
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Med. , 15 November 2023
Sec. Intensive Care Medicine and Anesthesiology
Volume 10 - 2023 | https://doi.org/10.3389/fmed.2023.1280013
Background: Postoperative cognitive dysfunction (POCD) is a postoperative complication that often occurs in the elderly. This systematic review and meta-analysis aimed to compare intravenous anesthetics (propofol) with inhalation anesthetics (sevoflurane) regarding the occurrence of POCD in the elderly who underwent non-cardiac surgery.
Methods: The investigators searched for published articles from the PubMed, Embase, Web of Science, Scopus, Cochrane, and Clinicalkey databases. Clinical studies comparing the incidence of POCD in elderly patients undergoing intravenous or inhalation anesthesia in general were selected. Primary outcomes included the occurrence of POCD at 1, 3, and 7 days. The secondary outcomes were the patient’s plasma S-100β protein levels (pg*mL−1) and delayed neurocognitive recovery incidence 5–7 days after surgery.
Results: Fifteen studies including 3,817 patients were enrolled in the systematic review. Ten studies involving 1,829 patients were enrolled in the meta-analysis. The results demonstrate that there was no difference between the intravenous and inhalation groups in the incidence of POCD within 1–7 days (95% CI 0.73–1.26, p = 0.77) and the occurrence of delayed neurocognitive recovery 5–7 days after surgery (95% CI −353.15 to −295.44, p = 0.28). Plasma S-100β protein levels in the intravenous anesthesia group were lower than those in the inhalation group (95% CI 0.48–1.24, p < 0.001).
Conclusion: For elderly patients undergoing non-cardiac surgery, inhalation anesthesia was comparable to intravenous anesthesia in terms of the occurrence of short-term POCD. Inhalation anesthesia may cause greater damage to the nervous system, with delayed recovery of cognitive function after 5–7 days showing no difference.
Systematic review: identifier (CRD42021251317).
Among patients undergoing surgery, the proportion of older people is gradually increasing. Compared with adults, elderly patients are more likely to have postoperative cognitive dysfunction (POCD). Age is a risk factor for patients with (POCD) (1–3). The study by Kotekar et al. (4) found that the incidence of POCD was significantly greater in the 71–80-year-old group than in the 61–70-year-old group, while the rate of POCD in the 80-year-old group could reach 100%. POCD can severely impact the length of hospital stay and increase morbidity and mortality, especially in elderly patients undergoing surgery under general anesthesia (1, 2, 5–7). In non-cardiac surgery, older patients are at high risk for POCD. In non-cardiac surgery, 25–56% of older patients are affected by POCD in the first week after surgery (8).
The mechanism of POCD is currently unknown, and the effects of anesthesia on the occurrence of POCD during general anesthesia have been progressively realized (9). Sevoflurane, as a commonly used inhaled anesthetic, is believed to increase the incidence of POCD in older patients (10). Most recent animal experiments have focused on the effects of inhaled anesthetics on neurological function (11, 12), and the results of these seem to be unfavorable for the use of inhaled anesthetics in elderly patients (13). However, results from a number of studies have shown that sevoflurane intervention does not impair learning and memory. In some studies (14–16), it has been pointed out that intravenous and inhaled anesthetics have a neuroprotective effect in brain injury.
Currently, clinical studies on the impact of inhaled and intravenous anesthetics on the occurrence of POCD in older adults are relatively common, but a multi-center randomized controlled trial (RCT) (3) published in 2021 further investigated this controversial issue. After our search, however, there is no meta-analysis of studies published after 2018 on this topic. Therefore, we believe that a new study of this issue, in conjunction with recent clinical studies, is warranted. The purpose of this study is to conduct a systematic evaluation and meta-analysis to compare the effects of intravenous anesthetics (propofol) and inhalation anesthetics (sevoflurane) on the occurrence of POCD due to non-cardiac surgery in the elderly.
Our research has been registered with PROSPERO under registration number CRD42021251317. The systematic review and meta-analysis were performed according to Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines. We followed the PRISMA checklist to complete the meta-analysis. The researchers searched for articles published before 18 April in the PubMed, Embase, Web of Science, Scopus, Cochrane, and Clinicalkey databases. The search terms were: (cognition OR cognitive disorder OR cognitive deficit OR cognitive impairment OR cognitive function impairment OR cognitive dysfunction) AND (elderly patients OR aged OR the aged OR old people OR the elderly OR elder OR agedness) AND (volatile anesthetic OR inhalation anesthetic OR sevoflurane OR inhaled anesthetics OR inhalational anesthetic OR intravenous anesthetic OR TIVA OR total intravenous anesthesia OR propofol OR general anesthesia). The restrictive conditions for all search formulae were to search for titles, abstracts, and keywords. We had no restrictions on language. The searched literature was managed with EndNote X9 (Thomson Reuters, NY, United States). After excluding duplicates and non-clinical studies, the titles and abstracts were screened by the researcher. Finally, the researchers determined the included literature based on the full text. In addition, POCD did not include postoperative delirium in this study.
The studies included in the meta-analysis must meet the following criteria: clinical studies, comparison of intravenous anesthesia (propofol) and inhalation anesthesia in general (sevoflurane), and elderly patients receiving noncardiac surgery. Studies with the following characteristics were excluded: animal studies, study protocol, reviews, guidelines, conference abstract, without control, and different from inclusion criteria (not the elderly, different interventions, etc.).
The investigators used the Cochrane collaboration tool to obtain the overall bias of the included studies and used RevMan 5.3 (Review Manager. Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.) to make a risk of bias graph and summary.
We extracted the characteristics of the included studies, including source, location of study, year of publication, design, eligible population, operations, study period, and number of patients. The patient and intervention characteristics of the studies were evaluated in the meta-analysis. The data for the meta-analysis were extracted by L.L.H. and checked with Y.Z.
The primary outcome of this meta-analysis was the incidence of postoperative cognitive dysfunction (POCD) at 1, 3, and 7 days. The secondary outcomes were the patient’s plasma S-100β protein levels (pg*ml−1) and delayed neurocognitive recovery incidence 5–7 days after surgery.
RevMan 5.3 was used for all data analysis in this study. The inverse variance random effects model was used to analyze continuous variables and expressed as the mean difference (MD) of the 95% confidence interval (CI). For binary variables, we reported the odds ratios (OR) and used the Mantel–Haenszel method for analysis. For the data with p < 0.05 or I (2)>50% for heterogeneity detection, the random-effect model was used for analysis, while data with p > 0.05 or I (2)≤50% were selected for the fixed-effect model. If only one study is included, the fixed-effect model is also selected. For the results with high heterogeneity [I (2)≤75%], we conducted a sensitivity analysis to exclude studies with high heterogeneity. Moreover, we performed a subgroup analysis to assess the incidence of POCD in different time periods. The intravenous group was the reference group for OR calculations.
By searching the PubMed, Embase, Web of Science, Scopus, Cochrane, and Clinicalkey databases for literature titles, abstracts, and keywords, 6,458 articles were obtained. We used EndNote X9 to find duplicates, leaving 5,412 articles and preserving 947 clinical trials. The abstracts and titles of the remaining studies were screened, and 99 were related to intravenous anesthesia, inhaled anesthesia, or elderly patients. Through the screening of the full text of these studies, 15 included studies were finally determined (Study protocol: 7; Without control: 6; Different inclusion criteria: 70). The literature retrieval process is illustrated in Figure 1. Of the 15 included studies, we screened 11 for meta-analysis that included both primary and secondary outcomes.
We summarize the included studies’ characteristics in Table 1, including a total of 15 studies and 3,817 patients. Among these, 3,652 patients in 12 studies were from China [Shanghai (17–19), Jiaxing (5), Harbin (20), Guangxi (21), Guangdong (3), Jiangxi (22), Shandong (10), Chengdu (23), Beijing (24), and Shenzhen (25)], and the other three were from the USA (Kentucky) (26), Japan (Sapporo) (27), and Greece (28). Moreover, there were 13 studies published after 2015. Among the included studies, only one (22) was a retrospective study, and the rest were RCTs. Among the RCTs, four studies (10, 20, 21, 23) were double-blind and one was a multi-center study (3). All patients underwent non-cardiac surgery.
In the meta-analysis stage, we excluded five studies lacking outcome indicators and only evaluated 1,829 patients in 10 studies (all RCTs). Table 2 shows the characteristics of the patients in the evaluated studies. Only the study by Geng et al. (20) did not report the age of the patients, and the mean or median age of all other patients was >64 years. Six studies reported on BMI and there were no obese patients (BMI ≥ 30 kg/m−2). Only in three studies did the number of female patients exceed the number of male patients. The studies by Geng et al. (20) and Guo et al. (21) did not include ASA I patients, while the study by Nishikawa et al. did not include ASA III patients. In the study by Rohan et al. (26), the duration of anesthesia was the shortest, and in Zhang et al. (24) it was the longest. Qiao et al. (10) did not report it.
We summarize the intervention characteristics of the evaluated studies in Table 3. Of the 10 studies evaluated, four selected different narcotic induction methods in groups P and S, respectively. In the study by Liu et al. (17), 1.5 mg/kg propofol +2 μg/kg remifentanil +0.1 mg/kg vecuronium bromide intravenous was chosen in group P and 2 mg/kg propofol +2 μg/kg remifentanil +0.1 mg/kg vecuronium bromide in group S. In the study of Nishikawa et al. (27), a targeted propofol concentration of 4 mg/mL using a computer-assisted TCI system was chosen in group P and 5% sevoflurane and 100% oxygen at 6 L / min until the inspired-limb drug concentration was >4% in group S. Rohan et al. (26) used target concentrations of propofol that were adjusted to maintain adequate depth of anesthesia in group P and the incremental dose, tidal volume inhalation induction technique in group S. Tang et al. (23) used a standard induction protocol: midazolam (0.03–0.04 mg/kg, i.v.), fentanyl (0.002–0.003 mg/kg, i.v.), and vecuronium (0.15–0.2 mg/kg, i.v.), and chose propofol (1.5–2.0 mg/kg, i.v.) in group P and 8% sevoflurane (FGF 6 L/min, inhalation, decreased after loss of consciousness to 3–4%, FGF 1–2 L/min) in group S.
Ten studies selected different methods of anesthesia maintenance. Geng et al. (20) used propofol (target concentration 2.5–3.0 μg·mL−1) and remifentanil (0.2–0.3 μg·kg−1·min−1) in group P, and sevoflurane (1.0–1.5 MAC) and remifentanil (0.2–0.3 μg·kg−1·min−1) in group S. Guo et al. (21) chose sufentanil and rocuronium with propofol or sevoflurane. Li et al. (3) used remifentanil (0.1–0.5 μg · kg−1 · min−1) with intravenous propofol infusion (50–150 μg · kg−1 ·min−1) or sevoflurane (1.0–1.5 MAC). Glucocorticoids, nonsteroidal analgesics, and dexmedetomidine were avoided during surgery. Mei et al. (18) used propofol (629.8 ± 255.0 mg) by TCI or 1–4% sevoflurane. Nishikawa et al. (27) chose anesthesia maintenance combined with continuous epidural analgesia with 1.5% lidocaine (4–6 mL/h). Qiao et al. (10) used an intravenous infusion of remifentanil (commenced at 0.15 μg/kg/min) and a 5-mg bolus of cisatracurium besylate was administered every 30 min according to clinical need with propofol administered by TCI (effect site concentration 4 μg/mL) or sevoflurane (1MAC). Tang et al. (23) chose remifentanil (9–12 mg/kg per h, continuous i.v. infusion) and vecuronium (intermittent i.v. infusion) with propofol (6–10 mg/kg per h) or sevoflurane (2–3%). Zhang et al. (24) used remifentanil (sufentanil) and rocuronium (cisatracurium) with propofol infusion or inhaled sevoflurane.
We used RevMan 5.3 to summarize the bias of the included studies as shown in Figures 2, 3. It is denoted as high-risk, low-risk, or unclear. Of the 14 studies included in the risk of bias assessment, one (22) was a retrospective study with a high overall risk of bias. Eight studies mentioned random sequence generation methods, and seven described how to mask assignments. Six of the studies did not blind investigators and patients, and the outcome assessment was not blinded in four.
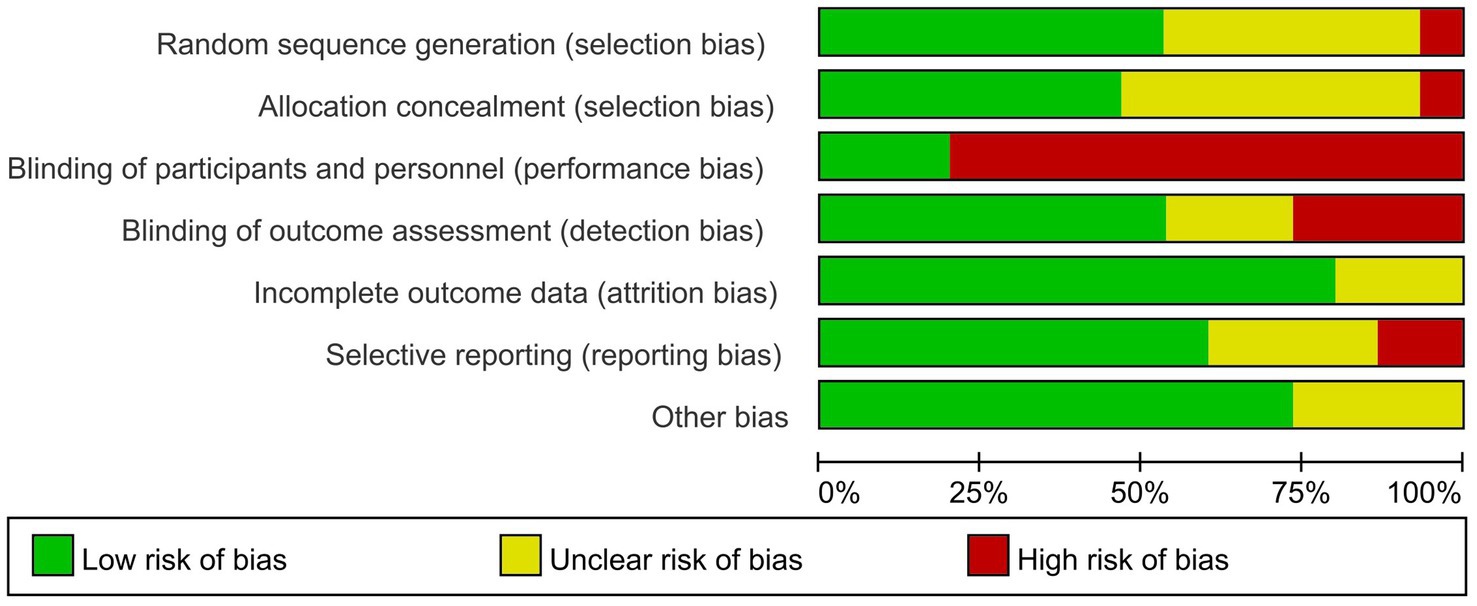
Figure 2. Risk of bias graph: review authors’ judgments about each risk of bias item presented as percentages across all included studies.
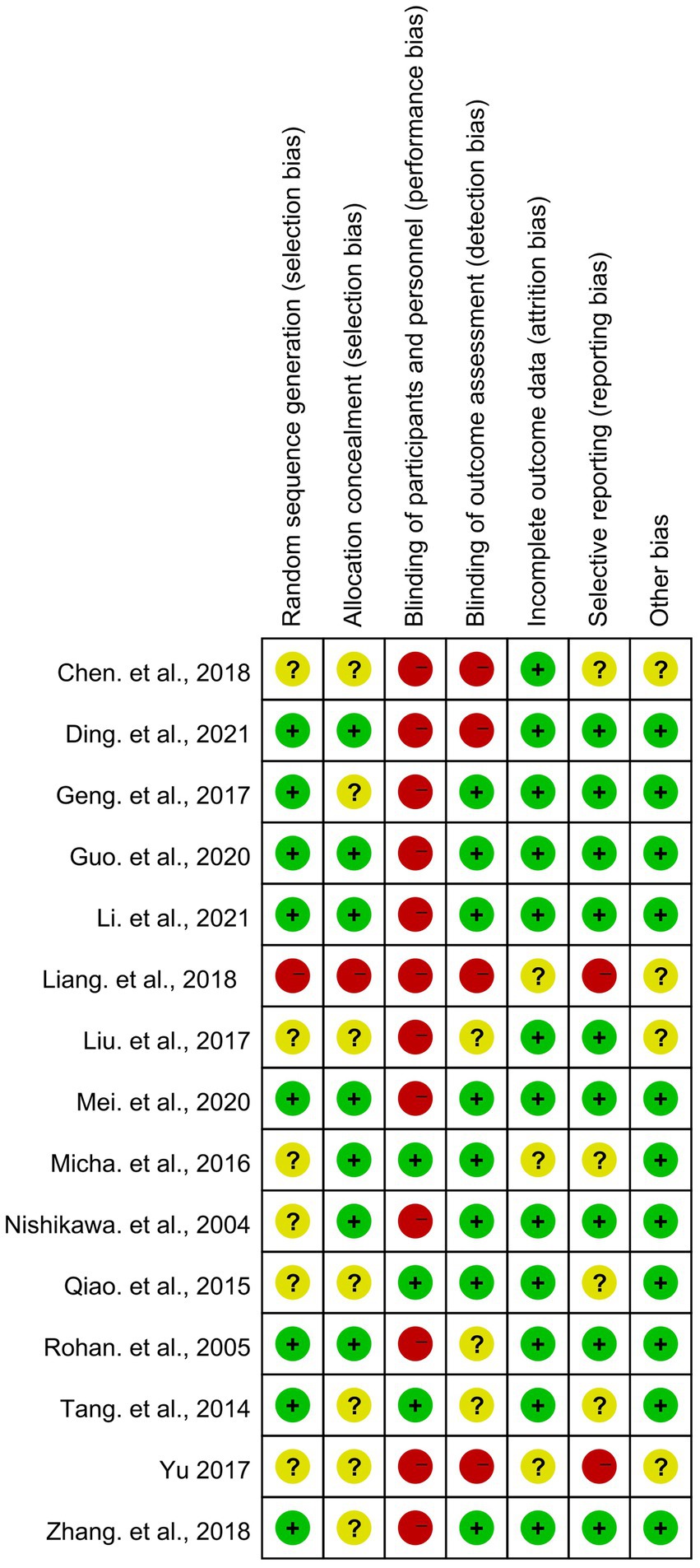
Figure 3. Risk of bias summary: review authors’ judgments about each risk of bias item for each included study.
The incidence of POCD at 1 day was reported in a sample size of 192. Across three studies (17, 26, 27), the incidence of POCD at 1 day was 3, 0, and 7 in the intravenous anesthesia group. The incidence of POCD at 1 day was 1, 0, and 7 in the inhalation anesthesia group. The pooled OR (95% CI) of it was 1.43 (95% CI 0.44–4.65), I (2) = 0%, n = 3 (Figure 4). Using a fixed-effects model, the result was not statistically significant (p = 0.55).
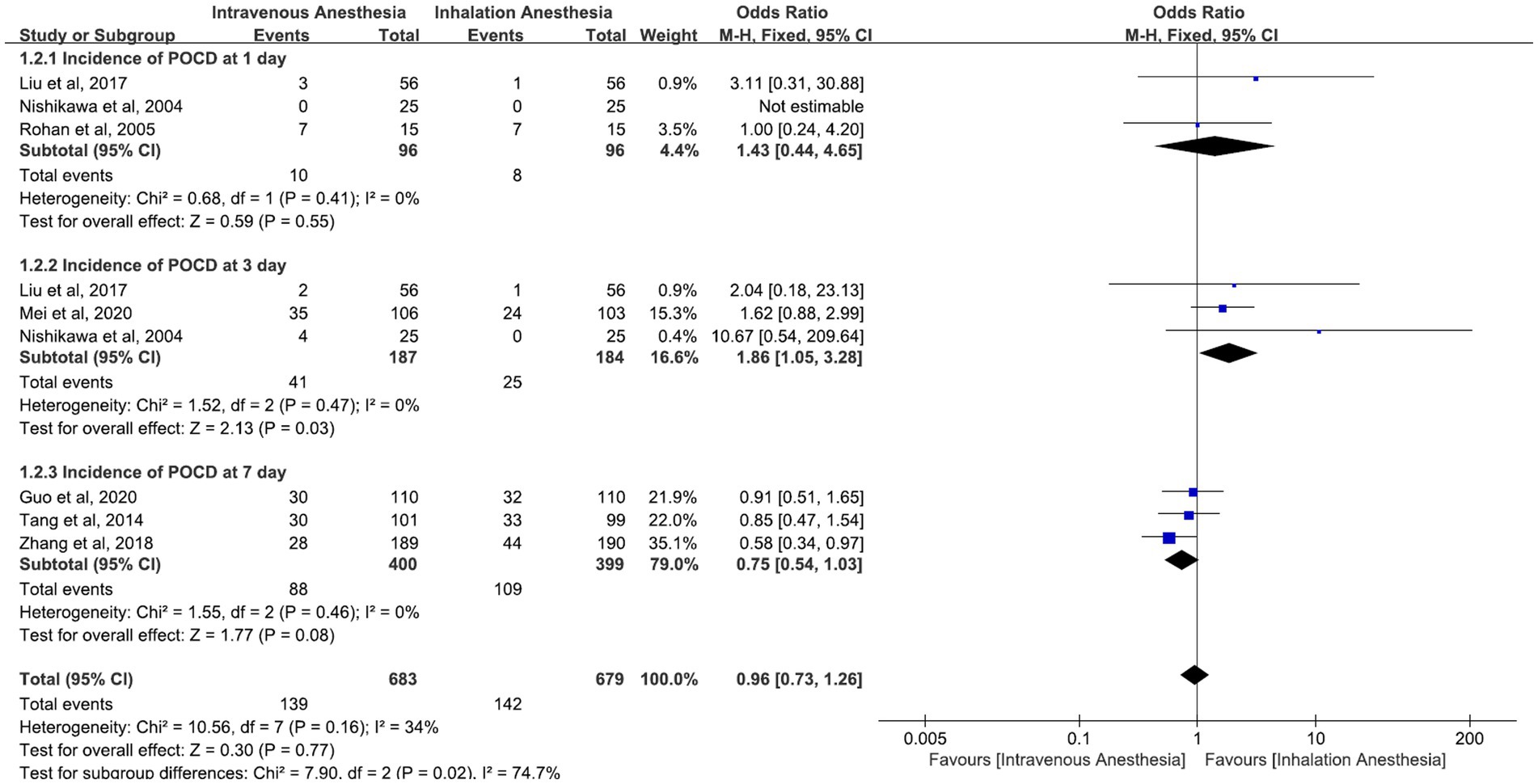
Figure 4. Incidence of POCD at 1–7 days postoperative comparison between intravenous anesthesia and inhalation anesthesia.
Studies reported the incidence of POCD at 3 days with a sample size of 371. Across three studies (17, 18, 27), the incidence of POCD at 3 days was 2,35, and 4 in the intravenous anesthesia group. The incidence of POCD at 3 days was 1, 24, and 0 in the inhalation anesthesia group. The pooled OR (95% CI) of it was 1.86 (95% CI 1.05–3.28), I (2) = 0%, n = 3 (Figure 4). Using a fixed-effects model, the result was statistically significant (p = 0.03).
Studies reported the incidence of POCD at 7 days with a sample size of 821. Across three studies (21, 23, 24), the incidence of POCD at 7 days was 30, 30, and 28 in the intravenous anesthesia group. The incidence of POCD at 7 days was 32, 33, and 44 in the inhalation anesthesia group. The pooled OR (95% CI) of it was 0.75 (95% CI 0.54 to 1.03), I (2)= 0%, n = 3 (Figure 4). Using a fixed-effects model, the result is not statistically significant (p = 0.08).
Studies reported the incidence of POCD at 1, 3, and 7 days with a sample size of 1,222. The pooled OR (95% CI) of it was 0.96 (95% CI 0.73 to 1.26), I (2) = 34%, n = 7 (Figure 4). Using a fixed-effects model, the result was not statistically significant (p = 0.77). The subgroup differences were statistically significant (p = 0.02).
In two studies (10, 26), the plasma S-100β protein level (pg*mL−1) in the intravenous anesthesia group was 1867.93 ± 50.51 (Mean ± SD) and 1,100 ± 400 (Mean ± SD). The plasma S-100β protein level in the inhalation anesthesia group was 2194.28 ± 63.72 (Mean ± SD), and 1,300 ± 200 (Mean ± SD). The pooled MD (95% CI) of the plasma S-100β protein levels was −324.30 (95% CI −353.15 to −295.44) in favor of the intravenous anesthesia group, I (2)= 15%, n = 2 (Figure 5). Using a fixed-effects model, the result was statistically significant (P < 0.00001).
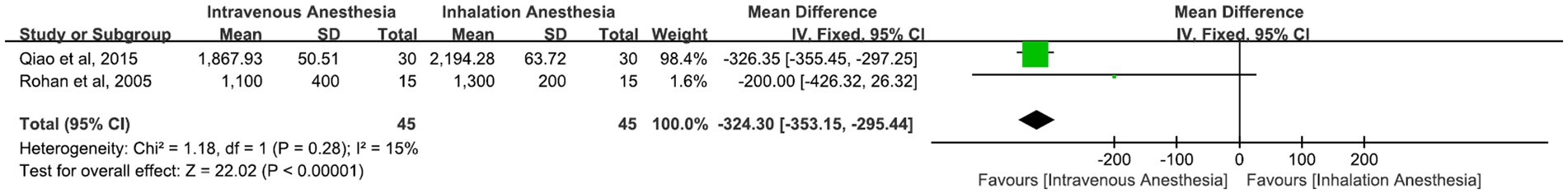
Figure 5. Plasma S-100β protein levels (pg*mL−1) postoperative comparison between intravenous anesthesia and inhalation anesthesia.
In one study (3), the delayed neurocognitive recovery incidence 5–7 days after surgery in the intravenous anesthesia group was 38 and 46 in the inhalation anesthesia group. The pooled OR (95% CI) of it was 0.77 (95% CI 0.48–1.24), n = 1 (Figure 6). Using a fixed-effects model, the result was not statistically significant (p = 0.28).
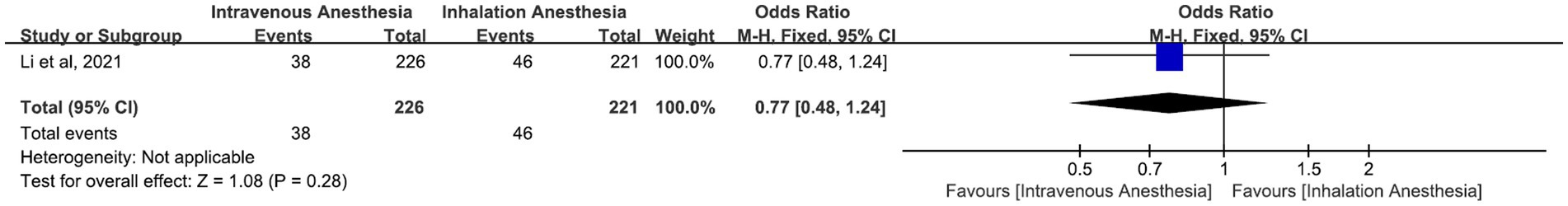
Figure 6. Delayed neurocognitive recovery incidence 5–7 days after surgery comparison between intravenous anesthesia and inhalation anesthesia.
We conducted a systematic review of 15 studies and a meta-analysis of 1,827 patients in 10 RCTs. Our results indicate that there was no significant difference between intravenous and inhaled anesthesia in the occurrence of POCD within 1–7 days and the incidence of delayed neurocognitive recovery 5–7 days after surgery. The plasma S-100β protein levels in the intravenous anesthesia group were lower than those in the inhalation anesthesia group.
The use of anesthetics has been a controversial topic and this review will provide an opinion on the choice of anesthetics for non-cardiac surgery in elderly patients. In our review and meta-analysis, sevoflurane was used to maintain anesthesia in the inhalation anesthesia group. We excluded desflurane and isoflurane considering that sevoflurane is preferred for induction or maintenance of anesthesia in most cases. At this point, our design differs from that of Miller et al. (29). Our results show that there was no significant difference between intravenous and inhalation anesthesia in the occurrence of POCD within 1–7 days after surgery. Moreover, the inhalation anesthesia group was better than the intravenous anesthesia group 3 days after surgery. This result was different from what we expected. This is because, according to previous studies (10, 20, 30, 31) and opinions, inhaled anesthetics will increase the risk of POCD in elderly patients. The reason for this difference may be related to the method of surgery, duration of anesthesia, and pre-operative medications. In a study favoring intravenous anesthesia, Qiao et al. (10) targeted elderly patients undergoing major surgery. The study by Geng et al. (20) was excluded from the sensitivity test due to significant heterogeneity. Furthermore, the conclusions of some recent studies can support our results. In a multicenter RCT designed by Li et al. (3), it was pointed out that the choice between propofol and sevoflurane did not affect the occurrence of POCD in elderly patients after laparoscopic surgery. Guo et al. (21) concluded in a double-blind RCT that sevoflurane did not significantly increase the incidence of POCD at 7 days and 3 months after surgery compared to propofol. In a study published in 2016 (32), sevoflurane use was associated with lower rates of POCD than propofol in patients with cerebral hypoxia. Recovery of neurocognitive function is strongly correlated with poor prognosis and the occurrence of adverse events after surgery. Before the study, Li et al. (3) assumed that the incidence of delayed recovery was lower in the propofol group than in the civilian group. They identified the incidence of delayed neurocognitive recovery 5–7 days after surgery as the primary outcome of the RCT. Controversy over the choice of anesthetic for non-cardiac surgery in elderly patients may persist in the context of unclear pathogenesis of POCD. However, without adequate research, it cannot be assumed that inhaled anesthetics are detrimental to a patient’s cognitive function.
S-100β protein has nerve tissue specificity and is a sensitive and specific marker of central nervous system damage (33, 34), especially in the elderly (35). Therefore, we chose the expression level of S-100β protein as an index to judge postoperative cognitive function. A meta-analysis conducted by Sun et al. (36) for postoperative cognitive function in elderly patients with lung cancer also added S-100β as an outcome indicator. Similar to our conclusion, Sun et al. also pointed out that the change in blood oxygen S-100β protein concentration in the sevoflurane group was significantly higher than that in the propofol group with statistical differences. These results all suggest that the use of pseudoephedrine to anesthetize older patients may result in more severe nerve damage and thus a greater risk of POCD than propofol. However, the measurement of S-100β as a laboratory indicator for assessing cognitive function may yield disparate results compared to behavioral studies, thereby accounting for the observed discrepancy in this study.
This meta-analysis has the following limitations. First, few articles were included in the systematic review because we had a rigorous literature screening, restricted the inhalation anesthesia group to intravenous anesthesia, and did not include studies published before 2000. In addition, we excluded studies with low quality and significant heterogeneity through a sensitivity analysis, so that the number of studies included in the meta-analysis was only 10. Second, this meta-analysis did not use the Mini-mental State Examination (MMSE) as an outcome indicator. In fact, we have performed subgroup analysis on the MMSE, but the heterogeneity of each subgroup was significant and the sensitivity analysis was limited. We believe that MMSE is a subjective approach. Also, the educational level, surgical method, and ASA classification of the patients included in each study were different, and most of the studies were from China. Finally, we did not analyze long-term outcomes because most POCD in the included studies occurred within 7 days of surgery. The long-term outcomes of non-cardiac surgical POCD in older patients have yet to be demonstrated.
This systematic review and meta-analysis showed that for elderly patients undergoing non-cardiac surgery, inhalation anesthesia in general was comparable to intravenous anesthesia in terms of the occurrence of short-term POCD. Inhalation anesthesia may cause greater damage to the nervous system, with delayed recovery of cognitive function after 5–7 days showing no difference. Given the limitations of the included studies, we look forward to updating this review with more high-quality RCTs in the future.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
HL: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Writing – original draft. ZY: Project administration, Resources, Writing – review & editing, Supervision, Validation.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-analyses; BMI, Body Mass Index; SD, standard deviation; IQR, Inter Quartile Range; ASA, American Society of Anesthesiologists; TIVA, total intravenous anesthesia; MAC, minimum alveolar concentration; TCI, target-controlled infusion; POCD, postoperative cognitive dysfunction; FGF, fresh gas flow; NR, no record; MMSE, Mini-mental State Examination.
1. Moller, JT, Cluitmans, P, Rasmussen, LS, Houx, P, Rasmussen, H, Canet, J, et al. Long-term postoperative cognitive dysfunction in the elderly ISPOCD1 study. ISPOCD investigators. Lancet. (1998) 351:857–61. doi: 10.1016/S0140-6736(97)07382-0
2. Monk, TG, Weldon, BC, Garvan, CW, Dede, DE, van der Aa, MT, Heilman, KM, et al. Predictors of cognitive dysfunction after major noncardiac surgery. Anesthesiology. (2008) 108:18–30. doi: 10.1097/01.anes.0000296071.19434.1e
3. Li, Y, Chen, D, Wang, H, Wang, Z, Song, F, Li, H, et al. Intravenous versus volatile anesthetic effects on postoperative cognition in elderly patients undergoing laparoscopic abdominal surgery. Anesthesiology. (2021) 134:381–94. doi: 10.1097/ALN.0000000000003680
4. Kotekar, N, Kuruvilla, CS, and Murthy, V. Post-operative cognitive dysfunction in the elderly: a prospective clinical study. Indian J Anaesth. (2014) 58:263–8. doi: 10.4103/0019-5049.135034
5. Chen, X-D, Xie, W, and Zhou, QH. Effect of propofol and sevoflurane on cognitive function among elderly patients undergoing elective surgery under anesthesia. Pak J Pharm Sci. (2018) 31:2909–13.
6. Rasmussen, LS, Larsen, K, Houx, P, Skovgaard, LT, Hanning, CD, and Moller, JT. Dysfunction IgTISoPC: the assessment of postoperative cognitive function. Acta Anaesthesiol Scand. (2001) 45:275–89. doi: 10.1034/j.1399-6576.2001.045003275.x
7. Price, CC, Garvan, CW, and Monk, TG. Type and severity of cognitive decline in older adults after noncardiac surgery. Anesthesiology. (2008) 108:8–17. doi: 10.1097/01.anes.0000296072.02527.18
8. Rasmussen, LS. Postoperative cognitive dysfunction: incidence and prevention. Best Pract Res Clin Anaesthesiol. (2006) 20:315–30. doi: 10.1016/j.bpa.2005.10.011
9. Terrando, N, Eriksson, LI, Ryu, JK, Yang, T, Monaco, C, Feldmann, M, et al. Resolving postoperative neuroinflammation and cognitive decline. Ann Neurol. (2011) 70:986–95. doi: 10.1002/ana.22664
10. Qiao, Y, Feng, H, Zhao, T, Yan, H, Zhang, H, and Zhao, X. Postoperative cognitive dysfunction after inhalational anesthesia in elderly patients undergoing major surgery: the influence of anesthetic technique, cerebral injury and systemic inflammation. BMC Anesthesiol. (2015) 15:154. doi: 10.1186/s12871-015-0130-9
11. Zhang, J, Tan, H, Jiang, W, and Zuo, Z. Amantadine alleviates postoperative cognitive dysfunction possibly by increasing glial cell line-derived neurotrophic factor in rats. Anesthesiology. (2014) 121:773–85. doi: 10.1097/ALN.0000000000000352
12. Zheng, B, Lai, R, Li, J, and Zuo, Z. Critical role of P2X7 receptors in the neuroinflammation and cognitive dysfunction after surgery. Brain Behav Immun. (2017) 61:365–74. doi: 10.1016/j.bbi.2017.01.005
13. Berger, M, Schenning, KJ, CHt, B, Deiner, SG, Whittington, RA, Eckenhoff, RG, et al. Perioperative neurotoxicity working G: best practices for postoperative brain health: recommendations from the fifth international perioperative neurotoxicity working group. Anesth Analg. (2018) 127:1406–13. doi: 10.1213/ANE.0000000000003841
14. Lasarzik, I, Winkelheide, U, Stallmann, S, Orth, C, Schneider, A, Tresch, A, et al. Assessment of postischemic neurogenesis in rats with cerebral ischemia and propofol anesthesia. Anesthesiology. (2009) 110:529–37. doi: 10.1097/ALN.0b013e318195b4fe
15. Zheng, YY, Lan, YP, Tang, HF, and Zhu, SM. Propofol pretreatment attenuates aquaporin-4 over-expression and alleviates cerebral edema after transient focal brain ischemia reperfusion in rats. Anesth Analg. (2008) 107:2009–16. doi: 10.1213/ane.0b013e318187c313
16. Bedirli, N, Bagriacik, EU, Emmez, H, Yilmaz, G, Unal, Y, and Ozkose, Z. Sevoflurane and isoflurane preconditioning provides neuroprotection by inhibition of apoptosis-related mRNA expression in a rat model of focal cerebral ischemia. J Neurosurg Anesthesiol. (2012) 24:336–44. doi: 10.1097/ANA.0b013e318266791e
17. Liu, Q, Liu, CL, Yang, XY, Ji, JW, and Peng, S. Influence of sevoflurane anesthesia on postoperative recovery of the cognitive disorder in elderly patients treated with non-cardiac surgery. Biomed Res. (2017) 28:4107–10.
18. Mei, X, Zheng, H-L, Li, C, Ma, X, Zheng, H, Marcantonio, E, et al. The effects of Propofol and sevoflurane on postoperative delirium in older patients: a randomized clinical trial study. J Alzheimers Dis. (2020) 76:1627–36. doi: 10.3233/JAD-200322
19. Yu, W. Anesthesia with propofol and sevoflurane on postoperative cognitive function of elderly patients undergoing general thoracic surgery. Pak J Pharm Sci. (2017) 30:1107–10.
20. Geng, YJ, Wu, QH, and Zhang, RQ. Effect of propofol, sevoflurane, and isoflurane on postoperative cognitive dysfunction following laparoscopic cholecystectomy in elderly patients: a randomized controlled trial. J Clin Anesth. (2017) 38:165–71. doi: 10.1016/j.jclinane.2017.02.007
21. Guo, L, Lin, F, Dai, H, Du, X, Yu, M, Zhang, J, et al. Impact of sevoflurane versus Propofol anesthesia on post-operative cognitive dysfunction in elderly Cancer patients: a double-blinded randomized controlled trial. Med Sci Monit. (2020) 26:e919293. doi: 10.12659/MSM.919293
22. Liang, LQ, Jiao, YQ, and Guo, SL. Effects of sevoflurane inhalation anesthesia on cognitive and immune function in elderly patients after abdominal operation. Eur Rev Med Pharmacol Sci. (2018) 22:8932–8. doi: 10.26355/eurrev_201812_16663
23. Tang, N, Ou, C, Liu, Y, Zuo, Y, and Bai, Y. Effect of inhalational anaesthetic on postoperative cognitive dysfunction following radical rectal resection in elderly patients with mild cognitive impairment. J Int Med Res. (2014) 42:1252–61. doi: 10.1177/0300060514549781
24. Zhang, Y, Shan, GJ, Zhang, YX, Cao, SJ, Zhu, SN, Li, HJ, et al. Propofol compared with sevoflurane general anaesthesia is associated with decreased delayed neurocognitive recovery in older adults. Br J Anaesth. (2018) 121:595–604. doi: 10.1016/j.bja.2018.05.059
25. Ding, F, Wang, X, Zhang, L, Li, J, Liu, F, and Wang, L. Effect of propofol-based total intravenous anaesthesia on postoperative cognitive function and sleep quality in elderly patients. Int J Clin Pract. (2021) 75:e14266. doi: 10.1111/ijcp.14266
26. Rohan, D, Buggy, DJ, Crowley, S, Ling, FKH, Gallagher, H, Regan, C, et al. Increased incidence of postoperative cognitive dysfunction 24 hr after minor surgery in the elderly. Can J Anaesth. (2005) 52:137–42. doi: 10.1007/BF03027718
27. Nishikawa, K, Nakayama, M, Omote, K, and Namiki, A. Recovery characteristics and post-operative delirium after long-duration laparoscope-assisted surgery in elderly patients: Propofol-based vs. sevoflurane-based anesthesia. Acta Anaesthesiol Scand. (2004) 48:162–8. doi: 10.1111/j.0001-5172.2004.00264.x
28. Micha, G, Tzimas, P, Zalonis, I, Kotsis, K, Papdopoulos, G, and Arnaoutoglou, E. Propofol vs sevoflurane anaesthesia on postoperative cognitive dysfunction in the elderly. A randomized controlled trial. Acta Anaesthesiol Belg. (2016) 67:129–37.
29. Miller, D, Lewis, SR, Pritchard, MW, Schofield-Robinson, OJ, Shelton, CL, Alderson, P, et al. Intravenous versus inhalational maintenance of anaesthesia for postoperative cognitive outcomes in elderly people undergoing non-cardiac surgery. Cochrane Database Syst Rev. (2018) 2018:CD012317. doi: 10.1002/14651858.CD012317.pub2
30. Cai, Y, Hu, H, Liu, P, Feng, G, Dong, W, Yu, B, et al. Association between the apolipoprotein E4 and postoperative cognitive dysfunction in elderly patients undergoing intravenous anesthesia and inhalation anesthesia. Anesthesiology. (2012) 116:84–93. doi: 10.1097/ALN.0b013e31823da7a2
31. Shoair, OA, Grasso Ii, MP, Lahaye, LA, Daniel, R, Biddle, CJ, and Slattum, PW. Incidence and risk factors for postoperative cognitive dysfunction in older adults undergoing major noncardiac surgery: a prospective study. J Anaesthesiol Clin Pharmacol. (2015) 31:30–6. doi: 10.4103/0970-9185.150530
32. Guo, JY, Fang, JY, Xu, SR, Wei, M, and Huang, WQ. Effects of propofol versus sevoflurane on cerebral oxygenation and cognitive outcome in patients with impaired cerebral oxygenation. Ther Clin Risk Manag. (2016) 12:81–5. doi: 10.2147/TCRM.S97066
33. Cao, XZ, Ma, H, Wang, JK, Liu, F, Wu, BY, Tian, AY, et al. Postoperative cognitive deficits and neuroinflammation in the hippocampus triggered by surgical trauma are exacerbated in aged rats. Prog Neuro-Psychopharmacol Biol Psychiatry. (2010) 34:1426–32. doi: 10.1016/j.pnpbp.2010.07.027
34. Benedict, C, Cedernaes, J, Giedraitis, V, Nilsson, EK, Hogenkamp, PS, Vagesjo, E, et al. Acute sleep deprivation increases serum levels of neuron-specific enolase (NSE) and S100 calcium binding protein B (S-100B) in healthy young men. Sleep. (2014) 37:195–8. doi: 10.5665/sleep.3336
35. Wiesmann, M, Missler, U, Gottmann, D, and Gehring, S. Plasma S-100b protein concentration in healthy adults is age- and sex-independent. Clin Chem. (1998) 44:1056–8. doi: 10.1093/clinchem/44.5.1056
Keywords: intravenous anesthesia, inhalation anesthesia, non-cardiac surgery, the elderly, cognitive function
Citation: Huang L and Zhang Y (2023) The effect of intravenous and inhalation anesthesia in general on the cognition of elderly patients undergoing non-cardiac surgery: a systematic review and meta-analysis. Front. Med. 10:1280013. doi: 10.3389/fmed.2023.1280013
Received: 19 August 2023; Accepted: 26 October 2023;
Published: 15 November 2023.
Edited by:
Somchai Amornyotin, Mahidol University, ThailandReviewed by:
Sang Hun Kim, Chosun University, Republic of KoreaCopyright © 2023 Huang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yong Zhang, eGJ0ZGZoQDE2My5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.