (not present) to two (very present), with a total score ranging from zero to 18. When the overall score was ≥5, patients were categorized as being at high risk. It demanded additional attention and an immediate response from those equipped to assess and treat critically ill patients. The nurses might have used the NIPDS to identify possible problems in patients even when vital signs did not meet the trigger threshold and other warning tools produced negative results. Although the authors claimed that the NIPDS outperformed the National Early Warning Scale (NEWS) (4), it was disputed whether the scale established on intuition could be used in the clinic. We thus discussed the evaluation indicators in the NIPDS by comparing multiple scales in anticipation of better refining and promoting the NIPDS.
Previous researchers have created a number of warning measures to detect early deterioration in patients' conditions (Figure 1). The NEWS was recognized as one of the most important clinical decision-making devices based on vital signs and was developed by the Royal College of Physicians (RCP) in the United Kingdom (5, 6). Studies showed that the NEWS had been recommended and implemented to enhance patient safety by grading acute illness severity and detecting patient deterioration (7, 8). Compared to the NIPDS, the NEWS had the following weaknesses. First, the NEWS could not express subtle clinical symptoms or changes in patients, so the scale was inapplicable in some cases where patients might have an acute ailment that did not always significantly interfere with vital signs in relation to their need for urgent care. For example, a patient with acute myocardial infarction might present with a NEWS < 5, but he had other signs and symptoms that required emergency care. Furthermore, the NEWS could generate a large number of false-positive patients and an additional workload for clinicians (9). Another warning tool is the Dutch-Early-Nurse-Worry-Indicator-Score (DENWIS), which is based on the concern of nurses about patients and comprises nine indicators (breathing, circulation, rigors, mentation, agitation, pain, unexpected trajectory, patients' feelings, and nurses' subjective observations) (10). Although studies showed that the DENWIS performed well in predicting unplanned admission to the intensive care unit and unexpected mortality (11, 12), the score indicators might be explained in various ways, so the nurses would cause doubt in the process of assessing. The next 5-level warning tool, the Worry Factor Score (WFS), was graded by the concern of nurses. A score of 0 or 1 indicated that the nurses did not believe the patient was actively deteriorating, but a score >1 suggested that the nurses' concern about patient deterioration had increased (13). This score revealed a great effect in predicting rapid response team calls, transfer to the intensive care unit, and resuscitation calls (13). Nonetheless, the WFS might be assessed differently by nurses if they were working without any clinical clues to guide them. Furthermore, other existing early warning scales, such as the Modified Early Warning Score (MEWS), Rapid Emergency Medicine Score (REMS), Acute Physiology and Chronic Health Evaluation II (APACHE II), Oxford Acute Severity of Illness Score (OASIS), and Multiple Organ Dysfunction Score (MODS), were based on the patient's objective deterioration and ignored the medical staff's subjective judgment (Table 1). Most encouragingly, Haegdorens et al. developed a high-quality and practicable instrument called NIPDS. Nevertheless, the writers might have overlooked something beyond intuition.
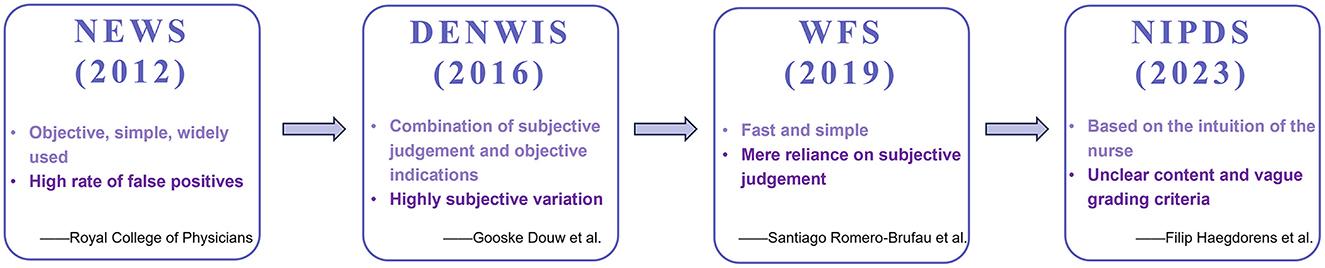
Figure 1. Time–axis plot of various caring scales. NEWS, National Early Warning Scale; DENWIS, Dutch-Early-Nurse-Worry-Indicator-Score; WFS, Worry Factor Score; NIPDS, Nurse Intuition Patient Deterioration Scale.
However, other concerns have to be addressed. First and foremost, the authors did not clearly differentiate between “1-present” and “2-very present.” According to Benner et al., nurse intuition is “a judgment without a rationale, a direct apprehension, and response without recourse to calculative rationality” (14), which cannot be defined and was influenced by factors such as years of work, ward environment, experience, and educational level (15, 16). As a result, if authors are unable to establish objective standards for defining “present” and “very present,” nurses will be unable to use the NIPDS to make appropriate judgments about patients. Second, we believe some items that might confuse nurses need to be updated and enhanced. For instance, the second item's description was inadequate, with no objective indicators. As a result, assessing patients' feelings was challenging, especially for those with communication and consciousness difficulties. Furthermore, in item 7, the change in skin color was a continual process that was not always typical in some circumstances. It was particularly unsuited for the black race and might have been influenced by the natural skin color, making it difficult to observe. The problems mentioned above had the potential to exacerbate the wide difference in final grading results and to impair the judgment of nurses in real-life practice. Additionally, NIPDS measurement data were only acquired from one hospital, so the small sample size may have reduced the accuracy and dependability. The widespread adoption of hospitals in other nations and regions, such as the NEWS, would increase the validity and influence of the scale (17). Finally, the NIPDS validation is insufficient. When evaluating the NIPDS, the writers only used the NEWS. In reality, patient deterioration is assessed using scales such as MEWS, OASIS, MODS, REMS, and APACHE II (Table 1). As a result, the NIPDS should be compared to numerous scales in a variety of clinical situations to provide a more objective and realistic assessment.
Previous studies have shown that vital signs, urine output, and pain are essential indicators of the condition of patients (18, 19). However, the NIPDS was not integrated with the aforementioned indicators. Patients would be at risk of undetected clinical change if vital signs were ignored (20). Of course, it was not advisable to focus only on vital signs and ignore the subjective judgment and intuition of nurses. As a result, we would recommend an approach that combines the NIPDS and the NEWS. In other words, it assesses patient deterioration based on the intuition of nurses and scores numerous physiological markers at the same time. Furthermore, to determine whether the NIPDS was more effective than other scales, the NIPDS should be prospectively validated in other hospitals, healthcare systems, patient categories, and wards as soon as possible during the validation phase. We highly valued the authors' original and novel thoughts. However, using nursing intuition to anticipate patient deterioration requires more research.
FZ: Writing—original draft. JZ: Writing—original draft, Writing—review & editing. HL: Writing—review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by grants from the Special Fund for Youth of Applied Foundational Research Program of Qingdao (No. 19-6-2-43-cg).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Siv KS, Sturle G, Tine L, Irene R, Anners L. The experiences of nurses implementing the modified early warning score and a 24-hour on-call mobile intensive care nurse: an exploratory study. Inten Crit Care Nurs. (2016) 34:33–41. doi: 10.1016/j.iccn.2015.07.008
2. Massey D, Chaboyer W, Aitken L. Nurses' perceptions of accessing a medical emergency team: a qualitative study. Austral Crit Care. (2014) 27:133–8. doi: 10.1016/j.aucc.2013.11.001
3. Olsen SL, Søreide E, Hillman K, Hansen BS. Succeeding with rapid response systems - a never-ending process: a systematic review of how health-care professionals perceive facilitators and barriers within the limbs of the RRS. Resuscitation. (2019) 144:75–90. doi: 10.1016/j.resuscitation.2019.08.034
4. Haegdorens F, Wils C, Franck E. Predicting patient deterioration by nurse intuition: the development and validation of the nurse intuition patient deterioration scale. Int J Nurs Stud. (2023) 142:104467. doi: 10.1016/j.ijnurstu.2023.104467
5. Endo T, Khoujah D, Motohashi T, Shinozaki T, Tsushima K, Fujitani S, et al. The national early warning score on admission predicts severe disease and in-hospital mortality of the coronavirus disease 2019 delta variant: a retrospective cohort study. Acute Med Surg. (2023) 10:e851. doi: 10.1002/ams2.851
6. Langkjaer CS, Bundgaard K, Bunkenborg G, Nielsen PB, Iversen KK, Bestle MH, et al. How nurses use national early warning score and individual early warning score to support their patient risk assessment practice: a fieldwork study. J Adv Nurs. (2023) 79:789–97. doi: 10.1111/jan.15547
7. McGinley A, Pearse RM. A national early warning score for acutely ill patients. BMJ. (2012) 345:e5310. doi: 10.1136/bmj.e5310
8. Bavalia R, Stals MAM, Mulder FI, Bistervels IM, Coppens M, Faber LM, et al. Use of the national early warning score for predicting deterioration of patients with acute pulmonary embolism: a post-hoc analysis of the years study. Emerg Med J. (2023) 40:61–6. doi: 10.1136/emermed-2021-211506
9. Haegdorens F, Monsieurs KG, De Meester K, Van Bogaert P. The optimal threshold for prompt clinical review: an external validation study of the national early warning score. J Clin Nurs. (2020) 29:4594–603. doi: 10.1111/jocn.15493
10. Douw G, Schoonhoven L, Holwerda T, Huisman-de Waal G, van Zanten AR, van Achterberg T, et al. Nurses' worry or concern and early recognition of deteriorating patients on general wards in acute care hospitals: a systematic review. Crit Care. (2015) 19:230. doi: 10.1186/s13054-015-0950-5
11. Douw G, Huisman-de Waal G, van Zanten AR, van der Hoeven JG, Schoonhoven L. Nurses' ‘worry' as predictor of deteriorating surgical ward patients: a prospective cohort study of the dutch-early-nurse-worry-indicator-score. Int J Nurs Stud. (2016) 59:134–40. doi: 10.1016/j.ijnurstu.2016.04.006
12. Douw G, Huisman-de Waal G, van Zanten ARH, van der Hoeven JG, Schoonhoven L. Capturing early signs of deterioration: the dutch-early-nurse-worry-indicator-score and its value in the rapid response system. J Clin Nurs. (2017) 26:2605–13. doi: 10.1111/jocn.13648
13. Romero-Brufau S, Gaines K, Nicolas CT, Johnson MG, Hickman J, Huddleston JM. The fifth vital sign? Nurse worry predicts inpatient deterioration within 24 hours. JAMIA Open. (2019) 2:465–70. doi: 10.1093/jamiaopen/ooz033
14. Leslie N-B. Book Review: Benner P, Tanner C, Chesla C, Expertise in Nursing Practice: Caring, Clinical Judgment, and Ethics, Second Edition, Springer Publishing: New York, 2009, 497 Pp.: 9780826125446, Us\$60.00 (Pbk). Nurs Ethics. (2010) 17:675. doi: 10.1177/0969733010376334
15. Bogossian F, Cooper S, Cant R, Beauchamp A, Porter J, Kain V, et al. Undergraduate nursing students' performance in recognising and responding to sudden patient deterioration in high psychological fidelity simulated environments: an australian multi-centre study. Nurse Educ Today. (2014) 34:691–6. doi: 10.1016/j.nedt.2013.09.015
16. Odell M, Victor C, Oliver D. Nurses' role in detecting deterioration in ward patients: systematic literature review. J Adv Nurs. (2009) 65:1992–2006. doi: 10.1111/j.1365-2648.2009.05109.x
17. Williams B. The national early warning score: from concept to NHS implementation. Clin Med. (2022) 22:499–505. doi: 10.7861/clinmed.2022-news-concept
18. Burdeu G, Lowe G, Rasmussen B, Considine J. Clinical cues used by nurses to recognize changes in patients' clinical states: a systematic review. Nurs Health Sci. (2021) 23:9–28. doi: 10.1111/nhs.12778
19. Gondim ÉS, Gomes EB, Matos JHF, Pinto SL, Oliveira CJ, Alencar A. Technologies used by nursing to predict clinical deterioration in hospitalized adults: a scoping review. Rev Bras Enferm. (2022) 75:e20210570. doi: 10.1590/0034-7167-2021-0570
Keywords: nurse intuition, patient deterioration, scale development, predict, NEWS
Citation: Zhao F, Zhao J and Liu H (2024) Commentary: Predicting patient deterioration by nurse intuition: the development and validation of the Nurse Intuition Patient Deterioration Scale. Front. Med. 11:1259449. doi: 10.3389/fmed.2024.1259449
Received: 27 July 2023; Accepted: 05 January 2024;
Published: 25 January 2024.
Edited by:
Benedikt Treml, Innsbruck Medical University, AustriaReviewed by:
Antonio Bonacaro, University of Parma, ItalyCopyright © 2024 Zhao, Zhao and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Heng Liu, aGVuZ2xpdUBxZHUuZWR1LmNu
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.