
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med. , 29 August 2023
Sec. Gastroenterology
Volume 10 - 2023 | https://doi.org/10.3389/fmed.2023.1259728
Background: Helicobacter pylori (H. pylori) infection is the most important risk factor for gastric cancer. Eradication of H. pylori significantly reduces the incidence and mortality of gastric cancer. H. pylori resistance to antibiotics and a gradual decline in eradication rates are gaining more and more attention. Our study aimed to address the correlation between endoscopic manifestations and the eradication effect of H. pylori.
Methods: We retrospectively reviewed outpatients in our hospital with H. pylori infection undergoing eradication therapy from January 2022 to March 2023. Both the primary diagnosis and eradication of H. pylori after treatment were confirmed by a 13C urea breath test. Patients were treated with a proton pump inhibitor (PPI)-based quadruple therapy. Clinical characteristics and endoscopy manifestations within 7 days before or after patients were diagnosed with H. pylori infection were analyzed.
Results: From January 2022 to March 2023, a total of 323 patients were enrolled in this study. There were 138 male patients and 185 female patients. The mean age of patients was 45.62 ± 13.04 years. The H. pylori initial eradication rate was 82.0%. Univariate analysis of factors affecting H. pylori eradication showed that sex, age, and endoscopic manifestations including diffuse redness, multiple white, and flat elevated lesions, and atrophy were significantly associated with the failure of H. pylori eradication therapy. A multivariable logistic regression model analysis of these five factors showed that patients aged over 60 years with multiple white and flat elevated lesions in the endoscopic examination are significantly less likely to eradicate H. pylori with empirical quadruple therapy. On the other hand, patients with diffuse redness were significantly more likely to eradicate H. pylori infection with empirical quadruple therapy.
Conclusion: Our study shows that age over 60 years old, multiple white and flat elevated lesions in endoscopic examination are independent risk factors of initial H. pylori eradication failure with empirical quadruple therapy, while diffuse redness in endoscopic examination is a protective factor of initial H. pylori eradication failure with empirical quadruple therapy, while diffuse redness in endoscopic examination is a protective factor. For patients with these risk factors, a drug sensitivity test or H. pylori resistance gene mutation detection may be more appropriate. However, further mechanism studies or prospective studies are needed to prove our findings.
Helicobacter pylori (H. pylori) is a gram-negative microaerophilic bacterium that infects the epithelial lining of the stomach. It is one of the most prevalent bacterial infections in human beings worldwide. It is estimated that 50% of the global population is infected with H. pylori (1). Numerous researchers have discovered that H. pylori infection is directly associated with gastric diseases, including chronic gastritis, gastric and duodenal peptic ulcer, gastric adenocarcinoma, and gastric mucosa-associated lymphoid tissue (MALT) lymphoma (2, 3). In 1994, the International Agency for Research on Cancer classified H. pylori as a class I carcinogen for gastric cancer (4). Meanwhile, several large cohort studies have highlighted the importance of H. pylori eradication and shown that the eradication of H. pylori significantly decreases gastric cancer incidence with no increase in the likelihood of adverse consequences (5, 6). Thus, experts have reached a consensus that the screening and eradication of H. pylori should be adopted as a public health policy to prevent gastric cancer in high-risk populations.
Bismuth quadruple therapy (BQT) is the main empirical therapy for initial H. pylori eradication therapy in most areas. It consists of a proton pump inhibitor (PPI) or histamine-2 receptor antagonist, bismuth, and two antibiotics. Amoxicillin, clarithromycin, levofloxacin, metronidazole, furazolidone, and tetracycline are optional antibiotics. The course of treatment is usually 10 or 14 days (7–9). However, the eradication rate ranges from 77.6% to 98.0% (7, 10). Large-scale H. pylori eradication treatment and inappropriate treatment regimens have led to increasing resistance rates to multiple antibiotics, which results in a gradual decline in H. pylori eradication rates, especially in areas with high H. pylori prevalence. Currently, repeated empirical eradication of H. pylori treatment is common in clinical practice, which will result in a great waste of medical resources and an increased psychological burden on patients and their relatives. Therefore, successful eradication of H. pylori on initial treatment is very important. Nowadays, drug sensitivity tests and H. pylori resistance gene mutation detection can enable personalized, promising salvage treatments and achieve comparably high eradication rates (11). However, the drug sensitivity test for H. pylori takes a long time and is hampered by a relatively high rate of false negatives (11). Meanwhile, H. pylori resistance gene mutation detection is not easy to get access, especially in developing countries where the H. pylori infection rate is relatively higher (12). Thus, further study in distinguishing high-risk patients is needed to better customize the application of H. pylori resistance gene mutation detection and decrease the failure of H. pylori eradication. As H. pylori infection is directly associated with gastric diseases, which usually cause stomach upset, patients infected with H. pylori often underwent endoscopy examinations. Is there a correlation between the endoscopic manifestations and H. pylori eradication failure? Is it possible that we distinguish patients who have a high risk of failing the empirical BQT based on their endoscopic manifestations? To address these questions, we conducted this retrospective study. In this study, we described the clinical characteristics and endoscopic manifestations of the enrolled outpatients in our hospital with H. pylori infection undergoing eradication therapy. We also evaluate the risk factors for H. pylori eradication failure, especially the correlation between endoscopic manifestations and H. pylori eradication failure.
From January 2022 to March 2023, 323 outpatients at our hospital were enrolled. The following were the inclusion criteria: 1. Patients aged at least 18; 2. Patients underwent endoscopy examination within 7 days of being diagnosed with H. pylori infection; 3. After endoscopy examination, patients were treated with a PPI-based quadruple therapy: PPI (omeprazole 40 mg or pantoprazole 40 mg or rabeprazole 10 mg or esomeprazole 20 mg); clarithromycin (500 mg); amoxicillin (1,000 mg), and bismuth potassium citrate capsules (220 mg) each twice/day for 14 days; 4. Patients had H. pylori tests 1–3 months after the quadruple H. pylori eradication therapy; 5. Both primary diagnosis and eradication of H. pylori after therapy were confirmed by the 13C urea breath test (13C-UBT), which was recommended by both Chinese and American guidelines (7, 13). Before undergoing 13C-UBT, patients were required to stop taking antibiotics, bismuth, proton pump inhibitors, H2-receptor antagonists, or other medicines that might interfere with the result of the examination for at least 4 weeks. Clinical characteristics, including patients' age, sex, if they have clinical symptoms such as epigastric pain, nausea, or dyspepsia, and the duration of their symptoms were obtained from their medical records. We retrospectively analyzed these data. This study was approved by the Ethics Committee of Tongji Medical College, and all patient information was kept private.
Each subject was requested to swallow a pill containing 75 mg 13C urea with 20 ml of water in the morning. Exhaled air was collected in sampling tubes 30 min later. 13CO2 values were determined using a gas isotope ratio mass spectrometer, and a delta over baseline (DOB) value was used to express the difference between 30 min and baseline. The concentration of 13CO2 at 30 min that exceeded the baseline by more than 3.8 parts per thousand (>0.38%) was regarded as a positive indicator of H. pylori infection.
We selected the endoscopic manifestations of the enrolled patients as potential factors that might affect the eradication of H. pylori infection. These endoscopic manifestations included: reflux esophagitis, gastritis, peptic ulcers, and duodenitis. Because the Kyoto classification is a kind of gastritis classification that is associated with H. pylori infection (14), for the manifestation of gastritis, we selected diffuse redness, raised erosion, depressive erosion, multiple white and flat elevated lesions, and atrophy from the Kyoto classification.
Data were analyzed using SPSS statistical package version 27.0. Descriptive statistics such as percentages, means, and standard deviations were used to describe the data. The chi-square test was used to assess failure-success differences in H. pylori eradication. Multivariate analyses were performed using binary non-conditional logistic regression to identify predictors of failure of eradication using BQT. The Hosmer–Lemeshow test was checked to assess the model's fitness to conduct logistic regression. The odd's ratio with 95% confidence intervals was calculated for each of the independent variables using a P-value of < 0.05 as the level of significance.
From January 2022 to March 2023, a total of 323 patients were enrolled in this study. Their clinical characteristics are listed in Table 1. There were 138 male patients and 185 female patients. The male-to-female ratio was 1:1.34. The mean age of patients was 45.62 ± 13.04 years. The youngest patient was 18 years old, whereas the oldest was 75 years old. Most people were between 40 and 60 years old. The overall H. pylori initial eradication rate (success of therapy) was 82.0%, while 58 patients (18%) failed to eradicate H. pylori with the empirical BQT. A total of 297 (92.0%) patients had symptoms when they came to the clinic, while 26 (8.0%) patients had no symptoms. A total of 168 (56.6%) patients had clinical symptoms for no more than 6 months. A total of 129 (43.4%) patients' symptoms lasted for more than 6 months. In addition, the number and percentage of patients for each kind of endoscopic manifestation are shown in Table 1. There were 101 (31.3%) patients with diffuse redness, 97 (30%) patients with raised erosion, 50 (15.5%) patients with depressive erosion, 18 (5.6%) patients with multiple white and flat elevated lesions, 164 (50.8%) patients with atrophy, 30 (9.3%) patients with reflux esophagitis, 67 (20.7%) patients with peptic ulcer, and 54 (12.4%) patients with duodenitis.
Typical endoscopic manifestation pictures are shown in Figure 1. Univariate analysis of factors that might affect H. pylori eradication failure showed that sex, age, and endoscopic manifestations including diffuse redness, multiple white and flat elevated lesions, and atrophy were significantly associated with the failure of H. pylori eradication therapy (Table 2).
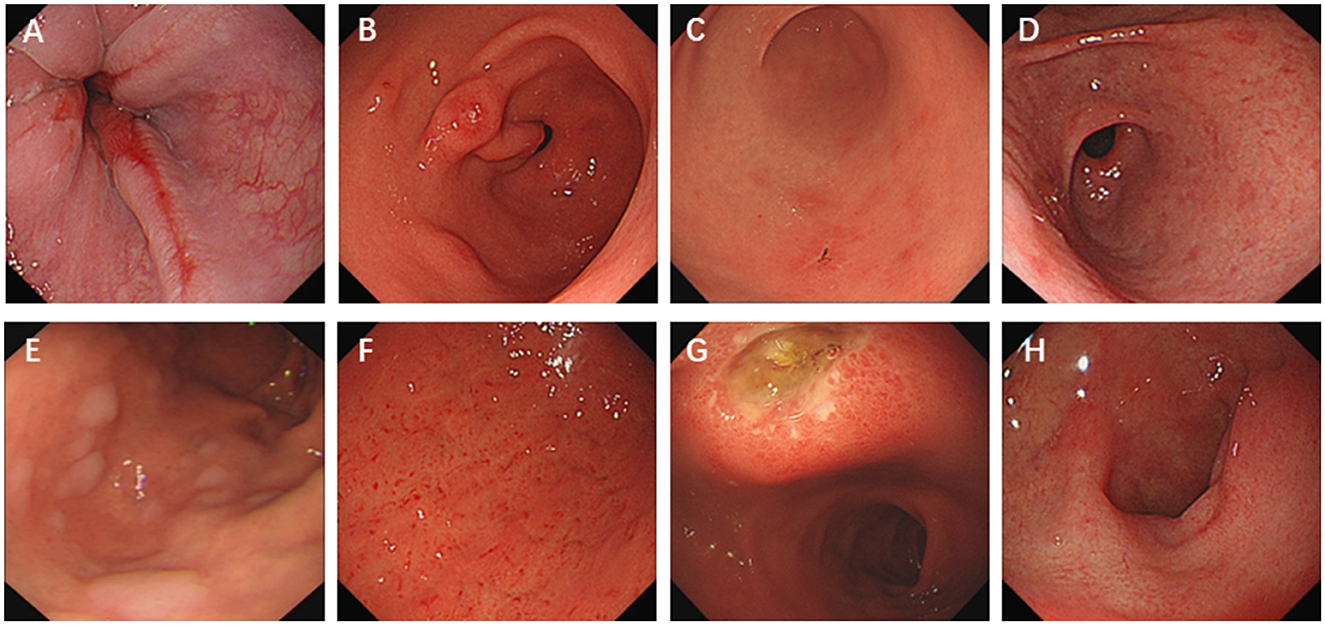
Figure 1. Typical images of endoscopic manifestations selected in this study. (A) Reflux esophagitis, gastritis, (B) raised erosion, (C) depressive erosion, (D) atrophy, (E) multiple white and flat elevated lesions, (F) diffuse redness, (G) peptic ulcer, and (H) duodenitis.
The failure rates of male and female patients were 13.0% and 21.6%, respectively (P = 0.047). The failure rate of patients who were aged more than 60 was as high as 41.4%, while the rate was 14.8% for patients who were aged not more than 60 (P < 0.001). Patients whose endoscopic findings included diffuse redness showed a failure rate of 8.9%, while the remaining patients had a significantly higher failure rate of 22.1% (P = 0.010). Patients whose endoscopic findings included multiple white and flat elevated lesions showed a failure rate of 50%, while patients who did not have multiple white and flat elevated lesions showed a significantly lower failure rate of 16.1% (P < 0.001). In addition, patients who were diagnosed with atrophy showed a failure rate of 24.4% and the remaining patients had a significantly lower failure rate of 11.3% (P = 0.002).
Logistic regression analysis was performed by the abovementioned five factors selected through univariate analysis. Results revealed that age, diffuse redness, and multiple white and flat elevated lesions were factors affecting the result of the eradication therapy. Patients aged more than 60 years were significantly less likely to eradicate H. pylori infection compared to patients aged no more than 60 years (OR: 0.348, 95% CI:0.155–0.784, p = 0.011). Those patients with multiple white and flat elevated lesions were significantly less likely to eradicate H. pylori infection with empirical quadruple therapy compared to those without multiple white and flat elevated lesions (p = 0.002). On the other hand, patients with diffuse redness were significantly more likely to eradicate H. pylori infections compared to those without diffuse redness (p = 0.049) (Table 3).
H. pylori eradication is very important in curing chronic gastritis and peptic ulcers. Population-based eradication of H. pylori is also effective in reducing the incidence of gastric adenocarcinoma and gastric MALT (7, 15). Because of the wide application of empirical BQT in the eradication therapy of H. pylori infection, together with factors such as coccoid transformation, host CYP2C19 gene polymorphisms, and inappropriate treatment regimens, a gradual decline in H. pylori eradication rates has been reported in previous studies (16, 17). Improving the eradication rate on initial treatment is critical to reduce antibiotic resistance (18). Worldwide, the initial eradication rate ranges from 77.6% to 98.0% (7, 10). The eradication rate in this study ranges from 50% to 91.1%. Patients aged more than 60 and patients with endoscopic examination showing multiple white and flat elevated lesions have lower eradication rates. While patients with endoscopic examination showing diffused redness showed the highest eradication rate (91.1%).
Our study showed that the initial eradication rate for patients over 60 years old is lower. Some studies showed that the elderly population had no significantly increased resistance to antibiotics commonly used to eradicate H. pylori such as amoxicillin and furazolidone, but their resistance to quinolones (levofloxacin) and clarithromycin had increased (13, 19). It may decrease the eradication rate among elderly people. In addition, elderly people in China usually have a lower level of education. It significantly impacts patients' adherence to a multi-drug regimen with frequent side effects, which will affect the result of the initial eradication rate. Meanwhile, the elderly population often has one or more conditional diseases at the time of treatment, so choosing the proper drugs to improve the initial eradication rate is important. Therefore, drug sensitivity test or H. pylori resistance gene mutation detection may be critical in elderly people.
Diffuse redness is a very important endoscopic manifestation in the Kyoto classification. It indicates a current infection of H. pylori and is related to active inflammation. Multiple white and flat elevated lesions are pathologically characterized by a hyperplasia of the foveolar epithelium, in which inflammatory cell infiltration is extremely low (20). Multiple white and flat elevated lesions are considered to be associated with long-term PPI use (21). In this study, these two endoscopic manifestations were associated with the initial eradication rate. Our study showed that patients with diffuse redness had a higher success eradication rate. While patients with multiple white and flat elevated lesions had a lower success eradication rate. The mechanism for this phenomenon is unknown. The possible mechanisms may relate to the characteristics of the bacteria. Unique characteristics of different H. pylori subtypes may affect its drug resistance as well as its ability to induce active inflammation. An example is when non-mucoid spiral H. pylori turned into mucoid-coccoid form, its antibiotic resistance changed at the same time (22). This study is the first study about the correlation between H. pylori eradication rate and endoscopic manifestations. More research is needed in future to explore their relations and the underlying mechanism.
There are some limitations to this study. The first limitation is that our study population is from a single medical center, and selection bias may exist. It may result in a lack of statistical reliability. A multicenter prospective study is needed to confirm the results we have found. The second limitation is that this is a retrospective analysis of clinical record data without mechanism experiments. Thus, lab experiments are also needed to reveal the mechanism underlying the phenomenon.
Our study shows that age over 60 years old, multiple white and flat elevated lesions in endoscopic examination are independent risk factors of initial H. pylori eradication failure with empirical quadruple therapy, while diffuse redness in endoscopic examination is a protective factor of initial H. pylori eradication failure with empirical quadruple therapy, while diffuse redness in the endoscopic examination is a protective factor. For patients with these risk factors, a drug sensitivity test or H. pylori resistance gene mutation detection may be more appropriate. However, further mechanism studies or prospective studies are needed to prove our findings.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving humans were approved by Ethics Committee of Tongji Medical College. The studies were conducted in accordance with the local legislation and institutional requirements. The Ethics Committee/Institutional Review Board waived the requirement of written informed consent for participation from the participants or the participants' legal guardians/next of kin because all the information of patients were kept private.
XL: Formal analysis, Resources, Writing—original draft, Writing—review and editing. HL: Formal analysis, Resources, Writing—review and editing. LH: Conceptualization, Project administration, Resources, Supervision, Writing—review and editing, Funding acquisition.
This study was funded by the National Natural Science Foundation of China (No. 82203802).
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
H. pylori, Helicobacter pylori; PPI, proton pump inhibitor; MALT, mucosa-associated lymphoid tissue lymphoma; BQT, bismuth quadruple therapy; 13C-UBT, 13C urea breath test.
1. Hooi JKY, Lai WY, Ng WK, Suen MMY, Underwood FE, Tanyingoh D, et al. Global prevalence of Helicobacter pylori infection: systematic review and meta-analysis. Gastroenterology. (2017) 153:420–9. doi: 10.1053/j.gastro.2017.04.022
2. Suerbaum S, Michetti P. Helicobacter pylori infection. N Engl J Med. (2002) 347:1175–86. doi: 10.1056/NEJMra020542
3. Ayala G, Escobedo-Hinojosa WI. de la Cruz-Herrera CF, Romero I. Exploring alternative treatments for Helicobacter pylori infection. World J Gastroenterol. (2014) 20:1450–69. doi: 10.3748/wjg.v20.i6.1450
4. Schistosomes, liver flukes and Helicobacter pylori. IARC Monogr Eval Carcinog Risks Hum. (1994) 61:1–241.
5. Pan KF, Zhang L, Gerhard M, Ma JL, Liu WD, Ulm K, et al. A large randomised controlled intervention trial to prevent gastric cancer by eradication of Helicobacter pylori in Linqu County, China: baseline results and factors affecting the eradication. Gut. (2016) 65:9–18. doi: 10.1136/gutjnl-2015-309197
6. Chiang TH, Chang WJ, Chen SL, Yen AM, Fann JC, Chiu SY, et al. Mass eradication of Helicobacter pylori to reduce gastric cancer incidence and mortality: a long-term cohort study on Matsu Islands. Gut. (2021) 70:243−50. doi: 10.1136/gutjnl-2020-322200
7. Chey WD, Leontiadis GI, Howden CW, Moss SF. ACG clinical guideline: treatment of Helicobacter pylori infection. Am J Gastroenterol. (2017) 112:212–39. doi: 10.1038/ajg.2016.563
8. Lee YC, Dore MP, Graham DY. Diagnosis and treatment of Helicobacter pylori Infection. Annu Rev Med. (2022) 73:183–95. doi: 10.1146/annurev-med-042220-020814
9. Song Z, Chen Y, Lu H, Zeng Z, Wang W, Liu X, et al. Diagnosis and treatment of Helicobacter pylori infection by physicians in China: A nationwide cross-sectional study. Helicobacter. (2022) 27:e12889. doi: 10.1111/hel.12889
10. Luther J, Higgins PD, Schoenfeld PS, Moayyedi P, Vakil N, Chey WD. Empiric quadruple vs. triple therapy for primary treatment of Helicobacter pylori infection: Systematic review and meta-analysis of efficacy and tolerability. Am J Gastroenterol. (2010) 105:65–73. doi: 10.1038/ajg.2009.508
11. Guo Z, Tian S, Wang W, Zhang Y, Li J, Lin R. Correlation analysis among genotype resistance, phenotype resistance, and eradication effect after resistance-guided quadruple therapies in refractory Helicobacter pylori infections. Front Microbiol. (2022) 13:861626. doi: 10.3389/fmicb.2022.861626
12. Cui R, Song Z, Suo B, Tian X, Xue Y, Meng L, et al. Correlation analysis among genotype resistance, phenotype resistance and eradication effect of Helicobacter pylori. Infect Drug Resist. (2021) 14:1747–56. doi: 10.2147/IDR.S305996
13. Ding SZ, Du YQ, Lu H, Wang WH, Cheng H, Chen SY, et al. Chinese consensus report on family-based helicobacter pylori infection control and management (2021 Edition). Gut. (2022) 71:238–53. doi: 10.1136/gutjnl-2021-325630
14. Toyoshima O, Nishizawa T. Kyoto classification of gastritis: advances and future perspectives in endoscopic diagnosis of gastritis. World J Gastroenterol. (2022) 28:6078–89. doi: 10.3748/wjg.v28.i43.6078
15. Wang F, Meng W, Wang B, Qiao L. Helicobacter pylori-induced gastric inflammation and gastric cancer. Cancer Lett. (2014) 345:196–202. doi: 10.1016/j.canlet.2013.08.016
16. Gebeyehu E, Nigatu D, Engidawork E. Helicobacter pylori eradication rate of standard triple therapy and factors affecting eradication rate at Bahir Dar city administration, Northwest Ethiopia: A prospective follow up study. PLoS ONE. (2019) 14:e0217645. doi: 10.1371/journal.pone.0217645
17. Xue Y, Zhou LY, Lu HP, Liu JZ. Recurrence of Helicobacter pylori infection: incidence and influential factors. Chin Med J (Engl). (2019) 132:765–71. doi: 10.1097/CM9.0000000000000146
18. Zhong Z, Zhan B, Xu B, Gao H. Emphasizing the importance of successful eradication of Helicobacter pylori on initial treatment. Am J Cancer Res. (2022) 12:1215–21.
19. Gao C, Fan YH. Effect and safety of Helicobacter pylori eradication treatment based on molecular pathologic antibiotic resistance in chinese elderly people. Infect Drug Resist. (2022) 15:3277–86. doi: 10.2147/IDR.S371113
20. Uedo N, Yamaoka R, Yao K. Multiple white flat lesions in the gastric corpus are not intestinal metaplasia. Endoscopy. (2017) 49:615–6. doi: 10.1055/s-0043-106434
21. Kim GH. Proton pump inhibitor-related gastric mucosal changes. Gut Liver. (2021) 15:646–52. doi: 10.5009/gnl20036
Keywords: Helicobacter pylori, H. pylori eradication, H. pylori resistance, endoscopic manifestation, personalized treatment
Citation: Luo X, Li H and He L (2023) Correlation analysis of endoscopic manifestations and eradication effect of Helicobacter pylori. Front. Med. 10:1259728. doi: 10.3389/fmed.2023.1259728
Received: 16 July 2023; Accepted: 08 August 2023;
Published: 29 August 2023.
Edited by:
Jinhang Gao, Sichuan University, ChinaCopyright © 2023 Luo, Li and He. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Li He, TGlIZTE5ODkwM0BvdXRsb29rLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.