- 1Third Department of Sports Medicine, Wangjing Hospital, China Academy of Chinese Medical Sciences, Beijing, China
- 2Beijing Key Laboratory of Bone Setting Technology of Traditional Chinese Medicine, Beijing, China
- 3Second Department of Spine, Wangjing Hospital, China Academy of Chinese Medical Sciences, Beijing, China
- 4Department of Orthopedics, Tianjin Hospital, Tianjin, China
Background: Traditional Chinese exercises (TCEs) have played a significant role in treating various diseases. However, there is limited research assessing the efficacy of TCEs in treating Lumbar disc herniation (LDH). This study aimed to systematically evaluate the effects of four commonly used TCEs (Baduanjin, Yijinjing, Taichi, and Wuqinxi) on pain and disability in elderly patients with LDH.
Objectives: To assess the quality of relevant randomized controlled trials (RCTs) to provide evidence support for the treatment of LDH.
Methods: RCTs were identified through eight databases. Meta-analysis and trial sequence analysis (TSA) were conducted using RevMan 5.4, Stata 17.0, and TSA 0.9.
Results: A total of 22 RCTs, involving 1931 patients, were included in the analysis. TCEs exhibited a superior effectiveness in treating LDH compared to the control group. However, the TSA analysis suggested the possibility of false positives, indicating the need for more high-quality RCT evidence. Nevertheless, TCEs showed reliable results in significantly improving the VAS score and JOA score of LDH patients.
Conclusion: Current evidence indicates that the four TCEs have advantages in treating LDH in middle-aged and elderly individuals. However, considering the limitations of this study, we need to exercise caution in drawing conclusions, and further research is required to validate these findings.
Systematic Review Registration: http://www.crd.york.ac.uk/PROSPERO, identifier [CRD42023431633].
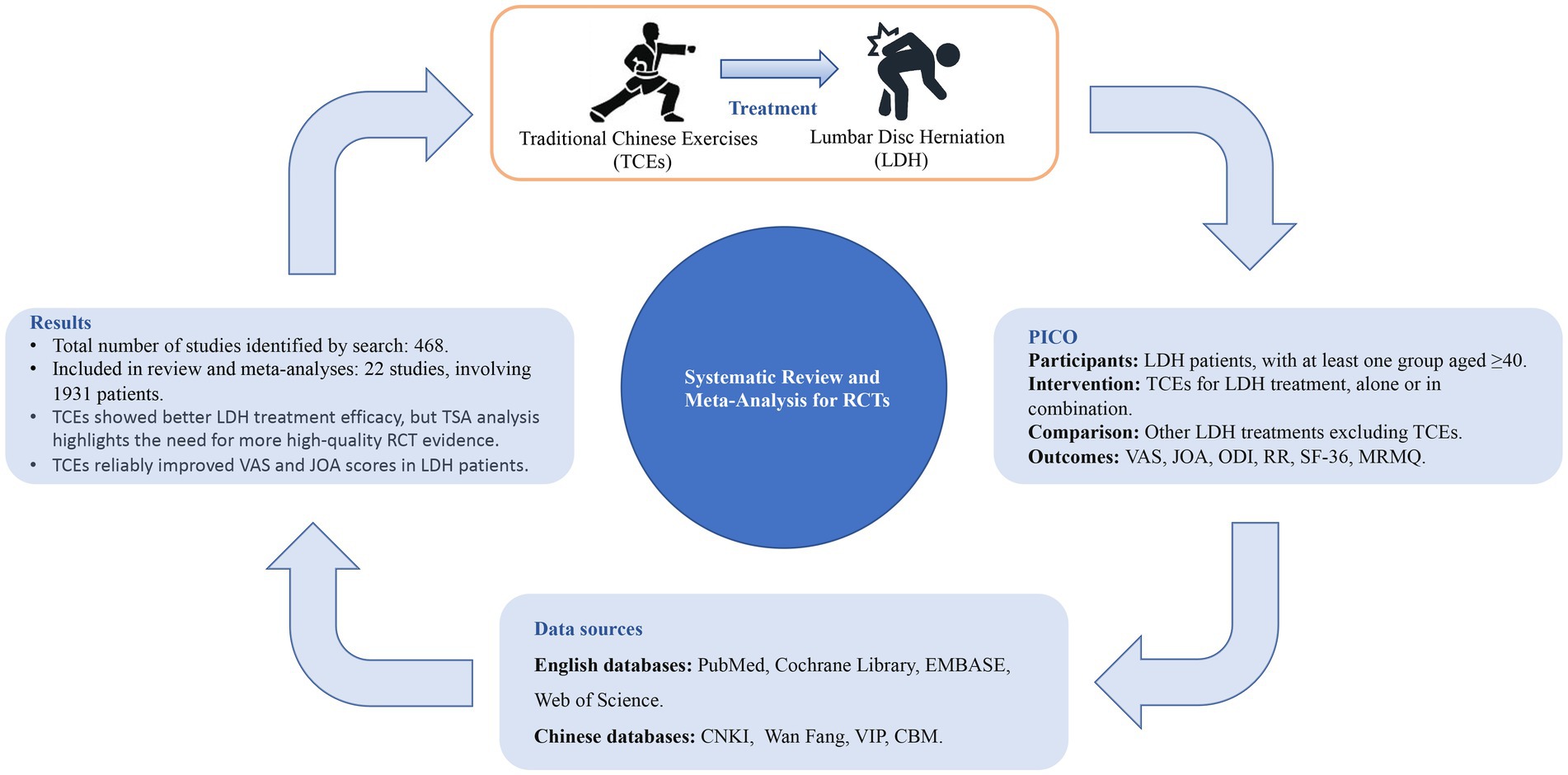
Graphical Abstract. CNKI, China National Knowledge Infrastructure; Wan Fang, Wan Fang data; VIP, China Science and Technology Journal Database; CBM, Chinese Biomedical Literature Database; RCTs, randomized controlled trial; TSA, trial sequence analysis; VAS, visual analog scale; JOA, Japanese orthopedic association Scores; ODI, oswestry disability index; RR, response rate; SF-36, 36-Item Short Form Survey; MRMQ, Modified Roland-Morris Disability Questionnaire.
1. Introduction
Lumbar disc herniation (LDH) is a prevalent source of pain in the lower back and legs among adults. This condition significantly impacts their health and quality of life, placing a substantial burden on both society and families. LDH occurs when the nucleus pulposus of an intervertebral disc protrudes from its normal position, leading to the development of this ailment (1). Apart from lumbar spinal stenosis, spondylolisthesis, and fractures, herniated intervertebral discs have been found to be the primary cause of radicular pain (2).
Research has demonstrated that more than 90% of individuals within the middle-aged and elderly cohorts who suffer from LDH exhibit mechanical anomalies within their spinal and musculoskeletal structures (3). The lifetime prevalence of lumbar pain is 84%, with higher incidence rates among middle-aged and elderly populations, with 60% of patients also experiencing symptoms of leg pain (4). Chronic lumbar pain and limited lower limb function caused by LDH have led to poor quality of life and high disability rates among patients, indicating the need for treatment with high social costs (5).
However, China is also facing the enormous medical challenge brought about by population aging. According to survey and projected results, by 2050, there will be 400 million citizens in China aged 65 and above, including 150 million who are 80 years and older (6). Hence, as we aim to enhance the diagnosis and treatment of LDH, we must address its significant societal costs and explore cost-effective methods to ameliorate or cure symptoms in middle-aged and elderly LDH patients. LDH can be treated through surgical and non-surgical means, with most researchers advocating non-surgical options as the primary approach (7–8).
Traditional Chinese exercises (TCEs), through inheritance and reform, have been widely used as a conservative and complementary therapy in the treatment of mental disorders, endocrine disorders, orthopedic diseases, and the management of obesity (9–12). TCEs such as Baduanjin (BDJ), Yijinjing (YJJ), Taichi (TC), and Wuqinxi (WQX) have also been proven to improve pain and physical function in patients with LDH (13), showing good treatment effects in middle-aged and elderly patients (14, 15). TCEs present notable advantages. Firstly, they necessitate no specialized facilities or expensive equipment, allowing for flexibility in practice locations and timing. Secondly, TCEs effectively improve aerobic capacity, muscle strength, and balance. Thirdly, their low cost and straightforward technical requirements facilitate seamless community-wide adoption, endowing TCEs with considerable clinical value (16).
The evidence regarding the improvement of pain and disability in LDH through TCEs remains controversial. Therefore, the present systematic review aimed to assess the impacts of TCEs on pain and disability among middle-aged and elderly patients with LDH. This review offers evidence-based information that can be utilized in the clinical implementation of TCEs for LDH.
2. Methods
2.1. Data sources and search strategies
The Materials We conducted a comprehensive search across eight electronic databases, including four English databases (PubMed, Cochrane Library, EMBASE, and Web of Science) and four Chinese databases (China National Knowledge Infrastructure [CNKI], Wan Fang data [Wan Fang], China Science and Technology Journal Database [VIP], and Chinese Biomedical Literature Database [CBM]), from inception to May 1, 2023. No language restrictions were imposed. The search was performed by three researchers (WZ, GW, RX), and any discrepancies between the researchers were resolved through discussion. Additionally, all potentially relevant articles were examined and discussed to identify any additional studies.
The primary search terms used were (“traditional Chinese exercises” OR “qi gong” OR “Qigong” OR “Tai Chi” OR “tai ji” OR “ba duan jin” OR “Baduanjin” OR “yi jin jing” OR “Yijinjing” OR “Five-animal exercises” OR “wu qin xi” OR “Wuqinxi”) and (“lumbar disc herniation” OR “disc herniation”). To identify additional relevant studies, we examined the reference lists of relevant reviews. The World Health Organization International Clinical Trials Registry Platform (ICTRP) and the Chinese Clinical Trial Registry (ChiCTR) were also searched to identify ongoing or unpublished studies. In case of necessity, the reviewers made direct contact with the authors of the included studies. No restrictions were applied in terms of publication language or status.
2.2. Study selection and eligibility
2.2.1. Types of studies
The objective of this meta-analysis was to examine the effectiveness of TCEs including BDJ, YJJ, TC, and WQX in reducing pain and disability levels in middle-aged and elderly patients with LDH. All the studies considered in this analysis were RCTs and were not restricted based on publication status. Excluded from the analysis were cross-sectional studies, animal experiments, systematic reviews and meta-analyses, disease guidelines, as well as studies for which we did not have access to the full texts.
2.2.2. Types of participants
Participants included in the study had a clinical diagnosis of LDH, with at least one group having an average age of 40 years or older. There were no specific restrictions based on gender or nationality.
2.2.3. Types of intervention
The control interventions encompassed various approaches such as waiting list, education, routine rehabilitation therapy, acupuncture, medicine, other modern exercise therapy, and alternative treatments that did not involve TCEs. It is crucial to highlight that TCEs were the exclusive exposure factor, with all other interventions remaining uniform across both groups.
2.2.4. Types of measured outcomes
The focus of assessment will concentrate on evaluating the effectiveness of treatment through pre- and post-treatment efficacy evaluations, encompassing visual analog scale (VAS), Japanese orthopedic association Scores (JOA), and oswestry disability index (ODI). Additionally, secondary outcome measures of interest will comprise of response rate (RR), 36-Item Short Form Survey (SF-36), and Modified Roland-Morris Disability Questionnaire (MRMQ).
2.3. Data synthesis and extraction
The extraction of data was carried out independently by two reviewers (WZ, GW) according to pre-established criteria. The reviewers collected the following data: (1) fundamental details such as the first author’s name, publication year, and country; (2) participant characteristics including sample size and average age; (3) study design information such as interventions, outcomes, and duration of follow-up. Any disagreements were resolved through discussions between two reviewers and through communication with a third researcher (JZ). Duplicate articles were excluded using the EndnoteX20 software.
2.4. Literature quality assessment
Two researchers (WZ and GW) autonomously appraised the literature’s quality incorporated into this investigation, employing the methodological quality assessment criteria delineated in the Cochrane Handbook for Systematic Reviews of Interventions. A third researcher, JZ, was consulted to resolve any disagreements and finalize the results. The risk of bias assessments for all the included randomized controlled trials (RCTs) were reported as per the guidelines provided in the Cochrane Handbook for Systematic Reviews of Interventions. The criteria mainly considered were: (A) random sequence generation, (B) allocation concealment design treatment, (C) participant and rater blinding, (D) withdrawal and loss of follow-up, (E) incomplete outcome data and selective outcome reporting, and (F) other sources of bias. The evaluation methods employed were categorized as high risk of bias, low risk of bias, or unknown risk of bias.
2.5. Statistical analysis
The meta-analysis was performed using RevMan version 5.3 (The Cochrane Collaboration, Software Update, Oxford, United Kingdom). In the meta-analysis, the between-group mean differences of the studies for continuous outcomes were converted to the standardized mean difference (SMD) with 95% confidence intervals (CI). A random effects model was employed to account for clinical heterogeneity. In cases where there was no substantial heterogeneity (I2 ≤ 50%), a fixed-effects model was utilized. However, if significant heterogeneity was present, a random-effects model was applied. Subgroup analysis was conducted based on different types of control interventions and treatment effect modifiers. To assess the risk of publication bias, a funnel plot was used in meta-analyses including more than nine trials. Statistical significance was considered at p < 0.05. Trial Sequential Analysis (TSA) version 0.9 was used to perform trial sequence analysis.
3. Results
3.1. Study selection
At the beginning, 486 potentially relevant articles were gathered from the databases mentioned, namely PubMed, Cochrane Library, EMBASE, Web of Science, CNKI, Wang Fang, VIP, and CBM. Among them, 221 duplicate articles were eliminated by employing EndNote software for verification. By reviewing titles and/or abstracts, 201 articles that did not meet the criteria were excluded, resulting in 64 studies after the initial screening. After thoroughly examining the full text, 22 studies were ultimately included. Please review the PRISMA Flow Diagram (17) prepared in accordance with PRISMA guidelines (Figure 1).
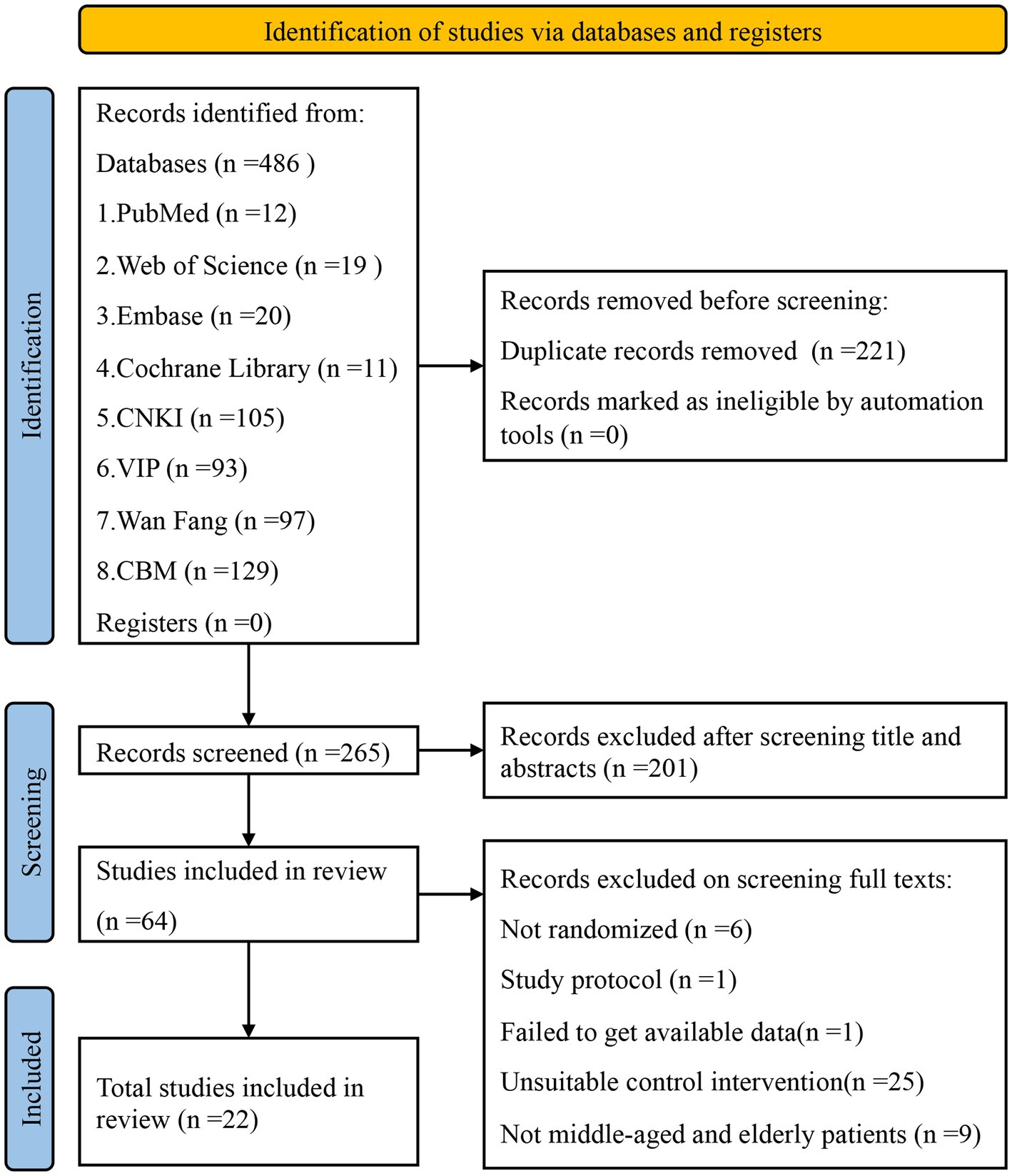
Figure 1. PRISMA flow chart of studies through the review. PRISMA, preferred reporting items for systematic reviews and meta-analyses.
3.2. Study characteristics
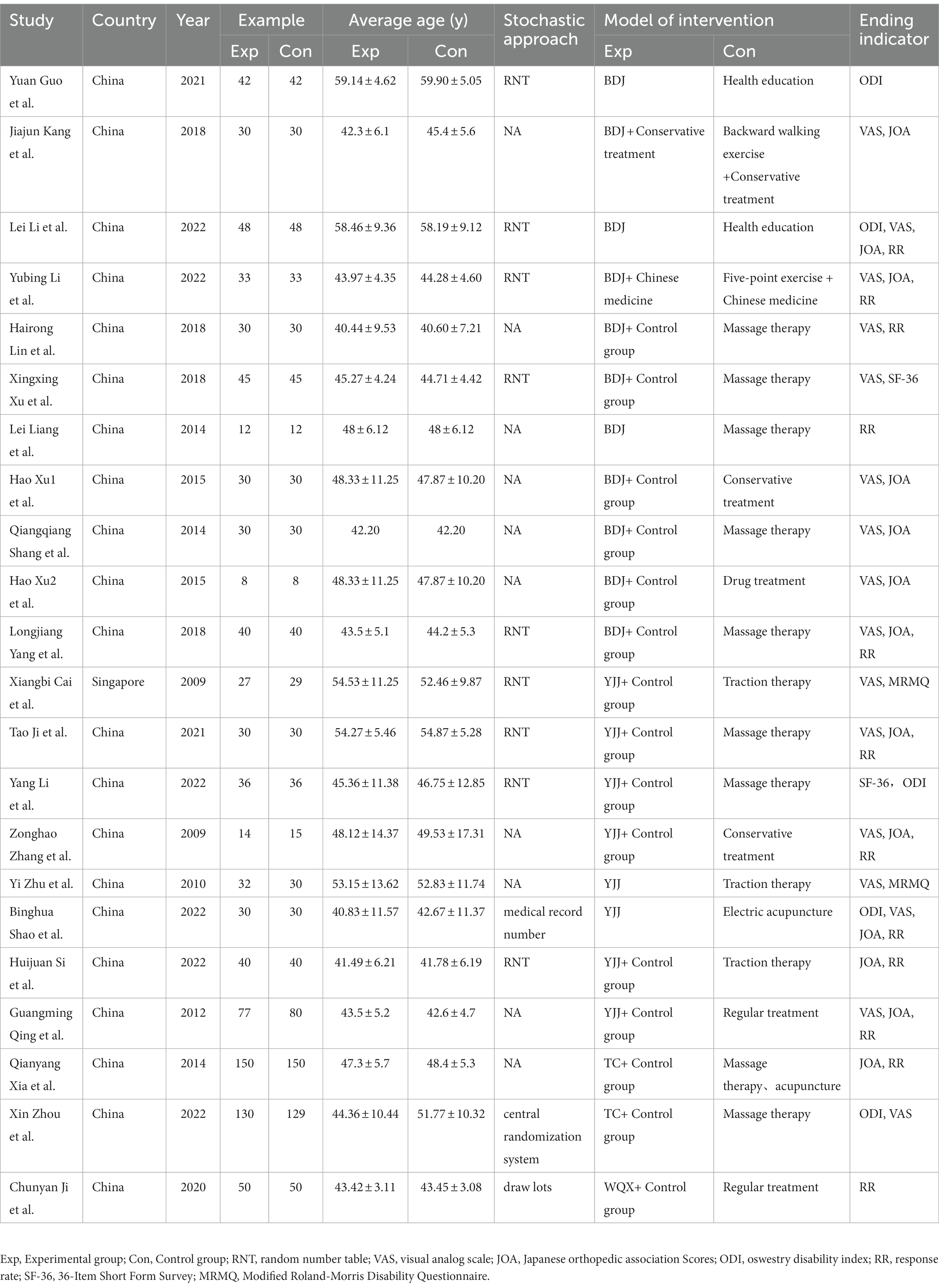
A total of 22 trials (18–39) with a parallel randomized control design were identified. In this review, a total of 1931 participants were included, with 964 in the experimental group and 967 in the control group. One study (22) was conducted in Singapore, while the remaining studies were conducted in China. Lastly, detailed characteristics of the 22 included trials were provided in Table 1.
3.3. Quality assessment of the included literature
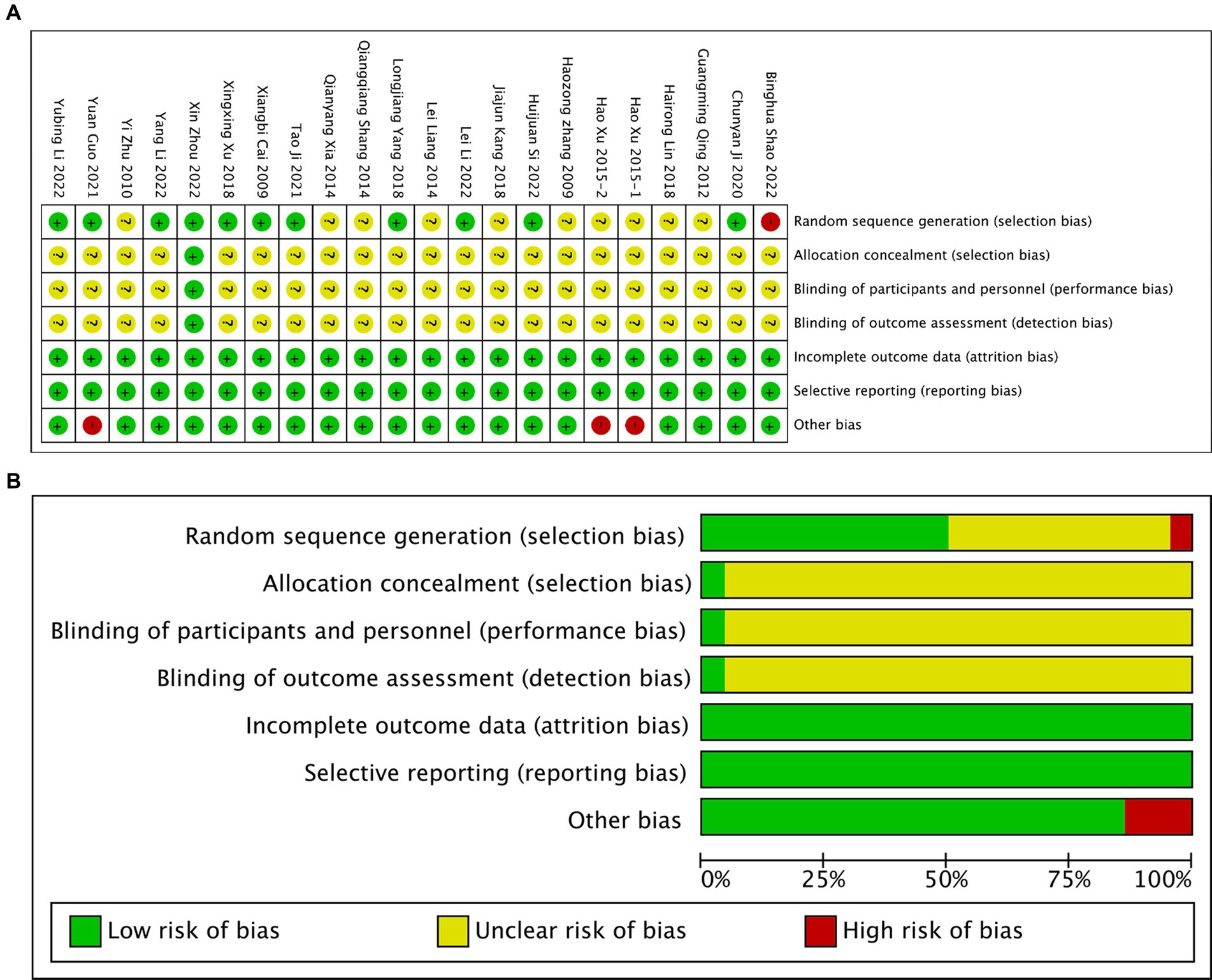
The results of the literature quality assessment can be observed in Figure 2. All the trials included in this review were randomized, with nine of them employing random number tables for allocation (19–21, 23, 24, 26–28, 30–33). Only one trial (32) mentioned allocation concealment, which can be attributed to the unique nature of TCEs. It is important to note that blinding is challenging to implement in trials involving TCEs as an intervention. No relevant protocols were identified on the ClinicalTrials.gov website. In most studies, the intervention group received TCEs in combination with other treatments (such as traditional therapies, stretching, acupuncture, and medication therapy). These intervention groups were compared to control groups receiving corresponding traditional treatment methods. The frequency of treatment in the intervention group varied from three times per week to twice daily.
3.4. Effectiveness
3.4.1. VAS score
In the studies included a total of 16 experiments utilized VAS score to evaluate the pain associated with LDH. The application of a random-effect model for meta-analysis revealed a statistically significant finding that the VAS score in the treatment group was lower than that of the control group [MD = −0.66, 95% CI (−0.89, −0.42) and p < 0.01; Figure 3A]. However, it is important to note that there was a high level of heterogeneity among the studies (I2 = 77%, p < 0.01). A funnel plot analysis demonstrated no evident publication bias (Begg’s Test p = 0.964, Egger’s test p = 0.253; Figures 3B,C). To further validate the results, a sensitivity analysis was conducted, and the outcomes indicated that although there was considerable heterogeneity among the studies, the results remained robust (Figure 3D). Based on the different types of TCES, a subgroup analysis was performed for exercise types, including 9 experiments focused on Baduanjin (BDJ) and 6 experiments on Yijinjing (YJJ), which were then included in the META analysis (Figure 3E). The results showed that the VAS scores of the BDJ group were significantly lower than those of the control group [MD = −0.58, 95% CI (−0.87, −0.28) and p < 0.01], and similarly, the VAS scores of the YJJ group were significantly lower than those of the control group [MD = −0.75, 95% CI (−1.28, −0.23) and p < 0.01]. A META regression analysis was conducted for the subgroups, and the results indicated [95% CI (−0.74, 0.40) and p = 0.536], signifying that there was no significant difference in the degree of improvement in VAS scores between the two groups.
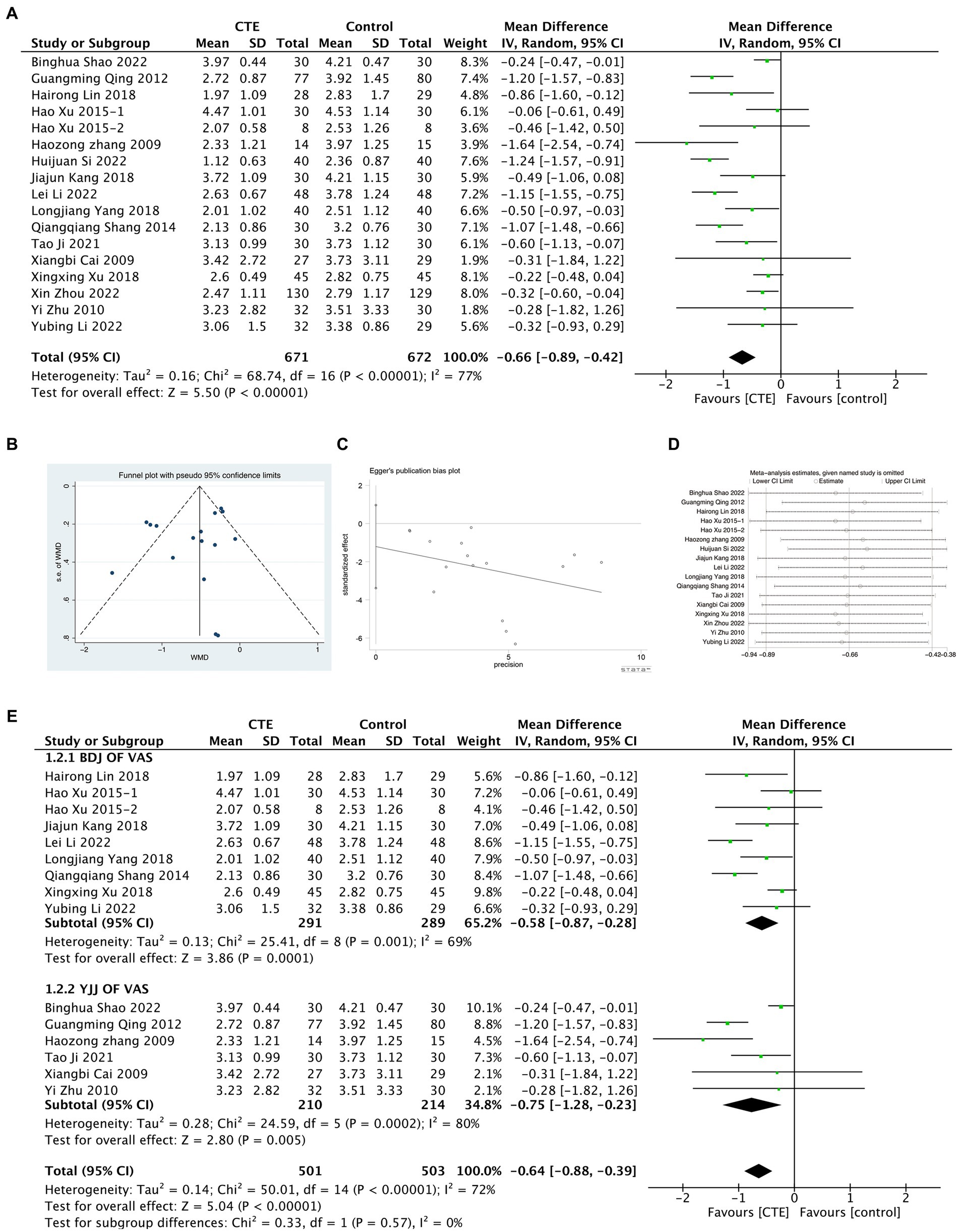
Figure 3. Meta-analysis results graph of VAS scores. (A) Forest plot comparing VAS scores between the treatment group and the control group. (B,C) Funnel plot of publication bias analysis results. (D) Sensitivity analysis results graph. (E) Forest plot of subgroup analysis between BDJ group and YJJ group.
3.4.2. JOA score
A total of 13 experiments were included in the study to evaluate the functional impairment of LDH using the JOA score. Meta-analysis, employing the random effect model, indicated a significant difference in the JOA score between the treatment and control groups [MD = 3.01, 95% CI (2.38, 3.64), p < 0.01; Figure 4A]. However, considerable heterogeneity was observed among the studies (I2 = 81%, p < 0.01). Publication bias was identified after conducting a funnel plot and tests of Begg and Egger (p = 0.127 and p = 0.026, respectively; Figures 4B,C). To address this bias, a sensitivity analysis was performed, confirming the robustness of the results despite the high heterogeneity (Figure 4D). Furthermore, subgroup analyses were carried out on studies with more than two experiments, based on different types of TCEs. The results demonstrated that the BDJ group exhibited a significantly higher JOA score than the control group [MD = 2.75, 95% CI (2.14, 3.35), p < 0.00001], whereas the YJJ group had a significantly lower JOA score [MD = 4.11, 95% CI (2.09, 6.13), p < 0.01]. Subgroup meta-regression analysis did not indicate a significant difference in the improvement of VAS between the two groups [95% CI (−0.97, 3.11), p < 0.01; Figure 4E].
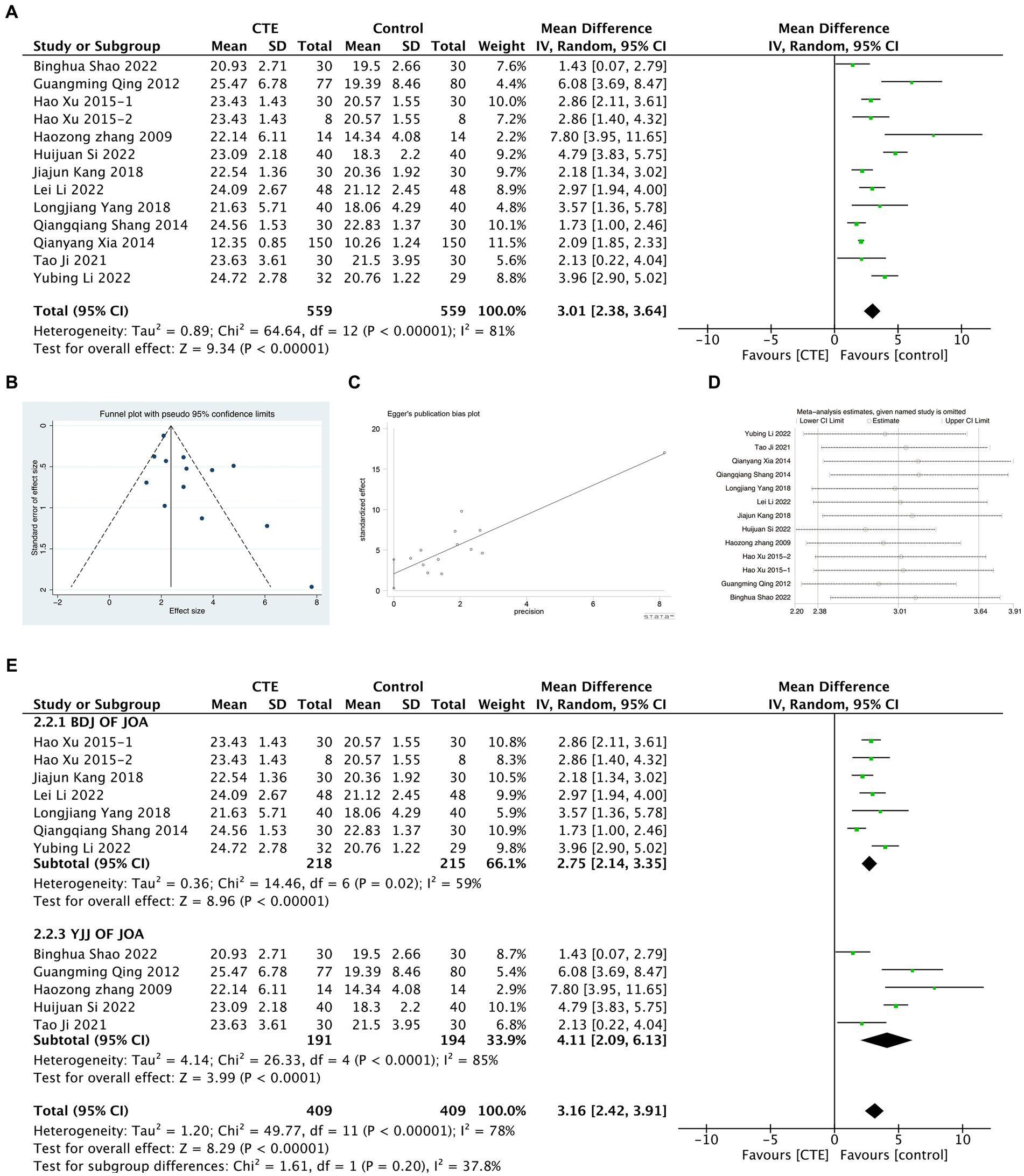
Figure 4. Meta-analysis results graph of JOA scores. (A) Forest plot comparing JOA scores between the treatment group and the control group. (B,C) Funnel plot of publication bias analysis results. (D) Sensitivity analysis results graph. (E) Forest plot of subgroup analysis between BDJ group and YJJ group.
3.4.3. ODI score
A total of five experiments were included in the study, which utilized the ODI score. The meta-analysis, using a random-effects model, revealed a significant difference in the ODI score between the treatment and control groups, with statistical significance [MD = −3.36, 95% CI (−6.23, −0.49), p = 0.02, I2 = 98%; Figure 5A]. Due to the limited number of included studies, the detection of publication bias was not conducted. However, the sensitivity analysis confirmed the robustness of the results (Figure 5D). Nevertheless, one study (23) demonstrated significant differences compared to the other four studies in the sensitivity analysis. Consequently, this study was excluded, and subsequent meta-analysis was performed, resulting in a significant decrease in heterogeneity [MD = −0.94, 95% CI (−1.34, −0.55), p < 0.01, I2 = 49%; Figure 5B]. These findings indicated that the excluded study was the main source of heterogeneity. Additionally, subgroup analysis was conducted on studies that included two experiments, based on different types of TCEs. The analysis results revealed no significant differences in improving the ODI score compared to the control group for both the Baduanjin and Yijinjing exercise types. The combined subgroups exhibited high heterogeneity (I2 = 98%), with the Baduanjin group demonstrating even higher heterogeneity (I2 = 99%), further supporting the notion that the study conducted by Li (23) was the primary source of heterogeneity (Figure 5C). The meta-regression analysis for the subgroups showed no significant association between the heterogeneity among the studies and the type of exercise [95% CI (−15.54, 20.60), p = 0.608].
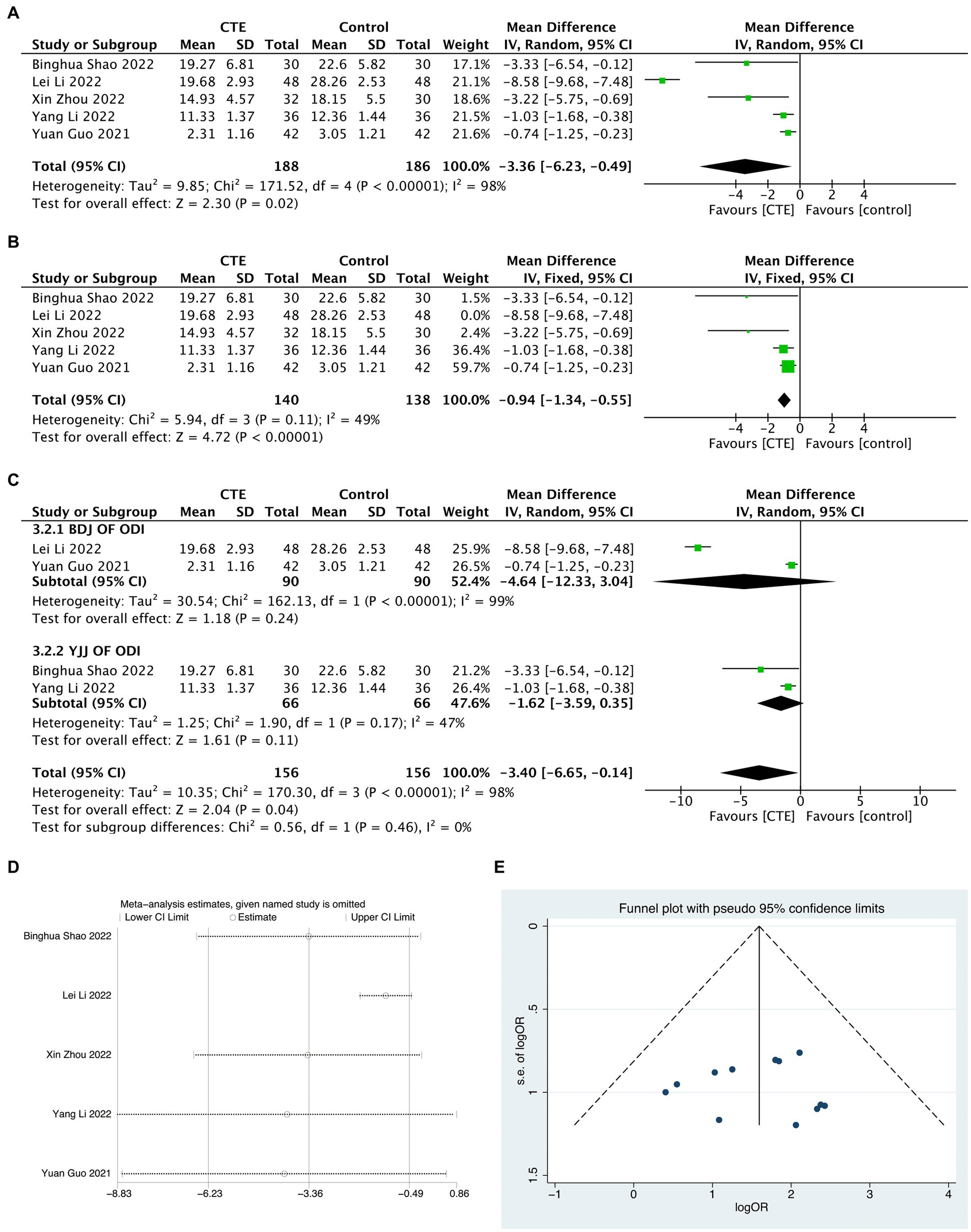
Figure 5. Meta-analysis results graph of ODI scores and response rate. (A) Meta-analysis results graph of ODI scores. (B) Forest plot of ODI scores after sensitivity analysis. (C) Forest plot of ODI scores after sensitivity analysis. (D) Sensitivity analysis results graph of ODI scores. (E) Funnel plot of publication bias analysis results for response rate.
3.4.4. Response rate
A total of 12 studies were included in the analysis, using Response Rate to indicate treatment efficacy. Due to low heterogeneity after combining the studies (I2 = 0%), a fixed-effect model was employed for the META analysis [OR = 5.34, 95% CI (3.18, 8.95), and p < 0.01; Figure 6A]. Funnel plot analysis did not reveal any significant publication bias (Begg p = 0.945, Egger p = 0.931; Figure 5E). Subgroup analysis was conducted for studies that included 2 experiments, and the results indicated that both Baduanjin and Yijinjing demonstrated significant effects on DLH (Figure 6B).
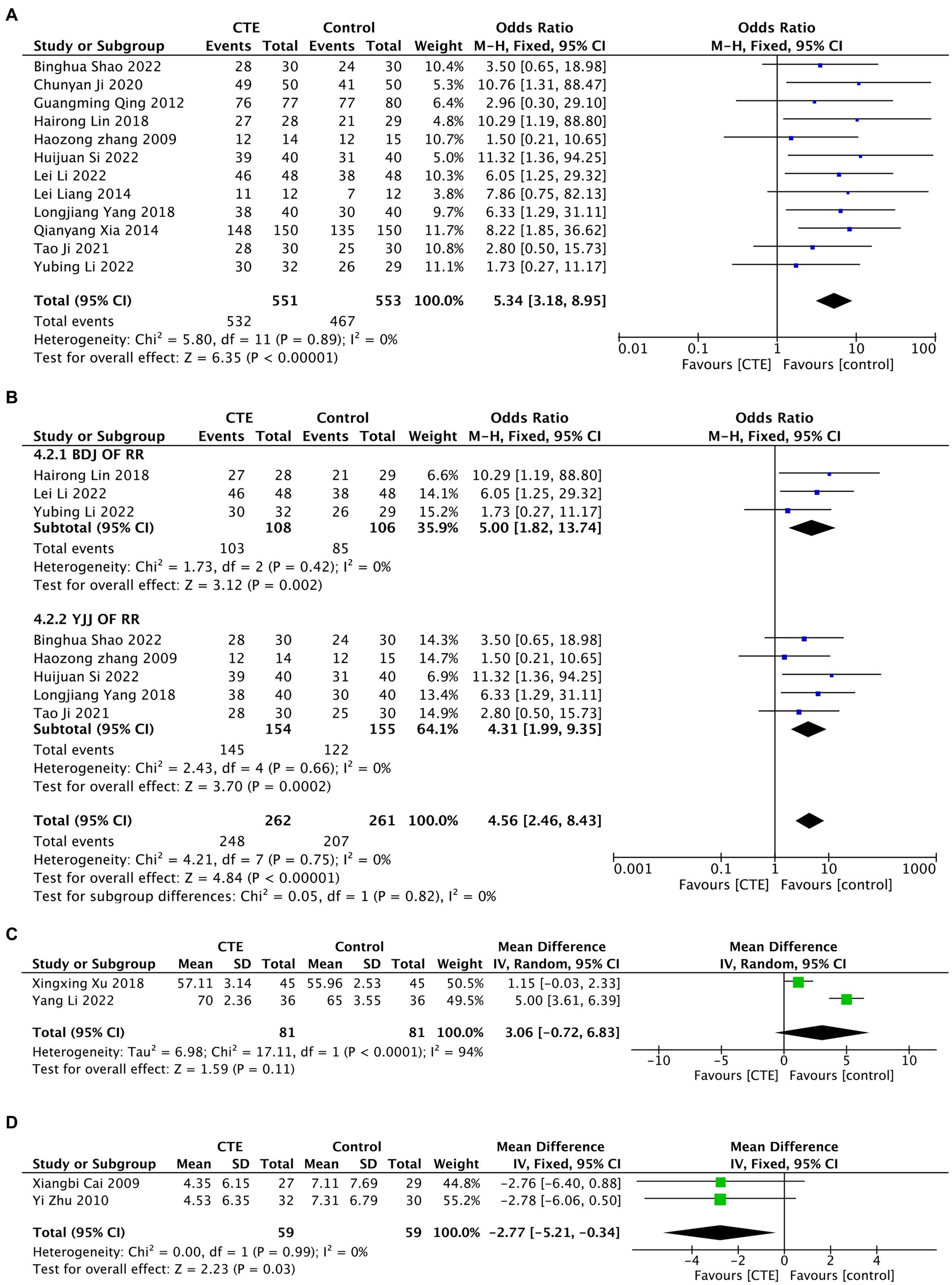
Figure 6. Meta-analysis results graph. (A) Forest plot of meta-analysis results graph for response rate. (B) Forest plot of subgroup analysis for response rate in BDJ group and YJJ group. (C) Forest plot of meta-analysis results graph for SF-36. (D) Forest plot of meta-analysis results graph for MRMQ scores.
3.4.5. SF-36 score
Two studies using the SF-36 score were included in the analysis. Due to significant heterogeneity, a random-effects model was employed for the meta-analysis [MD = 3.06, 95% CI (−0.72, 6.83), and p = 0.11, I2 = 94%; Figure 6C]. These findings suggest that TCEs may not effectively improve the SF-36 score for LDH. However, the sensitivity analysis indicated that the meta-analysis results were not robust, and the high heterogeneity may be attributed to the inclusion of two studies with different types of exercise and the limited number of studies included (Figure 7A).
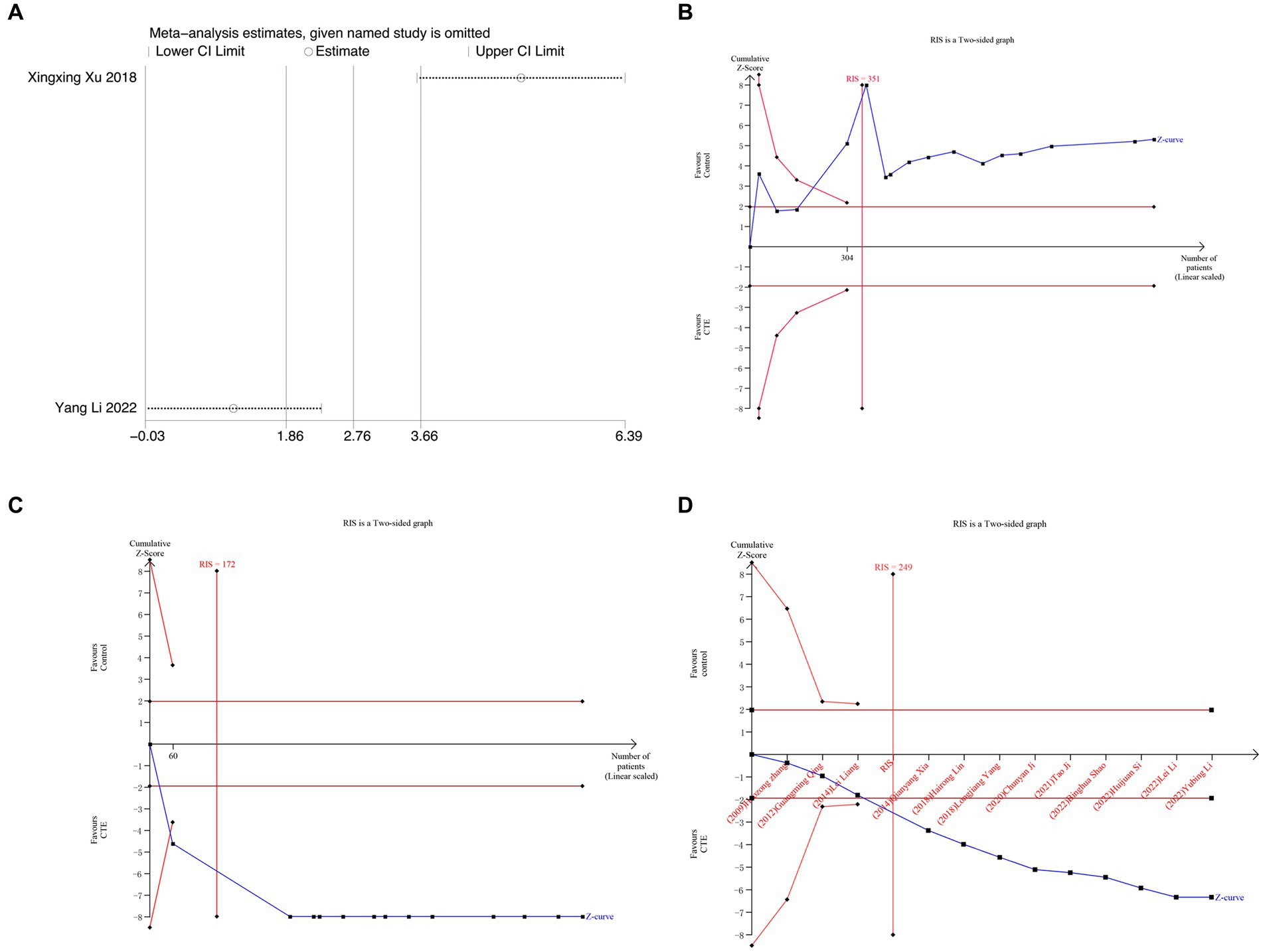
Figure 7. Meta-analysis and TSA analysis results graph. (A) Sensitivity analysis results graph for SF-36 scores. (B) VAS scores TSA analysis results graph. (C) TSA analysis results graph of JOA scores. (D) TSA analysis results graph of response rate.
3.4.6. MRMQ score
Two studies were included in the analysis, and the MRMQ score was utilized in the research. Given the low heterogeneity, a fixed-effects model was employed for the meta-analysis, revealing a statistically significant reduction in SF-36 scores of LDH with TCEs [MD = −2.77, 95% CI (−5.21, −0.34), p = 0.03, I2 = 0%; Figure 6D]. Furthermore, the patient function improved as a result.
3.4.7. Safety
None of the 22 studies indicated that participants experienced any significant adverse reactions or uncomfortable symptoms.
3.5. Trial sequence analysis
Separate TSA was carried out for VAS, JOA, and RR. The required information size (RIS) was determined for each outcome measure: 351 for VAS, 172 for JOA, and 249 for RR. RIS was calculated by considering statistical indicators such as the type I error probability (α = 0.05), type II error probability (β = 0.2), mean difference, and variance data obtained from this meta-analysis. The results of TSA for VAS (Figure 7B) and JOA (Figure 7C) demonstrated that the cumulative Z value surpassed both the traditional and TSA thresholds, leading to a positive conclusion before the expected information quantity was reached. This suggests that CTEs exhibit a beneficial effect compared to the control group in reducing pain and improving function among LDH patients, and the evidence is conclusive. Nevertheless, the TSA results for RR (Figure 7D), which represents the efficacy rate, hinted at a possibility of false positive statistical difference. This indicates the necessity for future high-quality RCT studies to confirm the findings.
4. Discussion
4.1. Diagnosis of LDH
The diagnosis of LDH is challenging due to its multifaceted nature. The latest guidelines from the Japanese Orthopaedic Association emphasize a comprehensive approach, integrating symptoms, medical history, physical exams, and radiological findings. Consistency, particularly between physical exams and imaging, is crucial (40). The North American Spine Society similarly recommends a combined approach, using Manual Muscle Testing, Sensory Testing, Supine Straight Leg Raise, Lasegue Sign, and Crossed Lasegue Sign in conjunction with advanced imaging, primarily MRI, CT or CT myelography may complement when needed (41).
Prudent clinical judgment necessitates circumventing a sole reliance on radiological findings for diagnosis, as a comprehensive systematic study has illuminated the moderate diagnostic accuracy of the three imaging techniques (MRI, CT, CT myelography), potentially leading the clinician astray (42). Typical LDH symptoms include lumbar-sacral, lower limb, and perineal pain, sensory deficits, and, in severe cases, urinary and fecal dysfunction (43).
All patients included in this study had a confirmed diagnosis of LDH, albeit based on a comprehensive assessment of findings. Nevertheless, there exists inconsistency among the reference clinical practice guidelines consulted. Therefore, continuous updates to LDH clinical guidelines and intensified training of healthcare providers are imperative to enhance diagnostic consistency, ultimately fostering advancements in the treatment and research of LDH.
4.2. Clinical implications
The treatment of LDH is continually evolving, with two main approaches: conservative and surgical, as outlined in the latest clinical treatment guidelines (44). Conservative treatment remains the first-line therapy for LDH because symptoms tend to gradually improve as the herniated disc material causing them is absorbed. However, the choice between conservative and surgical treatments should be based on the patient’s individual circumstances and evidence from evidence-based medicine.
Lower back pain is one of the most common symptoms associated with LDH, with approximately 159.1 out of every 100,000 people worldwide seeking hospital treatment for disc-related lower back pain (45). It is typically categorized into no-radicular low back pain and radicular low back pain for differential treatment. Evidence-based medical research suggests that surgical treatment does not significantly outperform conservative treatment for no-radicular low back pain. However, for LDH accompanied by radicular low back pain, while conservative treatment can be effective (46), surgical treatment has short-term advantages in pain relief, although these advantages tend to diminish in long-term follow-ups (47, 48). For the elderly population under this study, evidence-based medicine research indicates that exercise can help alleviate the severity of lower back pain in older adults and may be considered as a medical intervention for this demographic (49).
However, it is important not to overlook the potential for exercise-induced biomechanical factors in the spine that can trigger or exacerbate lower back pain. Recent research by Baraldo et al. (50) on the relationship between lower back pain and strength training in elite athletes has found that the overall prevalence of lower back pain among athletes is at least 40%. In athletes engaged in high-intensity weightlifting, the probability of developing radiating lower back pain is as high as 54%. This may be attributed to the heavy loads placed on the spine during weightlifting, leading to increased risk of muscle injury and disc herniation, ultimately contributing to lower back pain. Their research also found that female athletes or older athletes have a higher incidence of illness. This suggests that doctors or physical therapists, when devising exercise plans for LDH patients, should consider both the nature of the exercise and the characteristics of the exercise population, to reduce the adverse effects of incorrect exercise.
Disability is one of the severe consequences of LDH, encompassing not only limited lumbar spine mobility, lower limb muscle weakness, and lower limb sensory impairment (40), but also a decrease in the patient’s ability to perform daily activities and interact socially due to LDH, leading to psychological disorders such as depression, insomnia, and reduced communication skills. This gradually evolves into a global public health issue awaiting better solutions, implying a significant societal cost (5). Multiple research findings suggest that when treating LDH and lower back pain, the patient’s psychological factors must be considered (51). Ballestra et al. (52) latest review found that for chronic lower back pain patients with a strong desire for pain relief, personalized counseling and treatment plans should be provided, adhering to a patient-centered care approach and a better understanding of the patient’s emotions and psychology, as patient expectations are significantly related to treatment outcomes. This suggests that physicians and family members, when combined with the correct treatment methods and strong patient motivation for recovery, can lead to a more optimistic prognosis.
TCEs are a form of patient-initiated physical activity that has gained widespread popularity in China and globally as a fitness regimen. Notable for their gentle exercise routines and moderate force application, TCEs have demonstrated applications and have been reported in the improvement of human balance, flexibility, skeletal muscle function, cardiovascular health, and respiratory system diseases, among others (53, 54).
4.3. TCEs treatment for LDH
TCEs, which encompass a wide range of exercise forms, were studied in this research, with a focus on the four most common forms: BDJ, YJJ, TC, and WXQ. Specifically, there were 11experiments on BDJ, 8 experiments on YJJ, 2 experiments on TC, and 1 experiment on WXQ. The mean age of the study participants was confined to individuals aged 40 years and older, as degenerative spinal changes leading to LDH are more prone to manifest in the middle-aged and elderly individuals. The analysis of the results showed promising findings, indicating significant therapeutic effects of all four TCEs in treating LDH. Notably, BDJ and YJJ demonstrated significant improvements in VAS scores and JOA scores of LDH. However, sub-group analysis revealed that these exercise modalities did not have a significant impact on ODI scores. This could potentially be attributed to the limited number of eligible studies and high heterogeneity, as determined through sensitivity analysis and META regression analysis. The statistical results for SF-36 and MRMQ scores varied, but caution is advised due to the limited number of studies included for these two indicators.
According to the existing literature, TCEs have the potential to alleviate pain and functional impairments in LDH patients through various mechanisms. Firstly, TCEs aid in the improvement of osteoporosis and the increase of bone mineral density. There is a widely recognized association between bone density and the occurrence of LDH (55, 56). As individuals age, a decline in bone mineral density becomes a major contributor to fractures and degenerative changes in the elderly. Therefore, enhancing or preserving bone density is a crucial treatment approach for LDH. For middle-aged and elderly individuals with low bone mass, exercise serves as an effective method to stimulate bone formation (57). TCEs, being aerobic exercises, have demonstrated the ability to regulate bone mineral density. For instance, BDJ applies pressure stimulation on the skeleton, which contributes to the regulation of bone mass (58). Regular and moderate TCEs can also modulate the endocrine system by promoting the secretion of hormones such as estrogen and irisin, which facilitate bone formation (59). As a result, this improvement in bone density can effectively alleviate patient pain (60).
Additionally, TCEs have been shown to improve muscle strength, enhance patient stability, and address mobility limitations. Moderate exercise with Tai Chi has been found to effectively improve balance and leg strength in patients (61). Furthermore, YJJ can improve skeletal muscle quality in middle-aged and elderly individuals with muscle loss (62). A study conducted in Spain revealed that Tai Chi significantly reduces acute pain in patients with muscle pain (63) and decreases the likelihood of falls and balance loss in older adults (64). Biomechanical experimentation showed that WQX, primarily performed while kneeling, can strengthen the lumbar muscles and increase spinal mobility (65). Moreover, a retrospective cohort study indicated that practicing Tai Chi can delay the imaging degeneration of LDH in middle-aged and older adults (15). As a complementary therapy, TCEs may also contribute to spinal balance (66) and provide relief from lower back pain (67). These studies collectively support the effectiveness of TCEs in improving pain and mobility limitations in patients.
In addition, there is evidence from evidence-based medicine supporting the benefits of TCEs in improving mental well-being (68), regulating the endocrine system (69), alleviating symptoms of arthritis (70), and helping middle-aged and elderly individuals reduce oxidative stress (71). For example, practicing BDJ can enhance cognitive function in older adults and alleviate musculoskeletal pain in chronic disease patients, thereby significantly improving sleep quality (72, 73). Enhancing mental well-being and regulating the endocrine system can significantly improve individuals’ daily life abilities, social interactions, and self-rehabilitation potential. Consequently, these improvements can provide valuable assistance in the rehabilitation of individuals with LDH.
This study has certain limitations. Firstly, among the RCTs included in this study, apart from one conducted in Singapore, the remaining 21 were all conducted in mainland China, which could introduce bias in the research results due to geographical constraints. Secondly, the number of studies for certain indicators is too limited to perform a more detailed and accurate data synthesis. The accuracy of the current stage’s data synthesis results is questionable, and further high-quality RCT research is needed in the future for validation. In the future, if more high-quality RCT articles are published, we will continue this study.
5. Conclusion
This study summarizes the evidence of TCEs treatment for Middle-Aged and Elderly Patients LDH from 22 RCT trials. Our preliminary meta-analysis suggests a significant efficacy of TCE in improving Pain and Disability, with no reported adverse events in the RCTs, indicating the preliminary safety of this treatment approach. However, caution must be exercised when interpreting these findings due to the limited number of studies for some outcome measures and the presence of high heterogeneity. In conclusion, the results of this study indicate a promising trend, suggesting that TCEs could be a feasible and relatively safe treatment option for LDH.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
WZ: Data curation, Methodology, Writing – original draft. GW: Writing – original draft. RX: Writing – original draft. JZ: Funding acquisition, Writing – review & editing. LZ: Funding acquisition, Writing – review & editing. CW: Funding acquisition, Writing – review & editing. HX: Funding acquisition, Writing – review & editing. CC: Funding acquisition, Writing – review & editing. YD: Visualization and Writing – review & editing.
Funding
The author (s) declare financial support was received for the research, authorship, and/or publication of this article. This research was funded by the National key research and development program (No. 2021YFC1712800), the National Natural Science Foundation of China (Nos. 81930118, 82274557, 81904232), the Fundamental Research Funds for the Central public welfare research institutes (No. ZZ13-YQ-038).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
TCEs, Traditional Chinese Exercises; LDH; Lumbar Disc Herniation; CNKI; China National Knowledge Infrastructure; Wan Fang; Wan Fang data; VIP; China Science and Technology Journal Database; CBM; Chinese Biomedical Literature Database; RCTs; randomized controlled trial; TSA; trial sequence analysis; BDJ; Baduanjin; YJJ; Yijinjing; TC; Taichi; WQX; wuqinxi; PRISMA; Preferred Reporting Items for Systematic Reviews and Meta-Analyses; VAS; visual analog scale; JOA; Japanese orthopedic association Scores; ODI; oswestry disability index; RR; response rate; SF-36; 36-Item Short Form Survey; MRMQ; Modified Roland-Morris Disability Questionnaire.
References
1. Cunha, C, Silva, AJ, Pereira, P, Vaz, R, Goncalves, RM, and Barbosa, MA. The inflammatory response in the regression of lumbar disc herniation. Arthritis Res Ther. (2018) 20:251. doi: 10.1186/s13075-018-1743-4
2. Ropper, AH, and Zafonte, RD. Sciatica. N Engl J Med. (2015) 372:1240–8. doi: 10.1056/NEJMra1410151
3. Xu, J, Ding, X, Wu, J, Zhou, X, Jin, K, Yan, M, et al. A randomized controlled study for the treatment of middle-aged and old-aged lumbar disc herniation by Shis spine balance manipulation combined with bone and muscle guidance. Medicine (Baltimore). (2020) 99:e23812. doi: 10.1097/MD.0000000000023812
4. Han, Q, Meng, F, Chen, M, Lu, X, Zhao, D, Wu, D, et al. Comparison between PE-TLIF and MIS-TLIF in the treatment of middle-aged and elderly patients with single-level lumbar disc herniation. J Pain Res. (2022) 15:1271–82. doi: 10.2147/JPR.S371635
5. Mutubuki, EN, Luitjens, MA, Maas, ET, Huygen, F, Ostelo, R, van Tulder, MW, et al. Predictive factors of high societal costs among chronic low back pain patients. Eur J Pain. (2020) 24:325–37. doi: 10.1002/ejp.1488
6. Fang, EF, Scheibye-Knudsen, M, Jahn, HJ, Li, J, Ling, L, Guo, H, et al. A research agenda for aging in China in the 21st century. Ageing Res Rev. (2015) 24:197–205. doi: 10.1016/j.arr.2015.08.003
7. Ruan, W, Feng, F, Liu, Z, Xie, J, Cai, L, and Ping, A. Comparison of percutaneous endoscopic lumbar discectomy versus open lumbar microdiscectomy for lumbar disc herniation: a meta-analysis. Int J Surg. (2016) 31:86–92. doi: 10.1016/j.ijsu.2016.05.061
8. Schoenfeld, AJ, and Weiner, BK. Treatment of lumbar disc herniation: evidence-based practice. Int J Gen Med. (2010) 3:209–14. doi: 10.2147/ijgm.s12270
9. Yang, T, Guo, Y, Cheng, Y, and Zhang, Y. Effects of traditional Chinese fitness exercises on negative emotions and sleep disorders in college students: a systematic review and Meta-analysis. Front Psychol. (2022) 13:908041. doi: 10.3389/fpsyg.2022.908041
10. Kong, L, Ren, J, Fang, S, He, T, Zhou, X, and Fang, M. Traditional Chinese exercises on pain and disability in middle-aged and elderly patients with neck pain: a systematic review and Meta-analysis of randomized controlled trials. Front Aging Neurosci. (2022) 14:912945. doi: 10.3389/fnagi.2022.912945
11. Xie, YH, Liao, MX, Wang, MY, Fernando, WCHA, Gu, YM, Wang, XQ, et al. Traditional Chinese mind and body exercises for neck pain: a Meta-analysis of randomized controlled trials. Pain Res Manag. (2021) 2021:5426595. doi: 10.1155/2021/5426595
12. Qin, Y, Xia, W, Huang, W, Zhang, J, Zhao, Y, and Fang, M. The beneficial effect of traditional Chinese exercises on the Management of Obesity. Evid Based Complement Alternat Med. (2020) 2020:2321679. doi: 10.1155/2020/2321679
13. Zhang, B, Xu, H, Wang, J, Liu, B, and Sun, G. A narrative review of non-operative treatment, especially traditional Chinese medicine therapy, for lumbar intervertebral disc herniation. Biosci Trends. (2017) 11:406–17. doi: 10.5582/bst.2017.01199
14. Zhang, YP, Hu, RX, Han, M, Lai, BY, Liang, SB, Chen, BJ, et al. Evidence base of clinical studies on Qi gong: a bibliometric analysis. Complement Ther Med. (2020) 50:102392. doi: 10.1016/j.ctim.2020.102392
15. Deng, C, and Xia, W. Effect of tai chi Chuan on degeneration of lumbar vertebrae and lumbar discs in middle-aged and aged people: a cross-sectional study based on magnetic resonance images. J Int Med Res. (2018) 46:578–85. doi: 10.1177/0300060517734115
16. Lan, C, Chen, SY, Lai, JS, and Wong, AM. Tai chi chuan in medicine and health promotion. Evid Based Complement Alternat Med. (2013) 2013:502131. doi: 10.1155/2013/502131
17. Page, MJ, Moher, D, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. (2021) 372:n160. doi: 10.1136/bmj.n160
18. Xia, QY. Observation of the Therapeutic Effect of Acupuncture, Tui Na, and Tai Chi in Treating Lumbar Disc Herniation. Chinese Manipulation & Rehabilitation Medicine (2014) 2:86–87.
19. Ji, CY. Analysis of the application effect of Wuqinxi in nursing Conservative management of lumbar disc herniation. Healthful Friend (2020) 1:192.
20. Li, H, and Che, HY. Application effect of health education combined with Baduanjin training inpatients with lumbar disc herniation. China Medical Herald (2022) 19:169–72.
21. Li, Y, Wang, WY, Si, MR, Ji, Q, Cai, J, and Wang, GM. Application effect of yijinjing exercise in patients with lumbar disc herniationduring remission period. China Medical Herald. (2022) 19:124–8. doi: 10.20047/j.issn1673-7210.2022.25.28
22. Xu, H, Fang, SC, JIn, C, Zhang, WZ, Cao, JH, and Lu, YC. Application of Baduanjin qigong in the treatment of low back and leg pain caused by lumbar disc herniation. Hunan Journal of Traditional Chinese Medicine (2015) 31:65–7. doi: 10.16808/j.cnki.issn1003-7705.2015.08.032
23. Yang, LG, and Zhang, XJ. Clinical effect analysis of massage combined with Baduanjin qigong training to improve lumbar disc herniation in rehabilitation period. Diet Health (2018) 5:102–3. doi: 10.3969/j.issn.2095-8439.2018.28.128
24. Yubing Li, HQ, Cai, Y, Liang, H, Peng, D, and Tian, T. Clinical observation of eight-section brocade exercise combined with disc decoction on the treatment of lumbar intervertebral disc herniation with liver and kidney Defciency. Chinese J Trad Med Traumatol Orthopedics. (2022) 30:45–9.
25. Hairong, L. Clinical observation on massage combined with Baduanjin qigong training to improve lumbar intervertebral disc herniation in rehabilitation period. Chinese Manipulation and Rehabilitation Medicine (2018) 39–41. doi: 10.19787/j.issn.1008-1879.2018.07.016
26. Binghua, S. Clinical observation on the effect of electroacupuncture combined with Yijinjing exercise on lumbar intervertebral disc herniation. Chengdu Sport University (2015). p. 48.
27. Tao, J. Clinical research on massage manipulation combined with yijinjing training for the treatment oflumbar intervertebral disc herniation (liver-kidney deficiency type). Heilongjiang University of Chinese Medicine (2021). p. 48. doi: 10.27127/d.cnki.ghlzu.2021.000478
28. Huijuan, S. Clinical study on the effect of lumbar four-dimensional traction combinec with Yijinjing functional exercise on patients with lumbar disc herniation. Chinese and Foreign Medical Research (2022) 5:168–172. doi: 10.14033/j.cnki.cfmr.2022.18.044
29. Shang, Q. Clinical study on the effect of practicing Baduanjin qigong on the prognosis of patients with lumbar disc herniation. China & Foreign Med Treatment. (2014) 33:151–2. doi: 10.16662/j.cnki.1674-0742.2014.29.003
30. Xingxing Xu, LH, Ma, L, and Zhang, J. Effect of BADUANJIN exercises combined with TUINA on low back painand life quality of patients with non-acute-phase lumbar disc herniation. J Trad Chinese Orthopedics Traumatol. (2018) 30:18–22.
31. Yuan Guo, YL. Effect of continuous nursing based on Baduanjin qigong exercise on the quality of life of patients with lumbar disc herniation. Hunan. J Tradit Chin Med. (2021) 37:86–8. doi: 10.16808/j.cnki.issn1003-7705.2021.02.036
32. Zhou, X, Kong, L, Ren, J, Song, P, Wu, Z, He, T, et al. Effect of traditional Chinese exercise combined with massage on pain and disability in patients with lumbar disc herniation: a multi-center, randomized, controlled, assessor-blinded clinical trial. Front Neurol. (2022) 13. doi: 10.3389/fneur.2022.952346
33. Xiangbi, C. The effect on low back pain caused by lumbar discherniation with health oigong·yijinjing (muscle tendon changing classic qigong) exercise treatment. Nanjing University Of Chinese Medicine (2009). p. 86.
34. Hao Xu, XC, Jin, C, Zhang, W, and Huang, X. Effects of eight dan jin on serum IL-1β, IL-6 and TNF-α in patients with lumbar disc herniation. Hunan. J Tradit Chin Med. (2015) 31:16–17. doi: 10.16808/j.cnki.issn1003-7705.2015.11.006
35. Jiajun Kang, YJ, and Zhengzhou, Y. Observation of Baduanjin qigong on conservative management and prevention of recurrence of lumbar intervertebral disc herniation. Chinese Manipulation Rehab Med. (2018) 9:33–5. doi: 10.19787/j.issn.1008-1879.2018.05.015
36. Zonghao, Z. Observation on the clinical efficacy of the Yi Jin Jing technique in patients with lumbar disc herniation. Liaoning Journal of Traditional Chinese Medicine (2009) 36:451–2. doi: 10.13192/j.ljtcm.2009.03.134.zhangzh.028
37. Yi, Z, Li, N, and Jin, HZ. Observation on the effects of 2-Week YiJinjing gong practice and pelvic traction in the treatment of acute low back pain in patients with lumbar intervertebral disc herniation. Chinese Journal of Sports Medicine. (2010) 288–90. doi: 10.16038/j.1000-6710.2010.03.012
38. Lei Liang, YZ, Li, H, and Li, J. Study on effect of ridge eight section brocade in prevention and treatment ofumbar disc Herniaion. Sichuan sports. Science. (2014) 33:31–4.
39. Qing, M. Study on the curative effective of Taiji boxing in treatment of lumbar disc herniation. Modern Preven Med. (2012) 39:4170–2.
40. Kaito, T, and Yamato, Y. The essence of clinical practice guidelines for lumbar disc herniation, 2021: 3. Diagnosis. Spine Surg Relat Res. (2022) 6:325–8. doi: 10.22603/ssrr.2022-0044
41. Kreiner, DS, Hwang, SW, Easa, JE, Resnick, DK, Baisden, JL, Bess, S, et al. S. North American spine, an evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J. (2014) 14:180–91. doi: 10.1016/j.spinee.2013.08.003
42. Kim, JH, van Rijn, RM, van Tulder, MW, Koes, BW, de Boer, MR, Ginai, AZ, et al. Diagnostic accuracy of diagnostic imaging for lumbar disc herniation in adults with low back pain or sciatica is unknown; a systematic review. Chiropr Man Therap. (2018) 26:37. doi: 10.1186/s12998-018-0207-x
43. Cheng, ZX, Zheng, YJ, Feng, ZY, Fang, HW, Zhang, JY, and Wang, XR. Chinese Association for the Study of pain: expert consensus on diagnosis and treatment for lumbar disc herniation. World J Clin Cases. (2021) 9:2058–67. doi: 10.12998/wjcc.v9.i9.2058
44. Sakai, D. The essence of clinical practice guidelines for lumbar disc herniation, 2021: 4. Treatment. Spine Surg Relat Res. (2022) 6:329–32. doi: 10.22603/ssrr.2022-0045
45. Melman, A, Lord, HJ, Coombs, D, Zadro, J, Maher, CG, and Machado, GC. Global prevalence of hospital admissions for low back pain: a systematic review with meta-analysis. BMJ Open. (2023) 13:e069517. doi: 10.1136/bmjopen-2022-069517
46. Trager, RJ, Cupler, ZA, Srinivasan, R, Casselberry, RM, Perez, JA, and Dusek, JA. Association between chiropractic spinal manipulation and gabapentin prescription in adults with radicular low back pain: retrospective cohort study using US data. BMJ Open. (2023) 13:e073258. doi: 10.1136/bmjopen-2023-073258
47. Chou, R, Baisden, J, Carragee, EJ, Resnick, DK, Shaffer, WO, and Loeser, JD. Surgery for low back pain: a review of the evidence for an American pain society clinical practice guideline. Spine. (2009) 34:1094–109. doi: 10.1097/BRS.0b013e3181a105fc
48. Koivunen, K, Pernaa, KI, and Saltychev, M. Back pain and radicular pain after lumbar microdiscectomy. BMC Surg. (2023) 23:210. doi: 10.1186/s12893-023-02114-3
49. Zhang, SK, Yang, Y, Gu, ML, Mao, SJ, and Zhou, WS. Effects of low Back pain exercises on pain symptoms and activities of daily living: a systematic review and Meta-analysis. Percept Mot Skills. (2022) 129:63–89. doi: 10.1177/00315125211059407
50. Baraldo, L, Battaglino, A, Piscitelli, D, Pellicciari, L, Sánchez-Romero, EA, Cotella, D, et al. The correlation between low back pain and strength training in elite athletes: a literature review. Retos. (2023) 48:727–31. doi: 10.47197/retos.v48.97449
51. Knezevic, NN, Candido, KD, Vlaeyen, JWS, Van Zundert, J, and Cohen, SP. Low back pain. Lancet. (2021) 398:78–92. doi: 10.1016/S0140-6736(21)00733-9
52. Ballestra, E, Battaglino, A, Cotella, D, Rossettini, G, Sanchez-Romero, EA, and Villafane, JH. Do patients’ expectations influence conservative treatment in chronic low Back pain? A narrative review. Retos. (2022) 46:395–403. doi: 10.47197/retos.v46.93950
53. Qi, F, Soh, KG, Nasiruddin, NJM, Leong, OS, He, S, and Liu, H. Effect of Taichi Chuan on health-related physical fitness in adults: a systematic review with meta-analysis. Complement Ther Med. (2023) 77:102971. doi: 10.1016/j.ctim.2023.102971
54. Wan, X, Shen, J, and He, G. Effects of traditional Chinese exercises on frailty, quality of life, and physical function on frail and pre-frail older people: a systematic review and Meta-analysis. J Frailty Aging. (2022) 11:407–15. doi: 10.14283/jfa.2022.52
55. Livshits, G, Ermakov, S, Popham, M, Macgregor, AJ, Sambrook, PN, Spector, TD, et al. Evidence that bone mineral density plays a role in degenerative disc disease: the UK twin spine study. Ann Rheum Dis. (2010) 69:2102–6. doi: 10.1136/ard.2010.131441
56. Salo, S, Leinonen, V, Rikkonen, T, Vainio, P, Marttila, J, Honkanen, R, et al. Association between bone mineral density and lumbar disc degeneration. Maturitas. (2014) 79:449–55. doi: 10.1016/j.maturitas.2014.09.003
57. Turner, CH, and Robling, AG. Designing exercise regimens to increase bone strength. Exerc Sport Sci Rev. (2003) 31:45–50. doi: 10.1097/00003677-200301000-00009
58. Sun, C, Qi, B, Huang, X, Chen, M, Jin, Z, Zhang, Y, et al. Baduanjin exercise: a potential promising therapy toward osteoporosis. Front Med (Lausanne). (2022) 9:935961. doi: 10.3389/fmed.2022.935961
59. Sun, W, Zhang, XA, and Wang, Z. The role and regulation mechanism of Chinese traditional fitness exercises on the bone and cartilage tissue in patients with osteoporosis: a narrative review. Front Physiol. (2023) 14:1071005. doi: 10.3389/fphys.2023.1071005
60. Mehta, NM, Malootian, A, and Gilligan, JP. Calcitonin for osteoporosis and bone pain. Curr Pharm Des. (2003) 9:2659–76. doi: 10.2174/1381612033453622
61. Yuen, M, Ouyang, HX, Miller, T, and Pang, MYC. Baduanjin qigong improves balance, leg strength, and mobility in individuals with chronic stroke: a randomized controlled study. Neurorehabil Neural Repair. (2021) 35:444–56. doi: 10.1177/15459683211005020
62. Wei, M, Meng, D, Guo, H, He, S, Tian, Z, Wang, Z, et al. Hybrid exercise program for sarcopenia in older adults: the effectiveness of explainable artificial intelligence-based clinical assistance in assessing skeletal muscle area. Int J Environ Res Public Health. (2022) 19:9952. doi: 10.3390/ijerph19169952
63. Segura-Jimenez, V, Romero-Zurita, A, Carbonell-Baeza, A, Aparicio, VA, Ruiz, JR, and Delgado-Fernandez, M. Effectiveness of tai-chi for decreasing acute pain in fibromyalgia patients. Int J Sports Med. (2014) 35:418–23. doi: 10.1055/s-0033-1353214
64. Zhong, D, Xiao, Q, Xiao, X, Li, Y, Ye, J, Xia, L, et al. Tai chi for improving balance and reducing falls: an overview of 14 systematic reviews. Ann Phys Rehabil Med. (2020) 63:505–17. doi: 10.1016/j.rehab.2019.12.008
65. Chang, XQ, Chen, XP, Shen, YX, Wang, K, Huang, SJ, Qi, Y, et al. The deer play in Wuqinxi and four-point hand-knee kneeling positions for training core muscle function and spinal mobility. Front Bioeng Biotechnol. (2022) 10:965295. doi: 10.3389/fbioe.2022.965295
66. Huston, P, and McFarlane, B. Health benefits of tai chi: what is the evidence? Can Fam Physician. (2016) 62:881–90.
67. Li, H, Ge, D, Liu, S, Zhang, W, Wang, J, Si, J, et al. Baduanjin exercise for low back pain: a systematic review and meta-analysis. Complement Ther Med. (2019) 43:109–16. doi: 10.1016/j.ctim.2019.01.021
68. Zou, L, Yeung, A, Quan, X, Hui, SS, Hu, X, Chan, JSM, et al. Mindfulness-based Baduanjin exercise for depression and anxiety in people with physical or mental illnesses: a systematic review and Meta-analysis. Int J Environ Res Public Health. (2018) 15:321. doi: 10.3390/ijerph15020321
69. Wen, J, Lin, Y, Cai, Q, Chen, Y, Chen, Y, Ren, S, et al. Baduanjin exercise for type 2 diabetes mellitus: a systematic review and meta-analysis of randomized controlled trials. Evid Based Complement Alternat Med. (2017) 2017:8378219. doi: 10.1155/2017/8378219
70. Li, R, Chen, H, Feng, J, Xiao, Y, Zhang, H, Lam, CW, et al. Effectiveness of traditional Chinese exercise for symptoms of knee osteoarthritis: a systematic review and meta-analysis of randomized controlled trials. Int J Environ Res Public Health. (2020) 17:7873. doi: 10.3390/ijerph17217873
71. Chen, D, Zhao, G, Fu, J, Sun, S, Huang, X, Su, L, et al. Effects of traditional Chinese exercise on oxidative stress in middle-aged and older adults: a network meta-analysis. Int J Environ Res Public Health. (2022) 19:8276. doi: 10.3390/ijerph19148276
72. Zou, L, Yeung, A, Quan, X, Boyden, SD, and Wang, H. A systematic review and meta-analysis of mindfulness-based (Baduanjin) exercise for alleviating musculoskeletal pain and improving sleep quality in people with chronic diseases. Int J Environ Res Public Health. (2018) 15:206. doi: 10.3390/ijerph15020206
Keywords: lumbar disc herniation, Baduanjin, Yijinjing, Taichi, Wuqinxi, traditional Chinese exercises
Citation: Zhang W, Wang G, Xie R, Zhan J, Zhu L, Wan C, Xie H, Cai C and Du Y (2023) Traditional Chinese exercises on pain and disability in middle-aged and elderly patients with lumbar disc herniation: a systematic review and meta-analysis of randomized controlled trials. Front. Med. 10:1265040. doi: 10.3389/fmed.2023.1265040
Edited by:
Lei Kuang, Central South University, ChinaReviewed by:
Eleuterio A. Sánchez Romero, European University of Madrid, SpainEron Grant Manusov, The University of Texas Rio Grande Valley, United States
Copyright © 2023 Zhang, Wang, Xie, Zhan, Zhu, Wan, Xie, Cai and Du. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiawen Zhan, emhhbmppYXdlbjEyQDEyNi5jb20=; Liguo Zhu, emhsZzk1QGFsaXl1bi5jb20=; Chunyou Wan, d2FuY2h1bnlvdXhzQDE2My5jb20=
†These authors have contributed equally to this work and share first authorship
 Weiye Zhang
Weiye Zhang Gewen Wang1†
Gewen Wang1† Rong Xie
Rong Xie Liguo Zhu
Liguo Zhu Hualong Xie
Hualong Xie