- 1Department of Infectious Diseases, Tianjin Second People’s Hospital, Tianjin, China
- 2Department of Surgery, Tianjin Second People's Hospital, Tianjin, China
- 3Out-patient Department, Tianjin Second People's Hospital, Tianjin, China
- 4Affiliated Infectious Disease Hospital of Nantong University, Nantong, Jiangsu, China
- 5Tianjin Association of STD/AIDS Prevention and Control, Tianjin, China
Background: Antiretroviral therapy (ART) prolongs lifespan and decreases mortality of HIV infected patients. However, many patients do not achieve optimal immune reconstitution. The influence of non-optimal immune recovery on non-AIDS related diseases is not well defined in aged HIV-infected patients receiving ART.
Methods: A retrospective study was conducted at Tianjin Second People’s Hospital, China to evaluate the association of an inadequate immunological response and non-AIDS diseases in HIV infected patients ≥60 years of age and virally suppressed for at least 2 years by ART.
Results: The study included patients (n = 666) who initiated ART between August 2009 and December 2020. The prevalence of patients with an inadequate immunological response was 29.6%. The percentage of non-AIDS diseases such as hypertension, cardiovascular disease (CVD), diabetes, tumor, and chronic kidney disease (CKD) was 32.9, 9.9, 31, 4.1, and 13%, respectively. In addition to baseline CD4+ T cell counts, CVD and tumor were associated with poor immune reconstitution in aged Chinese HIV-1 infected patients. The adjusted odds ratios (95% confidence interval) were AOR 2.45 (95% CI: 1.22–4.93) and 3.06 (95% CI: 1.09–8.56, p = 0.03). Inadequate immunological response was associated with greater mortality (AOR: 2.83, 95% CI: 1.42–5.67, p = 0.003) in this cohort.
Conclusion: These results tend to demonstrate appropriate drug selection at ART initiation and prevention of non-AIDS complications during ART decreased mortality of and an inadequate immunological response in aged HIV infected patients.
Introduction
Antiretroviral therapy (ART) effectively controls HIV replication, increasing CD4+ T counts, and decreasing mortality. However, 9–40% of patients living with HIV (PLWH) fail to achieve CD4+ T cell count normalization and are referred to as “inadequate immunological responders,” (INRs) (1–3). Although the definition of INR was different in previous studies, the total CD4 T cell counts threshold of <200 or < 350 cells/μl at 2 years after ART initiation and persist HIV viral load undetectable or less than 20 copies/ml was more popular. Previous studies found that INRs are at greater risk of morbidity, mortality (4, 5), and non-AIDS related events.
ART has improved patient lifespan and changed HIV from a life-threatening illness to a chronic one. As a result, the number of aged HIV infected patients has increased. Aged HIV infected patients receiving ART have a reduced immune response (6, 7). At same time, aging with HIV infection has significant challenges, including inflammation due to chronic immune activation, cardiovascular disease, bone loss, and non-AIDS related cancers (8). According the literature, INR was associated with increased risk of non-AIDS defining events such as cardiovascular disease and even death.
The persons aged 65 years and over was defined as senior citizen (9). However, UNAIDS records PLWH aged 50 or over need provide appropriate prevention and demand age-appropriate health services (10). Previous study indicated that aged 60 years and over was associate with poor immune recovery and higher mortality (11). But no previous study has investigated the prevalence and prognostic of INR and non-AIDS related diseases in this special population. This study identifies INR risk factors and the burden of non-AIDS diseases in aged PLWH. The relationship of INRs to non-AIDS diseases is also described.
Methods
Study population
This study was conducted at Tianjin Second People’s Hospital, China, which has been a hospital designated for the treatment of HIV since July 2004. This study’s methodology conformed to the Declaration of Helsinki and was approved by the ethics committee of Tianjin Second People’s Hospital. ≥ 60 years HIV positive patients receiving ART for more than 2 years, with suppressed virology, were included in this study. After authorization by the ethics committee, available patient data were obtained from the electronic medical records of the hospital.
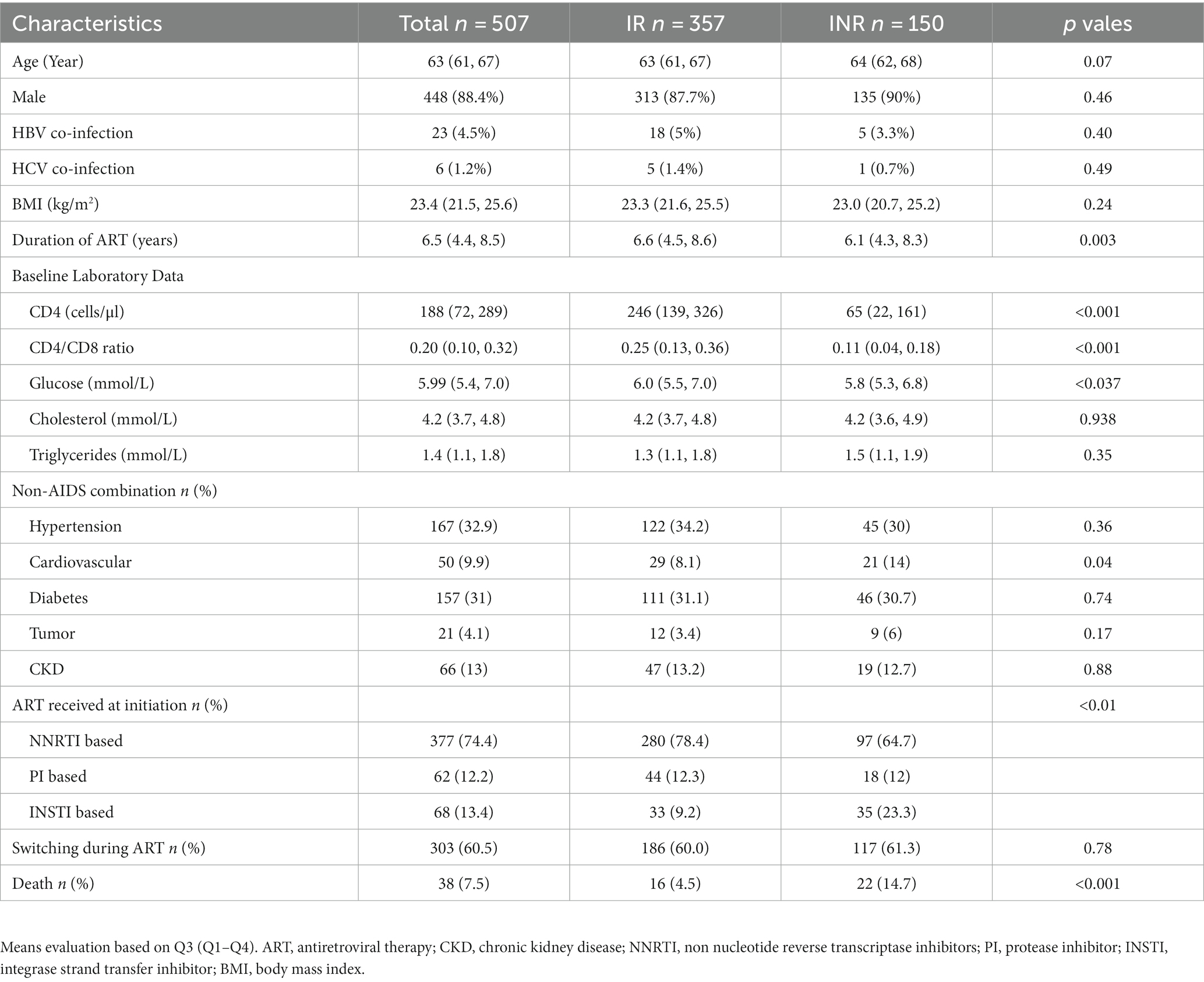
Information was collected for approximately 666 ART patients ≥60 years of age, with virologic success through January 2023. Exclusion criteria included; incomplete information (29), loss to follow-up (30), ART time less than 2 years (92), and virologic failure (8). Data for 507 PLWH comprised the final study group. Of the 507 individuals, 150 patients had CD4 + T cell counts less than 350 cells/ml. A flow chart of patient characteristics and selection is presented in Figure 1.
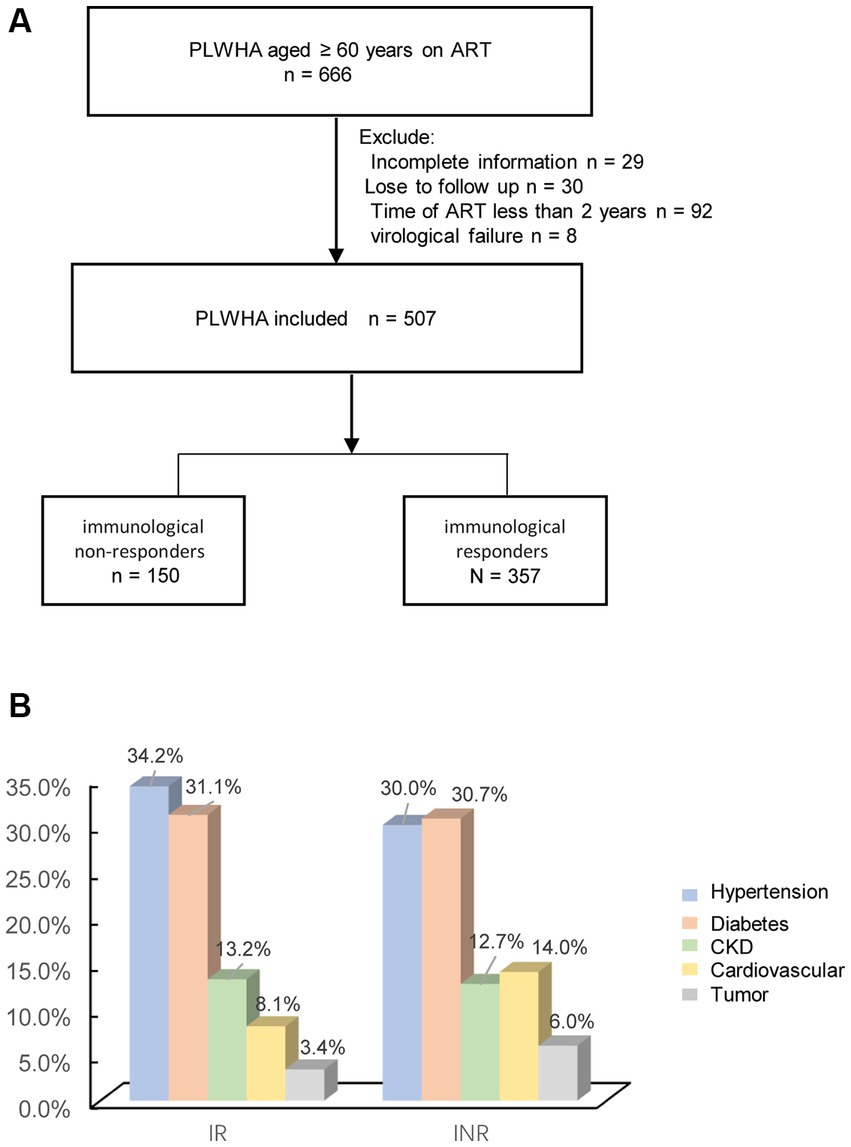
Figure 1. (A) Flow chart showing patient characteristics and selection; (B) the percentage of non-AIDS diseases.
Definitions
CVD (myocardial infarction, stroke, coronary artery intervention, or death from chronic atherosclerotic cardiovascular disease); chronic renal disease, CKD (end-stage renal disease or eGFR <60 mL/min/ cm2); tumor (all cancers); diabetes (history of diabetes); hypertension (history of hypertension), INRs (CD4+T cell count below 350 cells/μl at 2 years after ART initiation, with undetectable plasma HIV RNA). Immunological responders (IRs, CD4+T cell counts above 350/μl at 2 years after ART initiation with with undetectable plasma HIV RNA). HIV virologic failure was defined as two consecutive measurements with HIV RNA > 200 copies/ml after 6 months of ART.
Data collection
Retrospective data, including demographic and clinical/laboratory characteristics, were collected from medical records. Variables included; age, gender, HIV transmission route, co-infection with HBV, co-infection with HCV, diabetes, hypertension, CVD, tumor, and CKD. CD4+ T cell counts were stratified at baseline as >200, 50–199, and < 50 cells/μl.
Statistical analysis
Statistical analysis was performed using SPSS 25.0 software (SPSS, Chicago, IL, United States) and GraphPad 8 (GraphPad Software, La Jolla, CA, United States). Because of skewed statistical distributions, numerical data are presented as medians with interquartile ranges (IQR); categorical variables are presented as percentages. Differences between two groups were analyzed using the Mann–Whitney U test (nonparametric). Logistic regression and Cox proportional regression models were used to evaluate risk factors associated with poor immune reconstitution after 2 years of ART, and mortality. Kaplan–Meier curves were computed for this cohort. Log-rank testing was carried out to evaluate differences in cumulative death in HIV-infected patients, with or without INR. Demographic variables (gender, age) and clinical/laboratory characteristics (CD4+ T cell counts at baseline, CVD, hypertension, diabetes, co-infection with HBV, and co-infection with HCV) were investigated as risk factors. A p value <0.05 was considered statistically significant.
Results
Demographic and clinical characteristics of HIV infected patients
A total of 507 aged PLWH were included in the analysis. Of these 150 (29.6%) had poor CD4 + T cell recovery (INR). The median age was 63 (IQR 61, 67), and the male to female ratio was 8.45:1. Twenty-three (4.5%) were co-infected with HBV, six (1.2%) were co-infected with HCV. The median BMI was 23.4 (IQR21.5, 25.6), the median CD4 T+ cell count at baseline was 188 (IQR72, 289) cells/μl. The percentages of non-AIDS associated diseases are shown in Figure 1B. The percentages of hypertension, CVD, diabetes, tumor, and CKD were; 32.9% (167), 9.9% (50), 31% (157), 4.1% (21), and 13% (66), respectively. In this cohort, 38/507 (7.6%) of the patients died with 3,547 person-years of follow-up. Patients with INR had lower CD4+T cell counts (65 vs. 246, p < 0.001), greater percentage of CVD (13.6% vs. 8.1%, p = 0.046), and a greater death ratio (13.1% vs. 4.2%). All descriptive statistics for study variables are presented in Table 1. The laboratory data after 2 years ART was shown in Supplementary Table S1.
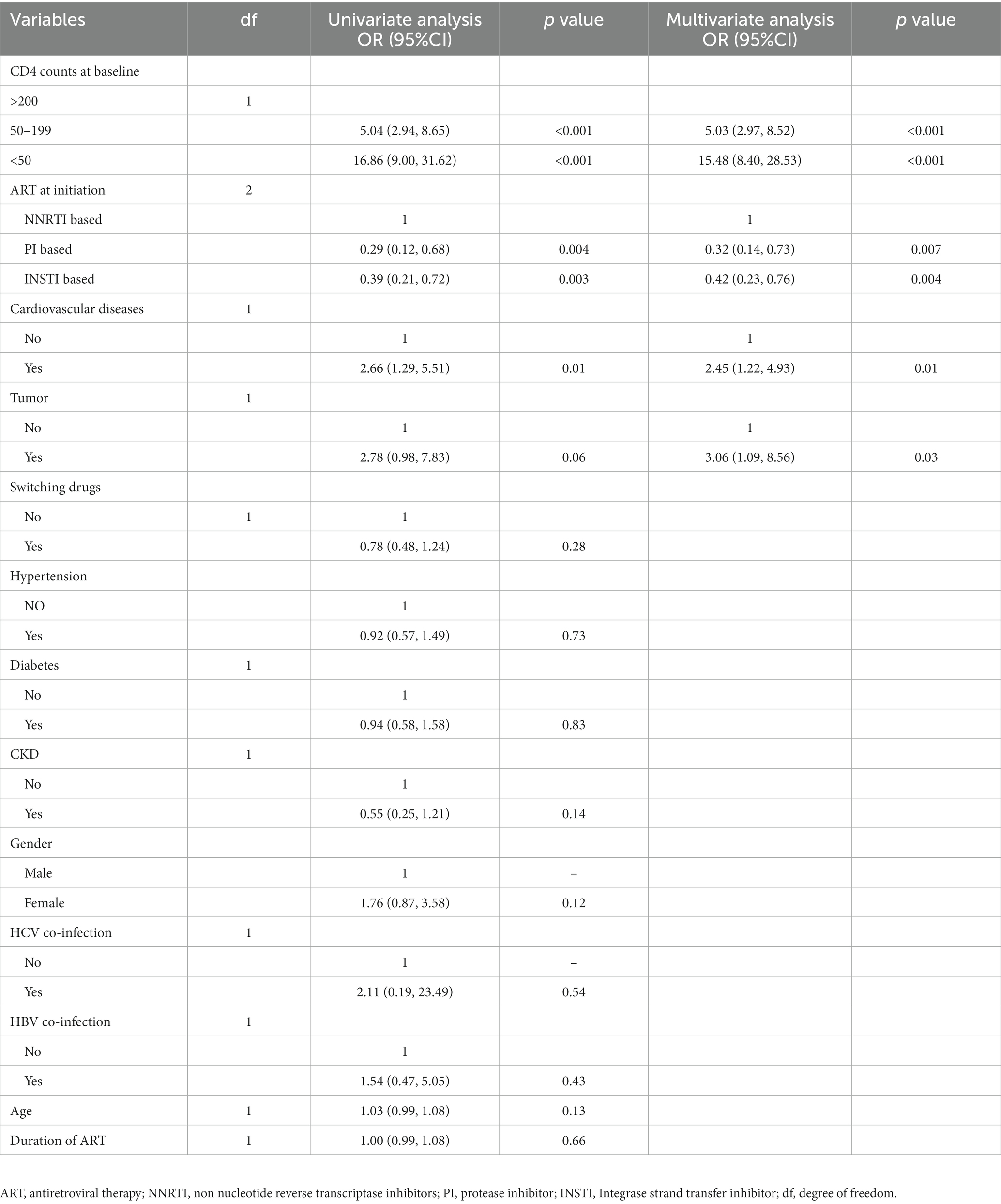
Cardiovascular diseases associated with higher risk of poor CD4+ T cell recovery
The multivariate logistic regression model found the following associations with poor immune reconstitution in elderly Chinese HIV-1 infected patients. These were; CVD (adjusted odds ratio (AOR): 2.45, 95% confidence interval (CI): 1.22–4.93, p = 0.01), tumor (AOR: 3.06, 95% confidence interval: 1.09–8.58, p = 0.03), baseline CD4+ T cell counts 50–199 cells/μl (AOR: 5.03, 95% confidence interval: 2.97–8.52, p < 0.001), and CD4+ T cells counts <50 cells/μl (AOR15.48, 95% CI:8.40–28.53, p < 0.001). Associations with decreased probability of poor CD4+ T cell recovery were protease inhibitor (PI) based (AOR: 0.32, 95% CI: 0.14–0.73, p = 0.01) and integrase strand transfer inhibitor (INSTI) based (AOR: 0.42, 95% CI: 0.23–0.76, p = 0.01), Table 2.
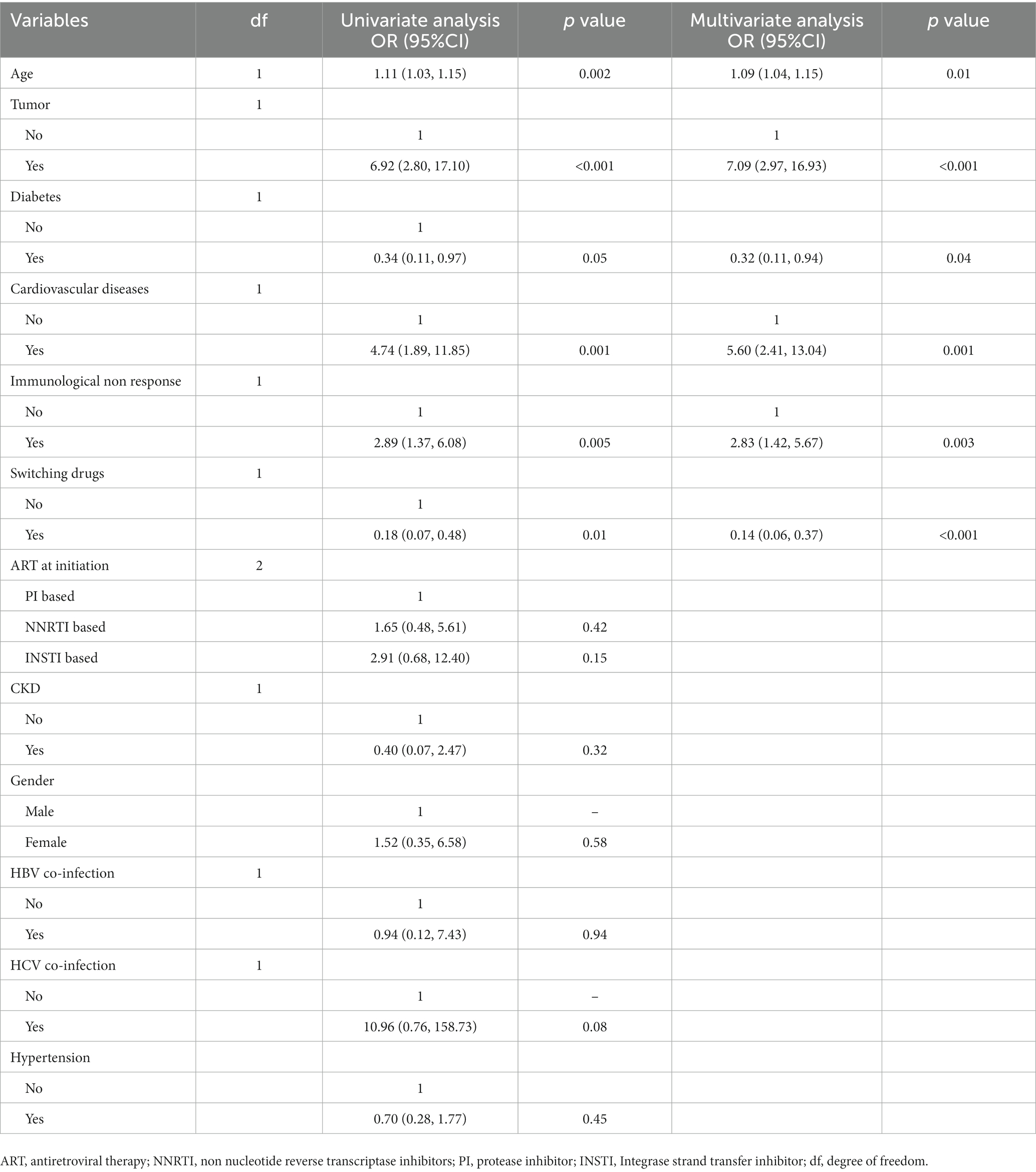
Outcomes for virologic suppressed PLWH after 2 years of ART
Thirty-eight (7.6%) patients died during 3,547 person-years of follow-up. The main causes of death were; tumor (12) (endometrial carcinomas n = 1, anal cancer n = 2, lung cancer n = 2, stomach cancer n = 2, pancreatic cancer n = 1, leukemia n = 1, cholangiocarcinoma n = 1, and unidentified cancer n = 2), CVD (n = 11), opportunistic infections (OIs) (n = 7) (Mycobacterium tuberculosis n = 1, pneumocystis pneumonia n = 3, co-infected with bacteria n = 2, co-infected with other viruses, Covid-19, n = 2). Among these, OIs were only found in the INR group. Log-rank testing showed a significant difference between patients with and without CVD (p < 0.001), INR (p < 0.001), and tumor (p < 0.001).
The multivariate Cox logistic regression model found the following associated with increased mortality in elderly Chinese HIV-1 infected patients after 2 years of ART, Table 2. These were; HIV infection with CVD (adjusted odds ratio (AOR): 5.60, 95% CI: 2.41–13.04, p = 0.001), tumor (AOR: 7.09, 95% CI: 2.97–16.93, p < 0.01), INR (AOR: 2.83, 95% CI: 1.42–5.67, p = 0.003), and older age (AOR: 1.09, 95% CI: 1.04–1.15, p = 0.01). Change in ART drugs during ART (AOR: 0.14, 95%CI 0.06–0.37) was associated with decreased mortality (Table 3).
Discussion
In this study, 150 (29.6%) aged PLWH were INR, which is consistent with a previous study (12). Aged INRs with successful ART had a higher mortality and exhibited greater CVD and lower baseline CD4+ T cell counts. The increased mortality of patients with INR was associated with higher OIs, which demonstrates the importance of OIs in aged INR patients.
Although ART has reduced worldwide HIV related mortality and morbidity, INR patients with virologic suppression still have a greater probability of poor outcomes and no obvious CD4+ T cell recovery. Baseline CD4+ T cell counts, advanced age, co-infection with HCV, thymic dysfunction, immune activation, and genetic factors contribute to poor immune recovery (13, 14). By statistical analysis, baseline CD4+ T cell counts was associated with INR. We also found that non-AIDS diseases and initial ART drug combinations were associated with INR. These results demonstrate the importance of ART third drug selection as well as the prevention of non-AIDS diseases in PLWH, as the means by which to decrease the probability of INR.
Persistent inflammation and immune activation exacerbate tissue damage in PLWH, increasing the risk for non-AIDS-related co-morbidities that are commonly observed in PLWH and advanced age (15). Further, long term ART and advanced age are associated with CVDs such as heart diseases and stroke. In this study’s cohort, the prevalence of CVD was lower than in HIV/AIDS patients more than 60 years since the IPEC/FIOCRUZ cohort (15) (9.9% vs. 27.5%), but comparable with the rate of a Spanish HIV/AIDS cohort (13%) (16). CVD self-report without health care personnel examination may explain the lower rate found in this study.
Hypertension was found in 33.1% of all patients in this study, which is greater (33.1% vs. 30.3%) than rates reported for the IPEC/FIOCRUZ cohort. In this study, there was a greater prevalence of diabetes among elderly patients (31% vs. 4.6%) compared to the IPEC/FIOCRUZ cohort, which was also greater than rates observed for the Chinese general population (≥ 60 years, 31% vs. 26.7) (17). Genetic differences and dietary habits may explain these results.
In a previous study the main risks for death in patients receiving ART have changed from OIS to non-AIDS-defining malignancies and CVD (18, 19). For this cohort of patients, seven deaths (18%) were due to OIs, all of which were with in INR group. These findings suggest that aged HIV infected patients with poor immune recovery require careful follow-up consideration of CD4+ T cells counts, as a means by which to minimize mortality (Figure 2).
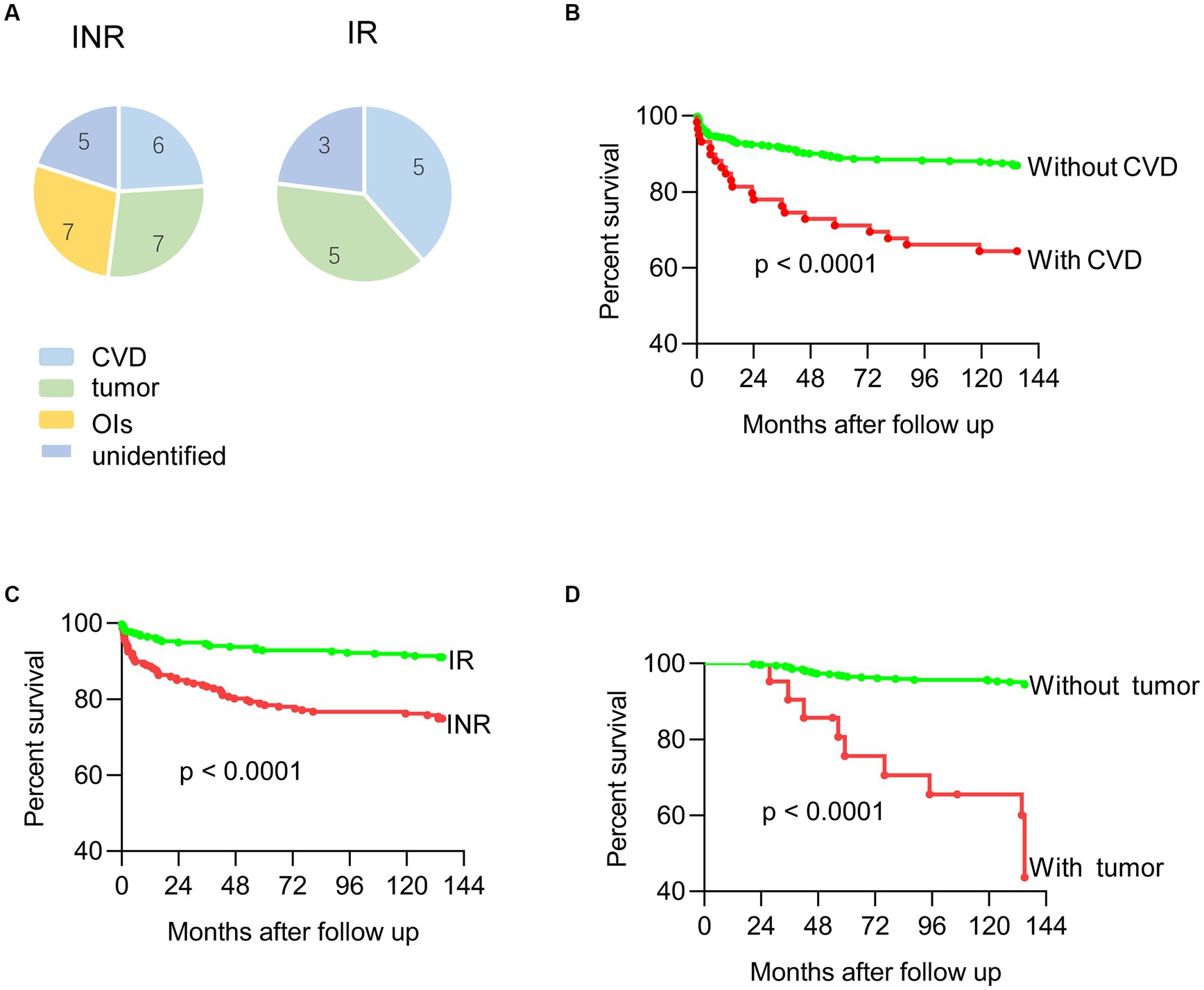
Figure 2. (A) Death of immune non-responders and immune responders; (B) mortality curves of HIV infected patients with or without CVD; (C) mortality curves of HIV infected patients with or without tumor; (D) mortality curves of HIV infected patients with or without immune recovery.
Previous studies found that death risk for patients receiving continuous ART with CD4+ T cell counts >500 cells/μl was similar to patients with full immune recovery. INRs have twice the number fatal and non-fatal non-AIDS diseases compared to IRs (20, 21). In this study, a greater mortality rate was found for INR patients, indicating that close clinical attention is required for INR patients, particularly those with OIs and non-AIDS diseases.
Treatment option at ART initiation for INR patients are still debated. INSTI-based was confirmed a faster viral load suppression and immune recovery than PI-based regimens after ART in early HIV infection (22). Another multicenter study observed INSTI-based initiation gained faster immune restoration but lose the priority in long time follow up (23). Intensified INSTI-based three drugs versus four drugs regimen include boost PI, showed comparable responses in immunological recovery after ART initiation (24). In this study, we also recommend the use of INSTI-based and PI-based, but not NNRTI- ART for treatment initiation.
There are limitations to this study. First, the inherent bias of a retrospectively designed study is a limitation. Second, the initiation and diagnosis of non-AIDS related diseases was not adequately recorded in the patients’ medical records. Third, data were only derived from the Tianjin HIV tertiary health center. Future studies should examine the effects of non-AIDS diseases on immune recovery of patients similar to those investigated by this study.
Conclusion
In conclusion, this study identifies the risk factors for poor immune recovery of aged HIV infected patients. Baseline CD4+ T cell counts, CVD, tumor, and initial ART drug are strongly associated with poor immune recovery. Greater mortality and a greater risk for INR in an aged population argues for close monitoring of ART treatment effects and non-AIDS complication during ART. Switching ART drugs during treatment was associated with lower mortality rates, therefore, the initial treatment selection might affect mortality rates. Immune reconstitution differences after ART drug initiation demonstrate drug selection to be important for aged patients. Further research is needed to determine whether alterations in ART drug selection would improve immune reconstitution and better clinical outcomes.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by Medical Ethics committee of Tianjin Second People’s Hospital Approval certificate of Ethical Review [2020]49. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
LF: Data curation, Formal analysis, Methodology, Writing – original draft. PL: Data curation, Validation, Formal analysis, Investigation, Writing – original draft. AY: Data curation, Investigation, Supervision, Writing – original draft. DL: Data curation, Methodology, Writing – original draft. ZW: Data curation, Writing – original draft. YW: Data curation, Writing – original draft. DZ: Data curation, Writing – original draft. MZ: Writing – original draft, Supervision, Validation. PM: Writing – original draft, Funding acquisition, Project administration.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was funded by the Tianjin Key Medical Discipline (Specialty) Construction Project (No. ZD02) and the Tianjin Science and Technology Cultivation Project (No. RC20019). The source of funds played no role in study design, data collection, analysis, the decision to publish, or preparation of the manuscript.
Acknowledgments
We acknowledge the work of HIV health care providers for their diagnosis, nursing, and treatment of HIV/AIDS patients at the Tianjin Second People’s Hospital. We also acknowledge the work of the members of the Tianjin Institute of Hepatology, Tianjin Second People’s Hospital for measurement of CD4+ T cell counts and HIV viral load. We thank International Science Editing (http://www.internationalscienceediting.com) for editing this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2023.1259871/full#supplementary-material
References
1. Yang, X, Su, B, Zhang, X, Liu, Y, Wu, H, and Zhang, T. Incomplete immune reconstitution in HIV/AIDS patients on antiretroviral therapy: challenges of immunological non-responders. J Leukoc Biol. (2020) 107:597–612. doi: 10.1002/JLB.4MR1019-189R
2. Rb-Silva, R, Goios, A, Kelly, C, Teixeira, P, João, C, Horta, A, et al. Definition of immunological nonresponse to antiretroviral therapy: a systematic review. J Acquir Immune Defic Syndr. (2019) 82:452–61. doi: 10.1097/QAI.0000000000002157
3. Nakanjako, D, Kiragga, AN, Musick, BS, Yiannoutsos, CT, Wools-Kaloustian, K, Diero, L, et al. Frequency and impact of suboptimal immune recovery on first-line antiretroviral therapy within the international epidemiologic databases to evaluate AIDS in East Africa. AIDS (London, England). (2016) 30:1913–22. doi: 10.1097/QAD.0000000000001085
4. Kelley, CF, Kitchen, CM, Hunt, PW, Rodriguez, B, Hecht, FM, Kitahata, M, et al. Incomplete peripheral CD4+ cell count restoration in HIV-infected patients receiving long-term antiretroviral treatment. Clin Infect Dis. (2009) 48:787–94. doi: 10.1086/597093
5. Baker, JV, Peng, G, Rapkin, J, Abrams, DI, Silverberg, MJ, MacArthur, RD, et al. CD4+ count and risk of non-AIDS diseases following initial treatment for HIV infection. AIDS (London, England). (2008) 22:841–8. doi: 10.1097/QAD.0b013e3282f7cb76
6. Ahn, MY, Jiamsakul, A, Khusuwan, S, Khol, V, Pham, TT, Chaiwarith, R, et al. The influence of age-associated comorbidities on responses to combination antiretroviral therapy in older people living with HIV. J Int AIDS Soc. (2019) 22:e25228. doi: 10.1002/jia2.25228
7. Han, N, Wright, ST, O'Connor, CC, Hoy, J, Ponnampalavanar, S, Grotowski, M, et al. HIV and aging: insights from the Asia Pacific HIV observational database (APHOD). HIV Med. (2015) 16:152–60. doi: 10.1111/hiv.12188
8. Zicari, S, Sessa, L, Cotugno, N, Ruggiero, A, Morrocchi, E, Concato, C, et al. Immune activation, inflammation, and non-AIDS co-morbidities in HIV-infected patients under long-term ART. Viruses. (2019) 11. doi: 10.3390/v11030200
10. UNAIDS. (2013). HIV and aging: special supplement to the UNAIDS report on the global AIDS epidemic 2013. Geneva: UNAIDS.
11. Sabin, CA, Smith, CJ, d'Arminio Monforte, A, Battegay, M, Gabiano, C, Galli, L, et al. Response to combination antiretroviral therapy: variation by age. AIDS (London, England). (2008) 22:1463–73. doi: 10.1097/QAD.0b013e3282f88d02
12. Ocheretyaner, ER, Yusuff, J, and Park, TE. Immunologic and virologic responses to antiretroviral therapy in treatment-naïve, HIV-infected elderly patients. Int J STD AIDS. (2019) 30:1304–10. doi: 10.1177/0956462419872857
13. Gunda, DW, Kilonzo, SB, Kamugisha, E, Rauya, EZ, and Mpondo, BC. Prevalence and risk factors of poor immune recovery among adult HIV patients attending care and treatment Centre in northwestern Tanzania following the use of highly active antiretroviral therapy: a retrospective study. BMC Res Notes. (2017) 10:197. doi: 10.1186/s13104-017-2521-0
14. Carvalho-Silva, WHV, Andrade-Santos, JL, Souto, FO, Coelho, AVC, Crovella, S, and Guimarães, RL. Immunological recovery failure in cART-treated HIV-positive patients is associated with reduced thymic output and RTE CD4+ T cell death by pyroptosis. J Leukoc Biol. (2020) 107:85–94. doi: 10.1002/JLB.4A0919-235R
15. Torres, TS, Cardoso, SW, Velasque Lde, S, Marins, LM, Oliveira, MS, Veloso, VG, et al. Aging with HIV: an overview of an urban cohort in Rio de Janeiro (Brazil) across decades of life. Braz J Infect Dis. (2013) 17:324–31. doi: 10.1016/j.bjid.2012.10.024
16. Manrique, L, Aziz, M, and Adeyemi, OM. Successful immunologic and virologic outcomes in elderly HIV-infected patients. J Acquir Immune Defic Syndr. (1999) 2010) 54:332–3. doi: 10.1097/QAI.0b013e3181d2eef1
17. Li, Y, Teng, D, Shi, X, Qin, G, Qin, Y, Quan, H, et al. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: national cross sectional study. BMJ. (2020) 369:m997. doi: 10.1136/bmj.m997
18. Althoff, KN, Gebo, KA, Moore, RD, Boyd, CM, Justice, AC, Wong, C, et al. Contributions of traditional and HIV-related risk factors on non-AIDS-defining cancer, myocardial infarction, and end-stage liver and renal diseases in adults with HIV in the USA and Canada: a collaboration of cohort studies. Lancet HIV. (2019) 6:e93–e104. doi: 10.1016/S2352-3018(18)30295-9
19. Farahani, M, Mulinder, H, Farahani, A, and Marlink, R. Prevalence and distribution of non-AIDS causes of death among HIV-infected individuals receiving antiretroviral therapy: a systematic review and meta-analysis. Int J STD AIDS. (2017) 28:636–50. doi: 10.1177/0956462416632428
20. El-Sadr, WM, Lundgren, J, Neaton, JD, Gordin, F, Abrams, D, Arduino, RC, et al. CD4+ count-guided interruption of antiretroviral treatment. N Engl J Med. (2006) 355:2283–96. doi: 10.1056/NEJMoa062360
21. van Lelyveld, SF, Gras, L, Kesselring, A, Zhang, S, De Wolf, F, Wensing, AM, et al. Long-term complications in patients with poor immunological recovery despite virological successful HAART in Dutch ATHENA cohort. AIDS (London, England). (2012) 26:465–74. doi: 10.1097/QAD.0b013e32834f32f8
22. Girometti, N, Lander, F, McOwan, A, Nwokolo, N, Boffito, M, and Whitlock, G. Rapid ART start in early HIV infection: time to viral load suppression and retention in care in a London cohort. HIV Med. (2020) 21:613–5. doi: 10.1111/hiv.12900
23. Veil, R, Poizot-Martin, I, Reynes, J, Goujard, C, Seng, R, Delobel, P, et al. Virological and immunological impact of integrase inhibitor-based regimens initiated during primary HIV-1 infection. AIDS (London, England). (2020) 34:493–500. doi: 10.1097/QAD.0000000000002447
24. Mondi, A, Pinnetti, C, Lorenzini, P, Plazzi, MM, Abbate, I, Camici, M, et al. Virological and immunological outcomes of an intensified four-drug versus a standard three-drug antiretroviral regimen, both integrase Strand transfer inhibitor-based, in primary HIV infection. Pharmaceuticals (Basel, Switzerland). (2022) 15. doi: 10.3390/ph15040403
Keywords: HIV/AIDS, inadequate immunological responders, non-AIDS related, cardiovascular disease, tumor
Citation: Fan L, Li P, Yu A, Liu D, Wang Z, Wu Y, Zhang D, Zou M and Ma P (2023) Prevalence of and prognosis for poor immunological recovery by virally suppressed and aged HIV-infected patients. Front. Med. 10:1259871. doi: 10.3389/fmed.2023.1259871
Edited by:
Daniel Diaz, National Autonomous University of Mexico, MexicoReviewed by:
Paola Di Carlo, University of Palermo, ItalySouheil-Antoine Younes, Emory University, United States
Copyright © 2023 Fan, Li, Yu, Liu, Wang, Wu, Zhang, Zou and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ping Ma, bWFwaW5ndGlhbmppbkAxNjMuY29tLmNu; Meiyin Zou, em91bWVpeWluQDEyNi5jb20=
†These authors have contributed equally to this work
 Lina Fan1†
Lina Fan1† Ping Ma
Ping Ma