
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med., 23 November 2023
Sec. Healthcare Professions Education
Volume 10 - 2023 | https://doi.org/10.3389/fmed.2023.1272893
This article is part of the Research TopicInsights in Healthcare Professions Education: 2023View all 16 articles
 Fabian Stoehr1†
Fabian Stoehr1† Yang Yang1†
Yang Yang1† Lukas Müller1
Lukas Müller1 Phyllis Gerstenmeier1
Phyllis Gerstenmeier1 Daniel Pinto dos Santos2,3
Daniel Pinto dos Santos2,3 Pavel Dietz4
Pavel Dietz4 Andreas Weimer5
Andreas Weimer5 Michael Ludwig6
Michael Ludwig6 Roman Kloeckner7
Roman Kloeckner7 Johannes Matthias Weimer8*
Johannes Matthias Weimer8*Introduction: The best way to impart knowledge to medical students is still unclear. Therefore, we designed a blended learning course in thoracic radiology including both “traditional” in-class time as well as online learning modules. The aims were (1) to investigate students’ attitudes toward this blended learning approach; and (2) to test whether it improved their knowledge about thoracic radiology.
Methods: A prospective study was conducted at the local medical center; 156 fourth-year medical students completed this study. Before and after the course, students had to complete (1) questionnaires to investigate their attitudes (7-point Likert scale); and (2) an objective test to assess their knowledge (multiple-choice/free text questions; results as % of correct answers).
Results: Regarding (1), the course led to an improvement in all items compared to baseline, exemplary: interest in thoracic radiology (precourse 4.2 vs. 5.4 postcourse) and the fulfillment of students’ expressed requirements regarding the teaching content (4.5 precourse vs. 6.2 postcourse). Furthermore, the great majority (88%) of our participants wished for more online learning offerings in the future. Regarding (2), the course led to improved knowledge on the objective test (precourse: 40% vs. postcourse: 63% correct answers).
Conclusion: This feasibility study showed the successful design and implementation of a blended learning approach in thoracic radiology. Furthermore, it revealed medical students’ positive attitudes toward this approach and showed an increased knowledge in thoracic radiology. Thus, such approaches might be used to enrich the teaching armamentarium in medical education and to further enhance interest and knowledge in thoracic diseases among medical students.
The best way to impart knowledge to medical students is still unclear and remains the focus of ongoing research (1–4). In the vast majority of medical schools, teaching is still based mainly on traditional, ex cathedra concepts (4–6). Previous studies have proposed that students’ discontent with the current teaching system might be one of the various reasons for their declining participation rates in recent years (2, 7–9).
However, there is growing interest in more innovative, student-centered approaches including, in particular, online teaching and learning (2, 9, 10). As a reaction, such online-based formats have been added to radiology education curricula, with great success regarding the effectiveness of learning and positively influencing students’ attitudes toward learning (11–16). Notably, blended learning approaches attracted much attention in recent years (17–20). In its essence, blended learning combines both online and onsite learning resulting in a beneficial mix and allowing for a possible greater educational impact (19–21). In a “flipped classroom,” an autonomous, online-based learning phase precedes a face-to-face, onsite learning session (18, 22). In the online phase, students actively and autonomously acquire knowledge serving as a basis for the face-to-face phase. In the subsequent onsite phase, the main focus is to deepen the acquired knowledge and to further enhance the learning process (18, 20).
If used properly, this shift from instructor-centered teaching to student-centered learning can promote accelerated learning and might foster i.a. the learning and motivation (18–21).
On the other hand, the success of this blended learning course strongly depends on an adequate acquisition of knowledge in the online phase (18, 22). Thus, students’ motivation to actively participate and to prepare themselves prior to the face-to-face session is crucial. From lecturers’ perspective, a “traditional” onsite course has to be transformed into an online/hybrid format (14, 18). As a dedicated teaching platform and multimedia material is required, this requires additional effort and can be a time-consuming and potentially expensive process.
Over the last 2 years, the coronavirus disease 2019 (COVID-19) pandemic has acted as a catalyst for such innovative concepts as lecturers were forced to critically rethink teaching formats in medical education (22–28). As a positive consequence, several attempts have been made to implement various teaching formats (22–26). However, as courses were mostly implemented under considerable time pressure, they can be seen as “emergency remote teaching” instead of dedicated and embedded in a structured, curricular framework. Nevertheless, even after overcoming the pandemic, such innovative and “digitally supported” teaching concepts are not provided throughout all medical universities.
Thus, we designed a blended learning course in thoracic radiology and implemented it into the teaching curriculum of our faculty. In the scenario chosen for this study and as mentioned above, students had to acquire basic knowledge independently outside the classroom before attending a live didactic course (17, 29). For this purpose, we developed an online platform, which served as a basis for the online education part.
We deliberately chose thoracic radiology as the subject because it is (1) a common field in diagnostic imaging; and (2) includes basic knowledge almost every medical student will need as a doctor (30, 31). First, we aimed to investigate students’ general interest in this blended learning approach. Second, we aimed to test whether this specific course design can improve students’ knowledge and understanding about thoracic radiology.
This study was conducted prospectively at the Department of Diagnostic and Interventional Radiology, University Medical Center Mainz. It was performed in accordance with the “Checklist for Reporting Results of Internet E-Surveys (CHERRIES)” (32) and with the “Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies” (33) (Checklist S1). Institutional review board approval was waived by the Ethics Committee of the Medical Association of Rhineland-Palatinate.
For this study, a dedicated course on thoracic radiology was designed using a blended learning approach. The course was part of the officially predetermined curriculum of our university medical center, delivered to fourth-year medical students and embedded into a pre-existing curricular course in radiology; other courses of the officially predetermined curriculum included i.a. Interventional Radiology, Cardiovascular Radiology, Oncological Imaging and Neuroradiology. It was conducted as a hybrid course consisting of a structured online learning platform and one 90-min dedicated onsite course with face-to-face teaching. Before the online part as well as after the onsite part, participants’ knowledge about thoracic radiology as well as their attitudes toward the course design was captured. To this end, dedicated questionnaires as well as an objective knowledge test were designed (see section 2.3 for more details). Before each part of the course (online and onsite), participants were informed that the survey results would be anonymous and that they were collected for research purposes only. Figure 1 gives an overview of the setup of our blended learning course.
The course program was based on the “Radiological Curriculum for Undergraduate Medical Education in Germany” of the German Radiological Society (DRG) (30) as well as on the “Curriculum for Undergraduate Radiological Education” of the European Society of Radiology (ESR) (31). Design and implementation of the course followed the waterfall model (34) and was a multi-stage process.
Online teaching was performed via a dedicated, newly designed online learning platform. Content was composed by a consortium of several experts in the field of thoracic radiology, pulmonology, and didactics. Images were drawn by a web designer; the online learning platform was built by a professional programmer and could be accessed via a standard web browser. The platform consisted of six modules, which had to be studied by the students autonomously before the onsite course was given. Modules transmitted knowledge about technical basics as well as normal and pathological findings in X-ray, CT, and ultrasonography. Modules were: basics chest X-ray, basics chest CT, basics ultrasonography, pathological findings chest imaging, pathological findings CT/X-ray and pathological findings ultrasonography. An example of the structure of the online learning platform is provided in the Supplementary Figure S1.
In order to enhance the learning experience, online content was enriched with different features (clickable color highlighting, video loops on demand, image magnification). An example of how each of these features was used in the platform is provided the Supplementary Figure S2.
Onsite courses were given as 90-min face-to-face seminars. Based on the modules mentioned above, there was a case-based discussion in which the participants could deepen their understanding in thoracic radiology. In order to have the same knowledge base, modules of the onsite and online part matched. Courses were carried out as block training on a daily basis during 2 weeks in July 2022 and given by consultant radiologists with considerable experience in thoracic imaging. Group size for the onsite courses was 8–10 students.
A dedicated questionnaire was designed together with the Institute of Occupational, Social and Environmental Medicine (ASU) of the University Medical Center Mainz. The questionnaire comprised various sections covering in particular the following topics: interest and knowledge of thoracic radiology; the students’ expressed requirements for teaching content and teaching medium in thoracic radiology; the use of online learning in general and in thoracic radiology; attitudes toward online learning before, during, and after the pandemic; and technical aspects of online learning as well as the current and possible future role of online learning. In the questionnaire, particular attention was paid to the assessment of the online learning platform as it was newly designed for this course. Participants were asked to answer the questions using a 7-point Likert scale. Compared with a 5-point scaling system, a 7-point Likert scale provides higher variance and thus higher reliability. Other scales such as 9- or even 11-point scales would not add any more value regarding the information obtained and could even strain our participants’ abstraction capabilities. The questionnaires are provided in the Supplementary material (Precourse evaluation S2 and Postcourse evaluation S3).
The objective test was based on the content of this thoracic radiology course as well as on the curricula of the “German Radiological Society” (DRG) and the “European Society of Radiology” (ESR) for undergraduate radiological teaching (30, 31). It was composed by a consortium of several experts in the field of thoracic radiology, pulmonology, and didactics. For a more balanced assessment, multiple-choice as well as free text questions were used. Design of the questions corresponded to current specifications (35, 36). The entire test is provided in the Supplementary material (Quiz thoracic radiology S4).
The questionnaires and objective test underwent a two-step validation to further enhance the quality of the study. First, cognitive pretesting was performed on a sample of 10 participants (medical students in their last year; feedback was given via oral survey) (37); second, pilot testing was performed on a cohort of 25 participants (medical students in their last year; feedback was given via written survey) (38).
Survey results were collected via an established online survey tool (SurveyMonkey1). After the questionnaires and the test were designed, web links were encoded in QR codes, which were implemented in the presentations of the courses. Students were asked to scan the QR codes with their smartphones to access the questionnaires. In case of technical problems, we provided tablets. Final survey results were exported from SurveyMonkey as a CSV file and subsequently analyzed using R 4.2.2 (A Language and Environment for Statistical Computing, R Foundation for Statistical Computing2; last accessed February 2023). Figures were plotted using the ggplot2 and Likert packages (39). Means and standard deviations were calculated to analyze the results regarding descriptive statistical analysis (40), regression analysis was performed to identify possible relationships between variables (see section 3.3 for detailed description).
In total, 156 of 160 students completed the questionnaires (97.5% response rate). Demographic data recorded were gender (40.4% male, 59.6% female), age (mean 25.9 years), current study year (mean fourth study year) as well as possible vocational training before medical studies. A tabular overview is provided in the Supplementary Table S5.
The following survey results are presented in written form as well as graphically (Figures 2–8). To increase comprehensibility, the text contains only the key findings and summarizes “strongly disagree,” “disagree,” and “somewhat disagree” as disagreement, and “somewhat agree,” “agree,” and “strongly agree” as agreement. For statistical analyses, the original 7-point categories were used.
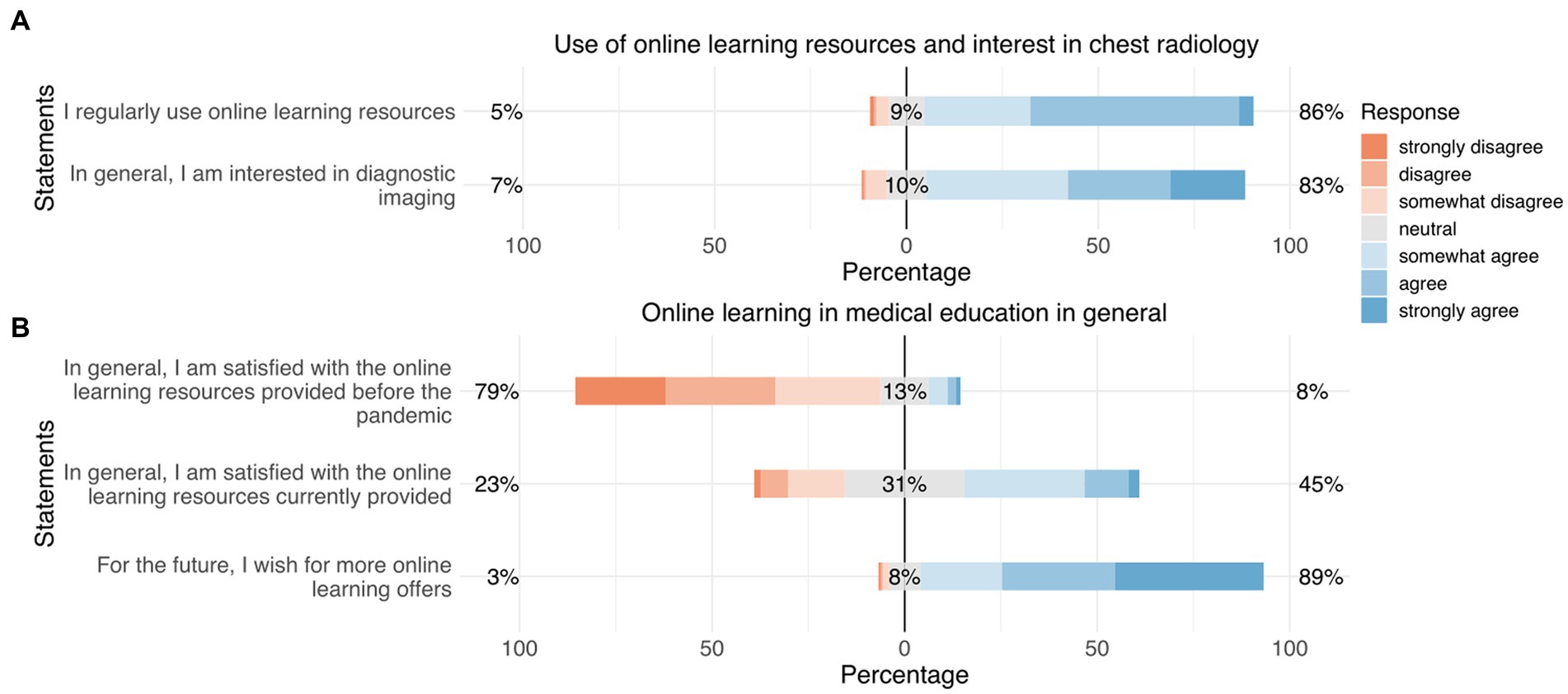
Figure 2. Responses regarding “use of online learning resources and interest in thoracic radiology” (A) and “online learning in medical education in general” (B). Orange represents “disagreement,” gray represents “neutral,” and blue represents “agreement.”
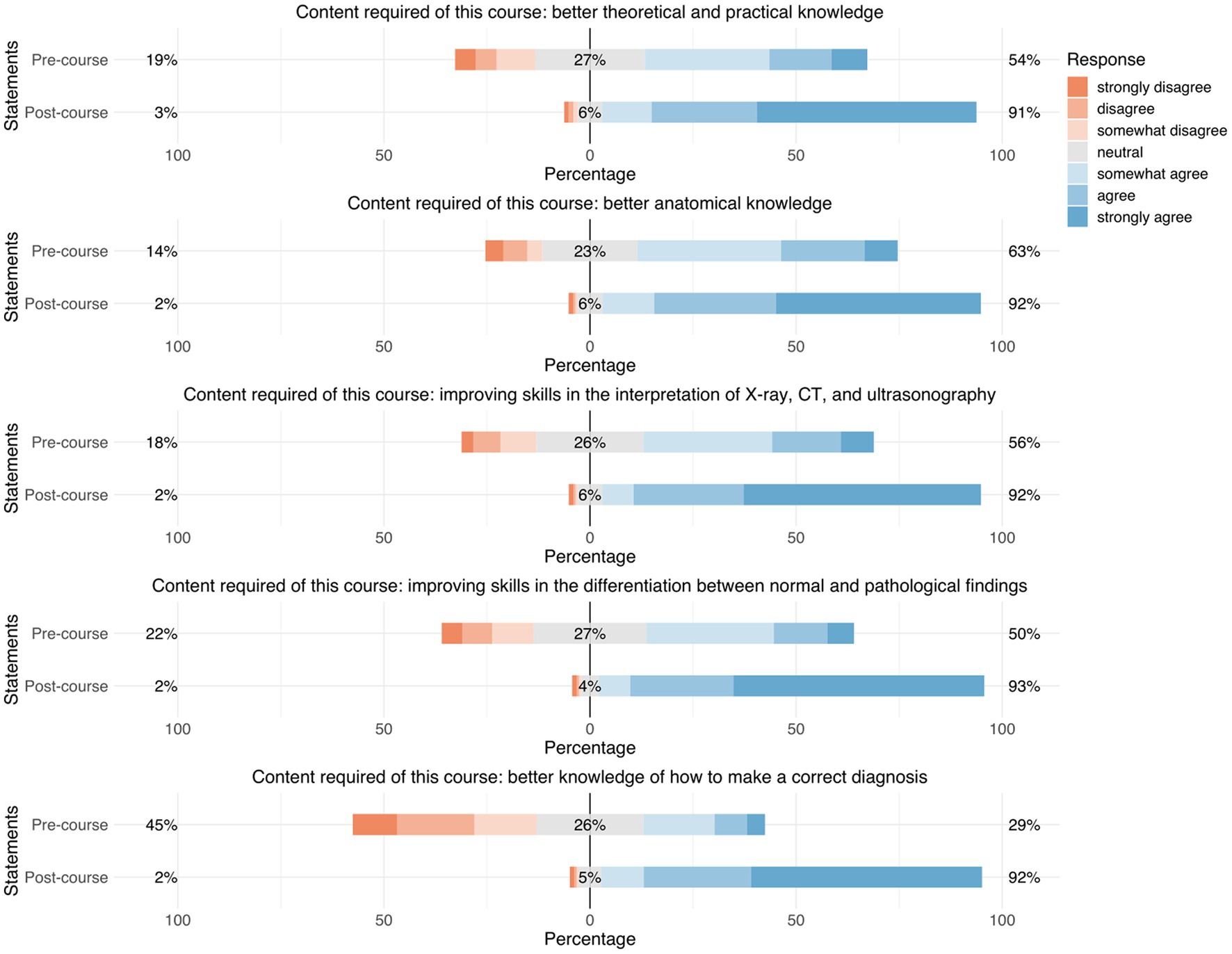
Figure 3. Responses regarding “requirements on teaching content in thoracic radiology.” Precourse results are compared to postcourse results. Orange represents “disagreement,” gray represents “neutral,” and blue represents “agreement.”
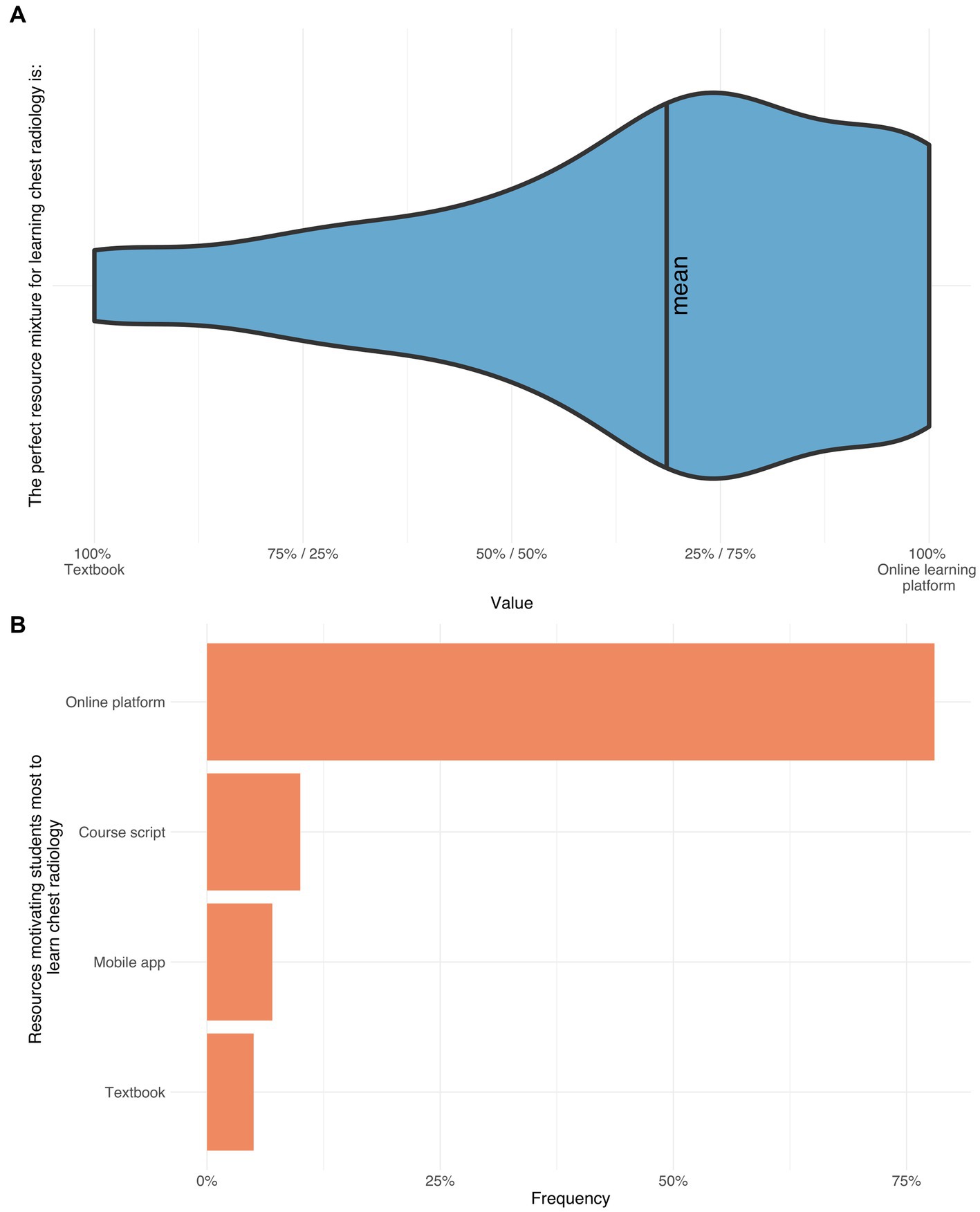
Figure 4. The upper violin plot depicts the preferred teaching type (online platform vs. textbook/lecture notes) (66%) (A). The bars demonstrate the ranking of the teaching types motivating the participants most to learn thoracic radiology: Online platform (78%), course script (10%), app (7%), and textbook (5%) (B).
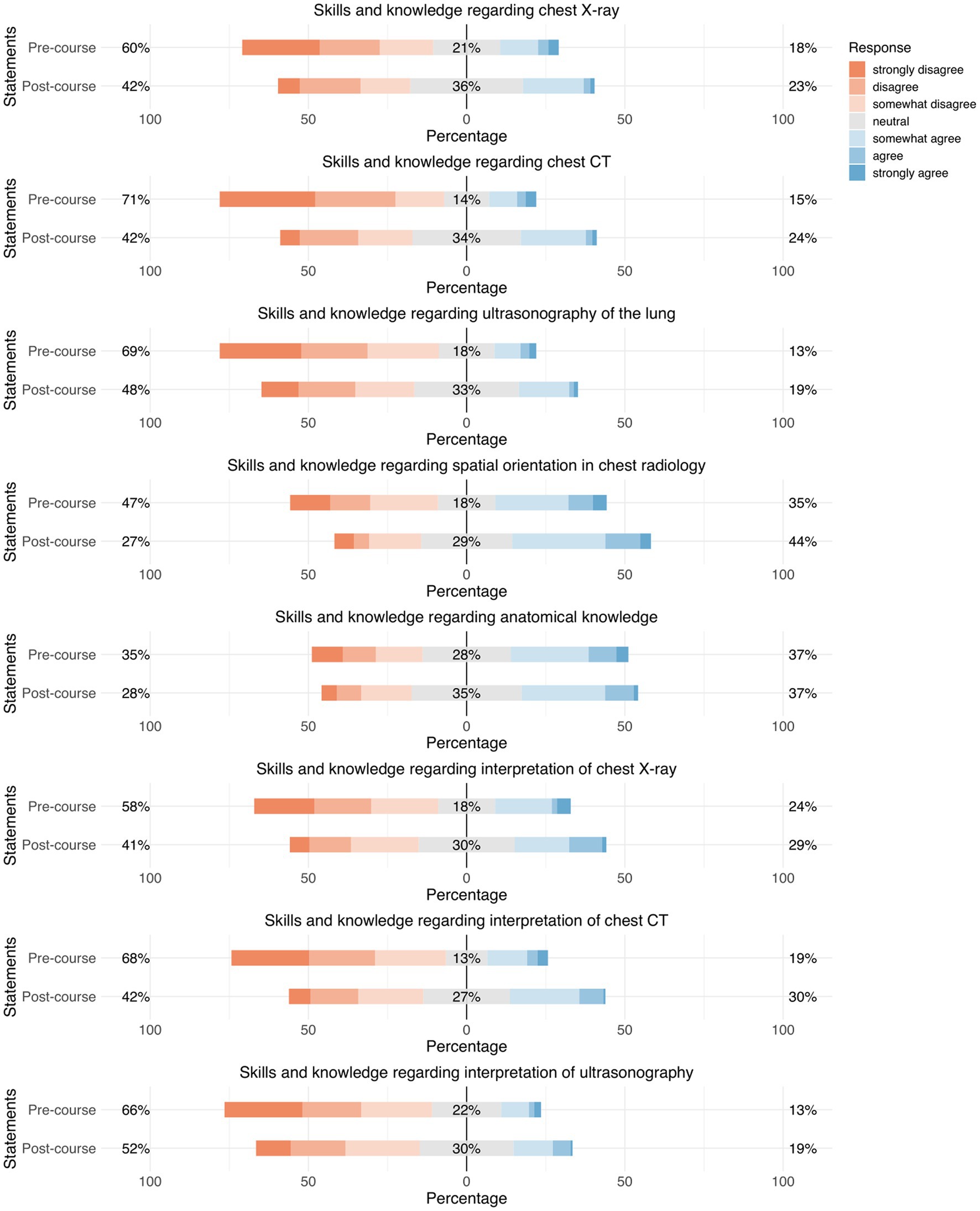
Figure 5. Responses regarding “subjective self-assessment of knowledge in thoracic radiology.” Precourse results are compared to postcourse results. Orange represents “disagreement,” gray represents “neutral,” and blue represents “agreement.”
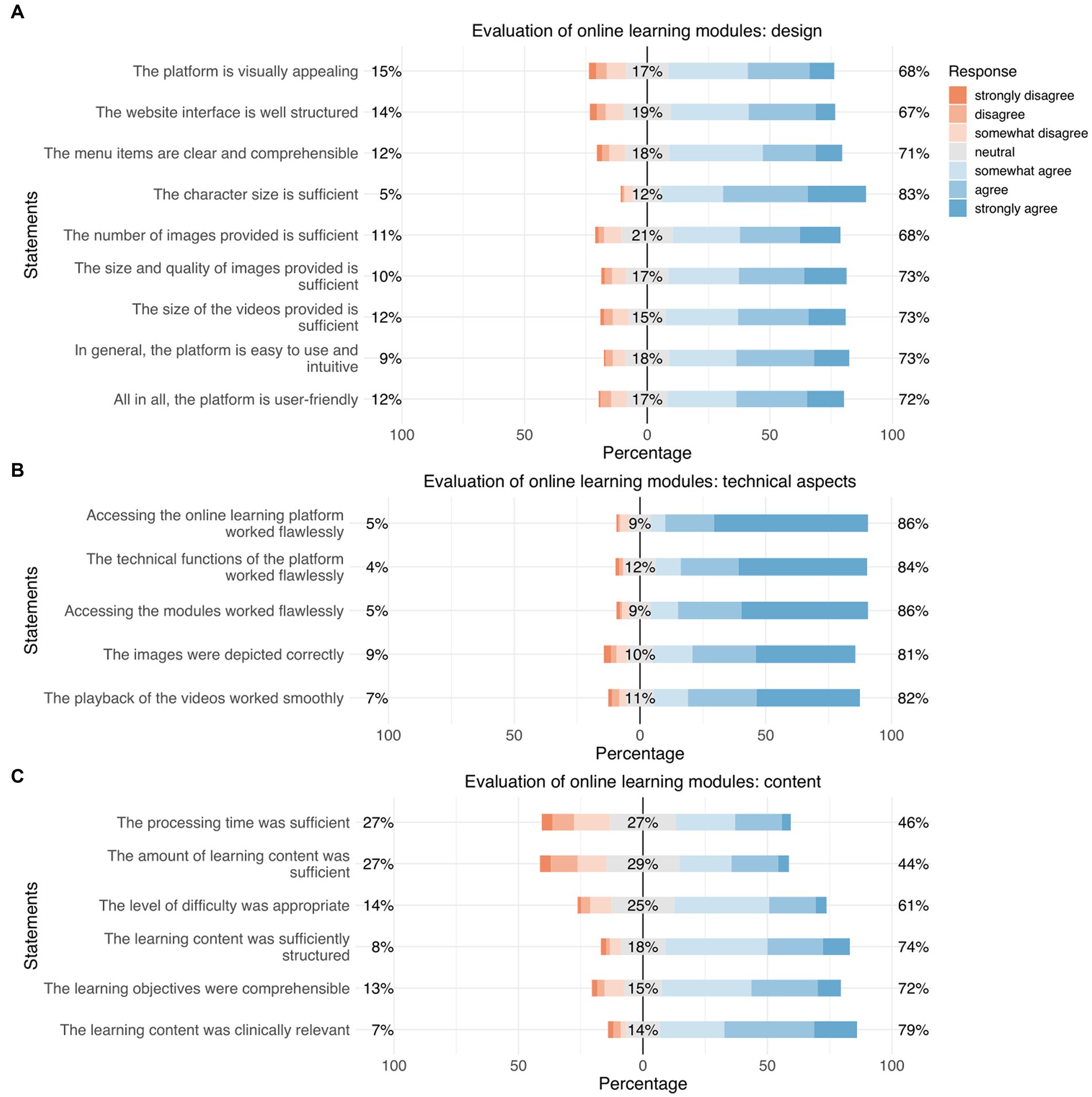
Figure 6. Responses regarding “evaluation of the online learning modules: design” (A), “evaluation of the online learning modules: technical aspects” (B), and “evaluation of the online learning modules: content” (C). Orange represents “disagreement,” gray represents “neutral,” and blue represents “agreement.”
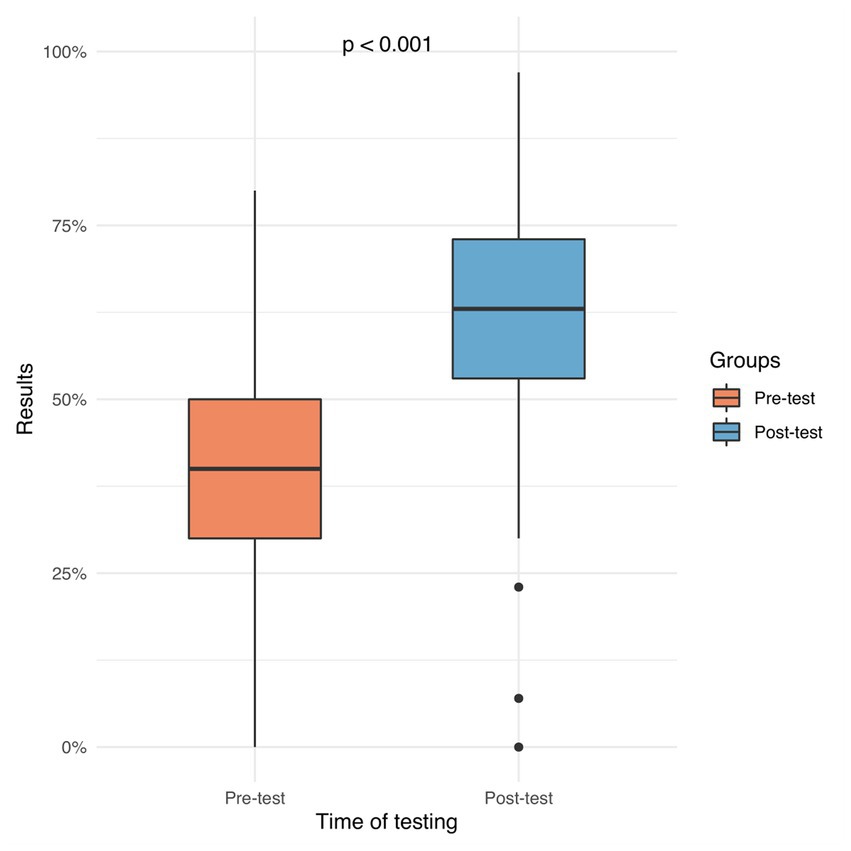
Figure 7. The left plot depicts the precourse results (mean 40%, IQR 30–50%). The right plot depicts the postcourse results (mean 63%, ICR 53–73%). This was statistically significant (p < 0.001).
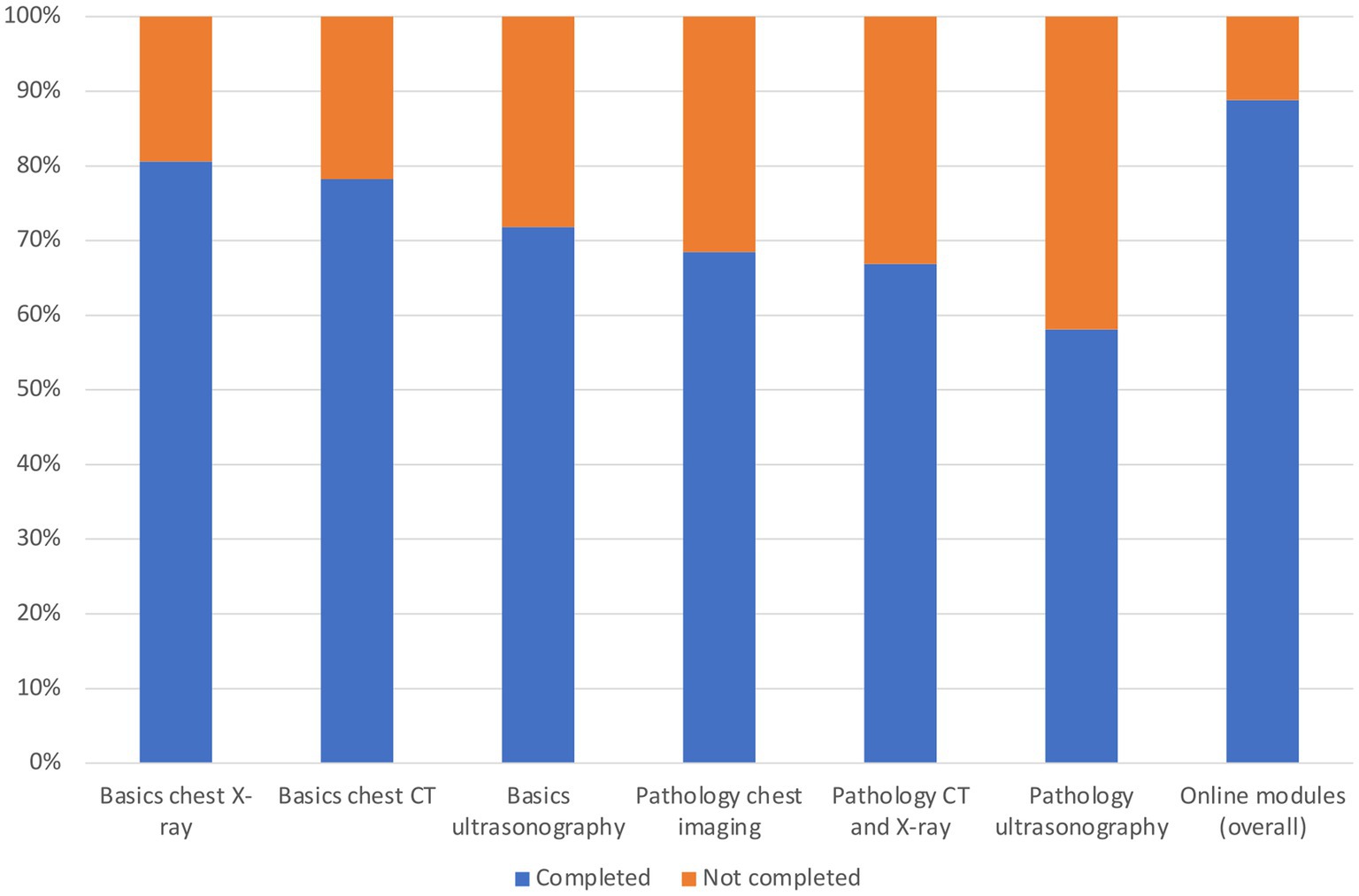
Figure 8. Completion rates of each module in %. Blue represents completion, whereas orange represents lack of completion/no completion.
A great majority of the participants stated that they use online learning media (86%), with an average of 12 h of use per week. This remained unchanged after the course. One-fourth of our participants had already used online learning media before (27%). If online learning media were used, online learning platforms were ranked in first place (16%), before eBooks (10%) and apps (12%).
Prior to the course, an overwhelming majority stated that they were interested in diagnostic imaging in thoracic radiology (83%). Before the course, only one-third of the participants stated that they had previous experience in thoracic radiology (31%), mostly from textbooks (37%), followed by curricular courses (21%) and webinars (11%) (Figure 2).
Only a few participants were satisfied with the online learning courses provided before the pandemic (8%). About the half of our participants were satisfied with the online courses provided during the pandemic (45%). However, the great majority of the participants wished for more online learning offerings in the future (89%) (Figure 2).
Before the course, participants demanded a better theoretical and practical knowledge of thoracic radiology (54%), a better understanding of thoracic anatomy (63%), and to be able to better differentiate between pathological and normal findings (50%). After the course, an overwhelming majority of our participants stated that their requirements for teaching content were fulfilled regarding their theoretical and practical knowledge of thoracic radiology (91%), their understanding of thoracic anatomy (92%), and their ability to differentiate between pathological and normal findings (93%) (Figure 3).
Before the course, a great majority of the participants ranked online learning platforms as their preferred learning type that would motivate them the most to learn thoracic radiology (70%), before scripts/lecture notes (10%), apps (7%), and books (5%). After the course, these high expectations were fulfilled as the great majority stated that online learning platforms motivated them to become involved with thoracic radiology, even in the future (73%). Furthermore, students chose the online platform as their preferred teaching type (Figure 4).
Before the course, participants stated that they had rather little knowledge of thoracic radiology in general; for example, knowledge about X-ray (18%), CT (15%), ultrasonography (13%), spatial orientation (35%), and thoracic anatomy in general (37%) (Figure 5).
After the course, participants stated that they had the same or improved knowledge regarding all items; for example, knowledge about X-ray (59%), CT (58%), ultrasonography (52%), spatial orientation (73%), and thoracic anatomy in general (72%) (Figure 5).
In general, participants were satisfied with the online learning modules; for example, regarding user friendliness (72%), playback of the videos (82%), content (74%), and the level of difficulty of the learning materials (61%) (Figure 6).
Before the course, participants achieved a mean score of 40% on the objective test. After the course, participants achieved a mean score of 63% on the objective test (Figure 7).
Furthermore, a detailed analysis of the completion rates of the modules of our blended learning course was performed - broken down by each module separately. Results were depicted graphically (Figure 7) as well as in tabular form (Supplementary Table S7) (completion “yes/no” in %). Interestingly, a total of 11% of our participants did not complete any module.
Based on these results, we aimed to investigate if there is a possible relationship between the completion of the modules and the results in the knowledge test. For this purpose, (sub-) results of the knowledge test were analyzed, again broken down by each module separately. Supplementary Table S10 provides detailed information including results in pre- and posttest (mean ± standard deviation) and possible differences between pre- and posttest (“gain/loss of knowledge”) including its statistical significance (p-value) and its effect size (Cohen’s d). As a conclusion, regarding all modules there is a statistically significant knowledge gain between pre- and posttest.
In order to identify possible relationships between the completion of the modules and the (sub-) results in the posttest, a regression analysis was performed. Supplementary Table S8 provides a summary of the most important findings regarding the effect on the posttest. All data from the regression analysis (including analysis of the pretest) is provided in the Supplementary material (Supplementary Tables S8, S9).
In summary, completion of the modules leads to significantly better results in the posttest. However, even more interesting is the “no module” subgroup – those 11% of participants who did not complete any module (Supplementary Table S7). As those 11% only attended the onsite part of our blended learning course, they could somehow serve as a comparative internal reference group. According to our results, this subgroup has significantly worse results in the posttest regarding all modules (Supplementary Table S8). Of course, this conclusion must be considered with the utmost care as the “no module” subgroup was never intended to serve as a reference group. However, there is a trend that those participants who have completed both parts of the blended learning course perform better than those who have not completed both parts.
Furthermore, as a head-to-head comparison between the novel learning approach presented herein and conventional teaching methods was not possible, we performed an “internal quality control” in order to investigate a possible change of knowledge of the participants. To this end, we compared the official examination results of the year in which our study took place to examination results from the previous year. The results from this analysis are provided in the Supplementary material (Internal quality control S6). In summary, there was no statistically significant difference regarding the examination results.
This feasibility study showed the successful design of a blended learning approach in thoracic radiology and its implementation into a pre-existing radiology curricular course. Furthermore, it revealed medical students’ positive attitudes toward this approach and showed an increased knowledge in thoracic radiology. As the best way of transferring knowledge in medical education is still unclear, such approaches might be used to enrich the teaching armamentarium and to further enhance interest and knowledge in thoracic diseases among medical students.
One explanation for these positive results might be the increased flexibility of self-determined learning, and our results are in line with this notion. Students appreciated the broad online course content, which they could use anywhere at any time and at their own pace without having to attend a class. Another point is that the flexibility of self-determined learning could be particularly important in meeting the needs of an increasingly diverse student community (41). The maximal learning and teaching flexibility provided by such courses could accommodate, for example, students with disabilities and thus further enhance inclusivity (41).
On the other hand, from students’ perspective, it requires higher stringency, commitment and intrinsic motivation as they - as first - have to obtain knowledge at their own (21). This includes, e.g., watching prerecorded lectures and/or completing online education modules (17). As this is an additional learning burden compared to traditional classroom teaching, approval among students may soon disappear. And in fact, previous studies suggest that both medical students and lecturers had difficulty motivating themselves (or the students, respectively) to follow online courses (2, 9). In order to be successful, thus, students’ motivation to engage with it is crucial. Possible solutions to this include, e.g., learning content that is designed “activating” as possible by, e.g., videos or short quizzes. Furthermore, a structured framework including learning goals and timetables for each learning module are necessary to guide students through the information jungle (14). These steps are necessary to improve students learning behavior in a successful and self-determined manner and to avoid leaving students behind. Interestingly, our results indicate that students were additionally motivated to become involved with thoracic radiology after using our modules. They even plan to use the modules in the future in order to refresh their knowledge of the subject. Such a refresher might be of particular interest before clerkships in, for example, pulmonology or thoracic surgery.
From lecturers’ perspective, the prior onsite course was changed from instructor-centered teaching to student-centered learning. This step can be somewhat critical and requires high commitment as lecturers have to face new requirements and “evolve” from being the (only) source of information to being a “guide on the side” helping students in the “information jungle” (14). However, this step is most crucial to further enhance students’ learning experience, to show them that they are benefitting from their own efforts and – thus - to avoid motivational problems on both sides (14, 42).
Taking the above-mentioned steps together, at best, this leads to a maximum effective in-class time in which students and teachers can really focus on core topics that are, e.g., difficult to understand and need more time for explanation. From students’ perspective, this might result in an enhanced learning effect.
Despite the possible benefits of a blended learning approach, there is no doubt that the implementation of new teaching concepts require additional effort (43, 44). This is especially true for the transition from traditional, onsite teaching to online or hybrid teaching. First, IT infrastructure has to be installed or adjusted to online teaching. Mostly, its installation results in both a time-intensive and expensive process depending on the local conditions of the institution (43). Regarding the course on thoracic radiology presented herein, radiology departments might have an advantage compared to other specialties as solid IT-solutions or IT-infrastructure might be already available making the switch to online teaching easier.
Furthermore, faculty and lecturers are required to adapt the teaching concept to an online format which is again time-consuming. However, once the material has been made suitable for an online module, it has to be updated periodically, but the lecturer does not have to present the same lecture over and over again. Regarding content creation, a clearly defined curriculum including time tables and learning goals helps here as mentioned above (14). Furthermore, triggered by the pandemic, there is a bouquet of online available teaching resources including online teaching platforms as well as a wide variety of national and international guidelines which can be used for content creation (30, 31). For example, the German Radiological Society launched an interactive online learning platform providing a broad variety of online courses comprising prerecorded lectures, case-based training, educational imaging data, etc., for medical students as well as professionals.3 Such innovative teaching projects not only allow for broad “knowledge on demand” but may also enhance the harmonization of radiological teaching content in the future. This is especially true when it comes to inter-faculty implementation of a certain curriculum involving more than one medical school as such tools might provide a certain level of standardization.
Results from previous studies suggest that there is a trend is toward digital learning and teaching in medical education (2, 9, 23, 26, 45). However, there is lots of room for improvement and constant further development is crucial.
Due to the specific course design within the framework of a regular curricular radiology course and the curricular regulations of the faculty a head-to-head comparison between our blended learning approach and conventional classroom teaching was not possible. Consequently, statements regarding the superiority of our learning approach compared to conventional approaches are limited. However, an “internal quality control” regarding a possible change of knowledge on the objective test results was performed. In summary, there was no statistically significant difference regarding the examinations results [see also point 3.3 of our results section as well as our Supplementary material (Internal quality control S6)]. Despite these results, however, it must be said that the comparability is limited, and it is difficult to draw conclusions from this: (1) Examinations used for this quality control do not only contain thoracic radiology questions but represent the entire spectrum of the curricular radiology course and (2) the groups including their learning environment are not equal.
Furthermore, this study is questionnaire-based and subject to typical pitfalls. We had to consider selection bias, meaning that interested participants were more likely to complete the questionnaire (46). However, as courses were delivered to all fourth-year medical students, there was no preselection of the participants. Furthermore, the high response rate of our study implies that the pool of participants was representative of the students. Second, there was a potential for social desirability bias, meaning that participants chose the answer they assumed to be favorable (47). In order to attenuate this, we chose an anonymous, untraceable study design and informed the participants that the results were for research purposes only. Due to the specific course design, the onsite course always followed the online part. Thus, we cannot exclude position bias, meaning that participants might have been influenced by the sequence in which the content was presented (48). Furthermore, this blended learning approach was integrated into a pre-existing curricular radiology course which might have affected participants’ knowledge and attitudes toward our blended learning course due to “surrounding” learning activities. Regarding technical issues, the tools used by the participants for their online teaching were not standardized and this use of different tools may have affected the results.
Due to the short follow-up of 2 weeks, this study can only provide a snapshot as we did not examine long-terms effects. Further longitudinal assessments several months or even years after the study would be valuable to examine effects on long-term retention, a possible impact on the development of clinical skills and the practical application of knowledge. As this study included only medical students as participants, such follow-up studies could, for example, also focus on lecturers’ attitudes toward this teaching concept. Such an approach might reveal possible differences in students’ and lecturers’ attitudes toward possible teaching concepts in the future. As this is a single-center study with a specific cohort of students, its findings may not be easily generalizable to other medical schools or student populations limiting the external validity of the study. Thus, further studies should include different medical schools from different nations to investigate the potential of this teaching concept in order to help harmonizing medical curricula around the world.
Finally, this study mainly focused on the assessment of knowledge gain as primary learning objective. However, besides the acquisition of knowledge and practical skills there is an ongoing discourse including fundamental aspects of medical education, of what constitutes effective learning and of the professional attributes required of doctors (49). As medical educators should prepare learners in the best way for their future professional roles it is crucial to expand our perspectives about learning and to consider several relevant learning theories as the foundation of teaching and learning approaches in medical education (4, 49).
This feasibility study showed the successful design and implementation of a blended learning approach in thoracic radiology into a pre-existing radiology teaching curriculum. First, our study revealed medical students’ great interest in and acceptance of this learning approach. Second, the learning approach presented herein led to an increased knowledge in an objective test in thoracic radiology. Thus, approaches as the one presented herein might further stimulate the evolution of teaching and learning in medical education. However, further studies including, e.g., head-to-head comparisons with conventional teaching approaches as well as studies focusing on lecturers’ attitudes toward new learning approaches are necessary to generate more evidence regarding these novel teaching and learning approaches.
Data cannot be shared publicly because of institutional and national data policy restrictions imposed by the Ethics committee since the data contain potentially identifying study participants’ information. Data are available upon request (contact via d2VpbWVyQHVuaS1tYWluei5kZQ==) for researchers who meet the criteria for access to confidential data (please provide the manuscript title with your enquiry).
The studies involving humans were approved by Ethik-Kommission bei der Landesärztekammer Rheinland-Pfalz. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
FS: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. YY: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. LM: Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Resources, Software, Validation, Visualization, Writing – review & editing. PG: Conceptualization, Data curation, Investigation, Validation, Writing – review & editing. DP: Data curation, Formal analysis, Investigation, Methodology, Software, Supervision, Visualization, Writing – review & editing. PD: Conceptualization, Data curation, Investigation, Supervision, Validation, Writing – review & editing. AW: Data curation, Investigation, Validation, Writing – review & editing. ML: Data curation, Investigation, Validation, Writing – review & editing. RK: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – review & editing. JW: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. FS and LM are supported by the Clinician Scientist Fellowship “Else Kröner Research College: 2018_Kolleg.05.” The study was supported by a grant of the Carl Zeiss Foundation (https://www.carl-zeiss-stiftung.de). The funders had no role in the design of the study, in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
This study includes parts of the doctoral thesis of one of the author (PG). We thank all participating students and lecturers for supporting our study. We would like to also thank C. Christe for her help in revising the figures. Furthermore, we want to thank Professor Christoph Düber for his continuous support.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2023.1272893/full#supplementary-material
CHECKLIST S1 | Guideline for reporting observational studies.
PRECOURSE EVALUATION S2 | Questionnaire investigating various aspects of teaching and learning in radiology and medical education (precourse).
POSTCOURSE EVALUATION S3 | Questionnaire investigating various aspects of teaching and learning in radiology and medical education (postcourse).
QUIZ THORACIC RADIOLOGY S4 | Test consisting of both multiple-choice and free text questions on thoracic radiology.
SUPPLEMENTARY TABLE S5 | Demographic characteristics of the participants.
INTERNAL QUALITY CONTROL S6 | Examination results from the year 2021 compared to the examination results from 2022 (the year in which our study took place) (“test”).
SUPPLEMENTARY TABLE S7 | Completion rates of the modules (%).
SUPPLEMENTARY TABLE S8 | Results of the regression analysis investigating various influencing factors regarding their impact on the objective knowledge test (“posttest”).
SUPPLEMENTARY TABLE S9 | Results of the regression analysis investigating various influencing factors regarding their impact on the objective knowledge test (“pretest”).
SUPPLEMENTARY TABLE S10 | (Sub-)results of the knowledge tests, broken down by each module separately.
SUPPLEMENTARY FIGURE S1 | Overview of the structure of the online learning platform for thoracic radiology.
SUPPLEMENTARY FIGURE S2 | Examples of several features which were included to enrich the teaching content of the online learning platform.
1. Chakraborty, P, Mittal, P, Gupta, MS, Yadav, S, and Arora, A. Opinion of students on online education during the COVID-19 pandemic. Hum Behav Emerg Technol. (2020) 3:357–65. doi: 10.1002/hbe2.240
2. Stoehr, F, Müller, L, Brady, A, Trilla, A, Mähringer-Kunz, A, Hahn, F, et al. How COVID-19 kick-started online learning in medical education—the Digi med study. PLoS One. (2021) 16:e0257394. doi: 10.1371/journal.pone.0257394
3. Rose, S. Medical student education in the time of COVID-19. JAMA. (2020) 323:2131. doi: 10.1001/jama.2020.5227
4. Skochelak, SE, and Stack, SJ. Creating the medical schools of the future. Acad Med. (2017) 92:16–9. doi: 10.1097/ACM.0000000000001160
5. Irby, DM, Cooke, M, and BC, OB. Calls for reform of medical education by the Carnegie foundation for the advancement of teaching: 1910 and 2010. Acad Med. (2010) 85:220–7. doi: 10.1097/ACM.0b013e3181c88449
6. McGaghie, WC, Issenberg, SB, Petrusa, ER, and Scalese, RJ. Revisiting ‘a critical review of simulation-based medical education research: 2003-2009. Med Educ. (2016) 50:986–91. doi: 10.1111/medu.12795
7. Nevins, EJ, Moori, PL, Alexander, L, Richards, B, Bleasdale, V, and Sharma, AK. Could attendance at medical school be improved? A prospective study of medical education at the University of Liverpool: study of attendance at a UK medical school. MedEdPublish. (2016) 5:78. doi: 10.15694/mep.2016.000078
8. Desalegn, AA, Berhan, A, and Berhan, Y. Absenteeism among medical and health science undergraduate students at Hawassa university, Ethiopia. BMC Med Educ. (2014) 14:81. doi: 10.1186/1472-6920-14-81
9. Stoehr, F, Müller, L, Brady, AP, Catalano, C, Mildenberger, P, Mähringer-Kunz, A, et al. Online teaching in radiology as a pilot model for modernizing medical education: results of an international study in cooperation with the ESR. Insights Imaging. (2021) 12:141. doi: 10.1186/s13244-021-01092-5
10. Attardi, SM, and Rogers, KA. Design and implementation of an online systemic human anatomy course with laboratory. Anat Sci Educ. (2015) 8:53–62. doi: 10.1002/ase.1465
11. Afzal, S, and Masroor, I. Flipped classroom model for teaching undergraduate students in radiology. J Coll Physicians Surg Pak. (2019) 29:1083–6. doi: 10.29271/jcpsp.2019.11.1083
12. Ge, L, Chen, Y, Yan, C, Chen, Z, and Liu, J. Effectiveness of flipped classroom vs traditional lectures in radiology education. Medicine. (2020) 99:e22430. doi: 10.1097/MD.0000000000022430
13. Tan, N, Bavadian, N, Lyons, P, Lochhead, J, and Alexander, A. Flipped classroom approach to teaching a radiology medical student clerkship. J Am Coll Radiol. (2018) 15:1768–70. doi: 10.1016/j.jacr.2018.07.017
14. European society of radiology (ESR). ESR statement on new approaches to undergraduate teaching in radiology. Insights Imaging. (2019) 10:109. doi: 10.1186/s13244-019-0804-9
15. Weimer, J, Rolef, P, Müller, L, Bellhäuser, H, Göbel, S, Buggenhagen, H, et al. FoCUS cardiac ultrasound training for undergraduates based on current national guidelines: a prospective, controlled, single-center study on transferability. BMC Med Educ. (2023) 23:80. doi: 10.1186/s12909-023-04062-1
16. Weimer, JM, Rink, M, Müller, L, Dirks, K, Ille, C, Bozzato, A, et al. Development and integration of DOPS as formative tests in head and neck ultrasound education: proof of concept study for exploration of perceptions. Diagnostics. (2023) 13:661. doi: 10.3390/diagnostics13040661
17. Prober, CG, and Heath, C. Lecture halls without lectures — a proposal for medical education. N Engl J Med. (2012) 366:1657–9. doi: 10.1056/NEJMp1202451
18. Tolks, D, Schäfer, C, Raupach, T, Kruse, L, Sarikas, A, Gerhardt-Szép, S, et al. An introduction to the inverted/flipped classroom model in education and advanced training in medicine and in the healthcare professions. GMS. J Med Educ. (2016) 33:46. doi: 10.3205/zma001045
19. Means, B, Toyama, Y, Murphy, R, and Baki, M. The effectiveness of online and blended learning: a Meta-analysis of the empirical literature. Teach Coll Rec. (2013) 115:1–47. doi: 10.1177/016146811311500307
20. Vallée, A, Blacher, J, Cariou, A, and Sorbets, E. Blended learning compared to traditional learning in medical education: systematic review and meta-analysis. J Med Internet Res. (2020) 22:e16504. doi: 10.2196/16504
21. Vavasseur, A, Muscari, F, Meyrignac, O, Nodot, M, Dedouit, F, Revel-Mouroz, P, et al. Blended learning of radiology improves medical students’ performance, satisfaction, and engagement. Insights Imaging. (2020) 11:61. doi: 10.1186/s13244-020-00865-8
22. Darras, KE, Spouge, RJ, de Bruin, ABH, Sedlic, A, Hague, C, and Forster, BB. Undergraduate radiology education during the COVID-19 pandemic: a review of teaching and learning strategies. Can Assoc Radiol J. (2021) 72:194–200. doi: 10.1177/0846537120944821
23. Moszkowicz, D, Duboc, H, Dubertret, C, Roux, D, and Bretagnol, F. Daily medical education for confined students during COVID-19 pandemic: a simple videoconference solution. Clin Anat. (2020) 33:927–8. doi: 10.1002/ca.23601
24. Finn, GM, Brown, MEL, Laughey, W, and Dueñas, A. Pandemicpedagogy: using twitter for knowledge exchange. Med Educ. (2020) 54:1190–1. doi: 10.1111/medu.14242
25. Huddart, D, Hirniak, J, Sethi, R, Hayer, G, Dibblin, C, Rao, BM, et al. MedStudentCovid: how social media is supporting students during COVID-19. Med Educ. (2020) 54:951–2. doi: 10.1111/medu.14215
26. Rohr, JM, Mukherjee, M, Donnelly, A, Sprinkle, S, Martinez Duarte, E, and Yuil, VA. Successful integration of thyroid cytopathology and surgical pathology education in an E-module format. J Pathol Inform. (2022) 13:100124. doi: 10.1016/j.jpi.2022.100124
27. Woolliscroft, JO. Innovation in response to the COVID-19 pandemic crisis. Acad Med. (2020) 95:1140–2. doi: 10.1097/ACM.0000000000003402
28. Saiyad, S, Virk, A, Mahajan, R, and Singh, T. Online teaching in medical training: establishing good online teaching practices from cumulative experience. Int J Appl Basic Med Res. (2020) 10:149–55. doi: 10.4103/ijabmr.IJABMR_358_20
29. Ramnanan, C, and Pound, L. Advances in medical education and practice: student perceptions of the flipped classroom. Adv Med Educ Pract. (2017) 8:63–73. doi: 10.2147/AMEP.S109037
30. Deutsche Röntgengesellschaft (DRG). White paper: radiological curriculum for undergraduate medical education in Germany. Rofo. (2016) 188:1017–23. doi: 10.1055/s-0042-116026
31. European Society of Radiology. Curriculum for undergraduate radiological education. (2021). Available at: https://www.myesr.org/app/uploads/2023/08/esr_curriculum_for_undergraduate_radiological_education_june_2021.pdf
32. Eysenbach, G. Improving the quality of web surveys: the checklist for reporting results of internet E-surveys. J Med Internet Res. (2004) 6:e34. doi: 10.2196/jmir.6.3.e34
33. von Elm, E, Altman, DG, Egger, M, Pocock, SJ, Gøtzsche, PC, Vandenbroucke, JP, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Epidemiology. (2007) 370:1453–7. doi: 10.1016/S0140-6736(07)61602-X
34. Gemino, A, Horner Reich, B, and Serrador, PM. Agile, traditional, and hybrid approaches to project success: is hybrid a poor second choice? Proj Manag J. (2021) 52:161–75. doi: 10.1177/8756972820973082
35. Tu, W, Hibbert, R, Kontolemos, M, Dang, W, Wood, T, Verma, R, et al. Diagnostic radiology residency assessment tools: a scoping review. Can Assoc Radiol J. (2021) 72:651–60. doi: 10.1177/0846537120981581
36. DiSantis, DJ. A step-by-step approach for creating good multiple-choice questions. Can Assoc Radiol J. (2020) 71:131–3. doi: 10.1177/0846537119888358
37. Lenzner, T, Neuert, C, and Otto, W, Cognitive Pretesting. GESIS Survey Guidelines. Mannheim: GESIS (2016).
38. Hassan, ZA, Schattner, P, and Mazza, D. Doing a pilot study: why is it essential? Malays Fam Physician. (2006) 1:70–3.
39. Bryer, J, and Speerschneider, K. Package “likert” (2016). Available at: https://cran.r-project.org/web/packages/likert/likert.pdf
40. Knapp, TR. Treating ordinal scales as interval scales: an attempt to resolve the controversy. Nurs Res. (1990) 39:121–3. doi: 10.1097/00006199-199003000-00019
41. DeLisa, JA, and Lindenthal, JJ. Commentary: reflections on diversity and inclusion in medical education. Acad Med. (2012) 87:1461–3. doi: 10.1097/ACM.0b013e31826b048c
42. Brown, SD, Rider, EA, Jamieson, K, Meyer, EC, Callahan, MJ, DeBenedectis, CM, et al. Development of a standardized Kalamazoo communication skills assessment tool for radiologists: validation, multisource reliability, and lessons learned. Am J Roentgenol. (2017) 209:351–7. doi: 10.2214/AJR.16.17439
43. O’Doherty, D, Dromey, M, Lougheed, J, Hannigan, A, Last, J, and McGrath, D. Barriers and solutions to online learning in medical education – an integrative review. BMC Med Educ. (2018) 18:130. doi: 10.1186/s12909-018-1240-0
44. Maloney, S, Haas, R, Keating, JL, Molloy, E, Jolly, B, Sims, J, et al. Breakeven, cost benefit, cost effectiveness, and willingness to pay for web-based versus face-to-face education delivery for health professionals. J Med Internet Res. (2012) 14:e47. doi: 10.2196/jmir.2040
45. Syed, S, Rastogi, A, Bansal, A, Kumar, A, Jindal, A, Prakash, A, et al. Future of e-learning in medical education—perception, readiness, and challenges in a developing country. Front Educ. (2021) 6:598309. doi: 10.3389/feduc.2021.598309
46. Bethlehem, J. Selection bias in web surveys. Int Stat Rev. (2010) 78:161–88. doi: 10.1111/j.1751-5823.2010.00112.x
47. Furnham, A. Response bias, social desirability and dissimulation. Pers Individ Dif. (1986) 7:385–400. doi: 10.1016/0191-8869(86)90014-0
48. Murdock, BB. The serial position effect of free recall. J Exp Psychol. (1962) 64:482–8. doi: 10.1037/h0045106
Keywords: medical education, online learning, blended learning, radiology education, thoracic imaging
Citation: Stoehr F, Yang Y, Müller L, Gerstenmeier P, Pinto dos Santos D, Dietz P, Weimer A, Ludwig M, Kloeckner R and Weimer JM (2023) A blended learning approach for teaching thoracic radiology to medical students: a proof-of-concept study. Front. Med. 10:1272893. doi: 10.3389/fmed.2023.1272893
Received: 04 August 2023; Accepted: 31 October 2023;
Published: 23 November 2023.
Edited by:
Lynn Valerie Monrouxe, The University of Sydney, AustraliaReviewed by:
Florian Recker, University of Bonn, GermanyCopyright © 2023 Stoehr, Yang, Müller, Gerstenmeier, Pinto dos Santos, Dietz, Weimer, Ludwig, Kloeckner and Weimer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Johannes Matthias Weimer, V2VpbWVyQHVuaS1tYWluei5kZQ==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.